Abstract
Introduction:
This report describes the use of a combination of a retrograde femoral nail and distal femur locking plate for the treatment of an open intra-articular distal femur fracture in a 99-year-old female. The purpose of this report is to highlight that nail-plate fixation constructs can be performed percutaneously and expeditiously even in extremely old patients; therefore, patient age should not be a limiting factor in choosing this construct to allow for immediate weight-bearing.
Case Report:
The patient was a 99-year-old female who presented to the emergency room after a fall. Plain radiographs demonstrated a comminuted supracondylar distal femur fracture with a sagittal intercondylar split (OTA classification 33A3.3). She was indicated for operative repair and was fixed with a combination of a retrograde Stryker T2 alpha nail and Stryker distal femur locking plate. This method was chosen to allow the patient to be weight-bearing as tolerated after surgery so she could immediately start work with physical therapy to work towards getting back to her pre-injury ambulatory status. At 3 months post-operatively, she had minimal pain, no difficulties with activities of daily living, and was ambulating with the assistance of a cane. At 9 months post-operatively, she was ambulating with a cane (pre-injury status). She did not report any pain, and her radiographs illustrated fracture site consolidation. Furthermore, her short musculoskeletal functional assessment score was the same as it was pre-injury (81).
Conclusion:
This case supports the idea of using a nail-plate combination for repair of intra-articular distal femur fractures, even in the very elderly as the patient’s functional outcome data reached pre-injury levels. In addition, it allows even elderly patients to begin early weight-bearing and decreases complications related to lack of extremity use.
Keywords: Distal femur, femoral nail, distal locking plate, geriatric, open fracture
Learning Point of the Article:
Age should not deter orthopedic surgeons from using this specific fixation method in patients with a distal femur fracture.
Introduction
Distal femur fractures in the elderly result predominantly from low-energy trauma due to osteoporosis and have an incidence of 0.4% of all fractures [1]. Surgical treatment is performed with the goal of achieving pain control, improving patient mobility to allow for hygiene, and to achieve weight bearing as rapidly as possible. To achieve immediate weight-bearing-as-tolerated status, there is no consensus regarding the best fixation construct with studies suggesting single plate, dual plate, retrograde nail, or combination nail-plate constructs [1]. We report a case of an elderly open intra-articular distal femur fracture that was treated with the combination of retrograde intramedullary nailing and locking plate fixation. The purpose of this case report is to highlight that patient age should not be a limiting factor in choosing this construct to allow for immediate weight-bearing.
Case Report
The patient was a 99-year-old female, a community ambulator with a cane, who presented after a fall from a standing height. Her past medical history was notable for hypertension, hyperlipidemia, chronic kidney disease stage 3A, and anemia. There was an obvious deformity of the left thigh as well as a punctate wound over the anterior distal thigh measuring two centimeters. She had a normal distal neurovascular examination. Plain radiographic images were obtained of her left femur and knee demonstrating a comminuted supracondylar distal femur fracture with a sagittal intercondylar split (OTA classification 33A3.3) (Fig. 1a and b). A CT scan of her knee was obtained confirming her radiographic findings (Fig. 2a-c) and air around the fracture site.
Figure 1.

Injury Radiographs; Anteroposterior (a) and lateral (b) radiographs of a comminuted supracondylar, intra-articular distal femur fracture (sagittal intercondylar split) [AO/OTA 33A3.3].
Figure 2.
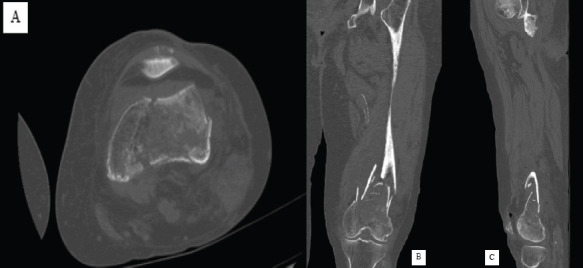
Injury CT Scan; An axial (a), coronal (b), and sagittal (c) CT scan of comminuted supracondylar, intra-articular distal femur fracture (sagittal intercondylar split) [AO/OTA 33A3.3].
The patient was indicated for operative repair of the intra-articular and femoral shaft components. She received standard open fracture antibiotic prophylaxis for a Type 1 open distal femur fracture which included 2 g intravenous Cefazolin. Pre-operative protocols were undertaken and informed consent was obtained. Standard perioperative antibiotics were administered, and sterile prepping and draping were performed.
The open fracture site was first extended into an anterolateral approach to the distal femur to allow for proper visualization of the zone of injury, and the open fracture was irrigated and debrided. Attention was first turned to the intra-articular component where two cannulated 5.0 mm screws were placed percutaneously from medial to lateral to compress the fracture line.
Next, the femoral shaft component was addressed and a retrograde nail was inserted across the fracture. The decision was then made to further stabilize the intra-articular distal component via additional plate and screw fixation. Through the anterolateral incision, a distal femur locking plate was applied to the bone and a series of locking screws were placed proximally and distally (Fig. 3a and b).
Figure 3.
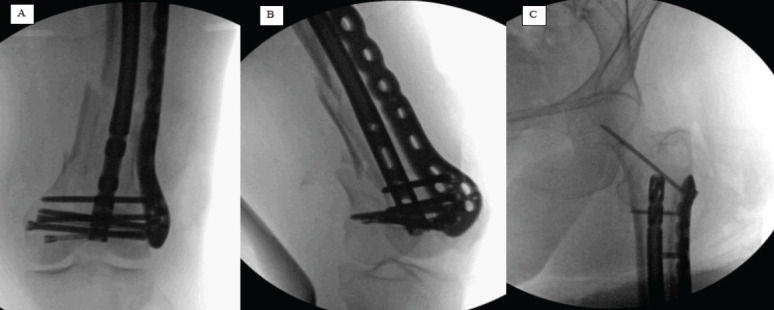
Intraoperative Radiographs; Anteroposterior (A) and lateral (B) intraoperative fluoroscopy of retrograde femoral nail in combination with distal femur locking plate along with anteroposterior intraoperative fluoroscopy of a femoral neck reinforcement screw originating from proximal portion of distal femur locking plate [C].
Due to the patient’s pathological fracture secondary to osteoporosis, a reinforcement screw was placed from the plate across her femoral neck and head to minimize the risk of future fracture in this area (Fig. 3c). The surgical wounds were closed with absorbable braided sutures for the subcutaneous tissues and nylon sutures for the skin. The patient was transferred to the recovery room in stable condition.
At baseline, she ambulated with a cane. She was made weight-bearing-as-tolerated immediately after surgery. Physical therapy began on post-operative day one. She needed a rolling walker to ambulate but was able to take four steps. She continued to improve her ambulatory status as she walked five feet, six feet with two 90° turn, eight feet, and finally ten feet on post-operative day eight. She was discharged to a rehab facility for further care.
At 3 months follow-up, she reported minimal pain and was independently ambulating with a walker (Fig. 4). She was having no difficulty with her activities of daily living. At her most recent 9-month follow-up visit, she was back to ambulating with a cane and subjectively felt better than she did at her 3-month visit. She had no tenderness to palpation and had no pain with prolonged walking or other activities of daily living. Her X-rays demonstrated union at the fracture site with consolidation of her callus on three out of four cortices (Fig. 5a and b). She had returned to her baseline level before surgery with her reported short musculoskeletal functional assessment (SMFA) at 9 months (81) equivalent to her baseline pre-injury SMFA (81).
Figure 4.

Patient ambulating; patient ambulating with the use of a walker at 3 months post-operatively.
Figure 5.

Nine-month post-operative radiographs; anteroposterior (a) and lateral (b) radiographs at 9 months postoperatively demonstrating bony union across the fracture site.
Discussion
This case illustrates the effectiveness of combined intramedullary nail and plate fixation for intra-articular distal femur fractures in elderly patients. This patient was able to function independently and returned to her baseline functional status. Because she was allowed to bear her full weight immediately, and she had a stiff construct that minimized motion at the fracture site thereby decreasing pain, she likely was able to maintain her extremity muscle mass and minimize atrophy [2]. In addition, immediate loading of the fracture site stimulates healing so it was advantageous to make her weight-bearing as tolerated [3]. It is possible that a single construct alone may have been sufficient to allow immediate weight-bearing, however, the addition of another form of fixation likely increased the likelihood of immediate weight-bearing [4].
Literature is limited regarding the outcomes of patients treated with this specific fixation combination, although their mortality and morbidity are comparable to femoral neck fractures which have been studied extensively [5]. In addition, distal femur fractures have been studied following intramedullary nailing or plate and screw fixation [3, 6-8]. The patient’s outcome agrees with recent findings regarding the nail-plate combination surgery for distal femur fractures. Galante et al. reported on fourteen patients with a comminuted distal articular femur fracture who were treated with a nail-plate combination. At 1 year, all patients could bear full weight with mild pain or no pain at all [7]. The case reported here showed resolution of pain at the 6-month follow-up visit in a patient who is significantly older than those included in the case series (99 years old vs. 48.5 ± 18.05 years old). Liporace et al. reported positive outcomes for their cohort of 15 patients (mean age 74.8 ± 5.8 years) who had nail-plate repair; all of the patients who followed up healed and remained ambulatory, albeit most had to use an assistive device [8].
The advantages of the nail-plate fixation technique for distal femur fractures is based on the idea of added axial loading tolerance from the nail combined with the torsional stability from the plate [9]. Fontenot et al. undertook a biomechanical study comparing the nail-plate combination to other fixation techniques. The lateral locking plate was used as a baseline in the study, and the nail-plate combination was found to have the highest baseline stiffness. It was significantly higher than two out of the three comparison groups as well [10]. Loading in the axial plane was also evaluated. Again, the nail-plate combination had the most number of cycles until reaching failure and was again significantly greater than two out of the three comparison groups one of which being just the lateral locking plate [10].
Conclusions
This case supports the idea of using a nail-plate combination for the repair of intra-articular distal femur fractures in the very elderly. Functional outcome data suggests that patients do very well after this procedure and there is a biomechanical basis for its advantages. This is the oldest patient noted in the literature to have a combined intramedullary nail and plate fixation to return to baseline functional and ambulatory status 9 months following surgery.
Clinical Message.
Nail-plate combination fixation is a suitable technique for patients of all ages as it maximizes functional outcome scores and leads to early weight-bearing.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Aggarwal S, Rajnish RK, Kumar P, Srivastava A, Rathor K, Ul Haq R. Comparison of outcomes of retrograde intramedullary nailing versus locking plate fixation in distal femur fractures:A Systematic Review and Meta-analysis of 936 patients in 16 studies. J Orthop. 2023;36:36–48. doi: 10.1016/j.jor.2022.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dirks ML, Wall BT, van de Valk B, Holloway TM, Holloway GP, Chabowski A, et al. One week of bed rest leads to substantial muscle atrophy and induces whole-body insulin resistance in the absence of skeletal muscle lipid accumulation. Diabetes. 2016;65:2862–75. doi: 10.2337/db15-1661. [DOI] [PubMed] [Google Scholar]
- 3.Windolf M, Ernst M, Schwyn R, Arens D, Zeiter S. The relation between fracture activity and bone healing with special reference to the early healing phase - A preclinical study. Injury. 2021;52:71–7. doi: 10.1016/j.injury.2020.10.050. [DOI] [PubMed] [Google Scholar]
- 4.Lieder CM, Gaski GE, Virkus WW, Kempton LB. Is immediate weight-bearing safe after single implant fixation of elderly distal femur fractures? J Orthop Trauma. 2021;35:49–55. doi: 10.1097/BOT.0000000000001882. [DOI] [PubMed] [Google Scholar]
- 5.Konda SR, Pean CA, Goch AM, Fields AC, Egol KA. Comparison of short-term outcomes of geriatric distal femur and femoral neck fractures. Geriatr Orthop Surg Rehabil. 2015;6:311–5. doi: 10.1177/2151458515608225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Egol KA, Broder K, Fisher N, Konda SR. Repair of displaced partial articular fracture of the distal femur:The Hoffa fracture. J Orthop Trauma. 2017;31(Suppl 3):S10–1. doi: 10.1097/BOT.0000000000000896. [DOI] [PubMed] [Google Scholar]
- 7.Galante C, Djemetio MD, Fratus A, Cattaneo S, Ronchi S, Domenicucci M, et al. Management of distal femoral fractures with metaphyseal and articular comminution (AO/OTA 33C) using nail and plate fixation:A technical note and case series of 14 patients. Eur J Orthop Surg Traumatol. 2023;33:3519–29. doi: 10.1007/s00590-023-03577-z. [DOI] [PubMed] [Google Scholar]
- 8.Liporace FA, Yoon RS. Nail plate combination technique for native and periprosthetic distal femur fractures. J Orthop Trauma. 2019;33:e64–8. doi: 10.1097/BOT.0000000000001332. [DOI] [PubMed] [Google Scholar]
- 9.Kontakis MG, Giannoudis PV. Nail plate combination in fractures of the distal femur in the elderly:A new paradigm for optimum fixation and early mobilization? Injury. 2023;54:288–91. doi: 10.1016/j.injury.2022.11.035. [DOI] [PubMed] [Google Scholar]
- 10.Fontenot PB, Diaz M, Stoops K, Barrick B, Santoni B, Mir H. Supplementation of lateral locked plating for distal femur fractures:A biomechanical study. J Orthop Trauma. 2019;33:642–8. doi: 10.1097/BOT.0000000000001591. [DOI] [PubMed] [Google Scholar]


