Abstract
This study examined concordance between physiological arousal and subjective distress during a laboratory challenge task. Data were collected during the multisite VA Cooperative Study 334 in the early 1990s examining psychophysiological arousal among combat-exposed Vietnam veterans with (n = 775) and without (n = 369) posttraumatic stress disorder (PTSD). Study participants were presented with 6 standardized neutral scenes and 6 standardized combat scenes. Participants provided a subjective rating of distress after each slide. During the presentation, levels of heart rate (HR) and skin conductance (SC) were recorded. Using linear mixed effects modeling, both HR level and SC level exhibited significant positive associations with subjective distress ratings (pr = .33, p < .001 and pr = .19, p < .001, respectively). Individuals with PTSD demonstrated greater concordance between their distress ratings and SC level during exposure to combat slides than participants without PTSD (pr = .28, p < .001 vs. pr = .18, p < .001). Although a significant association was found between subjective distress and HR reactivity and SC reactivity, these findings were not moderated by PTSD status. The results of these analyses suggest that patients’ reports of distress during exposure-based treatments might serve as approximate measures of actual physiological arousal.
In exposure-based treatments for posttraumatic stress disorder (PTSD), it is standard practice to have a client rate the degree of distress or discomfort that he or she experiences while confronting trauma memories and other trauma-related stimuli (e.g., Foa, Hembree, & Rothbaum, 2007; Shapiro, 1995). This practice reflects an assumption that higher self-report ratings accurately indicate higher levels of physiological activity (e.g., sweaty palms, heart palpitations; see Foa & Rothbaum, 1998). The extent to which this assumption, however, is correct remains unclear because very few studies have tested this hypothesis empirically.
To date, only three studies within the PTSD literature have examined the question of concordance between self-reported distress and physiological arousal. In the first study, Blanchard, Hickling, Taylor, Loos, and Gerardi (1994) found a significant, moderately sized correlation (r = .39, p < .01, n = 50) between subjective distress and heart rate (HR) levels during a trauma imagery task for motor vehicle accident victims. Subsequently, McDonagh-Coyle et al. (2001) examined correlations between subjective emotional distress and heart rate change scores (i.e., imagery period–baseline period) among victims of childhood sexual abuse during a script-driven imagery task. These investigators found no significant associations between HR reactivity and subjective distress during the trauma imagery condition. Most recently, among a sample of police officers, Pole, Neylan, Best, Orr, and Marmar (2003) found no significant correlations between subjective distress and skin conductance (SC) reactivity. Although each of these studies included samples with a range of PTSD symptoms, none of them looked at whether carrying a PTSD diagnosis affected concordance between self-reported distress and physiological arousal.
There may be several explanations for the discrepant findings across these three studies, including using only single data points to compute correlations between self-report ratings and physiological indicators, obtaining self-report ratings long after the emotion-eliciting stimuli were presented, not controlling for medication use or comorbid psychiatric conditions, and different self-report measures used across studies. One explanation that might be more notable than the others, however, is that these three studies differed in whether they examined the extent to which physiological levels (Blanchard et al., 1994) or physiological reactivity (McDonagh-Coyle et al., 2001; Pole et al., 2003) was associated with participants’ self-reports. Physiological level refers to phasic activity, which is an individual’s evoked response to a specific stimulus (Stern, Ray, & Quigley, 2001). In contrast, physiological reactivity refers to the change between phasic activity and tonic activity; that is, the change between an individual’s evoked response and the background level of activity which occurs prior to presentation of a stimulus (Stern et al., 2001).
From a statistical perspective, given that the possible range of values for physiological reactivity is more restricted than the possible range of values for physiological level, we might expect that self-reports of distress would be more highly associated with physiological levels than with physiological reactivity. This possibility is consistent with the results of the available studies that have examined this question (i.e., Blanchard et al., 1994; McDonagh-Coyle et al., 2001; Pole et al., 2003). Because only three studies, however, have examined the degree to which self-reported distress is concordant with either physiological levels or reactivity in PTSD samples, and none have examined the extent to which self reported distress is concordant with physiological levels and reactivity within the same sample, more research is needed to determine which possibility is correct. Notably, any future research should attempt to answer this question by conducting concordance analyses for both physiological levels and reactivity using the same data, examining whether PTSD symptoms affect this relationship, and using data analytic techniques that take better advantage of multiple data points and control for potentially important comorbid conditions.
The current investigation examined the degree to which physiological levels and reactivity corresponded to self-reported distress during exposure to trauma reminders as part of a laboratory challenge procedure administered to veterans with and without PTSD. Linear mixed effects modeling for longitudinal analysis was used as the analytic technique (cf. Rellini, McCall, Randall, & Meston, 2005) to take full advantage of multiple data points for each measure. Given that the associations between the various response channels are stronger when the elicited emotion is sufficiently intense (Ludwick-Rosenthal & Neufeld, 1985; Mauss, Levenson, McCarter, Wilhelm, & Gross, 2005), we hypothesized that participants would demonstrate greater concordance between self-reported distress and physiological activity during exposure to trauma-related content. We also hypothesized that individuals with PTSD would show greater concordance between the Subjective Units of Distress Scale (SUDS; Wolpe, 1958) and physiological activity than those participants without PTSD during exposure to trauma-related stimuli. Finally, based on both past literature and statistical considerations, we hypothesized that self-reported distress would be more concordant with physiological levels than with physiological reactivity, particularly for individuals with PTSD.
Method
Participants and Procedure
The current study used archival data from 1,144 male U.S. veterans who served in the Vietnam theater of operations and who participated in VA Cooperative Study #334 (CSP 334), a multisite study of psychophysiological responsivity to trauma-related audiovisual and imaginal depictions among Vietnam veterans with and without PTSD (see Keane et al., 1998). These data included multiple observations of several response channels over time for participants with and without PTSD. The sample included 775 individuals who were diagnosed with current combat-related PTSD according to the Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev.; DSM-III-R; American Psychiatric Association, 1987) criteria, and 369 individuals who had never met criteria for PTSD. The mean age of the sample was 43.30 years (SD = 3.73) and the mean number of years of education was 13.88 (SD = 2.44). Sixty-seven percent of the sample self-identified as Caucasian, 19% as African American, 9% as Hispanic, and 4% as other. Fifty-one percent of the sample indicated that they were currently married (see Keane et al., 1998 for additional information about sample demographics).
To qualify for participation, veterans could not have medical conditions or be taking medication that might affect their psychophysiological responding. Written informed consent was obtained following a complete study description and opportunity for questions. The experimental protocol was approved by the institutional review board at each of the 15 study sites that participated in CSP 334.
Measures
Diagnostic assessment.
PTSD, major depressive disorder (MDD), and substance use disorder (SUD) diagnoses were derived using the Structured Clinical Interview for the DSM-III-R (SCID-I; Spitzer, Williams, Gibbons, & First, 1989). Antisocial personality disorder (ASPD) diagnosis was determined with the Structured Clinical Interview for DSM-III-R Axis II Personality Disorders (SCID-II; Spitzer, Williams, Gibbon, & First, 1990). Experienced clinicians received study-specific training and administered the interviews. All interviews were recorded, and approximately 10% were reviewed by another member of the study team. Interrater reliability was acceptable (κs ranged from .66–.68; see Keane et al., 1998).
A full description of task procedures and measurement can be found in Keane et al. (1998). We present only key information pertaining to the current study. A psychophysiological challenge task involving standardized neutral and combat images with an accompanying soundtrack was administered after participants completed the clinical interview and questionnaire portion of the study. Before beginning the task, participants listened to audiotaped instructions that described the procedure and practiced making ratings using the SUDS (Wolpe, 1958) on a computer screen by means of a joystick. Ratings were accomplished by positioning a computer-generated arrow along a line that reflected the amount of distress they felt. The position of the arrow was translated to a numeric value ranging from 0 (no distress) to 100 (the most that could be imagined). Next, participants were presented with six neutral images that depicted outdoor scenes and were accompanied by classical piano music. Each scene was presented for 1 minute followed immediately by a SUDS rating. After a 5-minute rest–recovery period, participants were presented with six combat images that depicted events in the Vietnam warzone and were accompanied by a matching soundtrack (e.g., gun shots, helicopter sounds). Each combat image was presented for 1 minute followed immediately by a SUDS rating. Thus, there were six SUDS ratings for each content area.
Heart rate level and SC level were among the measures recorded during the presentation of the neutral and combat images. Electronic signals were sampled twice per second, converted to digital values, and stored on a computer for postprocessing. Heart rate was recorded from 9-mm-diameter Sensor Medics (Homestead, FL) Ag/AgCl electrodes filled with Beckman (Beckman Instruments, Fullerton, CA) electrolyte paste and attached by adhesive collars at standard lead I (arm) sites. Electrodes were connected to a Coulbourn (Coulbourne Instruments, Whitehall, PA) High Gain Bioamplifier (S75–01), and the output was directed from the amplifier to a Coulbourn Tachometer (S77–26) to yield a beat-by-beat voltage that was proportional to interbeat interval. SC was measured directly with a Coulbourn Isolated Skin Conductance coupler (S71–23) using a constant 0.5-V output through 9-mm diameter Sensor Medics Ag/AgCl electrodes filled with an isotonic paste (Fowles et al., 1981). The electrodes were attached to the hypothenar surface of participants’ nondominant hands, separated by 14 mm (see Keane et al., 1998). Data were summarized as means for 30-s time blocks (e.g., two values for each 1-min audiovisual presentation). Because there was only one SUDS rating per image, these two 30-s means were averaged to produce one value for each of the physiological measures per image.
Data Analysis
To test the primary hypotheses of this study, we used linear mixed effects modeling (Hierarchical Linear Modeling, Version 6.34; HLM; Raudenbush, Bryk, & Congdon, 2005). Mixed effects models account for the dependency in the data due to individual assessment occasions being nested, or clustered, in individual participants. Thus, they provide accurate estimations of regression coefficients that represent the associated unit change between the predictor and criterion variables. The use of HLM is ideal for situations in which multiple assessments occur within one individual, as is the case with the measurement of multiple response channels across time points in the present study. In the current design, the multiple measurements of physiological activity and self-reports of distress were the Level 1 variables that were nested within individuals at Level 2. Thus, the Level 1 component of the model estimated the within-subject relationship between physiological activity and self-reports of distress, whereas the Level 2 component of the model examined whether or not these within-subject effects significantly varied as a function of between-group effects, including individual difference variables such as diagnostic status. We allowed the intercept and slope to vary randomly among participants and allowed covariance to be unstructured in modeling the data.
Separate models tested the association between SUDS ratings as a time-varying predictor of HR level and SC level. Slide content (coded 1 = combat, 0 = neutral) was added as a Level 1 (i.e., time varying) predictor and PTSD diagnostic status (coded 1 = present, 0 = absent) was added as a Level 2 predictor in these models. Level 1 interactions were evaluated by adding product terms (see Cohen, Cohen, West, & Aiken, 2003) to the Level 1 component of the model, and cross-level interactions (i.e., SUDS [Level 1] × PTSD diagnostic status [Level 2]) were evaluated by including Level 2 predictors of the Level 1 associations (e.g., PTSD as a predictor of the SUDS-physiological measure association to assess the PTSD-SUDS two-way interaction). The final regression model included all main effects, two-way, and three-way interactions among the predictors. Because we expected more variability in physiological responding in response to combat slides than in response to neutral slides, when examining physiological levels, we used the HLM estimation option that allowed us to model heterogeneous Level 1 variance as a function of slide content (Raudenbush et al., 2005).
Prior to testing the primary study hypotheses, we conducted preliminary analyses to examine the need to include several variables that could potentially affect physiological activity. Specifically, given prior findings showing associations with either increased or decreased physiological activity and/or self-reporting of arousal, we considered the potential effects of MDD, ASPD, SUD, nicotine use (i.e., smoking), and Hispanic ethnic status on concordance rates (e.g., Humphreys et al., 2011; Iacono, Carlson, & Malone, 2000; Ishikawa, Raine, Lencz, Bihrle, & LaCasse, 2001; Pole, Kaloupek, & Keane, 2006; Sigmon & Nelson-Gray, 1992; Taylor, 2004; Taylor, Carlson, Iacono, Lykken, & McGue, 1999). Because our primary hypotheses involved the association between SUDS and physiological arousal and (for levels) the interaction of SUDS and slide content predicting physiological activity, we examined the presence of significant two-way interactions between these additional variables and SUDS ratings, as well significant three-way interactions between these additional variables, SUDS ratings, and slide content. Then, a hierarchical approach was adopted to emulate more traditional analysis of variance-(ANOVA) based approaches within the mixed effects model framework. For each outcome, the first model evaluated all main effects, and the second and third models evaluated two-way and three-way interactions, respectively. As recommended by Cohen and colleagues (2003), each main effect was evaluated when in the presence of all other main effects, each two-way interaction was evaluated in the presence of all main effects and all other two-way interactions, and the three-way PTSD Status × SUDS × Slide Content was evaluated in the presence of all main effects and two-way interactions. The primary hypotheses of the study involved the Level 1 association between SUDS ratings and physiological activity (main effect of SUDS ratings) and how this association varied as a function of slide content and PTSD status (involving two- and three-way interactions between SUDS ratings and each of the other predictors). Therefore, for brevity we only report the results involving this main effect and these two-way (PTSD Status × SUDS, SUDS × Slide Content) and three-way (PTSD Status × SUDS × Slide Content) interactions.
The analyses described above were used to investigate the correspondence between levels of self-reports of distress (i.e., SUDS) and physiological levels (i.e., HR and SC) during both neutral and combat slides. A second set of analyses was conducted to investigate the correspondence between reactivity in self-reports of distress and reactivity in physiological activity, with reactivity being defined as the difference in levels (both self-report and physiological) exhibited during neutral versus combat slides. In other words, these analyses examined the degree to which changes in self-reports were associated with changes in HR and SC. The first step of the reactivity analyses consisted of creating reactivity scores for SUDS, HR, and SC. To do this, we used HLM models with SUDS, HR, and SC as Level-1 outcomes in three separate analyses that included a dummy-coded variable representing slide content (0 = neutral, 1 = combat) as a Level-1 predictor variable. The Level-1 regression coefficient associated with the dummy-coded slide variable provided an estimate of the difference in the outcome variable when viewing neutral slides compared with combat slides. As described by Griffin (1997), the Level-1 empirical Bayes estimates of this regression coefficient that HLM derived for each participant were saved into a separate data file (Raudenbush et al., 2005) producing reactivity estimates for SUDS, HR, and SC for each participant. This approach has been used to compute individual change scores that can be saved for subsequent analyses (e.g., Iverson et al., 2011; Walling, Suvak, Howard, Taft, & Murphy, 2012).
Once the reactivity scores were derived, a series of hierarchical regression analyses were conducted to examine the association between reactivity in SUDS and reactivity in the physiological variables, and to determine whether this association varied as a function of PTSD status. The regression analyses were conducted in three steps. Step 1 consisted of regressing the SUDS scores on the mean-centered physiological reactivity scores (separate analyses for HR and SC) to evaluate the bivariate association between the SUDS and physiological variables reactivity scores. Relevant additional predictors (e.g., ASPD) and PTSD status were entered in Step 2, and a PTSD status × physiological variable interaction term was entered into Step 3. For the current study, we only consider Step 1, which estimates the overall relationship between physiological reactivity and SUDS reactivity, and Step 3, for which the interaction term tested whether the association between reactivity in the physiological variable and reactivity in SUDS varied as a function of PTSD status. Step 2 was not evaluated because the parent study from which the data were drawn (Keane et al., 1998) reported on the association between PTSD and reactivity with other variables in the model. Effects sizes for all analyses are presented as partial correlation coefficients (pr) for each coefficient and are evaluated according to the threshold values suggested by Kirk (1996) for small (.10), medium (.24), and large (.37) effect sizes.
Results
Comorbidities
Regarding the influence of comorbidities, three significant comorbidity × SUDS two-way interactions emerged for the SC level. A current diagnosis of MDD was associated with a stronger association between the SUDS and SC level (b = .004, t = 2.23, p < .05, pr = .07), whereas current SUD (b = −.003, t = −1.974, p < .05, pr = .06) or ASPD (b = −.01, t = −1.97, p < .05, pr = .06) was associated with a weaker association between SUDS and SC level. None of the additional comorbidity × SUDS × slide content three-way interactions predicting SC level were statistically significant. For HR level, only one significant comorbidity × SUDS interaction emerged. A diagnosis of ASPD (b = −.02, t = −2.40, p < .05, pr = .08) was associated with a smaller association between the SUDS and HR level. Again, for the HR level, no significant three-way interactions emerged. Therefore, the main effects of MDD, SUD, and ASPD were included in the model in Step 1 (main effects) of the multilevel regression analyses predicting SC level, and product terms representing interactions between these variables and SUDS were included in the model in Step 2 (two-way interactions) and Step 3 (three-way interactions) of the SC level multilevel regression analyses. Only ASPD and the ASPD × SUDS interaction were included in the multilevel regression analyses predicting HR level.
Heart Rate Level and SUDS Association
The main effect of SUDS was statistically significant, with a sizable effect size, indicating that SUDS ratings were positively associated with HR level when collapsed across PTSD status and slide content and controlling for ASPD (see Table 1). A significant slide content × SUDS interaction also emerged (b = .02, t = 3.88, p < .001, pr = .13); the association between SUDS and HR level was stronger for combat slides than neutral slides (see Table 1).
Table 1.
Summary of Hierarchical Linear Modeling Analyses Predicting Associations Between Physiological Levels and Subjective Units of Distress Scale Ratings
| HR Level (n = 937) |
SC Level (n = 907) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Predictors | b | SE | t | df | pr | b | SE | t | df | pr |
|
| ||||||||||
| SUDS main effects | ||||||||||
| All slides/all participantsa | 0.023 | 0.002 | 11.07 | 934 | .33*** | 0.004 | 0.001 | 5.98 | 906 | .19*** |
| Slide × SUDS interaction | ||||||||||
| Neutral/all participants | 0.010 | 0.004 | 2.79 | 934 | .09** | 0.0005 | 0.001 | 0.70 | 906 | .02 |
| Combat/all participants | 0.027 | 0.002 | 10.79 | 934 | .33** | 0.004 | 0.001 | 6.36 | 906 | .21*** |
| PTSD × SUDS interactionb | ||||||||||
| All slides | ||||||||||
| No PTSD | 0.026 | 0.004 | 6.13 | 932 | .19*** | 0.005c | 0.001 | 3.14 | 902 | .10* |
| PTSD | 0.030 | 0.004 | 7.42 | 932 | .23*** | 0.011d | 0.001 | 9.15 | 902 | .29*** |
| PTSD Status × Slide × | ||||||||||
| SUDS interactionb | ||||||||||
| Neutral No PTSD | 0.017 | 0.007 | 2.47 | 932 | .08* | 0.002 | 0.002 | 0.94 | 902 | .03 |
| PTSD | 0.012 | 0.004 | 2.79 | 932 | .09* | 0.001 | 0.001 | 0.57 | 902 | .02 |
| Combat No PTSD | 0.026 | 0.005 | 5.63 | 932 | .18*** | 0.001c | 0.001 | 0.70 | 902 | .02 |
| PTSD | 0.028 | 0.003 | 8.84 | 932 | .28*** | 0.005d | 0.001 | 5.02 | 902 | .16*** |
Note. HR = heart rate; SC = skin conductance; SUDS = Subjective Units of Distress Scale. Asterisks signify statistically significant differences within groups.
The variables identified in the text (i.e., major depressive disorder, substance use disorder, and antisocial personality disorder for SC level and antisocial personality disorder for HR level) were included in the main effects step.
When examining PTSD × SUDS two-way and PTSD × SUDS × Combat Slide three-way interactions main effects of major depressive disorder, substance use disorder, and antisocial personality disorder as well as interactions between these variables and SUDS were included in the model predicting SC level. For the HR level models, only antisocial personality disorder and the interaction between this variable and SUDS were included.
and
signify statistically significant differences between groups.
p < .05.
p < .01.
p < .001.
Neither the PTSD Status × SUDS two-way (b = .003, t = .57 p > .05, pr = .02) interaction nor the PTSD Status × Slide Content × SUDS three-way (b = .01, t = .81, p > .05, pr = .03) interaction was statistically significant, indicating that the association between the SUDS and HR level did not differ as a function of PTSD status. In sum, HR level was positively associated with SUDS across both groups and both types of slide content. This effect, however, was significantly stronger when participants (irrespective of PTSD status) viewed combat slides relative to when they viewed neutral slides.
Association Between SC Level and SUDS
Similar to the findings for HR level, the main effect of SUDS was also statistically significant, with a small-to-medium effect size, indicating that SUDS ratings were positively associated with SC level when collapsed across PTSD status and slide content. Results for two-way interactions are presented in Table 1, but are not interpreted because there was a significant PTSD status × slide content × SUDS ratings three-way interaction (b = .005, t = 2.25, p < .05, pr = .07). The three-way interaction is depicted in Figure 1, with the Slide Content × SUDS interaction as a function of PTSD diagnosis. The Slide Content × SUDS interaction was significant for the PTSD group (b = .004, t = 3.45, p < .01, pr = .11), but not for the no PTSD group (b = −.001, t = −.39, p > .05, pr = .01). The association between SC level and SUDS ratings was significantly stronger for participants with PTSD when presented with combat images (as SUDS increased by one unit, SC level increased by .004 μs) compared with neutral images (as SUDS increased by one unit, SC level increased by .001 μs). In contrast, the association between SC level and SUDS ratings did not significantly differ as a function of slide content in participants without PTSD (as SUDS increased by one unit, SC level increased by .001 μs for neutral images and by .0004 μs for combat images). In other words, the strength of the association between SC level and SUDS significantly varied as a function of PTSD status while viewing combat slides (b = .004, t = 2.85, p < .01, pr = .09); this difference between the groups was associated with a small effect size. On the other hand, the relationship between SUDS and SC level did not significantly differ across the groups while viewing neutral slides (b = −.001, t = −.51, p > .05, pr = .02).
Figure 1.
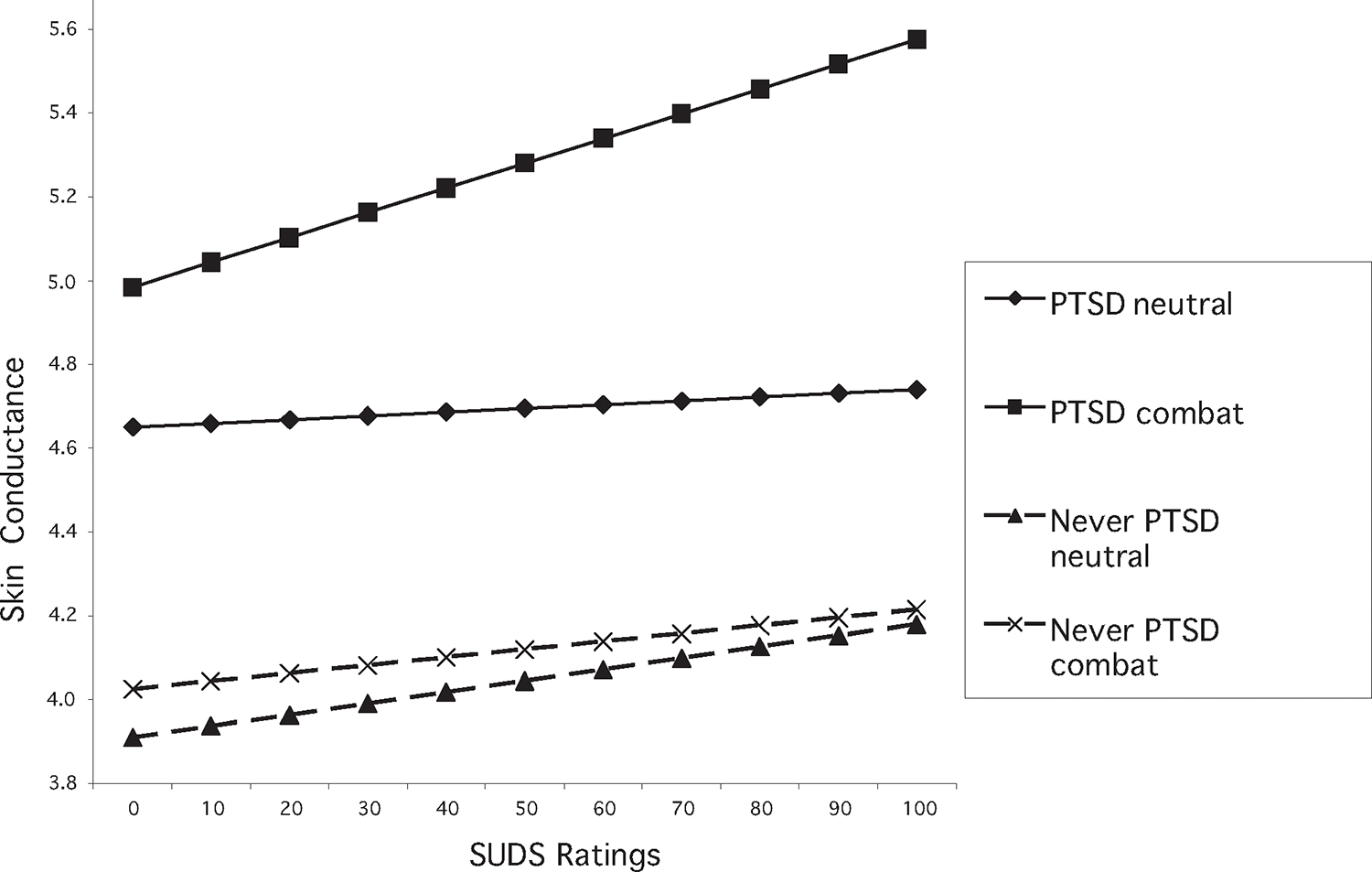
Three-way interaction between slide content, posttraumatic stress disorder status (PTSD), and Subjective Units of Distress Scale (SUDS) for skin conductance level.
Association Between Reactivity and SUDS
The initial HLM analyses that were used to derive reactivity scores indicated a significant mean level increase in SUDS reactivity (b = 38.63, t = 44.34, p < .001, pr = .82), HR reactivity (b = 1.04, t = 6.24, p < .001, pr = .21), and SC reactivity (b = .51, t = 13.01, p < .001, pr = .40) from neutral slide viewing to combat slide viewing. The variance component of the model indicated substantial variability across participants in these reactivity scores: VARSUDS = 25.62, χ2(955) = 10033.33, p < .001; VARHR = 23.03, χ2(939) = 14045.50, p < .001; VARSC = 1.31, χ2(901) = 14979.41, p < .001. The purpose of the regression analyses described below was to examine whether individual differences in SUDS reactivity was related to individual differences in HR reactivity and SC reactivity, and whether these associations significantly varied as a function of PTSD status.
The results of the hierarchical regression analyses are presented in Table 2. Step 1 of the analyses indicated that SUDS reactivity was significantly associated with both HR reactivity (small–medium effect size) and SC reactivity (medium effect size). Nonsignificant SUDS × PTSD Interactions in Step 3 indicated that these associations did not significantly differ as a function of PTSD status. To protect against the chances of making a Type II error we reanalyzed the data removing the additional predictors (e.g., ASPD). The SUDS Reactivity × Physiological Reactivity interaction terms again did not approach statistical significance.
Table 2.
Summary of Multiple Regression Analysis Predicting Estimates of Physiological Reactivity
| Outcome | Variable | b | SE | β | pr |
|---|---|---|---|---|---|
|
| |||||
| HR Reactivity (n = 1,046) | |||||
| Step 1 | (R2 = .03) | ||||
| SUDS | .03*** | .06 | .18 | .18 | |
| Step 2 | (R2 = .04) SUDS | .03*** | .01 | .14 | .13 |
| ASPD | −.29 | .48 | −.02 | −.02 | |
| PTSD | .98** | .31 | .10 | .10 | |
| Step 3 | (R2 = .04) | ||||
| SUDS | .03** | .01 | .17 | .09 | |
| ASPD | −.29 | .48 | −.02 | −.02 | |
| PTSD | .94** | .32 | .10 | .09 | |
| PTSD × SUDS | −.01 | .01 | −.03 | −.02 | |
| SC Reactivity (n = 1,046) | |||||
| Step 1 | (R2 = .06) | ||||
| SUDS | .01*** | .00a | .24 | .24 | |
| Step 2 | (R2 = .08) | ||||
| SUDS | .20*** | .00a | .18 | .19 | |
| ASPD | −.27* | .11 | −.07 | −.07 | |
| SUD | −.10 | .10 | −.03 | −.03 | |
| MDD | .08 | .08 | .03 | .03 | |
| PTSD | .26** | .08 | .11 | .11 | |
| Step 3 | (R2 = .08) | ||||
| SUDS | .01** | .00 | .16 | .08 | |
| ASPD | −.28* | .11 | −.07 | −.07 | |
| SUD | −.11 | .10 | −.03 | −.03 | |
| MDD | .08 | .08 | .03 | .03 | |
| PTSD | .28** | .08 | .12 | .10 | |
| PTSD × SUDS | .00b | .00b | .05 | .03 | |
Note. HR Reactivity = Change in heart rate from neutral to combat slides; SC Reactivity = change in skin conductance from neutral to combat slides; SUDS = Subjective Units of Distress Scale (mean centered); ASPD = antisocial personality disorder diagnosis; SUD = substance abuse disorder; MDD = major depression disorder diagnosis; PTSD = posttraumatic stress disorder diagnosis; PTSD × SUDS = PTSD × SUDS interaction (product) term; b = unstandardized regression coefficient; SE b = the standard error of the unstandardized regression coefficient; β = the standardized regression coefficient; pr = partial correlation coefficient.
Estimate = .001.
Estimate = .003.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Discussion
Results of this investigation supported our hypothesis that participants would demonstrate greater concordance between subjective distress and physiological arousal during exposure to trauma-related content. Specifically, after controlling for the effects of comorbid MDD, SUD, and ASPD, participants demonstrated greater concordance between their distress ratings and SC level during exposure to trauma-related content than neutral content. Similarly, after controlling for comorbidity, we also found a significant and large association between HR level and SUDS, and this association was larger for combat-related stimuli than for neutral stimuli. Results also revealed that the concordance between the physiological levels and SUDS ratings was fairly robust within groups. Our use of a mixed effects modeling approach (which may more fully reflect the degree to which physiological indicators of arousal correspond to self-ratings of distress) in this study reinforces the significant findings of the one prior study that examined these relations with less sophisticated statistical methods (Blanchard et al., 1994).
Results partially supported our hypothesis that individuals with PTSD would show greater concordance among response channels than participants without PTSD during exposure to trauma-related stimuli. Specifically, participants with PTSD demonstrated greater concordance between their distress ratings and SC level, but not HR level, during exposure to trauma-related content than participants without PTSD. These findings are consistent with the well-accepted notion that SC level is a purer indicator of sympathetic activation than HR level (i.e., arousal; Davis & Cowles, 1989) and suggests that individuals can adequately observe and report on their own arousal response.
Interestingly, results from our analyses examining the association between physiological reactivity and self-reported distress portrayed a different picture. Similar to our results involving physiological levels, we found that physiological reactivity and self-reports of distress were significantly concordant. These results differ from those of past studies that found no association between physiological reactivity and self-report (i.e., McDonagh-Coyle, 2001; Pole et al., 2003). Unlike our findings regarding the relationship between self-reported distress and SC level, however, concordance was not moderated by PTSD diagnostic status for either HR reactivity or SC reactivity. Taken together, these findings suggest that whereas self-reported distress is concordant with both physiological levels and physiological reactivity, only concordance with physiological levels (i.e., SC) is moderated by PTSD status.
One possible explanation for why PTSD status did not moderate the concordance between self-reported distress and physiological reactivity is that calculating reactivity restricted the range of values, thereby making a moderating relationship difficult to observe. This may also be why other researchers have struggled to identify a significant association between self-reported distress and physiological responsivity when using change scores with trauma survivors. Without employing the sophisticated analyses utilized in the current study, past investigations (i.e., McDonagh-Coyle, 2001; Pole et al., 2003) may not have been able to detect even the presence of the concordance.
The current investigation has a number of strengths. This study is the first to use mixed effects modeling to examine concordance between subjective distress and physiological arousal during a psychophysiological challenge in which participants with and without PTSD were confronted by trauma-related stimuli. In addition to allowing us to take advantage of multiple data points while controlling for potentially comorbid conditions, the use of this methodology allowed us to apply an estimation procedure that corrected for heterogeneity of variance in physiological levels as a function of slide content. This procedure allows us to have a higher level of confidence that our results are not an artifact of a restricted range of variance.
Another strength of the current investigation is its examination of the concordance between self-reported distress and both physiological levels and physiological reactivity using the same dataset. The fact that both of these assessments of responsivity were concordant with self-reported distress gives further credence to our conclusion that these two response channels are associated. Finally, the present study improved upon past research by obtaining self-report ratings immediately after emotion-eliciting stimuli, thus reducing the effects of potential memory biases.
The findings of the current study also suggest several assessment and treatment implications. Previous research has attempted to demonstrate that psychophysiological challenge tasks can be used to discriminate individuals with PTSD from those without the disorder, but these studies have yielded mixed results (e.g., Blanchard, Kolb, Pallmeyer, & Gerardi, 1982; Blanchard, Kolb, & Prins, 1991; Keane et al., 1998; Orr, Pitman, Lasko, & Herz, 1993). The results of the current study suggest that rather than examining the degree to which changes in HR, SC, or other physiological indices in response to trauma-related stimuli can discriminate between those with and without PTSD, it might be fruitful for investigators to explore the extent to which the concordance between response channels (particularly between skin conductance and SUDS) can be employed to make such between-group discriminations. Our findings suggest this may be particularly useful to examine in regards to physiological levels rather than reactivity.
The current findings also highlight the importance of employing multiple methods of assessment to adequately capture data from the three response systems (i.e., clinical interviews, psychological testing, and psychophysiological assessment) during the assessment and treatment of those with PTSD (Keane, Wolfe, & Taylor, 1987; Sloan & Kring, 2007). When present, discordance among the response channels may be the result of a number of factors, including an individual’s inability to accurately reflect upon and report their current level of distress when confronted by aversive stimuli, dissociation, defensive response style, behavioral or cognitive avoidance, compromised defensive responding, or some combination thereof (Lipanen, Saarjarvi, & Lauerma, 2004; Sloan & Kring, 2007). Additional research should examine factors other than trauma-related cues that determine the degree to which responses channels are concordant with one another among individuals with PTSD. In addition, in instances of disagreement among self-reported emotional experience, expressive behavior, and objective physiological indicators of distress or arousal, clinicians should carefully determine which response channel(s) should be the primary target for treatment based upon the idiographic nature of the presenting problem. Our finding that subjective distress in response to trauma-related stimuli more closely mirrors SC level among those with PTSD than among those without the disorder suggests that future researchers and clinicians should pay particular attention to the degree to which self-report corresponds to SC level under various conditions.
In terms of treatment, these results suggest that the practice of using patient self-reports of distress during exposure-based treatments as an estimate of actual physiological arousal may be a reasonable and appropriate clinical practice. Even though our findings suggest a fairly strong association between self-report and levels of physiological arousal, however, clinicians and researchers should not assume that an individual’s self-report of distress can and should completely substitute for objective measurement of physiological arousal to trauma-related stimuli, especially because subjective distress may be influenced by nonphysiological constructs, such as response style, cognitive reappraisal, and emotion regulation. Doing so may yield unexpected and theoretically inconsistent results such as the finding that within-session reductions in self-reported distress are not associated with exposure-based treatment outcomes for individuals with PTSD (e.g., Jaycox, Foa, & Morral, 1998; van Minnen & Foa, 2006).
There are several limitations to the present study. The extent to which these results generalize to nonmilitary trauma populations, across sex and gender, and to less chronic samples is unknown. Also, we may have underestimated the degree of concordance between response channels as a result of having participants rate their subjective distress only after presentation of each trauma-related stimulus was terminated and averaged across a full minute, whereas response may be highest during and immediately following presentation. Another factor that may have led to an underestimation of the concordance between response channels is that participants rated their level of distress rather than their level of arousal. Although these constructs are likely to be related, distress may be more similar to the valence dimension (i.e., hedonic quality) of emotional experience, whereas arousal refers to the perceived level of activation associated with an emotional response (e.g., Bush, 1973; Russell, 1978). Future investigations of concordance should consider the measurement of a self-report construct that is conceptually and theoretically matched to the physiological indices of interest. The additional examination of concordance to idiographic stimuli may provide a richer source of PTSD assessment. An additional limitation was the use of DSM-III-R criteria to determine PTSD diagnosis. Although replication using current diagnostic criteria is warranted, previous studies have demonstrated good agreement between DSM-III-R and DSM-IV PTSD diagnoses (e.g., Schwarz & Kowalski, 1991). Finally, although we were able to identify and include several additional relevant independent variables in our analyses, we were unable to examine the importance of traumatic brain injury (TBI) to the association between self-reported distress and physiological reactivity to trauma-related stimuli. TBI symptoms can overlap with PTSD symptoms and may have significant effects on physiological arousal and self-reported distress.
Overall, the current study suggests that individuals’ self-reported distress is generally a reliable indicator of physiological arousal (assessed by both physiological levels and physiological reactivity), particularly in response to trauma-related stimuli. This appears to be particularly true for individuals with PTSD, who demonstrated high levels of concordance between self-reported distress and skin conductance levels. The results of this study have important implications for both the assessment and treatment of PTSD. Perhaps most importantly, the implications of the current findings suggest that the practice of using patient self-reports of distress during exposure-based treatments for PTSD as an estimate of actual physiological arousal may be a reasonable and appropriate clinical practice. Continued research in this area is important to further strengthen our ability to identify and treat individuals suffering from this devastating disorder.
Acknowledgments
This research was supported by the VA Cooperative Studies Program of the Veterans Health Administration under designation CS-334.
References
- American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., rev.). Arlington, VA: Author. [Google Scholar]
- Blanchard EB, Hickling EJ, Taylor AE, Loos WR, & Gerardi RJ (1994). The psychophysiology of motor vehicle accident related posttraumatic stress disorder. Behavior Therapy, 25, 453–467. doi: 10.1016/S0005-7894(05)80157-1 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Kolb LC, Pallmeyer TP, & Gerardi RJ (1982). A psychophysiological study of post-traumatic stress disorder in Vietnam veterans. Psychiatric Quarterly, 54, 220–229. doi: 10.1007/BF01064817 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Kolb LC, & Prins A (1991). Psychophysiological responses in the diagnosis of post-traumatic stress disorder in Vietnam veterans. Journal of Nervous and Mental Disease, 179, 99–103. doi: 10.1097/00005053-199102000-00006 [DOI] [PubMed] [Google Scholar]
- Bush LE (1973). Individual differences multidimensional scaling of adjectives denoting feelings. Journal of Personality and Social Psychology, 25, 50–57. doi: 10.1037/h0034274 [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, & Aiken LS (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Davis C, & Cowles M (1989). Some sources of variation in skin conductance. Canadian Journal of Psychology, 43, 97–103. doi: 10.1037/h0084211 [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, & Rothbaum B (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences: Therapist guide. New York, NY: Oxford University Press. [Google Scholar]
- Foa EB, & Rothbaum BO (1998). Treating the trauma of rape: Cognitive-behavioral therapy for PTSD. New York, NY: Guilford Press. [Google Scholar]
- Fowles DC, Christie MJ, Edelberg R, Grings WW, Lykken DT, & Venables PH (1981). Publication recommendations for electrodermal measurements. Psychophysiology, 18, 232–239. doi: 10.1111/j.1469-8986.1981.tb03024.x [DOI] [PubMed] [Google Scholar]
- Griffin MA (1997). Interaction between individuals and situations: Using HLM procedures to estimate reciprocal relationships. Journal of Management, 23, 759–773. doi: 10.1177/014920639702300604 [DOI] [Google Scholar]
- Humphreys KL, Foley K, Feinstein BA, Marx BP, Kaloupek DG, & Keane TM (2011). The influence of externalizing comorbidity on psychophysiological reactivity among veterans with posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, doi: 10.1037/a0022644 [DOI] [Google Scholar]
- Iacono WG, Carlson SR, & Malone SM (2000). Identifying a multivariate endophenotype for substance use disorders using psychophysiological measures. International Journal of Psychophysiology, 38, 81–96. doi: 10.1016/S0167-8760(00)00132-X [DOI] [PubMed] [Google Scholar]
- Ishikawa SS, Raine A, Lencz T, Bihrle S, & LaCasse L (2001). Autonomic stress reactivity and executive functions in successful and unsuccessful criminal psychopaths from the community. Journal of Abnormal Psychology, 110, 423–432. doi: 10.1037//0021-843X.110.3.423 [DOI] [PubMed] [Google Scholar]
- Iverson KM, Gradus JL, Resick PA, Suvak MK, Smith K, & Monson C (2011). Cognitive-behavioral therapy for PTSD reduces risk of intimate partner violence. Journal of Consulting and Clinical Psychology, 79, 193–202. doi: 10.1037/a0022512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaycox LH, Foa EB, & Morral AR (1998). Influence of emotional engagement and habituation on exposure therapy for PTSD. Journal of Consulting and Clinical Psychology, 66, 185–192. doi: 10.1037//0022-006X.66.1.185 [DOI] [PubMed] [Google Scholar]
- Keane TM, Kolb LC, Kaloupek DG, Orr SP, Blanchard EB, Thomas RG, & Lavori PW (1998). Utility of psychophysiology measurement in the diagnosis of posttraumatic stress disorder: Results from a Department of Veterans Affairs cooperative study. Journal of Consulting and Clinical Psychology, 66, 914–923. doi: 10.1037/0022-006X.66.6.914 [DOI] [PubMed] [Google Scholar]
- Keane TM, Wolfe J, & Taylor KL (1987). Post-traumatic stress disorder: Evidence for diagnostic validity and methods of psychological assessment. Journal of Clinical Psychology, 43, 32–43. [DOI] [PubMed] [Google Scholar]
- Kirk RE (1996). Practical significance: A concept whose time has come. Educational and Psychological Measurement, 56, 746–759. doi: 10.1177/0013164496056005002 [DOI] [Google Scholar]
- Lipanen T, Saarjarvi S, & Lauerma H (2004). Exploring the relations between depression, somatization, dissociation and alexithymia: Overlapping or independent constructs? Psychopathology, 37, 200–206. doi: 10.1159/000080132 [DOI] [PubMed] [Google Scholar]
- Ludwick-Rosenthal R, & Neufeld RW (1985). Heart beat interoception: A study of individual differences. International Journal of Psychophysiology, 3, 57–65. doi: 10.1016/0167-8760(85)90020-0 [DOI] [PubMed] [Google Scholar]
- Mauss IB, Levenson RW, McCarter L, Wilhelm FH, & Gross JJ (2005). The tie that binds? Coherence among emotion experience, behavior, and physiology. Emotion, 5, 175–190. doi: 10.1037/1528-3542.5.2.175 [DOI] [PubMed] [Google Scholar]
- McDonagh-Coyle A, McHugo GJ, Friedman MJ, Schnurr PP, Zayfert C, & Descamps M (2001). Psychophysiological reactivity in female sexual abuse survivors. Journal of Traumatic Stress, 14, 667–683. doi: 10.1023/A:1013081803429 [DOI] [PubMed] [Google Scholar]
- Orr SP, Pitman RK, Lasko NB, & Herz LR (1993). Psychophysiologic assessment of posttraumatic stress disorder imagery in World War II and Korean combat veterans. Journal of Abnormal Psychology, 102, 152–159. doi: 10.1037/0021-843X.102.1.152 [DOI] [PubMed] [Google Scholar]
- Pole N, Kaloupek D, & Keane TM (2006, November). Are Hispanic Americans at greater risk for PTSD? Paper presented at the annual meeting of the International Society for Traumatic Stress Studies, Hollywood, CA. [Google Scholar]
- Pole N, Neylan TC, Best SR, Orr SP, & Marmar CP (2003). Fear-potentiated startle and posttraumatic stress symptoms in urban police officers. Journal of Traumatic Stress, 16, 471–479. doi: 10.1023/A:1025758411370 [DOI] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A, & Congdon R (2005). HLM 6 for Windows (Version 6) [Computer software]. Lincolnwood, IL: Scientific Software International, Inc. [Google Scholar]
- Rellini AH, McCall KM, Randall PK, & Meston CM (2005). The relationship between women’s subjective and physiological sexual arousal. Psychophysiology, 42, 116–124. doi: 10.1111/j.1469-8986.2005.00259.x [DOI] [PubMed] [Google Scholar]
- Russell JA (1978). Evidence of convergent validity on the dimensions of affect. Journal of Personality and Social Psychology, 36, 1152–1168. doi: 10.1037/0022-3514.36.10.1152 [DOI] [Google Scholar]
- Schwarz ED, & Kowalski JM (1991). Posttraumatic stress disorder after a school shooting: Effects of symptom threshold selection and diagnosis by DSM-III, DSM-III-R, or proposed DSM-IV. The American Journal of Psychiatry, 148, 595–597. Retrieved from http://ajp.psychiatryonline.org/journal.aspx?journalid=13 [DOI] [PubMed] [Google Scholar]
- Shapiro F (1995). Eye movement desensitization and reprocessing: Basic principles, protocols, and procedures. New York, NY: Guilford Press. [Google Scholar]
- Sigmon ST, & Nelson-Gray RO (1992). Sensitivity to aversive events in depression: Antecedent, concomitant, or consequent? Journal of Psychopathology and Behavioral Assessment, 14, 225–246. doi: 10.1007/BF00962630 [DOI] [Google Scholar]
- Sloan DM, & Kring AM (2007). Measuring changes in emotion during psychotherapy: Conceptual and methodological issues. Clinical Psychology: Science and Practice, 14, 307–322. doi: 10.1111/j.1468-2850.2007.00092.x [DOI] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbons M, & First MB (1989). Structured Clinical Interview for DSM-II-R-Patient Version (SCID-P). New York, NY: Psychiatric Institute. [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, & First MB (1990). Structured Clinical Interview for DSM-III-R Personality Disorder. Washington, DC: American Psychiatric Press. [Google Scholar]
- Stern RM, Ray WJ, & Quigley KS (2001). Psychophysiological recording (2nd ed.). Oxford, England: Oxford University Press. [Google Scholar]
- Taylor J (2004). Electrodermal reactivity and its association to substance use disorders. Psychophysiology, 41, 982–989. doi: 10.1111/j.1469-8986.2004.00236.x [DOI] [PubMed] [Google Scholar]
- Taylor J, Carlson SR, Iacono WG, Lykken DT, & McGue M (1999). Individual differences in electrodermal responsivity to predictable aversive stimuli and substance dependence. Psychophysiology, 36, 193–198. doi: 10.1111/1469-8986.3620193 [DOI] [PubMed] [Google Scholar]
- van Minnen A, & Foa EB (2006). The effect of imaginal exposure length on outcome of treatment for PTSD. Journal of Traumatic Stress, 19, 427–438. doi: 10.1002/jts.20146 [DOI] [PubMed] [Google Scholar]
- Walling SM, Suvak MK, Howard J, Taft CT, & Murphy C (2012). Race/ethnicity as a predictor of change in working alliance during cognitive behavioral therapy for intimate partner violence perpetrators. Psychotherapy: Theory, Research, Practice, Training, 49, 180–189. doi: 10.1037/a0025751 [DOI] [PubMed] [Google Scholar]
- Wolpe J (1958). Psychotherapy by reciprocal inhibition. Stanford, CA: Stanford University Press. doi: 10.1037/10575-013 [DOI] [Google Scholar]


