Lesson
The delayed onset of thyroid eye disease is well recognised but less commonly perceived in routine clinical practice and this case report serves as a reminder for a high index of suspicion in at-risk patients.
Keywords: Grave's disease, thyroid eye disease, thyroid receptor antibodies, radioactive iodine, COVID vaccination
This case report discusses the onset of de novo thyroid eye disease (TED) after COVID-19 vaccination, occurring several years after administration of radioactive iodine therapy (RAI) for Grave's disease (GD).
Case presentation
A 52-year-old lady, who had previously been treated with RAI for an overactive thyroid gland, presented five years later with symptoms of dryness and protrusion of her left eye that was initially noticed within a few weeks after receiving the first dose of COVID mRNA vaccine in 2021. Clinical examination revealed exophthalmos, lid lag, and erythema in the left eye (Figures 1–2). The clinical activity and severity (CAS) score were 2 (scoring positively for active lid swelling and definite conjunctival redness). The patient had been a smoker with a 40-pack year history and had high cholesterol levels of 6.6 mmol/L (<5.1 mmol/L).
She was initially treated for an overactive thyroid gland with a titrating dose of carbimazole between 2012 and 2015 and subsequently given RAI in 2016 as definitive treatment for hyperthyroidism (Table 1). There were no eye signs at all during these few years and her thyroid functions remained stable. Of note, her euthyroid status was maintained clinically and biochemically on a consistently static dose of levothyroxine 75/100 micrograms on alternate days throughout the five years following RAI therapy and even at the time of development of TED (Table 2) and thereafter also for a further three years. Interestingly, no alterations to the dosage of levothyroxine were required in between or subsequently.
Table 1.
Thyroid functions and treatment given to the patient prior to COVID-19 pandemic with stable thyroid functions on fixed dose levothyroxine (note TRAb titre pre-RAI).
| Nov 2012 | Jul 2013 | Dec 2013 | Jul 2014 | May 2015 | Jan 2016 | Mar 2016 | Apr 2016 | Jun 2016 | Aug 2016 | Jan 2017 | Apr 2017 | Apr 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TSH (0.3–5) mIU/L | 0.01 | 0.01 | 0.02 | 0.91 | 0.24 | 0.02 | 1.06 | 0.09 | 82.18 | 0.06 | 0.10 | 0.27 | |
| Free T4 (8- 19) pmol/ L | 14 | 25 | 12 | 12 | 17 | 19 | 11 | 13 | 3 | 20 | 16 | 19 | |
| Free T3 (2.1–6) pmol/L | 5.4 | 12.3 | - | - | - | 6.5 | 4.6 | 4.1 | - | 5.3 | - | - | |
| TRAb (0.0-0.9 IU/L) | 2.5 | ||||||||||||
| Treatment | Carbimazole 5-10 mg | Carbimazole 5 mg | Carbimazole 10 mg | Wait and watch | Levothyroxine 100 mcg | Levothyroxine 75/100 mcg | |||||||
| Intervention/Event | Radioactive Iodine | ||||||||||||
Table 2.
Thyroid functions and treatment given to the patient subsequent to the pandemic and post mRNA COVID vaccination with rising tide of TRAb titres.
| Mar 2020 | Mar 2021 | Apr 2021 | May 2021 | Sep 2021 | Dec 2021 | Aug 2022 | Dec 2022 | May 2023 | Jun 2023 | Mar 2024 | Apr 2024 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TSH (0.3–5) mIU/L | 0.17 | - | - | – | 3.77 | 1.81 | 2 | 0.32 | 16.15 | 1.49 | 1.24 | 1.09 |
| Free T4 (8- 19) pmol/ L | 20 | - | - | 12 | 15 | 15 | 18 | 12 | - | - | 13.5 | |
| Free T3 (2.1–6) pmol/L | - | - | - | - | - | - | - | - | - | - | - | - |
| TRAb (0.0-0.9 IU/L) | - | - | - | - | 45.2 | 37.8 | 37.6 | - | - | - | 118.1 | |
| Treatment | Levothyroxine 75/100 mcg consistently with no change to the dose at any stage | |||||||||||
| Intervention/event | COVID Vaccine 1 | Eye symptoms develop | COVID Vaccine 2 | |||||||||
Thyroid receptor antibodies (TRAb) levels significantly worsened from 2.5 IU/L (0.1–0.9) before RAI therapy to 45 IU/L (0.1–0.9) a few weeks following the onset of TED. This continued to rise thereafter as well to 118 IU/L (Tables 1 & 2).
The patient has remained symptom free with lubricant eye drops although she has ongoing TED, but with her CAS score remaining at 2 (hence not treated with intravenous methyl prednisolone which is offered with active disease classed when CAS score is ≥3). She has been referred for left orbital decompression procedure as a form of ophthalmic rehabilitation surgery, at her request and choice.
Discussion
The patient was hypothyroid post-RAI therapy and required stable doses of levothyroxine. The dose remained unchanged despite developing TED following COVID-19 vaccination, five years later. The temporal correlation of the onset of TED with COVID-19 vaccination was significant. It serves as a reminder for generalists and specialists, to be aware of and remain alert to explore the cause of a latent trigger for TED, after prior treatment for GD. The adjuvants in COVID-19 vaccines serving as a trigger for immune dysregulation, including reactivation of thyroid remnants by TRAb, are likely explanations in this patient. The TRAb levels increased shortly after receiving the second dose of the COVID-19 vaccine with worsening TED associated with rising titres of TRAb. Grave's orbitopathy (GO) is the predominantly major extrathyroidal manifestation of GD. The selection of treatment should be centred on the assessment of CAS score of GO. 1 Prompt referral to specialised centres is essential for most patients with GO. The risk factors include smoking, thyroid dysfunction, raised cholesterol, high serum level of TRAb, and RAI treatment. However, in this patient TED manifested several years after RAI therapy, which is very likely triggered by the COVID-19 vaccination as clearly demonstrated in the sequential timeline (Table 2).
The safety and effectiveness of the various types of COVID-19 vaccines, including mRNA-based, viral vector-based, and inactivated vaccines, have been well recognised. The protection is conferred by vaccines against severe SARS-CoV-2 infection through the induction of neutralising antibodies of the anti-spike protein. However, SARS-CoV-2 vaccines have been associated with complications, such as thyroid disorders. 2 Various propositions have been suggested to describe the potential association between SARS-CoV-2 vaccination and hyperthyroidism, including (a) immune system hyper-stimulation, (b) molecular mimicry and (c) autoimmune/autoinflammatory syndrome induced by adjuvants (ASIA). 3
It is also imperative to remember that COVID-19 infection per se is a cause for new onset and flare-up of GD, 4 and it is important to recognise the association between COVID-19 vaccination as well as thyroid function abnormalities, whilst corroborating clinical findings for early diagnosis and treatment. In our patient, her CAS score of 2 did not meet the criteria for intravenous steroids and the lid lag and exophthalmos on the left side were what affected her predominantly, warranting referral for surgical intervention. She did not have any of the features of eye lid erythema, chemosis, caruncle/plica inflammation, spontaneous orbital pain, gaze evoked orbital pain, increased proptosis of >2 cm, eye mobility issues subjectively or visual acuity loss on Snellen's chart, which are all the other criteria for a high CAS score and therefore, there was no indication for intravenous methyl prednisolone treatment.
Figure 1.
Left lid lag.
Figure 2.
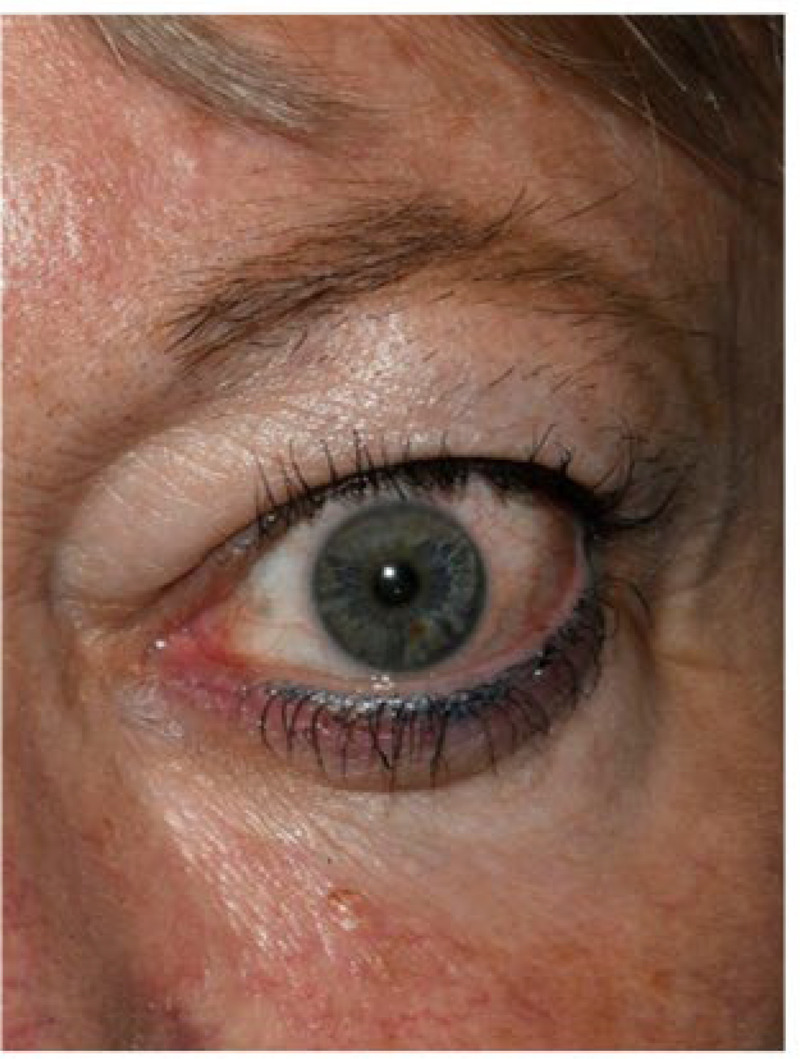
Exophthalmos left eye.
Clinicians providing care should alert patients to be aware of the risks and they should seek assistance with a view to further treatment should the signs and symptoms of TED recur.5–7 The development of TED subsequent to COVID-19 vaccination in patients with previously well controlled thyroid functions on chronically stable doses of levothyroxine replacement therapy is very uncommon. 8 Moreover the onset of TED several years after having prior RAI treatment, and not having had any previously documented eye signs or symptoms is extremely rare indeed. 9 Patients can present with very non-specific symptoms and signs in this context.
Conclusion
We describe an interesting presentation of TED that progressed to thyroid orbitopathy requiring the need to consider orbital decompression surgery, in a patient who developed elevated TRAb levels following COVID-19 vaccination. The patient had no eye symptoms attributable to TED prior to the vaccination and her thyroid functions remained stable both during the pre-vaccination and post vaccination period. It is vital that clinicians counsel at-risk patients about this rare occurrence even if they are clinically and biochemically euthyroid on fixed dose levothyroxine post-RAI. TED tends to occur in approximately a quarter of patients with GD and delays has been observed in patients presenting to ophthalmologists, when inflammatory changes in the orbit that are debilitating may already have occurred. 1 ° Clinicians should remain vigilant, especially in patients who are already clinically and biochemically euthyroid, on fixed dose levothyroxine post RAI.
Key messages
COVID vaccination can trigger the onset of TED even several years after definitive treatment of GD.
TED can occur in patients previously treated with RAI and rendered permanently hypothyroid.
The onset of eye symptoms and signs can happen even with normal thyroid functions.
Prior symptoms of TED are not necessarily a pre-requisite to alert clinicians.
Patients must be counselled about the need to remain vigilant re TED.
Acknowledgements
The authors would like to thank our patient for kindly consenting to publish this manuscript and to the clinical photography department at UHNM NHS Trust for the support with the photo images.
Footnotes
Competing interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. This case-based review was accepted as a poster presentation at the Joint Irish-UK Endocrine Meeting 2024, Belfast on 14–15 October 2024.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: We have obtained patient consent for publication of this manuscript and the images.
Contributorship: AM, JJ and RJ wrote the initial draft and reviewed the literature. GIV revised the article and examined the evidence base. AUN conceptualised the theme, edited the discussion and cross-checked the references.
Provenance: Not commissioned, peer reviewed by Sudeshna Patra.
ORCID iD: George I Varughese https://orcid.org/0009-0008-5522-8623
References
- 1.Bartalena L, Kahaly GJ, Baldeschi L, et al. EUGOGO †. The 2021 European group on Graves’ orbitopathy (EUGOGO) clinical practice guidelines for the medical management of Graves’ orbitopathy. Eur J Endocrinol 2021;185(4):G43–G67. [DOI] [PubMed] [Google Scholar]
- 2.Jafarzadeh A, Nemati M, Jafarzadeh S, Nozari P, Mortazavi SMJ. Thyroid dysfunction following vaccination with COVID-19 vaccines: a basic review of the preliminary evidence. J Endocrinol Invest 2022;45(10):1835–1863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pla Peris B, Merchante Alfaro AÁ, Maravall Royo FJ, Abellán Galiana P, Pérez Naranjo S, González Boillos M. Thyrotoxicosis following SARS-COV-2 vaccination: a case series and discussion. J Endocrinol Invest 2022;45(5):1071–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sebastian WP, Parisa A, Pandya M, Anees A. Graves’ disease exacerbation with impending thyroid storm after SARS-CoV-2 infection: a case report. Am J Case Rep 2024;25:e941311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hung CW, Hung CH. Reactivation of Graves’ disease and thyroid eye disease following COVID-19 vaccination – a case report. Ocul Immunol Inflamm 2023;31(6):1286–1290. [DOI] [PubMed] [Google Scholar]
- 6.Fujita H, Makino S, Hasegawa T, et al. Thyroid eye disease following administration of the BNT162B2 COVID-19 vaccine. QJM 2023;116(2):130–132. [DOI] [PubMed] [Google Scholar]
- 7.Park KS, Fung SE, Ting M, et al. Thyroid eye disease reactivation associated with COVID-19 vaccination. Taiwan J Ophthalmol 2022;12(1):93–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubinstein TJ. Thyroid eye disease following COVID-19 vaccine in a patient with a history Graves’ disease: a case report. Ophthalmic Plast Reconstr Surg 2021;37(6):e221–e223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Im Teoh JH, Mustafa N, Wahab N. New-onset thyroid eye disease after COVID-19 vaccination in a radioactive iodine-treated Graves’ disease patient: a case report and literature review. J ASEAN Fed Endocr Soc 2023;38(1):125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Edmunds MR, Boelaert K. Knowledge of thyroid eye disease in Graves’ disease patients with and without orbitopathy. Thyroid 2019;29(4):557–562. [DOI] [PubMed] [Google Scholar]



