Abstract
Background
Displaced tibial tubercle (TT) fractures in adolescents are typically treated with open reduction and internal fixation. While metallic screw (MS) fixation provides strong stability, it often results in a high incidence of postoperative screw head protrusion or irritation, leading to additional removal surgery. Bioabsorbable screw (BS) fixation presents an alternative that may avoid these issues, though its stability has not yet been extensively documented in the literature. This study aims to compare the efficacy of BS versus MS in the fixation of TT fractures.
Methods
A retrospective analysis was conducted on adolescent patients with TT fractures who underwent surgical treatment from September 2015 to September 2023. Patients were divided into two groups based on the fixation method: The BS group and the MS group. Data collected included patient demographics, fracture details, treatment strategies, radiological and clinical rehabilitation outcomes, and postoperative complications. Knee joint function was evaluated using the Lysholm and Tegner scores. Statistical analysis was performed to identify differences between the variables of the two groups.
Results
A total of 30 patients with 32 fractures were included, with 15 fractures in the BS group and 17 in the MS group. The average follow-up period was 42.1 (range: 12.0-109.5) months. The demographic characteristics, fracture details, and treatment strategies were comparable between the two groups. No significant differences were observed between the groups in fracture healing time, time to return to pre-injury activities, or knee joint function as assessed by the Lysholm and Tegner scores at the final follow-up. However, compared with the MS group, the BS group showed a shorter time to regain full range of motion (ROM) in the knee joint and experienced lower rates of postoperative hardware irritation and joint stiffness.
Conclusions
Both BS and MS fixations are safe and effective for treating adolescent TT fractures. BS fixation has the advantages of avoiding hardware irritation, facilitating earlier recovery of knee joint ROM, reducing the incidence of joint stiffness, and eliminating the need for additional removal surgery.
Clinical trial number
Not applicable.
Keywords: Tibial tubercle fracture, Adolescent, Bioabsorbable screw, Metallic screw
Background
Adolescent tibial tubercle (TT) fractures are a rare sports-related injury, accounting for 0.4–2.7% of pediatric fractures [1–3]. In recent years, the incidence has been rising due to increased participation of children in high-intensity sports [4]. The primary goals of treatment are to restore the knee’s extensor mechanism, realign the articular cartilage surface of proximal tibia, and address associated injuries [2, 5]. Surgery is selected for 88% of patients with TT fractures, with the majority undergoing open reduction and internal fixation using metallic screw (MS). Following treatment, 99.8% of patients achieved fracture healing, and 98.9% returned to competitive or pre-injury activities [1]. However, the complication rate associated with MS fixation for TT fractures is as high as 18-28% [1, 2, 6]. The most common complications are irritation symptoms related to screw protrusion, including bursitis, pain, and impaired joint function [1, 2, 4, 5].
Limited soft tissue protection and high frequency of knee joint movement are responsible for the irritation symptoms caused by the exposed screw heads and washers of MS on the bone cortex [4, 7, 8]. This issue affects 44% of patients with TT fractures, often necessitating a second surgery to remove the MS [4]. In the 1980s, biodegradable α-hydroxy polyester materials were introduced clinically for bone or ligament fixation. Among these, Poly-L-lactic acid (PLLA) screws, which do not require a second removal surgery, have been widely used in pediatric and adolescent fractures [9–11]. The literature describes surgical techniques for bioabsorbable screw (BS) implantation, such as pre-drilling the bone cortex to countersink the screw head or trimming excess screw head length with an oscillating saw, which effectively prevents hardware protrusion [10]. However, since the bending and shear strength of PLLA is significantly lower than that of traditional metal materials, its clinical application has mostly been limited to the fixation of non-weight-bearing bone fractures where less fixation strength is required. The efficacy of PLLA screws in the fixation of adolescent TT fractures remains uncertain.
This study aims to evaluate the efficacy of BS versus MS in the fixation of adolescent TT fractures. We hypothesize that BS fixation is a safe and effective treatment option for adolescent TT fractures, with the potential to improve treatment outcomes as a superior alternative to MS fixation.
Methods
Patients and grouping
The study was approved by the Institutional Review Board ([2023]-E-179-R). A retrospective review was conducted among adolescent patients with acute tibial tubercle fractures who underwent surgical treatment at our center from September 2015 to September 2023. Inclusion criteria were: Fractures that met the modified Ogden classification, treatment with screw fixation, age under 18 years, and a follow-up period of over 12 months. Exclusion criteria included: Incomplete clinical or imaging data, multiple fractures, systemic diseases such as osteogenesis imperfecta, or a history of lower limb surgery. Eligible patients were divided into two groups based on the fixation method: The BS group and the MS group. The choice of internal fixation type was based on the preferences of the patients and their guardians, with no bias from the surgeons.
Patient demographic characteristics were collected, including sex, age, BMI, affected side, and history of osteochondral diseases. Fracture details were recorded, including the mechanism of injury and involved sports activities, associated injuries, modified Ogden classification, and presence of neurovascular damage or compartment syndrome. Management strategies were documented, including the number and size of screws used intraoperatively, and the postoperative rehabilitation plans for range of motion (ROM) and muscle strength. Rehabilitation outcomes were assessed, including the time to complete radiographic fracture healing (defined as complete disappearance of the fracture line on X-rays), the time to regain full knee ROM, the degree of ROM recovery at the final follow-up, the time to return to pre-injury activities as well as the Lysholm and Tegner scores at the final follow-up. Surgical complications were recorded, including any loss of flexion relative to the contralateral side and extension limitations with a flexion contracture greater than 5° [4, 12].
Surgical technique
All surgeries were performed using open reduction. After achieving anatomical reduction of the fracture under direct vision and C-arm fluoroscopy, fixation was performed using either 3.5–4.5 mm solid, partially threaded BS (composed of poly-L-lactic acid and hydroxyapatite) or hollow, partially threaded MS (composed of titanium alloy), depending on the size of the bone fragment. The TT fragment was secured with compression following the steps of positioning, drilling, tapping, and screw insertion. In the BS group, a recess matching the size of the screw head was drilled into the bone cortex to countersink the screw head. In the MS group, washers were used to prevent cortical bone damage or perforation. For type VI fractures, two additional Kirschner wires were used for retrograde cross fixation of the proximal epiphysis. Ruptures of the patellar tendon at the tibial insertion were woven and secured with suture anchors, while sleeve avulsions at the inferior pole of the patella and grade III meniscal tears were directly sutured.
Postoperative management
Postoperatively, the knee joint was immobilized in an extended position using a hinged brace, and weight-bearing was prohibited. At 3 weeks postoperatively, if tolerated by the patient, exercises with a ROM of 0 to 30° were initiated, with touch-down weight-bearing allowed under the protection of a brace. At 6 weeks postoperatively, the brace was removed, full ROM exercises were introduced, and a gradual transition to full weight-bearing was initiated. All patients were followed up in the outpatient clinic until fracture healing and activity resumption were confirmed. Afterwards, regular telephone follow-ups were conducted for at least 12 months.
Statistical analysis
Data were analyzed using SPSS 19.0 (IBM, Armonk, NY). Normally distributed continuous variables were presented as mean ± standard deviation (x ± s) and compared using the independent samples t-test. Non-normally distributed continuous variables were presented as median (Q1, Q3) and compared using the Mann-Whitney U test. Categorical variables, presented as frequencies (n) and percentages (%), were compared using the χ² test or Fisher’s exact test. A P-value of < 0.05 (two-sided) was considered statistically significant.
Results
Basic data
The study included 32 fractures in 30 patients, with 2 patients having bilateral fractures. There were 28 males and 2 females, with a mean age of 13.3 ± 1.0 (range 10.8–14.7) years and a mean BMI of 27.3 ± 3.5 (range 21.0-36.1) kg/m². Eighteen fractures involved the left side, while 14 fractures involved the right side. One patient with bilateral involvement had a history of Osgood-Schlatter disease.
Twenty-six fractures were caused by eccentric contraction of the quadriceps muscle during knee flexion, while 6 fractures were caused by concentric contraction of the quadriceps muscle during knee extension, and 10 fractures were accompanied by knee twisting at the time of injury. The sports activities involved included: 10 cases of running, 6 cases of basketball, 3 cases of soccer, 3 cases of jumping, 1 case of taekwondo, 1 case of stair climbing, and 6 cases of accidental falls.
The modified Ogden classification included 6 type Ia fractures, 3 type Ib fractures, 3 type IIa fractures, 6 type IIb fractures, 6 type IIIa fractures, 6 type IIIb fractures, and 2 type VIa fractures. Associated injuries included 12 cases of patellar tendon rupture at the tibial insertion, 8 cases of sleeve avulsion at the inferior pole of the patella, 6 cases of grade I to II cruciate ligament tears, and 2 cases of grade III meniscal tears. No neurovascular injuries or compartment syndrome were observed.
Intergroup comparison
The BS group (poly-L-lactic acid [PLA]/hydroxyapatite [HA]) included 15 fractures, while the MS group (titanium alloy) included 17 fractures. The average follow-up period was 39.4 months for the BS group and 44.5 months for the MS group. In the MS group, all patients had their screws removed at an average of 8.8 ± 4.1 (range 3.8–20.1) months postoperatively.
There were no significant differences between the two groups in terms of the proportion of males, age, BMI, distribution of modified Ogden classifications, incidence of each type of associated injury, average number of screws used per fracture fixation, or the time to discontinue immobilization in the extended position and initiate ROM and weight-bearing exercises (Table 1).
Table 1.
Intergroup comparison of demographic characteristics, fracture details, and treatment strategies
| Variables | All Patients (n = 30) | Bioabsorbable screw group (n = 14) | Metallic screw group (n = 16) | P-Value |
|---|---|---|---|---|
| Fractures (cases) | 32 | 15 | 17 | - |
| Demographic Characteristics | ||||
| Gender (male) | 28 (93.3) | 13 (92.9) | 15 (93.8) | P = 1.0 |
| Age (years) | 13.3 ± 1.0 (10.8–14.7) | 13.0 ± 1.3 (10.8–14.7) | 13.5 ± 0.7 (11.5–14.6) | P = 0.21 |
| BMI (kg/m²) | 27.3 ± 3.5 (21.0-36.1) | 27.9 ± 2.8 (23.3–32.8) | 26.6 ± 4.1 (21.0-36.1) | P = 0.38 |
| Fracture Details | ||||
| Associated Injuries | P > 0.05 | |||
| Rupture of the patellar tendon at the tibial insertion | 12 (37.5) | 4 (26.7) | 8 (47.1) | |
| Sleeve-like avulsion of the inferior pole of the patella | 8 (25.0) | 4 (26.7) | 4 (23.5) | |
| Grade I to II tears of cruciate ligament | 6 (18.8) | 3 (20.0) | 3 (17.6) | |
| Grade III tears of meniscus | 2 (6.3) | 1 (6.7) | 1 (5.9) | |
| Ogden Classification | P > 0.05 | |||
| Type I | 9 (28.1) | 4 (26.7) | 5 (29.4) | |
| Type II | 9 (28.1) | 4 (26.7) | 5 (29.4) | |
| Type III | 12 (37.5) | 6 (40.0) | 6 (35.3) | |
| Type VI | 2 (6.3) | 1 (6.7) | 1 (5.9) | |
| Type VI | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Treatment Strategies | ||||
| Number of Screws Used (pieces) | 3.1 ± 1.1 (1–6) | 3.2 ± 1.2 (2–6) | 3.1 ± 1.1 (1–5) | P = 0.73 |
| Start Time for Flexion-Extension and Weight-Bearing (weeks) | 6.3 ± 3.3 (2–12) | 6.1 ± 3.1 (3–12) | 6.5 ± 3.6 (2–12) | P = 0.78 |
| Time of Screw Removal (months) | - | - | 8.8 ± 4.1 (3.8–20.1) | - |
Continuous variables are expressed as mean ± standard deviation (range), and categorical variables are expressed as frequency (percentage)
There were no significant differences between the two groups in terms of time to complete radiographic healing (12.1 ± 1.0 vs. 12.6 ± 2.7 weeks, P = 0.57), time to return to pre-injury activities (4.4 ± 1.2 vs. 5.1 ± 1.7 months, P = 0.23), or the Lysholm scores (94.8 ± 6.0 vs. 95.9 ± 5.4, P = 0.57) and the Tegner scores (6.7 ± 1.5 vs. 6.9 ± 0.8, P = 0.63) at the final follow-up (Table 2) (Figs. 1 and 2). However, the BS group demonstrated a shorter time to regain full ROM in the knee joint (3.8 ± 1.2 vs. 5.2 ± 1.6 months, P = 0.02) and a lower incidence of knee flexion range deficit (6.7% vs. 35.3%, P = 0.09) at the final follow-up compared to the MS group (Table 2).
Table 2.
Intergroup comparison of radiological and clinical rehabilitation
| Variables | All Patients (n = 30) | Bioabsorbable screw group (n = 14) | Metallic screw group (n = 16) | P-Value |
|---|---|---|---|---|
| Fractures (cases) | 32 | 15 | 17 | — |
| Radiological Rehabilitation | ||||
| Time to complete healing (weeks) | 12.4 ± 2.1 (9.0-16.9) | 12.1 ± 1.0 (10.5–13.6) | 12.6 ± 2.7 (9.0-16.9) | P = 0.57 |
| Clinical Rehabilitation | ||||
| Time to regain full range of motion (months) | 4.5 ± 1.6 (2–8) | 3.8 ± 1.2 (2–6) | 5.2 ± 1.6 (3–8) | P = 0.02 |
| Time to return to pre-injury activity (months) | 4.8 ± 1.5 (3–9) | 4.4 ± 1.2 (3–6) | 5.1 ± 1.7 (3–9) | P = 0.23 |
| Degree of range of motion recovery at the last follow-up | P = 0.09 | |||
| No flexion loss | 25 (78.1) | 14 (93.3) | 11 (64.7) | |
| Flexion loss of 0–10° | 2 (6.3) | 0 (0.0) | 2 (11.8) | |
| Flexion loss of 10–20° | 3 (9.4) | 1 (6.7) | 2 (11.8) | |
| Flexion loss>20° | 2 (6.3) | 0 (0.0) | 2 (11.8) | |
| Flexion contracture>5° | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Degree of activity level recovery at the last follow-up | ||||
| Lysholm score | 95.3 ± 5.6 (82–100) | 94.8 ± 6.0 (85–100) | 95.9 ± 5.4 (82–100) | P = 0.57 |
| Tegner score | 6.8 ± 1.2 (3–8) | 6.7 ± 1.5 (3–8) | 6.9 ± 0.8 (6–8) | P = 0.63 |
Continuous variables are expressed as mean ± standard deviation (range), and categorical variables are expressed as frequency (percentage)
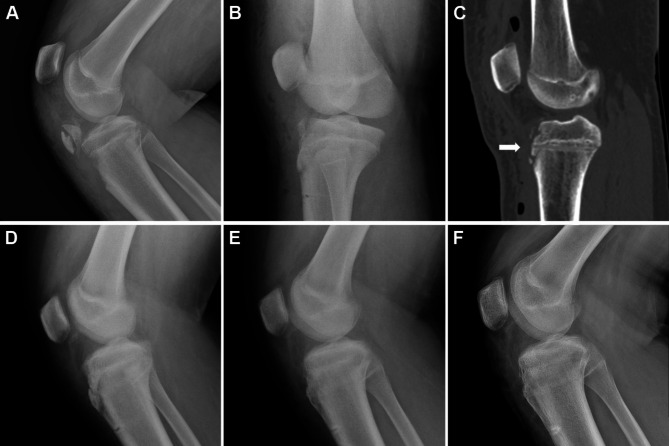
Fig. 1.
Radiological examinations of a 13.9-year-old boy with an Ogden type IIB tibial tubercle fracture. (A) Preoperative X-ray; (B) Immediate postoperative X-ray; (C) Immediate postoperative CT scan, showing the tunnel of the bioabsorbable screw (arrow); (D) X-ray at 6 weeks postoperative; (E) X-ray at 3 months postoperative; (F) X-ray at 6 months postoperative
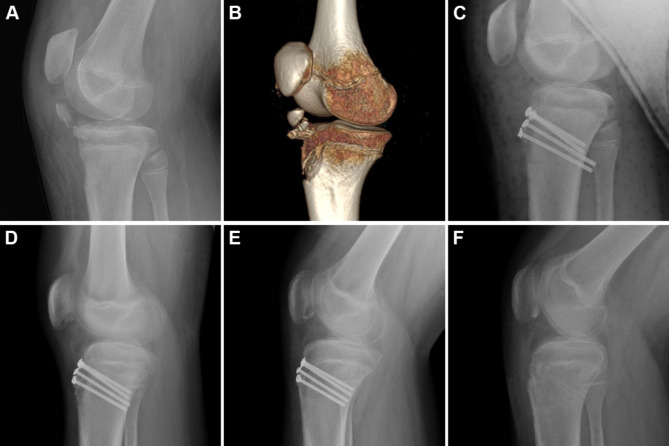
Fig. 2.
Radiological examinations of a 13.5-year-old boy with an Ogden type IB tibial tubercle fracture. (A) Preoperative X-ray; (B) Preoperative CT reconstruction; (C) Immediate postoperative X-ray; (D) X-ray at 1 month postoperative; (E) X-ray at 4 months postoperative; (F) X-ray at 7 months postoperative
The incidence of hardware irritation or residual pain (6.7% vs. 41.2%, P = 0.04) was lower in the BS group compared to the MS group, as was the incidence of joint stiffness or restricted ROM (6.7% vs. 35.3%, P = 0.09). Additionally, there were no significant differences between the two groups in the incidence of joint clicking without locking, extension weakness, heterotopic ossification of the patellar tendon, or numbness around the incision site (Table 3). No bone healing disorders such as bone nonunion, delayed healing, refracture, clinically significant implant degradation reactions, or growth arrest or deformities were observed in either group.
Table 3.
Intergroup comparison of postoperative complications
| Variables | All Patients (n = 30) | Bioabsorbable screw group (n = 14) | Metallic screw group (n = 16) | P-Value |
|---|---|---|---|---|
| Fractures (cases) | 32 | 15 | 17 | — |
| Postoperative Complications | ||||
| Hardware irritation or residual pain | 8 (25.0) | 1 (6.7) | 7 (41.2) | P = 0.04 |
| Joint stiffness or restricted range of motion | 7 (21.9) | 1 (6.7) | 6 (35.3) | P = 0.09 |
| Knee flexion catching without locking | 4 (12.5) | 2 (13.3) | 2 (11.8) | P = 1.0 |
|
Weak extension Heterotopic ossification of the patellar tendon |
2 (6.3) 1 (3.1) |
1 (6.7) 1 (6.7) |
1 (5.9) 0 (0.0) |
P = 1.0 P = 0.47 |
| Numbness around the incision | 1 (3.1) | 1 (6.7) | 0 (0.0) | P = 0.47 |
Continuous variables are expressed as mean ± standard deviation (range), and categorical variables are expressed as frequency (percentage)
Discussion
The treatment of TT fractures in adolescents requires careful planning before making decisions, as it may impact both activity resumption and joint preservation [1, 2]. This study found that both poly-L-lactic acid BS and titanium alloy MS are safe and effective for TT fracture fixation. However, fixation with BS offers additional benefits through the countersinking of screw heads. It can prevent hardware irritation, facilitate earlier recovery of knee joint ROM, reduce the incidence of joint stiffness, and eliminate the need for secondary removal surgery.
Adolescent TT fractures are commonly sports-related injuries. In this study, 80% of patients sustained their injuries during sports activities, aligning with the reported incidence of 66-86% in the literature [4, 6]. The age of onset in this study was concentrated around an average age of 13.3 years, slightly younger than the 14.2–15.0 years reported in the literature, but still within the period of TT ossification and fusion [6, 13]. During this period, the fibrous cartilage in the TT cartilage-bone transition zone gradually transitions to columnar cartilage, resulting in reduced tensile strength and increased susceptibility to avulsion fractures [3, 5, 13]. Most patients in this study were male, comprising 93.3% of the cohort, consistent with the 83–97% incidence reported in the literature [1, 2]. This gender disparity is likely due to the later closure of growth plates in males, stronger quadriceps muscles, and more frequent participation in high-intensity sports [2, 4]. The left limb was more commonly affected, accounting for 56% in this study, close to the 59% incidence reported in the literature, which may be related to right-handed athletes relying more on their left lower limb for force generation [2]. The classic injury mechanism involves violent concentric or eccentric contraction of the quadriceps during extreme knee extension or flexion [1–3, 5]. However, this study found that 33.3% of the injuries were also related to knee twisting. Fractures were predominantly classified as Ogden type III, accounting for 40% in this study, which is similar to the 41-50.6% range reported in the literature [2, 4]. The most common associated injury was patellar tendon avulsion, with an incidence of 40% in this study, which is higher than the 2.4-13.3% incidence reported in the literature [2, 12]. Contributing factors include a history of Osgood-Schlatter disease (OSD) and extreme BMI [4–6]. In this study, one patient with bilateral involvement had a history of OSD, and most of the other patients were obese children subjected to abnormal loads and vulnerable epiphysis, with an average BMI of 27.3 kg/m².
Displaced or intra-articular TT fractures are typically treated with open reduction and compression screw fixation [1–3, 5]. Titanium alloy, known for its excellent biocompatibility, mechanical properties, and corrosion resistance, has been used clinically since the 1950s [14]. Titanium alloy screw fixation for tibial tubercle fractures yields satisfactory outcomes, with 99.8% of patients achieving fracture healing and 98.9% returning to pre-injury activity levels [1]. However, in the 1980s, biodegradable and bioabsorbable materials, such as alpha-hydroxy polyesters represented by PLLA, were introduced clinically. PLLA/HA screws, known for their excellent biocompatibility, mechanical properties, degradability, and bone-inductive effects, have replaced titanium alloy screws in some applications [9, 15]. PLLA screws are widely used for the fixation of long bone metaphyses and epiphyses, short bones, and small bone fragments in children, with the incidence of fixation failure or rejection being less than 5% [10, 16]. However, PLLA screws have initial bending and shear strengths of 300 MPa and 200 MPa, respectively, which are close to cortical bone but significantly inferior to titanium alloy screw [10, 17]. Consequently, their application in the fixation of weight-bearing bone fractures is limited, and their safety and efficacy in TT fracture fixation remain uncertain.
In this study, 15 patients with TT fractures fixed with PLLA/HA screws achieved complete radiographic healing in an average of 12.1 weeks, which is comparable to MS fixation. No cases of nonunion, delayed healing, or refracture were observed. Patients regained full knee ROM in an average of 3.8 months, which is shorter than the 15.1–22.3 weeks reported for metal screw fixation in the literature [2, 18]. Patients returned to pre-injury activities in an average of 4.4 months, consistent with the 17.7–28.9 weeks reported for metal screw fixation in the literature [2, 12]. At the final follow-up, among the 15 patients, one experienced localized tenderness, incision numbness, joint clicking, and limited knee flexion due to heterotopic ossification of the patellar ligament at 12 months postoperatively. Another patient had extension weakness without restriction at 12 months postoperatively, and a third patient experienced joint clicking without locking at 15 months postoperatively. However, no cases of bone healing disorders, clinically significant implant degradation reactions, or growth arrest or deformities were observed. Overall, this study found that PLLA/HA screws provide reliable mechanical support for TT fracture fixation, resulting in favorable healing and rehabilitation outcomes.
Although surgical treatment generally yields favorable outcomes, the postoperative complication rate for TT fractures ranges from 18–28.3% [1, 2, 6]. Among these, irritation related to protruding MS was the most common, accounting for 68.4–73.7% of all complications [2, 5, 6]. Haber et al. reported that 44% of surgically treated patients experienced symptoms of hardware protrusion or irritation [4]. While countersinking MS theoretically addresses this issue, its clinical application has not been widely adopted [4, 19, 20]. This is mainly because adolescents with growth potential may still require implant removal due to growth arrest or deformities, screw breakage, or personal preference [21]. The countersunk design can lead to screw heads being encapsulated by callus, which complicates removal and increases the risk of iatrogenic injury. However, in the clinical application of BS, techniques have been introduced to avoid hardware protrusion. These include countersinking the hole for the screw head into the cortical bone or trimming the excess part of the screw head with a small oscillating saw [10]. This study found that embedding the heads of PLLA/HA screws into the cortical bone can effectively alleviate irritation symptoms caused by hardware protrusion. The incidence of irritation symptoms in the MS group was 41.2%, which is consistent with the literature-reported rates ranging from 6–44% [1, 2, 4–6]. In contrast, the incidence of irritation symptoms in the BS group was significantly lower, which is only 6.7%. Among the 15 patients, one case exhibited residual tenderness at the implant site caused by screw head irritation within 6 months postoperatively. Physical examination revealed no erythema or fluctuant papules, and radiographs showed no signs of osteolysis [16, 22]. The symptoms resolved spontaneously over the 12-month follow-up. Additionally, while the literature reports that 2-5% of patients may develop limb length discrepancy or genu recurvatum at 8–13 months postoperatively [2, 4, 13], none of the 15 patients in this study exhibited growth arrest or deformities. Accumulation of degradation products beyond the tissue’s clearance capacity will cause foreign body reactions. However, surgeons can reduce the adverse reactions by avoiding malvascularisation and reducing the surface area of the implant [16, 23]. The proximal tibia, with its abundant cancellous bone and vasculature, provides a robust blood supply and efficient absorption capacity for degradation fragments. Furthermore, this study demonstrated that the use of an average of 3.2 PLLA/HA screws did not result in any clinically or radiologically significant foreign body reactions during an average follow-up period of 39.4 months. However, Böstman OM et al. [16] reported that PLLA implants degrade slowly, with polymer residues detectable up to 57 months post-implantation, and a 0.2% incidence of foreign body reactions occurring 4–5 years after surgery. Additionally, Drogset JO et al. [24] and Warden WH et al. [25] noted that MRI findings indicate PLLA implants can be fully absorbed within 7–10 years post-implantation, though residual intraosseous cavities or fluid collections may persist without clinical symptoms. In conclusion, the necessity of long-term follow-up should be emphasized.
The reoperation rate following TT fracture treatment can be as high as 19-57%, with most of these procedures involving implant removal [1, 4]. The risks associated with implant removal, including hardware damage or retention, nerve or vascular injury, wound healing disturbances and infection, should not be underestimated. Preventing the need for removal can help avoid these complications and reduce secondary physical and psychological trauma [26, 27]. The use of PLLA/HA screws, with their countersinking technique and inherent favorable biodegradability, effectively minimizes the risk of hardware protrusion or irritation, thereby reducing the need for secondary removal surgeries.
Recent literature recommends immobilization of TT fracture with a long-leg cast or brace for 3–4 weeks postoperatively, followed by gradual initiation of knee joint functional exercises [3, 18]. Compared to BS, fixation with MS are more likely to result in hardware protrusion or irritation. Phillips et al. suggested that discomfort caused by such complications may reduce the patient’s willingness and ability to perform knee joint functional exercises [28]. Accordingly, this study found that the time required to regain full knee ROM after fixation with MS (5.2 months) was significantly longer than with BS (3.8 months). Additionally, Reahl et al. indicated that the timing of discontinuing knee immobilization and initiating functional exercises after tibial plateau fracture surgery is a risk factor for knee stiffness [29]. In this study, patients with metal screw fixation showed poorer adherence to functional exercises, with a resulting knee flexion range that did not reach the level of the uninjured side in 35.3% of patients at the final follow-up. Although the incidence observed in this study exceeds the 14.4% of flexion loss reported by Arkader A et al. [12], a knee flexion of 120° is adequate for virtually all activities of daily living [18]. Moreover, this study found that the restricted range of flexion could be partially alleviated after screw removal, further underscoring the negative impact of MS fixation on the ROM recovery. In conclusion, this study suggests that fixation with BS indirectly enhances the speed and level of joint functional recovery by reducing hardware protrusion or irritation. Greater mobility or faster recovery of functional status in daily activities can minimize the negative impact of injuries on families [18].
This study has several limitations. Firstly, as a single-center retrospective study, the fixation method was chosen based on the surgeon’s preference and the guardian’s wishes. The diagnostic and treatment strategies implemented by different surgeons were not strictly uniform, which might potentially influence the final results. Future prospective studies are therefore needed. Secondly, power analysis shows that for the proportions of hardware irritation and range of motion loss, sample size of 28 in both the BS and MS groups would provide greater than 0.8 power to detect differences between the group proportions. The sample size in this study is limited, and larger cohorts are required to provide validation and support for the conclusions. Lastly, while patients were followed up in the outpatient clinic until fracture healing and activity resumption, subsequent follow-up was conducted by phone. This reliance on patient-reported discomfort, in the absence of physical examinations or imaging studies, may result in an underestimation of potential long-term subclinical complications, highlighting the necessity of continued monitoring of long-term outcomes.
Conclusions
Both BS made of PLLA and MS made of titanium alloy are safe and effective for the fixation of TT fractures. However, compared to MS, BS, through countersinking of the screw heads, can effectively prevent hardware irritation, facilitate earlier recovery of knee joint ROM, reduce the incidence of joint stiffness, and eliminate the need for secondary removal surgery. Therefore, the results of this study advocate for the preferential use of PLLA-based BS for the fixation of TT fractures in adolescents.
Acknowledgements
Not applicable.
Abbreviations
- TT
Tibial tubercle
- MS
Metallic screw
- BS
Bioabsorbable screw
- ROM
Range of motion
Author contributions
CT: Conceptualization, Methodology, Investigation, Writing-Original Draft. WYW: Conceptualization, Methodology, Investigation. ZDJ: Resources, Writing-Review & Editing, Supervision. FW: Resources. SBJ: Resources. WQ: Resources, Writing-Review & Editing, Supervision. All authors reviewed the manuscript.
Funding
Not applicable.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study adhered to the principles of the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) of Beijing Children’s Hospital ([2023]-E-179-R), which waived the need for consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kalifis G, Marin Fermin T, Seil R, et al. Tibial tubercle fractures are sports injuries in male adolescents with a considerable risk of complications and reoperations: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2023;31(7):2624–34. [DOI] [PubMed] [Google Scholar]
- 2.Pretell-Mazzini J, Kelly DM, Sawyer JR, et al. Outcomes and complications of tibial tubercle fractures in Pediatric patients: a systematic review of the literature. J Pediatr Orthop. 2016;36(5):440–6. [DOI] [PubMed] [Google Scholar]
- 3.Cole WW 3rd, Brown SM, Vopat B, et al. Epidemiology, diagnosis, and management of tibial tubercle avulsion fractures in adolescents. JBJS Rev. 2020;8(4):e0186. [DOI] [PubMed] [Google Scholar]
- 4.Haber DB, Tepolt FA, McClincy MP, et al. Tibial tubercle fractures in children and adolescents: a large retrospective case series. J Pediatr Orthop B. 2021;30(1):13–8. [DOI] [PubMed] [Google Scholar]
- 5.Reyes CD, Wu W, Pandya NK. Adolescent tibial tubercle fracture: review of outcomes and complications. Curr Rev Musculoskelet Med. 2023;16(9):392–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jardaly A, Conklin M, Ashley P, et al. Closed reduction in the treatment of tibial tubercle fractures. Injury. 2021;52(6):1336–40. [DOI] [PubMed] [Google Scholar]
- 7.Xie Y, Cai L, Deng Z, et al. Absorbable screws Versus Metallic screws for Distal Tibiofibular Syndesmosis injuries: a Meta-analysis. J Foot Ankle Surg. 2015;54(4):663–70. [DOI] [PubMed] [Google Scholar]
- 8.May H, Alper Kati Y, Gumussuyu G, et al. Bioabsorbable magnesium screw versus conventional titanium screw fixation for medial malleolar fractures. J Orthop Traumatol. 2020;21(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang B, Yang M, Kou Y, et al. Absorbable implants in sport medicine and arthroscopic surgery: a narrative review of recent development. Bioact Mater. 2023;31:272–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rokkanen PU, Böstman O, Hirvensalo E, et al. Bioabsorbable fixation in orthopaedic surgery and traumatology. Biomaterials. 2000;21(24):2607–13. [DOI] [PubMed] [Google Scholar]
- 11.Greenhagen RM, Johnson AR, Joseph A. Internal fixation: a historical review. Clin Podiatr Med Surg. 2011;28(4):607–18. [DOI] [PubMed] [Google Scholar]
- 12.Arkader A, Schur M, Refakis C, et al. Unicortical fixation is sufficient for Surgical Treatment of Tibial Tubercle Avulsion fractures in Children. J Pediatr Orthop. 2019;39(1):e18–22. [DOI] [PubMed] [Google Scholar]
- 13.Pandya NK, Edmonds EW, Roocroft JH, et al. Tibial tubercle fractures: complications, classification, and the need for intra-articular assessment. J Pediatr Orthop. 2012;32(8):749–59. [DOI] [PubMed] [Google Scholar]
- 14.Sarraf M, Rezvani Ghomi E, Alipour S, et al. A state-of-the-art review of the fabrication and characteristics of titanium and its alloys for biomedical applications. Biodes Manuf. 2022;5(2):371–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ibrahim AM, Koolen PG, Kim K, et al. Absorbable biologically based internal fixation. Clin Podiatr Med Surg. 2015;32(1):61–72. [DOI] [PubMed] [Google Scholar]
- 16.Böstman OM, Pihlajamäki HK. Adverse tissue reactions to bioabsorbable fixation devices. Clin Orthop Relat Res. 2000;(371):216–27. [PubMed]
- 17.Zhu W, Huang J, Lu W, et al. Performance test of Nano-HA/PLLA composites for interface fixation. Artif Cells Nanomed Biotechnol. 2014;42(5):331–5. [DOI] [PubMed] [Google Scholar]
- 18.Huang K, Houlihan N, Arkader A, et al. Early knee range of Motion following Operative Treatment for Tibial Tubercle Avulsion Fractures is safe. J Pediatr Orthop. 2022;42(9):516–20. [DOI] [PubMed] [Google Scholar]
- 19.Bulut T, Gursoy M, Ertem H. Fully threaded headless compression screw versus partially threaded cancellous lag screw in medial malleolus fractures: clinical and radiological outcomes. Eur J Trauma Emerg Surg. 2021;47(1):179–85. [DOI] [PubMed] [Google Scholar]
- 20.Barnes H, Cannada LK, Watson JT. A clinical evaluation of alternative fixation techniques for medial malleolus fractures. Injury. 2014;45(9):1365–7. [DOI] [PubMed] [Google Scholar]
- 21.Loder RT, Feinberg JR. Orthopaedic implants in children: survey results regarding routine removal by the pediatric and nonpediatric specialists. J Pediatr Orthop. 2006;26(4):510–9. [DOI] [PubMed] [Google Scholar]
- 22.Böstman OM, Pihlajamäki HK. Late foreign-body reaction to an intraosseous bioabsorbable polylactic acid screw. A case report. J Bone Joint Surg Am. 1998;80(12):1791–4. [DOI] [PubMed] [Google Scholar]
- 23.Böstman O, Pihlajamäki H. Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials. 2000;21(24):2615–21. [DOI] [PubMed] [Google Scholar]
- 24.Drogset JO, Straume LG, Bjørkmo I, et al. A prospective randomized study of ACL-reconstructions using bone-patellar tendon-bone grafts fixed with bioabsorbable or metal interference screws. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):753–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Warden WH, Chooljian D, Jackson DW. Ten-year magnetic resonance imaging follow-up of bioabsorbable poly-L-lactic acid interference screws after anterior cruciate ligament reconstruction. Arthroscopy. 2008;24(3):370. [DOI] [PubMed] [Google Scholar]
- 26.Kasai T, Matsumoto T, Iga T, et al. Complications of implant removal in ankle fractures. J Orthop. 2019;16(3):191–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raney EM, Freccero DM, Dolan LA, et al. Evidence-based analysis of removal of orthopaedic implants in the pediatric population. J Pediatr Orthop. 2008;28(7):701–4. [DOI] [PubMed] [Google Scholar]
- 28.Phillips R, Hilton C, Sousa Filho LF et al. Behaviour change and rehabilitation adherence in adults with tendinopathy: a scoping review. Disabil Rehabil Published Online Febr 29, 2024. [DOI] [PubMed]
- 29.Reahl GB, Marinos D, OʼHara NN, et al. Risk factors for knee stiffness surgery after Tibial Plateau fracture fixation. J Orthop Trauma. 2018;32(9):e339–43. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.