Abstract
Blunt trauma is a common cause of renal injuries, usually managed conservatively unless there's hemodynamic instability, which warrants surgery. We present a case of a 22-year-old male with isolated Grade 5 renal injury, diagnosed via CT scan after blunt trauma. Despite the severity, he was successfully treated without surgery through conservative management in the ICU, with frequent monitoring and stabilization of his condition. While the best approach for hemodynamically stable Grade 5 renal injuries remains debated, our case suggests that conservative management is a viable option when patients are carefully monitored for any signs of instability.
Keywords: Conservative management and grade 5 renal injury
1. Introduction
Renal trauma is rare and occurs in up to 5 % of all trauma patients and at in 10 % of patients with abdominal trauma. However, the kidneys are the most injured organ in the genitourinary system.1. About 90 % of renal injuries are the result of blunt abdominal trauma, and only 2 % require surgical intervention.2.
The organ injury severity scale developed by the American Association for the Surgery of Trauma (AAST) is the most widely used classification system for traumatic renal injuries. It classifies renal trauma from grade 1 to grade 5 (AAST). This system has been prospectively validated in several studies to predict clinical outcomes and the need for surgical interventions.3.
More than 90 % of patients with renal trauma are generally managed conservatively.4 According to shared a report of Nerli et al.5 69 out of 114 patients with grade 5 renal injury were managed non-operatively, only 8 of them needed delayed surgical exploration for both renal and non-renal indication. Moreovere, Van der Wilden et al.6 reported 154 of 206 patients with grade 4 and grade 5 blunt renal injury were managed non-operatively, which was successful for 142 of 154 patients (92.2 %), and failed for 12 patients (7.8 %) with no significant difference in failure between grade 4 and 5. In contrast, most patients with Grade 4 and 5 injuries usually present with associated major injuries and consequently may require surgical intervention.7. However, the optimal management of isolated Grade 5 injuries in a hemodynamically stable patient remains controversial.8.
Although embolization or open surgery may sometimes be required with interventional radiology particularly for severe cases.2. Though there is limited evidence about the optimal management of grade 5 renal injuries, recent reports suggest conservative management can be considered as an alternative treatment option.2. Here we report a case of Grade 5 renal injury successfully managed conservatively.
1.1. Case presentation
A 22-year-old male presented to the emergency department with a complaint of severe flank pain after sustaining blunt trauma to his left flank with a large water pipe.
On examination, the patient's blood pressure was 80/40 mmHg and pulse rate was 100 beats per minute. Abdominal examination revealed ecchymosis and a tender, palpable left flank mass. The rest of the abdomen was soft and non-tender. Gross hematuria was noted during catheterization.
Immediate resuscitation was initiated with crystalloids, and a response in blood pressure to 100/70 mmHg was noted after administration of 3 L of normal saline. Laboratory examination indicated that the serum hematocrit was 48.8 %. Urinalysis showed +3 blood on dipstick.
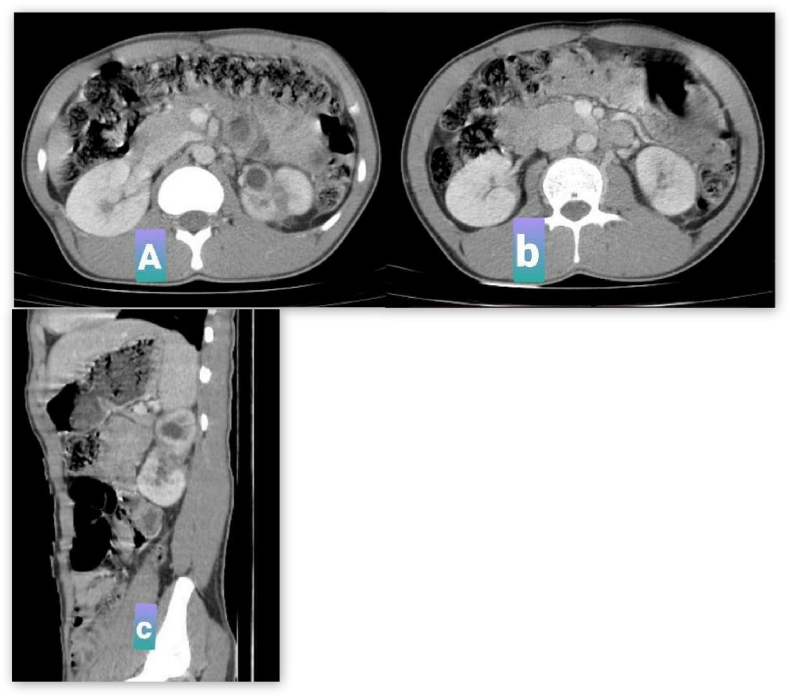
CT scan of the abdomen and pelvis showed multiple lacerations of the left Kidney, including a mid-pole full-thickness laceration dividing the upper and lower segments with huge perirenal hematoma. These findings were consistent with Grade 5 renal injury (shattered Kidney) see Fig. 1 for details.
Fig. 1.
Initial CT-scan, 1A and 1B are transverse plane, 1C: is sagittal plane, the figure shows multiple laceration of left kidney (shattered) with mid pole full thickness laceration dividing upper and lower with significant peri-renal hematoma.
The patient was counselled about the options for treatment, and the informed decision was made to proceed with conservative management. He was also informed that operative intervention could be performed at any time during the observation if deemed necessary. He was admitted to the central ICU and was placed on close observation of vital signs and fluid balance. Serum hematocrit values were checked serially. The patient had episodes of hypotension, and his initial hematocrit dropped to 38.5 % at 12 hours. He was transfused with a total of 4 units of whole blood, and his hematocrit stabilized at 32.5 % after 48 hours of presentation. Afterwards, the patient remained hemodynamically stable with no additional problems and was discharged on the 7th day.
Follow-up visits at 2 and 6 weeks were uneventful. A Follow-up CT scan done at three months showed resolution of perirenal hematoma and fusion of the upper and lower segments with mild hydronephrosis of the upper segment. No extravasation of contrast was observed see Fig. 2.
Fig. 2.
Follow up CT-scan, 2A and 2B are transverse planes which shows complete resolution of peirenal hematoma, no extravasation, there is mild hydronephrosis in the upper segment.2C is sagittal plane which shows healing of the two segments together.
2. Discussion
Blunt traumas to the Kidney are more common, accounting for up to 90 % of renal injuries. Such injuries most commonly result from motor vehicle accidents. A direct blow to the flank or abdomen is another common cause.8,9. Parenchymal contusions or lacerations are the most common injuries, whereas renal vascular injuries occur in less than 5 % of blunt abdominal trauma.3.
The presence of hematuria and hypotension are the two critical clinical signs suggestive of significant renal injury. Urinalysis showing >5 red blood cells per high power field, a positive urine dipstick, or gross hematuria raises the concern for renal injury.10,11. Nonetheless, it is important to note these findings are neither sensitive nor specific. Furthermore, there is a poor correlation between the severity of hematuria and the severity of renal injury.9. Shariat et al. reported that hematuria was absent in 7 % of Grade 4 injuries.12
CT scan remains the gold-standard imaging modality for evaluating renal trauma.3. CT imaging is sensitive and specific for demonstrating parenchymal lacerations and urinary extravasations and for determining the size and location of surrounding retroperitoneal hematoma.13. CT can also demonstrate concurrent intra-abdominal injuries to other organs and accurately identify and grade renal injury.14
The AAST classifies renal injuries into five grades of severity based on the degree of laceration and vascular injury (Table 1).6,15. Although the AAST system is primarily based on surgical findings, a CT scan demonstrates all the findings that correlate with surgical observations, providing the most definitive grading information.16,17.
Table 1.
The American Association for the Surgery of Trauma (AAST) severity scaling of renal injury.
| Grade | Type of injury | Description of injury |
|---|---|---|
| 1 | Contusion | Microscopic or gross hematuria, urologic studies normal |
| Hematoma | Non-expanding subcapsular hematoma without parenchymal laceration | |
| 2 | Hematoma | Non-expanding perirenal hematoma confirmed to renal retroperitoneum |
| Laceration | <1 cm parenchymal depth of renal cortex without urinary extravasation | |
| 3 | Laceration | >1cm parenchymal depth of renal cortex without collecting system rupture or urinary extravasation |
| 4 | Laceration | parenchymal laceration extending through renal cortex, medulla, and collecting system |
| Vascular | Main renal artery or vein injury with contained hematoma | |
| 5 | Laceration | Completely shattered kidney |
| Vascular | Avulsion of renal hilum which devascularizes kidney |
CT scan imagining is indicated in blunt abdominal trauma if there is gross hematuria or microscopic hematuria with shock (defined as systolic blood pressure <90 mmHg). In addition, a CT scan is recommended in cases suggesting underlying renal injury, such as flank ecchymosis, fracture of the lower ribs, and thoracolumbar spine, regardless of the presence or absence of hematuria.8, 9, 10. In our case, the patient presented with hypotension and gross hematuria, and CT scan imaging effectively identified the extent of renal injury.
Recent guidelines recommend conservative management in hemodynamically stable patients with Grade 1–4 renal injury following blunt trauma. In contrast, isolated Grade 5 injuries are relatively rare; thus, treatment recommendations are less clear.18,19. Historically, Grade 5 injuries were regarded as an indication for surgical exploration, leading to nephrectomy in most cases.11.
However, there is a recent paradigm shift towards conservative management. Primary conservative management is associated with a lower rate of nephrectomies without any increase in immediate or long-term morbidity.3.
Conservative management involves admission to the ICU with close follow of vital signs and serial hematocrit determination. Repeat abdominal CT-scan with delayed phase is recommended 72 hours after the initial trauma for grade 3–5 injuries.2. Our patient was successfully managed conservatively. Close monitoring of the patient and subsequent management of hemodynamic instability were crucial for optimal outcomes.3,15,.18. Our patient was successfully managed conservatively. Close monitoring of the patient and subsequent management of hemodynamic instability were crucial for optimal outcomes.
Continuing hemodynamic instability unresponsive to aggressive resuscitation due to renal hemorrhage requires surgical exploration, irrespective of the mode of injury.3. Thus, in blunt renal trauma, life-threatening renal bleeding remains the only absolute indication for surgical exploration. Relative indications include devitalized renal parenchyma (>50 %), persistent urinary extravasation unresponsive to conservative means such as ureteral stent placement or nephrostomy.9,15.
Both immediate and long-term complications of high-grade renal trauma can be significant and require follow-up.12,19. Persistent urinary extravasation with urinoma is the most common complication, occurring in 1–7% of all patients with renal trauma. However, urinary extravasation resolves spontaneously in the majority (75–85 %) of the cases.3,8. Persistent extravasation after blunt trauma often responds to the insertion of a retrograde stent and/or percutaneous nephrostomy.9,7. Hypertension is a rare complication of renal trauma occurring in 5 % of cases. The incidence is directly related to the severity of renal injury, and thus, patients with Grade 4 and 5 injuries should have periodic blood pressure monitoring in the long term.8,18.
3. Conclusion
In conclusion, clinicians should have a high index of suspicion of renal injury suspicion in any patient presenting with hematuria and hypotension following blunt trauma. CT scan is beneficial in establishing the diagnosis and assessing the extent of renal injury. Although the optimal management of hemodynamically stable isolated Grade 5 renal injury remains unclear, conservative management can be considered an option in carefully selected patients without significantly increasing the risk of complications. Close monitoring and early detection and management of hemodynamic instability are essential for optimal outcomes.
CRediT authorship contribution statement
Abdirahman Burale: Writing – review & editing, Writing – original draft, Methodology, Investigation, Data curation. Elias Sertse: Conceptualization. Solomon Bishaw: Writing – original draft, Methodology, Formal analysis. Ferid A. Abubeker: Writing – original draft, Investigation, Formal analysis, Data curation, Conceptualization. Musse Ahmed: Investigation, Formal analysis, Data curation, Conceptualization. Samatar Abshir Mohamed: Formal analysis, Data curation, Conceptualization. Hassan Sh Abdirahman Elmi: Writing – review & editing, Supervision, Conceptualization.
Consent for publication
Informed written and signed consent of publication was taken from the patient.
Funding
This research did not receive any funding
Acknowledgements
We want to express our sincere gratitude and appreciation to the residents and nurses in the surgical department.
References
- 1.Erlich T., Kitrey N.D. Renal trauma: the current best practice. Therap Adv Urol. 2018 Oct;10(10):295–303. doi: 10.1177/1756287218785828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedland S.J., Eilber K.S., Palapattu G.S., et al. Conservative management of a grade 4 renal laceration in a child. Rev Urol. 2001;3(1):40–41. winter. [PMC free article] [PubMed] [Google Scholar]
- 3.Aldiwani M., Georgiades F., Omar I., et al. Traumatic renal injury in a UK major trauma centre - current management strategies and the role of early re-imaging. BJU Int. 2019 Oct;124(4):672–678. doi: 10.1111/bju.14752. [DOI] [PubMed] [Google Scholar]
- 4.Shewakramani S., Reed K.C. Genitourinary trauma. Emerg Med Clin North Am. 2011 Aug;29(3):501–518. doi: 10.1016/j.emc.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 5.Nerli R.B., Sharma V., Kajagar B.M., et al. Grade V renal injury – short and long term outcome. Open J Trauma. 2017 Mar;13(1):20–25. doi: 10.17352/ojt.000005. 1. [DOI] [Google Scholar]
- 6.Van der Wilden G.M., Velmahos G.C., D'Andrea K.J., et al. Successful nonoperative management of the most severe blunt renal injuries: a multicenter study of the research consortium of New England Centers for Trauma. JAMA Surg. 2013 Oct;148(10):924–931. doi: 10.1001/jamasurg.2013.2747. [DOI] [PubMed] [Google Scholar]
- 7.Long J.A., Fiard G., Descotes J.L., et al. High-grade renal injury: non-operative management of urinary extravasation and prediction of long-term outcomes. BJU Int. 2013 Apr;111(4 Pt B):E249–E255. doi: 10.1111/j.1464-410x.2012.11578.x. [DOI] [PubMed] [Google Scholar]
- 8.Chouhan J.D., Winer A.G., Johnson C., et al. Contemporary evaluation and management of renal trauma. Can J Urol. 2016 Apr;23(2):8191–8197. [PubMed] [Google Scholar]
- 9.Brandes S.B., McAninch J.W. Renal trauma: a practical guide to evaluation and management. Sci World J. 2004;4(S1):31–40. doi: 10.1100/tsw.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris A.C., Zwirewich C.V., Lyburn I.D., et al. Ct findings in blunt renal trauma. Radiographics. 2001 Oct;21(Suppl_1):S201–S214. doi: 10.1148/radiographics.21.suppl_1.g01oc07s201. [DOI] [PubMed] [Google Scholar]
- 11.Santucci R.A., McAninch J.W. Diagnosis and management of renal trauma: past, present, and future. J Am Coll Surg. 2000 Oct;191(4):443–451. doi: 10.1016/s1072-7515(00)00695-5. [DOI] [PubMed] [Google Scholar]
- 12.Shariat S.F., Jenkins A., Roehrborn C.G., et al. Features and outcomes of patients with grade IV renal injury. BJU Int. 2008 Sep;102(6):728–733. doi: 10.1111/j.1464-410x.2008.07638.x. ; discussion 733. [DOI] [PubMed] [Google Scholar]
- 13.Sancak E.B., Resorlu M., Akbas A., et al. Isolated Grade 5 Kid Injury Due Anim Attack. Case Rep Int J Nephrol Kidney Failure. 2016;2(2) doi: 10.16966/2380-5498.127. [DOI] [Google Scholar]
- 14.Chong S.T., Cherry-Bukowiec J.R., Willatt J.M., et al. Renal trauma: imaging evaluation and implications for clinical management. Abdom Radiol (NY) 2016 Aug;41(8):1565–1579. doi: 10.1007/s00261-016-0731-x. [DOI] [PubMed] [Google Scholar]
- 15.Erlich T., Kitrey N.D. Renal trauma: the current best practice. Ther Adv Urol. 2018 Oct;10(10):295–303. doi: 10.1177/1756287218785828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alonso R.C., Nacenta S.B., Martinez P.D., et al. Kidney in danger: CT findings of blunt and penetrating renal trauma. Radiographics. 2009 Nov;29(7):2033–2053. doi: 10.1148/rg.297095071. [DOI] [PubMed] [Google Scholar]
- 17.Dayal M., Gamanagatti S., Kumar A. Imaging in renal trauma. World J Radiol. 2013 Aug;5(8):275–284. doi: 10.4329/wjr.v5.i8.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bryk D.J., Zhao L.C. Guideline of guidelines: a review of urological trauma guidelines. BJU Int. 2016 Feb;117(2):226–234. doi: 10.1111/bju.13040. [DOI] [PubMed] [Google Scholar]
- 19.Tait C.D., Somani B.K. Renal trauma: case reports and overview. Case Rep Urol. 2012;2012(1) doi: 10.1155/2012/207872. [DOI] [PMC free article] [PubMed] [Google Scholar]