Abstract
Introduction:
The peripheral radioulnar articulation and the bony radioulnar articulation make up the distal radioulnar joint (DRUJ), a diarthrodial trochoid synovial joint stabilizers for soft tissues. Of the DRUJ’s stability, only around 20% may be attributed to the bony articulation. Treatment for DRUJ injuries resulting from a solely ligamentous rupture varies and is subject to debate. Usually, non-operative care is coupled with occupational therapy, activity modification, brace or splint immobilization, and pain management.
Aim:
The aim of this study was to analyze comprehensive management approaches for acute DRUJ instability post-distal radius fracture.
The key takeaway from the article is that TFCC repair may not be essential, with K-wire stabilization providing better range of motion and cast immobilization offering stronger grip, but further large-scale controlled trials are required to fully assess these treatment options in terms of patient satisfaction and functional outcomes.
Materials and Methods:
After primary fixation of the respective fractures (distal end radius fracture or distal end ulna fracture or both) by ORIF with Plating or CRIF with K-wiring or by Traction for casting, the distal radio ulna joint instability is stabilized by casting, closed reduction internal fixation (CRIF) with K-wiring or open triangular fibrocartilage complex (TFCC) repair and the outcome is measured by grip strength, range of motion with DASH and MMWS scores by follow up and compared.
Results:
Between the groups, there was no discernible variation in grip strength (P > 0.05). A noteworthy variation in flexion was seen among the groups (P < 0.05). The groups’ differences in extension were statistically significant (P < 0.05). Pronation did not significantly differ across the groups (P > 0.05). Supination did not differ significantly between the groups (P > 0.05). The DASH scores of the groups did not differ significantly (P > 0.05). Between the groups, there was a significant difference in MMWS (P < 0.05).
Conclusion:
The major findings of analysis have suggested that the time, effort, and cost of TFCC repair do not appear to be necessary, however, there may be trade-offs between various treatments, with K-wire stabilization offering a better range of motion and cast immobilization a stronger grip.
Keywords: DRUJ Instability, TFCC repair, K-wiring, Casting
Learning Point of the Article:
The key takeaway from the article is that TFCC repair may not be essential, with K-wire stabilization providing a better range of motion and cast immobilization offering a stronger grip, but further large-scale controlled trials are required to fully assess these treatment options in terms of patient satisfaction and functional outcomes.
Introduction
The peripheral radioulnar articulation and the bony radioulnar articulation make up the distal radioulnar joint (DRUJ), a diarthrodial trochoid synovial joint stabilizers for soft tissues. Of the DRUJ’s stability, only around 20% may be attributed to the bony articulation [1]. The structures around the DRUJ, formed by the triangular fibrocartilage discus (TFC), the radioulnar ligaments (RULs) and the ulnocarpal ligaments (UCLs) called the triangular fibrocartilage complex (TFCC), are the main soft-tissue stabilizers. Because of the DRUJ’s intricate mobility and function, injuries to this joint need specific attention [2]. Forearm fractures, including ulnar styloid fractures, Essex-Lopresti injuries, and distal radius fractures, are frequently associated with acute traumatic DRUJ injuries; reports of these occurrences range from 10 to 19%. In the majority of these situations, DRUJ stability can be recovered once the fracture has been effectively treated [3, 4].
Treatment for DRUJ injuries resulting from a solely ligamentous rupture varies and is subject to debate. Usually, non-operative care is coupled with occupational therapy, activity modification, brace or splint immobilization, and pain management [5]. Should conservative therapy prove ineffective in reducing symptoms, distal radiolunar ligament repair, using open or arthroscopic techniques, ought to be contemplated [6, 7]. The procedure is a minimally invasive DOB augmentation.
Aim
The aim of this study was to analyze comprehensive management approaches for Acute DRUJ instability post-distal radius fracture.
Materials and Methods
For casting the patient is seated, a stockinette is applied and soft roll is used for undercast padding from the deltoid insertion to the distal palmar crease with a slit in the cotton wool for the first web space. The cotton wool is gently wound around the forearm giving an overlap of 50% The POP roll is dipped in the water and applied with one complete turn around the wrist it is then passed through the first web space and continues proximally around the forearm in the same manner as the soft roll with an overlap of 50% with elbow in 90° flexion and full supination. Cast is molded to the desired shape and the initial set of the plaster can be folded over at the ends and around the thumb and ensure uniform thickness of the cast the plaster roll should remain in contact with the cast while the cast is formed to avoid overtightening. The hand the exercises for the patient may now be explained and a sling is provided to support the weight of the cast.
For CRIF with K-Wiring, the patient was placed supine on the table of operation with a radiolucent hand table. Scrubbing, painting, and draping of the upper limb is done. After the necessary fixation forearm is supinated and appropriate-sized k-wire is passed transversely from about 1 cm below the ulna styloid to about 1cm below the radial styloid with a drill under fluoroscopic guidance. The remaining k-wire is cut and bent. Pin tract dressing is done and stabilized in a slab.
For TFCC repair, the patient was placed supine on the table of operation. Scrubbing, painting, and draping of the upper limb is done. Through the palmar surgical approach, the ulnar fovea is exposed through a transverse capsulotomy of the DRUJ without exploring the floor of the ECU tendon sheath and the superficial dorsal limb. ECU tendon sheath and the ulnotriquetral ligament are dissected to expose TFCC’s distal aspect. The suture anchor technique is used to suture back the deep palmar and dorsal limbs of the TFCC to the fovea after the scar tissue in the fovea is curettage.
Results
According to Table 1 and Fig. 1, the mean age of CRIF with k-wiring for der and casting patients was 49.18 years (SD = 17.29), the mean age of CRIF with k-wiring for der and TFCC repair patients was 36.33 years (SD = 2.30), the mean age of ORIF with plating for der and casting patients was 50.79 years (SD = 11.93), and the mean age of ORIF with plating for der and TFCC repair patients was 54.0 years. As per ANOVA, there was no significant difference in age between groups (P > 0.05).
Table 1.
Age
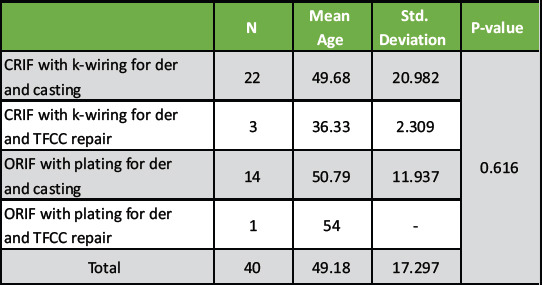
Figure 1.
Sex.
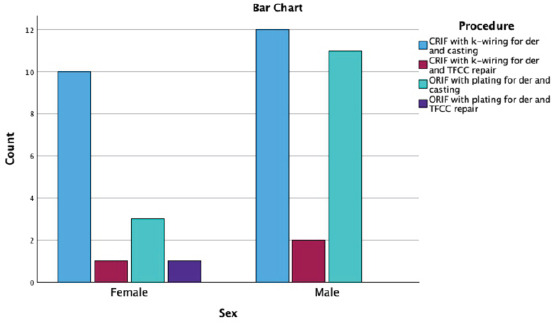
As per Table 2 and Fig. 2, there were 10 females and 12 males for CRIF with k-wiring for der and casting, 1 female and 2 males for CRIF with k-wiring for der and TFCC repair, 3 females and 11 males for ORIF with plating for der and casting, and 1 female for ORIF with plating for der and TFCC repair. As per Chi-square, there was no significant association between sex and procedure (P > 0.05).
Table 2.
Sex
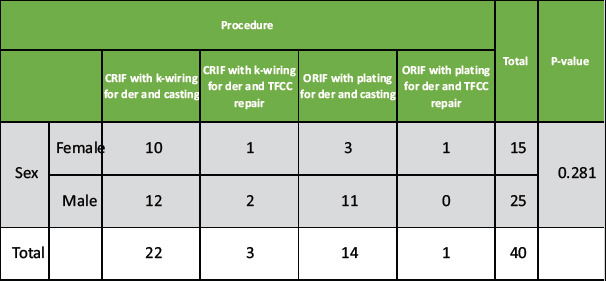
Figure 2.
Outcome.
As per Table 3 and Fig. 3, patients with ORIF with plating for der and casting had the highest grip strength (kg) (42.57 ± 15.33), whereas patients with ORIF with plating for der and TFCC repair had the lowest grip strength (kg) (17.0). As per ANOVA, there was no significant difference in grip strength between the groups (P > 0.05).
Table 3.
Comparing grip strength
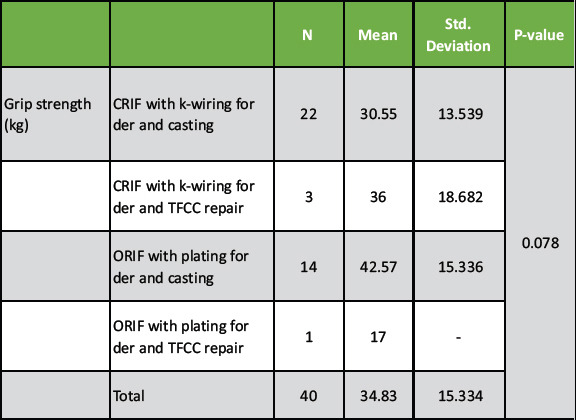
Figure 3.
DRUJ Instability.
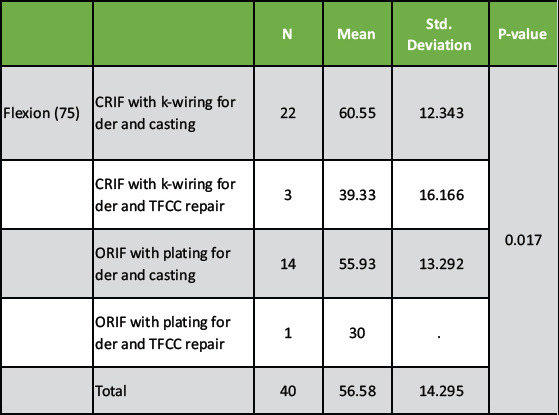
As per Table 4, patients with CRIF with k-wiring for der and casting had the highest flexion (75) (60.55 ± 12.34), whereas patients with ORIF with plating for der and TFCC repair had the lowest flexion (75) (30.0). As per ANOVA, there was a significant difference in flexion between the groups (P < 0.05).
Table 4.
Comparing flexion
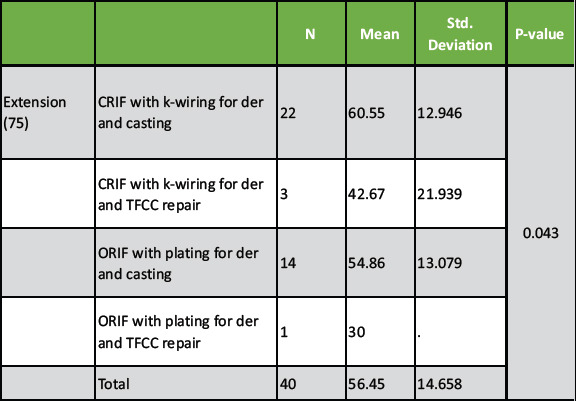
As per Table 5, patients with CRIF with k-wiring for der and casting had the highest extension (75) (60.55 ± 12.94), whereas patients with ORIF with plating for der and TFCC repair had the lowest extension (75) (30.0). As per ANOVA, there was a significant difference in extension between the groups (P < 0.05).
Table 5.
Comparing extension
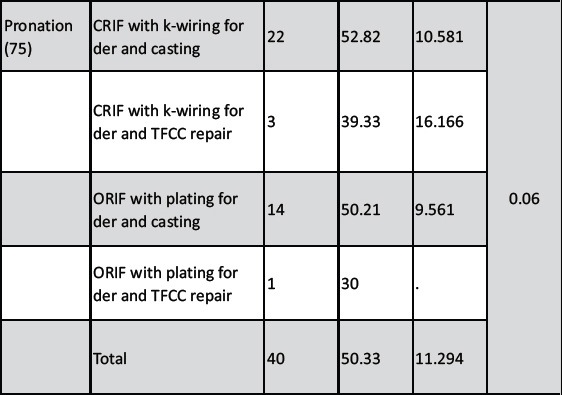
As per Table 6, patients with CRIF with k-wiring for der and casting had the highest pronation (75) (52.82 ± 10.58), whereas patients with ORIF with plating for der and TFCC repair had the lowest pronation (75) (30.0). As per ANOVA, there was no significant difference in pronation between the groups (P > 0.05).
Table 6.
Comparing pronation
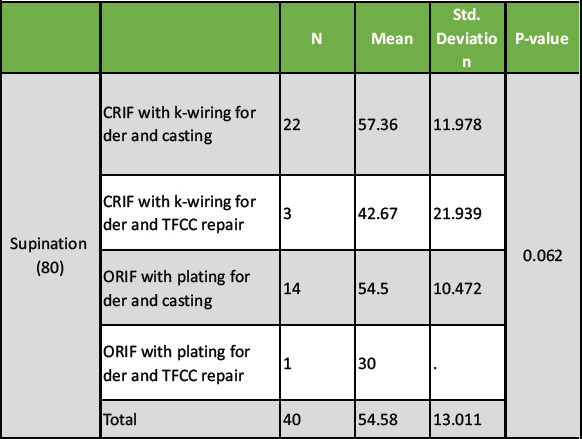
As per Table 7, patients with CRIF with k-wiring for der and casting had the highest supination (80) (57.36 ± 11.97), whereas patients with ORIF with plating for der and TFCC repair had the lowest supination (80) (30.0). As per ANOVA, there was no significant difference in supination between the groups (P > 0.05).
Table 7.
Comparing supination
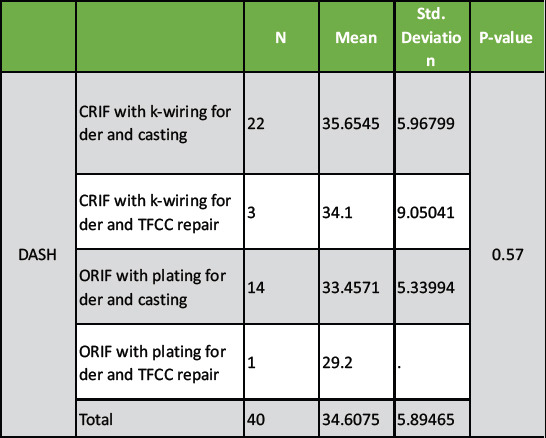
As per Table 8, patients with CRIF with k-wiring for der and casting had the highest DASH score (35.65 ± 5.96), whereas patients with ORIF with plating for der and TFCC repair had the lowest DASH score (29.20). As per ANOVA, there was no significant difference in DASH score between the groups (P > 0.05).
Table 8.
Comparing DASH
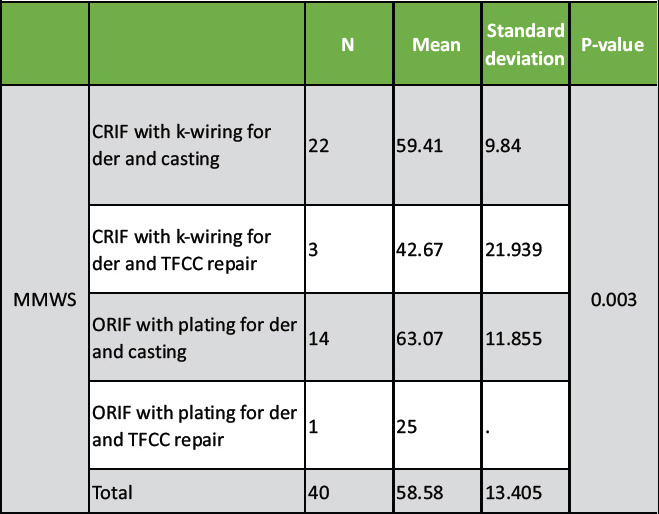
As per Table 9, patients with ORIF with plating for der and casting had the highest MMWS (63.07 ± 11.85), whereas patients with ORIF with plating for der and TFCC repair had the lowest MMWS (25.00). As per ANOVA, there was a significant difference in MMWS between the groups (P < 0.05).
Table 9.
Comparing MMWS
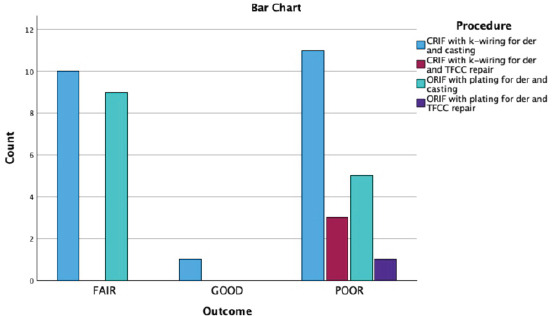
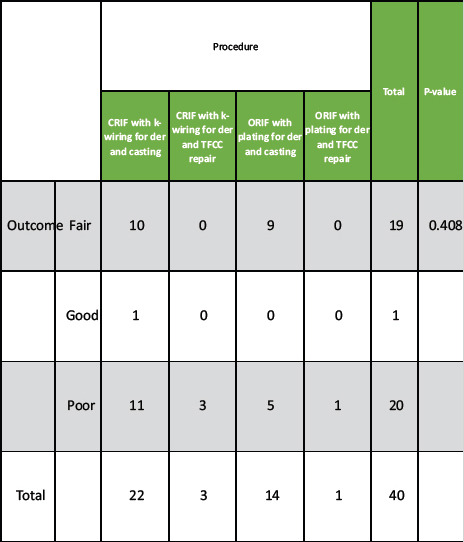
As per Table 10, out of 19 patients who had fair outcome, 10 had CRIF with k-wiring for der and casting and 9 had ORIF with plating for der and casting. Further, out of 20 patients who had poor outcome, 11 had CRIF with k-wiring for der and casting and 14 had ORIF with plating for der and casting. Further, as per ANOVA, there was no significant association between outcome and procedure (P > 0.05).
Table 10.
Outcome
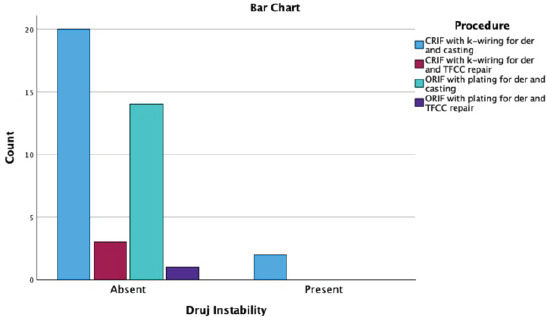
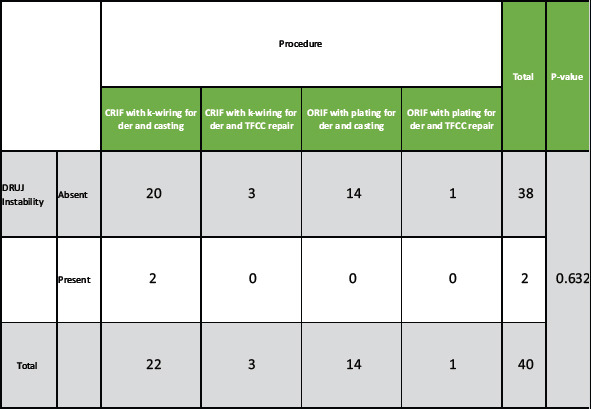
As per Table 11, out of 38 patients in which DRUJ instability was absent, 20 had CRIF with k-wiring for der and casting and 14 had ORIF with plating for der and casting. Further, out of 2 patients in which DRUJ Instability was present, 2 had CRIF with k-wiring for der and casting. Further, as per ANOVA, there was no significant association between DRUJ Instability and procedure (p>.05).
Table 11.
DRUJ instability
Discussion
The treatment groups that were identified included both surgical and conservative approaches, more invasive TFCC surgery or cast immobilization and K-wire stabilization of the ulna and radius. The DASH and MMWS were used to quantify patient outcomes. The DASH revealed no differences between the groups, whereas the MMWS preferred K-wire stabilization over TFCC repair. The MMWS is a physician-based rating system that takes into account the pain, grip strength, active flexion/extension arc, and return to work or activity capacity of the physician [8]. Considering that K-wire patients had stronger grips than TFCC patients did, it makes sense to observe a similar tendency in the MMWS score. It is interesting to note that patients self-administer the DASH based on their opinion of their level of recovery.
As per the study of Rubio (2021) [9], when TFCC repair was compared to K-wire and cast immobilization, in terms of functional outcome markers, grip strength, or range of motion, it did not show any better treatment improvement. The requirement for TFCC surgery is eliminated by prior research that supports the theory that stable anatomic DRF fixation is sufficient to produce a favorable long-term clinical outcome. Research has also shown that 97% of patients experience no discomfort and that residual DRUJ laxity is common (45%) after an untreated TFCC injury following DRF surgery.
Furthermore, the study of Vignesh and Singh (2022) [10] also emphasized that, even while the influence of ulnar styloid fractures on DRUJ instability was not directly addressed in this study, therapy for these fractures. A recent study by Giddins (2023) [11] has shown that the functional and clinical results of DRF therapy have not been found to be significantly correlated with an ulnar styloid fracture, regardless of the size or displacement of the ulnar styloid fragment, despite some research suggesting that ulnar styloid base fractures may lead to joint instability.
Conclusion
The major findings of analysis have suggested that the time, effort, and cost of TFCC repair do not appear to be necessary, however, there may be trade-offs between various treatments, with K-wire stabilization offering a better range of motion and cast immobilization a stronger grip. Larger controlled trials, on the other hand, ought to be carried out to clarify these variations and their effects on patient satisfaction and functional outcomes.
Clinical Message.
The evaluation suggests that the resources spent on TFCC repair may not be warranted. K-wire stabilization greatly improves mobility, enabling faster recovery for patients. Conversely, cast immobilization can enhance grip strength, which is crucial for rehabilitation. Considering these elements is vital for achieving the best patient outcomes and tailoring treatment to specific recovery objectives considering their unique needs and lifestyles. A holistic strategy can result in improved long-term results and higher patient satisfaction with reducing complications and recovery time.
Biography





Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Spies CK, Langer M, Müller LP, Oppermann J, Unglaub F. Distal radioulnar joint instability:Current concepts of treatment. Arch Orthop Trauma Surg. 2020;140:639–50. doi: 10.1007/s00402-020-03371-0. [DOI] [PubMed] [Google Scholar]
- 2.Qazi S, Graham D, Regal S, Tang P, Hammarstedt JE. Distal radioulnar joint instability and associated injuries:A literature review. J Hand Microsurg. 2021;13:123–31. doi: 10.1055/s-0041-1730886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chhabra AB, Yildirim B. Adult distal radius fracture management. J Am Acad Orthop Surg. 2021;29:e1105–16. doi: 10.5435/JAAOS-D-20-01335. [DOI] [PubMed] [Google Scholar]
- 4.Barger J, Lasa S, Dell'Oca AF, Jupiter J. Operative stabilization of distal radius fractures presenting with ulnar head subluxation/dislocation addresses distal radioulnar joint instability without further stabilization procedures. J Orthop Trauma. 2022;36:e174–81. doi: 10.1097/BOT.0000000000002286. [DOI] [PubMed] [Google Scholar]
- 5.Ross PR, Chung KC. Instability in the setting of distal radius fractures:Diagnosis, evaluation, and treatment. Hand Clin. 2020;36:417–27. doi: 10.1016/j.hcl.2020.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Li C, Kong L, Shi X, Zhang Z, Lu J, Zhang B. Predictive factors of distal radioulnar joint instability after surgical treatment of distal radius fractures. Medicine (Baltimore) 2023;102:e36505. doi: 10.1097/MD.0000000000036505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hruby LA, Haider T, Laggner R, Gahleitner C, Erhart J, Stoik W, et al. Standard radiographic assessments of distal radius fractures miss involvement of the distal radioulnar joint:A diagnostic study. Arch Orthop Trauma Surg. 2021;142:1075–82. doi: 10.1007/s00402-021-03801-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carr LW, Adams B. Chronic distal radioulnar joint instability. Hand Clin. 2020;36:443–53. doi: 10.1016/j.hcl.2020.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Rubio F. Distal radioulnar joint, distal ulna injury, and lunate facet considerations in distal radius fractures. J Orthop Trauma. 2021;35:s11–6. doi: 10.1097/BOT.0000000000002202. [DOI] [PubMed] [Google Scholar]
- 10.Vignesh S, Singh C. Management of chronic distal radio-ulnar joint (DRUJ) instability using adams-berger technique-a report of two cases in different scenarios. J Orthop Rep. 2022;1:100058. [Google Scholar]
- 11.Giddins G. The distal radioulnar joint after distal radial fractures:When and how do we need to treat pain, stiffness or instability? J Hand Surg Eur Vol. 2023;48:230–45. doi: 10.1177/17531934221140238. [DOI] [PubMed] [Google Scholar]
- 12.Moritomo H. Open repair of the triangular fibrocartilage complex from palmar aspect. J Wrist Surg. 2015;4:2–8. doi: 10.1055/s-0034-1398474. [DOI] [PMC free article] [PubMed] [Google Scholar]


