Abstract
Background
This study aimed to determine the status of in-hospital cardiac rehabilitation (CR) and hospital-associated disability (HAD) for patients with acute myocardial infarction (AMI) aged >80 years.
Methods and Results
This study involved the Japanese Registry of All Cardiac and Vascular Diseases and the Diagnosis Procedure Combination databases, and included patients who were hospitalized with AMI from April 2014 to March 2021. Patients were categorized by the daily amount of CR: NA, not applicable; Low, 20–30 min; Moderate, 30–40 min; and High, >40 min. Activities of daily living were assessed using the Barthel index (BI) score, and evaluated at both admission and discharge. This study defined HAD as a ≥5-point decrease in BI score at discharge compared with admission. A total of 12,061 eligible patients were selected (age 83.0 years; 36.4% female), of which 2.7% had HAD (NA, 2.0%; Low, 4.7%; Moderate, 2.6%; High, 2.6%). The Low group was more likely to develop HAD. Chronological trends in hospital stay and incidence rate of HAD gradually decreased with the increased in-hospital CR participation rate. The multivariable logistic regression analysis revealed that the daily amount of CR was selected as an independent associated factor for preventing HAD (odds ratio 0.737; 95% confidence interval 0.567–0.960; P=0.023).
Conclusions
Our results revealed that higher amounts of in-hospital CR for patients with AMI should be performed, especially in octogenarians.
Key Words: Acute myocardial infarction, Hospital-associated disability, In-hospital cardiac rehabilitation, Octogenarian
The number of patients with acute myocardial infarction (AMI), especially older patients, has gradually increased with aging demographics in Japan, despite the recent dramatic advances in pharmacological treatment and cardiovascular intervention.1 Older patients frequently have several comorbidities, including kidney disease, pulmonary disease, and physical frailty.2 Therefore, older patients are more likely to experience declines in physical function at discharge due to excessive bed rest or physical inactivity during hospitalization.3–5
Hospital-associated disability (HAD), which is a decline in activities of daily living (ADL) during hospitalization, is a widely accepted concept among older hospitalized patients.6 The incidence of HAD in older patients (i.e., age >65 years) who have received acute-phase medical treatment is approximately 10–30% in patients with heart failure (HF), transcatheter aortic valve implantation (TAVI), and cardiovascular surgery.7–10 However, these reports are inconsistent, including a single-center registry, relatively smaller sample size, and different definition criteria of HAD. Two major large-scale nationwide observational studies revealed that prevalence rates of HAD were 7%11 and 37.1%12 in older patients with HF, but the data of older patients with AMI remains unclear. Patients with AMI are clinically characterized by short hospital stays, which are becoming shorter annually. While the length of hospital stay has been shortened, HAD in the older population has recently been considered as a major problem in Japanese society.
Therefore, this study aimed to determine the status of in-hospital cardiac rehabilitation (CR) and HAD in patients with AMI aged >80 years, also known as octogenarians, using a large real-world nationwide database in Japan.
Methods
Data Sources
This study involved the Japanese Registry of All Cardiac and Vascular Diseases and the Diagnosis Procedure Combination (JROAD-DPC) discharge database as data sources, which is a nationwide registry, and a medical database with information on admission and discharge for cardiovascular diseases, clinical examinations and treatment status, patient status and hospital overview that is collected by the Japanese Circulation Society (JCS).13 JROAD specifically covers all cardiovascular training facilities, and DPC data is collected from more than 1,000 facilities of JROAD annually.13,14 The database consists of inpatient information, including age, sex, body mass index (BMI), medical diagnosis, performance scale for ADL, comorbidities, treatments, medications, discharge status, and hospitalization costs. Each patient’s principal diagnosis or comorbidity was coded using the International Classification of Diseases and Related Health Problems, 10th revision. Informed consent was waived as no personal information was included. Patient data were anonymized using original DPC data.
Study Design and Population
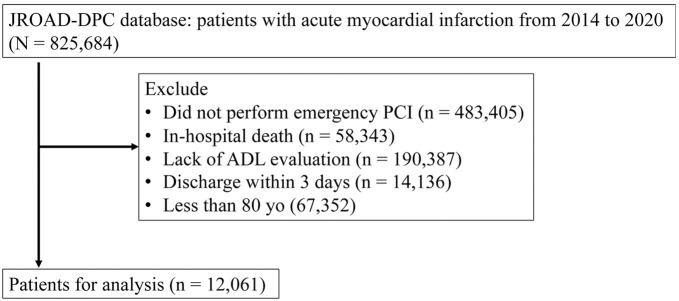
This retrospective nationwide registry study used the JROAD-DPC database. Detailed patient-level analysis was conducted to determine the association of the daily amount of in-hospital CR on the incidence of HAD during the perioperative stages of the percutaneous coronary intervention (PCI) procedure. Figure shows the selection methodology of the study participants. Data extraction targeted patients who underwent emergency PCI under disease codes I21 or I22 from April 2014 to March 2021. This study excluded patients who were aged <80 years of age, who died during hospitalization, were diagnosed with coronavirus disease-2019 during hospitalization, or were missing information in their records, including age, BMI, emergency admission status, and ADL levels measured using the BI score. Patients whose hospital stay was ≤3 days were excluded due to the ambiguous effects of in-hospital CR and the brief hospitalization durations on HAD outcomes.
Figure.
Flow chart for the inclusion of study participants. ADL, activities of daily living; JROAD-DPC, Japanese Registry of All Cardiac and Vascular Diseases-Diagnosis Procedure Combination; PCI, percutaneous coronary intervention.
The Ethics Committee of Seijo University, under the stewardship of the principal investigator (N.F.), approved the protocol of this study (Institutional Study No. 2022C0015). Additionally, endorsements were conferred by the Japanese Association of Cardiac Rehabilitation and the JCS. The design of the JROAD-DPC study adhered to the ethical standards outlined in the World Medical Association’s Declaration of Helsinki. The National Cerebral and Cardiovascular Center in Osaka, Japan, granted Institutional Review Board approval. The board dispensed with the need for individual informed consent, adopting an ‘opt-out’ approach, due to the anonymization of personally identifiable information within the study.
Clinical Outcome Measures
Data collection encompassed several parameters: patient demographics, comorbidity, medication, mechanical treatment (i.e., percutaneous cardiopulmonary support/intra-aortic balloon pump, hemodialysis, and ventilator), perioperative complications (i.e., pneumonia, delirium, and stroke), discharge locations, length of hospital stay, and associated hospitalization costs. The hospitalization costs included both bundled payments and fee-for-service transactions, with the exclusion of costs related to meals.
ADL Assessment and Definition of HAD
ADL before hospitalization and at discharge were evaluated using the Barthel index (BI),15 consisting of 10 items including eating, transferring, and toileting, and scored on a 4-point scale (15, 10, 5, and 0 points) according to ability. In general, BI scores of ≥85, 60, 40, and 0 out of a possible 100 points are considered as independent, partially independent, requiring major assistance, and requiring total assistance with ADL, respectively. The present study, with reference to previous studies,9,12 defined HAD as a decrease of at least 5 points on the BI at discharge compared with the BI in a stable condition before hospitalization.
Statistical Analysis
Categorical variables are presented as number and percentages, whereas continuous variables are presented as means±standard deviation, or medians (interquartile range). We categorized all patients according to the daily amount of in-hospital CR as: NA, not applicable; low, 1.0–1.5 units per day (1 unit for a 20-min program); moderate, 1.5–2.0 units per day; and high, >2.0 units per day. A chi-square test, 1-way analysis of variance, and Kruskal-Wallis test were conducted to compare the occurrence of HAD among groups. Chronological trends in HAD incidence, length of hospital stay, and in-hospital CR participation rate rates were also examined.
Bivariable and multivariable logistic regression analyses were conducted to investigate the association of the amount of in-hospital CR with the occurrence of HAD. The multivariable logistic regression model was adjusted for a comprehensive set of baseline covariates, including age, sex, BMI, BI at admission, comorbidity profile, prescribed medications, and perioperative complications.
Statistical Package for the Social Sciences version 26.0 software package (SPSS Inc., Tokyo, Japan) was used for statistical analyses, and statistical significance was set at P values of <0.05.
Results
Baseline Characteristics
The analysis included 12,061 patients of the initial 825,684 patients screened (Figure). The median (interquartile range) for age was 83 (81–86) years, BMI was 22.6 (20.3–24.6) kg/m2, and patients were predominantly male (63% of the patients). The BI scores at admission were 100 (100–100) points. Prevalence of the comorbid conditions of hypertension, dyslipidemia, diabetes, and HF were 72%, 85%, 72%, and 34%, respectively. The median length of hospital stay was 12 (9–17) days.
Within the 12,061 patients analyzed, 4,815 (40.0%) patients were in the NA group, 2,636 (21.8%) in the low group, 2,495 (20.6%) in the moderate group, and 2,115 (17.6%) in the high group. Table 1 shows the baseline demographic and clinical characteristics of the study participants. The incident rate of HAD was 2.6% in total participants, 4.7% in the low group, and 5.4% in the low group with females. Table 2 illustrates the chronological trends in HAD incidence, length of hospital stay, and in-hospital CR participation rate. The in-hospital CR participation rate increased with the chronological transition, whereas the length of hospital stay and the incidence of HAD demonstrated a decreasing trend.
Table 1.
Demographic and Clinical Characteristics of Octogenarian Patients With AMI According to Daily Amount of In-Hospital CR
| Total | Did not participate |
Low (1.0–1.49 units) |
Moderate (1.5–1.99 units) |
High (≥2.0 units) |
P value | |
|---|---|---|---|---|---|---|
| n | 12,061 | 4,815 | 2,636 | 2,495 | 2,115 | |
| Age (years) | 83 [81–86] | 83 [81–86] | 84 [82–87] | 83 [82–86] | 83 [81–86] | <0.001 |
| Male (%) | 63.3 | 64.9 | 61.9 | 61.8 | 63.5 | 0.220 |
| BMI | 22.5 [20.5–24.6] | 22.6 [20.7–24.7] | 22.5 [20.6–24.5] | 22.4 [20.6–24.4] | 22.5 [20.3–24.6] | <0.001 |
| Charlson index | 2 [1–3] | 2 [1–3] | 2 [1–3] | 2 [1–3] | 2 [1–3] | 0.566 |
| Comorbidity (%) | ||||||
| Diabetes | 29.7 | 30.7 | 28.1 | 29.1 | 29.8 | 0.143 |
| Hypertension | 71.9 | 70.8 | 72.4 | 72.1 | 73.4 | <0.001 |
| Hyperlipidemia | 67.4 | 43.4 | 38.8 | 40.3 | 40.6 | <0.001 |
| Hyperuricemia | 5.7 | 5.7 | 6.0 | 5.5 | 5.4 | 0.773 |
| CVD | 0.9 | 0.9 | 0.8 | 0.8 | 1.3 | 0.220 |
| CKD | 7.4 | 8.1 | 7.8 | 7.5 | 5.2 | <0.001 |
| Pulmonary disease | 4.3 | 4.1 | 4.7 | 4.0 | 4.3 | 0.577 |
| Medication (%) | ||||||
| Antiplatelet | 64.4 | 62.5 | 61.3 | 66.8 | 69.7 | <0.001 |
| ACE/ARB | 45.5 | 39.5 | 46.6 | 50.4 | 52.2 | <0.001 |
| β-blocker | 42.1 | 35.0 | 45.3 | 47.7 | 47.9 | <0.001 |
| Statin | 57.0 | 52.4 | 55.8 | 61.0 | 64.2 | <0.001 |
| Oral DM | 14.9 | 14.1 | 14.0 | 16.0 | 16.8 | <0.001 |
| Treatment (%) | ||||||
| Dialysis | 2.6 | 3.4 | 2.8 | 1.8 | 1.2 | <0.001 |
| Respirator | 7.0 | 4.4 | 10.2 | 7.6 | 8.5 | <0.001 |
| IABP/PCPS | 7.0 | 4.2 | 9.2 | 8.4 | 9.0 | <0.001 |
| Discharge location (%) | <0.001 | |||||
| Home | 95.2 | 96.4 | 92.6 | 95.7 | 95.0 | |
| Transfer | 3.4 | 2.4 | 5.3 | 3.0 | 3.4 | |
| Nursing facility | 1.4 | 1.1 | 2.0 | 1.2 | 1.5 | |
| Hospital stay (days) | 12 [8–17] | 8 [5–14] | 14 [10–19] | 14 [8–16] | 15 [11–20] | <0.001 |
| BI at admission | 100 [75–100] | 100 [75–100] | 100 [55–100] | 100 [55–100] | 100 [45–100] | <0.001 |
| BI at discharge | 100 [75–100] | 100 [60–100] | 100 [55–100] | 100 [45–100] | 100 [60–100] | <0.001 |
| HAD, total (%) | 2.6 | 2.0 | 4.7 | 2.5 | 2.5 | <0.001 |
| HAD, male (%) | 1.9 | 1.6 | 2.7 | 1.9 | 1.9 | <0.001 |
| HAD, female (%) | 3.8 | 2.6 | 5.4 | 3.6 | 3.5 | <0.001 |
Data are presented as percentages, or median [interquartile range]. Low, 1.0–1.5 units per day; Moderate, 1.5–2.0 units per day, and High, >2.0 units per day. ACE, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; BI, Barthel index; BMI, body mass index; CKD, chronic kidney disease; CR, cardiac rehabilitation; CVD, cerebrovascular disease; DM, diabetes; HAD, hospital-associated disability; IABP, intra-aortic balloon pump; PCPS, percutaneous cardiopulmonary support.
Table 2.
Chronological Trends in Percentage of CR Participation Rate, Length of Hospital Stay, and Incidence Rate of HAD
| 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | |
|---|---|---|---|---|---|---|---|
| In-hospital CR participation rate (%) | 45.2 | 53.0 | 57.6 | 59.4 | 63.1 | 64.4 | 69.1 |
| Length of hospital stay (days) | 15.3 | 14.7 | 14.5 | 14.6 | 14.3 | 13.7 | 13.3 |
| Incidence rate of HAD (%) | 3.4 | 3.5 | 3.2 | 2.6 | 2.5 | 2.4 | 2.1 |
CR, cardiac rehabilitation; HAD, hospital-associated disability.
Table 3 shows the multivariable logistic regression analysis with HAD occurrence as the outcome in 7,246 patients who participated in the in-hospital CR. The daily amount of in-hospital CR was selected as an independent related factor after adjustment for confounding factors.
Table 3.
Bivariable and Multivariable Logistic Regression Analysis for HAD With Daily Amount of In-Hospital CR
| B | SE | P value | OR | 95% CI of OR | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Bivariable | −0.219 | 0.087 | 0.012 | 0.803 | 0.677 | 0.953 |
| Multivariable | −0.305 | 0.134 | 0.023 | 0.737 | 0.567 | 0.960 |
Adjusted model: age, sex, BMI, BI at admission, comorbidity profile, prescribed medications, and perioperative complications. CI, confidence interval; OR, odds ratio. Other abbreviations as in Table 1.
Discussion
The results of the present study using the JROAD-DPC database indicate that HAD incidence was 2.6–5.4% in octogenarians with AMI. Furthermore, the chronological transition demonstrated an increasing in-hospital CR participation rate and a decreasing trend in HAD incidence. To the best of our knowledge, this is the first study to focus on patients with AMI aged >80 years and to determine the incidence of HAD.
Participation Rate of In-Hospital CR in Octogenarians With AMI
The results of this study indicate that the non-participation rate of in-hospital CR was approximately 40%; this slightly higher non-participation rate may have influenced the results. Previous findings of the JROAD-DPC database reported that the participation rate of in-hospital CR in patients with acute coronary syndrome was 44%.16 In this study, a high proportion was observed due to the inclusion of patients aged >80 years. Moreover, the length of hospital stay in AMI patients has been decreasing each year, as shown in Table 2, with the NA group having an average of 8 days. This reflects the shorter duration of the in-hospital CR implementation period. Therefore, it was considered that these results reflect the real-world of AMI in Japan.
Incidence Rate of HAD in Octogenarians With AMI
The results of this study revealed that the prevalence of HAD was 2.6–5.4%. The decline in ADL associated with hospitalization is of great concern in Japan and other developed countries with aging populations. The incidence of HAD was 10–38% in older patients with HF,7,8,12 18.6% in post-cardiac surgery,10 and 18–24% in post-TAVI,9,16 with lower rates in octogenarians with AMI. The relatively less-invasive acute care and shorter hospital stay may be associated with the lower incidence of HAD in patients with AMI. These aforementioned previous studies included patients who underwent in-hospital rehabilitation treatment, but the implementation rate of the in-hospital rehabilitation setting is approximately 40% for HF and 74% for post-cardiac surgery;17 thus, not all patients are included in the previous study. A previous report on older patients with HF using DPC data reported a 7% incidence of HAD,11 and the incidence may be lower with DPC data. This study revealed a 60% in-hospital CR participation rate, and the incidence of HAD ranged from 2.7–5.4% when assessed in the group that had in-hospital CR, indicating that the incidence of HAD in octogenarians with AMI is lower than in older patients with HF or those with TAVI.
Moreover, the in-hospital CR participation rate demonstrated an increase from 42.5% to 69.1% during the 7-year study period, and the average length of hospital stay and the incidence rate of HAD exhibited a decrease from 15.3 to 13.7 days and 3.6% to 2.6%, respectively. This is a retrospective observational study; thus, a causal-effect association of increased in-hospital CR participation rate with decreased length of hospital stay and decreased incidence of HAD cannot be shown. A previous study reported that early mobilization was an associated factor of independence in ADL at discharge and length of hospital stay18 and indicated that the increased in-hospital CR participation rate may have contributed to the lower HAD incidence.
Factors Associated With HAD Incidence
The results of this study determined the daily amount of in-hospital CR as an independent factor associated with HAD incidence. Previous studies have reported older age, female sex, lower BMI, comorbidities, lower pre-hospital ADL, and low cognitive function as factors associated with HAD incidence in older patients with HF.11,12 Moreover, an association between HAD and in-hospital physical activity, including step count19 and rehabilitation time,20 has previously been reported among patients with HF. Thus, this study supports the previous study in terms of independent associated factors of HAD in octogenarians with AMI. Some recent studies have revealed that early rehabilitation (within 3 days of admission) reduced hospital stay and readmissions after discharge.21,22 These results indicate that the amount of in-hospital CR may be important in preventing HAD in octogenarians with AMI.
Study Limitations
This study had several potential limitations. First, the exclusion of patients with missing data for the BI score at admission introduces the potential for selection bias in this study based on DPC database. Second, a retrospective study may leave residual bias from unidentified confounders, including severity of AMI, CR program details, patient’s physical and psychological conditions, and hospital level. Therefore, we cannot describe the relationship between HAD and these confounding factors. Third, since the subitems of the BI are unclear, it is unknown whether those items are likely to decline. Last, the absence of pre-admission BI scores guided us to rely on the differential BI at discharge relative to admission as a proxy for HAD, in line with a previous study. Despite these limitations, this is the first study to reveal the prevalence of HAD in octogenarians with AMI in a large nationwide database. The JROAD-DPC database obtained data from 1,231 hospitals using the Japanese DPC/PDPS claim data. In Japan, 1,755 hospitals used the DPC/PDPS system in 2019.12 Therefore, the JROAD-DPC database covered 70% of Japanese cardiovascular practice and is considered as real-world clinical data in Japan. Additionally, Japan is the front-runner of super-aged societies; thus, these results can help future clinical practice globally.
Conclusions
Our results from a nationwide inpatient database revealed a 2.0–5.6% prevalence rate of HAD in octogenarians with AMI. Furthermore, the implementation rate of in-hospital CR increased, the incidence of HAD decreased in the chronological transition, and the amount of daily CR was selected as a factor associated with HAD incidence. Additionally, our results also indicated that adequate time for in-hospital CR might be effective at preventing HAD in octogenarians with AMI.
Sources of Funding
None.
Disclosures
Y.M., Y. Ohya, S. Miura and H.I. are members of Circulation Reports’ Editorial Team.
IRB Information
The study protocol was approved by the Ethics Committee of Seijo University (Institutional Study No. 2022C0015).
Acknowledgments
We appreciate the contributions of all investigators, clinical research coordinators, and data managers involved in the JROAD-DPC study.
References
- 1. Yasuda S, Miyamoto Y, Ogawa H.. Current status of cardiovascular medicine in the aging society of Japan. Circulation 2018; 138: 965–967. [DOI] [PubMed] [Google Scholar]
- 2. Murad K, Kitzman DW.. Frailty and multiple comorbidities in the elderly patient with heart failure: Implications for management. Heart Fail Rev 2012; 17: 581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Creditor MC.. Hazards of hospitalization of the elderly. Ann Intern Med 1993; 118: 219–223. [DOI] [PubMed] [Google Scholar]
- 4. Graf C.. Functional decline in hospitalized older adults. Am J Nurs 2006; 106: 58–67. [DOI] [PubMed] [Google Scholar]
- 5. Covinsky KE, Pierluissi E, Johnston CB.. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA 2011; 306: 1782–1793. [DOI] [PubMed] [Google Scholar]
- 6. Yaku H, Ozasa N, Morimoto T, Inuzuka Y, Tamaki Y, Yamamoto E, et al.. Demographics, management, and in-hospital outcome of hospitalized acute heart failure syndrome patients in contemporary real clinical practice in Japan: Observations from the prospective, multicenter Kyoto congestive heart failure (KCHF) registry. Circ J 2018; 82: 2811–2819. [DOI] [PubMed] [Google Scholar]
- 7. Takabayashi K, Kitaguchi S, Iwatsu K, Morikami Y, Ichinohe T, Yamamoto T, et al.. A decline in activities of daily living due to acute heart failure is an independent risk factor of hospitalization for heart failure and mortality. J Cardiol 2019; 73: 522–529. [DOI] [PubMed] [Google Scholar]
- 8. Saitoh M, Saji M, Kozono-Ikeya A, Arimitsu T, Sakuyama A, Ueki H, et al.. Hospital-acquired functional decline and clinical outcomes in older patients undergoing transcatheter aortic valve implantation. Circ J 2020; 84: 1083–1089. [DOI] [PubMed] [Google Scholar]
- 9. Morisawa T, Saitoh M, Otsuka S, Takamura G, Tahara M, Ochi Y, et al.. Perioperative changes in physical performance affect short-term outcome in elderly cardiac surgery patients. Geriatr Gerontol Int 2021; 21: 676–682. [DOI] [PubMed] [Google Scholar]
- 10. Ogawa M, Yoshida N, Nakai M, Kanaoka K, Sumita Y, Kanejima Y, et al.. Hospital-associated disability and hospitalization costs for acute heart failure stratified by body mass index: Insight from the JROAD/JROAD-DPC database. Int J Cardiol 2022; 367: 38–44. [DOI] [PubMed] [Google Scholar]
- 11. Takahashi T, Iwata K, Morisawa T, Kato M, Kono Y, Taya M, et al.. Incidence of hospitalization-associated disability in older patients with heart failure. Circ J 2024; 88: 672–679. [DOI] [PubMed] [Google Scholar]
- 12. Yasuda S, Nakao K, Nishimura K, Miyamoto Y, Sumita Y, Shishido T, et al.. The current status of cardiovascular medicine in Japan: Analysis of a large number of health records from a nationwide claim-based database, JROAD-DPC. Circ J 2016; 80: 2327–2335. [DOI] [PubMed] [Google Scholar]
- 13. Yasuda S, Miyamoto Y, Ogawa H.. Current status of cardiovascular medicine in the aging society of Japan. Circulation 2018; 138: 965–967. [DOI] [PubMed] [Google Scholar]
- 14. Mahoney FI, Barthel DW.. Functional evaluation: The Barthel index. Md State Med J 1965; 14: 61–65. [PubMed] [Google Scholar]
- 15. Kono Y, Mukaino M, Ozawa Y, Mizutani K, Senju Y, Ogasawara T, et al.. Clinical impact of non-lying time on hospital-associated functional decline in older patients undergoing transcatheter aortic valve implantation. Heart Vessels 2024; 39: 266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kanaoka K, Iwanaga Y, Fukuma N, Nakai M, Sumita Y, Nishioka Y, et al.. Trends and factors associated with cardiac rehabilitation participation: Data from Japanese nationwide databases. Circ J 2022; 86: 1998–2007. [DOI] [PubMed] [Google Scholar]
- 17. Watanabe S, Hirasawa J, Naito Y, Mizutani M, Uemura A, Nishimura S, et al.. Association between the early mobilization of mechanically ventilated patients and independence in activities of daily living at hospital discharge. Sci Rep 2023; 13: 4265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Agmon M, Zisberg A, Gil E, Rand D, Gur-Yaish NG, Azriel M.. Association between 900 steps a day and functional decline in older hospitalized patients. JAMA Intern Med 2017; 177: 272–274. [DOI] [PubMed] [Google Scholar]
- 19. Kato M, Mori Y, Watanabe D, Onoda H, Fujiyama K, Toda M, et al.. Relationship between average daily rehabilitation time and decline in instrumental activity of daily living among older patients with heart failure: A preliminary analysis of a multicenter cohort study, SURUGA-CARE. PLoS One 2021; 16: e0254128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kono Y, Izawa H, Aoyagi Y, Ishikawa A, Sugiura T, Mori E, et al.. Predictive impact of early mobilization on rehospitalization for elderly Japanese heart failure patients. Heart Vessels 2020; 35: 531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fleming LM, Zhao X, DeVore AD, Heidenreich PA, Yancy CW, Fonarow GC, et al.. Early ambulation among hospitalized heart failure patients is associated with reduced length of stay and 30-day readmissions. Circ Heart Fail 2018; 11: e004634. [DOI] [PubMed] [Google Scholar]
- 22. e-Stat.. Statistics of Japan. 2022. https://www.e-stat.go.jp/en/ (accessed July 30, 2024).