Abstract
Introduction:
Extreme beak calcaneal fractures (Type 2 Lee’s tuberosity avulsion fractures) are rare injuries, accounting for only 1.3–3% of all calcaneal fractures. These injuries are considered as surgical emergency as they can lead to significant functional impairment and soft-tissue compromise if not promptly managed. This study evaluates the efficacy of cannulated cancellous (CC) screw fixation for these fractures.
Materials and Methods:
A prospective study of 14 patients with extreme beak calcaneal fracture (Type 2 Lee’s - tuberosity avulsion fractures) treated with CC screw fixation was conducted in VMMCH, Karaikal, Puducherry between June 2022 and June 2023. Patients were followed for a minimum of 12 months. Functional outcomes were assessed using the American Orthopedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot scale.
Results:
The mean AOFAS score at the final follow-up was 89.3 (range 78–98). Radiographic union was achieved in all cases by 20 weeks with a mean union time of 13.09 weeks in closed fractures and 18 weeks in open fractures. One patient developed a superficial wound infection without any alarming signs of hardware issues, which resolved eventually. No hardware failures or need for revision surgeries were observed.
Conclusion:
Early intervention with CC screw fixation appears to be an effective and safe technique for the treatment of extreme beak calcaneal fracture (Type 2 Lee’s – tuberosity avulsion fractures), resulting in excellent functional outcomes and a low complication rate.
Keywords: Calcaneal fracture, extreme beak, tuberosity avulsion, American orthopedic foot and ankle society scoring, cannulated cancellous screw fixation, Achilles tendon
Learning Point of the Article:
Extreme beak calcaneal fracture (Type 2 Lee) is a surgical emergency, early intervention with Cannulated Cancellous Screw fixation results in favorable outcome.
Introduction
Extreme beak calcaneal fracture (type 2 Lee’s fractures) are relatively rare injuries, accounting for approximately 1.3–3% of all calcaneal fractures. The incidence is highest in elderly particularly in women. This type of fracture requires timely interference and treated as surgical emergency within 6 h to avoid skin necrosis and soft-tissue compromise. Despite their rarity, these fractures can result in significant functional impairment if not promptly managed [1]. They can lead to soft-tissue compromise, chronic pain and alterations in gait mechanics. In addition, non-union or malunion may contribute to the development of subtalar arthritis if there is an intra-articular extension. Several risk factors have been identified for calcaneal tuberosity avulsion fractures. Osteoporosis plays a significant role, especially in elderly patients [2]. Other contributing factors include diabetes mellitus [3-8] and peripheral neuropathy which can affect bone quality and proprioception [9, 10].
The calcaneal tuberosity serves as the insertion point for the Achilles tendon, the strongest tendon in the human body. The Achilles tendon originates from the distal end of the triceps surae muscle group (average length of approximately 15 cm) and inserts into the middle third of the posterior surface of calcaneal tuberosity of varying width of 1.2–2.5cm [11, 12]. Anatomical studies have shown that in some individuals, the Achilles tendon has an extensive insertion into the calcaneal tuberosity, which may predispose them to avulsion fractures [13]. The overall calcaneus is composed primarily of cancellous bone encapsulated by a relatively thin cortical shell. The density of the trabecular structure determines the overall strength of the calcaneus and the calcaneal tuberosity. In patients with osteoporosis or other conditions affecting bone quality, the decreased trabecular density can increase the risk of avulsion fractures.
The mechanism of injury typically involves a sudden, strong contraction of the gastrocnemius-soleus complex, often with the ankle in a dorsiflexed position. This creates a tensile force through the Achilles tendon that can exceed the strength of the bone at its insertion, resulting in an avulsion fracture [14, 15, 16, 17].
Combined with the above anatomy, a more extensive insertion of the Achilles tendon at the calcaneal tuberosity will lead to a more vertical direction of force and even avulsion fractures. Collectively, the distraction force generated by the Achilles tendon at the calcaneal tuberosity and the trabecular density of the calcaneus will play a major role in the occurrence of fractures.
Several classification systems have been proposed for calcaneal tuberosity avulsion fractures. The Lee classification [18], which is widely used, describes four types of fractures: Type I: Simple extra-articular avulsion fracture (sleeve fracture) Type II: Beak fracture with a large fragment Type III: Infrabursal avulsion fracture from the middle third of the posterior tuberosity Type IV: Beak fracture with a small triangular fragment (Fig. 1).
Figure 1.
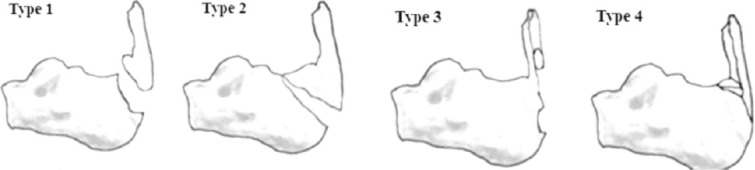
Lee classification for calcaneal tuberosity avulsion fractures.
More recently, the Carnero Martín de Soto classification has been introduced, which focuses on fracture displacement as a predictor of complications. This system classifies fractures as Type 1 (displacement <2 cm) or Type 2 (displacement ≥2 cm), with Type 2 fractures associated with a higher risk of soft-tissue complications.
While conservative management is limited to only undisplaced fracture, surgical intervention is mandatory for displaced fractures or those involving a large portion of the calcaneal tuberosity. Various surgical techniques have been described, including closed reduction and internal fixation (CRIF) with cannulated cancellous (CC) screw fixation, open reduction and internal fixation with plates and screws, tension band wiring, suture anchor suture bridge techniques, side-locking loop suture (SLLS) techniques, etc. The use of CC screws for the fixation of calcaneal tuberosity avulsion fractures has gained popularity due to its ease of application and promising results. This technique offers several potential advantages, including minimal soft-tissue dissection, strong interfragmentary compression and early mobilization.
The primary aim of this prospective study was to evaluate the functional outcomes of extreme beak calcaneal fractures – Type 2 Lee’s tuberosity avulsion fractures. Although multiple case reports are documented, there is a limited literature support specifically evaluating the outcomes of CC screw fixation focusing on such fractures (Type 2 Lee) in larger samples. Secondary objectives included assessing the rate of complications, time to fracture union and return to pre-injury activities.
Materials and Methods
This prospective study was conducted at our institution between June 2022 and June 2023. The study protocol was approved by the institutional ethics committee (I.E.C APPROVAL NO IEC/VMMCH/24/APR/95). All patients provided written informed consent before participation.
Inclusion criteria
Age 18 years or older, acute open or closed, extreme beak calcaneal fracture: Type 2 Lee’s tuberosity avulsion fractures, displacement of more than 1 cm.
Exclusion criteria
Pathological fractures, concomitant ipsilateral lower extremity fractures, and severe medical comorbidities precluding surgery.
Pre-operative assessment
A thorough history and physical examination are crucial in the diagnosis of calcaneal tuberosity avulsion fractures. Patients typically present with acute pain and swelling in the posterior heel region, often following a traumatic event or sudden forceful dorsiflexion of the ankle. Physical examination should include an assessment of skin integrity, as the displaced bone fragment can cause tension on the overlying skin, potentially leading to necrosis. The Silverskiöld test can be used to assess the gastrocnemius-soleus complex, while the Thompson test may be positive if there is concomitant Achilles tendon disruption. Plain radiographs, including lateral and axial views of the calcaneus, are usually sufficient to diagnose the fracture. Computed tomography (CT) scans can provide more detailed information about fracture morphology and displacement [19]. Magnetic resonance imaging (MRI) may be useful in cases where there is suspicion of concomitant Achilles tendon injury or in fractures with minimal bony involvement. CT and MRI are not done routinely, but only when indicated as discussed above. The choice between conservative and surgical management depends on several factors, including fracture displacement, soft-tissue condition, and patient characteristics. Non-surgical treatment may be considered only for non-displaced or minimally displaced fractures. However, surgical intervention is mandatory for fractures with displacement >1 cm, those involving a large portion of the calcaneal tuberosity, or cases with a high risk of soft-tissue complications. It is treated as surgical emergency within 6 h preferably or at the earliest after standard pre-anesthetic check-up.
Operative technique
Under regional anesthesia, the patient was positioned prone on the operating table with a bump under the ipsilateral hip to internally rotate the foot. A pneumatic tourniquet was applied to the proximal thigh and inflated to 300 mmHg after limb exsanguination. The operative site was prepared and draped in a sterile fashion. A minimally invasive posterior approach was utilized. A small, incision was made along the lateral aspect of the Tendo Achilles proximal to the tuberosity. Careful dissection through the subcutaneous tissue was performed, with special attention given to identifying and protecting the sural nerve.
The reduction is aided by plantar flexion, using a bump under the ankle. The fracture was visualized and reduced under C-arm guidance. A large reduction clamp was carefully applied with one arm on the superior aspect of the tuberosity and the other through the heel pad, ensuring anatomic reduction of the fracture and subtalar joint if involved. Guide wires were placed across the fracture site from superoposterior to inferoanterior direction, perpendicular to the fracture line. The appropriate screw length was measured, and the guide wires were overdrilled with a cannulated drill bit. Depending on the fracture fragment size one or two 6.5 mm or 4.0 mm CC screws of sharma surgicals, SSPL, India (partial or fully threaded) were then inserted over the guide wires. The screws tip were positioned just anterior to the weight-bearing portion of the tuberosity, ensuring bicortical purchase into the thick plantar surface of the calcaneal tuberosity for rigid fixation. In cases of osteoporotic bone and small fragment with risk of splintering while inserting the screw, washers were added to enhance stress distribution over avulsed fragment. C-arm was used to confirm adequate reduction and proper hardware placement. The wound was thoroughly irrigated and closed in layers. A sterile dressing was applied, followed by a well-padded short leg splint with the ankle in plantar flexion to neutralize distracting forces (Tendo Achilles pull) on the fixation. This technique allows for minimal soft-tissue dissection while providing strong interfragmentary compression. The use of cannulated compression screws offers the advantages of precise placement and the potential for early mobilization, which may contribute to improved outcomes.
Post-operative protocol
Postoperatively, patients were placed in a short leg splint with the ankle in plantar flexion. Non-weight bearing was advised for the first 6 weeks. At 2 weeks, the splint was removed, and a removable boot was applied. Passive range of motion exercises were initiated at this time. Progressive weight bearing was allowed starting at 6 weeks, with full weight bearing typically achieved by 10–12 weeks based on clinical and radiographic evidence of healing.
Follow-up and outcome measures
Patients were followed at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months postoperatively. At each visit, a clinical examination was done and radiographs were performed every 3 months and at final follow-up. The primary outcome measure was the American Orthopedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot scale, administered at the 12-month follow-up [20]. Secondary outcome measures included visual analogue scale (VAS) for pain, time to radiographic union, complications, and return to pre-injury activities [21]. Assessment of radiographic union in a fracture of cancellous bone fixed by compression screw is not straightforward as in the case of cortical bone, since after achieving satisfactory compression by screws, the fracture line cannot be appreciated well, hence, in follow-up we look for the – absence of sclerosis of the fracture line/gap formation/displacement of the fracture fragment/screw loosening and subsequent implant failure (which are considered as non-union). Malunion is diagnosed by the tilting of the fracture fragment mostly due to the malreduction caused by the asymmetric compression of the fragment, which was not tolerated intraoperatively.
Case illustrations
Case 1
A 38-year-old male presented with right heel pain following a fall from a ladder. Radiographs and X-ray revealed a displaced extra-articular calcaneal extreme beak fracture Lee Type 2. The patient underwent emergency early CRIF with CC screw fixation as described with trauma to surgery interval 5 h. At 12-month follow-up, the patient had an AOFAS score of 94, with complete return to pre-injury activities and no pain (Fig. 2).
Figure 2.

(A) pre-operative X-ray, (B) pre-operative clinical picture showing the skin impalement (black arrow), (C) intraoperative picture showing sural nerve identification and preservation, (D) post-operative X-ray showing cannulated cancellous screw fixation, (E-G) range of movements and X-ray after union at final follow-up.
Case 2
A 33-year-old male with right open grade 3A calcaneal extreme beak fracture Lee Type 2, with lateral malleolus fracture, with heal pad avulsion following motor vehicle accident, X-ray showed significant displacement of calcaneal beak fracture. Thorough wound debridement done and calcaneal fracture fixed with CC screws and K-wiring done for fibula, trauma to surgery interval 12 h (due to delayed presentation). Wound healed by 4 weeks without infection. His 12-month AOFAS score was 82, with residual stiffness and near-complete return to activities (Fig. 3).
Figure 3.

(a) pre-operative X-ray showing calcaneal beak fracture and lateral malleolus fracture, (b) pre-operative clinical image of the open fracture, (c) intraoperative C-arm image, (d) immediate post-operative clinical image, (e) clinical image after wound healing. (f) immediate post-operative X-ray with cannulated cancellous screws and k-wires for added fixation, (g) post-operative X-ray at 6 weeks, (h) post-operative X-ray showing fracture union at final follow-up, (i, J, k) post-operative range of movements after union at final follow-up.
Case 3: A 52-year-old male sustained a left calcaneal extreme beak fracture Lee Type 2 with avulsed fragment tenting on the skin causing impalement after a fall from bullock cart. X-ray showed significant displacement. Following CC screw fixation, the patient experienced an uneventful recovery and the skin texture returned to supple. Trauma to surgery interval is 7 hours (after a fall). Her 12-month AOFAS score was 90, with complete return to pre-injury activities and no pain (Fig. 4).
Figure 4.

(A) pre-operative X-ray showing calcaneal beak fracture and lateral malleolus fracture, (B) pre-operative clinical image of the open fracture, (C) intraoperative C-arm image, (D) immediate post-operative clinical image, (E) clinical image after wound healing. (F) immediate post-operative X-ray with cannulated cancellous screws and k-wires for added fixation, (G) post-operative X-ray at 6 weeks, (H) post-operative X-ray showing fracture union at final follow-up, (I-K) post-operative range of movements after union at final follow-up.
Results
Demographic data
The study included 14 patients (9 males, 5 females) with a mean age of 42.3 ± 10.7 years. The mechanism of injury was fall in 8 cases (57.1%), sports-related injury in 4 cases (28.6%), and motor vehicle accident in 2 cases (14.3%). All the fractures were Lee Type 2. The mean time from injury to surgery was 12–18 h. All the patients were extra-articular fractures, 3 (21.4) of them had open fractures and 11 (78.5) of them had closed fracture. Three cases of osteoporotic bone or small fragment with risk of splintering were noted intraoperatively hence, fixation was augmented with washer. Mean tourniquet time was 53 min in closed fractures and 72 min for open fractures.
Clinical outcomes
The mean AOFAS Ankle-Hindfoot scale score at 12-month follow-up was 89.3 ± 6.2 (range 78–98). Eleven patients (78.6%) achieved excellent results (90–100 points), while three patients (21.4%) with open fractures had good results (80–89 points). The mean VAS pain score improved significantly from 7.8 ± 1.2 preoperatively to 1.3 ± 0.9 at final follow-up (P < 0.001).
Radiographic outcomes
Radiographic union was achieved in 12 patients by 12–16 weeks, with mean union time of 13.09 weeks and in two patients with open fracture union was achieved by 16–20 weeks, with mean union time of 18 weeks postoperatively. Radiographic union was achieved completely in all case by 20 weeks. No cases of non-union, malunion or hardware failure were observed.
Complications
One patient (7.1%) developed a superficial wound infection and delayed wound healing, which resolved with a course of antibiotics and regular dressing. No deep infections, neurovascular injuries, or complex regional pain syndrome were observed.
Return to activities
Twelve patients (85.7%) returned to their pre-injury level of activity by the 6-month follow-up. The remaining two patients with open injury (14.3%) reported minor limitations in high-impact activities but had returned to daily activities without any discomfort.
Discussion
This prospective study demonstrates that CC screw fixation is an effective and safe technique for the treatment of extreme beak calcaneal fracture – Type 2 Lee’s tuberosity avulsion fractures. Our results show excellent to good functional outcomes, with a mean AOFAS score of 89.3 at 12-month follow-up. This is comparable to or better than results reported in previous studies using other fixation methods for similar fractures.
The mean AOFAS Ankle-Hindfoot scale score of 89.3 in our study is comparable to or better than most of the studies in our comparison. For instance, Takahashi et al. [22] reported a score of 87 using CC screw fixation, while our study achieved a slightly higher score. Our results are also similar to those reported by Squires et al. [23] with 87.5. However, some studies using alternative techniques, such as Khazen et al. [24] with suture anchor fixation and Zhang and Wu [25] with L-shaped hook plate, reported slightly higher AOFAS scores (94.3 and 93.8, respectively). This suggests that while CC screw fixation produces excellent results, there may be room for further optimization or comparison with these alternative techniques. Our study achieved higher union rate, which is consistent with several other studies in the comparison, Takahashi et al. [22] and Zhang and Wu [25]. This high union rate underscores the effectiveness of CC screw fixation in promoting fracture healing. Our study’s complication rate of 7.1% (one case of superficial infection) and zero reoperation rate is comparable to or lower than most studies in the comparison. For example, Gitajn et al. [26] and Yu et al. [27] reported a higher rate of reoperation of 35% and 10%, respectively. Notably, Khazen et al. [24] and Banerjee et al. [28] reported lower complication rates (0% and 5.6%, respectively) with suture anchor fixation, suggesting that this technique for its potential to minimize complications in Type 1, 3, 4 Lee’s types of fractures. Our study’s finding that 85.7% of patients returned to their pre-injury level of activity at follow-up is a significant outcome. While not all studies in our comparison reported on return to activities, this high rate of functional recovery supports the efficacy of CC screw fixation in restoring patients’ quality of life. While our results are promising, it is important to note that CC screw fixation is preferable only in Lee Type 2 and may not be suitable for all types of calcaneal tuberosity avulsion fractures. For example, in cases with very small or osteoporotic bone fragments, or those involving significant Achilles tendon disruption, alternative fixation methods may be necessary, especially in Lee Type 1, 3 and 4. Other fixation techniques described in the literature include suture anchor techniques [6, 29, 30], suture bridge techniques [31, 32, 33], SLLS techniques [34, 35] and plate fixation [25, 36]. Each of these methods has its own indications, advantages, and potential drawbacks. The choice of fixation technique should be tailored to the specific fracture pattern, bone quality, and soft-tissue condition. While our study demonstrates favorable outcomes, it is important to note its limitations, including the retrospective study design and a relatively small sample size (n = 14) compared to some larger studies like Squires et al. [23] with 22 patients and Gitajn et al. [26] with 30 patients. Future research could benefit from larger, multi-center studies to further validate these findings benefit from larger, multi-center studies to further validate these findings.
Conclusion
Early intervention with CC screw fixation appears to be an effective and safe technique for the treatment of extreme beak calcaneal fracture (type 2 Lee’s tuberosity avulsion fractures) which is a surgical emergency, due to its potential soft-tissue complications. This approach results in excellent to good functional outcomes, high rates of fracture union, and a low soft-tissue complication rate. The minimally invasive nature of the technique, combined with stable fixation, allows for early rehabilitation, prevention of soft-tissue compromise, earlier weight bearing and return to activities. While further research is needed, our results suggest that CC screw fixation should be considered as a viable option in the imminent surgical management of extreme beak calcaneal fracture.
Clinical Message.
Extreme beak calcaneal fracture (type 2 Lee’s tuberosity avulsion fracture) is a surgical emergency, due to its potential soft-tissue complications. Early intervention with CC screw fixation appears to be an effective and safe technique with favorable outcomes.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Rammelt S, Zwipp H. Calcaneus fractures:Facts, controversies and recent developments. Injury. 2004;35:443–61. doi: 10.1016/j.injury.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Rufai A, Ralphs JR, Benjamin M. Structure and histopathology of the insertional regions of the human Achilles tendon. J Orthop Res. 1995;13:585–93. doi: 10.1002/jor.1100130414. [DOI] [PubMed] [Google Scholar]
- 3.Greenhagen RM, Highlander PD, Burns PR. Double row anchor fixation:A novel technique for a diabetic calanceal insufficiency avulsion fracture. J Foot Ankle Surg. 2012;51:123–7. doi: 10.1053/j.jfas.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Hong CC, Lim JX, Tan JH, Pearce CJ. Outcomes of operatively treated calcaneal tuberosity avulsion fractures. Injury. 2022;53:1276–82. doi: 10.1016/j.injury.2021.12.046. [DOI] [PubMed] [Google Scholar]
- 5.Krentz A, Fitzgerald M, Wright A, Nattrass M. Spontaneous fractures in patients with diabetic neuropathy. J R Coll Physicians Lond. 1989;23:111–3. [PMC free article] [PubMed] [Google Scholar]
- 6.Levin ME, Boisseau VC, Avioli LV. Effects of diabetes mellitus on bone mass in juvenile and adult-onset diabetes. N Engl J Med. 1976;294:241–5. doi: 10.1056/NEJM197601292940502. [DOI] [PubMed] [Google Scholar]
- 7.Reddy GK. Cross-linking in collagen by nonenzymatic glycation increases the matrix stiffness in rabbit Achilles tendon. Exp Diabesity Res. 2004;5:143–53. doi: 10.1080/15438600490277860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reddy G. Glucose-mediated in vitro glycation modulates biomechanical integrity of the soft tissues but not hard tissues. J Orthop Res. 2003;21:738–43. doi: 10.1016/S0736-0266(03)00006-8. [DOI] [PubMed] [Google Scholar]
- 9.Jeffcoate W, Lima J, Nobrega L. The Charcot foot. Diabet Med. 2000;17:253–8. doi: 10.1046/j.1464-5491.2000.00233.x. [DOI] [PubMed] [Google Scholar]
- 10.Prisk VR, Wukich DK. Ankle fractures in diabetics. Foot Ankle Clin. 2006;11:849–63. doi: 10.1016/j.fcl.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Yu SM, Yu JS. Calcaneal avulsion fractures:An often forgotten diagnosis. AJR Am J Roentgenol. 2015;205:1061–7. doi: 10.2214/AJR.14.14190. [DOI] [PubMed] [Google Scholar]
- 12.Calleja M, Connell DA. The Achilles tendon. Semin Musculoskelet Radiol. 2010;14:307–22. doi: 10.1055/s-0030-1254520. [DOI] [PubMed] [Google Scholar]
- 13.Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. Am J Sports Med. 2002;30:287–305. doi: 10.1177/03635465020300022501. [DOI] [PubMed] [Google Scholar]
- 14.Schepers T, Ginai AZ, Van Lieshout EM, Patka P. Demographics of extra-articular calcaneal fractures:Including a review of the literature on treatment and outcome. Arch Orthop Trauma Surg. 2008;128:1099–106. doi: 10.1007/s00402-007-0517-2. [DOI] [PubMed] [Google Scholar]
- 15.Robb CA, Davies MB. A new technique for fixation of calcaneal tuberosity avulsion fractures. Foot Ankle Surg. 2003;9:221–4. [Google Scholar]
- 16.Biell WC, 3rd, Morgan JM, Wagner WF, Gabriel R. Neuropathic calcaneal tuberosity avulsion fractures. Clin Orthop Relat Res. 1993;269:8–13. [PubMed] [Google Scholar]
- 17.Cooper DE, Heckman JD. The heel of Achilles:Calcaneal avulsion fracture from a gunshot wound. Foot Ankle. 1989;9:204–6. doi: 10.1177/107110078900900411. [DOI] [PubMed] [Google Scholar]
- 18.Lee SM, Huh SW, Chung JW, Kim DW, Kim YJ, Rhee SK. Avulsion fracture of the calcaneal tuberosity:Classification and its characteristics. Clin Orthop Surg. 2012;4:134–8. doi: 10.4055/cios.2012.4.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87–95. [PubMed] [Google Scholar]
- 20.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–53. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 21.Schepers T, Ginai AZ, Mulder PG, Patka P. Radiographic evaluation of calcaneal fractures:To measure or not to measure. Skeletal Radiol. 2007;36:847–852. doi: 10.1007/s00256-007-0330-6. [DOI] [PubMed] [Google Scholar]
- 22.Takahashi Y, Takegami Y, Tokutake K, Asami Y, Takahashi H, Kato M, et al. Analysis of calcaneal avulsion fractures treated surgically and nonsurgically:A retrospective multicenter study. JB JS Open Access. 2024;9:e23. doi: 10.2106/JBJS.OA.23.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Squires B, Allen PE, Livingstone J, Atkins RM. Fractures of the tuberosity of the calcaneus. J Bone Joint Surg Br. 2019;83:55–61. doi: 10.1302/0301-620x.83b1.11184. [DOI] [PubMed] [Google Scholar]
- 24.Khazen GE, Wilson AN, Ashfaq S, Parks BG, Schon LC. Fixation of calcaneal avulsion fractures using screws with and without suture anchors:A biomechanical investigation. Foot Ankle Int. 2018;39:99–103. doi: 10.3113/FAI.2007.1183. [DOI] [PubMed] [Google Scholar]
- 25.Qiang Zhang, Chan Zhu, Zongde Wu, et al. Calcaneal Tuberosity Fracture (Beak Fracture) Fixation Using a Pre-contoured “L-form”Hook Plate:A Retrospective Study, 12 August 2021. PREPRINT (Version 1) available at Research Square. [https://doi.org/10.21203/rs.3.rs-775085/v1] [Google Scholar]
- 26.Gitajn IL, Abousayed M, Toussaint RJ, Vrahas M, Kwon JY. Calcaneal avulsion fractures:A case series of 33 patients describing prognostic factors and outcomes. Foot Ankle Spec. 2015;8:10–7. doi: 10.1177/1938640014548323. [DOI] [PubMed] [Google Scholar]
- 27.Yu GR, Pang QJ, Yu X, Chen DW, Yang YF, Li B, et al. Surgical management for avulsion fracture of the calcaneal tuberosity. Orthop Surg. 2013;5:196–202. doi: 10.1111/os.12058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Banerjee R, Chao JC, Taylor R, Siddiqui A. Management of calcaneal tuberosity fractures. J Am Acad Orthop Surg. 2012;20:253–8. doi: 10.5435/JAAOS-20-04-253. [DOI] [PubMed] [Google Scholar]
- 29.Janis L, Lam AT, Espiritu T, Ploot E, Husain ZS. A comparison of soft-tissue anchors in tendo Achilles reattachment. J Foot Ankle Surg. 2001;40:195–207. doi: 10.1016/s1067-2516(01)80019-3. [DOI] [PubMed] [Google Scholar]
- 30.Ninomiya H, Watanabe M, Kamimura K. Innovative fixation technique for avulsion fractures of the calcaneal tuberosity. J Foot Ankle Surg. 2021;60:218–20. doi: 10.1053/j.jfas.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Beitzel K, Mazzocca AD, Obopilwe E, Boyle JW, McWilliam J, Rincon L, et al. Biomechanical properties of double-and single-row suture anchor repair for surgical treatment of insertional Achilles tendinopathy. Am J Sports Med. 2013;41:1642–8. doi: 10.1177/0363546513487061. [DOI] [PubMed] [Google Scholar]
- 32.Cox JT, Shorten PL, Gould GC, Markert RJ, Barnett MD, Jr, Laughlin RT. Knotted versus knotless suture bridge repair of the Achilles tendon insertion:A biomechanical study. Am J Sports Med. 2014;42:2727–33. doi: 10.1177/0363546514549004. [DOI] [PubMed] [Google Scholar]
- 33.Clanton TO, Haytmanek CT, Williams BT, Civitarese DM, Turnbull TL, Massey MB, et al. A biomechanical comparison of an open repair and 3 minimally invasive percutaneous Achilles tendon repair techniques during a simulated, progressive rehabilitation protocol. Am J Sports Med. 2015;43:1957–64. doi: 10.1177/0363546515587082. [DOI] [PubMed] [Google Scholar]
- 34.Wakatsuki T, Imade S, Uchio Y. Avulsion fracture of the calcaneal tuberosity treated using a side-locking loop suture (SLLS) technique through bone tunnels. J Orthop Sci. 2016;21:690–3. doi: 10.1016/j.jos.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 35.Imade S, Mori R, Uchio Y. Modification of side-locking loop suture technique using an antislip knot for repair of Achilles tendon rupture. J Foot Ankle Surg. 2013;52:553–5. doi: 10.1053/j.jfas.2013.03.036. [DOI] [PubMed] [Google Scholar]
- 36.Agni N, Fearon P. Calcaneal tuberosity fixation using a locking compression hook plate. J Foot Ankle Surg. 2016;55:891–3. doi: 10.1053/j.jfas.2016.03.012. [DOI] [PubMed] [Google Scholar]


