Abstract
Objectives:
Late-life psychological symptoms in older adults such as depression and apathy have been increasingly associated with increased risk of cognitive and functional decline. The goal of this study was to conduct a confirmatory factor analysis of the Geriatric Depression Scale (GDS), pooling 3 unique cohorts of older adults to 1) develop a novel measurement model that distinguishes apathy from other domains of depression including dysphoria and cognitive concern and 2) evaluate if the measurement model distinguishes older adult populations with varied risk for cognitive decline.
Methods:
We pooled the baseline waves of three older adult cohorts (N=1421). With the aim of partitioning apathy from other constructs that compose the GDS and with a PCA suggesting 3-component solution, we then conducted a confirmatory factor analysis (CFA) using lavaan and less R.
Results:
CFA yielded 3 factors: dysphoria, apathy, and cognitive concern. All the dysphoria, apathy, and cognitive concern factors showed acceptable unidimensionality with α=.76, .59, and .54, respectively. The Cognitive Risk Primary Care cohort had significantly higher mean dysphoria, apathy and cognitive concern scales.
Conclusions:
This culturally, linguistically, and educationally diverse sample population yielded factors with acceptable reliability and good face validity. This strategy has resulted in a generalizable measurement model to identify people at risk for Alzheimer’s disease and related dementia. In particular, the apathy scale score can be used to identify older adults at risk for cognitive and functional decline across research and clinical settings.
Keywords: Geriatric Depression Scale, Apathy, Dysphoria, Factor Analysis, Older adults
Introduction
Approximately 6.7 million older Americans are currently living with Alzheimer’s dementia today, and the impact to individuals, families, and society is profound [1]. It not only results in cognitive decline but leads to distressing impairments in behavior and daily function. The burden of care falls on family members and caregivers, often resulting in emotional, physical, and financial strain [2]. Late-life psychological symptoms in older adults such as depression and apathy have been increasingly associated with increased risk of cognitive and functional decline.3,4 This association has even been conceptualization as Mild Behavioral Impairment, a predementia syndrome characterized by: “later life acquired, sustained and impactful neuropsychiatric symptoms of any severity that cannot be better accounted for by other formal medical and psychiatric nosology [5–7].”
Apathy, an important component of Mild Behavioral Impairment is a psychological syndrome characterized by lack of motivation, interest, goal-directed activity, and diminished emotion [8–12]. In contrast, the dysphoric component of depression is characterized by sadness, feelings of guilt, negative thoughts and feelings, helplessness, despair, pessimism, self-criticism, anxiety, and suicidal thoughts [13]. In older adults and people with neurologic illnesses, apathy has been linked to both functional and cognitive outcomes including incident frailty and dementia [14–20]. Current literature highlights apathy as a separate entity from depression, which is uniquely correlated (independent of depressive symptoms) to cognitive and functional decline in neurologic diseases like stroke, Parkinson’s disease (PD) and dementia [21–25]. Apathy predicts worse functional outcomes [26,27] and cognitive decline post stroke and in PD [19,27,28]. Further, recent studies indicate that apathy mediates the association between depression and cognitive decline in PD [29] and functional decline in persons with stroke and traumatic brain injury [30]. Funes and colleagues found that apathy mediates the relationship between depression and cognitive impairment [31].
Apathy is also a common behavioral phenomenon with a prevalence of 20-30% noted in community dwelling older adults [14,16,18]. Both van Dalen et al and Bock et al have identified an association between apathy in community dwelling older adults and incident dementia [15,32]. Furthermore, this association appears early in the dementia pathway as we found that apathy was associated with incident predementia syndromes [16]. Predementia syndromes are a constellation of cognitive deficits in varied domains that do not meet the criteria for dementia but are highly predictive of progression to dementia and may represent a prodromal phase [33–35]. Given an increasing body of literature that links apathy with incident dementia in community dwelling older adults, [15,20] assessment of apathy will be important in preventing or slowing progression to dementia, as it will allow for the identification of individuals who may benefit from treatment targeted to early neurodegenerative processes.
The majority of studies in community dwelling cohorts have employed varied measures of apathy, most of which are based on subscales of existing depression tools [14,16,18,20,36]. While an apathy specific tool like the Apathy Evaluation Scale is useful in clinical trials where apathy is the primary outcome, participants may find it burdensome to complete both depression and apathy assessment tools due to overlapping symptoms [37]. Moreover, assessing apathy based on existing depressive tools allows investigators to explore apathy in relation to other domains like dysphoria and cognitive concerns in well-established cohorts without increased questionnaire burden.
The Geriatric Depression Scale is a widely used tool, which was developed to assess depression, as a multi-domain construct, in older adults [38,39]. Data reduction methodologies, such as principal component analysis, have been frequently applied to identify distinct factors in the 30-item GDS Long Form [40–47]. These studies consistently identified dysphoria and withdrawal/apathy factors, even though the total number of factors varied across cohorts. A few studies have conducted confirmatory factor analysis to validate the factor structure of the GDS across cohorts [41,42,44]. However, the primary objective of these studies was not to parse out apathy, an important predictor of cognitive and functional decline.
The goal of this study was to conduct a confirmatory factor analysis of the GDS, pooling 3 unique cohorts of older adults (community dwelling, international south Indian, and cognitive risk in primary care) in order to 1) develop a novel measurement model that distinguishes apathy from other domains of depression including dysphoria and cognitive concern and 2) evaluate if the measurement model distinguishes older adult populations with varied risk for cognitive decline. The resultant measurement model should identify higher levels of apathy, dysphoria, and cognitive concern in higher risk populations.
Methods
Sample Population
We pooled the baseline waves of three Albert Einstein COM older adult cohorts. All study protocols were approved by the Albert Einstein College of Medicine Institutional Review Board and participants completed written consent.
Community Cohort
A sample of 538 community dwelling older adults (≥65 years old) without dementia enrolled in the Central Control of Mobility and Aging Study from 2011-2017 were included in this study. The primary aims of this prospective cohort study are to determine the cognitive and neural predictors of mobility in late life. As previously described, participants were contacted by mail and telephone from population lists in Westchester County, NY [48]. A structured telephone interview was administered to potential participants to obtain verbal assent, assess medical history and rule out dementia [49]. Participants who passed the telephone interview received comprehensive neuropsychological, psychological, and mobility assessments as well as a structured neurological examination. Community participants were followed yearly.
Kerala Study
We included a sample of 238 participants enrolled in the Kerala-Einstein Aging Study (KES), a community-based cohort study that was originally established in 2008 and is based in the Kozhikode district in Kerala, India. In 2023, KES received new funding to focus on novel risk factors (apathy and traumatic brain injury) and the brain pathology for motoric cognitive risk syndrome (MCR), a predementia syndrome characterized by the presence of slow gait and subjective cognitive concerns in individuals without dementia or disability [50]. Participants similarly completed comprehensive neuropsychological, psychological, and mobility assessments as well as magnetic resonance imaging of the brain.
Cognitive Risk Primary Care
Our study also included 600 participants enrolled in the 5-Cog Battery to improve detection of cognitive impairment and dementia study, a randomized controlled trial in predominantly Black and Hispanic older adults from Bronx County, NY who are presenting to primary care with cognitive concerns [51]. The study will validate a novel 5-minute cognitive assessment coupled with an electronic medical record-embedded decision tree to overcome the barriers of current cognitive assessment paradigms in primary care and facilitate improved dementia care.
Geriatric Depression Scale
Participants in all three cohorts completed the 30-item Geriatric Depression Scale (GDS) Long Form.39 The strength of the GDS in older adult populations is that it was developed for use in older adults including those with somatic and cognitive complaints. It utilizes a yes/no format and a score of 0–9 is considered normal; 10–19 indicates mild depression and ≥20 severe depression [52]. The GDS has been shown to be a reliable screening tool in people with mild cognitive impairment [53]. We utilized the GDS completed in the baseline assessment wave for all cohorts.
Statistical Analysis
Data from the three cohorts were pooled. After data harmonization, bivariate analyses by cohort were conducted using SPSS version 28 (SPSS Inc. Chicago, IL). Continuous variables were evaluated using ANOVA tests and categorical variables were evaluated using chi-square tests. Fisher’s exact test was used when the expected count for less than 5 in greater than 20% of the cells.
With the aim of partitioning apathy from other constructs that compose the GDS and with a PCA suggesting 3-component solution, we then conducted a confirmatory factor analysis (CFA) [54] using two R-based statistical analyses packages (i.e., less R and lavaan; RStudio, PBC, Boston, MA). Lavaan and lessR apply Maximum Likelihood Estimation (MLE), a non-linear optimization algorithm commonly used in latent variable analyses tasks, allowing selection of parameter values that make the observed data most probable, given a sample space (i.e., a listwise inter-item correlation matrix). Informed by prior literature on the psychometric properties of the GDS, we used the CFA to parse apathy from two other, substantive components or factors reported to comprise the GDS: dysphoria and cognitive concern. We dropped items with low item-factor correlations and/or if items loaded strongly on both factors. Decisions to retain or drop items were assessed iteratively. Dysphoria, apathy, and cognitive concern scale scores were calculated as the mean of the items for each case. Given that individual items were dichotomous, computed scale scores were continuous, ranging from 0 to 1. Mean dysphoria, apathy, and cognitive concern scale scores for the community and memory clinic cohorts were then compared using independent t-tests.
Results
Descriptive Analyses
Table 1 highlights the distinct characteristics of the three cohorts included in the analyses. Most notably the cohorts significantly differed by: mean age, with the Kerala cohort being the youngest (68.9 ± 5.39 years); gender, with the Community cohort having more women (72.2%); ethnicity, with the Cognitive Risk Primary Cohort being most diverse; and years of education, with the Kerala cohort having the fewest years of education (9.9 ± 3.95 years). In addition, both the Kerala and Cognitive Risk Primary Care cohorts endorsed higher levels of depression (7.5 ± 6.15 and 7.5 ± 6.21, respectively) than the Community cohort. Indicators of locomotor and cognitive and motor function also significantly varied by cohort with, the Cognitive Risk Primary Care cohort having the slowest mean gait velocity (64.4 cm/s ± 19.14) and the highest proportion of participants with MCR (17.3%).
Table 1:
Baseline Characteristics by Cohort.
| Community N=538 | Kerala N=238 | Cognitive Risk Primary Care N=600 | |||
|---|---|---|---|---|---|
| Variable | Mean (SD) | Mean (SD) | Mean (SD) | Statistic | P-Value |
| Age, yrs | 76.0 (6.49) | 68.9 (5.39) | 72.9 (6.38) | F=112.97 | <.001 |
| Female, %(N) | 55.2 (297) | 35.7 (85) | 72.2 (433) | F=99.70 | <.001 |
| Ethnicity % (N) | X2=1548.62 | <.001 | |||
| Non Hispanic White | 80.1 (431) | 0 | 1.0 (2) | ||
| Non Hispanic Black | 16.2 (87) | 0 | 38.3 (74) | ||
| Hispanic | 2.0 (11) | 0 | 54.4 (105) | ||
| International South Asian | 0 | 100 (238) | 0 | ||
| Education, yrs | 14.6 (2.95) | 9.9 (3.95) | 11.3 (4.11) | F=177.96 | <.001 |
| Geriatric Depression Score (0-30) | 4.7 (3.93) | 7.5 (6.15) | 7.5 (6.21) | F=39.79 | <.001 |
| Gait velocity, (cm/s) | 98.3 (22.44) | 74.9 (21.80) | 64.4 (19.14) | F=359.11 | <.001 |
| MCIa, % (N) | 13.9 (75) | 30.5 (58) | 10.8 (65) | <.001 | |
| MCRb, % (N) | 5.6 (30) | 5.5 (13) | 17.3 (104) | F=49.20 | <.001 |
cohorts described in methods section
MCI: Mild Cognitive Impairment
MCR: Motoric Cognitive Risk Syndrome
Confirmatory Factor Analysis
Table 2 illustrates the item to factor correlations for the 3 factors: dysphoria, apathy, and cognitive concern. The factors were named based on the clinical relevance of the items that loaded highest on to these specific factors. All the dysphoria, apathy, and cognitive concern factors showed acceptable unidimensionality [55] with α=.76, .59, and .54, respectively.
Table 2:
Confirmatory Factor Analysis item-Factor Correlation Matrix.
| Factor Description | Item description | Dysphoria | Apathy | Cognitive concern |
|---|---|---|---|---|
| Dysphoria (8 items; α=.76) | GDS16 Do you feel downhearted and blue? | .67 | .52 | .43 |
| GDS25 Do you frequently feel like crying? | .65 | .43 | .44 | |
| GDS10 Do you often feel helpless? | .63 | .46 | .44 | |
| GDS06 Are you bothered by thoughts you can t get out of your head? | .59 | .45 | .43 | |
| GDS09 Do you feel happy most of the time? | .49 | .53 | .41 | |
| GDS17 Do you feel pretty worthless the way you are now? | .44 | .33 | .37 | |
| GDS08 Are you afraid that something bad is going to happen to you? | .42 | .40 | .36 | |
| GDS07 Are you in good spirits most of the time? | .39 | .38 | .36 | |
| Apathy (7 items; α=.59) | GDS21 Do you feel full of energy? | .36 | .48 | .38 |
| GDS20 Is it hard for you to get started on new projects? | .38 | .48 | .47 | |
| GDS04 Do you often get bored? | .44 | .47 | .39 | |
| GDS28 Do you prefer to avoid social occasions? | .37 | .44 | .30 | |
| GDS02 Have you dropped many of your activities and interests? | .44 | .41 | .40 | |
| GDS19 Do you find life very exciting? | .26 | .35 | .24 | |
| GDS12 Do you prefer to stay at home rather than go out and do things? | .13 | .29 | .19 | |
| Cognitive concern (4 items; α=.54) | GDS26 Do you have trouble concentrating? | .45 | .44 | .61 |
| GDS30 Is your mind as clear as it used to be? | .33 | .44 | .55 | |
| GDS14 Do you feel you have more problems with memory than most? | .34 | .32 | .44 | |
| GDS29 Is it easy for you to make decisions? | .35 | .36 | .32 | |
| Dysphoria | 1.00 | .82 | .76 | |
| Apathy | .82 | 1.00 | .81 | |
| Cognitive concern | .76 | .81 | 1.00 |
Factor Scores
Factor scores were calculated for the participants using the mean of the factor item responses, such the scores are continuous values between 0 and 1. To assess face validity, mean factors scores were compared by cohort. Overall, the Cognitive Risk Primary Care cohort had significantly higher mean dysphoria, apathy and cognitive concern scales (Figure 1). Also, the apathy scale score was elevated across cohorts, highlighting the prevalence of this risk factor. Table 3 shows the post hoc analysis. Of note, the Kerala and Cognitive Risk Primary Care cohorts did not differ significantly dysphoria or apathy score, suggesting that the Kerala cohort may have a similar risk profile.
Figure 1:
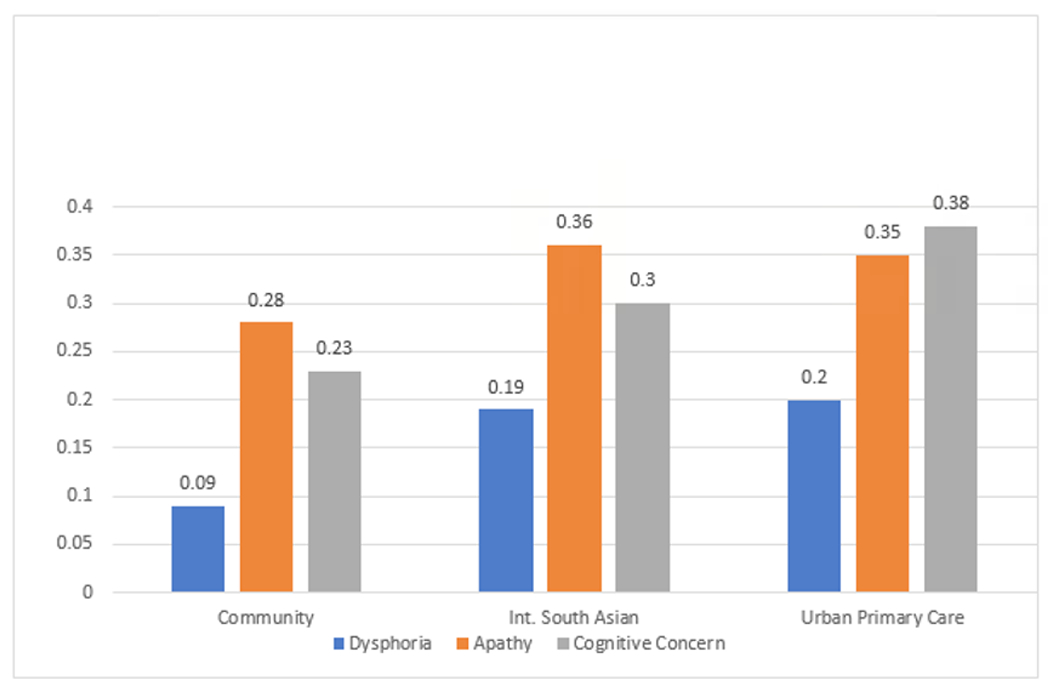
Comparison of Baseline Scale Scores by Cohort.
Table 3:
Bonferroni Multiple Comparisons of Mean Scale Scores by Cohort.
| Dependent Variable | Reference Cohort | Comparison Cohort | Mean Difference (I-J) | Std. Error | P-Value | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
|
Dysphoria |
Community | Kerala | −.101* | 0.01 | 0.00 | −0.14 | −0.07 |
| Cognitive Risk Primary Care | −.110* | 0.01 | 0.00 | −0.14 | −0.08 | ||
| Kerala | Community | .102* | 0.01 | 0.00 | 0.07 | 0.14 | |
| Cognitive Risk Primary Care | −0.01 | 0.02 | 1.00 | −0.05 | 0.03 | ||
| Cognitive Risk Primary Care | Community | .110* | 0.01 | 0.00 | 0.08 | 0.14 | |
| Kerala | 0.01 | 0.02 | 1.00 | −0.03 | 0.05 | ||
|
Apathy |
Community | Kerala | −.077* | 0.02 | 0.00 | −0.12 | −0.03 |
| Cognitive Risk Primary Care | −.065* | 0.02 | 0.00 | −0.11 | −0.02 | ||
| Kerala | Community | .077* | 0.02 | 0.00 | 0.03 | 0.12 | |
| Cognitive Risk Primary Care | 0.01 | 0.02 | 1.00 | −0.04 | 0.06 | ||
| Cognitive Risk Primary Care | Community | .065* | 0.02 | 0.00 | 0.02 | 0.11 | |
| Kerala | −0.01 | 0.02 | 1.00 | −0.06 | 0.04 | ||
| Cognitive Concern | Community | Kerala | −.068* | 0.02 | 0.02 | −0.13 | −0.01 |
| Cognitive Risk Primary Care | −.152* | 0.02 | 0.00 | −0.21 | −0.10 | ||
| Kerala | Community | .06800* | 0.02 | 0.02 | 0.01 | 0.13 | |
| Cognitive Risk Primary Care | −.08373* | 0.03 | 0.01 | −0.15 | −0.02 | ||
| Cognitive Risk Primary Care | Community | .15173* | 0.02 | 0.00 | 0.10 | 0.21 | |
| Kerala | .08373* | 0.03 | 0.01 | 0.02 | 0.15 | ||
Discussion
Our study utilized a pooled analysis of three diverse older adult cohorts to confirm the presence of 3 distinct factors: dysphoria, apathy, and cognitive concern in the GDS. This culturally, linguistically, and educationally diverse sample population yielded factors with acceptable reliability and good face validity. Elevated levels of apathy was also send across cohorts, highlighting apathy as a common risk factor for cognitive and functional decline across cohorts. Furthermore, comparison of mean scale scores by cohort confirmed our hypothesis that the Cognitive Risk Primary Care cohort would endorse the highest levels of dysphoria, apathy, cognitive concern. Our findings contribute to the literature demonstrating the stable presence of dysphoria and apathy factors in the GDS across diverse cohorts [41,42,44,56–59] and supports the use of an apathy subscale to identify risk populations in studies, where the Apathy Evaluation Scale may not be available.
One strength of this study was the ability to evaluate the GDS in over 1000 older adults across an American community dwelling, American primary care and international cohorts, rather than in individual cohorts. Strikingly, the reliability of the GDS subscale remained acceptable, despite the questionnaire being administered in three different languages. This strategy has resulted in a generalizable measurement model to identify people at risk for Alzheimer’s disease and related dementia. Secondly, our study underscores the utility of the GDS as an instrument to guide individual level clinical assessment, treatment monitoring, as well as to explore outcomes in prospective cohort studies. Specifically, apathy, an early risk factor for cognitive and functional decline,14,15,32,60 has often been assessed utilizing the GDS3A subscale. The GDS3A consists of extraction [61]) of the following three items from the Geriatric Depression Scale (GDS) Long Form [52] (score range 0–3 points) [62]: 1) Have you dropped many of your activities and interests? Positive response: Yes; 2) Do you prefer to stay at home, rather than going out and doing new things? Positive response: Yes; and 3) Do you feel full of energy? Positive response: No. A score of two or more indicates presence of apathy. But the GDS3A has variable sensitivity (29-69%) and specificity (85-93%) when compared to the AES [36,63] in a cohort of community-dwelling older adults.64 Our measurement model is a more robust approach to leveraging the GDS to assess apathy.
Our study had some notable limitations. In order to conduct this analysis, we had to harmonize data elements from different studies (such as ethnicity, education, MCI and MCR status), therefore data quality and data harmonization was limited. Also, cognitive assessments varied by cohort and therefore specific cognitive domains and global cognitive function could not be directly compared. Finally, the Apathy Evaluation Scale [65] was not available to evaluate the sensitivity and specificity of the apathy scale score.
Our future directions include further validation of the apathy scale score against the Apathy Evaluation Scale to establish the sensitivity, specificity, and potential cutpoints for the scale score. The role of dysphoria, apathy and cognitive concern will be explored using these scale scores to identify neural (vascular pathology, gray matter volume), biological (inflammatory cytokines, genomic and proteomic assays), and functional (gait velocity, falls) correlates in our current cohorts and other available older adult cohorts. Finally, we plan to pilot the GDS derived scale scores in clinical settings to identify those who would most benefit from early intervention to prevent cognitive and functional decline.
Conclusion
In this study, our pooled analysis of culturally, linguistically, and educationally diverse older adults confirmed the presence of 3 distinct factors: dysphoria, apathy, and cognitive concern in the GDS. This strategy has resulted in a generalizable measurement model to identify people at risk for Alzheimer’s disease and related dementia. In particular, the apathy scale score can be used to identify older adults at risk for cognitive and functional decline across research and clinical settings.
Acknowledgements
We thank all the participants of the Central Control of Mobility in Aging, Kerala-Einstein Aging Study, and 5-Cog Battery to improve detection of cognitive impairment and dementia study.
Funding
The three cohorts, Mirnova Ceide, Joe Verghese, and Emmeline Ayers were supported by funding from the National Institute of Aging (R01AG044007, R01AG039330, UH3NS105565, R01AG057548).
Footnotes
Conflict of Interest
The authors do not have any potential conflicts of interest that may influence the results or interpretations of the manuscript.
Ethical Considerations
All study protocols were approved by the Albert Einstein College of Medicine Institutional Review Board and participants completed written consent.
References
- 1.(2023) Alzheimer’s disease facts and figures. Alzheimer’s & dementia : the journal of the Alzheimer’s Association 19: 1598–1695. [DOI] [PubMed] [Google Scholar]
- 2.Aranda MP, Kremer IN, Hinton L, Zissimopoulos J ,Whitmer RA, et al. (2021) Impact of dementia: Health disparities, population trends, care interventions, and economic costs. J Am Geriatr Soc 69: 1774–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsuoka H, Yamaguchi H (2011) Path dependence in social and psychological risk factors for dementia. Dementia & neuropsychologia 5: 2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wuthrich VM, Rapee RM, Draper B, Brodaty H, Low LF, et al. (2019) Reducing risk factors for cognitive decline through psychological interventions: a pilot randomized controlled trial. Int psychogeriatri 31: 1015–1025. [DOI] [PubMed] [Google Scholar]
- 5.Ismail Z, Aguera-Ortiz L, Brodaty H, Cieslak A, Cummings J, et al. (2017) The Mild Behavioral Impairment Checklist (MBI-C): A Rating Scale for Neuropsychiatric Symptoms in Pre-Dementia Populations. J Alzheimer’s dis 56: 929–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ismail Z, Gatchel J, Bateman DR, Ferreira BR, Cantillon M, et al. (2017) Affective and emotional dysregulation as pre-dementia risk markers: exploring the mild behavioral impairment symptoms of depression, anxiety, irritability, and euphoria. Int Psychogeriatr 30: 185–196. [DOI] [PubMed] [Google Scholar]
- 7.Ismail Z, Smith EE, Geda Y, Sultzer D, Brodaty H, et al. (2016) Neuropsychiatric symptoms as early manifestations of emergent dementia: Provisional diagnostic criteria for mild behavioral impairment. Alzheimer’s Dement 12: 195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marin RS, Fogel BS, Hawkins J, Duffy J, Krupp B (1995) Apathy: a treatable syndrome. J neuropsychiatry clin neurosci 7: 23–30. [DOI] [PubMed] [Google Scholar]
- 9.Naarding P, Janzing JG, Eling P, van der Werf S, Kremer B (2009) Apathy is not depression in Huntington’s disease. J neuropsychiatry clin neurosci 21: 266–270. [DOI] [PubMed] [Google Scholar]
- 10.Oguru M, Tachibana H, Toda K, Okuda B, Oka N (2009) Apathy and depression in Parkinson disease. J geriatr psychiatry neurol 23: 35–41. [DOI] [PubMed] [Google Scholar]
- 11.Starkstein SE, Ingram L, Garau ML, Mizrahi R (2005) On the overlap between apathy and depression in dementia. J neurol, neurosurg, psychiatry 76: 1070–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marin RS (1990) Differential diagnosis and classification of apathy. Am J Psychiatry 147: 22–30. [DOI] [PubMed] [Google Scholar]
- 13.Camargo CHF, Serpa RA, Jobbins VA, Berbetz FA, Sabatini JS (2018) Differentiating Between Apathy and Depression in Patients With Parkinson Disease Dementia. Am j of Alzheimer’s dis other demen 33: 30–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayers E, Shapiro M, Holtzer R, Barzilai N, Milman S, et al. (2017) Symptoms of Apathy Independently Predict Incident Frailty and Disability in Community-Dwelling Older Adults. J clin psychiatry 78: 529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bock MA, Bahorik A, Brenowitz WD, Yaffe K (2020) Apathy and risk of probable incident dementia among community-dwelling older adults. Neurology 95: 3280–3287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ceïde ME, Warhit A, Ayers EI, Kennedy G, Verghese J (2020) Apathy and the Risk of Predementia Syndromes in Community Dwelling Older Adults. J Gerontol 75: 1443–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chilovi BV, Conti M, Zanetti M, Mazzù I, Rozzini L, et al. (2009) Differential impact of apathy and depression in the development of dementia in mild cognitive impairment patients. Dement and geriatr cogn disord 27: 390–398. [DOI] [PubMed] [Google Scholar]
- 18.Clarke DE, Ko JY, Lyketsos C, Rebok GW, Eaton WW (2010) Apathy and cognitive and functional decline in community-dwelling older adults: results from the Baltimore ECA longitudinal study. Int psychogeriatr 22: 819–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fitts W, Weintraub D, Massimo L, Chahine L, Chen-Plotkin A, et al. (2015) Caregiver report of apathy predicts dementia in Parkinson’s disease. Parkinsonism relat disord 21: 992–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Dalen JW, Van Wanrooij LL, van Charante EPM, Richard E, van Gool WA (2018) Apathy is associated with incident dementia in community-dwelling older people. Neurology 90: 82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maillet A, Krack P, Lhommee E, Météreau E, Klinger H, et al. (2016)The prominent role of serotonergic degeneration in apathy, anxiety and depression in de novo Parkinson’s disease. Brain 139: 2486–2502. [DOI] [PubMed] [Google Scholar]
- 22.Nagayama H, Maeda T, Uchiyama T, Hashimoto M, Nomoto N, et al. (2016) Anhedonia and its correlation with clinical aspects in Parkinson’s disease. J neurol sci 372: 403–407. [DOI] [PubMed] [Google Scholar]
- 23.Tang WK, Chen YK, Liang HJ, Chu WCW, Mok TVC, et al. (2013) Location of infarcts and apathy in ischemic stroke. Cerebrovasc dis 35: 566–571. [DOI] [PubMed] [Google Scholar]
- 24.Landes AM, Sperry SD, Strauss ME, Geldmacher DS (2001)Apathy in Alzheimer’s disease. J Am Geriatr Soc 49: 1700–1707. [DOI] [PubMed] [Google Scholar]
- 25.Starkstein SE, Petracca G, Chemerinski E, Kremer J (2001) Syndromic validity of apathy in Alzheimer’s disease. Am j psychiatry 158: 872–877. [DOI] [PubMed] [Google Scholar]
- 26.Hama S, Yamashita H, Shigenobu M, Watanabe A, Hiramoto K, et al. (2007) Depression or apathy and functional recovery after stroke. Int j geriatr psychiatry 22: 1046–1051. [DOI] [PubMed] [Google Scholar]
- 27.Mikami K, Jorge RE, Moser DJ, Jang M, Robinson RG (2013)Incident apathy during the first year after stroke and its effect on physical and cognitive recovery. Am j geriatric psychiatry 21: 848–854. [DOI] [PubMed] [Google Scholar]
- 28.Ziropadja L, Stefanova E, Petrovic M, Stojkovic T, Kostic VS (2012) Apathy and depression in Parkinson’s disease: the Belgrade PD study report. Parkinsonism relat disord 18: 339–342. [DOI] [PubMed] [Google Scholar]
- 29.Szymkowicz SM, Jones JD, Timblin H, Ryczek CA, Taylor WD, et al. (2021) Apathy as a Within-Person Mediator of Depressive Symptoms and Cognition in Parkinson’s Disease: Longitudinal Mediation Analyses. Am J Geriatri Psychiatry 30: 664–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Green SL, Gignac GE, Watson PA, Brosnan N, Becerra R, et al. (2021) Apathy and Depression as Predictors of Activities of Daily Living Following Stroke and Traumatic Brain Injuries in Adults: A Meta-Analysis. Neuropsychol rev 32: 51–69. [DOI] [PubMed] [Google Scholar]
- 31.Funes CM, Lavretsky H, Ercoli L, St Cyr N, Siddarth P (2018) Apathy Mediates Cognitive Difficulties in Geriatric Depression. Am Geriatr Psychiatry 26: 100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Van Dalen JW, van Wanrooij LL, Moll van Charante EP, Brayne C, van Gool WA, et al. (2018) Association of Apathy With Risk of Incident Dementia: A Systematic Review and Meta-analysis. JAMA Psychiatry 75: 1012–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Albert MS, DeKosky ST, Dickson D, Feldman HH, Gamst A, Nick CF, et al. (2011. )The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers dement 7: 270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Burns A, Zaudig M (2002) Mild cognitive impairment in older people. Lancet 2002 360: 1963–1965. [DOI] [PubMed] [Google Scholar]
- 35.Panza F, D’Introno A, Colacicco AM, Capurso C, Parigi DA, et al. (2006)Cognitive frailty: Predementia syndrome and vascular risk factors. Neurobiol aging 27: 933–940. [DOI] [PubMed] [Google Scholar]
- 36.Clarke DE, Ko JY, Kuhl EA, van Reekum R, Salvador R, et al. (2011) Are the available apathy measures reliable and valid? A review of the psychometric evidence. J psychosom res 70: 73–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ishii S, Weintraub N, Mervis JR (2009) Apathy: a common psychiatric syndrome in the elderly. J Am Med Dir Assoc 10: 381–393. [DOI] [PubMed] [Google Scholar]
- 38.Sheikh JI, Yesavage JA, Brooks JO 3rd, Friedman L, Gratzinger P, et al. (1991)Proposed factor structure of the Geriatric Depression Scale. Int psychogeriatr 3: 23–28. [DOI] [PubMed] [Google Scholar]
- 39.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al. (1982) Development and validation of a geriatric depression screening scale: a preliminary report 17: 37–49. [DOI] [PubMed] [Google Scholar]
- 40.Adams KB (2001) Depressive symptoms, depletion, or developmental change? Withdrawal, apathy, and lack of vigor in the Geriatric Depression Scale. Gerontologist 41: 768–777. [DOI] [PubMed] [Google Scholar]
- 41.Adams KB, Matto HC, Sanders S (2004) Confirmatory factor analysis of the geriatric depression scale. Gerontologist 44: 818–826. [DOI] [PubMed] [Google Scholar]
- 42.He J, Zhong X, Yao S (2019) Factor structure of the Geriatric Depression Scale and measurement invariance across gender among Chinese elders. Front psychol 238: 136–141. [DOI] [PubMed] [Google Scholar]
- 43.Kim G, DeCoster J, Huang CFH, Bryant AN (2007) A meta-analysis of the factor structure of the Geriatric Depression Scale (GDS): the effects of language. Int psychogeriatr 25:71–81. [DOI] [PubMed] [Google Scholar]
- 44.Cheng ST, Chan AC. Withdrawal, apathy and lack of vigor in late life depression: factorial validity and relationship to diagnosis. Aging & mental health 11: 532–537. [DOI] [PubMed] [Google Scholar]
- 45.Ertan T, Eker E (2000) Reliability, validity, and factor structure of the geriatric depression scale in Turkish elderly: are there different factor structures for different cultures? Int psychogeriatr 12: 163–172. [DOI] [PubMed] [Google Scholar]
- 46.Huang S-S, Liao Y-C, Wang W-F (2017)The Factor Structure for the Geriatric Depression Scale in Screening Depression in Taiwanese Patients with Very Mild to Moderate Dementia. International Journal of Gerontology 11: 36–40. [Google Scholar]
- 47.Salamero M, Marcos T (1992) Factor study of the Geriatric Depression Scale. Acta psychiatr Scand 86: 283–286. [DOI] [PubMed] [Google Scholar]
- 48.F-loltzer R, Mahoney JR, Izzetoglu M, Wang C, England S, (2015) Online fronto-cortical control of simple and attention-demanding locomotion in humans. NeuroImage 112: 152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Galvin JE, Roe CM, Powlishta KK, Coats MA, Muich SJ, et al. (2005) The AD8: a brief informant interview to detect dementia. Neurology 65: 559–564. [DOI] [PubMed] [Google Scholar]
- 50.Sathyan S, Ayers E, Blumen H, Blumen H, Weiss FE, et al. (2023) Epidemiology of Motoric Cognitive Risk Syndrome in the Kerala Einstein Study: Protocol for a Prospective Cohort Study. JMIR res protoc 12: 49933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chalmer R, Ayers E, Weiss EF, Malik R, Ehrlich A, et al. (2022) The 5-Cog paradigm to improve detection of cognitive impairment and dementia: clinical trial protocol. Neurodegener dis manag 12: 171–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al. (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J psychiatr res 17: 37–49. [DOI] [PubMed] [Google Scholar]
- 53.Debruyne H, Van Buggenhout M, Le Bastard N, Aries M, Audenaert M, et al. (2009) Is the geriatric depression scale a reliable screening tool for depressive symptoms in elderly patients with cognitive impairment? Int j geriatr psychiatr 24: 556–562. [DOI] [PubMed] [Google Scholar]
- 54.Sindik J (2013) Simple robust method for quasi-confirmatory factor analysis (three examples). Coll antropol 37: 1071–1080. [PubMed] [Google Scholar]
- 55.Streiner DL (2003) Starting at the beginning: an introduction to coefficient alpha and internal consistency. J pers assess 80: 99–103. [DOI] [PubMed] [Google Scholar]
- 56.Chau J, Martin CR, Thompson DR, Chang AM, Woo J (2006) Factor structure of the Chinese version of the Geriatric Depression Scale. Psychol health med 11: 48–59. [DOI] [PubMed] [Google Scholar]
- 57.Lai DW, Fung TS, Yuen CT (2005) The factor structure of a Chinese version of the Geriatric Depression Scale. International J psychiatry med 35: 137–148. [DOI] [PubMed] [Google Scholar]
- 58.Wongpakaran N, Wongpakaran T, Kuntawong P (2019) Evaluating hierarchical items of the geriatric depression scale through factor analysis and item response theory. Heliyon 5: e02300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhao H, He J, Yi J, Yao S (2019) Factor Structure and Measurement Invariance Across Gender Groups of the 15-Item Geriatric Depression Scale Among Chinese Elders. Front Psychol 10: 1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Clarke DE, Reekum R, Simard M, Streiner DL, Freedman M, et al. (2007) Apathy in dementia: an examination of the psychometric properties of the apathy evaluation scale. J neuropsychiatry clin neurosci 19: 57–64. [DOI] [PubMed] [Google Scholar]
- 61.Mitchell J, Mathews FHF, Yesavage JA (1993) A Multidimensional Examination of Depression among the Elderly. Research on Aging 15: 198–219. [Google Scholar]
- 62.Bertens AS, Moonen JE, de Waal MW, Foster-Dingley CJ, Ruijter WD, et al. (2016)Validity of the three apathy items of the Geriatric Depression Scale (GDS-3A) in measuring apathy in older persons. International j geriatr psychiatry 32: 421–428. [DOI] [PubMed] [Google Scholar]
- 63.Bertens AS, Moonen JE, de Waal MW, Foster-Dingley CJ, Ruijter WD, et al. (2017) Validity of the three apathy items of the Geriatric Depression Scale (GDS-3A) in measuring apathy in older persons. Int j geriatr psychiatry 32: 421–428. [DOI] [PubMed] [Google Scholar]
- 64.Van der Mast RC, Vinkers DJ, Stek ML, Bek MC, Westendorp RGF, et al. (2008) Vascular disease and apathy in old age. The Leiden 85-Plus Study. Int J geriatr psychiatry 23: 266–271. [DOI] [PubMed] [Google Scholar]
- 65.Marin RS, Biedrzycki RC, Firinciogullari S (1991) Reliability and validity of the Apathy Evaluation Scale. Psychiatry res 38: 143–162. [DOI] [PubMed] [Google Scholar]


