Abstract
Introduction:
The present scientific consensus is that the menstrual cycle (MC) and hormonal contraceptive (HC) cycle only influence performance trivially. Nevertheless, athletes perceive changes in performance that they associate with different phases of their hormonal cycle.
Methods:
A total of 959 female athletes completed a questionnaire, of which 750 were included in the present analysis. The questionnaire included questions about demographics and experiences of the MC and HC (symptoms, perceived impact on performance characteristics).
Results:
In total, 55% of athletes reported a natural MC while 45% reported HC use. Meanwhile, 56% of all athletes reported a decline in perceived performance during the bleeding or inactive phase, whereas 26% of all athletes reported no changes in performance over their hormonal cycle. All athletes reported an average of 10 ± 7 symptoms during hormonal cycles. The naturally menstruating (NM) group reported more symptoms than the HC group (p < .05). The most frequent symptoms reported were abdominal pain, bloating, and mood swings. Only 7% of all athletes (4.1% in NM and 11.3% in HC) reported an absence of any symptoms. Quantity of total symptoms was associated with a perceived decrease in performance (R2 = .138, p < .05). Hormonal cycles had the greatest negative effect on mental performance with 37% reporting a large to very large effect.
Conclusions:
Perceived negative effects on performance were similar in both NM and HC groups while perceived mental performance (e.g., mood and attention) appeared to be most affected by both MC and HC.
Keywords: menstrual cycle, hormonal contraceptives, sex hormones, mental performance, side effects
Female physiology is influenced by sex hormone fluctuations that occur during the menstrual cycle (MC) and during hormonal contraceptive (HC) use. In addition to reproductive function, estrogen and progesterone have several nonreproductive purposes in the body that may influence female health and even athletic performance (Elliott-Sale, McNulty, et al., 2020; Elliott-Sale, Ross, et al., 2020; McNulty et al., 2020; Oosthuyse & Bosch, 2010). So far, experimental studies have not been able to fully clarify whether, and how, hormonal cycle phases influence athlete performance. However, recent evidence suggests that the beginning of the MC (menstruation or early follicular phase) may have a minor or trivial negative effect on performance compared with other phases of the MC (McNulty et al., 2020). Although the current consensus view is that the impact of the MC and HC use on various aspects of physiology is only small or even nonexistent (D’Souza et al., 2023), it is important to recognize that 50%–80% of female athletes report that their MC affects performance (Armour et al., 2020; Carmichael et al., 2021; Solli et al., 2020). Individual athletes experience cycle-related symptoms such as cramps, gastrointestinal distress, and mood swings, especially a few days before, and during, menstruation. Naturally, these symptoms may affect their desire to exercise and, in more severe cases, may affect performance and/or the ability to exercise (Bruinvels et al., 2017, 2021; Ekenros et al., 2022; Martin et al., 2018; Solli et al., 2020).
The hormonal cycles are not just biological processes but can also influence biopsychological characteristics (Chrisler, 2013). To this end, the hormonal fluctuations within the MC and HC have a bidirectional relationship that also influences behavior. Although the mechanisms that control the MC or HC are physiologically similar, beliefs, attitudes, and culture impact how women subjectively experience their cycle (Chrisler, 2013).
About half of female athletes report using HC, with 70%–75% using oral contraceptive pills (Martin et al., 2018; Solli et al., 2020; Torstveit & Sundgot-Borgen, 2005). While oral contraceptive pills have been the most common form of female-controlled contraception, other forms of contraception, including hormonal intrauterine devices, have become popular in recent years, especially in the athletic population (Ekenros et al., 2022; Engseth et al., 2022). Combined HCs suppresses the body’s endogenous hormone production, resulting in significantly or completely attenuated concentrations of all the female sex hormones (De Leo et al., 2016). Progestin-only contraceptives, including hormonal intrauterine devices and minipills, can also modify the body’s endogenous hormone production and inhibit ovulation, although hormone profiles vary and ovulation may also occur (Apter et al., 2014). Both forms of HC can be used to manage or treat negative MC-associated symptoms or to support the treatment of other medical conditions, whereas HC use is not solely for family planning (Ekenros et al., 2022).
When evaluating the effects of MC and HC use on performance, the indirect effects of sex hormone fluctuations, including cycle-related symptoms, should be considered (Bruinvels et al., 2022). At present, athletes’ perceived effects of their respective MC or HC on various performance characteristics and associated symptoms are unclear (Paludo et al., 2022). It is essential to gather and analyze this information from athlete populations to better understand and support the overall health, well-being, and performance of female athletes. The aim of this study was to provide deeper insights into the perceived impact, and magnitude of impact, of the MC and the HC cycle (hormonal cycles) on various performance characteristics and associated symptoms in female athletes.
Methods
Study Design
The current study was a part of a larger cross-sectional study conducted with an online questionnaire created with the Webropol 3.0 Online Survey and Reporting Tool (Webropol Oy 2020). The questionnaire collected data from six domains: (a) participant characteristics; (b) low-energy-availability-related issues (i.e., injuries, gastrointestinal function, and MC); (c) disordered eating (including restrictive eating) and eating disorders; (d) menstrual cycle function and HC use; (e) athletes’ perception of the effects of hormonal cycle on performance; and (f) communication around MC (Ravi et al., 2021). The questionnaire required about 30 min to complete. This study reports data on participant characteristics, menstrual status and use of HC, as well as athlete perceptions of the impact of their MC or HC cycle on performance. Nota bene, when MC and HC cycle are referred to together, we will use the term “hormonal cycle(s).”
Recruitment and Participants
A link to the questionnaire was promoted by the Finnish Olympic Committee, national sports federations, and sports academies, and distributed via social media (e.g., Twitter, Instagram) in Finnish. The survey was available online for 4 months. Finnish-speaking female athletes who were at least 15 years old could participate in the study regardless of their level of performance. The study was reviewed by the Ethical Committee of the University of Jyväskylä. Before filling out the questionnaire, the athletes were informed about the aims of the study and the content of the questionnaire. They were informed that participation in the study was voluntary and that they were free to leave questions unanswered or decline to participate at any time. Initially, 959 athletes representing 74 different sports completed the questionnaire. Athletes were excluded from the analyses of the present study if (a) their questionnaire was incomplete (n = 90); (b) they were over 45 years of age (n = 24); (c) they reported a menstrual dysfunction, for example, amenorrhea or oligomenorrhea (n = 71); (d) they did not experience bleeding without HC (n = 6); or (e) they reported an endocrinal condition, such as endometriosis or gynecological cancer (n = 10) (Elliott-Sale et al., 2021; Koltun et al., 2020). Ultimately, 750 participants from 73 different sports fulfilled the inclusion criteria and were included in the final analysis (Figure 1).
Figure 1 —
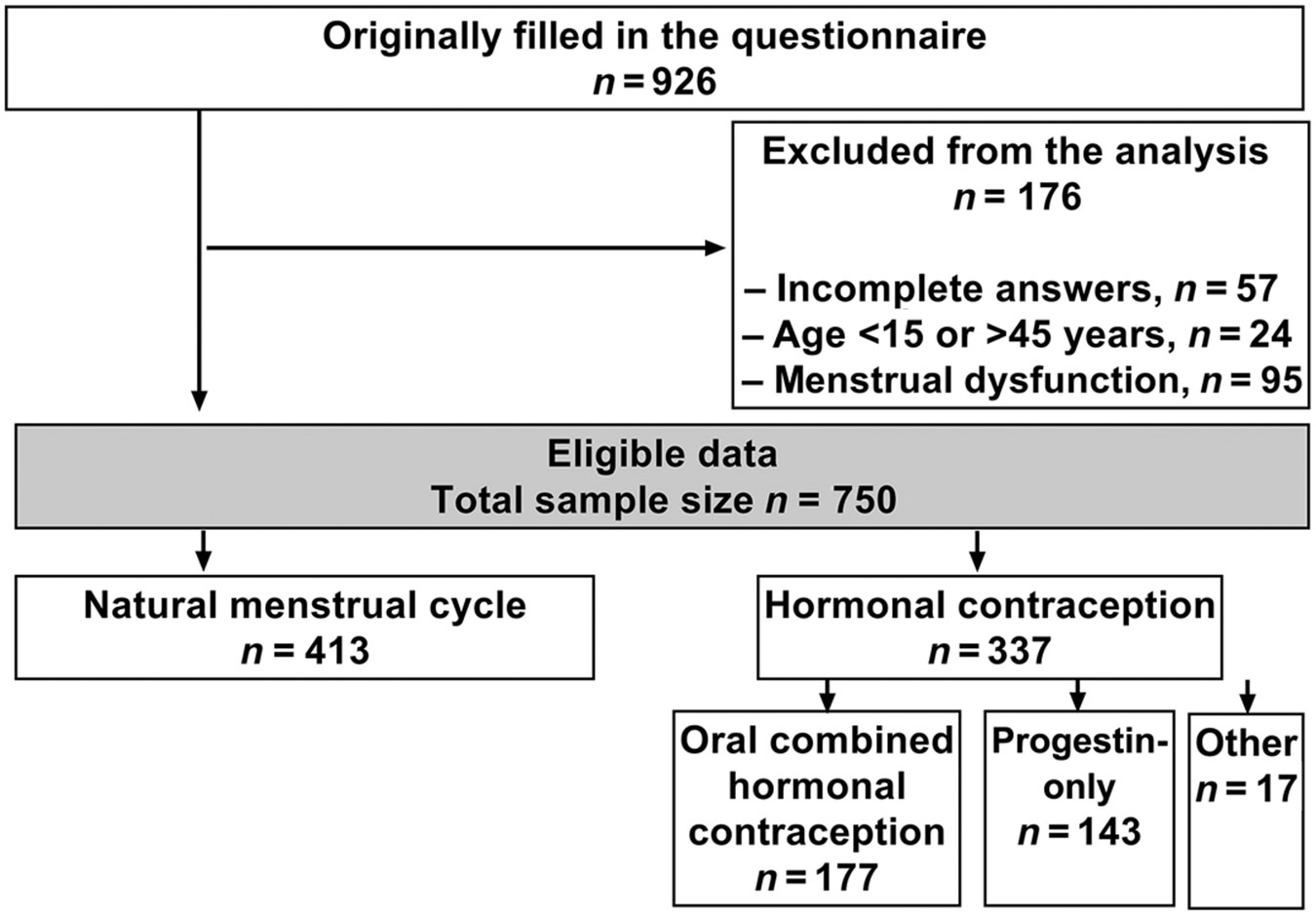
Flow chart of the included athletes and the prevalence of the type of hormonal contraceptives used.
Questionnaire
Data were collected via an online questionnaire designed according to the study’s aim and developed by an expert panel of former athletes, coaches, physiologists, and researchers with experience from similar projects and relevant medical expertise. Based on a pilot study of the questionnaire involving 12 athletes, minor modifications were made to the questions. Athletes provided self-reported information about their year of birth, height, weight, and annual training volume. Athletes indicated their competition level by selecting one of the following options: regional/district level athlete (30.0% of the athletes), national level athlete (42.1% of the athletes), or international level athlete (27.9% of the athletes).
Sixty questions were asked about menstrual status and HC use, as well as perceptions of the impact of the MC or HC cycle on performance. Current HC users completed an additional set of questions about the type of HC they were using and their motives to use HC. Changes in physical fitness (perceived quality of training), and performance (results in tests or competitions) during MC or HC, as well as MC- and HC-related negative side effects were recorded as described by Solli et al. (2020). Briefly, a simple four-phase definition of the MC/HC cycle was provided in which the first phase was defined as early follicular/inactive, the second phase as late follicular/early active, the third phase as early- or mid-luteal phase/mid-active phase, and the fourth phase as 1–4 days before the menstruation/inactive phase (Figure 2).
Figure 2 —
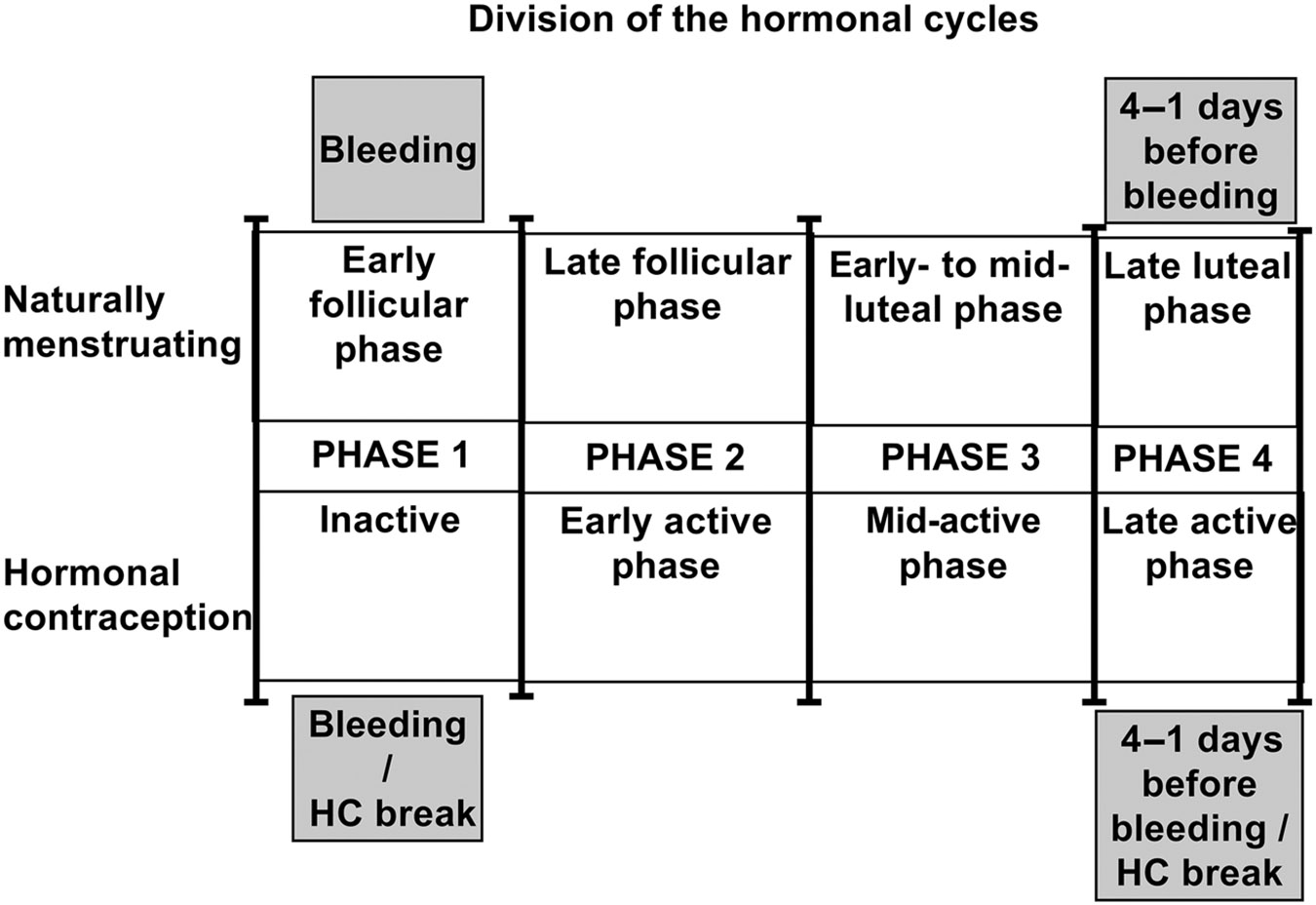
Division of hormonal cycles into four phases similar to Solli et al. (2020). Because of the self-reported nature of this study, the phases here should not be confused with the specific hormonal phases and respective hormonal concentrations outlined by Elliott-Sale et al. (2021). HC = hormonal contraceptive.
Symptoms were assessed in the same four phases using a list modified from Solli et al. (2020). Symptoms included: abdominal pain, bloating, constipation, decreased appetite, diarrhea, fatigue, headache, increased appetite, irritability, lower back pain, mood swings, nausea, pain radiating into the legs, weight decrease, weight gain, and other (with a prompt to describe what other symptoms may be experienced). The perceived effects on performance were asked in a multiple-choice table entitled “Which characteristics or skills are affected by your (menstrual/hormone) cycle and to which extent?” The questions were specific to endurance, speed, explosiveness, technique, skill, flexibility, tactics/cognitive skills, strength, and mental performance and were assessed on a 5-point Likert scale from 1 = no effect to 5 = very large effect. Finally, the athletes were asked about the possible changes they have made to training due to MC or HC symptoms using an open-ended question.
Statistics
Continuous variables were tested for normality before statistical analysis. Descriptive data for continuous variables were recorded as means (SD) and for categorical variables as totals and percentages. For the categorical variables, we combined “large” and “very large” as well as “small” and “medium” resulting in a condensed 3-point scale answer rather than a 5-point scale. For continuous variables, the Shapiro–Wilk test and standard visual inspection were used to examine the assumption of normality. Cross tabulations with Pearson’s chi-squared analyses were used to examine relationships between categorical variables, with Fisher’s exact tests used where <80% of the expected cell counts were >5. In line with Solli et al. (2020), the total score of side effects was calculated as the sum of reported symptoms during each phase of the MC or HC. Briefly, global differences in the number of side effects across the phases were assessed with linear mixed-effects models including MC or HC phase as a fixed factor and athlete as a random factor. Two separate logistic regression models were fitted to assess the association between the perceived physical performance and the experienced symptoms, while adjusting for body mass index, training volume, and HC use. The odds ratio for each variable and the associated 95% confidence interval were calculated. Nagelkerke R2 was obtained for all multiple models to estimate their accountability levels. For the analysis, the variable for the best and worst performance was changed to a dichotomous variable. To establish discriminant validity related to the coping factors, multi-collinearity was assessed to ensure each factor of coping was its own distinguishable factor (i.e., correlation > .90 between factors and a variance inflation factor > 10 indicates multi-collinearity) (Hair et al., 1998). In the present study, the variance inflation factor values ranged from 1.010 to 1.070. All statistical tests were two-sided, and p values < .05 were considered statistically significant. Statistical analyses were conducted using Statistical Package for the Social Sciences (version 27.0, IBM Corp.).
Results
The descriptive characteristics of the athletes that were included in the study are presented in Table 1. The naturally menstruating (NM) group was younger than the HC group (24.0 ± 7.7 vs. 25.2 ± 6.9, p < .05). Forty-five percent of athletes used HC. Combined oral contraceptives were used by 48%, vaginal ring by 4%, and patch by 1% of the HC group. The hormonal intrauterine device was used by 24%, the minipill by 14%, and the implant by 5% of HC users. In addition, 4% of athletes reported using some other type of HC method, for example, injection. The main reason given for using HC was to prevent pregnancy (86%). Other common reasons for HC used were to reduce bleeding (43%), to reduce menstrual pain (41%), and to regulate/plan menstrual bleeding (29%).
Table 1.
Participant Characteristics
| All participants (n = 750) |
Hormonal contraceptive group (n = 337) |
Naturally menstruating group (n = 413) |
Between groups (p) |
|
|---|---|---|---|---|
| Age (years) | 24.5 ± 7.4 | 25.2 ± 6.9 | 24.0 ± 7.7 | .024 |
| Body mass index (kg/m2) | 23.2 ± 3.4 | 23.3 ± 3.0 | 23.3 ± 3.7 | .990 |
| Yearly training volume (hr) | 570 ± 290 | 570 ± 290 | 560 ± 280 | .604 |
Note. Data presented as mean ± SD.
Hormonal Cycle and Performance
Regardless of group, most of the athletes (56%) reported that their perceived performance was worse in Phase 1 (early follicular/inactive) compared with other phases. Similarly, athletes reported most commonly (42%) that their best-perceived performance took place during Phase 2 (late follicular/early active). Athletes in the HC group reported that they experienced no differences between phases significantly more often than the NM group (p < .05). The competition level of the athletes had no effect on the phase in which performance was perceived as best or worst.
Perceived Influence of Hormonal Cycles on Characteristics of Performance
Perceived mental performance was affected more in the HC group compared with the NM group (43% vs. 33% reported a “large effect” or “very large effect,” p < .05; Figure 3).
Figure 3 —
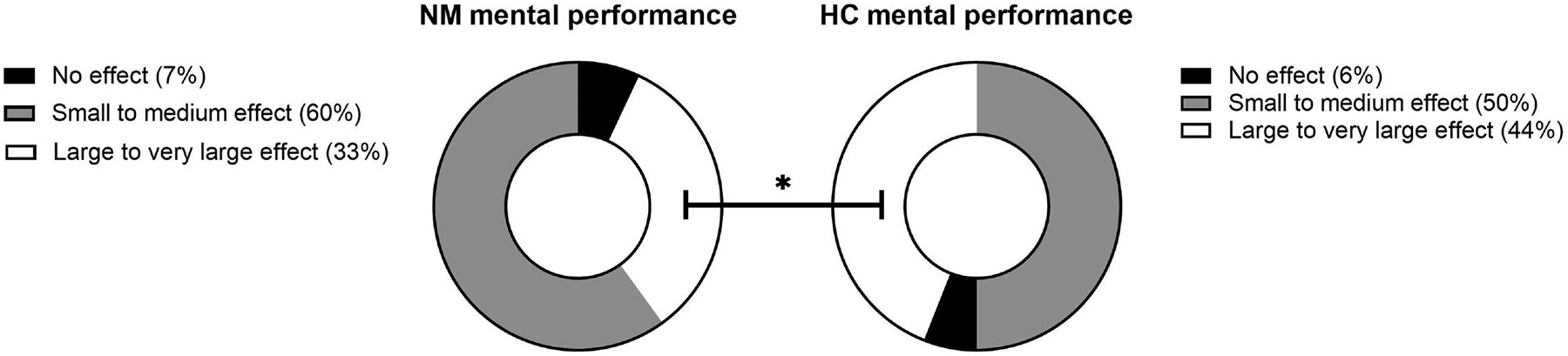
Difference between NM women and HC user in the perceived effect of hormonal cycles on mental performance. *Significant difference between NM and HC (p < .05). NM = naturally menstruating; HC = hormonal contraceptive.
No group differences were observed in any of the other performance characteristics and the combined data are presented in Figure 4.
Figure 4 —
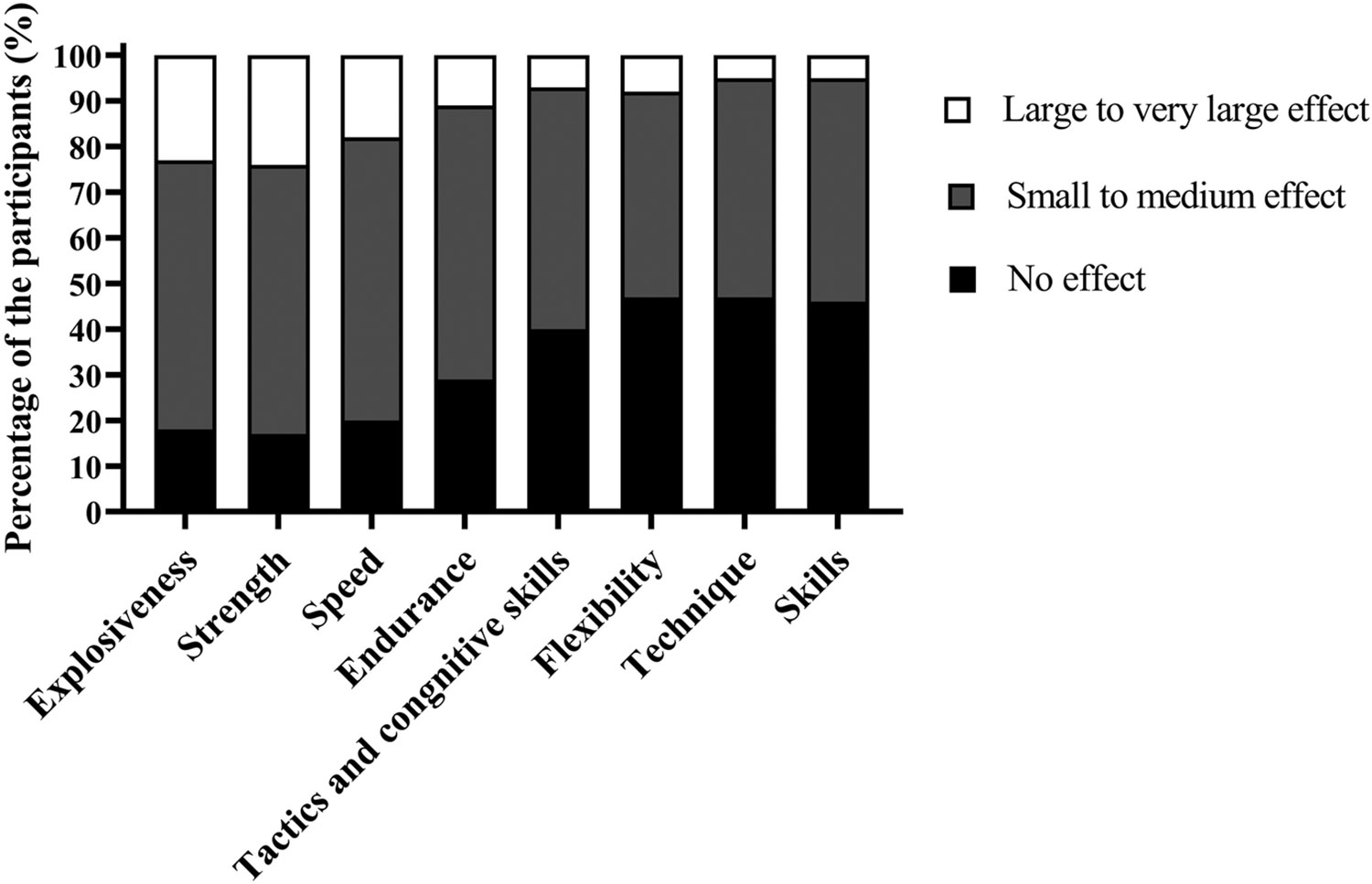
Perceived effects across all phases of the hormonal cycle on characteristics associated with performance.
In addition to mental performance, athletes perceived that their hormonal cycles negatively affected explosiveness, strength, and speed, as 24%, 24%, and 18% of the athletes reported a large to very large effect for this parameter, respectively. Other performance characteristics were negatively affected only a little with athletes reporting small to medium effects or no effect. Skills (47%), technique (47%), mobility (47%), and cognitive performance (40%) were most commonly reported not to be affected by the hormonal cycle (Figure 4).
Hormonal-Cycle-Related Symptoms
MC- and HC cycle-related symptoms in both groups are shown in Figure 5. An average of 10 ± 7 symptoms were reported by all athletes during their MC or HC. The NM group reported more symptoms than the HC group (11 ± 7 vs. 10 ± 7, p = .017). The most reported symptoms included abdominal pain, bloating, and mood swings. Fifty-five athletes (7% of athletes) did not report any symptoms for any phase of their cycle. The total number of symptoms reported differed significantly between phases (p < .001 for all phase comparisons). The highest quantity of symptoms was reported in Phases 1 and 4 (early follicular/inactive pill phase and late luteal/late active pill phase). During Phases 1 and 3, the HC group reported fewer symptoms than the NM group (5 ± 3 vs. 6 ± 3, p < .001 and 1 ± 1 vs. 1 ± 2, p < .05).
Figure 5 —
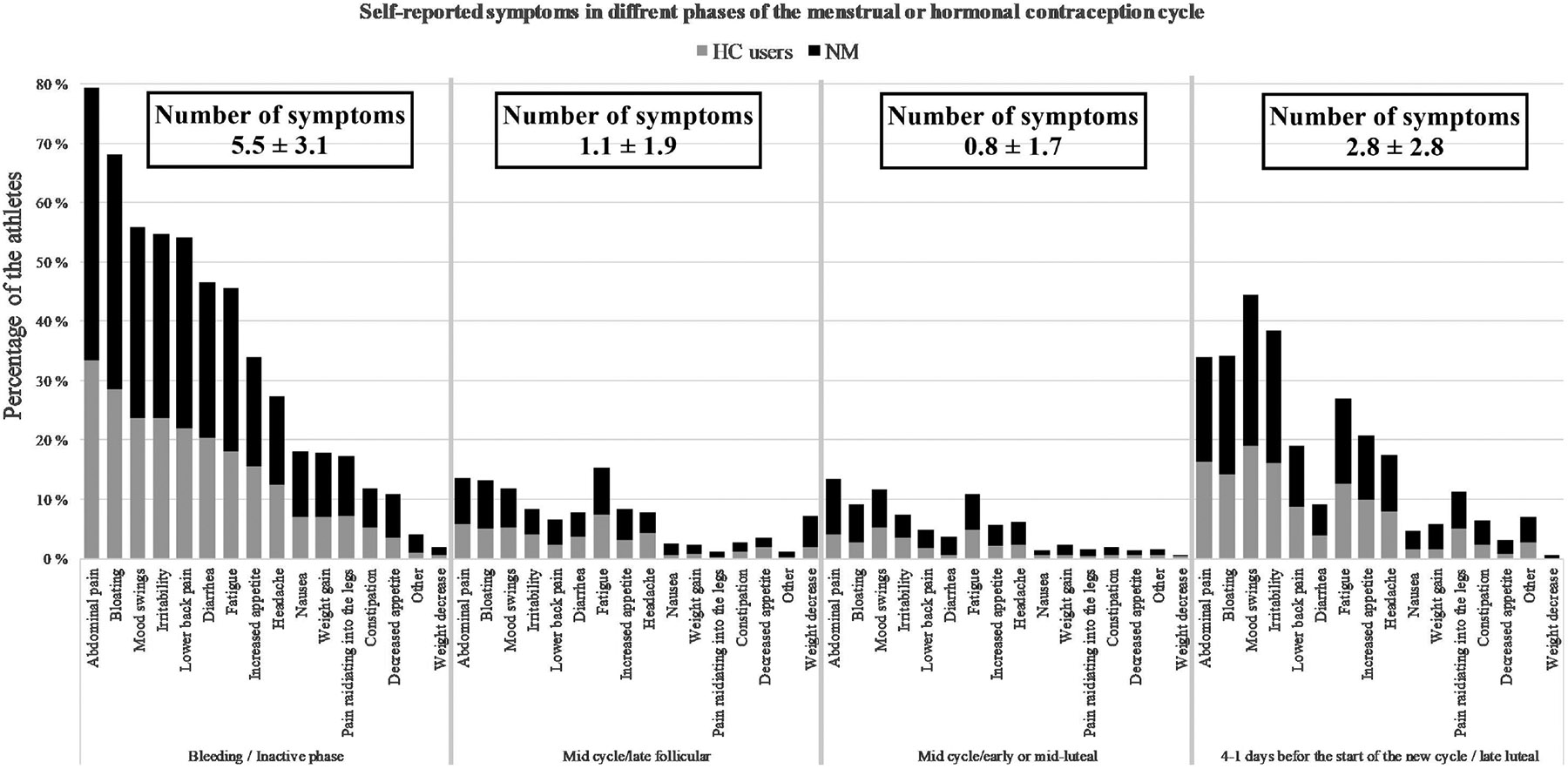
Symptoms reported for different phases of the menstrual cycle or hormonal contraceptive cycle, including the mean total number of symptoms reported by each respondent for each phase (±SD). Phase 1 corresponds with the bleeding/inactive phase, Phase 2 corresponds with midcycle/late follicular, Phase 3 corresponds with midcycle/early or mid-luteal, and Phase 4 corresponds with the end of the cycle/luteal phase (4–1 days before the start of new cycle). NM = naturally menstruating; HC = hormonal contraceptive.
Associations Between the Hormonal-Cycle-Related Symptoms and the Perceived Performance
Logistic regression models including participant characteristics (age, body mass index, training volume, and HC use), number of MC and HC symptoms, and subjective performance are presented in Table 2. In both models, the number of symptoms was significantly associated with subjective performance, unlike age, body mass index, training volume, or HC use. Among the explanatory variables in both models, the regression coefficient for the number of symptoms was statistically significant and the regression coefficients were positive (.138 and .141), the more the athlete reported symptoms during their MC, the more likely their performance was perceived as worst or best in one of the phases of her hormonal cycle.
Table 2.
Models 1 and 2 Have Been Analyzed With Logistic Regression Analysis and Presented in the Form of Odd Ratio (95% Confidence Interval) and R2 (Regression Coefficient)
| Model 1: A decrease in performance was experienced during some phase of the MC or HC |
Model 2: An increase in performance was experienced during some phase of the MC or HC |
|
|---|---|---|
| Age (years) | 0.994 [0.968, 1.020] R2: −.006 |
1.008 [0.984, 1.031] R2: .008 |
| Body mass index (kg/m2) | 1.000 [0.945, 1,057] R2: <.001 |
0.988 [0.937, 1.042] R2: −.12 |
| Yearly training load (hr) | 1.000 [1.000, 1.001] R2: <.001 |
1.000 [0.999, 1.000] R2: <.001 |
| Hormonal contraception | 0.732 [0.500, 1.071] R2: −.312 |
0.726 [0.509, 1.035] R2: −.321 |
| Number of symptoms |
1.148 [1.106, 1.191] R2: .138 |
1.152 [1.113, 1.192] R2: .141 |
| Nagelkerken R2 | .166 | .192 |
| Correctly predicted observations (%) | 75.9 | 71.5 |
Note. Statistically significant results (p < .05) are in bold. MC = menstrual cycle; HC = hormonal contraceptive.
Perceived Effects of MC and HC on Training
A total of 20% in the NM group and 18% in the HC group had modified their training at least twice due to MC- or HC-related symptoms. No differences were observed between the NM and HC groups. Ways in which training was modified are presented in Table 3.
Table 3.
Changes Made to Training Due to Menstrual Cycle Symptoms
| Change made to training | Frequency of response (% of all athletes) |
|---|---|
| Decreased training (intensity/volume) | 72 (9.6) |
| Canceled or rescheduled training sessions | 58 (7.8) |
| Avoided specific training modes and/or selected an unplanned training mode | 21 (2.8) |
| Decreased training volume | 12 (1.6) |
| Rescheduled a high-intensity training session | 7 (0.9) |
| Decreased duration of training session | 4 (0.5) |
| Not completed a training session | 3 (0.4) |
| Periodized training around symptoms | 3 (0.4) |
| Increased stretching/recovery activities | 1 (0.1) |
A total of 14% in the NM and 10% in the HC groups reported that they take their hormonal cycle into consideration when planning training. No differences were observed between the NM and HC groups. A list of the modifications that the athletes had made to their training is shown in Table 3.
Discussion
The aim of this study was to evaluate the perceived impact and magnitude of impact of the MC and the HC cycle on various characteristics of performance in relation to hormonal cycle-associated symptoms in female athletes. The NM and HC groups reported similar experiences in terms of perceived performance changes during their respective hormonal cycles. Performance was perceived to be the worst during the early follicular phase for the NM group and in the inactive phase for the HC group (i.e., during menstrual/withdrawal bleeding) while performance was perceived to be best in the early- or mid-luteal phase/late active phase for the NM and HC groups, respectively. The NM group was more likely to report differences in performance between the phases of their cycle than the HC group. Perceived mental performance was the parameter most strongly influenced by hormonal cycles, with HC users reporting a greater negative effect than the NM group. A total of 93% of athletes reported at least one hormonal-cycle-related symptom, with the most common symptoms being: abdominal pain, bloating, mood swings, and irritability. A greater number of hormonal-cycle-related symptoms experienced were associated with a perceived decline in performance thereby emphasizing the importance of an individual approach to symptom assessments on performance.
Most athletes in this study reported that their performance varied between the different phases of the hormonal cycles. Meanwhile, almost all athletes (93%) reported symptoms related to their hormonal cycle, which is consistent with previous studies in athletes (Ekenros et al., 2022; Solli et al., 2020). The total number of reported symptoms related to hormonal cycles was slightly higher in the NM group than in the HC group while previous studies have reported that there is no difference in the number of symptoms between HC users and nonusers (Engseth et al., 2022; Oxfeldt et al., 2020; Solli et al., 2020). In the present study, the difference in the number of symptoms between NM and HC reached statistical significance even if the difference between the number of symptoms reported by the NM and HC groups was relatively small. Nevertheless, hormonal-cycle-related symptoms should not be overlooked in HC users.
In the present study, most symptoms were reported at the beginning of the follicular phase for the NM group and in the inactive phase for the HC group (i.e., during menstrual/withdrawal bleeding) and at the end of the luteal phase for the NM group or just before the end of the active phase for the HC group, in line with previous studies (Brown et al., 2021; Findlay et al., 2020; Martin et al., 2018; Solli et al., 2020). The NM group reported a higher number of hormonal-cycle-related symptoms than the HC group at the beginning of the hormonal cycle and in the early- or mid-luteal phase/mid-active phase. Interestingly, there was no difference in the reported symptoms 4–1 days prior to the start of a new MC (late luteal phase) or inactive phase.
The most commonly reported symptoms during the MC were abdominal pain and bloating. Among the athletes, the HC group reported only slightly fewer symptoms than the NM group, which may indicate that the use of HC does not eliminate all hormonal-cycle-related symptoms even though HC is often prescribed to reduce MC-related symptoms (Wong et al., 2009). While the main reason given for using HC in the present study was to prevent pregnancy (86%) more than 40% of the athletes reported that they used HC to reduce bleeding and to relieve menstrual pain. Similarly, Engseth et al. (2022) reported that many athletes use HC to mitigate negative menstrual-related symptoms that interfere with training and competitions (Engseth et al., 2022). Nevertheless, it is important to understand that HC use does not “eliminate” or “even out” symptoms in all users and that those with severe symptoms prior to HC use may only have mitigated symptoms (Ekenros et al., 2022).
We observed that hormonal cycle affected mental performance more in the HC group compared with the NM group. This finding is in line with previous research reporting that various mental symptoms, such as negative mood and anxiety, can lower an athlete’s motivation and energy levels and thus impair their performance (Brown et al., 2021; Findlay et al., 2020). In addition to mental performance, athletes reported that their hormonal cycles negatively influenced explosiveness and strength while, for instance, skill, flexibility, technique, and tactics/cognitive abilities remained largely unaffected or the perceived effect was only small to moderate. Meta-analyses of experimental studies investigating the effects of different phases of the MC and HC on performance (strength, aerobic, and anaerobic performance) have concluded that the influence of MC or HC on performance at the group level is only “trivial” (Elliott-Sale et al. 2020; McNulty et al. 2020). Nevertheless, it is essential to understand that this research represents group-level analyses and that individual athletes may experience challenging, if not debilitating, symptoms that are associated with their hormonal cycles.
In the present study, athletes reported that hormonal-cycle-related symptoms were experienced the most in phases of the MC and HC for which performance was also perceived to be the worst. The more symptoms athletes reported, the more likely they were to report performance being the worst possible in one of the phases of the MC. On the other hand, when fewer symptoms were reported, it was more likely that the athlete had not reported a difference in performance between phases of the MC or HC. This finding is in line with the study by McNulty et al. (2023) who showed that the magnitude of symptoms during bleeding was associated with a perceived reduction in exercise performance in recreationally active women. Similarly, negative symptoms related to the first phase of the MC such as abdominal pain and menstrual flow itself are reported to be associated with a negative perceived effect on performance (Bruinvels et al., 2021; Constantini et al., 2005; Findlay et al., 2020; Solli et al., 2020). Overall, there is only limited high-quality research on the associations between female sex hormone fluctuation during hormone cycles and performance that relates only to athletes or elite athletes (Castanier et al., 2021). Our study, in line with Ekenros et al. (2022), suggests that the indirect effects of hormonal-cycle-related symptoms should be considered in studies that aim to evaluate the effect of hormonal cycles on athletic performance.
Most athletes in the present study did not consider it necessary to change their training due to hormonal-cycle-related symptoms. However, almost 20% of the athletes had changed their training more than once due to their hormonal cycle. This is consistent with the previous research in which 22% of endurance athletes (Solli et al., 2020) and 13% of elite athletes in power, endurance, and technical sports (Oxfeldt et al., 2020) reported that they had changed their training due to hormonal-cycle-related symptoms. In the present study, athletes who reported changing their training due to hormonal-cycle-related symptoms indicated that they generally decreased their training volume and/or intensity. In the extensive study by Bruinvels et al. (2021) (~6,800 participants), a higher menstrual symptom index led to changes in training more often than changes or cancellations of competitions (Bruinvels et al., 2021). To better understand this phenomenon, the reasons for athletes and coaches changing training may require more investigation.
Strengths and Limitations
The results of the present study provide important information regarding female athletes’ hormonal-cycle-related symptoms and their perceived impact on performance. However, there are some limitations that should be considered. First, the study was a cross-sectional study conducted as an online survey; therefore, no assumptions about causality can be made. Second, due to self-report and subjective nature of the survey, it is not possible to draw conclusions about the actual sex hormone fluctuations that occur during the MC or HC and, for example, popular and social media may influence athletes’ responses because these media contain opinions and information about hormonal cycles affecting performance that may or may not be accurate. Third, the HC group included athletes taking a variety of HCs, including both combined HCs and progestin-only HCs. These HCs result in different hormonal profiles and hormonal fluctuations that may influence results. Regrettably, in the present study, the questionnaire did not include questions or scales to clarify the severity of the symptoms, which should also be considered when assessing their effects on perceived performance. It should be noted that overall, the results of the logistic regression analyses indicated that the effect of symptoms on performance during the MC or HC can be predicted to some degree; however, the explanatory power of the models remained relatively small in both models, which suggests that the respective models cannot predict the variation of the variables accurately. This highlights the importance of an individualized approach when working with female athletes. In future research, it would be important to develop a validated tool to identify female athletes who have symptoms and believe that their athletic performance, wellbeing, or ability to train and compete is affected by their hormonal cycle.
Conclusions
In the present study, the NM group and the HC group reported similar experiences in terms of performance changes during their respective hormonal cycles, where symptoms were associated with a perceived decline in performance. These findings emphasize the need for symptom assessment when examining the effects of hormonal cycles on performance. As mental performance appeared to be most affected by hormonal cycles, it may be worthwhile to increase educational awareness regarding MC- and HC-related symptoms and explore possible interventions and methods to target hormonal-cycle-related symptoms and mental performance. Finally, it is important to remember that every athlete is unique and that there are athletes who do not experience hormonal-cycle-related symptoms or significant negative changes in their perceived performance. In addition, it should be recognized that while HCs may mitigate MC symptoms, changes in both exogenous and endogenous hormones that may be associated with symptoms can still occur and may still be perceived as negative/positive for performance.
Key Points.
The most commonly used hormonal contraceptive (HC) method was combined oral contraceptives (42% of the HC group), followed by hormonal intrauterine device (24% of the HC group), and progestin-only oral contraceptives (14% of the HC group).
Hormonal cycle symptoms were associated with a perceived reduction in performance; symptom assessment is important when investigating the impact of hormonal cycles on performance.
The naturally menstruating and HC groups reported similar experiences in terms of perceived performance changes during their respective hormonal cycles. Both groups reported mental performance to be negatively affected most by their hormonal cycles.
Acknowledgments
The authors want to thank all of the athletes who participated in this study. Furthermore, the authors want to express their gratitude to the Finnish Olympic Committee and all of the National Sports Federations and Sports Academies for promoting this study to their athletes. This study was conducted with the European Regional Development Fund #A74999 and Urheiluopistosäätiö, Grant Number 20190110 (Ihalainen).
References
- Apter D, Gemzell-Danielsson K, Hauck B, Rosen K, & Zurth C (2014). Pharmacokinetics of two low-dose levonorgestrel-releasing intrauterine systems and effects on ovulation rate and cervical function: Pooled analyses of phase II and III studies. Fertility and Sterility, 101(6), 1656–1662.e4. 10.1016/j.fertnstert.2014.03.004 [DOI] [PubMed] [Google Scholar]
- Armour M, Parry KA, Steel K, & Smith CA (2020). Australian female athlete perceptions of the challenges associated with training and competing when menstrual symptoms are present. International Journal of Sports Science & Coaching, 15(3), 316–323. 10.1177/1747954120916073 [DOI] [Google Scholar]
- Brown N, Knight CJ, & Forrest LJ (2021). Elite female athletes’ experiences and perceptions of the menstrual cycle on training and sport performance. Scandinavian Journal of Medicine & Science in Sports, 31(1), 52–69. 10.1111/SMS.13818 [DOI] [PubMed] [Google Scholar]
- Bruinvels G, Blagrove RC, Goldsmith E, Shaw L, Martin D, & Piasecki J (2022). How lifestyle changes during the COVID-19 global pandemic affected the pattern and symptoms of the menstrual cycle. International Journal of Environmental Research and Public Health, 19(20), Article 13622. 10.3390/IJERPH192013622/S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruinvels G, Burden RJ, Cushway T, Brown N, Pedlar C, & Richards T (2017). The impact of heavy menstrual bleeding (menorrhagia) and iron status in exercising females. British Journal of Sports Medicine, 51(4), Article 304. 10.1136/bjsports-2016-097372.53 [DOI] [Google Scholar]
- Bruinvels G, Goldsmith E, Blagrove R, Simpkin A, Lewis N, Morton K, Suppiah A, Rogers JP, Ackerman KE, Newell J, & Pedlar C (2021). Prevalence and frequency of menstrual cycle symptoms are associated with availability to train and compete: A study of 6812 exercising women recruited using the Strava exercise app. British Journal of Sports Medicine, 55(8), 438–443. 10.1136/BJSPORTS-2020-102792 [DOI] [PubMed] [Google Scholar]
- Carmichael MA, Thomson RL, Moran LJ, & Wycherley TP (2021). The impact of menstrual cycle phase on athletes’ performance: A narrative review. International Journal of Environmental Research and Public Health, 18(4), Article 1667. 10.3390/ijerph18041667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castanier C, Bougault V, Teulier C, Jaffré C, Schiano-Lomoriello S, Vibarel-Rebot N, Villemain A, Rieth N, Le-Scanff C, Buisson C, & Collomp K (2021). The Specificities of elite female athletes: A multidisciplinary approach. Life, 11(7), Article 622. 10.3390/LIFE11070622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrisler JC (2013). Teaching taboo topics: Menstruation, menopause, and the psychology of women. Psychology of Women Quarterly, 37(1), 128–132. 10.1177/0361684312471326 [DOI] [Google Scholar]
- Constantini NW, Dubnov G, & Lebrun CM (2005). The menstrual cycle and sport performance. Clinics in Sports Medicine, 24(2), e51–e82. 10.1016/J.CSM.2005.01.003 [DOI] [PubMed] [Google Scholar]
- De Leo V, Musacchio MC, Cappelli V, Piomboni P, & Morgante G (2016). Hormonal contraceptives: Pharmacology tailored to women’s health. Human Reproduction Update, 22(5), 634–646. 10.1093/HUMUPD/DMW016 [DOI] [PubMed] [Google Scholar]
- D’Souza AC, Wageh M, Williams JS, Colenso-Semple LM, McCarthy DG, Mckay AKA, Elliott-Sale KJ, Burke LM, Parise G, MacDonald MJ, Tarnopolsky MA, & Phillips SM (2023). Menstrual cycle hormones and oral contraceptives: A multi-method systems physiology-based review of their impact on key aspects of female physiology. Journal of Applied Physiology, 135(6), 1284–1299. 10.1152/JAPPLPHYSIOL.00346.2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekenros L, von Rosen P, Solli GS, Sandbakk Ø, Holmberg HC, Hirschberg AL, & Fridén C (2022). Perceived impact of the menstrual cycle and hormonal contraceptives on physical exercise and performance in 1,086 athletes from 57 sports. Frontiers in Physiology, 13, Article 954760. 10.3389/FPHYS.2022.954760/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott-Sale KJ, McNulty KL, Ansdell P, Goodall S, Hicks KM, Thomas K, Swinton PA, & Dolan E (2020). The effects of oral contraceptives on exercise performance in women: A systematic review and meta-analysis. Sports Medicine, 50(10), 1785–1812. 10.1007/s40279-020-01317-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott-Sale KJ, Minahan CL, de Jonge XAKJ, Ackerman KE, Sipilä S, Constantini NW, Lebrun CM, & Hackney AC (2021). Methodological considerations for studies in sport and exercise science with women as participants: A working guide for standards of practice for research on women. Sports Medicine, 51(5), 843–861. https://pubmed.ncbi.nlm.nih.gov/33725341/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott-Sale KJ, Ross E, Burden R, & Hicks K (2020). The BASES expert statement on conducting and implementing female athlete-based research. The Sport and Exercise Scientist, 65, 6–7. [Google Scholar]
- Engseth TP, Andersson EP, Solli GS, Morseth B, Thomassen TO, Noordhof DA, Sandbakk Ø, & Welde B (2022). Prevalence and self-perceived experiences with the use of hormonal contraceptives among competitive female cross-country skiers and biathletes in Norway: The FENDURA project. Frontiers in Sports and Active Living, 4, Article 873222. 10.3389/FSPOR.2022.873222/PDF [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findlay RJ, MacRae EHR, Whyte IY, Easton C, & Forrest LJ (2020). How the menstrual cycle and menstruation affect sporting performance: Experiences and perceptions of elite female rugby players. British Journal of Sports Medicine, 54(18), 1108–1113. 10.1136/BJSPORTS-2019-101486 [DOI] [PubMed] [Google Scholar]
- Hair JF, Anderson RE, Tatham RL, & Black WC (1998). Multi-variate data analysis (5th ed.). Prentice Hall. [Google Scholar]
- Koltun KJ, Williams NI, & De Souza MJ (2020). Female athlete triad coalition cumulative risk assessment tool: Proposed alternative scoring strategies. Applied Physiology Nutrition and Metabolism, 45(12), 1324–1331. 10.1139/APNM-2020-0131 [DOI] [Google Scholar]
- Martin D, Sale C, Cooper SB, & Elliott-Sale KJ (2018). Period prevalence and perceived side effects of hormonal contraceptive use and the menstrual cycle in elite athletes. International Journal of Sports Physiology and Performance, 13(7), 926–932. 10.1123/ijspp.2017-0330 [DOI] [PubMed] [Google Scholar]
- McNulty KL, Ansdell P, Goodall S, Thomas K, Elliott-Sale KJ, Howatson G, & Hicks KM (2023). The symptoms experienced by naturally menstruating women and oral contraceptive pill users and their perceived effects on exercise performance and recovery time post-training. Women in Sport and Physical Activity Journal, 1, Article 16. 10.1123/WSPAJ.2023-0016 [DOI] [Google Scholar]
- McNulty KL, Elliott-Sale KJ, Dolan E, Swinton PA, Ansdell P, Goodall S, Thomas K, & Hicks KM (2020). The effects of menstrual cycle phase on exercise performance in eumenorrheic women: A systematic review and meta-analysis. Sports Medicine, 50(10), 1813–1827. 10.1007/s40279-020-01319-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosthuyse T, & Bosch AN (2010). The effect of the menstrual cycle on exercise metabolism. Sports Medicine, 40(3), 207–227. [DOI] [PubMed] [Google Scholar]
- Oxfeldt M, Dalgaard LB, Jørgensen AA, & Hansen M (2020). Hormonal contraceptive use, menstrual dysfunctions, and self-reported side effects in elite athletes in Denmark. International Journal of Sports Physiology and Performance, 15(10), 1377–1384. 10.1123/IJSPP.2019-0636 [DOI] [PubMed] [Google Scholar]
- Paludo AC, Paravlic A, Dvořáková K, & Gimunová M (2022). The effect of menstrual cycle on perceptual responses in athletes: A systematic review with meta-analysis. Frontiers in Psychology, 13, Article 926854. 10.3389/FPSYG.2022.926854/BIBTEX [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravi S, Ihalainen JK, Taipale-Mikkonen RS, Kujala UM, Waller B, Mierlahti L, Lehto J, & Valtonen M (2021). Self-reported restrictive eating, eating disorders, menstrual dysfunction, and injuries in athletes competing at different levels and sports. Nutrients, 13(9), Article 3275. 10.3390/NU13093275/S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solli GS, Sandbakk SB, Noordhof DA, Ihalainen JK, & Sandbakk Ø (2020). Changes in self-reported physical fitness, performance, and side effects across the phases of the menstrual cycle among competitive endurance athletes. International Journal of Sports Physiology and Performance, 15(9), 1324–1333. 10.1123/ijspp.2019-0616 [DOI] [PubMed] [Google Scholar]
- Torstveit MK, & Sundgot-Borgen J (2005). Participation in leanness sports but not training volume is associated with menstrual dysfunction: A national survey of 1276 elite athletes and controls. British Journal of Sports Medicine, 39(3), 141–147. 10.1136/bjsm.2003.011338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong CL, Farquhar C, Roberts H, & Proctor M (2009). Oral contraceptive pill for primary dysmenorrhoea. Cochrane Database of Systematic Reviews, 4, Article 120. 10.1002/14651858.CD002120.PUB3/INFORMATION/EN [DOI] [Google Scholar]


