Abstract
Background
Healthy lifestyle improvement of older Chinese adults has drawn a lot of attention due to an exceeding ageing population in mainland China. The current study aims to investigate the beneficial functions of the multi-channel health information seeking on elders’ lifestyle self-management.
Objective
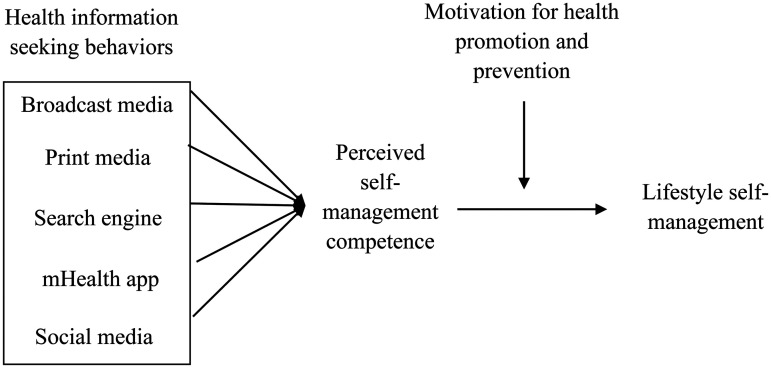
We conducted a mediation analysis to test the association between multi-channel information seeking behavior and lifestyle self-management, which mediates by perceived self-management competence. Meanwhile, we also test the moderation effect of perceived self-management competence on lifestyle management with motivation for health promotion and prevention as the moderator.
Methods
To examine this mediation and moderation effects, we conducted a quota sampling online survey in mainland China from June 11 to October 12, 2023. The final sample size was 898 Chinese respondents aged 60 or above, with 54.5% male.
Results
Health information seeking using the mHealth app (bp = .03, 95% CI: [.005, .055]) and social media (bp = .06, 95% CI: [.031, .086]) is positively associated with lifestyle self-management through perceived self-management competence. While broadcast media (bp = .01, 95% CI: [−.015, .040]), print media (bp = .01, 95% CI: [−.015, .026]), and search engine (bp = .02, 95% CI: [−.006, .043]) show no significant impact on lifestyle management. Furthermore, health promotion and prevention motivation shows a positive moderation effect on perceived self-management competence and lifestyle management.
Conclusions
Our findings show evidence supporting a cognitive mechanism of moderated mediation that links seeking health information to improve LSM in older Chinese adults. It is essential for health self-education and health promotion among older Chinese adults.
Keywords: Lifestyle, health information-seeking behavior, information foraging, motivation, digital health
Introduction
The global trend of population ageing has become inevitable due to the rise in life expectancy and the decline in fertility rates. China is no exception to this phenomenon. In 2000, it has also transitioned into an ageing society. 1 By 2050, it is expected that Chinese people aged over 65 will reach 365 million, accounting for 26.1% of the total population. 2 The accelerated ageing process has resulted in a prevalence of non-communicable diseases among older Chinese adults, including hypertension (36.9%) and diabetes (10.6%). 3 These diseases may also cause negative outcomes, such as reduced social participation and mental well-being. 4
Figure 1.
The proposed model.
Health self-management generally refers to the ability of individuals to self-examine and analyse their health status and factors that influenced their life, 5 broadly including protective actions, such as information-seeking, making medical decisions, and appropriate exercise. 6 There is substantial evidence that health self-management improves the health status of older adults7–9. The emergence of lifestyle self-management (LSM), as an important component of health self-management, among older adults has become the focus of interest. LSM is defined as the ability to adopt healthy lifestyle habits. 10 It is thought to be an effective approach to improving older adults’ physical and mental health status, allowing them to live longer and with a higher quality of life.11,12 Experimental studies have shown that good LSM has been important in improving older adults’ healthy behaviors and objective health indicators, such as blood pressure, blood sugar and waist circumference.13,14 However, compared to Chinese younger populations, older adults in mainland China have a lower health literacy level, 15 making it difficult for them to effectively manage their lifestyle. 4
Health information-seeking behavior (HISB) is an essential step in developing positive health outcomes including LSM. Prior studies showed that HISB is an effective strategy for bringing both positive physical and mental health outcomes.16–24 Specifically, HISB serves as a means to fill gaps in one's understanding, such as to acquire the knowledge they lack, to confirm or disconfirm their existing beliefs, and to use that information for strategic purposes. 25 However, existing studies have ignored one of the most vulnerable groups, namely older adults. In the Chinese context, as older adults take greater steps to access healthcare and maintain their health, 26 adequate and effective health information assists them in resolving their health concerns. Exploring how HISB affects LSM for older Chinese adults is crucial.
Additionally, studies have shown that older adults have been increasingly relying on multiple health information sources 27 rather than just healthcare providers. 28 However, few studies focus on the varying impact of various media sources on HISB for older Chinese adults. To fill these gaps, the current study focused on older Chinese adults and sought to explore (a) the association between HISB and LSM, and (b) examine the performance of HISB across five media channels, i.e., broadcast media, print media, search engine, mHealth app and social media, potentially leading to the development of health education for older adults seeking health information.
Literature review
Information foraging theory
The current study employed information foraging theory (IFT) 29 to conduct the conceptual model. IFT provides a unique theoretical perspective to understand individuals’ information searching by analogizing information-seeking behaviors to animal foraging. Animals determine the type of prey and the capture timing based on the cost and benefits of obtaining different prey. Similarly, individuals decide which media channels to use for information search based on their evaluation of the information environment and the anticipated costs and benefits of the search process.29–31 The vital principle of IFT is that individuals determine their information-seeking strategies (i.e., information diet) by assessing their capabilities and evaluating the cost and value of the search process (i.e., information cues). This evaluation guides them to focus on “patch” foraging activities and select specific media channels for information retrieval. 29 Chinese older adults’ HISB32–35 is consistent with this principle. For instance, TV was the most popular media source among older Chinese adults seeking COVID-19 information, as they believed it provided the most trust message for pandemic-related messages. 35 Some older chose mHealth apps to save time and effort, get rich and diverse health information, and get rewards. 33 In this study, we employed IFT to investigate the varying extent of HISB through media sources for a specific outcome among older Chinese adults.
Furthermore, we have introduced perceived health self-management competence (PSC) as a key cognitive function to understand the mechanism of how elders’ information foraging brings health outcomes. According to IFT, elders tend to select media channels for health information seeking that maximize benefits by cognitive assessments29–31. Ample empirical evidence found that enhancing individuals’ health management efficacy and ability is one of the main benefits of health information seeking.27,36 When seeking health-related information, benefit maximization can be understood as efficiently acquiring information that enhances their health self-management competence, ultimately leading to tangible health outcomes, that is improving their healthy lifestyle.
HISB and PSC
According to IFT, older adults’ HISB may considered as information patches foraging activities that heavily rely on multiple information sources rather than a single channel. 27 Various media channels demonstrate their characteristics to meet elders’ differential information-seeking needs. On the one hand, traditional media, including broadcast and print media, usually “push” information to their audiences. Therefore, audiences may have less control over the content of these media.37,38 Empirical evidence found that traditional media channels, especially broadcast media, obtain the most trust and are relied upon by older Chinese adults. 35 That is, elders may seek health information in these media channels with relatively low agency but high levels of media trust. On the other hand, the internet allows users to “pull” information at their discretion, thus encouraging more elders’ active HISB.37,38 These studies found several features of Internet channels that contribute to older adults’ preference for online health information foraging activities, such as ease of access, affordability, anonymity, and reliability. However, it is worth noting that their online HISB remains limited due to a lack of Internet skills, e-literacy, and untailored website design. 39
In general, HISB contributes to the improvement of PSC through several potential factors among older adults. First, HISB may improve older adults’ information accessibility and availability, empowering them to take action to improve their health and improving their confidence in health self-management. 40 Second, HISB is an effective way to train searching skills for older adults. According to the digital divide theory, older adults with computer-operating skills training and support can improve their mental states and increase self-belief in their abilities to use digital tools and platforms. 41 HISB provides older adults with more opportunities to use various health-related digital devices, enhancing their digital technological skills and boosting their confidence when searching for health information. Third, due to information source diversity and complementarity, receiving health information from a variety of sources could increase older adults’ health-related knowledge and enhance their adaptability and responsiveness in managing their health.27,36 Therefore, this study proposed the following hypothesis:
H1
HISB is positively related to PSC among older Chinese adults.
PSC and health self-management
PSC has also been identified as one of the evaluation criteria for determining individuals’ health self-management outcomes.42,43 The main reason is that PSC forested individuals’ positive mindset and empowered them by increasing their confidence and adherence to self-management.44,45 The increasing perceived autonomy support and autonomy motivation internalized the importance of good self-management, and increased their perceptions of competence in dealing with their illness, assisting patients in reducing disease distress and maintaining a physically active lifestyle.46–48 PSC should be a primary consideration for interventions that aim to affect LSM in older adults. Studies have shown that, regardless of different racial/ethnic groups, the sense of purpose in PSC encouraged older adults to overcome perceived barriers and move towards their goals and overcome, positively promoting the maintenance of healthy lifestyles. 49 Conversely, older adults who lack aspirations, goals or a negative mind might face challenges in maintaining autonomy in health self-care, 44 leading to them assuming a passive role in adopting strategies of health self-management. Thus, we proposed the following hypothesis:
H2
PSC is positively associated with LSM among older Chinese adults.
The mediation role of PSC
Prior studies found that PSC may act as a mediator between HISB and health outcomes. For example, Arora and his colleagues 46 found that PSC would be influenced by the difficulties in accessing health information for patients, which, in turn, affected patients’ negative psychosocial health. Likewise, enhancing PSC mediated the relationship between individuals engaged in observational learning and imitating others’ behaviors using an app to seek information and the maintenance of positive health and fitness behaviors. 50 In the current study, we introduced the PSC as one potential cognitive approach of information foraging to examine the mediated mechanism between HISB and LSM, and the varying extent of HISB via various channels on this cognitive structure. In light of these studies, we proposed that:
H3
PSC mediates the association between HISB and LSM among older Chinese adults.
The moderation role of health motivation
According to the self-determination theory, there are several motivations that encourage active health self-management. One of the most common motivations for self-management is the desire to feel good or to avoid negative health-related consequences, 51 such as motivation for health promotion and prevention (MHPP). MHPP refers to individuals’ motivations to actively and vigorously adopt risk-avoidance and prevention strategies. 52 MHPP indicates a higher-level motive with explicit health-related goals. 53 Those who place a high value on health self-management are more likely to engage in health-promoting behaviors than those who place a lower value. 54 For instance, older adults with higher autonomy motivation frequently see exercise as an enjoyable experience accompanied by a sense of accomplishment, and willingly engage in it, thereby recognizing its significant role in maintaining a desirable lifestyle and then taking actual actions. 55 Based on these studies, the proposed moderated effects of MHPP in this study will examine the extent of the relation between health behavioral intentions and actual adoption of LSM among older Chinese adults. Therefore, we proposed the hypothesis 4:
H4
MHPP positively moderates the association between PSC and LSM among older Chinese adults.
Methods
Design and participant
The study was approved by the University of Macau (SSHRE22-APP065-FSS) on September 13, 2022. The current study conducted an online survey in mainland China from June 11 to October 12, 2023. The sample was recruited by Qualtrics (https://www.qualtrics.com/), a well-known global survey company. Qualtrics sent the online survey link to respondents with informative consent. All participants provided written informed consent prior to participating. We collected the survey data with quota sampling based on age and gender distribution in mainland China according to the Seventh National Population Census. 56 Considering that the current study focused on older adults, only participants 60 years old or above were involved. The final sample size was 898. The result of a priori power analysis demonstrates that the minimum sample size of this study is 409. 57 Based on that, the current study has sufficient samples.
Measurement
Lifestyle self-management
Adopted to previous studies of healthy lifestyles, 58 lifestyle self-management was measured using six statements, including the quality of sleep, physical activity and social function. Participants were asked to indicate the extent to which they agreed with the statements: “Spending about 8 h sleeping every day’,” “Sticking to a regular bedtime schedule,” “Exercising actively,’’ “Exercising regularly,” “Having enough time for enjoyable activities,” “Having the best type of social activities to suit you” (from 1 = strongly disagree to 5 = strongly agree),. We averaged these scores to measure HSM, and a higher score presented a stronger agreement with the statements (M = 23.18, SD = 3.70, Cronbach's α = .80).
Health information-seeking behaviors
Drawn from prior studies,36,59 participants were asked to report the frequency of exposure to six media channels by a 4-point Likert scale (from 1 = never to 4 = always). This study integrated six channels into five channels,60,61 television and radio (broadcast media, M = 5.61, SD = 1.48, r = .43), newspaper (print media, M = 2.73, SD = 0.96), search engine (M = 2.92, SD = 0.81), mHealth app (M = 2.92, SD = 0.81) and social media (M = 2.94, SD = 0.78).
Perceived self-management competence
We developed from the perceived health competence scale 42 and diabetes self-management scale 62 to assess the level of health self-management competence among older adults. Participants were asked to rate their ability to manage their health on a five-point scale (from 1 = strongly disagree to 5 = strongly agree). This scale included five statements: “I have abilities to find effective solutions for problems that occur with managing my health”, “I am able to make my life easier by using various devices or seeking help”, “I handle my health well by effective skills”, “I succeed in the problems I undertake to manage my health”, and “I worked out well in preventing diseases”. We averaged the scores to create a new scale representing perceived self-management competence, a higher score indicated a higher competence (M = 19.30, SD = 3.00, Cronbach's α = .77).
Motivation for health promotion and prevention
Drawn from the psychometric properties of the health orientation scale, 52 MHPP was measured by five following statements: “I do things that keep me from becoming physically unhealthy,” “I am motivated to keep myself from becoming physically unhealthy,” “I try to avoid engaging in behaviors that undermine my physical health,” “I have a strong desire to keep myself physically healthy,” and “It's really important to me that I keep myself in proper physical health” (from 1 = strongly disagree to 5 = strongly agree). Personal health motivation was created by averaging these scores. A higher score presented a higher level of health motivation (M = 20.03, SD = 2.87, Cronbach's α = .77).
Control variables
Control variables included age, gender, education, and personal monthly incomes. Additionally, we controlled some health-related variables such as physical condition (i.e., “Obesity or high blood sugar,” “high blood pressure”, “heart conditions,” “chronic lung disease” and “arthritis or rheumatism”; 1 = yes, 0 = no) and mental health (i.e., “Little interest or pleasure in doing things”, “Feeling down, depressed, or hopeless”, “Feeling nervous, anxious, or on edge” and “Not being able to stop or control worrying”; from 1 = not at all to 4 = nearly every day), as our study aims to examine the effects of healthy behaviors among older adults. The descriptive details are shown in Table 1, and The frequency of five channels for health information seeking among older Chinese adults is shown in Table 2.
Table 1.
Descriptive characteristics of the sociodemographic and related variables.
| Natural scale | bp | |
|---|---|---|
| Age (years, M ± SD) | 63.51 ± 3.05 | 0.04 ± 0.03 |
| Birth gender (n, %) | ||
| Male | 489 (54.5%) | N/A |
| Female | 409 (45.5%) | N/A |
| Education (n, %) | ||
| Below primary school | 35 (3.9%) | N/A |
| Middle school | 98 (10.9%) | N/A |
| High school | 280 (31.2%) | N/A |
| Vocation school | 224 (24.9%) | N/A |
| College and above | 261 (29.1%) | N/A |
| Personal incomes (n, %) | ||
| ¥5000 and below | 155 (17.3%) | N/A |
| ¥5001–¥8000 | 317 (35.3%) | N/A |
| ¥8001–¥12,000 | 257 (28.6%) | N/A |
| ¥12,001–¥20,000 | 106 (11.8%) | N/A |
| ¥20,001 and above | 63 (7%) | N/A |
| Physical health (n, %) | ||
| Obesity or high blood sugar | 392 (43.7%) | N/A |
| High blood pressure | 478 (53.2%) | N/A |
| Heart conditions | 247 (27.5%) | N/A |
| Chronic lung disease | 215 (23.9%) | N/A |
| Arthritis or rheumatism | 404 (45%) | N/A |
| Mental health (M ± SD) | 6.80 ± 2.50 | 0.25 ± 0.23 |
| LSM (M ± SD) | 23.18 ± 3.70 | 0.72 ± 0.15 |
| HISB (M ± SD) | ||
| Broadcast media | 5.61 ± 1.48 | 0.60 ± 0.25 |
| Print media | 2.73 ± 0.96 | 0.58 ± 0.32 |
| Search engine | 2.92 ± 0.81 | 0.64 ± 0.27 |
| mHealth app | 2.92 ± 0.81 | 0.64 ± 0.27 |
| Social media | 2.94 ± 0.78 | 0.65 ± 0.26 |
| PSC (M ± SD) | 19.30 ± 3.00 | 0.72 ± 0.15 |
| MHPP (M ± SD) | 20.03 ± 2.87 | 0.55 ± 0.14 |
| N | 898 |
Note. M: Mean; SD: Standard deviation, N/A; Not applicable; LSM: lifestyle self-management, HISB: health information-seeking behavior; PSC: perceived self-management competence; MHPP: motivation for health promotion and prevention.
Table 2.
The frequency of channels for health information seeking among older Chinese adults.
| Channels, n (%) | Never | Sometimes | Usually | Always |
|---|---|---|---|---|
| Television | 37 (4.1) | 210 (23.4) | 409 (45.5) | 242 (26.9) |
| Radio | 124 (13.8) | 231 (25.7) | 374 (41.6) | 169 (18.8) |
| Print media | 118 (13.1) | 214 (23.8) | 357 (39.8) | 209 (23.3) |
| Search engine | 40 (4.5) | 210 (23.4) | 430 (47.9) | 218 (24.3) |
| mHealth app | 44 (4.9) | 201 (22.4) | 437 (48.7) | 216 (24.1) |
| Social media | 37 (4.1) | 192 (21.4) | 456 (50.8) | 213 (23.7) |
All the scales used in this study are derived from well-established literature (see references for details on each measure), with their validity confirmed by extensive empirical research. Additionally, Cronbach's α values for all scales exceed 0.77, indicating good reliability.
Data analysis
Mediating effects were testing using SPSS 26 and Process Macro 63 was used for the mediation and moderation analysis in this study. To compare variables and understand their effects, we converted all variables with the range of 0 to 1 by employing a min–max normalization, referred to as a percentage scale (bp). 64 Second, we conducted Model 4 and Model 1 of Process Macro 63 to examine the mediation and moderation effects. Finally, we used 95% confidence intervals (CIs) to estimate the effects of all variables with bootstrapping 5000 samples.
Results
As shown in Table 1, respondents had an average age of 63.51 years, with 54.5% male and 45.5% female. 46% of older Chinese adults reported having high school or less, and 35.3% had a personal income between 5001 and 8000 RMB per month. High blood pressure is the most prevalent physical condition, accounting for 53.2%, and nearly 45% of them reported poor mental health, which was lower than the average (6.80). The mean score LSM is 23.18, and approximately 48% of older adults fall below this level. Nearly half of older Chinese adults had significant PSC and MHPP scores that were above the mean (19.3 for PSC and 20.03 for MHPP). Furthermore, Table 2 shows that television was identified as the most popular medium, with nearly 27% of older Chinese adults reporting frequent use; nevertheless, 13.1% and 13.8% of them did not seek health information through radio and print media.
The bivariate correlations among primary variables were investigated in this study, shown in Table 3, highlighting the significant correlation observed among these variables.
Table 3.
Results of zero-order correlation.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | LSM | 1 | ||||||||
| 2 | Television | .12*** | 1 | |||||||
| 3 | Radio | .05 | .43*** | 1 | ||||||
| 4 | Print media | .09** | .41*** | .57*** | 1 | |||||
| 5 | Search engine | .14*** | .23*** | .29*** | .29*** | 1 | ||||
| 6 | mHealth app | .12*** | .30*** | .31*** | .38*** | .41*** | 1 | |||
| 7 | Social media | .17*** | .23*** | .29*** | .27*** | .42*** | .43*** | 1 | ||
| 8 | PSC | .62*** | .18*** | .09*** | .16*** | .21*** | .23*** | .25*** | 1 | |
| 9 | MHPP | .61*** | .16*** | .06 | .08* | .12*** | .13*** | .19*** | .72*** | 1 |
Note. LSM: lifestyle self-management; PSC: perceived health self-management competence; MHPP: motivation for health promotion and prevention.
*p < .05; **p < .01; ***p < .001.
H1 predicted that HISB was positively associated with older adults’ PSC. Table 4 shows that HISB via broadcast media (bp = .02, p > .05), print media (bp = .01, p > .05) and search engine (bp = .03, p > .05) was not significantly associated with PSC. In contrast, HISB via mHealth app (bp = .05, p < .05) and social media (bp = .10, p < .001) were positively associated with PSC. Thus, H1 was partly supported.
Table 4.
Path analysis testing the mediation models.
| bp | SE | 95% CI | p | |
|---|---|---|---|---|
| HISB → PSC | ||||
| Broadcast media → PSC | .02 | .02 | [−.027, .068] | .401 |
| Print media → PSC | .01 | .02 | [−.027, .045] | .630 |
| Search engine→ PSC | .03 | .02 | [−.010, .068] | .144 |
| MHealth app→ PSC | .05 | .02 | [.010, .091] | <.05 |
| Social media→ PSC | .10 | .02 | [.057, .139] | <.001 |
| PSC → LSM | .59 | .03 | [.532, .645] | <.001 |
| Direct effect | ||||
| Broadcast media → LSM | .02 | .02 | [−.025, .056] | .451 |
| Print media → LSM | −.02 | .02 | [−.046, .016] | .336 |
| Search engine → LSM | −.01 | .02 | [−.039, .029] | .772 |
| MHealth app → LSM | −.02 | .02 | [−.057, .013] | .209 |
| Social media → LSM | .03 | .02 | [−.008, .064] | .122 |
| Indirect effect | ||||
| Broadcast media → PSC → LSM | .01 | .01 | [−.015, .040] | / |
| Print media → PSC → LSM | .01 | .01 | [−.015, .026] | / |
| Search engine → PSC → LSM | .02 | .01 | [−.006, .043] | / |
| MHealth app→ PSC → LSM | .03 | .01 | [.005, .055] | / |
| Social media → PSC → LSM | .06 | .01 | [.031, .086] | / |
Note: bp: percentage scale; SE: standardized errors; CI: confidence interval; Covariates: sociodemographic variables: age, gender, education, personal income, physical health, mental health; LSM: lifestyle self-management; HISB, health information-seeking behavior; PSC: perceived health self-management competence; MHPP: motivation for health promotion and prevention.
H2 assumed the positive association between PSC and LSM, and the results supported this assumption (bp = .59, p < .001).
H3 predicted that PSC mediated the relationship between HISB and LSM. The statistical significance of indirect effects only occurs when older elders use the mHealth app (bp = .03, CI: [.005, .055]) and social media (bp = .06, CI: [.031, .086]) to seek health information. Conversely, the indirect effects of the association between HISB via broadcast media (bp = .01, CI: [−.015, .040]), print media (bp = .01, CI: [−.015, .026]), or search engine (bp = .02, CI: [−.006, .043]) and LSM through PSC were not statistically significant. Therefore, H3 was partially supported. Additionally, there was no direct effect of five media channels on LSM (bp = .02, p > .05 for broadcast media; bp = −.02, p > .05 for print media; bp = −.01, p > .05 for search engine; bp = −.02, p > .05 for mHealth app; bp = .03, p > .05 for social media), shown in Table 4. Thus, PSC completely mediated the effects of the mHealth app and social media usage on LSM, playing a positive mediated role in this relationship.
As shown in Table 5, The results supported the H4 that MHPP positively moderated the relationship between PSC and LSM (bp = .39, p < .05). Additionally, regardless of whether the level of MHPP was low (bp = .31, CI: [.224, .390]), medium (bp = .36, CI: [.288, .438]) or high (bp = .42, CI: [.329, .508]), PSC remained a positive and significant mediator. Thus, H4 was supported.
Table 5.
Multivariate regression results of LSM and moderated effects.
| bp | SE | 95% CI | p | |
|---|---|---|---|---|
| Age | .04 | .13 | [−.207, .295] | .733 |
| Gender (male = 1) | .01 | .01 | [−.005, .026] | .169 |
| Education | .05 | .02 | [.023, .082] | <.001 |
| Personal income | .03 | .02 | [.002, .061] | <.05 |
| Physical health | −.02 | .02 | [−.046, .014] | .298 |
| Mental health | −.05 | .02 | [−.090, −.018] | <.01 |
| Broadcast media | < .01 | .02 | [−.038, .040] | .957 |
| Print media | −.01 | .02 | [−.036, .024] | .698 |
| Search engine | < .01 | .02 | [−.030, .035] | .888 |
| mHealth app | −.01 | .02 | [−.047, .019] | .407 |
| Social media | .02 | .02 | [−.017, .051] | .334 |
| PSC | .36 | .04 | [.288, .438] | <.001 |
| MHPP | .38 | .04 | [.299, .461] | <.001 |
| PSC × MHPP | .39 | .15 | [.093, .684] | <.05 |
| Conditional effect sizes | ||||
| Low MHPP (M−1SD) | .31 | .04 | [.224, .390] | <.001 |
| Medium (M) | .36 | .04 | [.288, .438] | <.001 |
| High (M + 1SD) | .42 | .05 | [.329, .508] | <.001 |
Note: bp: percentage scale; SE: standardized errors; CI: confidence interval; LSM: lifestyle self-management; PSC: perceived self-management competence; MHPP: motivation for health promotion and prevention.
Discussion
This study highlights the importance of HISB in health promotion among older Chinese adults and emphasizes the crucial role of PSC in the relationship between HISB and LSM. The details are described below.
PSC: a potential cognitive structure between HISB and LSM
First, we identified a critical and positive mediator, namely perceived health self-management competence (PSC) between health information seeking hebavior (HISB) and lifestyle self-management (LSM). While HISB did not find direct effects on LSM from all media channels, the results did show indirect effects on LSM via PSC, emphasizing the importance of a one-rule-per-cycle approach (i.e., PSC) in the information-foraging process. As people age, “struggling for healthy survival” are basic instincts and inherent motivators for a healthy life. 39 The reliable and accurate information obtained from HISB through various channels helps older Chinese adults effectively look for solutions to take care of themselves. The sense of achievement raises their capability to take good care of their health by themselves, hence reducing stress and concerns of unexpected and unpredictable events, finally creating positive and desired results, such as LSM. Furthermore, the LSM of forethought helps older adults who believe they can effectively deal with external challenges by motivating and guiding them to properly plan and structure their lives. 65 As a result, PSC enhances older adults’ competence and confidence when seeking health information, motivating and increasing their persistence and commitment to LSM.
The differentiating role of HISB through multiple media channels
Second, the findings showed that HISB through various media channels may bring different outcomes. Specifically, we found that using mHealth apps and social media is positively related to PSC among older adults in China. However, we did not find the effects of PSC through other media channels, such as broadcast media, print media, and search engines. The outcomes were to be expected. The personalized functions in mHealth apps, such as reminders, game elements, social affordance, personalized interventions, and health education, 66 assist older adults in accessing rich health information with less time and effort and obtaining desired rewards from health information. 33 The social networking sites and interactivity provided by social media enable older adults to effectively obtain detailed and personalized information from online peer-to-peer social support groups.67,68 These findings indicate that older Chinese adults tend to take an active role in their care and decision-making processes via online HISB, 39 enhancing their sense of capability for health self-management. However, due to the passive nature of information consumption through traditional media, 60 older adults are more likely to passively encounter health self-management skills rather than actively seek desired information via broadcast or print media, which may alter their motives. Although search engine provides rich and specific content-oriented topics where people can look for their desired information by typing keywords, 36 it is important to note that a significant number of older adults in China lack the basic or advanced online information-seeking skills required for effective use of search engines. 69
According to the intensity of HISB through media sources on PSC, the impact of social media usage has a greater impact on PSC than mHealth app usage. While prior studies have shown that there may be significant overlap in the health information resources provided by mHealth apps and social media platforms, 36 our findings suggest that older adults perceive a greater acquisition of health self-management skills from using social media than from mHealth app applications. The plausible reason is that when older adults “hunt” for patches through various media channels, their perception of the usefulness and relevance of the information sources considered important foraging patches may differ. 30 Consequently, older adults may perceive varying levels of development of health-related self-management skills related to their health. According to the optimal foraging principle, we can deduce that older adults may prefer and choose to forage more useful and relevant patches through social media rather than other channels. This finding highlights the varying intermediate outcomes resulting from interaction with different media among older adults in China.
MHPP: an intrinsic motivation for health self-management
Third, we found the moderated role of MHPP between PSC and LSM. The finding indicated that the effects of PSC on LSM would be significantly enhanced with higher MHPP. The MHPP encourages older people to identify “one's willingness and ability” as a key motivator to enhance their LSM. 70 MHPP activated could boost older adults’ confidence and sense of self-efficacy when it comes to healthcare or self-management, which may further have a positive impact on their self-management practices. Furthermore, MHPP translates older adults’ lower-level health motives (i.e., PSC) into actual planning and behaviors. 53 This implies that, in line with self-determination theory, older adults who are highly self-determined in the domain of health promotion, 55 which may enhance their health awareness and drive their actions related to the promotion and prevention of health. Thereby, compared to the external motivation (i.e., PSC) obtained from HISB in older Chinese adults, MHPP can be considered an intrinsic motivation, which has been identified as one of the most influential predictors of sustained health behaviors among older adults. In light of this, we believe that MHPP serves as a greater superior intrinsic cognitive motive, suggesting that older Chinese adults should engage in foresting MHPP before doing tasks related to their health. This finding is consistent with prior studies demonstrating the importance of maintaining cognitive functional status is particularly important in older age groups than other age groups 53 and the importance of fundamental motivation of “one's willingness and ability”, 70 highlighting the significance of higher MHPP in health promotion for older Chinese adults.
Implications and limitations
This study has some implications. First, we adopted the IFT in the context of health-related information-seeking behavior. The findings shed light on the characteristics of older adults, adding to previous research that has overlooked this demographic. When a statistically significant mediating mechanism of PSC is detected, it also implies that behavioral intention of LSM (i.e., PSC) can be considered an effective external motivation obtained from HISB in older Chinese adults. Second, the extent to which older adults’ HISB contributed to their PSC varies according to the media sources used. This variation can be attributed to differences in cognitive abilities among older adults, as well as preferences and decisions. Third, we consider the moderated significance of intrinsic motives in health promotion. It is understandable for older Chinese adults to strengthen their health motives. Older adults with more intrinsic motives can promote their healthy behavior change more effectively than those without such motives.
Several limitations of this study should be noted. First, this study only examined the one of cognitive characteristics of HISB in relation to health promotion behaviors. However, older adults, especially older Chinese adults have different cognition performances in this pathway, such as cognition dissonance and perceived risks, which might contribute to different outcomes for LSM. Further studies could focus on other cognitive factors to explore more characteristics. Second, our findings were based on cross-sectional and self-reported data that only explored the effect of search activities via media sources on LSM in a limited period. Without considering other periods, future research could investigate the changes in cognitive abilities over time. One potential approach to overcome this limitation is to conduct panel data studies that observe the development of health behavior through search activities across different media sources. This would provide a more complete understanding of cognitive changes in older Chinese adults and their relationship to changes in health behavior over time. Third, an online survey requires participants to master internet access and necessary internet skills. This may exclude elders who don’t meet these requirements from the current study, thereby bringing bias. Future research could focus on older adults by conducting offline surveys, such as door-to-door or telephone surveys, to understand elders’ HISB more comprehensively. Finally, this study did not consider television as an independent media channel during the data analysis. Given that television is a significant source of health information for Chinese residents, 71 future research could benefit from a more refined classification of media channels. This would enable a more precise understanding of the various outcomes associated with multi-channel health information seeking among the elderly.
Conclusion
The current study aims to investigate the underlying mechanisms of how multi-channel health information seeking behaviour (HISB) is associated with lifestyle management (LSM) among older Chinese adults. The findings highlight the significant mediating roles of perceived health self-management competence (PSC) between HISB and LSM. Specifically, HISB using social media and mHealth app may positively associate with LSM through PSC, while HISB using print media, broadcast media, and search engines show no statistically significant effects on LSM. Moreover, motivation for health promotion and prevention (MHPP) positively moderates the association between PSC and LSM. That is, elders may gain greater benefits in improving their healthy lifestyle from HISB when they have a higher level of health promotion and prevention motivations.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076241305481 for Linking multiple-channel information seeking and lifestyle among Chinese older adults: A moderation and mediation analysis by Qingrui Li, Yifang Wu and Xinshu Zhao in DIGITAL HEALTH
Footnotes
Contributorship: QL contributed to conceptualization (lead); review and editing (lead); and writing‒original draft (equal). YW contributed to writing‒original draft (lead); writing‒review and editing (equal). YW contributed to software (lead); review and editing (equal). XZ contributed to writing‒review and editing (equal); conceptualization (support); and supervision. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Consent to participate: All participants provided written informed consent prior to participating.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported in part by grants of the 10.13039/501100004733 University of Macau, including CRG2021-00002-ICI, ICI-RTO-0010-2021, CPG2023-00003-FSS, Xinshu Zhao PI; Macau Higher Education Fund, HSS-UMAC-2020-02, Xinshu Zhao PI.
Ethical approval: This study analyzed secondary data. The data from a quota sampling Online Survey in China have obtained ethical approval.
Ethical considerations: The study was approved by the University of Macau (SSHRE22-APP065-FSS) on September 13, 2022.
ORCID iDs: Qingrui Li https://orcid.org/0000-0001-9711-4239
Yifang Wu https://orcid.org/0009-0006-8614-9683
Supplemental material: Supplemental material for this article is available online.
References
- 1.Lu J, Liu Q. Four decades of studies on population aging in China. China Popul Dev Stud 2019; 3: 24–36. [Google Scholar]
- 2.Fang EF, Scheibye-Knudsen M, Jahn HJ, et al. A research agenda for aging in China in the 21st century. Ageing Res Rev 2015; 24: 197–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu N, Xie X, Cai M, et al. Trends in health service needs, utilization, and non-communicable chronic diseases burden of older adults in China: evidence from the 1993 to 2018 National Health Service Survey. Int J Equity Health 2023; 22: 169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han Y, He Y, Lyu J, et al. Aging in China: perspectives on public health. Glob Health J 2020; 4: 11–17. [Google Scholar]
- 5.Green KE. Identification of the facets of self-health management. Eval Health Prof 1985; 8: 323–338. [DOI] [PubMed] [Google Scholar]
- 6.Hu X, Wang T, Huang D, et al. Impact of social class on health: the mediating role of health self-management. PLoS ONE 2021; 16: e0254692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cramm JM, Hartgerink JM, Steyerberg EW, et al. Understanding older patients’ self-management abilities: functional loss, self-management, and well-being. Qual Life Res 2013; 22: 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cramm JM, Twisk J, Nieboer AP. Self-management abilities and frailty are important for healthy aging among community-dwelling older people; a cross-sectional study. BMC Geriatr 2014; 14: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jonker AAGC, Comijs HC, Knipscheer KCPM, et al. Promotion of self-management in vulnerable older people: a narrative literature review of outcomes of the Chronic Disease Self-Management Program (CDSMP). Eur J Ageing 2009; 6: 303–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pettman TL, Misan GM, Owen K, et al. Self-management for obesity and cardio-metabolic fitness: description and evaluation of the lifestyle modification program of a randomised controlled trial. Int J Behav Nutr Phys Act 2008; 5: 53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calder PC, Carding SR, Christopher G, et al. A holistic approach to healthy ageing: how can people live longer, healthier lives? J Hum Nutr Diet 2018; 31: 439–450. [DOI] [PubMed] [Google Scholar]
- 12.Chei C-L, Lee JM-L, Ma S, et al. Happy older people live longer. Age Ageing 2018; 47: 860–866. [DOI] [PubMed] [Google Scholar]
- 13.Sutipan P, Intarakamhang U, Kittipichai W, et al. Effects of self-management program on healthy lifestyle behaviors among elderly with hypertension. Int J Behav Sci 2018; 13: 38–50. [Google Scholar]
- 14.Zhang M, Chao J, Li D, et al. The effect of older-person centered and integrated health management model on multiple lifestyle behaviors: a randomized controlled trial from China. Arch Gerontol Geriatr 2018; 79: 45–51. [DOI] [PubMed] [Google Scholar]
- 15.Xu L, Xie L, Li X, et al. A meta-analysis of factors influencing health literacy among Chinese older adults. J Public Health 2022; 30: 1-12. DOI: 10.1007/s10389-021-01638-3 [DOI] [Google Scholar]
- 16.Go E, You KH. Health-related online information seeking and behavioral outcomes: fatalism and self-efficacy as mediators. Soc Behav Personal Int J 2018; 46: 871–879. [Google Scholar]
- 17.Jiang S, Street RL. Pathway linking internet health information seeking to better health: a moderated mediation study. Health Commun 2017; 32: 1024–1031. [DOI] [PubMed] [Google Scholar]
- 18.Jin SW, Lee Y, Dia DA. Analyzing paths from online health information seeking to colorectal cancer screening using health literacy skills frame and cognitive mediation model. Patient Educ Couns 2019; 102: 416–423. [DOI] [PubMed] [Google Scholar]
- 19.Liu PL. COVID-19 Information seeking on digital media and preventive behaviors: the mediation role of worry. Cyberpsychology Behav Soc Netw 2020; 23: 677–682. [DOI] [PubMed] [Google Scholar]
- 20.Vellone E, Pancani L, Greco A, et al. Self-care confidence may be more important than cognition to influence self-care behaviors in adults with heart failure: testing a mediation model. Int J Nurs Stud 2016; 60: 191–199. [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Tian L, Huebner ES. Parental control and Chinese adolescent smoking and drinking: the mediating role of refusal self-efficacy and the moderating role of sensation seeking. Child Youth Serv Rev 2019; 102: 63–72. [Google Scholar]
- 22.Zhang L, Jiang S. Linking health information seeking to patient-centered communication and healthy lifestyles: an exploratory study in China. Health Educ Res 2021; 36: 248–260. [DOI] [PubMed] [Google Scholar]
- 23.Zhao X, Cai X. The role of risk, efficacy, and anxiety in Smokers’ cancer information seeking. Health Commun 2009; 24: 259–269. [DOI] [PubMed] [Google Scholar]
- 24.Zimmerman MS, Shaw G, Jr. Health information seeking behaviour: a concept analysis. Health Inf Libr J 2020; 37: 173–191. [DOI] [PubMed] [Google Scholar]
- 25.Brashers DE. Communication and uncertainty management. J Commun 2001; 51: 477–497. [Google Scholar]
- 26.Hao L, Xu X, Dupre ME, et al. Adequate access to healthcare and added life expectancy among older adults in China. BMC Geriatr 2020; 20: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chu L, Fung HH, Tse DCK, et al. Obtaining information from different sources matters during the COVID-19 pandemic. Gerontologist 2021; 61: 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Underhill C, McKeown L. Getting a second opinion: health information and the internet. Health Rep 2008; 19: 65. [PubMed] [Google Scholar]
- 29.Pirolli P, Card S. Information foraging. Psychol Rev 1999; 106: 643–675. [Google Scholar]
- 30.Dennis AR, Taylor NJ. Information foraging on the web: the effects of “acceptable” internet delays on multi-page information search behavior. Decis Support Syst 2006; 42: 810–824. [Google Scholar]
- 31.Pirolli P. Information foraging theory: adaptive interaction with information. Oxford, New York: Oxford University Press, 2007. [Google Scholar]
- 32.Liang J, Liu J-E, Mak YW, et al. Preliminary effects of a WeChat-based educational intervention on social participation among older adults in a community. Int J Older People Nurs 2023; 18: e12573. [DOI] [PubMed] [Google Scholar]
- 33.Pan J, Dong H. Mhealth adoption among older Chinese adults: a conceptual model with design suggestions. Int J Human–Computer Interact 2023; 39: 1072–1083. [Google Scholar]
- 34.Song L, Ge Y, Zhang X. The relationship between WeChat use by Chinese urban older adults living alone and their subjective well-being: the mediation role of intergenerational support and social activity. Psychol Res Behav Manag 2021; 14: 1543–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yu N, Jiang Z. Preference and trust: an investigation of information source of COVID-19 among people over 50 years. Asia Pac J Public Health 2020; 32: 476–478. [DOI] [PubMed] [Google Scholar]
- 36.Zhang L, Qin Y, Li P. Media complementarity and health information acquisition: a cross-sectional analysis of the 2017 HINTS-China survey. J Health Commun 2020; 25: 291–300. [DOI] [PubMed] [Google Scholar]
- 37.Nelson D, Kreps G, Hesse B, et al. The health information national trends survey (HINTS): development, design, and dissemination. J Health Commun 2004; 9: 443–460. [DOI] [PubMed] [Google Scholar]
- 38.Kelley MS, Su D, Britigan DH. Disparities in health information access: results of a county-wide survey and implications for health communication. Health Commun 2016; 31: 575–582. [DOI] [PubMed] [Google Scholar]
- 39.Pourrazavi S, Bazargan-Hejazi S. The model of online health information-seeking behavior among older adults. Biosoc Health J 2024; 1: 33–40. [Google Scholar]
- 40.Manafo E, Wong S. Health literacy programs for older adults: a systematic literature review. Health Educ Res 2012; 27: 947–960. [DOI] [PubMed] [Google Scholar]
- 41.Yan YY. Online health information seeking behavior in Hong Kong: an exploratory study. J Med Syst 2010; 34: 147–153. [DOI] [PubMed] [Google Scholar]
- 42.Smith MS, Wallston KA, Smith CA. The development and validation of the perceived health competence scale. Health Educ Res 1995; 10: 51–64. [DOI] [PubMed] [Google Scholar]
- 43.Togari T, Ikezaki S, Yamazaki Y, et al. The development of perceived health competence scale (PHCS) Japanese version. Jpn J Health Hum Ecol 2004; 70: 184–195. [Google Scholar]
- 44.McWilliam CL, Brown JB, Carmichael JL, et al. A new perspective on threatened autonomy in elderly persons: the disempowering process. Soc Sci Med 1994; 38: 327–338. [DOI] [PubMed] [Google Scholar]
- 45.Wang R, Zhou C, Wu Y, et al. Patient empowerment and self-management behaviour of chronic disease patients: a moderated mediation model of self-efficacy and health locus of control. J Adv Nurs 2022; 78: 1055–1065. [DOI] [PubMed] [Google Scholar]
- 46.Arora NK, Johnson P, Gustafson DH, et al. Barriers to information access, perceived health competence, and psychosocial health outcomes: test of a mediation model in a breast cancer sample. Patient Educ Couns 2002; 47: 37–46. [DOI] [PubMed] [Google Scholar]
- 47.Koponen AM, Simonsen N, Suominen S. Determinants of physical activity among patients with type 2 diabetes: the role of perceived autonomy support, autonomous motivation and self-care competence. Psychol Health Med 2017; 22: 332–344. [DOI] [PubMed] [Google Scholar]
- 48.Mohn J, Graue M, Assmus J, et al. Self-reported diabetes self-management competence and support from healthcare providers in achieving autonomy are negatively associated with diabetes distress in adults with type 1 diabetes. Diabet Med 2015; 32: 1513–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khan MM, Hill PL, O’Brien C. Hope and healthy lifestyle behaviors in older adulthood. Aging Ment Health 2023; 27: 1436–1442. [DOI] [PubMed] [Google Scholar]
- 50.Ekpezu AO, Wiafe I, Oinas-Kukkonen H. Enhancing perceived health competence: the impact of persuasive social support features in health and fitness apps. Int J Human–Computer Interact 2024; 40: 8076–8090. [Google Scholar]
- 51.Lee CC, Enzler CJ, Garland BH, et al. The development of health self-management among adolescents with chronic conditions: an application of self-determination theory. J Adolesc Health 2021; 68: 394–402. [DOI] [PubMed] [Google Scholar]
- 52.Masiero M, Oliveri S, Cutica I, et al. The psychometric properties of the Italian adaptation of the Health Orientation Scale (HOS). Health Qual Life Outcomes 2020; 18: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schüz B, Wurm S, Warner LM, et al. Health motives and health behaviour self-regulation in older adults. J Behav Med 2014; 37: 491–500. [DOI] [PubMed] [Google Scholar]
- 54.Hooker K, Kaus CR. Possible selves and health behaviors in later life. J Aging Health 1992; 4: 390–411. [Google Scholar]
- 55.Ferrand C, Martinent G, Bonnefoy M. Exploring motivation for exercise and its relationship with health-related quality of life in adults aged 70 years and older. Ageing Soc 2014; 34: 411–427. [Google Scholar]
- 56.National Bureau of Statistics of China. Main data of the seventh national population census. https://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817185.html (2021).
- 57.Jobst LJ, Bader M, Moshagen M. A tutorial on assessing statistical power and determining sample size for structural equation models. Psychol Methods 2023; 28: 207–221. [DOI] [PubMed] [Google Scholar]
- 58.Wang L, Luo J, Luo J, et al. The effect of internet use on adolescents’ lifestyles: a national survey. Comput Hum Behav 2012; 28: 2007–2013. [Google Scholar]
- 59.Rains SA, Ruppel EK. Channel complementarity theory and the health information-seeking process: further investigating the implications of source characteristic complementarity. Commun Res 2016; 43: 232–252. [Google Scholar]
- 60.Dutta-Bergman MJ. Primary sources of health information: comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Commun 2004; 16: 273–288. [DOI] [PubMed] [Google Scholar]
- 61.Zhao X, Zhu J-H, Li H, et al. Media effects under a monopoly: the case of Beijing in economic reform. Int J Public Opin Res 1994; 6: 95–117. [Google Scholar]
- 62.Wallston KA, Rothman RL, Cherrington A. Psychometric properties of the perceived diabetes self-management scale (PDSMS). J Behav Med 2007; 30: 395–401. [DOI] [PubMed] [Google Scholar]
- 63.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. 2nd ed. New York: Guilford Press, 2018. [Google Scholar]
- 64.Liu PL, Ye JF, Ao HS, et al. Effects of electronic personal health information technology on American women’s cancer screening behaviors mediated through cancer worry: differences and similarities between 2017 and 2020. Digit Health 2023; 9: 20552076231185271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol 2001: 52: 1–26. [DOI] [PubMed]
- 66.Liu N, Yin J, Tan SS-L, et al. Mobile health applications for older adults: a systematic review of interface and persuasive feature design. J Am Med Inform Assoc 2021; 28: 2483–2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Orr D, Baram-Tsabari A, Landsman K. Social media as a platform for health-related public debates and discussions: the polio vaccine on Facebook. Isr J Health Policy Res 2016; 5: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang L, Jung EH, Chen Z. Modeling the pathway linking health information seeking to psychological well-being on WeChat. Health Commun 2020; 35: 1101–1112. [DOI] [PubMed] [Google Scholar]
- 69.Wu D, Li Y. Online health information seeking behaviors among Chinese elderly. Libr Inf Sci Res 2016; 38: 272–279. [Google Scholar]
- 70.Choi S, Song M, Chang SJ, et al. Strategies for enhancing information, motivation, and skills for self-management behavior changes: a qualitative study of diabetes care for older adults in Korea. Patient Prefer Adherence 2014; 8: 219–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lu Q, Schulz PJ, Chang A. Medication safety perceptions in China: media exposure, healthcare experiences, and trusted information sources. Patient Educ Couns 2024; 123: 108209. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076241305481 for Linking multiple-channel information seeking and lifestyle among Chinese older adults: A moderation and mediation analysis by Qingrui Li, Yifang Wu and Xinshu Zhao in DIGITAL HEALTH