ABSTRACT
Introduction:
The ST population, residing in isolated, underdeveloped areas, faces significant health disparities compared to non-tribal communities. In particular, the lack of mental health infrastructure in these regions exacerbates their health challenges. Tribal communities possess distinct cultural beliefs surrounding health and illness, yet scant information exists regarding their physical and mental well-being. In addition, limited access to mental health services prevails, and many tribal individuals opt for traditional healing methods.
Methodology:
This study is part of the “Tele-mentoring for Rural Health Organizers of Chhattisgarh (TORENT)” project, which aims to equip rural health organizers and community health officers (CHOs) with training to screen, identify, counsel, refer, and follow up with community members facing mental health issues.
Results:
Covering 27 districts in Chhattisgarh, this study enlisted trained CHOs to employ the MERIT tool for mental health screenings. Among the tribal population, the study unveiled elevated rates of tobacco and alcohol use, anxiety, depression, hallucinations, and substance use disorders. Challenges in seeking professional help were widespread, driven by transportation difficulties and limited awareness. Field visits (77%) played a pivotal role in identifying cases, alongside self-referrals and referrals by Mitanin or ASHA workers. Notably, a significant proportion had a family history of alcohol use, with a preference for a locally brewed liquor called Mahua.
Discussion:
This study provides vital insights into the mental health status of Chhattisgarh’s tribal populations. It underscores their socioeconomic challenges, high prevalence of substance use disorders, and barriers to accessing mental health services. The study highlights the importance of delivering mental health care within tribal communities, emphasizing the engagement of locally available primary care health workers. Furthermore, it advocates for an integrated approach that acknowledges the role of faith healers in tribal communities’ mental health care.
Keywords: Challenges, indigenous population, mental health, solutions
Introduction
The scheduled tribes (ST) population is a marginalized community living in relatively socially isolated areas with poorer health indices than similar non-tribal populations.[1] This community has poor health infrastructure and even fewer mental health resources, and the situation is worse compared to other communities living in similar areas. There is scarce information available about the physical and mental health of tribal or “Adivasi” people.[2] They also have very minimal access to mental health services and information. The tribal people have unique cultural beliefs and practices about health and illness, which influence their health-seeking behavior. They often rely on traditional methods of healing, such as herbs, faith healing, and rituals, rather than modern medicine.[3]
Chhattisgarh is a state in central India that has a large tribal population. According to the 2011 census, approximately 31% of the people in Chhattisgarh belong to one of the 42 scheduled tribes recognized by the government. These tribes have their own culture, language, and traditions, but they also face many challenges and disadvantages in terms of health, education, and development. One of the major issues that affects the tribal population is mental health.[4] The National Mental Health Survey (NMHS) 2016 found that Chhattisgarh has a higher prevalence of mental disorders than the national average. The study estimated that 11.7% of the people in Chhattisgarh have some form of mental disorder, compared to 10.6% at the national level.[5] Chhattisgarh’s most common mental disorders (CMDs) are depression, anxiety, and substance use disorders. Substance use disorder is especially prevalent among the tribal population as they often consume alcohol and tobacco as part of their cultural practices.[6] However, the availability and accessibility of mental health services in Chhattisgarh are very poor. There is only one mental hospital in the state, located in Bilaspur, far from many tribal areas. There is also a lack of trained mental health professionals and awareness programs in the state.[7] Many tribal people do not seek help for their mental health problems due to stigma, lack of knowledge, or preference for traditional healing methods.
One of the challenges in addressing the mental health needs of the tribal population is the lack of adequate data and research on their health status and problems. There is a wide gap between the availability and accessibility of mental health services for tribal and non-tribal people in Chhattisgarh. Many studies have shown that tribal people have lower awareness, knowledge, and utilization of mental health services than non-tribal people.[8] Moreover, there is a misconception that tribal people are less prone to non-communicable diseases such as diabetes, depression, anxiety, and substance abuse than non-tribal people.[9,10] However, this is not true as many community-based studies have revealed that approximately 10% of tribal people suffer from CMDs such as substance abuse, depression, suicide, anxiety, and somatic complaints.[2,11,12] These CMDs can significantly impact the quality of life, productivity, and social functioning of tribal people. Therefore, there is an urgent need to conduct more research and generate more evidence on the mental health issues and needs of the tribal population in India.
Several studies have suggested empowering mental health services at all levels; specifically, primary health care centers should have the necessary systems and resources to deliver such services. These include staff training, task shifting, availability of psychotropic medications, provision of basic counseling services, and a clear referral system to the next level of care where specialized mental health services can be accessed by those who need them.[11,12]
Improving the health of marginalized and disempowered communities requires more than just increasing the number of health facilities. It also necessitates more coordinated efforts at the grassroots level to reach out to the population often neglected and underserved by the existing health system. One of the key strategies for the effective implementation of mental health services across different segments of society is to train the local workforce and volunteers who work in villages and subcenters, and who have a better understanding of the cultural and contextual factors that influence the mental health needs and behaviors of the community. To effectively address this treatment gap, upon the request of the Government of Chhattisgarh, the project for the rural health organizers (RHOs) and community health officers (CHOs) was undertaken for the early identification of psychiatric illness and reinforcing the referral and follow-up network closest to the community called as “Tele-mentoring for Rural health organizers of Chhattisgarh” aka TORENT. This paper highlights the status of mental health in the tribal population of Chhattisgarh. This research study focuses on the tribal population data collected by CHOs as part of the TORENT project.
Methodology
Study design
The TORENT project, where RHOs and CHOs are trained to screen, identify, counsel, refer, and follow up persons with mental health concerns in the community, covers the overall population, specifically people residing in rural and tribal/remote areas.
It is a first of its kind to train two different health cadres (i.e., RHOs and CHOs). This ambitious training program includes multiphase training where the participants are trained in hybrid mode (online followed by offline). The training module offers 18 online and 12 in-person hours for CHOs and 10 online hours for RHOs. Training for the CHOs included basic mental health. The online training consisted of nine sessions for 9 continuous weeks (one session per week) followed by offline/physical training for 2 days (6 hours each).
Each online session was for 2 hours, 1 hour for the clinical presentation of the topic and another for the case discussion and sharing self-experience by the participants. A pre- and post-assessment including questions on knowledge, attitude, and clinical practices of mental health was assessed via Google Forms before and after the training. The unique features of training are screening of mentally ill patients, continuous hand-holding, and awareness activities in the community on mental health and illness.
Screening tool
Mental Health Screening and Counselling Tool (MERIT) is a validated tool and serves as a valuable resource in mental health assessment. This tool involves a succinct set of 11 categorical questions designed to assist RHOs and CHOs in effectively screening individuals for various mental health conditions. These conditions encompass depression, anxiety, somatization, psychosis, alcohol and tobacco use disorders, and suicidality. One of the key advantages of MERIT is its user-friendly nature. A streamlined structure empowers healthcare professionals to swiftly administer the screening process. A noteworthy feature is its efficiency: the entire screening procedure can be completed within just 5 minutes per person. MERIT amalgamates simplicity and effectiveness, offering a practical means for RHOs and CHOs to carry out comprehensive mental health screenings.[13]
Settings and sample
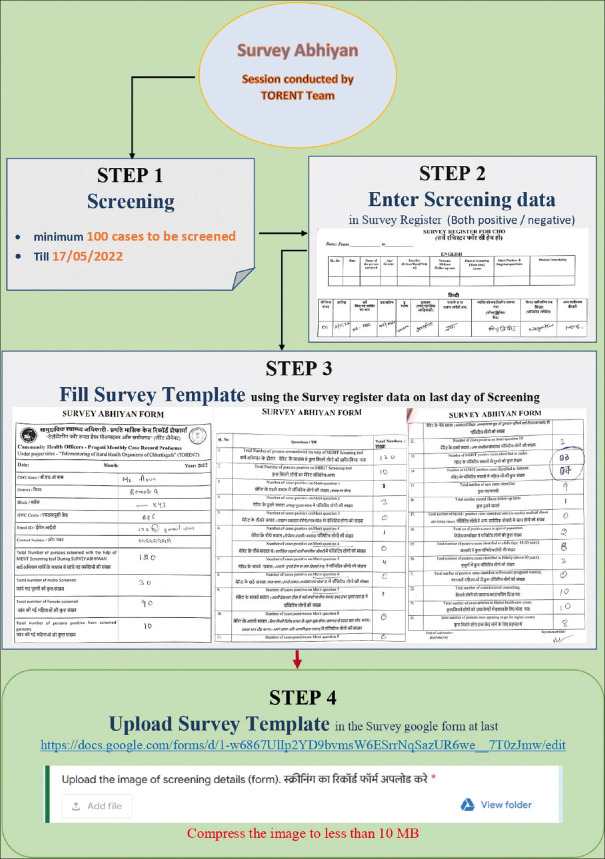
The data collection process utilized a purposive sampling technique. The initiative, known as “MERIT SURVEY MAHABHIYAN,” aimed to enrich the MERIT screening conducted by CHOs in Chhattisgarh. This comprehensive survey spanned 10 consecutive days, from May 1, 2022, to May 10, 2022, encompassing 27 districts, and was carried out by 1063 CHOs. The survey was conducted by CHOs who had undergone online and on-site training. These trained CHOs executed the survey within the community, and in primary health centers (PHCs), catering to Chhattisgarh’s general population. In addition to training, a demo video explaining the detailed procedure of MERIT SURVEY ABHIYAN was developed and circulated in the official WhatsApp groups of CHOs to ensure proper implementation of the procedure and minimize the occurrence of errors, as shown in Figure 1. The tool employed for the survey was the MERIT screening tool. A collaborative video consultation addressed behavioral issues detected through the MERIT screening. A team of mental health experts, comprising psychiatrists, psychiatric nurses, and nursing informatics specialists, conducted virtual sessions. The goal was to assist individuals flagged by CHOs for potential mental health concerns. Throughout the survey period, a total of 40,440 screenings were administered. From these screenings, 4327 cases were positive for diverse mental disorders. Notably, among the identified cases, 183 originated from tribal communities, as discerned by the CHOs. In addition to the MERIT screener questions, the survey also encompassed inquiries about referral points, nearby healthcare services offering mental health support, and reasons underlying reluctance to seek professional help in cases of mental illness. The focal point of this research study centered on the tribal population data, a facet gathered by CHOs as part of the broader TORENT project.
Figure 1.
A flowchart explaining the procedure of MERIT SURVEY ABHIYAN
Results
The sociodemographic characteristics of the 183 tribal cases are presented in Table 1. The mean (SD) age of the cases was 40.35 (16.08) years, with almost equal proportions of males (50.3%) and females (49.7%). Most of the cases were married (62.8%), lived in nuclear families (63.4%), and had an income of less than or equal to INR 10,000 per month (52.5%). The majority of the cases resided in kutcha houses (60.7%) made of mud, straw, or other low-quality materials.
Table 1.
Representing sociodemographic details of tribal population/cases
| Variables | Frequencies/Percentage | |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 40.35 (16.08) | |
| Gender | ||
| Male | 92 | 50.3 |
| Female | 91 | 49.7 |
| Marital status | ||
| Single | 49 | 26.8 |
| Married | 115 | 62.8 |
| Widow/Separated/Divorced | 19 | 10.4 |
| Type of family | ||
| Nuclear family | 116 | 63.4 |
| Joint family | 67 | 36.6 |
| Annual income | ||
| ≤10,000 | 96 | 52.5 |
| 11,000–25,000 | 43 | 23.5 |
| 26,000–50,000 | 25 | 13.7 |
| 51,000–75,000 | 06 | 3.3 |
| 76,000–1,00,000 | 04 | 2.2 |
| Above 1 lakh | 09 | 4.9 |
| Number of earning members in the family | ||
| No earning member | 27 | 14.8 |
| 1 earning member | 91 | 49.7 |
| 2 earning members | 65 | 35.5 |
| Type of house | ||
| Kutcha house | 111 | 60.7 |
| Semi pucca house | 53 | 29.0 |
| Pucca house | 19 | 10.4 |
| Family history of psychiatric illness | ||
| Yes | 12 | 6.6 |
| No | 171 | 93.4 |
| Family history of suicide | ||
| Yes | 4 | 2.2 |
| No | 179 | 97.8 |
| Family history of substance use | ||
| Yes | 145 | 79.2 |
| No | 38 | 20.8 |
| What kind of substance use in the family history | ||
| Alcohol | 67 | 36.6 |
| Tobacco | 36 | 19.7 |
| Both | 42 | 23 |
| Distance of the nearest health center with mental health facilities | ||
| <10 km | 41 | 22.4 |
| 11–30 km | 63 | 34.4 |
| 31–50 km | 45 | 24.6 |
| >50 km | 34 | 18.6 |
| Number of cases agreed to visit the higher center | ||
| Yes | 100 | 54.6 |
| No | 83 | 45.4 |
| The case was seen/contacted at | ||
| Field visit | 77 | 41.8 |
| HWC (self-visit with physical illness) | 60 | 32.8 |
| HWC (self-visit without physical illness) | 11 | 6.0 |
| Referred by ASHA/Mitanin | 35 | 19.1 |
| Visited faith healer | ||
| Yes | 109 | 59.7 |
| No | 74 | 40.2 |
| Taken any treatment for psychiatric illness | ||
| Yes | 56 | 30.4 |
| No | 114 | 62.0 |
| Taken but left | 13 | 7.1 |
Only 6.6% of the cases reported a positive family history of psychiatric illness, while 79.2% reported a family history of substance use, mainly alcohol (36.6%), tobacco (19.7%), or both (23%). Furthermore, 2.2% of the total reported cases had a family history of suicide. The distance from the nearest health center with mental health facilities varied from less than 10 km for 22.4% of the cases to more than 50 km for 18.6%, as shown in Figure 2. More than half of the cases (54.6%) agreed to visit the higher health center if needed, while 45.4% were unwilling to do so. The mode of contact for the cases was field visit for 41.8%, self-visit with physical illness for 32.8%, referral by ASHA/Mitanin for 19.1%, and self-visit without physical illness for 6%.
Figure 2.
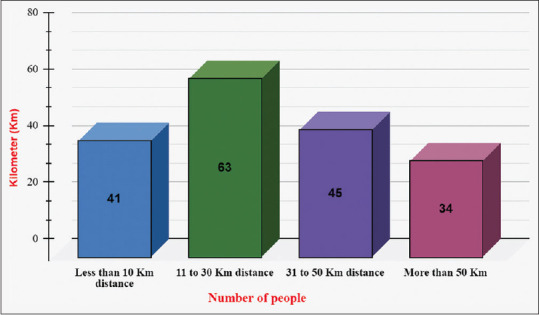
Distance of the nearest health centers with mental health facilities
The study examined the prevalence and patterns of psychiatric symptoms and substance use among 183 tribal cases in Chhattisgarh, as shown in Figure 3. The results showed that tobacco use was the most common symptom (86%), followed by alcohol use (71%). Other symptoms included anxiety (63%), depression (52%), hallucinations (46%), suspiciousness (36%), wandering/poor self-care (40%), excess happiness (32%), and suicide attempts (4%). The majority of the alcohol users consumed Indian-made liquor (Mahua) (109 cases), while only a few reported Indian-made foreign liquor (6 cases). The study also explored the barriers to seeking professional help for mental health problems among the tribal cases, as shown in Figure 4. The main reasons reported were transportation difficulties (80%), lack of insight, poor support (45%), loss of income (39%), financial constraints (35%), family disinterest (27%), living alone (26%), acute symptoms (17%), and no perceived dysfunction (15%).
Figure 3.
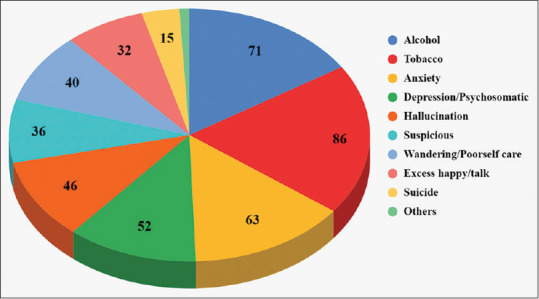
Description of psychiatric symptoms in the tribal population of Chhattisgarh
Figure 4.
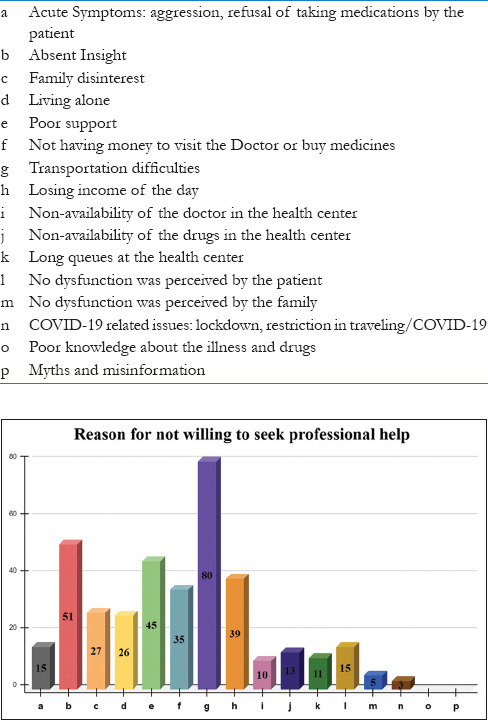
Description of various reasons given by the tribal population of Chhattisgarh for not being willing to seek professional help
Discussion
The study involves an innovative strategy of utilizing a digitally driven project to reach a marginalized population and explore the mental health status within tribal communities While previous research has predominantly focused on physical health problems excluding mental health, especially in various regions of India, this particular study, to the best of our knowledge, is among the first investigations to highlight issues associated with mental health within tribal populations of Chhattisgarh[3,14] that lack adequate access to services. As reflected in the study results presented in the table, the socioeconomic status of the cases revealed that most of them lived in kutcha houses, had an annual family income of less than INR 10,000, and had only one earning member in the family. Moreover, 27 cases (14.7%) had no earning member in the family. These sociodemographic factors may reflect the lower socioeconomic conditions of the tribal population and their impact on mental health. The National Mental Health Survey of India (NMHS-16) report has highlighted the high poverty headcount ratio in the state of Chhattisgarh.[7] According to the Oxford Poverty and Human Development Initiative Report, 70% of the total poor in Chhattisgarh are concentrated in the Bastar division, which is the main tribal belt of the state.[15] This observation suggests that lower socioeconomic conditions among the tribal population may contribute to their mental health issues. While previous research has predominantly focused on physical health problems excluding mental health, especially in various regions of India, this particular study, to the best of our awareness, is among the first investigations to highlight issues associated with mental well-being within tribal populations.[15]
The study sample comprised 183 tribal cases from rural and forest areas in Chhattisgarh. The mean age of the sample was 40.35 (SD = 16.08) years. This finding aligns with the outcomes of the NMHS-16 report, which identified the 4th and 5th decades of life as having the highest prevalence of psychiatric disorders. Contrary to the NMHS report’s finding that indicated more than a twofold prevalence of psychiatric disorders among males compared to females in the general population, no disparity in psychiatric morbidity between genders was observed in the current study.[16]
The study found that most of the cases had a family history of alcohol use and that they mainly consumed a country liquor called Mahua. Mahua is a traditional alcoholic beverage made from the flowers of the mahua tree (Madhuca longifolia), which grows in various parts of India. Mahua is the only spirit in the world derived from sweet blossoms. The Adivasi community, which constitutes the majority of the tribal population in India, has been using the mahua tree for various purposes for over a century. The mahua tree is a major source of income for them. Mahua consumption is considered to be a common practice among the tribal people.[17] The study also found that 78% of the cases had a positive family history of substance abuse, indicating a high prevalence of substance use disorders. The most common substances used in the cases were tobacco followed by alcohol, as shown in Figure 3, which is in line with the NMHS-16 report, which stated that Chhattisgarh has a higher proportion of tobacco users than the national average.[7,16]
The study reported that 2% of the cases had a family history of completed suicide, consistent with other studies that documented high rates of suicide among tribal communities.[18] The National Crime Record Bureau (NCRB) report of 2021 revealed that Chhattisgarh is among the top three states in India with the highest suicide rates. This observation highlights the need for mental health promotion in underserved areas of the state.[19]
The study revealed that most cases were reluctant to go to the centers for mental health care. One of the reasons for this could be the long distance between their homes and the nearest mental health professional, as shown in Figure 2. The study found that the minimum distance was 11–30 km for some cases, while for 42% of the cases, it was more than 30 km. This was also supported by the finding that transportation difficulties were the major reason for not seeking help. The study also reported that nearly half of the cases visited the center by themselves, while their spouse, relatives, or friends accompanied more than half. The study showed that most of the cases were first identified and contacted during field visits (77%), while some came to the center by themselves or were referred by Mitanin or ASHA workers. This finding suggests that for the tribal people, mental health care needs to be delivered to their doorstep as most of the doctors at primary care and specialty centers are in semi-urban and urban areas. The treatment gap cannot be bridged unless there is an equitable distribution of services. The study employed two trained cadres who were part of the community where the cases resided, which may have facilitated the effective detection and follow-up of these cases who had not received services so far.
The majority of the participants, 114 (62.0%), had no history of treatment or medication, while 13 (7.1%) had taken and discontinued the treatment. One possibility could be the difficulty in accessing mental health facilities due to the remote locations of many of these villages, situated far away from urban centers, resulting in considerable out-of-pocket expenditures.[2] In addition, in our study, 45.35% of the cases were not willing to visit a higher center. The people gave the following reasons: transportation, denial of mental illness, poor support and knowledge about the illness and treatment options, financial issues, and loss of income for the day. In previous research findings, the main reason for visiting local faith healers was their cost-effectiveness and easy availability.[20] The other reason could be the belief in faith healers. A significant proportion of the patients involved in our study sought assistance from practitioners of faith healing. Based on our experience and the insights gained from our examination of the faith healing process, it became evident that a considerable number of individuals sought the services of a faith healer known as “BAIGA,” meaning “medicine man,” a designation attributed to a tribal group. The Baiga tribe, which predominantly inhabits forested regions, stands out as one of the most ancient tribal communities. Notably, this tribal group holds the classification of Particularly Vulnerable Tribal Group (PVTG). Faith healers or traditional healers have been proven to be effective in making the system accessible to the general population in sub-Saharan countries. One such project, the Dawa-Dua project is an initiative that aims to integrate medical and religious approaches to treat mental illness through a collaboration of modern psychiatry medicine and faith-based treatment practices to benefit patients with limited access to mental health care and protect the human rights of patients.[16] Their involvement in the current treatment loop would be significant.
Recommendation
Primary-level interventions:
Tailor-made interventions for tribal communities.
Information, education, and communication (IEC) activities.
Targeted interventions: harm reduction, inclusive social beneficiary services.
Addressing inequality, poverty, and unemployment.
Acknowledging compensatory substance use due to stress.
Secondary-level interventions:
Screening and early identification using tools such as MERIT.
Early treatment augmentation at local levels.
Reducing the treatment gap and providing local treatment options.
Tertiary-level interventions:
Referral to specialized centers.
Community rehabilitation involving local community members.
Overcoming transportation and financial barriers.
Awareness and funding:
Government and NGOs to spread mental health information among Scheduled Tribe (ST) populations.
Lack of awareness about mental health in ST communities.
Increased funding for research and awareness programs.
Key stakeholders are involved in raising awareness among the public and policymakers.
Involvement of faith healers:
Develop a mental health model involving faith healers.
The significant role of faith healers in Indian and other cultures.
Incorporate faith healers to improve access to mental health care.
Consider the cultural roots of psychiatric morbidities.
Community involvement and coordination:
Select tribe members as volunteers to educate about harm (e.g. Mahua).
Coordinated efforts from government sectors (NCD, DMHP, NMHP) for affordable tribal mental health services.
Importance of separate programs/projects for tribal mental health.
Conclusion
This study underscores the pressing need for targeted mental health interventions in tribal populations, particularly in India. The findings reveal a stark reality where tribal communities grapple with high rates of substance use, anxiety, depression, and other mental health disorders, all exacerbated by a lack of access to appropriate care. It is evident that conventional approaches to mental health care fall short in reaching these underserved populations. The reluctance to seek professional help, often driven by transportation difficulties and a dearth of awareness, underscores the necessity for community-based mental health services. The involvement of local/primary care health workers, trained through initiatives such as TORENT, holds promise in bridging the treatment gap. In addition, the study highlights the pivotal role of faith healers in tribal communities. Their cultural significance and accessibility make them valuable allies in delivering mental health care services. Addressing the mental health challenges of tribal populations in Chhattisgarh requires a multipronged approach. It demands not only increased awareness and funding but also the active engagement of government, NGOs, and key stakeholders. Tailor-made interventions, community involvement, and a focus on socioeconomic factors are crucial steps forward. In conclusion, this study acts as a clarion call to prioritize the mental well-being of tribal communities in Chhattisgarh. It serves as a vital foundation upon which comprehensive, culturally sensitive, and accessible mental health services can be built, ultimately fostering the holistic development and well-being of these marginalized populations.
Ethics Approval Ref No
NIMHANS/29th IEC/BEH.SC.DIV/2021 Dated: 27/01/2022.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The author acknowledges the cooperation and support of tribal community and Primary care workers in executing this project.
Funding Statement
Funded by Government of Chhattisgarh, India
References
- 1.Tewari A, Kallakuri S, Devarapalli S, Jha V, Patel A, Maulik PK. Process evaluation of the systematic medical appraisal, referral and treatment (SMART) mental health project in rural India. BMC Psychiatry. 2017;17:385. doi: 10.1186/s12888-017-1525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Devarapalli S, Kallakuri S, Salam A, Maulik P. Mental health research on scheduled tribes in India. Indian J Psychiatry. 2020;62:617–30. doi: 10.4103/psychiatry.IndianJPsychiatry_136_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Islary J. Health and health seeking behaviour among tribal communities in India: A socio-cultural perspective. J Tribal Intellect Collective India. 2014;16:1–6. [Google Scholar]
- 4.Executive Summary –Tribal Health Report, India. [[Last accessed on 2023 Aug 08]]. Available from: https://tribalhealthreport.in/executive-summary/
- 5.Murthy RS. National Mental Health Survey of India 2015-2016. Indian J Psychiatry. 2017;59:21–6. doi: 10.4103/psychiatry.IndianJPsychiatry_102_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sreeraj VS, Prasad S, Khess CRJ, Uvais NA. Reasons for substance use: A comparative study of alcohol use in tribals and non-tribals. Indian J Psychol Med. 2012;34:242–6. doi: 10.4103/0253-7176.106020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gautham MS, Gururaj G, Varghese M, Benegal V, Rao GN, Kokane A, et al. The National Mental Health Survey of India (2016): Prevalence, socio-demographic correlates and treatment gap of mental morbidity. Int J Soc Psychiatry. 2020;66:361–72. doi: 10.1177/0020764020907941. [DOI] [PubMed] [Google Scholar]
- 8.Gupta D, Singh PK. The hidden cost of development—A review of mental health issues of displaced tribal populations in India. J Public Heal. 2018;26:717–23. [Google Scholar]
- 9.Tribal Health Report, India – First Comprehensive Report on Tribal Health in India. [[Last accessed on 2023 Aug 08]]. Available from: https://tribalhealthreport.in/
- 10.Rizwan SA, Kumar R, Singh AK, Kusuma YS, Yadav K, Pandav CS. Prevalence of hypertension in Indian tribes: A systematic review and meta-analysis of observational studies. PLoS one. 2014;9:e95896. doi: 10.1371/journal.pone.0095896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joshi R, Alim M, Kengne AP, Jan S, Maulik PK, Peiris D, et al. Task shifting for non-communicable disease management in low and middle income countries--A systematic review. PLoS One. 2014;9:e103754. doi: 10.1371/journal.pone.0103754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maulik PK, Kallakuri S, Devarapalli S, Vadlamani VK, Jha V, Patel A. Increasing use of mental health services in remote areas using mobile technology: A pre-post evaluation of the SMART Mental Health project in rural India. J Glob Health. 2017;7:010408. doi: 10.7189/jogh.07.010408. https://pubmed.ncbi.nlm.nih.gov/28400954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suhas S, Nirisha PL, Malathesh BC, Kulal N, Harshitha NR, Gajera G, et al. Inter-rater reliability and concurrent validity of a novel mental health screening and counselling tool for community health workers of India. Indian J Psychiatry. 2022;64(Suppl 3):S533. [Google Scholar]
- 14.Sutar R, Lahiri A, Diwan S, Satpathy P, Rozatkar A. Determinants of mental health care access in a tribal district of central India: Findings from a Health Camp. J Neurosci Rural Pract. 2021;12:335–42. doi: 10.1055/s-0041-1723071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Multidimensional poverty in Chhattisgarh: A measure for action [Google Scholar]
- 16.Singh LK, Giri AK, Chhalotre V, Sharma RK, Rao GN, Gopalkrishna G, et al. Prevalence of psychiatric disorders in Chhattisgarh: Findings from National Mental Health Survey. Indian J Psychol Med. 2023;45:573–9. doi: 10.1177/02537176221141615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. [[Last accessed on 2023 Aug 08]]. Explained: How Indias Country Liquor Mahua Is Still Policed Through Excise Laws. Available from: https://www.indiatimes.com/explainers/how-indias-country-liquor-mahua-is-still-policed-through-excise-laws-571943.html .
- 18.Singh PK, Singh RK, Biswas A, Rao VR. High rate of suicide attempt and associated psychological traits in an isolated tribal population of North-East India. J Affect Disord. 2013;151:673–8. doi: 10.1016/j.jad.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Mid-year E. Chapter –2 Suicides in India. 2010:169–89. [Google Scholar]
- 20.Burns JK, Tomita A. Traditional and religious healers in the pathway to care for people with mental disorders in Africa: A systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. 2015;50:867–77. doi: 10.1007/s00127-014-0989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]