ABSTRACT
Introduction:
With increased urbanization the prevalence of important public health problems like road traffic accidents (RTA) and depression are surging. This study was aimed to determine the association between RTA and depression among Indian population aged ≥45 years.
Methods:
Using Longitudinal Aging Study in India (LASI) dataset (April 2017–December 2018), we have conducted this study among older adults (45–59 years) and elderly (≥60 years) Indians. Bivariate analysis was conducted to estimate the prevalence of RTA and depression nationally and across aspirants, achievers, and front runner states. Multivariable logistic regression was conducted between RTA and depression, adjusted with demographic and socioeconomic; health related and behavioral factors. P value <0.05 was considered as statistically significant.
Results:
Prevalence of RTA was 1.84 (1.74-1.94)% nationally, highest among achiever states (2.04 (1.82–2.30)%). Prevalence of depression was 6.08 (5.90–6.26)% nationally, highest among aspirant states (7.02 (6.74–7.30)%). The adjusted odds of having accident was significantly 1.75 times higher among depressed (aOR 1.75, 95% CI 1.44–2.13) than non-depressed participants which was highest across front runners (aOR 1.86, 95%CI 1.26–2.72) followed by aspirant states (aOR 1.79, 95%CI 1.37–2.33).
Conclusion:
This study established the association between depression and road traffic accidents among older adults and elderly. Therefore, efforts must be taken to address mental health issues specially focusing on depression in them with proper policy implication more focused on front runners followed by aspirant states.
Keywords: Accidents, depression, elderly, LASI, older adults, RTA, road traffic accidents
Introduction
Longitudinal Aging Study in India (LASI) is India’s first and globally, the largest in Health and Retirement Study. The LASI is a full-scale national survey of scientific investigation of the health, economic, and social determinants and consequences of population aging in India. LASI Wave I was conducted in 2017–2018 with a sample of 72,250 adults (30,569 men and 41,681 women) aged ≥45 years and their spouses (irrespective of age) across all states and union territories (UTs) in India (excluding Sikkim). The Wave-1 India Report was released on 6 January 2021.[1]
In India, elderly persons (60 years and above) constitute 8.6% of the total population (India Census 2011), which is projected to reach 19% by 2050.[2] Depression is one of the most common illnesses in the elderly population. A study involving 16 States of India estimated that the prevalence of depression among Indian elderly population was 34.4% (95% CI: 29.3–39.7).[3] Among elderly people, chronic diseases, restricted mobility, bereavement, elderly abuse, isolation, and loss of income are major risk factors for depression, in addition to common risk factors in all age groups.[4] Patients with depressive disorders could be more liable to accidents than others for several reasons. Also, in patients under anti-depressants, the unwanted effects of anti-depressants may adversely affect cognitive and psychomotor function, thereby increasing the risk of accidents. In India, such as in most LMICs, the research output on key public health issues, including RTIs and mental health remains poor. Thus, this study was conducted to unveil the curtain from this important public health problem aiming at further health policy implementation.
Objective
To estimate the state wise distribution of prevalence of RTA and depression, to determine the association of road traffic accident (RTA) with depression among Indian population aged ≥45 years; overall and stratified into population staying in aspirants, achievers and front runner states.
Methods
The current analysis used LASI-1st wave data from 35 Indian states and union territories (UTs), with the exception of Sikkim. It is a longitudinal survey with a national representation that intends to collect detailed information on the psychological, social, economic, and health aspects of ageing in India. It was created to close the knowledge gap about comprehensive and globally comparable survey data on ageing in India. The National Institute on Ageing, the Government of India’s Ministry of Health and Family Welfare, and the United Nations Population Fund all provided funding for the study. The University of Southern California, the International Institute for Population Sciences, and the Harvard T.H. Chan School of Public Health are working together on it. The demography, health, economy, and social factors are just a few of the important topics it focuses on. There were 73,000 adult Indians in LASI.
Eligibility criteria
Participants more than equal to 45 years were included in this study. Participants not able to provide answers of the questionnaire themselves and did not provide consent were excluded. Thus, the final sample size was 66,606.
The study, which is the biggest of its kind in the world and the first of its kind in India, evaluates the scientific evidence in the context of variables like demographics, household economic status, chronic health conditions, symptom-based health conditions, functional health, mental health (cognition and depression), biomarkers, healthcare utilization, family and social networks, social welfare programs, employment, retirement, satisfaction, and life expectations. The survey intends to follow a representative sample of the older adult population every two years for the following 25 years, with a revised sample size to account for attrition due to death, migration, non-reachable, and non-response.[5]
Ethics
Ethical approval was granted by the Indian Council of Medical Research.[5]
Outcome variable
Road traffic accident was taken as outcome variable. “What is the cause of injury in the last two years” was asked during interview. Participants answering “traffic accident” were included for analysis.
Explanatory variable
The explanatory variable of interest was depression. The Composite International Diagnostic Interview—Short Form (CIDISF) scale was used to assess individuals with diagnosable major depressive episodes (MDEs).[6] It is a reliable, cost-effective, non-clinical survey instrument for diagnostic purposes that is comparable to the original CIDI scale. It provides an accurate diagnosis of depression and a trustworthy structured instrument for use with experienced interviewers.[7,8,9] The Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III), has accepted it.[10] It was developed as a non-clinical diagnostic tool for circumstances in which a clinician’s clinical examination and assessment of a patient’s mental health is impractical. Validation studies have shown that the CIDI-SF scale may accurately produce diagnostic categories for depressive episodes.[11] Comparability with other ageing research is improved by using CIDI-SF in LASI.[12] It is often utilized in comprehensive national surveys, such as the World Mental Health Survey,[7] the US National Health Interview Survey,[13] and the Canadian National Population Health Survey.[8]
In this study, CIDI-SF was translated into 16 significant regional languages in accordance with the approved translation standards provided by the WHO.[14] After survey and health investigators received training (over the course of five weeks), the translated LASI instrument was pretested in each of the regional languages as part of fieldwork. However, as they went outside the scope of this big research, the psychometric capabilities of the CIDI-SF were not extensively examined as part of this inquiry. The LASI national report and other sources give a more thorough explanation of the field survey implementation methods. In the LASI, people were classified as having probable depression (MDEs) if they checked yes to three or more of the CIDI-SF scale’s seven symptoms of depression.[5,15]
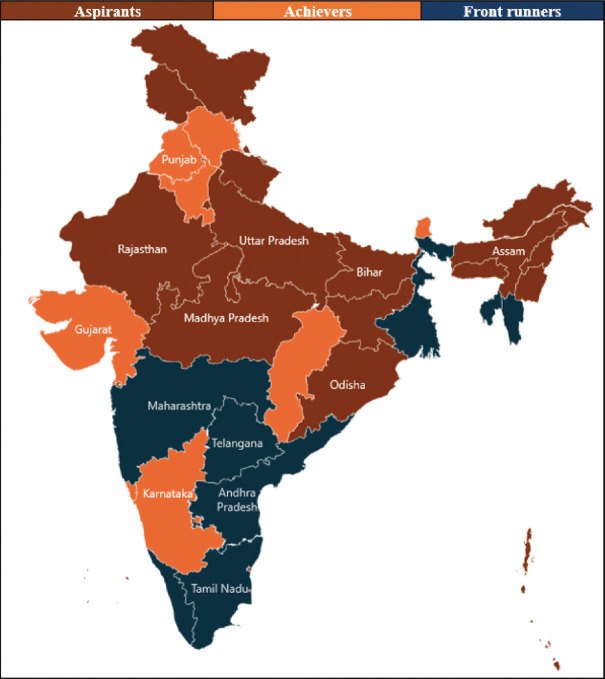
Figure 1 and Supplementary Table S1 documented the states and union territories listed as aspirants, achievers and front runners.
Figure 1.
Distribution of states/union territories as aspirants, achievers and front runners
Supplementary Table S1.
Distribution of states/union territories as aspirants, achievers and front runners
| States | State/Union territory |
|---|---|
| Aspirants | Andaman and Nicobar |
| Arunachal Pradesh | |
| Assam | |
| Bihar | |
| Delhi | |
| Jammu and Kashmir | |
| Jharkhand | |
| Lakshadweep | |
| Madhya Pradesh | |
| Manipur | |
| Meghalaya | |
| Nagaland | |
| Odisha | |
| Puducherry | |
| Rajasthan | |
| Uttar Pradesh | |
| Uttarakhand | |
| Achievers | Chhattisgarh |
| Goa | |
| Gujarat | |
| Haryana | |
| Himachal Pradesh | |
| Karnataka | |
| Punjab | |
| Sikkim | |
| Front runners | Andhra Pradesh |
| Chandigarh | |
| Dadra and Nagar Haveli | |
| Daman and Diu | |
| Kerala | |
| Maharashtra | |
| Mizoram | |
| Tamil Nadu | |
| Telangana | |
| Tripura | |
| West Bengal |
Covariates
Demographic and socioeconomic factors like- age (years 45–59, ≥60), gender (male, female), minimum education (illiterate, less than primary. primary completed, middle completed, secondary school, higher secondary, and Diploma/graduate), residence (rural, urban), marital status (unmarried, married/in live-in, Widow/separated/divorced), MPCE (monthly per capita expenditure—poorest, poorer, middle, richer, richest) quintile, health insurance (no, yes), occupation (unemployed, professional, and semi-professional— “legislators and senior officials, professionals, technicians and associate professionals,” clerical and skilled— “clerks, service workers and shopkeepers, skilled agriculture and fishery workers, craft and related trade worker, plant and machine operator,” unskilled); and health related and behavioral factors like physical activity (everyday, once per week, 1-3 times per week, once per month, never), self-rated health (excellent, very good, good, fair, poor), tobacco usage (no, yes) and alcohol consumption (no, yes) were taken as covariates for adjustment.
Statistical analysis
Prevalence was documented as frequency and percentage. Spatial distribution maps were created to display the distribution of RTA and depression prevalence at Indian sub-national level. We have Used STATA version 18 for data analysis (Stata Corp. 2018. Stata Statistical Software: Release 18. College Station, TX: Stata Corp LP.). Univariate logistic regression was conducted between outcome variable and each explanatory variable. To avoid multicollinearity among explanatory variables Variance inflation factor (VIF) was applied. VIF > 5 indicates high correlation between a given explanatory variable and other explanatory variables in the model, which might create problems with the regression analysis. Self-rated health and marital status had VIF>5 [Supplementary Table S2]. Hence, all the explanatory variables expect these two were included for final association. P value <0.05 were considered as statistically significant. P value <0.2 was taken for further multivariable logistic regression. Association was calculated in overall population and was further categorized into participants residing in aspirant, achiever, and front runner states.
Supplementary Table S2.
Distribution of various variables as per VIF (Variance inflation factor)
| Variable | VIF* |
|---|---|
| Depression | 1.14 |
| Age group (years) | 1.27 |
| Gender | 1.73 |
| Education | |
| Less than primary | 1.15 |
| Primary completed | 1.2 |
| Middle completed | 1.21 |
| Secondary school | 1.26 |
| Higher secondary | 1.17 |
| Diploma/graduate | 1.37 |
| Residence | 1.22 |
| Marital status | |
| Married/in live -in | 15.34 |
| Widow/separated/divorced | 15.58 |
| MPCE quintile | |
| Poorer | 1.62 |
| Middle | 1.64 |
| Richer | 1.67 |
| Richest | 1.75 |
| Health insurance | 1.05 |
| Occupation | |
| Professional and semi-professional | 1.16 |
| Clerical and skilled | 1.53 |
| unskilled | 1.42 |
| Physical activity | |
| More than once/week | 1.20 |
| Once/week | 1.12 |
| 1-3 times/month | 1.16 |
| Never | 1.69 |
| Self-rated health | |
| Very good | 4.79 |
| Good | 6.78 |
| Fair | 6.00 |
| Poor | 3.40 |
| Tobacco | 1.31 |
| Alcohol | 1.28 |
| Mean VIF | 2.80 |
*To avoid multicollinearityamong explanatory variables Variance inflation factor (VIF)was applied. VIF > 5 indicates high correlation between agiven explanatory variable and other explanatory variablesin the model, which might create problems with theregression analysis. Selfrated health and marital status hadVIF>5.
Results
The prevalence of road traffic accident in overall population was 1.84% which was highest in population residing in achiever states (2.04%) followed by aspirant (1.87%). The front runner states showed least prevalence of road traffic accidents (1.68%). The prevalence of depression was 6.08% in overall population which was highest in population residing in aspirant states (7.02%) followed by achiever states (5.74%). The front runner states showed least prevalence of depression (4.97%) [Table 1].
Table 1.
Prevalence of road traffic accident and depression in Indian population aged ≥45 years
| Variable | Prevalence (%) (95% confidence interval) | |||
|---|---|---|---|---|
|
| ||||
| Total (n=66606) | States categorization | |||
|
| ||||
| Aspirants (n=31005) | Achievers (n=13422) | Front runners (n=22179) | ||
| Road traffic accident | 1.84 (1.74–1.94) | 1.87 (1.72–2.02) | 2.04 (1.82–2.30) | 1.68 (1.52–1.86) |
| Depression | 6.08 (5.90–6.26) | 7.02 (6.74–7.30) | 5.74 (5.36–6.14) | 4.97 (4.69–5.26) |
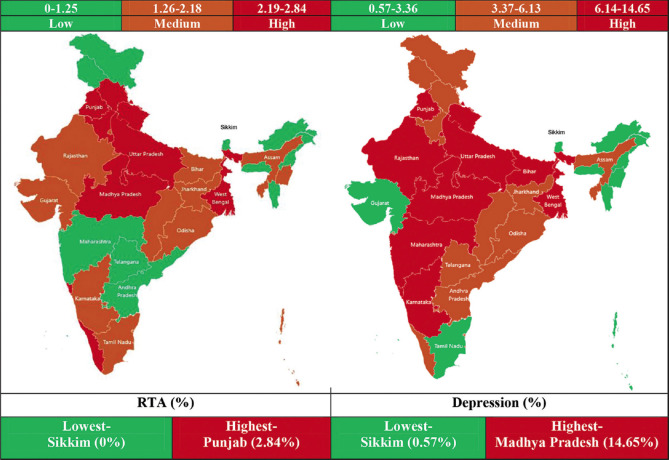
Punjab had the highest (2.84%) prevalence of RTA, while Sikkim had the lowest (%) prevalence. The highest and lowest prevalence of depression was documented in Madhya Pradesh (14.65%) and Sikkim (0.57%) [Figure 2 and Table 2].
Figure 2.
State/Union Territory wise distribution of participants as per prevalence of RTA and depression
Table 2.
State/union territory wise distribution of participants as per depression and RTA
| States/Union territories | Depression | RTA |
|---|---|---|
| Andaman and Nicobar | 1.35 | 1.53 |
| Andhra Pradesh | 3.38 | 0.83 |
| Arunachal Pradesh | 1.53 | 0.61 |
| Assam | 5.60 | 2.18 |
| Bihar | 10.46 | 2.09 |
| Chandigarh | 5.83 | 2.58 |
| Chhattisgarh | 5.37 | 1.74 |
| Dadra and Nagar Haveli | 2.73 | 0.81 |
| Daman and Diu | 3.32 | 2.21 |
| Delhi | 6.92 | 1.26 |
| Goa | 9.09 | 2.61 |
| Gujarat | 3.36 | 1.77 |
| Haryana | 6.09 | 2.39 |
| Himachal Pradesh | 4.86 | 2.23 |
| Jammu and Kashmir | 4.37 | 0.87 |
| Jharkhand | 5.88 | 1.53 |
| Karnataka | 7.83 | 2.11 |
| Kerala | 6.00 | 2.48 |
| Lakshadweep | 2.64 | 0.28 |
| Madhya Pradesh | 14.65 | 2.76 |
| Maharashtra | 7.93 | 1.20 |
| Manipur | 1.12 | 1.28 |
| Meghalaya | 2.13 | 0.34 |
| Mizoram | 0.89 | 0.44 |
| Nagaland | 2.16 | 0.17 |
| Odisha | 4.54 | 2.17 |
| Puducherry | 5.05 | 2.10 |
| Punjab | 8.27 | 2.84 |
| Rajasthan | 6.15 | 2.16 |
| Sikkim | 0.57 | 0.00 |
| Tamil Nadu | 3.12 | 1.84 |
| Telangana | 4.84 | 1.20 |
| Tripura | 3.64 | 2.01 |
| Uttar Pradesh | 12.54 | 2.77 |
| Uttarakhand | 6.42 | 2.46 |
| West Bengal | 6.17 | 2.59 |
| India | 6.08 | 1.84 |
More than half of population was female (53.40%). Prevalence of road traffic accident was higher in male (2.67%) than female (1.12%). Almost half of the population were elderly (≥60 years). Road traffic accidents were seen more in participants aged 45–59 years (2.20%). Almost half (47.07%) of the participants were illiterate. Accidents were most prevalent among participants educated at least higher secondary (3.23%). Almost three-fourth of the participants were married or in live-in relationships with 2.02% accident prevalence. Among MPCE quintiles, prevalence of accident was highest (2.24%) in richest and lowest (1.26%) in poorest population. Only 2.33% population has health insurance; among them 2.69% had accident. More than half of the population was unemployed (51.32%) having the least prevalence of accident (1.38%). Professional and semi-professional participants had the highest prevalence of accident (3.07%). Majority of the participants never performed any physical activity. Among them, accident prevalence was least (1.64%). Participants with poor self-rated health had highest accident prevalence (2.37%). Tobacco abusing participants (2.25%) had more accident prevalence than the non-abusers (1.61%). Participants with history of alcohol consumption had higher (1.84%) accident prevalence than the non-consumers (1.66%) [Table 3].
Table 3.
Various characteristics of Indian population aged ≥45 years
| Variable | Total (n=66606) n (%) | Road traffic accident cases (n=1225) n (%) | P |
|---|---|---|---|
|
| |||
| Demographic and socioeconomic factors | |||
| Sex | |||
| Male | 31039 (46.60) | 828 (2.67) | <0.001 |
| Female | 35567 (53.40) | 397 (1.12) | |
| Age group (years) | |||
| 45–59 | 34704 (52.10) | 762 (2.20) | <0.001 |
| ≥60 | 31902 (47.90) | 463 (1.45) | |
| Education (minimum) | |||
| Illiterate | 31,353 (47.07) | 405 (1.29) | <0.001 |
| Less than primary | 7,598 (11.41) | 158 (2.08) | |
| Primary completed | 8,761 (13.15) | 186 (2.12) | |
| Middle completed | 6,337 (9.51) | 155 (2.45) | |
| Secondary school | 5,953 (8.94) | 139 (2.33) | |
| Higher secondary | 2,852 (4.28) | 92 (3.23) | |
| Diploma/Graduate | 3,752 (5.63) | 90 (2.40) | |
| Residence | |||
| Rural | 43240 (64.92) | 777 (1.80) | 0.270 |
| Urban | 23366 (35.08) | 448 (1.92) | |
| Marital Status | |||
| Unmarried | 871 (1.31) | 7 (0.80) | <0.001 |
| Married/in live-in | 49949 (74.99) | 1011 (2.02) | |
| Widow/separated/divorced | 15786 (23.70) | 207 (1.31) | |
| MPCE quintile | |||
| Poorest | 13,181 (19.79) | 166 (1.26) | <0.001 |
| Poorer | 13,403 (20.12) | 217 (1.62) | |
| Middle | 13,371 (20.07) | 264 (1.97) | |
| Richer | 13,412 (20.14) | 282 (2.10) | |
| Richest | 13,239 (19.88) | 296 (2.24) | |
| Health insurance | |||
| No | 65121 (97.77) | 1185 (1.82) | 0.013 |
| Yes | 1485 (2.23) | 40 (2.69) | |
| Occupation | |||
| Unemployed | 34,180 (51.32) | 470 (1.38) | <0.001 |
| Professional and semi-professional | 1,597 (2.40) | 49 (3.07) | |
| Clerical and skilled | 16,683 (25.05) | 394 (2.36) | |
| Unskilled | 14,146 (21.24) | 312 (2.21) | |
|
| |||
| Health related and behavioral factors | |||
|
| |||
| Physical activity | |||
| Everyday | 15,672 (23.53) | 347 (2.21) | <0.001 |
| More than once/week | 4,559 (6.84) | 102 (2.24) | |
| Once/week | 2,396 (3.60) | 44 (1.84) | |
| 1-3 times/month | 3,274 (4.92) | 66 (2.02) | |
| Never | 40,705 (61.11) | 666 (1.64) | |
| Self-rated health | |||
| Excellent | 2,570 (3.91) | 40 (1.56) | <0.001 |
| Very good | 12,602 (19.18) | 198 (1.57) | |
| Good | 25,723 (39.16) | 446 (1.73) | |
| Fair | 18,137 (27.61) | 372 (2.05) | |
| Poor | 6,660 (10.14) | 158 (2.37) | |
| Tobacco usage | |||
| No | 42583 (63.93) | 684 (1.61) | <0.001 |
| Yes | 24023 (36.07) | 541 (2.25) | |
| Alcohol consumption | |||
| No | 54752 (82.20) | 907 (1.66) | <0.001 |
| Yes | 11854 (17.80) | 318 (1.84) | |
The adjusted odds of having accident was 1.75 times higher among depressed (aOR 1.75, 95% CI 1.44-2.13) participants than non-depressed ones with statistically significant difference. The prevalence of accident was 30% lower among elderly (≥60 years) than older adults (45–59 years) and 52% lower among females than males. The accident prevalence was 38% higher among participants with minimum education till higher secondary compared to diploma/graduates. With improving in the MPCE quintile the odds of having accident increased significantly [Table 4].
Table 4.
Univariate and multivariable logistic regression of road traffic accident and depression (Classification accuracy=98.16%)
| Characteristics | Univariate | Multivariable | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Crude odds ratio (95% Confidence interval) | P | Pseudo R2 | Adjusted odds ratio (95% Confidence interval) | P | Pseudo R2 | |
| Depression | 0.0314 | |||||
| No | Reference | - | 0.0017 | Reference | - | |
| Yes | 1.62 (1.33-1.97) | <0.001 | 1.75 (1.44-2.13) | <0.001 | ||
| Age (years) | ||||||
| 45-59 | Reference | - | Reference | - | ||
| ≥60 | 0.66 (0.58-0.74) | <0.001 | 0.0042 | 0.70 (0.61-0.79) | <0.001 | |
| Gender | ||||||
| Male | Reference | - | Reference | - | ||
| Female | 0.41 (0.37-0.47) | <0.001 | 0.0183 | 0.48 (0.41-0.56) | <0.001 | |
| Education | ||||||
| Diploma/Graduate | Reference | - | Reference | - | ||
| Illiterate | 0.53 (0.42-0.67) | <0.001 | 0.0093 | 0.82 (0.64-1.06) | 0.140 | |
| Less than primary | 0.86 (0.67-1.12) | 0.274 | 1.07 (0.81-1.41) | 0.654 | ||
| Primary completed | 0.88 (0.68-1.13) | 0.336 | 1.06 (0.81-1.39) | 0.673 | ||
| Middle completed | 1.02 (0.78-1.32) | 0.882 | 1.12 (0.85-1.48) | 0.415 | ||
| Secondary school | 0.97 (0.74-1.27) | 0.840 | 1.05 (0.80-1.39) | 0.722 | ||
| Higher secondary | 1.36 (1.01-1.82) | 0.043 | 1.38 (1.02-1.86) | 0.036 | ||
| Residence | ||||||
| Urban | Reference | - | Reference | - | ||
| Rural | 0.94 (0.83-1.05) | 0.270 | 0.0001 | - | - | |
| MPCE quintile | ||||||
| Poorest | Reference | - | Reference | - | ||
| Poorer | 1.29 (1.05-1.58) | 0.014 | 0.040 | 1.26 (1.03-1.54) | 0.028 | |
| Middle | 1.58 (1.30-1.92) | <0.001 | 1.52 (1.25-1.85) | <0.001 | ||
| Richer | 1.68 (1.39-2.04) | <0.001 | 1.57 (1.29-1.91) | <0.001 | ||
| Richest | 1.79 (1.48-2.17) | <0.001 | 1.63 (1.34-1.98) | <0.001 | ||
| Health insurance | ||||||
| No | Reference | - | Reference | - | ||
| Yes | 1.49 (1.09-2.06) | 0.014 | 0.0004 | 1.00 (0.73-1.39) | 0.985 | |
| Occupation | ||||||
| Unemployed | Reference | - | Reference | - | ||
| Professional and semi-professional | 2.27 (1.68-3.06) | <0.001 | 0.0073 | 1.18 (0.86-1.64) | 0.308 | |
| Clerical and skilled | 1.73 (1.52-1.99) | <0.001 | 1.14 (0.97-1.34) | 0.116 | ||
| Unskilled | 1.62 (1.40-1.87) | <0.001 | 1.07 (0.90-1.26) | 0.456 | ||
| Physical activity | ||||||
| Everyday | Reference | - | Reference | - | ||
| More than once/week | 1.01 (0.81-1.26) | 0.925 | 0.0021 | 1.05 (0.84-1.32) | 0.634 | |
| Once/week | 0.83 (0.60-1.13) | 0.235 | 0.88 (0.64-1.21) | 0.442 | ||
| 1-3 times/month | 0.91 (0.70-1.19) | 0.480 | 1.00 (0.76-1.30) | 0.995 | ||
| Never | 0.73 (0.64-0.84) | <0.001 | 0.97 (0.84-1.12) | 0.657 | ||
| Tobacco usage | ||||||
| No | Reference | - | Reference | - | ||
| Yes | 1.41 (1.26-1.58) | <0.001 | 0.0028 | 1.05 (0.92-1.20) | 0.444 | |
| Alcohol consumption | ||||||
| No | Reference | - | Reference | - | ||
| Yes | 1.64 (1.44-1.86) | <0.001 | 0.0042 | 1.10 (0.95-1.27) | 0.193 | |
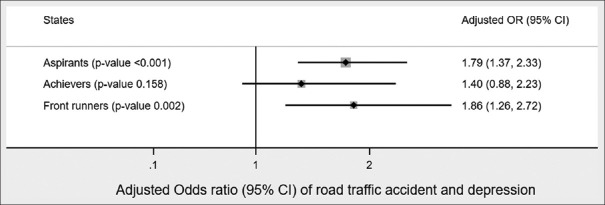
Figure 3 showing that the odds of accidents among depressed participants was highest (1.86 times more) in front runner states (aOR 1.86, 95%CI 1.26–2.72) than non-depressed ones followed by aspirant states (aOR 1.79, 95%CI 1.37–2.33) with statistically significant difference. Though the odds of accidents was lowest among depressed participants of achiever states (aOR 1.40, 95%CI 0.88–2.23) the difference was not statistically significant.
Figure 3.
Association of road traffic accidents with depression as per state categorization (classification accuracy 98.32%)
Discussion
The prevalence of depression was 6.08% in overall population. In contrast, a study involving 16 States of India estimated that the prevalence of depression among Indian elderly population was 34.4% (95% CI: 29.3–39.7).[3] The prevalence of accident was 30% lower among elderly (≥60 years) than older adults (45–59 years). This may be because of the tendency of the elderly (≥60 years) to stay indoor when compared to older adults (45–59 years) who still constitute the working population and are exposed to the risk of road traffic accidents. The prevalence of road traffic accident in overall population was 1.84%. The prevalence of accident was highest (2.24%) in richest and lowest (1.26%) in poorest population. This is in contrast to the fact that the prevalence of adverse road traffic health outcomes is higher among poor people and they experience more exposure to risk factors for various reasons, including living in high-risk environments and conditions. Moreover, in this group, risky behaviors including traffic-related risky behaviors are more common.[16] The odds of accident were 1.75 times higher among depressed (aOR 1.75, 95% CI 1.44–2.13) participants than non-depressed ones with statistically significant difference. This could be because that they are more liable to accidents than others for the reasons which include impaired attention and concentration (often due to pre-occupation with morbid or worrying thoughts); anxiety, which usually accompanies depression; irritability; agitation or retardation; fatigue after sleepless nights; and weakness due to insufficient food intake. In addition, depressed patients may take risks with little regard to the consequences, make suicidal gestures or attempts that go wrong, and take alcohol or other substances that impair functioning to relieve distress.[17] This was well documented in this study since participants abusing tobacco (2.25%) had prevalence of accidents higher than the non-abusers (1.61%), and those participants with history of alcohol consumption had higher (1.84%) accident prevalence than the non-consumers (1.66%). The odds of accidents among depressed participants were highest (1.86 times more) in front runner states (aOR 1.86, 95%CI 1.26–2.72) than non-depressed ones followed by aspirant states (aOR 1.79, 95%CI 1.37–2.33) with statistically significant difference. This could be due to the lack of social and mental support in front runner states owing to lack of joint families when compared to aspirant states. Professional and semi-professional participants had the highest prevalence of accident (3.07%). This in turn could be due to the work factors contributing to depression which includes: Skill utilization, decision authority, psychological demands, physical demands, number of hours worked, work schedule (irregular or regular), work schedule (daytime or night time), social support from co-workers, social support from supervisor and the family, job insecurity, recognition, job promotion, and bullying.[18]
The strength of our study was inclusion of large sample size leading to higher generalizability. Coming to limitations, due to the cross-sectional study design, causality could not be established. Recall bias and social desirability bias were not completely excluded due to self-reporting style of questionnaire. We recommend evidence-based community level large scale trials with regular follow-ups to strengthen our findings.
Conclusion
Though handful, available evidence established the association between depression and road traffic accidents among older adults and elderly. Therefore, efforts must be taken to address mental health issues in them. India has four types of resources to address geriatric mental health issues: (1) state-funded government psychiatric hospitals and nursing homes; (2) private psychiatric hospitals and nursing homes; (3) non-government organizations; and (4) the most important, informal sources—family as caregivers. But the focus of mental health care in India is still on tertiary care and acute management as opposed to developing primary care or rehabilitative services. Also, the research in RTIs and mental health has not received much attention from the scientific community due to a lack of focus in national policies and funding opportunities, especially in low- and middle-income countries (LMIC).[19] Advocacy and research activities are only left to a few organizations like the Indian Association for Geriatric Mental Health, Geriatric Society of India, Indian Academy of Geriatrics, and the Association of Gerontology.[20]
Therefore, government policies should consider this issue by training the peripheral health workers, involving medical colleges and routine camps in detecting mental health issues in older adults and the elderly, and connect them with psychiatrists via effective referral. Some new initiatives such as day care centers, old age residential homes, counseling, memory clinics, helplines, and recreational facilities may be developed both in rural and urban settings to ensure mental well-being among older adults and the elderly.
Ethical statement
Being a secondary analysis of a dataset freely available in the public domain, ethical approval for the present study was not deemed necessary. However, the ethical approval to conduct LASI was given by the Indian Council of Medical Research’s (ICMR) Central Ethics Committee on Human Research (CECHR).- International Institute for Population Sciences (IIPS) NP for, Health Care of Elderly (NPHCE), MoHFW HTHCS of, (USC) PH (HSPH) and the U of SC. Longitudinal Ageing Study in India (LASI) wave 1, 2017–18, India report. 2020.
Available from: https://www.iipsindia.ac.in/lasi [Internet]. [cited 2024 Feb 28].
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We want to convey our sincere gratitude towards the participants and Indian Council of Medical Research.
Funding Statement
Nil
References
- 1.LASI_India_Report_2020_compressed.pdf. [[Last accessed on 2023 Oct 10]]. Available from: https://www.iipsindia.ac.in/sites/default/files/LASI_India_Report_2020_compressed.pdf .
- 2.Agarwal A, Lubet A, Mitgang E, Mohanty S, Bloom DE. Population aging in India: Facts, issues, and options. [[Last accessed on 2023 Oct 10]]. Available from: https://www.hsph.harvard.edu/wp-content/uploads/sites/1288/2012/11/Population-Aging-in-India_PGDA-Working-Papers.pdf .
- 3.Pilania M, Yadav V, Bairwa M, Behera P, Gupta SD, Khurana H, et al. Prevalence of depression among the elderly (60 years and above) population in India, 1997-2016: A systematic review and meta-analysis. BMC Public Health. 2019;19:832. doi: 10.1186/s12889-019-7136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.International Institute for Population Sciences (IIPS),National Programme for Health Care of Elderly (NPHCE),MoHFW, Harvard T. H. Chan School of Public Health (HSPH)and the University of Southern California (USC) 2020. Longitudinal Ageing Study in India (LASI) Wave 1, 201718, India Report. Mumbai: International Institute for PopulationSciences; 2020. [[Last accessed on 2023 Sep 27]]. Available from: https://www.iipsindia.ac.in/sites/default/files/LASI_India_Report_2020_compressed.pdf . [Google Scholar]
- 6.Gigantesco A, Morosini P. Development, reliability and factor analysis of a self-administered questionnaire which originates from the World Health Organization's Composite International Diagnostic Interview –Short Form (CIDI-SF) for assessing mental disorders. Clin Pract Epidemiol Ment Health. 2008;4:8. doi: 10.1186/1745-0179-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) composite international diagnostic interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patten SB. Performance of the composite international diagnostic interview short form for major depression in community and clinical samples. Chronic Dis Can. 1997;18:109–12. [PubMed] [Google Scholar]
- 9.Kishore J, Kapoor V, Reddaiah VP. The Composite international diagnostic interview (CIDI): Its reliability and applicability in a rural community of Northern India. Indian J Psychiatry. 1999;41:350–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Pichot P. [DSM-III: The 3d edition of the Diagnostic and Statistical Manual of Mental Disorders from the American Psychiatric Association. Rev Neurol (Paris) 1986;142:489–99. [PubMed] [Google Scholar]
- 11.Nelson C. The Composite International Diagnostic Interview (CIDI) website. Bull World Health Organ. 1999;77:614. [Google Scholar]
- 12.Health and Retirement Study. International Sister Studies. [[cited 2023 Sep 27]]. [[Last accessed on 2023 Sep 27]]. Available from: https://hrs.isr.umich.edu/about/international-sister-studies . Available from: https://hrs.isr.umich.edu/about/internationalfamily-studies .
- 13.Patten SB, Brandon-Christie J, Devji J, Sedmak B. Performance of the composite international diagnostic interview short form for major depression in a community sample. Chronic Dis Can. 2000;21:68–72. [PubMed] [Google Scholar]
- 14.World Health Organization (WHO), Translation & linguistic evaluation protocol & supporting material. WHO/UNESCAP Project on Health and Disability Statistics. WHODAS 2.0 Translation package (Version 1.0). [cited 2023 Sep 27] [[Last accessed on 2023 Sep 27]]. Available from: https://terrance.who.int/mediacentre/data/WHODAS/Guidelines/WHODAS%202.0%20Translation%20guidelines.pdf .
- 15.Perianayagam A, Bloom D, Lee J, Parasuraman S, Sekher TV, Mohanty SK, et al. Cohort Profile: The Longitudinal Ageing Study in India (LASI) Int J Epidemiol. 2022;51:e167–76. doi: 10.1093/ije/dyab266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roshanfekr P, Khodaie-Ardakani MR, Sajjadi H, Malek Afzali Ardakani H. Income-related inequality in traffic accident health outcomes (Injury, disability and mortality): Evidence from the Nationwide Survey in Iran. Iran J Public Health. 2020;49:718–26. [PMC free article] [PubMed] [Google Scholar]
- 17.Edwards JG. Depression, antidepressants, and accidents. BMJ. 1995;311:887–8. doi: 10.1136/bmj.311.7010.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saade S, Parent-Lamarche A, Bazarbachi Z, Ezzeddine R, Ariss R. Depressive symptoms in helping professions: A systematic review of prevalence rates and work-related risk factors. Int Arch Occup Environ Health. 2022;95:67–116. doi: 10.1007/s00420-021-01783-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma N, Bairwa M, Gowthamghosh B, Gupta SD, Mangal DK. A bibliometric analysis of the published road traffic injuries research in India, post-1990. Health Res Policy Syst. 2018;16:18. doi: 10.1186/s12961-018-0298-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prakash O, Kukreti P. State of geriatric mental health in India. Curr Tran Geriatr Gerontol Rep. 2013;2:1–6. [Google Scholar]