Abstract
Objective:
To explore a model suitable for enhanced recovery after surgery (ERAS) for elderly patients with lung cancer in this region.
Methods:
A total of 200 elderly patients with lung cancer who were admitted to our department and received thoracoscopic surgery from January 1, 2020, to December 31, 2021, were enrolled as observation subjects and were randomly assigned to an ERAS group (100 cases) and a control group (100 cases). All patients were aware of and agreed to enter the study, and the protocols were approved by the hospital ethics committee (2021 Medical Ethics Review 26). The incidence of postoperative pulmonary complications, duration of postoperative chest tube, postoperative pain, and pulmonary function (including forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1)) on postoperative day 7 were compared between the 2 groups.
Results:
The incidence of postoperative pulmonary complications was significantly lower in the ERAS group (8.00%) than in the control group (18.00%). The incidence of postoperative atelectasis in the ERAS group (2%) was significantly lower than that in the control group (10%). The duration of postoperative chest tube in the ERAS group (2.57 ± 0.72 days) was significantly shorter than that in the control group (3.92 ± 1.54 days). The postoperative pain score of the ERAS group (2.14 ± 0.86) was significantly lower than that of the control group (3.78 ± 1.15). On postoperative day 7, both FVC and FEV1 in the ERAS group were significantly better than those in the control group. SPSS 20 was used for statistical analysis, and the P < .05 was considered clinically significant.
Conclusion:
The ERAS model established in our department can reduce the incidence of postoperative complications, relieve postoperative pain, and better protect the lung function of elderly patients with lung cancer. The model is worth promoting because it enhances recovery after surgery and reduces the family burden of patients.
Keywords: Complications, Enhanced recovery after surgery, Lung cancer, Thoracoscopic surgery, Uniportal thoracoscopic
INTRODUCTION
Lung cancer has become the leading malignant tumor in China in terms of incidence and mortality, with a large number of new cases every year.1,2 With the aging of the population in China, the number of elderly (≥60 years old) lung cancer patients continues to increase, accounting for approximately 50% of all lung cancer patients, and the diagnosis and treatment of elderly lung cancer patients is becoming a substantial challenge for clinicians.3,4 For elderly patients with resectable lung cancer, thoracoscopic radical resection is still the standard treatment approach. Based on postoperative pathological staging, some patients may require adjuvant radiochemotherapy, targeted therapy, or immunotherapy. With the development of thoracoscopic technology, surgical trauma has decreased, resulting in a corresponding increase in the 5-year survival rate for patients.5 However, lung cancer surgery is still an invasive surgery, and its impact on cardiopulmonary function is more significant than that of other surgical procedures. In addition, elderly patients have a poor physiological and psychological status, and most have underlying diseases such as hypertension, coronary heart disease, and chronic obstructive pulmonary disease. As a result, elderly patients with lung cancer generally have a slower postoperative recovery, a corresponding increase in the incidence of postoperative complications, and a longer hospital stay than do ordinary patients, imposing an additional financial burden on the patient’s family.6–8
Since the concept of enhanced recovery after surgery (ERAS) was introduced to China by Jieshou Li in 2007, it has gradually been incorporated into multiple surgical specialties. The core value of ERAS is to apply a series of measures that have been proven by evidence-based medicine to reduce the stress and trauma of surgery on patients, thereby reducing the postoperative hospital stay and accelerating the postoperative recovery of patients. For the rehabilitation of elderly patients with lung cancer, major centers or hospitals have experience, but there is a lack of high-level evidence-based data and guideline recommendations, and there are significant regional differences. For example, West China Hospital, Sichuan University, Qilu Hospital of Shandong University, and Nanjing General Hospital of Nanjing Military Command have reported their experience with the application of ERAS in thoracic surgery, providing inspiration for this study.18,19 The purpose of this study was to design a set of ERAS programs that are suitable for our department, easy to implement, and highly accepted by patients, aiming to accelerate recovery and discharge.
MATERIALS AND METHODS
Clinical Data and Grouping
A total of 200 elderly patients with lung cancer who were admitted to the Department of Thoracic and Cardiac Surgery from January 1, 2020, to December 31, 2021, were selected as observation subjects. The inclusion criteria were as follows: (1) patients with nonsmall-cell lung cancer who underwent thoracoscopic surgery, including lobectomy, pulmonary segmentectomy and wedge resection in our department; (2) age ≥ 60 years; (3) no severe cardiopulmonary disease (like coronary heart disease, valvulopathy, destroyed lung and bronchiectasia) before surgery; (4) family members were aware of and agreed to participate in the clinical trial, which received approval by the hospital ethics committee. The exclusion criteria were as follows: (1) patients with small cell lung cancer; (2) patients whose procedure was converted to open surgery or combined lobectomy due to various reasons; (3) patients who were transferred to the intensive care unit after surgery; (4) patients with visual and hearing impairment; (5) patients with a previous history of chest surgery or with chronic pain; (6) patients who had previously received radiotherapy, chemotherapy or immunotherapy; and (7) patients who refused to participate.
A total of 200 patients were enrolled in the study: 111 males and 89 females, with ages ranging from 60–87 years and an average age of 69.17 ± 5.74 years. The patients were randomly divided into an ERAS group and a control group by coin-toss. There were 100 patients in the ERAS group: 57 males and 43 females, with an average age of 68.82 ± 5.40 years. There were 100 patients in the control group: 54 males and 46 females, with an average age of 69.43 ± 6.04 years. There were no significant differences between the 2 groups in terms of sex, age, tumor location, smoking status (≥1 pack/day; <1 pack/day), duration of surgery and surgical status. The general information of the patients is provided in Table 1.
Table 1.
General Information
| Name | ERAS Group | Control Group | Statistical Value | P-value |
|---|---|---|---|---|
| Sex (patients, %) | ||||
| Male | 57 (57%) | 54 (54%) | χ2 = 0.182 | 0.669 |
| Female | 43 (43%) | 46 (46%) | ||
| Age (x ± s, years) | 68.82 ± 5.40 | 69.43 ± 6.04 | t = 0.807 | 0.193 |
| Tumor location (cases, %) | ||||
| Upper lobe of lung | 63 (63%) | 54 (54%) | χ2 = 1.899 | 0.387 |
| Middle lobe of lung | 5 (5%) | 8 (8%) | ||
| Lower lobe of lung | 32 (32%) | 38 (38%) | ||
| Smoking status (patients, %) | ||||
| Smoking (≥1 pack/day) | 68 (68%) | 65 (65%) | χ2 = 0.202 | 0.653 |
| Nonsmoking (<1 pack/day) | 32 (32%) | 35 (35%) | ||
| Duration of surgery (minutes) | 153.22 ± 65.11 | 163.88 ± 65.28 | t = −1.127 | 0.261 |
| Surgical condition | ||||
| Lobectomy | 59 | 66 | χ2 = 4.362 | 0.113 |
| Segmentectomy | 11 | 7 | ||
| Wedge resection | 30 | 17 |
Methods
This was a randomized controlled study. All patients provided informed consent for this study, and the enrolled patients were grouped by coin-toss. The postoperative rehabilitation training was completed under the guidance of doctors and nurses in our department. The patients in the ERAS group and the control group received preoperative oral education.
Preoperative education
The medical history of each participant was obtained to determine the presence or absence of underlying diseases and history of drug allergies. The patients were provided an introduction to the department environment and safety, visiting system and visiting hours, and doctors and nurses, as well as provided disease-related and surgery-related information. The 2 groups of patients were encouraged to exercise and maintain proper nutritional support before surgery. Patients in the ERAS group were also introduced to the concept and necessity of ERAS to relieve anxiety to better cooperate with the ERAS model; additionally, information regarding postoperative pain and analgesia and related analgesic drugs was provided.
Preoperative respiratory function exercise
For both the ERAS group and the control group, preoperative respiratory function exercises were taught to each participant by the nurses in charge. For the control group, the active cycle of breathing technique (ACBT) sputum discharge method and the balloon-blowing method were mainly included. (1) For the ACBT sputum discharge method, each patient developed an appropriate speed and depth of tidal breathing appropriate for their own conditions, with relaxed shoulders, abdominal breathing as much as possible, and coughing after holding the breath for 2–3 seconds at the end of inhalation to remove sputum. (2) For the balloon-blowing method, each patient took a deep breath, then blew a balloon vigorously for 1–2 seconds and then released it; the cycle was repeated 4–6 times. The ERAS group utilized a homemade simple respiratory function exerciser (self-developed by the department, patent number: ZL201930236718.4) and employed pursed lips abdominal breathing and respiratory gymnastics. (1) For the homemade simple respiratory function exerciser was used 4–6 times per day, 5–10 minutes each time; the postoperative frequency was the same as that before surgery, but the time was dynamically managed based on the postoperative recovery and physical strength of the patient, and a nurse was responsible for guidance and recording notes. (2) For pursed lips abdominal breathing, the patients were helped to a sitting or semirecumbent position. Each patients closed his or her mouth and inhaled deeply, held his or her breath for 2–3 seconds, puckered his or her lips as if going to whistle, leaned his or her chest slightly forward and exhaled slowly. (3) For the breathing gymnastics exercises, each patient was helped to abduct the upper limbs to approximately 150°, held his or her head with both hands, slowly opened the elbows with inhalation, held his or her breath for 2–3 seconds at the end of inhalation, and opened his or her hands naturally during exhalation.
Preoperative preparation
Research has shown that fasting for foods and liquids can cause thirst, dehydration hunger and aggravating stress response. The ERAS group strictly fasting for 6 hours and no water for 2 hours before operation. However, the control group followed the traditional approach.
Surgical condition
Patients in all groups underwent general anesthesia and double-lumen endotracheal intubation, and 1-lung ventilation of the contralateral lung was performed after the start of the procedure. In the ERAS group: (1) the effective ventilation volume was increased by a small tidal volume (5–6 ml/kg) and high respiratory rate (14–16 times/minute); the peak airway pressure was monitored in a <25 cm water column. (2) Intraoperative body temperature protection was performed by insulation blanket(3M) and keep patient's intraoperative body temperature not lower than 36°C. (3) Intraoperative fluid supply was controlled lower than 1000 ml to prevent pulmonary edema. (4) Generally, no indignant catheter would be placed if the estimated anesthetic time is less than 4 hours. While the control group also followed the traditional approach.
Postoperative analgesia
After surgery, patients in both groups were evaluated using a numeric rating scale (NRS). A score of 0 indicated no pain, a score of 1–3 indicated mild pain, a score of 4–6 indicated moderate pain, and a score of 7–9 indicated severe pain. Patient-controlled analgesic pumps (ondansetron injection 8 mg, sufentanil 100 μg, flurbiprofen axetil 50 mg add normal saline to 100 ml)were used for postoperative pain control in both groups. In the control group, when the NRS score was ≥4, diclofenac sodium sustained-release tablets (Tianjin Zhongxin Pharmaceutical, 50 mg) were given. The ERAS group began taking oral diclofenac sodium sustained-release tablets (Tianjin Zhongxin Pharmaceutical, 50 mg) from the day before surgery for preventive analgesia (1 tablet, twice per day).
Early ambulation after surgery
The family members or nurses assisted patients sitting up on the bed, and then the lower limbs were allowed to hang down on the side of the bed. After adapting to that position for 2–3 minutes, with no obvious dizziness, palpitation, chest tightness, the patient got out of bed and stood for 2–3 minutes. After adapting to that position, patients walked slowly in the hallway (approximately 120–180 meters). If dizziness was severe and blood oxygen saturation progressively decreased, ambulation was stopped. As the follow-up condition improved, the number of times and distance of ambulation increased appropriately.
Target Data
The differences in the incidence of postoperative pulmonary complications, postoperative drainage, postoperative pain, and pulmonary function (forced vital capacity [FVC] and forced expiratory volume in 1 second [FEV1]) on postoperative day 7 were compared between the 2 groups.
Statistical Methods
SPSS 20 was used for statistical analysis. Measurement data are presented as the mean ± standard deviation, and 2 independent sample t tests were used to compare the data between the 2 groups. Count data are expressed as a percentage, and the data between the 2 groups were compared using the χ2 test. The test level was α = 0.05.and the P <.05 was considered clinically significant.
RESULTS
The comparison of preoperative pulmonary function between the 2 groups of patients showed no significant differences in FVC or FEV1 (P > .05); the results are provided in Table 2.
Table 2.
Comparison of Preoperative Pulmonary Function between the 2 Groups of Patients
| Group | ERAS Group | Control Group | t value | P-value |
|---|---|---|---|---|
| Number of patients | 100 | 100 | ||
| FVC | 2.61 ± 0.69 | 2.52 ± 0.69 | 0.860 | 0.391 |
| FEV1 | 2.24 ± 0.59 | 2.19 ± 0.57 | 0.545 | 0.587 |
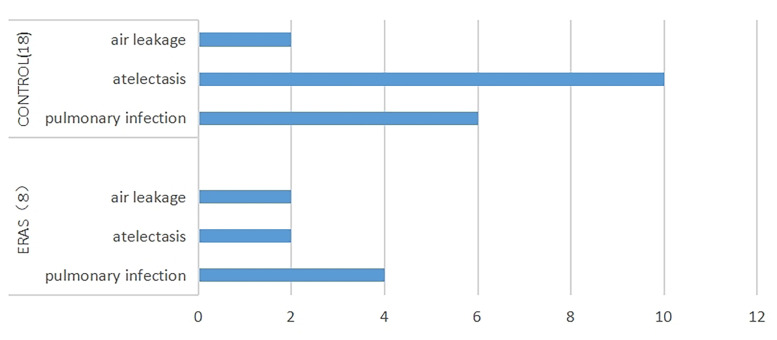
The incidence of postoperative pulmonary complications in the 2 groups. After thoracic surgery, postoperative pulmonary complications, such as pulmonary infection, atelectasis, air leakage, and respiratory failure, are common. In this study, 8 patients in the ERAS group had complications, including 4 cases of pulmonary infection, 2 cases of atelectasis, and 2 cases of air leakage. Eighteen patients in the control group had complications, including 6 cases of pulmonary infection, 10 cases of atelectasis, and 2 cases of air leakage. Respiratory failure was not observed in the 2 groups (Figure 1). The overall incidence of complications in the ERAS group (8%) was significantly lower than that in the control group (18%). Further analysis indicated that there was a significant difference in the incidence of postoperative atelectasis between the 2 groups, i.e., significantly lower in the ERAS group (2%) than in the control group (10%) (Table 3).
Figure 1.
Postoperative pulmonary complications.
Table 3.
Comparison of the Incidence of Postoperative Pulmonary Complications between the 2 Groups
| Group | ERAS Group | Control Group | Statistical Value | P-value |
|---|---|---|---|---|
| Number of patients | 100 | 100 | ||
| Incidence of postoperative pulmonary complications | 8% | 18% | χ2 = 4.421 | 0.036 |
| Incidence of pulmonary infection | 4% | 6% | χ2 = 0.421 | 0.516 |
| Incidence of atelectasis | 2% | 10% | χ2 = 5.674 | 0.017 |
Criteria for removing the chest tube (no air leakage and drainage ≤200ml) are same between the 2 groups. However, the postoperative drainage for patients in the ERAS group (2.57 ± 0.72 days) was significantly shorter than that for patients in the control group (3.92 ± 1.54 days). The postoperative pain score for patients in the ERAS group (2.14 ± 0.86 points) was significantly lower than that for patients in the control group (3.78 ± 1.15 points) (Table 4).
Table 4.
Postoperative Drainage and Pain in the 2 Groups
| Group | ERAS Group | Control Group | t value | P-value |
|---|---|---|---|---|
| Number of patients | 100 | 100 | ||
| Postoperative drainage (days) | 2.57 ± 0.72 | 3.92 ± 1.54 | −7.758 | 0.000 |
| Postoperative pain score | 2.14 ± 0.86 | 3.78 ± 1.15 | −5.320 | 0.017 |
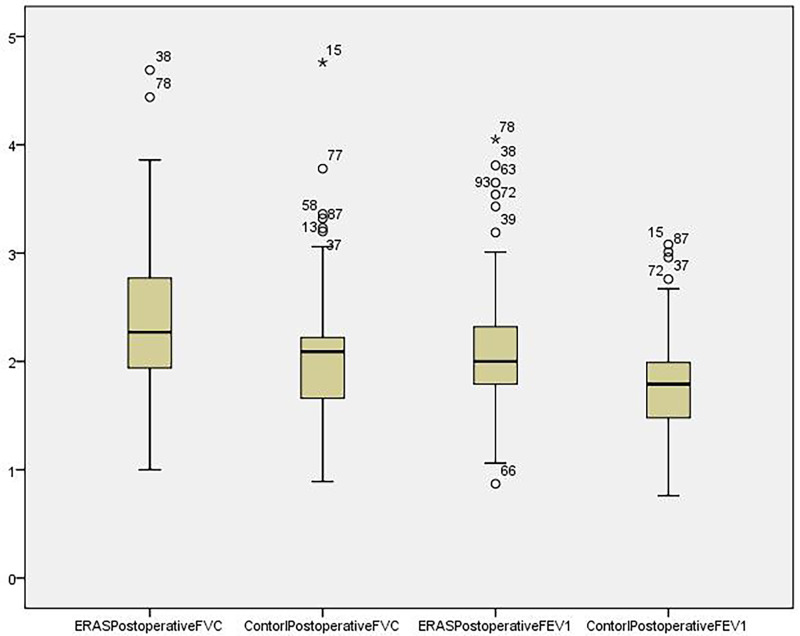
The pulmonary function on postoperative day 7 was shown by box diagram (Figure 2), both FVC and FEV1 in the ERAS group were significantly better than those in the control group (Table 5).
Figure 2.
Box plot of postoperative pulmonary function in the 2 groups.
Table 5.
Pulmonary Function on Postoperative Day 7
| Group | ERAS Group | Control Group | t value | P-value |
|---|---|---|---|---|
| Number of patients | 100 | 100 | ||
| FVC on postoperative day 7 | 2.41 ± 0.66 | 2.05 ± 0.58 | 4.024 | 0.000 |
| FEV1 on postoperative day 7 | 2.14 ± 0.55 | 1.77 ± 0.42 | 5.446 | 0.000 |
DISCUSSION
As a common malignant tumor, the number of new lung cancer cases is high every year. China is a major tobacco consuming country and one of the countries with a high incidence of lung cancer. Although the disease spectrum of lung cancer is changing and diagnosis is occurring at younger ages, current data indicate that elderly individuals still account for approximately 50% of all lung cancer patients. In addition, most elderly patients are complicated with cardiovascular diseases and pulmonary diseases, leading to varying degrees of postoperative complications and to the prolongation of postoperative hospital stays among elderly patients, even resulting in rehospitalization for a short period after surgery, placing a great burden on families and society. With the aging of the population, the vast majority of these patients must return to society and families as soon as possible after surgery; therefore, there is an extremely high necessity for ERAS.9–11
Existing data indicate that the ERAS model is only well developed for colorectal surgery, with a consensus among Chinese experts on ERAS for colorectal surgery. For thoracic surgery, there are not a large number of clinical trials or high-level evidence-based data for elderly patients with lung cancer. Moreover, the ERAS concept involves multiple aspects of the perioperative period, including anesthesia, surgery, and nursing. ERAS mainly includes effective preoperative respiratory exercises, minimally invasive surgery, early feeding, early ambulation, and controlled infusion. Most of the existing recommended measures are derived from clinical experience with colorectal surgery. There are still no high-level evidence-based data regarding the implementation of ERAS in the postoperative rehabilitation of elderly patients with lung cancer after thoracic surgery.12–13 The data indicate that measures such as smoking cessation for at least 2 weeks before surgery, preoperative respiratory function exercises, preoperative abdominal respiration and pursed lip breathing education and training, effective postoperative cough and sputum expectoration, early ambulation, nutritional assessment and necessary nutritional support, postoperative analgesia and early removal of the chest tube can accelerate the rapid postoperative recovery of lung cancer patients.14
This was a randomized controlled study. We fully considered the current situation of patients in this region and developed a series of perioperative measures for ERAS to investigate the effects of ERAS on the incidence of postoperative pulmonary complications, postoperative drainage, postoperative pain, pulmonary function on postoperative day 7 and postoperative hospital stay among elderly patients with lung cancer. We found that the incidence of postoperative pulmonary complications in the ERAS group was significantly lower than that in the control group. This result may be due to the strict preoperative smoking cessation and active breathing and sputum expectoration training. Smoking cessation can restore bronchial epithelial cilia motion, reduce chronic airway inflammation, reduce postoperative bronchial hyperresponsiveness, airway spasms, and increase airway resistance.15,16 Active sputum excretion training can allow patients to eliminate sputum as soon as possible after surgery and, to a certain extent, avoid the occurrence of atelectasis and pulmonary infection. Second, the short postoperative drainage and lower pain score in the ERAS group may also play a certain role in preventing the occurrence of pulmonary complications. In addition, due to the decrease in the incidence of complications, the postoperative hospital stay in the ERAS group was also shorter than that in the control group. In the last, we think there are several possibilities lead a shorter postoperative drainage time after operation. (1) Lower incidence of postoperative complications, especially lower incidence of postoperative air leakage. (2) Effective cough and sputum promote lung reexpansion. (3) Early ambulation after surgery encourages the fluid drainage.
Existing data indicate that elderly patients have poor thoracic compliance and weak postoperative respiratory muscle strength, resulting in poor pulmonary function reserve and a more significant postoperative pulmonary function reduction. In our study, the postoperative pulmonary function results indicated that both the FVC and FEV1 values were better in the ERAS group. This may be due to the following possible reasons. First, preoperative respiratory function exercise is equivalent to artificially increasing internal respiratory pressure, which can improve hypoxemia, alveolar collapse, and small airway spasms. With less pain, active coughing and sputum expectoration are more vigorous. Second, early postoperative ambulation can not only increase respiratory amplitude and alveolar ventilation, help expel respiratory secretions, and reduce the incidence of pulmonary infection and atelectasis but also promote the recovery of intestinal function and better nutrient absorption. In addition, psychologically, early ambulation reduces anxiety, which is conducive to improving pulmonary function and accelerating recovery.17
This study has some limitations. First, different surgeons choose different surgical approaches, mainly contains uniportal thoracoscopic surgery, single-operation port thoracoscopic surgery. The proportion of uniportal thoracoscopic surgery was 69% in ERAS group, while 64% in control group. Although there is no statistically significant difference in the proportion of surgical methods between the 2 groups(χ2 = 0.561, P = .454). If the surgical methods were standardized, the study results may be more accurate. Finally, this study lacked an assessment of long-term quality of life and follow-up, and thus, it is not known whether improvements in pulmonary function improve the long-term quality of life of patients.
Footnotes
Conflict of interest: No conflict of interest exits in the submission of this manuscript, and manuscript is approved by all authors for publication.
Contributor Information
Zhihai Wang, Department of Thoracic and Cardiovascular Surgery, Wuhu Hospital Affiliated to East China Normal University (Wuhu No. 2 People’s Hospital), Wuhu, Anhui, China. (Drs. Wang, Geng, Wu, and Tao).
Miaomiao Lin, Wannan Medical College, Wuhu, Anhui, China. (Dr. Lin).
Geng Geng, Department of Thoracic and Cardiovascular Surgery, Wuhu Hospital Affiliated to East China Normal University (Wuhu No. 2 People’s Hospital), Wuhu, Anhui, China. (Drs. Wang, Geng, Wu, and Tao).
Weiwei Wu, Department of Thoracic and Cardiovascular Surgery, Wuhu Hospital Affiliated to East China Normal University (Wuhu No. 2 People’s Hospital), Wuhu, Anhui, China. (Drs. Wang, Geng, Wu, and Tao).
Yong Tao, Department of Thoracic and Cardiovascular Surgery, Wuhu Hospital Affiliated to East China Normal University (Wuhu No. 2 People’s Hospital), Wuhu, Anhui, China. (Drs. Wang, Geng, Wu, and Tao).
References:
- 1.Cho S, Yang H, Kim K, et al. Pathology and prognosis of persistent stable pure ground-glass opacity nodules after surgical resection - sciencedirect. Ann Thorac Surg. 2013;96(4):1190–1195. [DOI] [PubMed] [Google Scholar]
- 2.Huang H-Z, Wang G-Z, Xu L-C, et al. Ct-guided hookwire localization before video-assisted thoracoscopic surgery for solitary ground-glass opacity dominant pulmonary nodules: radiologic-pathologic analysis. Oncotarget. 2017;8(64):108118–108129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen W, Zheng R, Zuo T, et al. National cancer incidence and mortality in China, 2012. Chinese Journal of Cancer Research. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liwczyński A, Kalinka E, Sierocka A, Iltchev P, Kowalski D, Marczak M. Population morbidity in elderly lung cancer patients from Poland with specific trends in elderly women. Prz Menopauzalny. 2019;18(3):161–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laursen LØ, Petersen RH, Hansen HJ, Jensen TK, Ravn J, Konge L. Video-assisted thoracoscopic surgery lobectomy for lung cancer is associated with a lower 30-day morbidity compared with lobectomy by thoracotomy. Eur J Cardiothorac Surg. 2015;49(3):870–875. [DOI] [PubMed] [Google Scholar]
- 6.Schussler O, Alifano M, Dermine H, et al. Postoperative pneumonia after major lung resection. Am J Respir Crit Care Med. 2006;173(10):1161–1169. [DOI] [PubMed] [Google Scholar]
- 7.Díaz-Ravetllat V, Ferrer M, Gimferrer-Garolera JM, Molins L, Torres A. Risk factors of postoperative nosocomial pneumonia after resection of bronchogenic carcinoma. Respir Med. 2012;106(10):1463–1471. [DOI] [PubMed] [Google Scholar]
- 8.Sandri A, Papagiannopoulos K, Milton R, et al. Major morbidity after video-assisted thoracic surgery lung resections: a comparison between the European society of thoracic surgeons definition and the thoracic morbidity and mortality system. J Thorac Dis. 2015;7(7):1174–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glotzer OS, Fabian T, Chandra A, Bakhos CT. Non-small cell lung cancer therapy: safety and efficacy in the elderly. Drug Healthc Patient Saf. 2013;5(1):113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalathiya RJ, Davenport D, Saha SP. Long-term survival after pneumonectomy for non-small-cell lung cancer. Asian Cardiovasc Thorac Ann. 2013;21(5):574–581. [DOI] [PubMed] [Google Scholar]
- 11.Gao K, Yu P-M, Su J-H, et al. Cardiopulmonary exercise testing screening and pre-operative pulmonary rehabilitation reduce postoperative complications and improve fast-track recovery after lung cancer surgery: a study for 342 cases. Thorac Cancer. 2015;6(4):443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183(6):630–641. [DOI] [PubMed] [Google Scholar]
- 13.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248(2):189–198. [DOI] [PubMed] [Google Scholar]
- 14.Kehlet H. Enhanced recovery after surgery (eras): good for now, but what about the future? Can J Anaesth. 2015;62(2):99–104. [DOI] [PubMed] [Google Scholar]
- 15.Aelony Y. Lung resection in the elderly. Chest. 2006;129(2):496–497. [DOI] [PubMed] [Google Scholar]
- 16.Simonsen DF, Søgaard M, Bozi I, et al. Risk factors for postoperative pneumonia after lung cancer surgery and impact of pneumonia on survival. Respir Med. 2015;109(10):1340–1346. [DOI] [PubMed] [Google Scholar]
- 17.Fagundes CP, Shi Q, Vaporciyan AA, et al. Symptom recovery after thoracic surgery: measuring patient-reported outcomes with the MD Anderson symptom inventory. J Thorac Cardiovasc Surg. 2015;150(3):613–619.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhenrong Z, Weifeng L, Deruo L. The influence of completion ratio of enhanced recovery after lung surgery on the prognosis of the elderly patients. Chine J Thorac Surg. 2017. [Google Scholar]
- 19.Guihe W, Kangwen C. Effect of enhanced recovery after surgery on the postoperative short-term nutrition indicators after laparoscopic gastrectomy for gastric cancer. J Abd Surg. 2017. [Google Scholar]