Abstract
Background
Over 300 therapies have been proposed for premenstrual syndrome. To date there has been only one survey conducted in the UK of PMS treatments prescribed by GPs, a questionnaire-based study by the National Association of Premenstrual Syndrome in 1989. Since then, selective serotonin re-uptake inhibitors have been licensed for severe PMS/PMDD, and governmental recommendations to reduce the dosage of vitamin B6 (the first choice over-the-counter treatment for many women with PMS) have been made. This study investigates the annual rates of diagnoses and prescribing patterns for premenstrual syndrome (1993–1998) within a computerised general practitioner database.
Methods
Retrospective survey of prescribing data for premenstrual syndrome between 1993–1998 using the General Practice Research Database for the West Midlands Region which contains information on 282,600 female patients
Results
Overall the proportion of women with a prescription-linked diagnosis of premenstrual syndrome has halved over the five years. Progestogens including progesterone were the most commonly recorded treatment for premenstrual syndrome during the whole study period accounting for over 40% of all prescriptions. Selective serotonin-reuptake inhibitors accounted for only 2% of the prescriptions in 1993 but rose to over 16% by 1998, becoming the second most commonly recorded treatment. Vitamin B6 accounted for 22% of the prescriptions in 1993 but dropped markedly between 1997 and 1998 to 11%.
Conclusions
This study shows a yearly decrease in the number of prescriptions linked to diagnoses for premenstrual syndrome. Progestogens including progesterone, is the most widely prescribed treatment for premenstrual syndrome despite the lack of evidence demonstrating their efficacy.
Background
It is estimated that between 85% to 97% of women of reproductive age experience some symptoms in the premenstrual phase of the cycle and about 30–40% of these women will seek help from their GP [1]. Premenstrual syndrome is defined as the recurrence of adverse physical and behavioural symptoms which recur in the luteal phase and which remit during, or after, menstruation; the symptoms are severe enough to significantly disrupt every day life for 3–5% of women [2]. The underlying cause of premenstrual syndrome remains unclear and speculative; many hypotheses have been suggested and numerous treatments advanced. The uncertainty as to the aetiology of premenstrual syndrome coupled with the very high placebo response has resulted in a large number of claims for potential therapies. There have been as many as 327 different treatments for premenstrual syndrome [3]. The variety of treatment approaches include hormonal preparations (oestrogen, oral contraceptives, GnRH analogues, danazol, progestogens and progesterone), diuretics, antidepressants, nutritional therapies (vitamin B6, mineral supplements and evening primrose oil), bromocriptine, surgery, complementary therapy and more recently light therapy and psychotherapy (cognitive and behavioural therapy) [4].
Despite this wide range of possible therapies for premenstrual syndrome no recent information concerning prescribing habits for premenstrual syndrome has been conducted in the UK. A survey of 658 women with self-reported PMS by Corney and Stanton [5] in 1990 found that vitamin B6 was the most widely used treatment, followed by evening primrose oil and then hormonal preparations. A similar survey of 220 women with self-reported PMS in the US found that dietary supplements and exercise were the most frequently suggested treatment option followed by progesterone and pain relievers [1]. Another recent survey found that of the 31% of women who reported severe premenstrual symptoms less than half sought any help for their condition. One of the reasons given was the belief that no effective treatments were available. Of those who used prescription medicines, paracetamol, vitamin B6, progesterone and oral contraceptives were the most frequently used treatments in the UK [6].
However, whilst these studies provide valuable information on what women are using to gain relief for their symptoms this does not necessarily reflect what General Practitioners are prescribing for this syndrome. A survey of diagnostic and treatment practices of US and Canadian primary care physicians reported in 1984 found that progesterone suppositories were the most widely prescribed treatment; 70% of all the surveyed physicians prescribed progesterone [7]. The National Association for Premenstrual Syndrome in 1989 assessed the treatment practices of 273 general practitioners in the UK by questionnaire. They found that 68% of general practitioners reported prescribing vitamin B6 and over half reported that they prescribed progestogens or progesterone for premenstrual symptoms [8].
In the last three years premenstrual syndrome has gained considerable media attention. In 1997, the UK Department of Health proposed to limit the sales of vitamin B6, a very popular self-help remedy for premenstrual syndrome, because of possible neurotoxic side effects at higher doses [9]. In 1999, the Medicines Control Agency granted the selective serotonin re-uptake inhibitor, fluoxetine, a license for use in severe premenstrual syndrome/premenstrual dysphoric disorder. This was the first time a licence has been granted specifically for premenstrual dysphoric disorder. There has also been heavy media and Internet promotion of 'natural' topical progesterone creams for PMS [10].
One of the issues highlighted in the 1989 UK postal survey of general practitioners [8] was the wide variety of treatments used by GPs to manage premenstrual syndrome. In order to determine current prescribing patterns, we used the General Practitioner Research Database (which records prescribing patterns and referrals) for the years 1993–1998 to identify prescriptions associated with the diagnosis of premenstrual syndrome.
Methods
The General Practitioner Research Database (GPRD) is an UK database, which records prescribing data and referrals and provides a valuable resource for analysing prescribing patterns. Anonymised records of individual patients are allocated a unique patient number. Data on medical events, patient problems and other doctor-patient interventions are captured in the database through the OXMIS (Oxford Medical Information System) dictionary. The OXMIS dictionary is an amalgamation of the eighth revision of the International Classification of Diseases (ICD-8) and the surgical operation codes used by the Office of National Statistics. During 1998 some practices started using Read codes. The Read codes were developed by James Read in the early 1980s to enable GPs to code and record relevant information from a patient encounter. Read codes are cross-referenced to the main national and international classifications. General Practitioners who provide data for the database have agreed to record the information in a standard manner to permit its use in research. The General Practitioner Research Database for the West Midlands former region contains 33 million records for prescribing or diagnosis for a population of 612 700 patients. The age sex profile of the patients for the West Midlands region matches that of England and Wales and represents 10% of the UK population [11].
For individual patient records, a gynaecologist (PMSOB) and a researcher (KW) reviewed the OXMIS and Read codes to select the codes which define premenstrual syndrome. Table 1 details the General Practice Research Database diagnoses used to identify premenstrual syndrome. All diagnoses of premenstrual syndrome with same-day prescriptions were extracted from the General Practice Research Database.
Table 1.
GPRD diagnoses for PMS
| OXMIS | 6269a | Tension premenstrual |
| 6269f | Syndrome premenstrual | |
| 6269mt | Tension menstrual | |
| READ | k584.00 | Premenstrual tension syndrome |
| k584.11 | Migraine menstrual |
Prescriptions were linked to diagnoses by patient identifier, date of prescription and diagnosis. Prescription rates for premenstrual syndrome were calculated for 1993–1998 (the prescription rate is defined as the number of prescriptions for a specific drug group linked to a diagnosis of premenstrual syndrome, divided by the total number of prescriptions linked to diagnosis of premenstrual syndrome for that year). Prescriptions were identified as either repeat or acute and were determined for each drug group.
The Medicines Control Agency was contacted for a list of drugs, which have been licensed for premenstrual syndrome, premenstrual tension, premenstrual mastalgia, premenstrual oedema or premenstrual dysphoric disorder. The British National Formulary (BNF March 2001) and Monthly Index of Medical Specialities (MIMS; October 2000) and the Compendium of Datasheets (1999–2000) were searched for indicated treatments for the same disorders. Any identified treatment indicated for premenstrual symptoms was subsequently cross-checked in the other publications.
Table 2: (see Additional File) shows the list of drugs which have either been licensed for premenstrual symptoms or which appear in the data sheet compendium, MIMS or the BNF as indicated for premenstrual symptoms.
Statistical analysis
The yearly trends in prescribing for the individual drugs were analysed using Armitage trend test, P < 0.05 was considered to be significant [12]. Armitages trend test is used when one wishes to compare proportions between groups where the groups are ordered, to establish whether there is an upward or downward trend in the proportions. Here the ordered groups are years and the data was analysed to determine whether the proportion of prescriptions linked to diagnoses of PMS is increasing or decreasing over time.
Results
A total of 5,891 women were diagnosed with premenstrual syndrome between 1993–8 and issued with 6,172 same-day prescriptions. Table 3 shows the rate of diagnosis of premenstrual syndrome fell from 0.92% (of the total female population in the West Midlands GPRD) in 1993 to 0.42% in 1998. The rate of prescribing fell from 1.01% to 0.67%. Prescribing fell for all the British National Formulary sub-groups except selective serotonin reuptake inhibitors.
Table 3.
Rates of diagnosis of premenstrual syndrome
| Year | Number of diagnoses | Number of same day prescriptions | Female population (GPRD) | % diagnoses | % same day prescriptions |
| 93 | 1533 | 1688 | 166845 | 0.92 | 1.01 |
| 94 | 1231 | 1325 | 172003 | 0.72 | 0.77 |
| 95 | 1178 | 1230 | 182204 | 0.65 | 0.68 |
| 96 | 863 | 861 | 131226 | 0.66 | 0.66 |
| 97 | 645 | 667 | 121754 | 0.53 | 0.55 |
| 98 | 441 | 401 | 105571 | 0.42 | 0.38 |
| 93–98 | 5891 | 6172 | 879602 | 0.67 | 0.70 |
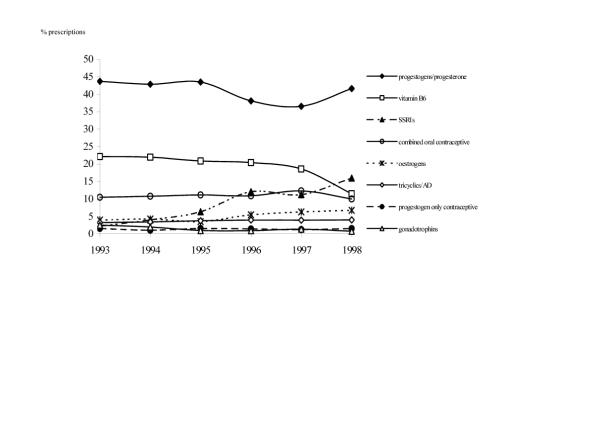
Figure 1 shows the rates of prescribing for the individual drug groups for 1993–1998. There was a significant downward trend (P < 0.05) in the prescription rates for vitamin B6, progesterone and progestogens and gonadotrophins and a significant upward trend over the study period for selective serotonin reuptake inhibitors. During the study period progestogens (including progesterone) were the most widely prescribed treatment comprising 44% in 1993 and still accounted for 42% of all prescriptions in 1998. There were significantly more prescriptions for progesterone and progestogens over the five-year period than any other drug type (P < 0.05). The most marked increase in prescriptions over the study period was for selective serotonin reuptake inhibitors; they represented only 2% of all prescriptions for premenstrual syndrome in 1993 but by 1998 accounted for 16% of all prescriptions. Similarly, the most marked fall in prescriptions was for prescriptions of vitamin B6 which fell from 22% in 1997 (the second most frequent prescription) to 11% in 1998.
Figure 1.
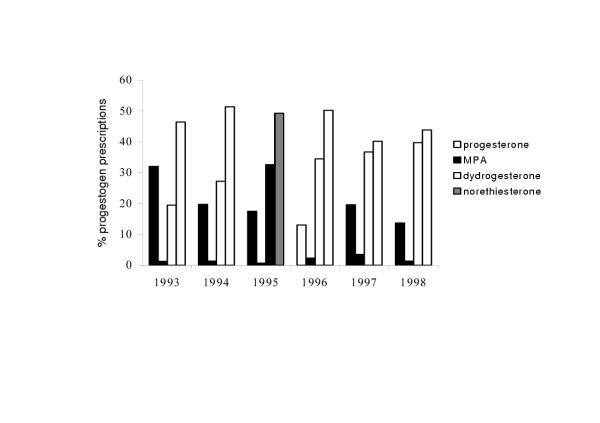
Figure 2 shows a detailed yearly breakdown of the different treatments, which make up the progestogen/progesterone category. There was a significant drop in the level of prescriptions for progesterone (32% in 1993; 14% in 1998 of prescriptions in this category) and a corresponding increase in the number of prescriptions for dydrogesterone (19% in 1993; 40% in 1998). Prescriptions for norethisterone remained nearly constant accounting for approximately 45% of all progestogen and progesterone prescriptions. There were very few prescriptions of medroxyprogesterone acetate for premenstrual syndrome during this study period (1–4%). Of the progesterone prescriptions all were for Cyclogest® which is progesterone administered as a suppository or pessary. There were no recorded prescriptions for Crinone®, the vaginal progesterone gel or for Gestone® (progesterone administered by injection). Natural progesterone is not recorded, as is it not a prescription medicine.
Figure 2.
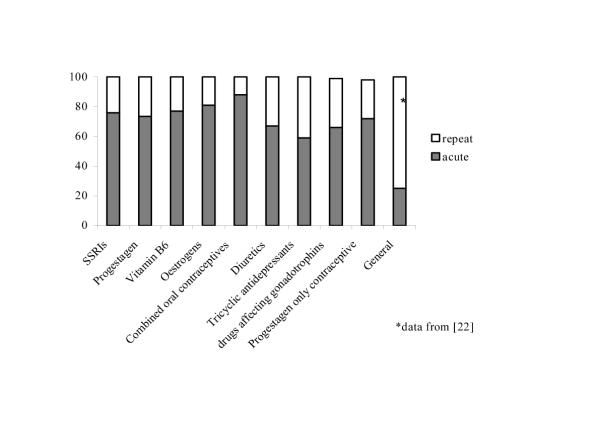
The proportions of repeat and acute prescriptions were determined for each drug group over the study period. The proportions could provide an indication of whether the women perceive the treatment to be efficacious; the greater the number of repeat prescriptions, then presumably the more successful the treatment is perceived as being. The variation in the ratio of repeat and acute prescriptions remained consistent across the study period for each group of drugs apart from diuretics. (The only significant difference in the number of acute and repeat prescriptions over time was for the subgroup of diuretics which showed a significant increase in the number of repeat prescriptions over the study period). However, there was some variation in the ratio of acute and repeat prescriptions when the yearly proportions of acute and repeat prescriptions for the individual drug groups were compared. Figure 3 shows the proportions of new and repeat prescriptions for the individual drug groups for 1996. Prescriptions linked to the diagnosis of premenstrual syndrome for tricyclic antidepressants were most likely to be repeated whereas prescriptions for oral contraceptives were the least likely to be repeated. Figure 3 also shows the general proportions of acute and repeat prescriptions, taken from reference [22].
Figure 3.
Discussion
There is a vast array of suggested treatments for premenstrual syndrome. The purpose of this study was to look at the diagnoses and associated prescription rates for the various medical treatment options for women presenting at a general practice with premenstrual syndrome
This study has revealed a surprising drop in the number of prescription-linked diagnoses of premenstrual syndrome. It is not immediately apparent why fewer women are being diagnosed with premenstrual syndrome, particularly as an analysis of the OXMIS code for another menstrual cycle disorder, heavy bleeding, showed that this diagnosis has remained relatively constant over the same period. A possible explanation is the recent increase in popularity of alternative, non-prescription treatments for premenstrual syndrome. A survey of medical herbalists in 1998 showed that the second most commonly treated condition was premenstrual syndrome [13]. It is therefore feasible that women are experiencing sufficient relief from these non-prescription treatments such that they no longer seek medical intervention.
A recent meta analysis of progesterone and progestogens has shown that neither treatment is efficacious in the management of PMS [14], however it is not surprising that progesterone and progestogens are the most commonly prescribed treatment for premenstrual syndrome. Dalton, who has been largely responsible for premenstrual syndrome becoming a recognised disorder, has enthusiastically advocated progesterone as a successful treatment for many years [15]. Progesterone is available in the UK, on prescription, as a pessary or suppository, vaginal gel or injection. Oral micronised progesterone is available in mainland Europe and the United States but not in the UK. Progestogens, synthetic analogues of progesterone, have been developed as oral preparations of progesterone. Of the progesterone preparations only Cyclogest®, (progesterone pessary/suppository) has a license for PMS in the UK. Dydrogesterone, norethisterone and an ethinyloestradiol/levonorgestrel combination (Ovranette®), all have a license for PMS (Table 2: see Additional File). Medroxyprogesterone acetate does not have a licence and is not recommended for PMS in MIMS, BNF or the drug datasheets and this could account for its low prescription rate, (less than 3% of the total hormonal prescriptions (figure 2)), although it has been trialed as a treatment for premenstrual syndrome [16].
The steady increase in the proportion of prescriptions of selective serotonin re-uptake inhibitors is in agreement with an overall increase in the number of prescriptions for this type of drug for other indications [17]. We anticipate this increase to continue as fluoxetine received a license for the treatment of severe premenstrual syndrome/premenstrual dysphoric disorder in 1999, and a recent meta analysis has shown it to be a highly effective treatment for this disorder [18].
It is possible that the sudden drop in vitamin B6 prescriptions from 19% in 1997 to 11% in 1998 results from proposals from the UK Department of Health to restrict the dosage available because of potential, although reversible, neurotoxic effects at very high doses [19].
Research into potential treatments for premenstrual syndrome has been restricted by the lack of accurate diagnostic techniques of the disorder in the study population. It is now widely accepted that the diagnosis of premenstrual syndrome can only be obtained through the structured evaluation of 1–3 months of prospective symptom recording and with the exclusion of any underlying psychiatric or medical disorder. Recent trials for premenstrual syndrome/premenstrual dysphoric disorder are conducted using these strict diagnostic criteria and therefore any reported efficacy can be considered to be proven for a woman with premenstrual syndrome. In practice this is not the same population that presents with the complaint of premenstrual syndrome. It has been estimated that between 25–75% of women who present with premenstrual syndrome actually have another medical condition [20]. The lack of suitable, easy to administer, diagnostic tools mean that virtually all diagnoses of premenstrual syndrome are made by self-assessment and up to half of these self-assessments have been shown to be incorrect [21]. This high level of incorrect assessment coupled with the known high placebo response [22] has probably resulted in the widespread use of inappropriate treatments and the inappropriate licensing of certain treatments. It is interesting that the number of repeat prescriptions for any drug group is so low in this study. A recent study estimated that repeat prescriptions generally account for 75% of all prescriptions [23]. The highest proportion of repeat prescriptions in this study was 50%, which was the proportion of repeat prescriptions for tricyclic antidepressants in 1997. It is possible that the lack of correct diagnosis and the failure to exclude other medical disorders are reflected in a low number of successful treatments and thus, repeat prescriptions.
An obvious limitation of this study is that premenstrual syndrome may be entered under a different diagnostic code to these searched on. There is frequent confusion in the clinical situation between premenstrual syndrome and other gynaecological disorders such as, dysmenorrhoea and the perimenopause, and in psychological disorders such as depression or anxiety. Similarly, this study can only reflect on what women are being prescribed and there is a large amount of evidence to suggest that most women with premenstrual syndrome will, at least initially, self-medicate [1,6,8].
Despite the recent concerns surrounding the interpretation of data from the General Practitioner Research Database [24], it remains a unique resource for providing information on the number of diagnoses and prescribing patterns for many disorders including premenstrual syndrome. This study has highlighted a dramatic drop in the number of women being given a diagnosis of premenstrual syndrome. It has also demonstrated the wide range of therapeutic techniques, which are currently being used in the management of this disorder. The development of effective treatments for premenstrual syndrome has been hampered by imprecise diagnostic standards, poorly controlled trials and the promotion of therapies which lack scientific support. We believe that the evidence for all possible treatment options for premenstrual syndrome should be assessed by critical appraisal and meta analysis to permit definitive statements to be made on the most efficacious management of premenstrual symptoms. Whilst this statement is true for all disorders, premenstrual syndrome treatments in particular highlight the result of prescribing practice based on inappropriate evidence.
Conclusions
• Prescription linked diagnoses of premenstrual syndrome fell four fold over the study period (1993–1998)
• Progestagens including progesterone are the most widely prescribed treatment for premenstrual syndrome
• Vitamin B6 was the second most frequently recorded prescription in 1993 but prescriptions halved between 1997 and 1998
• Prescriptions for selective serotonin re-uptake inhibitors increased dramatically between 1993 and 1998 and were the second most frequently prescribed treatment in 1998
• Significantly more prescriptions for all drug groups were acute rather than repeat, in contrast to other disorders.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Table 2
Contributor Information
Katrina M Wyatt, Email: k.m.wyatt@ex.ac.uk.
Paul W Dimmock, Email: oga03@keele.ac.uk.
Martin Frischer, Email: m.frischer@keele.ac.uk.
Paul W Jones, Email: p.w.jones@maths.keele.ac.uk.
Shaugn PM O'Brien, Email: sharoncammillare@hotmail.com.
References
- Kraemer GR, Kraemer RR. Premenstrual syndrome: diagnosis and treatment experiences. J Womens Health. 1998;7:893–907. doi: 10.1089/jwh.1998.7.893. [DOI] [PubMed] [Google Scholar]
- Johnson SR. Premenstrual syndrome therapy. Clin Obstet Gynecol. 1998;41:405–421. doi: 10.1097/00003081-199806000-00022. [DOI] [PubMed] [Google Scholar]
- Chakmakjian ZH. A critical assessment of therapy for the premenstrual tension syndrome. J Reprod Med. 1983;28:532–538. [PubMed] [Google Scholar]
- Wyatt KM, Dimmock PW, O'Brien PMS. Premenstrual syndrome. Clinical Evidence BMJ Publishing Group. 2000;Issue 4:1121–1133. [Google Scholar]
- Corney RH, Stanton R. A survey of 658 women who report symptoms of premenstrual syndrome. J Psychosom Res. 1991;35:471–482. doi: 10.1016/0022-3999(91)90042-M. [DOI] [PubMed] [Google Scholar]
- Hylan TR, Sundell K, Judge R. The impact of premenstrual symptomatology on functioning and treatment-seeking behavior: Experience from the United States, United Kingdom, and France. J Women's Health Gend Based Med. 1999;8:1043–1052. doi: 10.1089/jwh.1.1999.8.1043. [DOI] [PubMed] [Google Scholar]
- Lyon KE, Lyon MA. The premenstrual syndrome. A survey of current treatment practices. J Reprod Med. 1984;29:705–711. [PubMed] [Google Scholar]
- Stewart A. A rational approach to treating premenstrual syndrome. A women's nutritional advisory service publication for the National Association of Premenstrual Syndrome. 1989.
- Joint Food Safety and Standards Group. Survey of dietary supplements containing vitamin B6. London: Ministry of Agriculture Fisheries and Food. 1997.
- Lee JR. Natural progesterone. The multiple roles of a remarkable hormone Sebastopol, California: BLL Publishing. 1995.
- Hollowell J. The general practice research database: quality of morbidity data. Population Trends. 1997;87:36–40. [PubMed] [Google Scholar]
- Altman D. Practical Statistics for Medical Research. Chapman and Hall London.
- Barnes J, Ernst E. Traditional herbalists' prescriptions for common clinical conditions: A survey of members of the UK National Institute of Medical Herbalists. Phytotherapy Research. 1998;12:369–371. doi: 10.1002/(SICI)1099-1573(199808)12:5<369::AID-PTR304>3.3.CO;2-#. [DOI] [Google Scholar]
- Wyatt KM, Dimmock PW, Jones P, Obhrai M, O'Brien PMS. Efficacy of progesterone and progestogens a systematic review of their efficacy in the management of premenstrual syndrome. BMJ. 2001;323:776–780. doi: 10.1136/bmj.323.7316.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton K. The Premenstrual syndrome and progesterone therapy. 2nd Ed Chicago IL Year Book Medical Publisher. 1984.
- West CP. Inhibition of ovulation with oral progestins-effectiveness in premenstrual syndrome. Eur J Obstet Gynecol Reprod Biol. 1990;34:119–128. doi: 10.1016/0028-2243(90)90015-s. [DOI] [PubMed] [Google Scholar]
- Lawrenson RA, Tyrer F, Newson RB, Farmer RD. The treatment of depression in UK general practice: selective serotonin reuptake inhibitors and tricyclic antidepressants compared. J Affect Disord. 2000;59:149–57. doi: 10.1016/S0165-0327(99)00147-0. [DOI] [PubMed] [Google Scholar]
- Dimmock PW, Wyatt KM, Jones PW, O'Brien PMS. Efficacy of selective serotonin-reuptake inhibitors in premenstrual syndrome: a systematic review. Lancet. 2000;356:1131–1136. doi: 10.1016/S0140-6736(00)02754-9. [DOI] [PubMed] [Google Scholar]
- Wyatt KM, Dimmock PW, Jones PW, O'Brien PMS. Efficacy of vitamin B-6 in the treatment of premenstrual syndrome: systematic review. BMJ. 1999;318:1375–1381. doi: 10.1136/bmj.318.7195.1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortola JF. Issue in the diagnosis and research or premenstrual syndrome. Clin Obstet Gynecol. 1992;35:658–678. [Google Scholar]
- Plouffe L, Stewart K, Craft KS, Maddox MS, Rausch JL. Diagnostic and treatment results from a southeastern academic center-based premenstrual syndrome clinic: The first year. Am J Obstet Gynecol. 1993;169:295–307. doi: 10.1016/0002-9378(93)90079-x. [DOI] [PubMed] [Google Scholar]
- Freeman EW, Rickels K. Characteristics of placebo responses in medical treatment of premenstrual syndrome. Am J Psychiatry. 1999;156:1403–1408. doi: 10.1176/ajp.156.9.1403. [DOI] [PubMed] [Google Scholar]
- Harris CM, Dajda R. The scale of repeat prescribing. Br J Gen Pract. 1996;46:649–653. [PMC free article] [PubMed] [Google Scholar]
- Skegg DCG. Third generation oral contraceptives. BMJ. 2000;321:190–191. doi: 10.1136/bmj.321.7255.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 2