Summary
Background
Drug use disorder (DUD) poses a major public health crisis globally, necessitating immediate attention to global trends and future projections to develop effective health policies and interventions. Thus, we aimed to estimate the global trends in DUD mortality rates from 1990 to 2021 and future projections of DUD deaths until 2040 across 73 countries.
Methods
In this time-series analysis and modelling study, we investigated the global trends in DUD mortality rates from 1990 to 2021 using the WHO Mortality Database and forecasted future trends through 2040. Global trend analysis was analysed using a locally weighted scatter plot smoother (LOESS) curve, and future projections were calculated based on a Bayesian age-period-cohort analysis. In addition, we performed a decomposition analysis to identify the variations in DUD deaths, specifically examining factors such as population growth, ageing, and epidemiological changes.
Findings
Of the 73 countries included in the analysis of DUD mortality, 45 were high-income countries (HICs), and 28 were low to middle-income countries (LMICs). The LOESS estimates of the global DUD mortality rate were 1.84 deaths per 1,000,000 people (95% CI, −0.44 to 4.12) in 1990 and 13.09 deaths per 1,000,000 people (95% CI, 10.74–15.43) in 2021. Notably, HICs showed a significant increase in DUD mortality from 1.43 deaths per 1,000,000 people (95% CI, −1.55 to 4.42) in 1990 to 17.19 deaths per 1,000,000 people (95% CI, 13.84–20.53) in 2021. A significant increase in DUD mortality was observed among individuals aged 25–64 and males. Our analysis also identified associations between DUD mortality rates and several log-transformed parameters, including Human Development Index (β, 14.92; p < 0.0001), Socio-demographic Index (β, 11.80; p < 0.0001), reverse Gender Gap Index (β, −12.02; p < 0.0001), and Gini coefficient (β, −1.84; p < 0.0001). From 1990 to 2021, the increase in the number of DUD deaths globally can be attributed to two prominent factors: epidemiological change and population growth. In HICs, the impacts of epidemiological changes for increasing DUD mortality rates were particularly prominent compared to other factors. In the Bayesian age-period-cohort models, the predicted number of global DUD deaths up to 2040 were estimated to increase from 25.95 deaths per 1,000,000 people (95% credible interval [CrI], 24.72–27.28) in 2021 to 38.45 (95% CrI, 30.48–49.33) in 2030, and 42.43 (95% CrI, 23.67–77.77) in 2040.
Interpretation
An increasing trend in global DUD mortality was observed from 1990 to 2021, especially in HICs. Future DUD deaths were also predicted to increase until 2040 at the global level. Therefore, these findings suggest urgent and proactive strategies for DUD to reduce the mortality rates related to DUD are needed. However, further prospective research that accounts for potential confounding factors, such as socioeconomic variables and the quality of reporting data from individual countries, is imperative for more accurate estimation.
Funding
National Research Foundation and Ministry of Science and ICT of South Korea.
Keywords: Drug use, Mortality, Global trend, Prediction model
Research in context.
Evidence before this study
On May 20, 2024, we searched PubMed for studies reporting on the global trends or future projections of drug use disorder (DUD) mortality using the following terms “drug use disorder [MeSH Terms]”, “mortality/trends [MeSH Terms]”, “trends [MeSH Terms]” AND “drug use disorder [MeSH Terms]”, and “Forecasting [MeSH Terms] OR future projections [MeSH Terms]”. We then systematically collected and reviewed papers related to the global trends or future projections of DUD mortality. The existing research on DUD mortality rates and long-term trends on a global scale, drawing from official national statistics, remains limited. Also, there is a lack of future projections of DUD mortality until 2040 and on a large-scale global level. Although previous studies utilising the Global Burden of Disease Study (GBD) 2016 have documented a 44.2% increase in global alcohol use disorders and 27.3% opioid use disorders from 1990 to 2016, these studies primarily relied on meta-analytical methods characteristic of GBD data. In contrast, the World Health Organization (WHO) mortality database provides original reported data, offering a different methodological perspective. Our study seeks to supplement and extend the findings of previous GBD studies, aiming to provide a novel perspective on global suicide mortality rates alongside future projections.
Added value of this study
We aimed to estimate the global trends in DUD mortality rates from 1990 to 2021 and the future projection of DUD deaths until 2040 across 73 countries. The estimated global DUD mortality rate increased from 1.84 (95% CI, −0.44 to 4.12) deaths per 100,000 people in 1990 to 13.09 (10.74–15.43) deaths per 100,000 people in 2021 across 73 countries. High-income countries (HIC) showed a significant increase in DUD mortality from 1990 to 2021, particularly among middle-aged adults aged 25–64 and males. The future predicted number of global DUD deaths up to 2040 would increase from 25.95 (95% credible interval [CrI], 24.72–27.28) deaths in 2021 to 38.45 (95% CrI, 30.48–49.33) in 2030, and 42.43 (95% CrI, 23.67–77.77) in 2040.
Implications of all the available evidence
An increasing trend in global DUD mortality rates were observed from 1990 to 2021. The increase was particularly pronounced in HICs and among middle-aged adults, indicating that current interventions may be inadequate to contain the growing crisis. Therefore, findings suggest the need for more effective strategies and policies will be required to achieve a further reduction in global DUD mortality.
Introduction
Drug use disorders (DUD) pose a significant challenge to public health, necessitating immediate attention to their global trends and future projections to develop effective health policies and interventions.1 The aftermath of the COVID-19 pandemic has seen a surge in the prevalence of substance use disorders, particularly in North America, where an opioid crisis significantly impacted the United States and Canada.2 In 2019, the rates of opioid-related mortality were 15.8 and 6.4 per 100,000 individuals in the United States and Canada, respectively, highlighting the severity of this substance use crisis.3 In addition, the pandemic period accompanied a reduction in hospital admissions, coinciding with a surge in drug overdose fatalities.4 This reduction in hospital accessibility during the pandemic may have inadvertently contributed to the increase in mortality rates of DUD; such recent shifts are likely to influence international trends in DUD, suggesting the need for understanding global and longitudinal trends in DUD mortality.
DUD covers a wide spectrum of drug use, from illicit drugs such as heroin, morphine, opium, cannabis, amphetamines, and cocaine to the non-medical use of prescription drugs, notably pharmaceutical opioids. Drug dependence, a core aspect of DUD, is characterised by the compelling desire for the substance, impaired control over its use, withdrawal syndromes, tolerance, and significant time devoted to drug-related activities. These criteria are outlined by the International Classification of Diseases (ICD) 10th edition and DSM-IV.5
Furthermore, the consumption of substances such as alcohol and psychoactive stimulants is associated with heightened risks of various health complications, including fractures, cognitive impairments, cardiovascular diseases, and delirium, each contributing to the overall morbidity and mortality associated with DUD.6,7 Therefore, this study utilised the World Health Organization (WHO) Mortality Database to provide insights into the global trends in DUD mortality rates. It also aimed to estimate the future burden of DUD up to 2040 across 73 countries.
Methods
Study design
We investigated the global trends in the DUD mortality rate from 1990 to 2021 by utilising the WHO Mortality Database and forecasted future trends through 2040.8 For our study following GATHER and SAGER guidelines, we had four primary objectives: (1) including 73 countries to determine global trends over the years; (2) examining the association between DUD mortality and socioeconomic indicators; (3) conducting decomposition analysis to understand the factors attributed to changes in the DUD mortality trend; and (4) using mathematical modelling to predict trends up to the year 2040.9 This study used de-identified secondary data from the WHO Mortality Database, which collects and aggregates mortality data from member states based on civil registration systems. As the data are anonymised and publicly available, no informed consent from participants was required. The study protocol was approved by the Institutional Review Board of Kyung Hee University (KHSIRB-23-085).
Data sources and processing
The primary data source was the WHO Mortality Database, which annually aggregates mortality data by age, sex, and cause of death, reported by WHO member states through their civil registration systems.8 We extracted the number of DUD deaths across all available countries, sexes, and age groups from 1990 to 2021. The inclusion criteria required a minimum of 8 years of complete data within the observation timeframe; a total of 73 countries were included for the analysis (Supplementary Tables S1 and S2), while 36 countries that did not meet this criterion were excluded (Supplementary Table S3). Each country provided the WHO with data that were not adjusted for any incompleteness; the mortality values are reported as absolute numbers, including zero.8 We did not apply any imputation method for years not reported by some countries.10 The causes of death were categorised according to the ICD code. We identified DUD-related deaths using ICD-9 code (304) and ICD-10 codes (F11-16, F18-19, X42, and T40; Supplementary Table S4). All population data for each country were derived from the United Nations dataset to calculate the mortality rates.
To comprehensively investigate the global mortality rates associated with DUD based on economic conditions or geography across countries, our study stratified countries according to the following variables: income (high-income countries [HICs] and low and middle-income countries [LMICs]), Human Development Index (HDI; very high HDI, high HDI, and medium HDI), and geographical areas (Africa, Asia Pacific, Europe, Latin America and the Caribbean, and Northern America). Income was categorised based on economic status for each country, with the threshold set at $13,846 of the World Bank's Gross National Income per capita criteria (Supplementary Table S5).11 The HDI, developed by the United Nations, measures human development through factors such as health, knowledge, and living standards, with values ranging from 0 to 1.12 We classified countries based on their HDI values, defining very high HDI as 0.9 or above, high HDI as 0.89–0.8, and medium HDI as below 0.8 (Supplementary Table S6). Geographical areas were categorised based on region, as presented in Supplementary Table S7. This stratification enables us to discern distinctive characteristics among nations based on their economic or development profiles and regional affiliations.
Global trends analysis via locally estimated scatter plot smoother curve
Age-standardised DUD mortality rates were calculated to adjust for differences in population distributions across countries and over time (Supplementary Methods). Using the WHO World Standard Population, these rates were analysed for specific age groups, including under 25 years, from 25 to 64 years in 10-year intervals, and 65 years and above.8,13,14
For trend analysis, we employed a locally estimated scatter plot smoother (LOESS) curve, to generate a smoothed curve of global trends in DUD mortality over time for 73 countries (Supplementary Table S1 and Supplementary Methods).8 The LOESS curve serves as a smoothing technique that links data points while accounting for its variations, thus enabling the detection of the comprehensive trend within the data.15 The LOESS model is controlled by two main parameters, smoothing parameter (α) and polynomial degree parameter (λ). The α determines the range of local data points to be used, while the λ parameter specifies the degree of the polynomial for local regression based on the data points selected by α. The α was determined through the default optimisation procedure in the software (Supplementary Table S8 and Supplementary Methods), and λ was set to 1.8 The data were represented as mortality rates per 1,000,000 people and 95% confidence intervals (CI), with statistical significance established at two-sided p < 0.05.16, 17, 18 The CI for the predictions from the LOESS model was calculated by using the standard error for each predicted value, multiplying it by the t-value to obtain the upper and lower limits at a default level of 95%.19 Fitting of LOESS curve and visualisation were conducted by using SAS (version 9.4; SAS Inc., Cary, NC, USA) and Python software (version 3.11.4; Python Software Foundation, Wilmington, DE, USA), respectively.20
Association analysis of socio-economic indicators of DUD mortality
Four indices were utilised to analyse the association between DUD mortality and various socioeconomic indicators, including HDI, Socio-demographic Index (SDI), Gender Gap Index (GGI), and Gini coefficient (Supplementary Methods). The SDI from the Global Burden of Disease (GBD) study reflects developmental status with components such as income, education, and birth rates.21,22 The reverse GGI is a metric derived from the GGI, which the World Economic Forum developed. To make its interpretation more intuitive, the value was transformed by implementing the formula 1-GGI. The GGI quantifies gender inequality across economic participation, opportunities, education, health, and survival.23 The Gini coefficient, provided by the World Bank, assesses income inequality within an economy.24,25 HDI, SDI, and reverse GGI scale from 0 to 1, where values closer to 1 indicate high development or gender disparity.12,23,26 In contrast, the Gini coefficient ranges from 0 to 100, with higher values indicating significant income inequality.27
Scatter plots of log-transformed average DUD mortality rates against log-transformed indices from each institution were generated, with linear regression applied to evaluate associations. The results of the analysis, calculated through Python software, are presented as β coefficients and p-values.
Decomposition analysis in DUD mortality
Decomposition analysis was performed to investigate the impact of three factors, including population growth, population ageing, and epidemiological change, on the trends of DUD mortality rates from 1990 to 2021.28,29 Epidemiological change indicates the changes in DUD mortality rates after adjusting for age-specific and population size. The analysis, developed by Das Gupta, was conducted by using population data, age structure information, and the number of DUD mortality. To explore the sophisticated impact according to income level, we executed an analysis based on the classification between HICs and LMICs. The contributions of assessed factors are demonstrated as either increases or decreases in overall mortality deaths, represented by positive and negative values. More detailed explanations are provided in the Supplementary Methods.
Bayesian age-period-cohort statistical modelling
We utilised Bayesian age-period-cohort (BAPC) models to estimate DUD mortality rates from 2022 to 2040 in 73 countries (Supplementary Methods).30 These models operate on the assumption that the logit-transformed mortality risk for a particular age group and time period is a linear function of age, period, and cohort effects.31 This framework enables a comprehensive analysis of mortality rate changes over time, with each effect representing a distinct process: age effects reflect changes that occur over the life course of individuals; period effects capture changes driven by events or conditions in specific years, impacting all age groups equally; and cohort effects account for differences among individuals born in different periods, as older cohorts are replaced by younger ones with distinct characteristics. The BAPC model predicts mortality rates by incorporating age, period, and cohort effects, applying a logit transformation to compute the log-odds of mortality rates. Moreover, the model supports the investigation of various combinations of modelling by accommodating different effects of age, period, and cohort, through constant or linear time trends (random walk of the first or second order; Supplementary Methods).31,32 To determine the optimal parameters for each effect, we assessed the model prediction accuracy from 2011 to 2021, with 1990–2010 data. The root mean square errors (RMSE) were used as the evaluation metric.9 In addition, we employed the BAPC model on sex (male and female), HDI (very high HDI, high HDI, and medium HDI), and age group (<25, 25–34, 35–44, 45–54, 55–64, and ≥65 years) to account for heterogeneity. The model presented prediction results as age-standardised estimates and 95% credible intervals (CrI; Supplementary Methods). Statistical modelling with BAPC was performed using the ‘bamp’ package in R software (version 4.1.2; R Foundation, Vienna, Austria).30
Other analysis
To address potential data variability and capture comprehensive trends, two additional analyses were conducted. First, the socio-demographic index (SDI) was used as a weighting factor to address variability in data quality and reporting across countries, enabling the construction of a weighted LOESS curve. Second, an analysis comparing the before and during COVID-19 periods was performed to examine changes in the global trend related to the pandemic.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to the data in the study, and DKY had the final responsibility for the decision to submit for publication.
Results
Age-standardised DUD mortality rates were available for 73 countries from the WHO Mortality Database from 1990 to 2021 (Table 1 and Supplementary Table S9). The LOESS smoothed rate for DUD mortality was 1.84 deaths per 1,000,000 people (95% CI, −0.44 to 4.12) in 1990 and 13.09 deaths per 1,000,000 people (95% CI, 10.74–15.43) in 2021 (Fig. 1). Of the 73 countries, 45/73 (61.6%) HICs and 28/73 (38.4%) LMICs were included in the analysis (Supplementary Table S5). There was a significant 14.4 times increase in DUD mortality in HIC from 1.43 deaths per 1,000,000 people (95% CI, −1.55 to 4.42) in 1990 to 17.19 deaths per 1,000,000 people (95% CI, 13.84–20.53) in 2021 (Fig. 1). Both male and female in HIC show considerable changes in DUD mortality from 1990 to 2021, particularly the males in the HIC group have a significant upward trend in DUD mortality from 1990 to 2021 (Supplementary Figures S1 and S2 and Supplementary Tables S10 and S11).
Table 1.
LOESS smoothed DUD mortality rate (per 1,000,000 people) across variables in 73 countries, 1990–2021.
 |
Abbreviations: DUD, drug use disorder; CI, confidence interval; HICs, high-income country; LMICs, low- and middle-income country; LOESS, locally weighted scatterplot smoother.
Fig. 1.
Age-standardised DUD mortality rate (per 1,000,000 people) for the global, HICs, and LMICs population among 73 countries for the years 1990–2021.
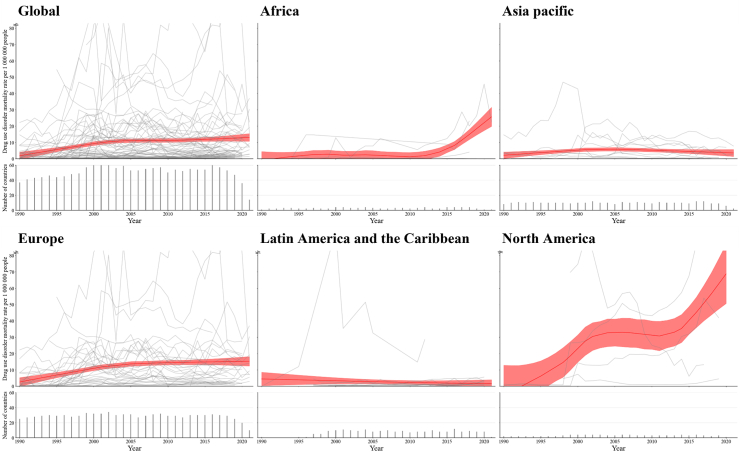
Considerable variations are evident between different geographical areas. Fig. 2 shows age-standardised LOESS smoothed curves of DUD mortality rates across the five continents among 73 countries from 1990 to 2021. The age-standardised of DUD mortality rates showed an upward trend in all continents except Latin America and Caribbean (Africa: −0.93 [−6.28 to 4.42] deaths per 1,000,000 people in 1990 and 25.69 [19.85–31.53] in 2021; Asia Pacific: 2.14 [0.16–4.14] in 1990 and 3.58 [1.43–5.70] in 2021; Europe: 2.61 [−0.08 to 5.30] in 1990 and 15.28 [12.42–18.14] in 2021; and North America: −5.08 [−23.02 to 12.87] in 1990 and 68.77 [50.67–86.88] in 2020), although in Latin America and the Caribbean appeared to have plateaued (Table 1). Similar trends in DUD mortality were observed when conducting the additional analysis with SDI-weighting age-standardised LOESS smoothed curves (Supplementary Table S12).
Fig. 2.
Age-standardised DUD mortality rate (per 1,000,000 people) across the globe and five continents among 73 countries.
There are considerable variation in the global trends of DUD mortality rates between males and females (Fig. 3 and Table 1); however, in Asia Pacific and Latin America and the Caribbean Africa and North America, no significant differences depending on sex groups was observed in the age-standardised DUD mortality rates for five continents by sex groups from 1990 to 2021 (Supplementary Figures S3–S7).
Fig. 3.
Age-standardised DUD mortality rate (per 1,000,000 people) for the global population by sex among 73 countries, 1990–2021.
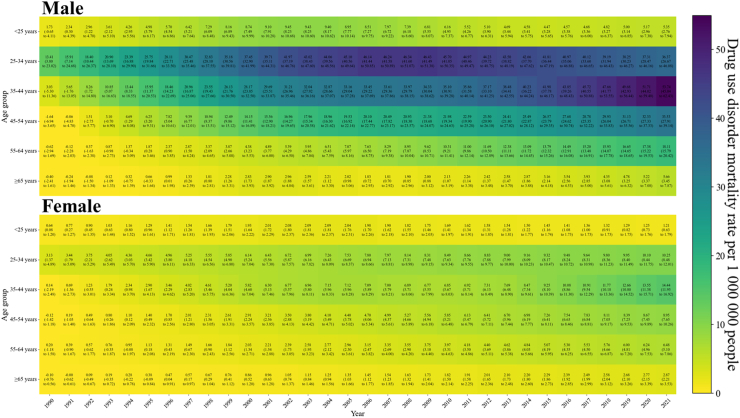
Younger age groups (under 25) indicated relatively stable trends in LOESS smoothed curves of DUD mortality rates. However, a significant increase in trends of LOESS smoothed curves for DUD mortality is observed in middle-aged adult populations, particularly in the groups aged 25–64 years (25–34 years: 8.45 [2.87–14.03] in 1990 and 23.79 [18.18–29.40] in 2021; 35–44 years: 1.68 [−3.39 to 6.74] in 1990 and 34.19 [28.91–39.48] in 2021; 45–54 years: −0.78 [−3.89 to 2.34] in 1990 and 20.96 [17.71–24.22] in 2021; and 55–64 years: −0.20 [−1.87 to 1.46] in 1990 and 12.23 [10.57–13.89] in 2021) (Fig. 4 and Table 1). These variations related to age groups are profound in males among global populations and specific continents, including Africa, Europe, and North America (Supplementary Figures S8–S12). Additional analysis for specific age and sex subgroups also showed similar patterns (Supplementary Tables S13–S30).
Fig. 4.
LOESS smoothed DUD mortality rate (per 1,000,000 people) by sex and age group among 73 countries, 1990–2021.
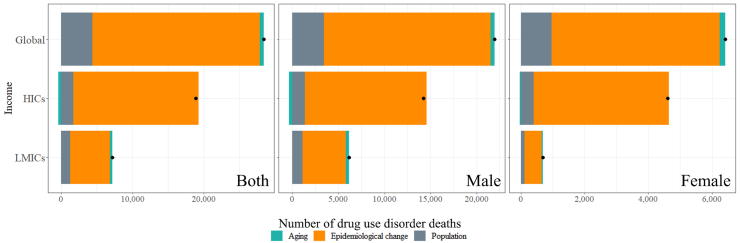
The age-standardised DUD mortality rates association with the log-transformed HDI (β, 14.92 [95% CI, 10.86–18.97], and p < 0.0001), SDI (11.80 [8.36–15.23], and p < 0.0001), reverse GGI (−12.02 [−17.38 to −6.66], and p < 0.0001), and Gini coefficient (−1.84 [−3.11 to −0.57], and p < 0.0001) (Fig. 5). Changes in DUD mortality between the baseline year and final year were decomposed into three components, including population ageing, population growth, and epidemiological change (Fig. 6). From 1990 to 2021, the increase in the number of DUD deaths can be attributed to three factors: population ageing contributed to an additional 600 deaths, epidemiological changes resulted in an increase of 23,411 deaths, and population growth led to a further increase of 4394 deaths (Supplementary Table S27). Particularly in HIC, the impacts of epidemiological changes for increasing DUD mortality rates are prominent as 17,506 deaths compared to other factors (Supplementary Table S27).
Fig. 5.
Correlation between age-standardised DUD mortality rate (per 1,000,000 people) and Human Development Index, Socio-demographic Index, reverse Gender Gap Index, and Gini coefficient.
Fig. 6.
Changes in the number of DUD deaths (per 1,000,000) associated with ageing, epidemiological change, and population from 1990 to 2021 by sex.
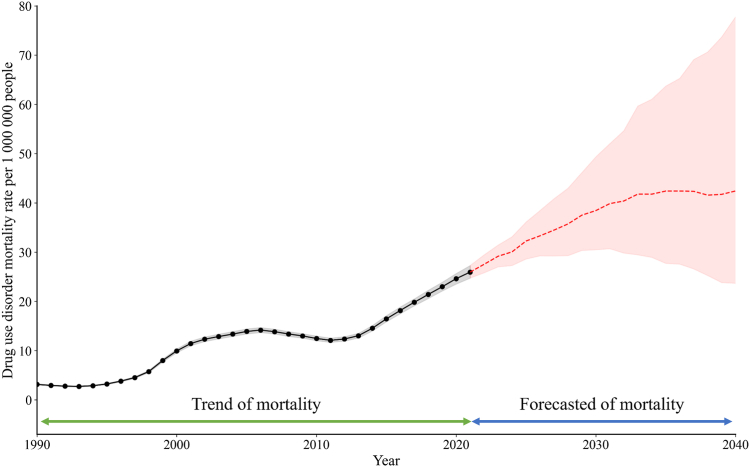
Based on the BAPC models, age-standardised DUD mortality rates were predicted to significantly increase in the number of DUD deaths from 25.95 deaths per 1,000,000 people (95% CrI, 24.72–27.28) in 2021 to 38.45 (30.48–49.33) in 2030, and 42.43 (23.67–77.77) in 2040 (Fig. 7 and Supplementary Table S28).
Fig. 7.
Projections in age-standardised DUD mortality rate (per 1,000,000 people) from 1990 to 2040 by Bayesian age-period-cohort models.
Discussion
This study revealed an overall increase in the estimated global age-standardised DUD mortality rates for 73 countries, from 1.84 to 13.09 deaths per 1,000,000 people from 1990 to 2021. This increase was more pronounced in HICs, with a substantial 12.02-fold rise in DUD mortality. Although several continents such as Africa, Asia Pacific, Europe, and North America exhibited upward trends, geographical variations were evident with North America and Africa showing significant surges. A significant increase in DUD mortality was observed among middle-aged adults and males. Our analysis also identified associations between DUD mortality rates and various indices, such as the HDI, SDI, reverse GGI, and Gini coefficient. From 1990 to 2021, the increase in the number of DUD deaths can be primarily attributed to two factors, including epidemiological change and population growth, with epidemiological change being particularly influential. In HICs, the impacts of epidemiological changes on increasing DUD mortality rates were particularly prominent compared to other factors. Based on BAPC models, projected future trends indicate a continued and significant rise in DUD mortality rates until 2040.
Previous studies on trends in DUD mortality focused on specific countries, shorter time frames, and lack of future projections.2,33,34 To our best knowledge, this is novel research on both global trends in DUD mortality over 30 years and future projections of DUD mortality up to 2040 by utilising the WHO Mortality Database. Furthermore, the other key strength of this study lies in its use of data from the WHO Mortality Database, distinguishing it from previous studies on global DUD mortality rates that primarily relied on the GBD database.5 Previous study using GBD data reported a significant increase in global DUD (e.g., 44.2% increase in alcohol use disorders and 27.3% opioid use disorders) from 1990 to 2016, well-aligning with the our findings.5 GBD has inherent characteristics such as meta-analytical methods.35 In contrast, the WHO mortality database has different methodological characteristics, utilising reported original data.8,36, 37, 38 This approach thereby enhances the data reliability. Furthermore, prior studies are more constrained in scope, typically extending only up to 2019 and covering specific age groups or shorter durations.35,39,40 Our research diverges from these previous studies by not only exploring the international trends in DUD mortality rates between 1990 and 2021 but also projected the estimated future burden of DUD deaths up to 2040, providing a projection analysis for 73 countries. Therefore, we can expand the understanding of global DUD mortality, along with the reported findings from previous GBD studies, thereby providing a novel perspective on global DUD mortality rates and future projections.
The observed increase in global age-standardised SUD mortality rates in our study aligns with previous findings indicating a rise in the prevalence of alcohol and drug use disorders since 1990, driven by population growth and ageing.5 This increase in prevalence, particularly in LMICs, may be attributed to different levels of healthcare infrastructure and access to treatment. LMICs allocate less than 1% of development assistance for health and government spending to address and care for people with mental and neurological DUD.41 Therefore, LMICs often encounter significant challenges in providing adequate substance misuse treatment and mental health services, which could explain the observed steeper increase in DUD mortality rates in these regions.41
However, the severity of DUD mortality is more profound in HICs. This could be due to relatively lower awareness about drug use and the tolerance of drug use in LMICs, particularly in regions where drug production is a major economic activity, potentially leading to underreporting or misclassification of DUD.42 Nonetheless, the steep increase in DUD mortality in HICs cannot be fully explained by these factors alone. In addition, our findings found that DUD mortality varies across global regions and countries. Particularly, North America shows a surge in DUD mortality. Factors such as substance availability, cultural attitudes toward substance use, and policy and enforcement differences play roles in this regional variation. In North America, the opioid crisis, significantly impacting the USA and Canada and predominantly affecting young and middle-aged adults, has been a major contributor to increased DUD mortality.2 In 2019, opioid-related deaths accounted for 15.8 and 6.4 per 100,000 people in the USA and Canada, respectively.3 While there is still lacking evidence for identifying the major drivers of this crisis, various potential drivers have been suggested for this crisis, including the role of pharmaceutical companies, regulatory inadequacies, increased rates of opioid prescribing, and the increased use of illegal heroin and synthetic opioids.3 This opioid crisis could be the primary factor behind the increased DUD mortality trends in North America.
Africa has also shown a significant surge in DUD mortality over the past decade. The long history of drug cultivation, production, trade, and consumption, including indigenous plants and herbs with psychoactive effects, such as cannabis, likely fuels the increasing DUD mortality trends.43 DUD mortality was increasing trends in Africa, wherein major production and trafficking regions such as Morocco (one of the top global producers of cannabis), all characterised by their proximity to major drug production regions and relatively lower psychological barriers against drug use.5,44 Recent years have shown a rise in large-scale trade and recreational use of opiates, synthetic psychoactive stimulants, and prescribed drugs, resulting in new threats across the continent.43 Coupled with high exposure to substances but lacking effective intervention strategies for DUD, these factors likely contribute to the increasing DUD mortality trends in Africa. Therefore, the rise in Africa might also be associated with socio-economic challenges and the growing availability of both illicit and prescription drugs. Our findings from the WHO Mortality database exclusively capture cases where DUD is recorded as the primary cause of death, and insights from other global dataset studies, such as the GBD, can complement these findings.5 DUD can indirectly induce deaths via developing life-threatening diseases or conditions such as cardiovascular disease, cirrhosis, and respiratory depression.5 In addition, individuals with DUD often experience delayed access to healthcare or poor prognosis after treatments, which can exacerbate underlying diseases or comorbid health conditions.45 Socioeconomic factors, including homelessness, unemployment, and social stigma, highly associated with DUD, further increase vulnerability and contribute to a high risk of mortality through indirect mechanisms, such as malnutrition, exposure to violence, and poor hygiene or housing environments, which are less likely to be captured in mortality databases focused solely on primary causes of death.45,46
More prevalent DUD mortality among middle-aged adults can be attributed to several factors. This demographic is vulnerable to exposure stressors such as career pressure, family responsibilities, and changes in social dynamics or family dynamics, and these vulnerabilities could be one of the potential causes of drug use. In addition, middle-aged adults may face barriers to accessing treatment for DUD due to social stigma, fear of career repercussions, and family responsibilities, resulting in untreated or inadequately managed conditions.47 Cumulative damage via relatively long-term exposure to drugs and untreated or inadequately managed status can lead to higher mortality attributed to DUD among those populations. Furthermore, this age group is also more likely to have developed comorbid conditions, such as cardiovascular diseases, liver diseases, or mental health disorders, which can be exacerbated by drug use, leading to higher mortality rates.48 Prescription drug use for managing chronic pain or other health conditions is more prevalent in middle-aged adults compared to young adults, potentially leading to misuse and the development of DUD.49
Furthermore, the association between DUD mortality rates and indices such as HDI, SDI, and reverse GGI suggest socioeconomic factors play a significant role. The observation of higher DUD mortality in more socio-economically developed countries suggests that higher HDI and SDI, indicative of socioeconomic development, might correlate with increased substance availability and lifestyle factors linked to urbanisation and economic growth.50 This trend suggests that higher socio-economic development, as indicated by indices like HDI and SDI, does not necessarily insulate against the rise in DUD mortality. This highlights the complexity of DUD mortality, influenced by factors like low treatment rates, delays in initiating treatment, the stigma associated with substance use disorders, and the poor availability of effective interventions for HIV and hepatitis C among those who inject drugs.5
This analysis shows the international trends in DUD mortality rates between 1990 and 2021 and the estimated future burden of DUD deaths up to 2040. However, this study has a number of limitations. First, our reliance on the WHO Mortality Database, which depends on reporting data from member countries, introduces potential incompleteness of data and variability in the quality among individual countries. To mitigate this, our analysis incorporates only datasets with complete records of at least eight years (Supplementary Table S3). Second, the availability of the WHO database is limited to 2021, preventing the inclusion of more recent trends. Although we performed an additional analysis comparing DUD mortality between the pre-pandemic (2017–2019) and the pandemic (2019–2021) periods (Supplementary Table S33), the short observation period after the outbreak of COVID-19 limits our ability to fully capture the long-term impact of COVID-19 on DUD mortality. When the WHO Mortality database is updated, we plan to conduct further studies to better understand the impacts of COVID-19. Third, there is a likelihood of underestimation in DUD mortality rates, as the WHO database only records primary causes of death based on ICD-10 codes, potentially overlooking DUD-related deaths. Fourth, discrepancies between ICD-10 codes and the disease codes used by the WHO Mortality Database impeded the identification of DUD. To mitigate this, we employed a more conservative definition for DUD, only using WHO codes linked to ICD-9 code (304) and ICD-10 codes (F11-16, F18-19, T40, and X42). Fifth, the WHO mortality database reports only the primary cause of death, defined as the disease or injury that directly initiated the sequence of events leading to death. While this allows for accurate identification of deaths directly caused by DUD, it may underestimate the impact of DUD on indirect deaths, such as those resulting from DUD-related cardiovascular diseases, cirrhosis, self-harm, or interpersonal violence.5 Sixth, our projections are based on the assumption that the influence of age, period, and cohort factors on DUD mortality will remain constant from 2021 to 2040, necessitating re-analysis in the event of significant phenomena impacting DUD mortality.9 However, we have potential opportunities to alter the course of future DUD mortality through public health interventions or policy changes involving those mentioned in our policy implications.51 Over the coming years, future trends in DUD mortality will be shaped by the effective implementation of existing policy options, such as controlled cannabis legalisation, taxation and regulation of drugs, needle and syringe programs, prescription guidelines, and the United Nations SDG 3.5.45,52 In addition, improving healthcare accessibility and developing effective policies and public health interventions will be imperative in determining the success of these efforts in reducing DUD mortality. Seventh, these projections are based on future population estimates from calculations by BAPC models, which inherently assume specific patterns in mortality, fertility, and migration.9 Eighth, while well-established methodologies were employed to capture global trends, the inherent characteristics of this approach may result in different estimates if alternative statistical methods or models are applied.8,9,53 Lastly, while we can provide international trends and future projections for DUD deaths, further well-designed prospective studies considering potential confounding factors, such as socioeconomic factors or quality of reported data from individual countries, are needed to estimate the risks of DUD mortality more accurately.5
The findings regarding the global age-standardised DUD mortality rate and projections for future DUD deaths hold several important policy implications. To reverse increasing trends in DUD mortality, additional research and targeted public health interventions are required. Expanding access to prevention and treatment of DUD, well-aligned with the United Nations Sustainable Development Goal (SDG) 3.5, is imperative, with a particular focus on both DUD and somatic comorbidity in people with DUD.45 While DUD primarily contributes to mortality, its secondary impacts, such as increased risk of comorbid life-threatening conditions, such as cardiovascular disease, self-harm, risky behaviours, and cirrhosis, must not be overlooked.45 Individuals with a history of hospitalisation for DUD face worse prognosis and delayed healthcare access, often exacerbating underlying diseases.45 Therefore, the projected increase in DUD deaths by 2040 underscores the critical need for proactive and long-term planning in public health strategies for DUD; support for further studies to investigate patterns of DUD is also needed. Therefore, addressing the upward trend of DUD mortality requires a multifaceted approach, including improved accessibility of healthcare, targeted interventions for vulnerable populations, and preventive strategies.
As trends of DUD mortality increase globally, particularly in HICs, comprehensive policy interventions are urgent and necessary. Taxation and regulation of some drugs, such as cannabis or prescribed drugs, can effectively reduce the harms associated with these drugs.5 Controlled cannabis legalisation policies, as seen in the United States and Canada, can mitigate adverse outcomes by managing drug distribution and use within a legal framework. In addition, the frequent progression from exposure to prescribed drugs for pain management to the development of DUD highlights the need for prescription guidelines to prevent over-prescription. Moreover, careless injection methods and poor hygiene associated with injection practices result in an increased risk of infectious diseases transmitted via needles and comorbid health outcomes. Needle and syringe programs can help mitigate mortality attributed to DUD.52 Lastly, the positive correlations between development indices and DUD mortality rates suggested that more developed countries should not underestimate the risks associated with DUD. In summary, proactive, long-term planning will be essential to mitigate the public health impact of DUD and reverse the projected increase in mortality.
In conclusion, there has been a marked and progressive increase in international DUD mortality since 1990, especially in HICs and the older population. Using models that explicitly adjusted for the effects of age, period, and cohort on trends in DUD mortality, future DUD deaths are predicted to increase up to 2040 at the global levels. These findings suggest urgent and proactive strategies to reduce the mortality rates related to DUD are needed.
Contributors
DKY had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. HJK, JK, and DKY have access to and verify the underlying study data. All authors approved the final version before submission. Study concept and design: SK, SW, HJK, JK, and DKY; Acquisition, analysis, or interpretation of data: SK, SW, HJK, JK, and DKY; Drafting of the manuscript: SK, SW, HJK, JK, and DKY; Critical revision of the manuscript for important intellectual content: HaL, HyL, JP, TK, GF, LB, MR, LS, GFLS, ED, CJN, and JL; Statistical analysis: SK, SW, HJK, JK, and DKY; Study supervision: HJK, JK, and DKY. DKY supervised the study and is the guarantor for this study. SK and SW contributed as first authors. HJK, JK, and DKY contributed as co-corresponding authors. DKY is a senior author. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
The lead authors (SK, HJK, JK, SW, and DKY) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Data sharing statement
The WHO Mortality database is a global collaborative dataset for mortality rates reported by WHO member countries. Study protocol and statistical code: available upon request from Dong Keon Yon (email: yonkkang@gmail.com), for qualified researchers and analyses aligned with the study objectives. Dataset: provided by the WHO under a data use agreement, accessible upon request after approval of a proposal.
Declaration of interests
All authors declare no competing interests.
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (RS-2024-00460379) and the MSIT (Ministry of Science and ICT), Korea, under the ITRC (Information Technology Research Center) support program (IITP-2024-RS-2024-00438239) supervised by the IITP (Institute for Information & Communications Technology Planning & Evaluation).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2024.102985.
Contributor Information
Hyeon Jin Kim, Email: hyeonjin7418@gmail.com.
Jiseung Kang, Email: wltmd1006@gmail.com.
Dong Keon Yon, Email: yonkkang@gmail.com.
Appendix ASupplementary data
References
- 1.Cantor J.H., Whaley C.M., Stein B.D., Powell D. Analysis of substance use disorder treatment admissions in the US by sex and race and ethnicity before and during the COVID-19 pandemic. JAMA Netw Open. 2022;5(9) doi: 10.1001/jamanetworkopen.2022.32795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomes T., Tadrous M., Mamdani M.M., Paterson J.M., Juurlink D.N. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1(2) doi: 10.1001/jamanetworkopen.2018.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Lancet Regional H.-A. Opioid crisis: addiction, overprescription, and insufficient primary prevention. Lancet Reg Health Am. 2023;23 doi: 10.1016/j.lana.2023.100557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomes T., Ledlie S., Tadrous M., Mamdani M., Paterson J.M., Juurlink D.N. Trends in opioid toxicity-related deaths in the US before and after the start of the COVID-19 pandemic, 2011-2021. JAMA Netw Open. 2023;6(7) doi: 10.1001/jamanetworkopen.2023.22303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2016 Alcohol and Drug Use Collaborators The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012. doi: 10.1016/S2215-0366(18)30337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gress T., Miller M., Meadows C., 3rd, Neitch S.M. Benzodiazepine overuse in elders: defining the problem and potential solutions. Cureus. 2020;12(10) doi: 10.7759/cureus.11042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tadrous M., Shakeri A., Chu C., et al. Assessment of stimulant use and cardiovascular event risks among older adults. JAMA Netw Open. 2021;4(10) doi: 10.1001/jamanetworkopen.2021.30795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ebmeier S., Thayabaran D., Braithwaite I., Bénamara C., Weatherall M., Beasley R. Trends in international asthma mortality: analysis of data from the WHO Mortality Database from 46 countries (1993-2012) Lancet. 2017;390(10098):935–945. doi: 10.1016/S0140-6736(17)31448-4. [DOI] [PubMed] [Google Scholar]
- 9.Kiyoshige E., Ogata S., O'Flaherty M., et al. Projections of future coronary heart disease and stroke mortality in Japan until 2040: a Bayesian age-period-cohort analysis. Lancet Reg Health West Pac. 2023;31 doi: 10.1016/j.lanwpc.2022.100637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barco S., Mahmoudpour S.H., Valerio L., et al. Trends in mortality related to pulmonary embolism in the European Region, 2000-15: analysis of vital registration data from the WHO Mortality Database. Lancet Respir Med. 2020;8(3):277–287. doi: 10.1016/S2213-2600(19)30354-6. [DOI] [PubMed] [Google Scholar]
- 11.Eldridge L., Garton E.M., Duncan K., Gopal S. Authorship of publications supported by NCI-funded grants involving low- and middle-income countries. JAMA Netw Open. 2024;7(3) doi: 10.1001/jamanetworkopen.2024.3215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bray F., Jemal A., Grey N., Ferlay J., Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012;13(8):790–801. doi: 10.1016/S1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 13.Ahmad O.B., Boschi-Pinto C., Lopez A.D., Murray C.J., Lozano R., Inoue M. Vol. 9. World Health Organization; Geneva: 2001. Age Standardization of Rates: A New WHO Standard; pp. 1–14. [Google Scholar]
- 14.Walker R.W., McLarty D.G., Kitange H.M., et al. Stroke mortality in urban and rural Tanzania. Adult morbidity and mortality project. Lancet. 2000;355(9216):1684–1687. doi: 10.1016/s0140-6736(00)02240-6. [DOI] [PubMed] [Google Scholar]
- 15.Cleveland W.S., Devlin S.J. Locally weighted regression: an approach to regression analysis by local fitting. J Am Stat Assoc. 1988;83(403):596–610. [Google Scholar]
- 16.Mansournia M.A., Nazemipour M. Recommendations for accurate reporting in medical research statistics. Lancet. 2024;403(10427):611–612. doi: 10.1016/S0140-6736(24)00139-9. [DOI] [PubMed] [Google Scholar]
- 17.Greenland S., Mansournia M.A., Joffe M. To curb research misreporting, replace significance and confidence by compatibility: a Preventive Medicine Golden Jubilee article. Prev Med. 2022;164 doi: 10.1016/j.ypmed.2022.107127. [DOI] [PubMed] [Google Scholar]
- 18.Mansournia M., Nazemipour M., Etminan M. P-value, compatibility, and S-value. Global Epidemiol. 2022;4 doi: 10.1016/j.gloepi.2022.100085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacoby W.G. Loess: a nonparametric, graphical tool for depicting relationships between variables. Elect Stud. 2000;19(4):577–613. [Google Scholar]
- 20.Cohen R.A., editor. An introduction to PROC LOESS for local regression. Proceedings of the Twenty-Fourth Annual SAS Users Group International Conference, Paper. SAS Institute Inc; Cary, North Carolina, USA: 1999. [Google Scholar]
- 21.Chong B., Jayabaskaran J., Kong G., et al. Trends and predictions of malnutrition and obesity in 204 countries and territories: an analysis of the Global Burden of Disease Study 2019. EClinicalMedicine. 2023;57 doi: 10.1016/j.eclinm.2023.101850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin Y.H., Hwang J., Kwon R., et al. Global, regional, and national burden of allergic disorders and their risk factors in 204 countries and territories, from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Allergy. 2023;78(8):2232–2254. doi: 10.1111/all.15807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Lancet 2020: a critical year for women, gender equity, and health. Lancet. 2020;395(10217):1. doi: 10.1016/S0140-6736(19)33170-8. [DOI] [PubMed] [Google Scholar]
- 24.Clarsen B., Nylenna M., Klitkou S.T., et al. Changes in life expectancy and disease burden in Norway, 1990-2019: an analysis of the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7(7):e593–e605. doi: 10.1016/S2468-2667(22)00092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Woolf S.H., Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA. 2019;322(20):1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sagar R., Dandona R., Gururaj G., et al. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. Lancet Psychiatry. 2020;7(2):148–161. doi: 10.1016/S2215-0366(19)30475-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Catalano M.T., Leise T.L., Pfaff T.J. Measuring resource inequality: the Gini coefficient. Numeracy. 2009;2(2):4. [Google Scholar]
- 28.Qi J., Li M., Wang L., et al. National and subnational trends in cancer burden in China, 2005-20: an analysis of national mortality surveillance data. Lancet Public Health. 2023;8(12):e943–e955. doi: 10.1016/S2468-2667(23)00211-6. [DOI] [PubMed] [Google Scholar]
- 29.Yip P.S.F., Zheng Y., Wong C. Demographic and epidemiological decomposition analysis of global changes in suicide rates and numbers over the period 1990-2019. Inj Prev. 2022;28(2):117–124. doi: 10.1136/injuryprev-2021-044263. [DOI] [PubMed] [Google Scholar]
- 30.Schmid V.J., Held L. Bayesian age-period-cohort modeling and prediction-BAMP. J Stat Software. 2007;21:1–15. [Google Scholar]
- 31.Holford T.R. Wiley StatsRef: Statistics Reference Online. John Wiley & Sons, Inc; Hoboken, NJ: 2014. Age–period–cohort analysis; pp. 1–25. [Google Scholar]
- 32.Hahn J.W., Woo S., Park J., et al. Global, regional, and national trends in liver disease-related mortality across 112 countries from 1990 to 2021, with projections to 2050: comprehensive analysis of the WHO Mortality Database. J Kor Med Sci. 2024;39:1–22. doi: 10.3346/jkms.2024.39.e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fujita-Imazu S., Xie J., Dhungel B., et al. Evolving trends in drug overdose mortality in the USA from 2000 to 2020: an age-period-cohort analysis. EClinicalMedicine. 2023;61 doi: 10.1016/j.eclinm.2023.102079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dwyer-Lindgren L., Bertozzi-Villa A., Stubbs R.W., et al. Trends and patterns of geographic variation in mortality from substance use disorders and intentional injuries among US counties, 1980-2014. JAMA. 2018;319(10):1013–1023. doi: 10.1001/jama.2018.0900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shen J., Hua G., Li C., Liu S., Liu L., Jiao J. Prevalence, incidence, deaths, and disability-adjusted life-years of drug use disorders for 204 countries and territories during the past 30 years. Asian J Psychiatr. 2023;86 doi: 10.1016/j.ajp.2023.103677. [DOI] [PubMed] [Google Scholar]
- 36.Ferrari A.J., Santomauro D.F., Aali A., et al. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2133–2161. doi: 10.1016/S0140-6736(24)00757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization WHO Mortality Database. 2023. https://platform.who.int/mortality
- 38.The Institute for Health Metrics and Evaluation Global Burden of Disease (GBD) 2023. https://www.healthdata.org/research-analysis/gbd
- 39.Castaldelli-Maia J.M., Bhugra D. Analysis of global prevalence of mental and substance use disorders within countries: focus on sociodemographic characteristics and income levels. Int Rev Psychiatry. 2022;34(1):6–15. doi: 10.1080/09540261.2022.2040450. [DOI] [PubMed] [Google Scholar]
- 40.Castelpietra G., Knudsen A.K.S., Agardh E.E., et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990-2019: findings from the Global Burden of Disease Study 2019. Lancet Reg Health Eur. 2022;16 doi: 10.1016/j.lanepe.2022.100341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Patel V., Chisholm D., Parikh R., et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. 2016;387(10028):1672–1685. doi: 10.1016/S0140-6736(15)00390-6. [DOI] [PubMed] [Google Scholar]
- 42.Hammarlund R., Crapanzano K.A., Luce L., Mulligan L., Ward K.M. Review of the effects of self-stigma and perceived social stigma on the treatment-seeking decisions of individuals with drug- and alcohol-use disorders. Subst Abuse Rehabil. 2018;9:115–136. doi: 10.2147/SAR.S183256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Onaolapo O.J., Olofinnade A.T., Ojo F.O., Adeleye O., Falade J., Onaolapo A.Y. Substance use and substance use disorders in Africa: an epidemiological approach to the review of existing literature. World J Psychiatry. 2022;12(10):1268–1286. doi: 10.5498/wjp.v12.i10.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Degenhardt L., Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70. doi: 10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- 45.Formánek T., Krupchanka D., Mladá K., Winkler P., Jones P.B. Mortality and life-years lost following subsequent physical comorbidity in people with pre-existing substance use disorders: a national registry-based retrospective cohort study of hospitalised individuals in Czechia. Lancet Psychiatry. 2022;9(12):957–968. doi: 10.1016/S2215-0366(22)00335-2. [DOI] [PubMed] [Google Scholar]
- 46.Li A., Toll M., Bentley R. Mapping social vulnerability indicators to understand the health impacts of climate change: a scoping review. Lancet Planet Health. 2023;7(11):e925–e937. doi: 10.1016/S2542-5196(23)00216-4. [DOI] [PubMed] [Google Scholar]
- 47.Jones K.F., Beiting K.J., Ari M., et al. Age-friendly care for older adults with substance use disorder. Lancet Healthy Longev. 2023;4(10):e531–e532. doi: 10.1016/S2666-7568(23)00174-5. [DOI] [PubMed] [Google Scholar]
- 48.Guo J., Huang X., Dou L., et al. Aging and aging-related diseases: from molecular mechanisms to interventions and treatments. Signal Transduct Target Ther. 2022;7(1):391. doi: 10.1038/s41392-022-01251-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lin J., Arnovitz M., Kotbi N., Francois D. Substance use disorders in the geriatric population: a review and synthesis of the literature of a growing problem in a growing population. Curr Treat Options Psychiatry. 2023;10:313–332. doi: 10.1007/s40501-023-00291-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rehm J., Shield K.D. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21(2):10. doi: 10.1007/s11920-019-0997-0. [DOI] [PubMed] [Google Scholar]
- 51.Vollset S.E., Ababneh H.S., Abate Y.H., et al. Burden of disease scenarios for 204 countries and territories, 2022–2050: a forecasting analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2204–2256. doi: 10.1016/S0140-6736(24)00685-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roberts H.H., Stone M., Isac A.J. Syringe services programs to reduce intravenous disease transmission in substance use disorders. Nurs Clin North Am. 2023;58(2):243–256. doi: 10.1016/j.cnur.2023.01.004. [DOI] [PubMed] [Google Scholar]
- 53.Blencowe H., Cousens S., Oestergaard M.Z., et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379(9832):2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.