Abstract
Introduction:
Calcific tendonitis is characterized by calcium hydroxyapatite crystal deposition in tendons, leading to inflammation and pain. While predominantly observed in the rotator cuff tendons of the shoulder, its occurrence in the rectus femoris tendon of the hip is exceedingly rare and poses a diagnostic challenge.
Case Report:
A 38-year-old female housewife presented with a 1-month history of left hip pain, which was dull, aching, and exacerbated by movements such as standing and walking. High-resolution computed tomography imaging showed calcification at the insertion of the left rectus femoris muscle. A magnetic resonance imaging confirmed the diagnosis, revealing no significant abnormalities in the hip joints or surrounding structures. The patient was diagnosed with calcific tendonitis at the insertion of the left rectus femoris muscle and was managed conservatively with rest, Non-steroidal anti-inflammatory drugs, and physical therapy. Follow-up visits were scheduled to monitor her progress and response to treatment.
Conclusion:
This case underscores the importance of thorough clinical and imaging evaluations in diagnosing calcific tendonitis in atypical locations. Conservative treatment proved effective, highlighting the need for tailored management strategies. Future research should focus on elucidating the pathogenesis and optimizing treatment for calcific tendonitis in uncommon sites.
Keywords: Calcific tendonitis, rectus femoris, hip pain, conservative management, imaging, case report
Learning Point of the Article:
Accurate diagnosis and effective conservative management of calcific tendonitis in the rectus femoris tendon hinge on comprehensive clinical evaluation and advanced imaging techniques.
Introduction
Calcific tendonitis is a condition marked by the deposition of calcium hydroxyapatite crystals within the tendons, leading to inflammation and pain. It is most frequently observed in the rotator cuff tendons of the shoulder but can also occur in other tendons, including those in the hip region, albeit rarely [1-3]. The disease progresses through several stages, beginning with a fibrocartilaginous transformation of the tendon, followed by calcium deposition, and eventually, resorption and healing of the tendon [3]. In the hip, calcific tendonitis can often mimic other conditions such as bursitis, arthritis, or tendinitis of different tendons, which complicates the diagnosis [4-6].
Despite being a well-documented condition, the exact pathogenesis of calcific tendonitis remains poorly understood. The literature lacks comprehensive data on the occurrence and management of calcific tendonitis specifically in the rectus femoris tendon. Most studies focus on the rotator cuff, leaving a significant gap in understanding regarding the clinical presentation, optimal diagnostic approach, and effective treatment strategies for calcific tendonitis in less common locations such as the hip [3, 7]. Furthermore, there is limited information on the long-term outcomes of various treatment modalities, particularly conservative versus interventional approaches, in managing calcific tendonitis of the rectus femoris [3, 8].
This paper presents a case of a 38-year-old female with calcific tendonitis of the left rectus femoris muscle, highlighting the clinical presentation, diagnostic process, and treatment plan. The report aims to contribute to the limited body of knowledge on this rare condition, offering insights into its management and potential outcomes.
Case Report
A 38-year-old female housewife presented to the outpatient department at RML Hospital with the chief complaint of pain in the left hip region that had persisted for 1 month. The patient had been asymptomatic until the sudden onset of pain, which began abruptly and progressively worsened over the initial 2 days. The pain was described as dull and aching in nature and was localized, not radiating to other regions. The discomfort was notably exacerbated by movements such as getting up from a sitting position, walking, and standing. However, the pain was alleviated by rest, the intake of painkillers, and lying down with the legs straightened. The patient reported no associated symptoms such as fatigue, weight loss, or loss of appetite. There was no history of trauma, fever, heavy exertion, or lifting weights that could have precipitated the condition. In addition, the patient denied having any chronic illnesses or a history of regular medication intake. Her past medical history was insignificant, with no previous significant illnesses or surgeries. The patient maintained a mixed diet and had a history of normal vaginal delivery. She reported a normal menstrual cycle with no irregularities. The family history was unremarkable for any similar musculoskeletal complaints or chronic diseases. Furthermore, the patient was a non-smoker and non-alcoholic, maintaining regular bladder and bowel habits. During the physical examination, tenderness was noted over the left anterior inferior iliac spine. No distal neurovascular deficits were observed, indicating that the nerve supply and blood flow to the area were intact. The range of motion in the left hip was assessed, revealing restricted and painful flexion up to 70°. Other movements of the hip, such as adduction, abduction, and extension, were painful but not restricted, suggesting that the primary issue was localized rather than affecting the entire hip joint.
Plain radiograph of pelvis with bilateral hips revealed suspicious calcific deposits in the lip of the left acetabulum (Fig. 1). Patient was given analgesics and rest for some time but she had some relief. Later a high-resolution axial series was obtained computed tomography (CT) scan. The CT findings revealed calcification at the insertion of the left rectus femoris muscle, anterior to the anterior inferior iliac spine (Fig. 2). Both hip joints appeared normal with no evidence of articular surface erosion, indicating that the joints themselves were not the source of the pain. The acetabular cups were normal in morphology, suggesting that the hip sockets were intact and unaffected. No significant joint effusion was seen, ruling out any major inflammatory process within the hip joint. The bilateral sacroiliac joint spaces were normal, indicating that the pain was not originating from these joints. In addition, the rest of the visualized muscles and soft-tissue planes were unremarkable, further localizing the problem to the insertion of the rectus femoris muscle. Correlating the CT findings with a magnetic resonance imaging (MRI) study, the diagnosis of calcific tendonitis at the insertion of the left rectus femoris muscle was confirmed. The MRI findings supported the absence of any significant abnormalities in the hip joints and surrounding structures, corroborating the diagnosis made through CT imaging (Fig. 3). Based on the clinical presentation, physical examination, and imaging studies, the patient was diagnosed with calcific tendonitis at the insertion of the left rectus femoris muscle, anterior to the anterior inferior iliac spine. The patient was advised to continue rest and avoid activities that exacerbated the pain, with follow-up visits scheduled to monitor progress and response to treatment.
Figure 1.

Plain radiograph of pelvis with bilateral hips showing calcific deposits in the lip of the left acetabulum
Figure 2.
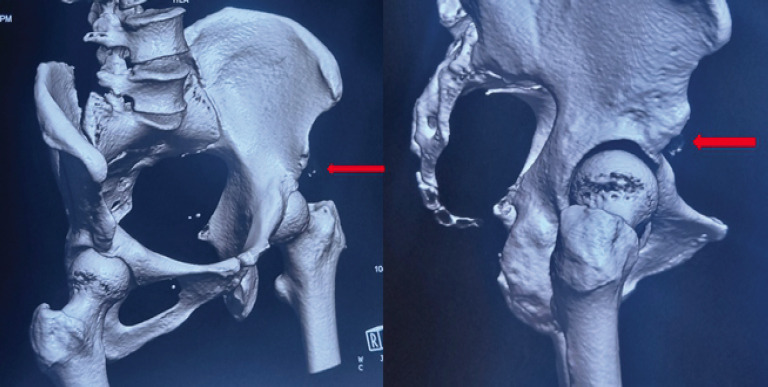
Computed tomography scan with 3D reconstruction of pelvis with bilateral hips showing calcific deposits in the lip of left acetabulum
Figure 3.
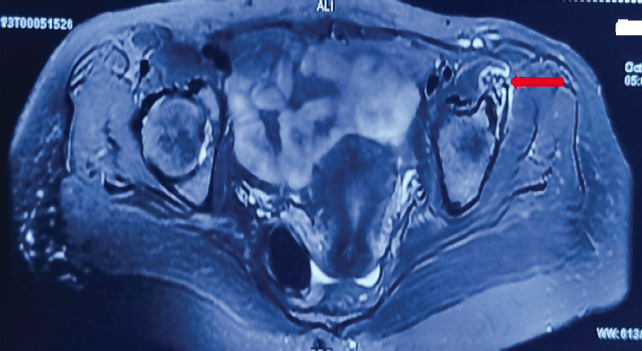
T2W-MRI of pelvis with bilateral hips showing calcific deposits in the lip of the left acetabulum
Discussion
Calcific tendonitis is a condition characterized by the deposition of calcium hydroxyapatite crystals in the tendons, leading to inflammation and pain [9]. It is most commonly observed in the rotator cuff tendons of the shoulder but can occur in other tendons, including those in the hip [10, 11]. The exact etiology of calcific tendonitis is not well understood, but it is thought to involve a combination of metabolic, genetic, and mechanical factors [12].
The pathophysiological process of calcific tendonitis typically involves three stages [13]. The first is the pre-calcific stage, which involves the fibrocartilaginous transformation of the tendon. This stage sets the groundwork for the subsequent deposition of calcium. The second stage, known as the calcific stage, is characterized by the formation and deposition of calcium crystals within the tendon. This stage can be further divided into three phases: The formative phase, where calcium crystals are initially deposited; the resting phase, where these crystals stabilize within the tendon; and the resorptive phase, during which the body attempts to reabsorb the calcium deposits, often accompanied by intense inflammation and pain. The final stage is the post-calcific stage, wherein the tendon undergoes healing and remodeling following the resorption of calcium deposits [13].
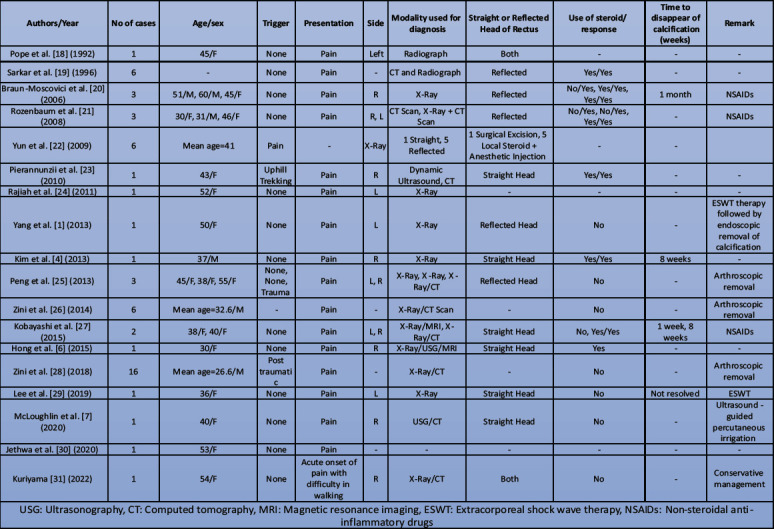
Patients with calcific tendonitis typically present with acute or chronic localized pain, often aggravated by movement and relieved by rest. In the hip, the condition can mimic other causes of hip pain, such as bursitis, arthritis, or tendonitis of other tendons, making imaging studies crucial for accurate diagnosis. Imaging plays a key role in the diagnosis and management of calcific tendonitis [3, 10, 14, 15]. Plain radiographs may reveal calcific deposits, but CT and MRI provide more detailed information regarding the extent and precise location of the calcification and associated soft-tissue changes [11, 14, 16, 17]. CT scans are particularly useful for identifying the characteristic calcific deposits, while MRI is excellent for assessing associated inflammatory changes and excluding other pathologies. A review of the literature reveals several important aspects of calcific tendinitis of the rectus femoris were tabulated in Table 1.
Table 1.
Review of literature of calcific tendinitis of the rectus femoris.
The management of calcific tendonitis involves a combination of conservative and interventional approaches [9, 11, 32-34]. Conservative treatment primarily includes rest, medications, and physical therapy. Rest involves avoiding activities that exacerbate the pain. Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to reduce inflammation and pain. Physical therapy focuses on exercises to improve the range of motion and strengthen the surrounding muscles. In cases where conservative treatment is ineffective, interventional options may be considered. Extracorporeal shock wave therapy is a non-invasive procedure that uses shock waves to break down the calcium deposits and stimulate healing. Another minimally invasive procedure is ultrasound-guided needle lavage, which involves aspirating the calcium deposits. In refractory cases, surgical removal of the calcific deposits may be necessary. The prognosis for calcific tendonitis is generally favorable, especially with appropriate treatment. Most patients experience significant improvement in symptoms with conservative management. Interventional treatments can provide relief for those with persistent symptoms. Recurrence of calcific deposits is uncommon, but regular follow-up may be warranted to monitor for potential complications. Through a combination of accurate diagnosis, effective treatment, and appropriate follow-up, patients with calcific tendonitis can achieve substantial relief and return to normal function.
Conclusion
The successful diagnosis and management of calcific tendonitis of the rectus femoris underscore the need for heightened clinical awareness and individualized treatment strategies. Future studies are warranted to further elucidate the pathogenesis and optimal management approaches for calcific tendonitis in atypical locations. This case contributes valuable insights to the limited body of literature on calcific tendonitis of the rectus femoris, emphasizing the efficacy of current diagnostic and therapeutic modalities in achieving favorable patient outcomes.
Clinical Message.
Accurate diagnosis of calcific tendonitis in atypical locations, such as the rectus femoris tendon, requires thorough clinical evaluation and advanced imaging.
Conservative management is effective, but individualized treatment strategies are crucial for optimal outcomes.
Biography
Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Yang JH, Oh KJ. Endoscopic treatment of calcific tendinitis of the rectus femoris in a patient with intractable pain. J Orthop Sci. 2013;18:1046–9. doi: 10.1007/s00776-012-0250-8. [DOI] [PubMed] [Google Scholar]
- 2.Zini R, Panascì M, Papalia R, Franceschi F, Vasta S, Denaro V. Rectus femoris tendon calcification:Arthroscopic excision in 6 top amateur athletes. Orthop J Sports Med. 2014;2:2325967114561585. doi: 10.1177/2325967114561585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saran S, Babhulkar JA, Gupta H, Chari B. Imaging of calcific tendinopathy:Natural history, migration patterns, pitfalls, and management:A review. Br J Radiol. 2024;97:1099–111. doi: 10.1093/bjr/tqae039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim YS, Lee HM, Kim JP. Acute calcific tendinitis of the rectus femoris associated with intraosseous involvement:A case report with serial CT and MRI findings. Eur J Orthop Surg Traumatol. 2013;23:233–9. doi: 10.1007/s00590-012-1156-z. [DOI] [PubMed] [Google Scholar]
- 5.Comba F, Piuzzi NS, Zanotti G, Buttaro M, Piccaluga F. Endoscopic surgical removal of calcific tendinitis of the rectus femoris:Surgical technique. Arthrosc Tech. 2015;4:e365–9. doi: 10.1016/j.eats.2015.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hong MJ, Kim YD, Park JK, Kang TU. Successful treatment of rectus femoris calcification with ultrasound-guided injection:A case report. Korean J Pain. 2015;28:52–6. doi: 10.3344/kjp.2015.28.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McLoughlin E, Iqbal A, Tillman RM, James SL, Botchu R. Calcific tendinopathy of the direct head of rectus femoris:A rare cause of groin pain treated with ultrasound guided percutaneous irrigation. J Ultrasound. 2020;23:425–30. doi: 10.1007/s40477-019-00402-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skalski M. Calcific Tendinosis of the Rectus Femoris. Radiology Case. Radiopaedia. [[Last accessed on 2024 Jul 23]]. Available from: https://radiopaedia.org/cases/calcific-tendinosis-of-the-rectus-femoris.10.53347/rid-62772 .
- 9.Catapano M, Robinson DM, Schowalter S, McInnis KC. Clinical evaluation and management of calcific tendinopathy:An evidence-based review. J Osteopath Med. 2022;122:141–51. doi: 10.1515/jom-2021-0213. [DOI] [PubMed] [Google Scholar]
- 10.Albano D, Coppola A, Gitto S, Rapisarda S, Messina C, Sconfienza LM. Imaging of calcific tendinopathy around the shoulder:Usual and unusual presentations and common pitfalls. Radiol Med. 2021;126:608–19. doi: 10.1007/s11547-020-01300-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim MS, Kim IW, Lee S, Shin SJ. Diagnosis and treatment of calcific tendinitis of the shoulder. Clin Shoulder Elb. 2020;23:210–6. doi: 10.5397/cise.2020.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sansone V, Maiorano E, Galluzzo A, Pascale V. Calcific tendinopathy of the shoulder:Clinical perspectives into the mechanisms, pathogenesis, and treatment. Orthop Res Rev. 2018;10:63–72. doi: 10.2147/ORR.S138225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harvie P, Pollard TC, Carr AJ. Calcific tendinitis:Natural history and association with endocrine disorders. J Shoulder Elbow Surg. 2007;16:169–73. doi: 10.1016/j.jse.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Ricci V, Mezian K, Chang KV, Özçakar L. Clinical/sonographic assessment and management of calcific tendinopathy of the shoulder:A narrative review. Diagnostics (Basel) 2022;12:3097. doi: 10.3390/diagnostics12123097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chianca V, Albano D, Messina C, Midiri F, Mauri G, Aliprandi A. Rotator cuff calcific tendinopathy:From diagnosis to treatment. Acta Biomed. 2018;89:186–96. doi: 10.23750/abm.v89i1-S.7022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merolla G, Singh S, Paladini P, Porcellini G. Calcific tendinitis of the rotator cuff:State of the art in diagnosis and treatment. J Orthop Traumatol. 2016;17:7–14. doi: 10.1007/s10195-015-0367-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nörenberg D, Ebersberger HU, Walter T, Ockert B, Knobloch G, Diederichs G, et al. Diagnosis of calcific tendonitis of the rotator cuff by using susceptibility-weighted MR imaging. Radiology. 2016;278:475–84. doi: 10.1148/radiol.2015150034. [DOI] [PubMed] [Google Scholar]
- 18.Pope TL, Jr, Keats TE. Case report 733. Calcific tendinitis of the origin of the medial and lateral heads of the rectus femoris muscle and the anterior iliac spin (AIIS) Skeletal Radiol. 1992;21:271–2. doi: 10.1007/BF00243072. [DOI] [PubMed] [Google Scholar]
- 19.Sarkar JS, Haddad FS, Crean SV, Brooks P. Acute calcific tendinitis of the rectus femoris. J Bone Joint Surg Br. 1996;78:814–6. [PubMed] [Google Scholar]
- 20.Braun-Moscovici Y, Schapira D, Nahir AM. Calcific tendinitis of the rectus femoris. J Clin Rheumatol. 2006;12:298–300. doi: 10.1097/01.rhu.0000249896.43792.62. [DOI] [PubMed] [Google Scholar]
- 21.Rozenbaum M, Slobodin G, Boulman N, Feld J, Avshovich N, Rosner I. Calcific tendonitis of the rectus femoris. J Clin Rheumatol. 2008;14:57. doi: 10.1097/RHU.0b013e318163bdad. [DOI] [PubMed] [Google Scholar]
- 22.Yun HH, Park JH, Park JW, Lee JW. Calcific tendinitis of the rectus femoris. Orthopedics. 2009;32:490. doi: 10.3928/01477447-20090527-13. [DOI] [PubMed] [Google Scholar]
- 23.Pierannunzii L, Tramontana F, Gallazzi M. Case report:Calcific tendinitis of the rectus femoris:A rare cause of snapping hip. Clin Orthop Relat Res. 2010;468:2814–8. doi: 10.1007/s11999-009-1208-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rajiah P, Ilaslan H, Sundaram M. Radiologic case study. Calcific tendinitis of the rectus femoris with intraosseous extension of calcification. Orthopedics. 2011;34:329. doi: 10.3928/01477447-20110317-32. [DOI] [PubMed] [Google Scholar]
- 25.Peng X, Feng Y, Chen G, Yang L. Arthroscopic treatment of chronically painful calcific tendinitis of the rectus femoris. Eur J Med Res. 2013;18:49. doi: 10.1186/2047-783X-18-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zini R, Panascì M, Papalia R, Franceschi F, Vasta S, Denaro V. Rectus femoris tendon calcification:Arthroscopic excision in 6 top amateur athletes. Orthop J Sports Med. 2014;2:2325967114561585. doi: 10.1177/2325967114561585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kobayashi H, Kaneko H, Homma Y, Baba T, Kaneko K. Acute calcific tendinitis of the rectus femoris:A case series. J Orthop Case Rep. 2015;5:32–4. doi: 10.13107/jocr.2250-0685.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zini R, Panascì M. Post-traumatic ossifications of the rectus femoris:Arthroscopic treatment and clinical outcome after 2 years. Injury. 2018;49:S100–4. doi: 10.1016/j.injury.2018.09.062. [DOI] [PubMed] [Google Scholar]
- 29.Lee CH, Oh MK, Yoo JI. Ultrasonographic evaluation of the effect of extracorporeal shock wave therapy on calcific tendinopathy of the rectus femoris tendon:A case report. World J Clin Cases. 2019;7:3772–7. doi: 10.12998/wjcc.v7.i22.3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jethwa T, Abadin A, Pujalte G. Rare case of symptomatic calcific tendinopathy of the origin of rectus femoris tendon. BMJ Case Rep. 2020;13:e236809. doi: 10.1136/bcr-2020-236809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuriyama A. Calcific tendinitis of rectus femoris. Clin Exp Emerg Med. 2022;9:160–1. doi: 10.15441/ceem.21.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Robinson DM, Schowalter S, McInnis KC. Update on evaluation and management of calcific tendinopathy. Curr Phys Med Rehabil Rep. 2021;9:57–69. [Google Scholar]
- 33.Scibek JS, Carcia CR. Presentation and conservative management of acute calcific tendinopathy:A case study and literature review. J Sport Rehabil. 2012;21:334–42. doi: 10.1123/jsr.21.4.334. [DOI] [PubMed] [Google Scholar]
- 34.Greis AC, Derrington SM, McAuliffe M. Evaluation and nonsurgical management of rotator cuff calcific tendinopathy. Orthop Clin North Am. 2015;46:293–302. doi: 10.1016/j.ocl.2014.11.011. [DOI] [PubMed] [Google Scholar]


