ABSTRACT
Our prospective case series evaluates the clinical feature, histopathological picture, and treatment of benign eyelid lesions in a tertiary referral setting. Participants were first nine patients referred to the author with unilateral eyelid swelling. Main outcome measures were clinical features, histopathological picture, and response to surgical intervention. Benign eyelid lesions in our case series were epidermal inclusion cyst, giant conjunctival inclusion cyst, epidermoid cyst, dermoid cyst, intradermal nevus, dermal nevus, apocrine hidrocystoma, capillary hemangioma, and lobular capillary hemangioma. The histopathological diagnosis of eight lesions were consistent with their respective clinical diagnosis, while one lesion was misdiagnosed. Surgical excision was done in all cases. One case underwent revision surgery for complication. This series highlights the importance of achieving higher diagnostic accuracy with thorough knowledge of clinical features and subsequent confirmation with histopathological analysis.
Keywords: Benign, eyelid, lesions, periocular
Introduction
Primary healthcare settings commonly see patients with eyelid lesions. Patient outcomes can be improved if lesions are diagnosed accurately and are promptly referred to an ophthalmologist for further management.
A wide spectrum of lesions can arise from the eyelid because various skin appendages are present in it.[1] Skin, subcutaneous tissue including its adnexa, striated muscle, tarsus with embedded meibomian glands, and the palpebral conjunctiva are layers of the eyelid. Both benign and malignant tumors can originate from any of these eyelid layers.[2] Although it is known that majority of eyelid lesions are benign, yet ideally all clinically benign-appearing eyelid lesions should undergo histopathological analysis to rule out malignancy.[3] Thorough knowledge of clinical features and subsequent confirmation with histopathological examination (HPE) aids in the early detection of tumors, more so in masquerade syndromes, and also in reinforcing an ophthalmologist’s clinical diagnostic acumen.[4]
We report on our experience with the management of these benign eyelid lesions at a tertiary referral setting.
Case Descriptions
Case 1
Epidermal inclusion cysts (epidermoid cysts) usually present as a smooth round or oval dome-shaped elevation.[2] The cystic space contains keratin and it is lined by keratinized stratified squamous epithelium. It enlarges progressively and may rupture with reactive inflammation around it. In our case, excision was followed by eyelid reconstruction as the size of the lesion was full-thickness and large enough to encompass more than one-third but less than 1/2 of eyelid width [Figure 1a1 and 1a2].
Figure 1.
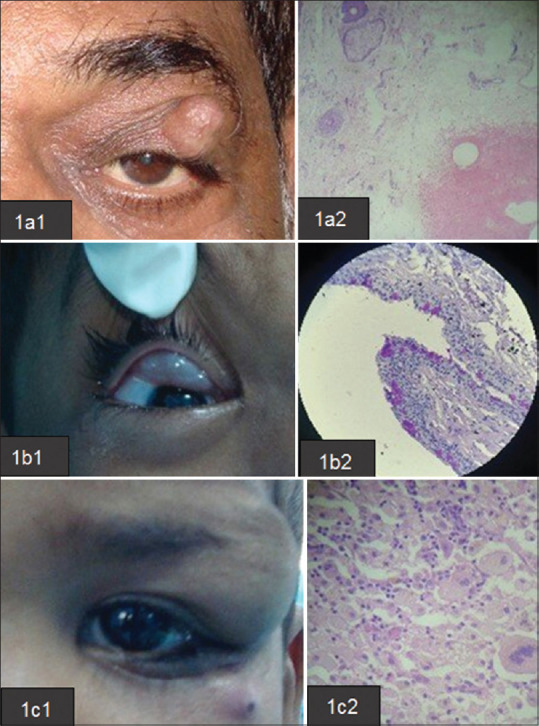
CASE 1: 1a1: Epidermal inclusion cyst; 1a2: HPE section shows cyst lined by squamous epithelium with granular layer and contains keratinous debris. CASE 2: 1b1: Giant conjunctival inclusion cyst; 1b2: HPE section shows cystic lumen lined by stratified cuboidal epithelium with focal flattened epithelium and PAS + goblet cells. CASE 3: 1c1: Epidermoid cyst; 1c2: HPE section shows cyst wall lined by keratinized stratified squamous epithelium with granular layer. Keratin debris are seen. Lymphoplasmacytic inflammation seen. Inflammatory and foreign body giant cell noted
Case 2
Giant conjunctival inclusion cyst is an uncommon adnexal lesion in children.[5] In our case, it is progressively enlarging, well-circumscribed, soft on palpation, with a slight blue color of the underlying conjunctival surface, and superomedially located in the upper eyelid [Figure 1b1 and 1b2]. It was causing mechanical ptosis. The content of fluid is clear. It was excised entirely by a modified noose technique, although a rupture occurred during dissection. Mechanical ptosis was corrected, and no recurrence was seen till the last follow-up.
Case 3 and case 4
Epidermoid/dermoid cyst is the most common cystic orbital lesion seen in children.[6] It is a choristoma, wherein the surface ectoderm gets entrapped. A dermoid cyst clinically appears as an eyelid tumor as a contiguous extension to an orbital lesion. The most common location is superotemporal, in relation to frontozygomatic suture. Both cases in our series presented to us in the fourth year of life as periorbital painless swelling along the orbital rim, which was noticed by parents in the first year only [Figures 1c1, 1c2 and 2a1, 2a2]. On computed tomography scans of orbit, both cases showed cyst content suggestive of fat based on Hounsfield No. The bone window showed no adjacent bony changes. In-toto excision of the cyst was done using a lid crease incision, with no complication in the post-op period.
Figure 2.
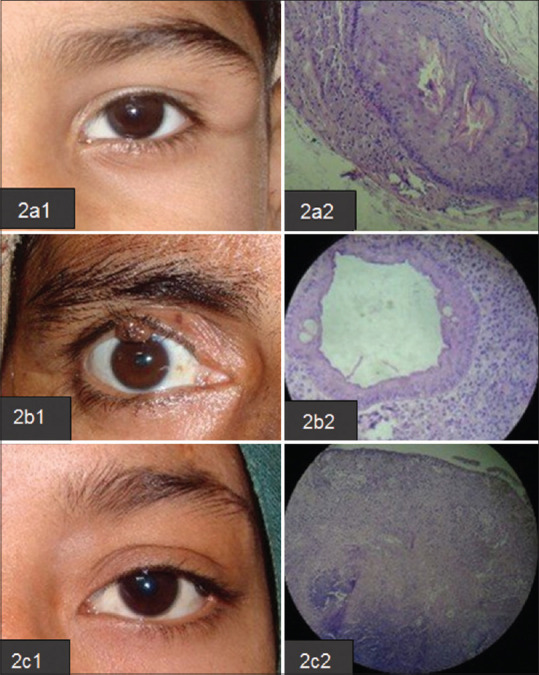
CASE 4: 2a1: Dermoid cyst; 2a2: HPE Section shows cyst wall lined by keratinized stratified squamous epithelium with granular layer. Keratin debris are seen. CASE 5: 2b1: Intradermal nevus; 2b2: HPE Section shows melanocytes in the dermis just below epidermis. Melanocytes are arranged in small symmetrical nests. Melanocytes mature with depth. Intranuclear pseudoinclusion seen. No mitotic activity seen. CASE 6: 2c1: Dermal nevus; 2c2: HPE Section shows nests of nevus cells with melanin pigmentation in the upper dermis
Case 5 and case 6
Nevus of the eyelid is characterized as a common benign melanocytic lesion.[2] These are a heterogeneous group of lesions, presenting with a wide variety of clinical and histological pictures. A type of intradermal nevus presents a homogeneous globular pattern. These globules may be arranged in a cobblestone pattern. The intradermal nevus, the most benign type of nevus, is known to transform into melanoma very rarely. In our series, both acquired types of nevus cases underwent shave excision with no recurrence [Figures 2b1, 2b2 and 2c1, 2c2].
Case 7
Apocrine hidrocystoma is a retention cyst. Its usual appearance is as a solitary translucent cystic nodule. It is located at the eyelid margin in adults. A blocked excretory duct of Moll’s gland is its origin. It has a very thin wall and contains clear or milky fluid.[7] Multiple lesions can be seen infrequently. Marsupialization of the cyst was done. No recurrence was seen till the last follow-up in our case [Figure 3a1 and 3a2].
Figure 3.
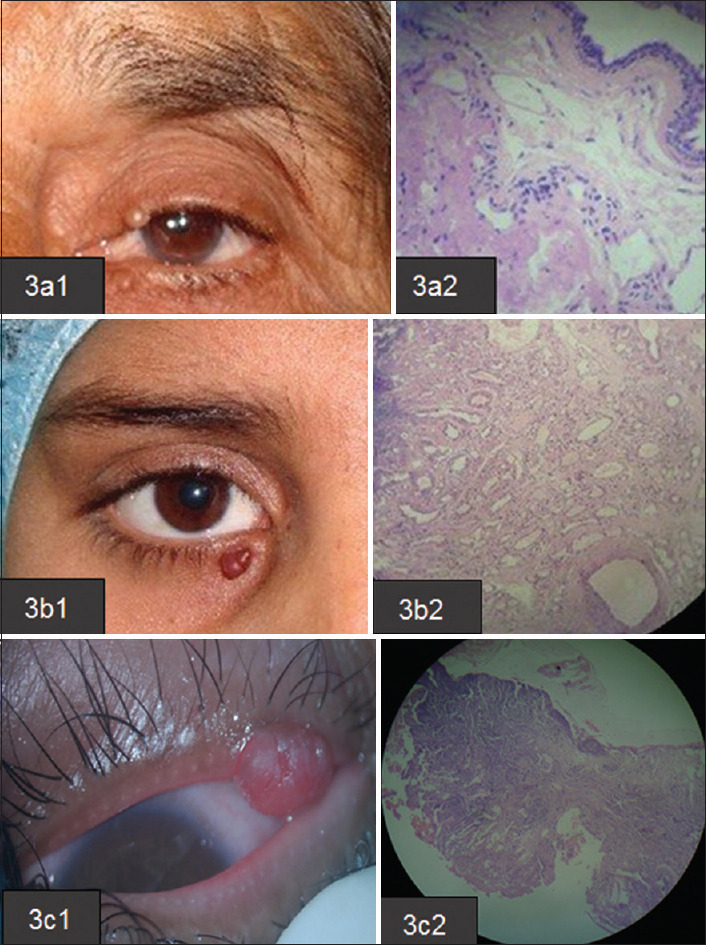
CASE 7: 3a1: Apocrine hidrocystoma; 3a2: HPE Section shows sub epithelial unilocular cyst. Cyst is lined by double layer of epithelial cells. Inner lining consists of cuboidal to low columnar cells with eosinophilic cytoplasm and focal apical snouting. CASE 8: 3b1: Capillary hemangioma; 3b2: HPE Section shows fibrocollagenous tissue lined by flattened keratinized stratified squamous epithelium. Subepithelium shows lobules of capillary sized vascular channels lined by single layer of flattened endothelial cells. Few large vessels are also seen in papillary dermis. Mild degree of lymphocytic inflammation is noted. CASE 9: 3c1: Lobular capillary hemangioma; 3c2: H and E stained section shows few polypoidal structure lined by stratified squamous epithelium. The sub-epithelial area shows lobular pattern of vascular proliferation separated by bands of connective tissue. The stroma contains scattered spindle cells and showing edema. Granulation tissue like area and focal areas of necrosis are also seen
Case 8
Capillary hemangioma is the most common benign vascular tumor of the eyelid in childhood.[8] It is a congenital hamartomatous lesion. The lesion size is variable. Our case is a superficial variant, localized to the epidermis and dermis. It is elevated, soft, reddish-purple colored, with small surface invaginations like a strawberry nevus.[2] Our case was small, localized, and amenable to excision with meticulous hemostasis [Figure 3b1 and 3b2]. The lesion was transected utilizing electrocautery.
Case 9
Pyogenic granuloma or lobular capillary hemangioma is a common vascular lesion of skin and mucous membranes in infancy and childhood.[9] On appearance, it is solitary, strawberry-like vegetation of exuberant granulation tissue, and presented the lobules of dilated and congested capillaries separated by fibrotic stroma. There is history of episodic bleeding from lesion in this case. Lobular capillary hemangioma can occasionally be confused with hemangioma. The characteristic differentiating pattern seen histologically is lobular arrangement of capillaries within the deep portion of the lesion. It was treated with tangential excision and cautery [Figure 3c1 and 3c2]. No recurrence was seen in follow up period.
Discussion
In our case series, nine patients presented with complaints of swelling or mass in either eyelid. The age range at presentation was 4-60 years. There were five females and four males. The left eye was involved in five of the cases, and the right eye in four cases. The upper lid was the most common site (n = 7) followed by the lower lid (n = 2) [Table 1].
Table 1.
Demographic and surgical intervention details of our case series
| Clinical details of the cases | Age | Sex | Laterality | Location | Diagnosis | Treatment | Follow-up (Months) | Improvement |
|---|---|---|---|---|---|---|---|---|
| Case 1 | 50 years | M | L | Upper eyelid | Epidermal inclusion cyst | Excision with eyelid reconstruction | 3 | Yes |
| Case 2 | 4 years | M | R | Upper palpebral conjunctiva | Giant conjunctival inclusion cyst | Excision | 1.5 | Yes |
| Case 3 | 4 years | M | L | Upper eyelid | Epidermoid cyst | In-toto excision | 1 | Yes |
| Case 4 | 4 years | M | L | Upper eyelid | Dermoid cyst | In-toto excision | 1.5 | Yes |
| Case 5 | 32 years | F | R | Upper eyelidmargin | Intradermal nevus | Shave excision | 1 | Yes |
| Case 6 | 17 years | F | L | Upper eyelid | Dermal nevus | Shave excision | Seen once | Yes |
| Case 7 | 60 years | F | L | Upper eyelid | Apocrine hidrocystoma | Marsupialization of the cyst | Seen once | Yes |
| Case 8 | 14 years | F | R | Lower eyelid | Capillary hemangioma | Excision with meticulous hemostasis | Seen once | Yes |
| Case 9 | 32 years | F | R | Lower eyelid | Lobular capillary hemangioma | Tangential excision and cautery | Seen once | Yes |
All nine cases were of benign origin [Table 2]. This is consistent with the findings of a study by Banerjee et al.,[1] where the frequency of benign eyelid lesions was found to be far more than malignant ones.
Table 2.
Eyelid lesions in our case series as per the WHO histological classification
| WHO histological classification | Type | Category | Lesions in our Case series |
|---|---|---|---|
| Case1 | Benign | Adnexal tumors | Epidermal inclusion cyst |
| Case 2 | Benign | Adnexal tumors | Giant conjunctival inclusion cyst |
| Case 3 | Benign | Adnexal tumors | Epidermoid cyst |
| Case 4 | Benign | Stromal tumors | Dermoid cyst |
| Case 5 | Benign | Epidermal tumors | Intradermal nevus |
| Case 6 | Benign | Epidermal tumors | Dermal nevus |
| Case 7 | Benign | Adnexal tumors | Apocrine hidrocystoma |
| Case 8 | Benign | Stromal tumors | Capillary hemangioma |
| Case 9 | Benign | Inflammatory andinfectious lesionsthat simulateneoplasms | Lobular capillary hemangioma |
Nevus (2 in no) was the most common benign lesion in our series. While a large study by Al-Faky et al.[4] shows sweat gland hidrocystoma to be the most common benign eyelid lesion due to characteristic dry climate.
In our series, the histopathological diagnosis of eight lesions was consistent with their respective clinical diagnosis, while one lesion, epidermal inclusion cyst, was misdiagnosed. However, all clinically diagnosed benign lesions were proven benign on histopathological analysis as well. While a large study conducted by Kersten et al.[3] revealed 13 cases to be malignant, and three to be premalignant on HPE out of a total of 692 clinically thought benign lesions.
In our series, all cases underwent surgical intervention. No case showed any recurrence during follow-up.
A repeat surgery was done in the case of an epidermal inclusion cyst for wound dehiscence.
Robb et al.[5] reported a similar case to our giant conjunctival inclusion cyst, although characteristic PAS+ goblet cells were absent in their histopathological analysis.
Pushker et al.[6] reported that most of the periorbital cysts were superotemporally located, in relation to frontozygomatic suture. They also noted a male preponderance. On histopathology, 25% of cases in their study showed associated chronic inflammation. Both of our cases were male children, and lesions superotemporally located, similar to the findings of their study. Also, the HPE of our case 3 diagnosed as an epidermoid cyst, which was greater than 1 cm in dimension, showed chronic inflammatory cells.
Banerjee et al.[1] reported nevus as the most common benign neoplastic lesion, similar to the findings of our case series. Al-Faky et al.[4] reported a clinically diagnosed lesion of nevus to be a basal cell papilloma, which is known to mimic other benign and malignant lesions. Also, junctional nevus, a variant of nevus, is known to have malignant potential. These findings emphasized the role of HPE in each case.
In a study by Dailey et al.,[10] the use of intralesional injection of trichloroacetic acid for large or confluent lesions in cases of hidrocystomas has been proved useful in contrast to our surgical method of intervention.
Haik et al.[8] have reported that females are more often affected than males with capillary hemangioma. The female-to-male ratio is 3:2. They have documented transection of small superficial variants with electrocautery. Our case also is a female child. Our mode of intervention was also similar although surgical excision is not the preferred mode of treatment for usual cases of capillary hemangiomas.
In a study by Patrice et al.,[9] none of the 149 lesions of lobular capillary hemangioma treated by full-thickness excision and linear closure recurred. However, the recurrence rate was 43.5% for tangential excision and cautery or cautery alone, a different outcome than ours.
Benign periocular lid lesions form a significant proportion of referrals to an oculoplastic service by primary health care givers. Streamlining these referrals without compromising patient safety can be achieved by enhancing familiarity with their clinical features and diagnosis by general practitioners.
Conclusion
Eyelids with their various histological elements can develop a wide range of lesions. Benign eyelid lesions occur more frequently than malignant ones. Benign epithelial lesions, cystic lesions, and melanocytic lesions are very common. Nevus is the most common lesion in our case series. Although the clinical diagnosis appears to be simple, diagnosing all benign eyelid lesions accurately, clinically alone, is not feasible. Therefore, histopathologic confirmation of all excised lesions is advised.
Declaration of patient’s consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Funding Statement
Nil
References
- 1.Banerjee P, Koka K, Alam MS, Subramanian N, Biswas J, Krishnakumar S, et al. The spectrum and clinicopathological correlation of eyelid lesions: Twenty years'experience at a tertiary eye care center in South India. Indian J Ophthalmol. 2022;70:43–50. doi: 10.4103/ijo.IJO_428_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pe'er J. Pathology of eyelid tumors. Indian J Ophthalmol. 2016;64:177–90. doi: 10.4103/0301-4738.181752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kersten RC, Ewing-Chow D, Kulwin DR, Gallon M. Accuracy of clinical diagnosis of cutaneous eyelid lesions. Ophthalmology. 1997;104:479–84. doi: 10.1016/s0161-6420(97)30288-7. [DOI] [PubMed] [Google Scholar]
- 4.Al-Faky YH. Epidemiology of benign eyelid lesions in patients presenting to a teaching hospital. Saudi J Ophthalmol. 2012;26:211–6. doi: 10.1016/j.sjopt.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robb RM, Elliott AT, Robson CD. Developmental conjunctival cyst of the eyelid in a child. J AAPOS. 2012;16:196–8. doi: 10.1016/j.jaapos.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Pushker N, Meel R, Kumar A, Kashyap S, Sen S, Bajaj MS. Orbital and periorbital dermoid/epidermoid cyst: A series of 280 cases and a brief review. Can J Ophthalmol. 2020;55:167–71. doi: 10.1016/j.jcjo.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Jakobiec FA, Zakka FR. A reappraisal of eyelid eccrine and apocrine hidrocystomas: Microanatomic and immunohistochemical studies of 40 lesions. Am J Ophthalmol. 2011;151:358–74. doi: 10.1016/j.ajo.2010.08.028. [DOI] [PubMed] [Google Scholar]
- 8.Haik BG, Karcioglu ZA, Gordon RA, Pechous BP. Capillary hemangioma (infantile periocular hemangioma) Surv Ophthalmol. 1994;38:399–426. doi: 10.1016/0039-6257(94)90172-4. [DOI] [PubMed] [Google Scholar]
- 9.Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): A clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267–76. doi: 10.1111/j.1525-1470.1991.tb00931.x. [DOI] [PubMed] [Google Scholar]
- 10.Dailey RA, Saulny SM, Tower RN. Treatment of multiple apocrine hidrocystomas with trichloroacetic acid. Ophthal Plast Reconstr Surg. 2005;21:148–50. doi: 10.1097/01.iop.0000155509.54813.93. [DOI] [PubMed] [Google Scholar]


