Abstract
Background
The sacroiliac joints (SIJ) are specialized articulations in the pelvis that allow load transfer between the upper and lower body. Traumatic pelvic disruption often requires surgical fixation of at least one of these joints. Subsequent SIJ pain is associated with asymmetries in joint laxity or stiffness. This pilot study examines SIJ stiffness in patients with intact sacroiliac screw fixation after posterior pelvic ring injuries. This information will prove valuable to informing surgeons about technique efficacy in SIJ injury stabilization.
Questions/purposes
This pilot study examined SIJ stiffness in patients with intact sacroiliac screw fixation to: (1) establish vibration energy color Doppler imaging (VECDI) SIJ intra-rater reliability; (2) measure SIJ stiffness in subjects following surgical fixation using VECDI; (3) compare stiffness data between post-surgical and healthy control subjects; (4) evaluate the relationship between stiffness data and pain and disability scores.
Methods
13 reliability and 19 experimental subjects were tested using VECDI. Subjects were placed into a side-lying position on top of a shaker apparatus that transmitted vibration energy to the pelvic ring while color Doppler images were taken from the bilateral posterior SIJ. One investigator performed SIJ measurements on healthy subjects to establish reliability and then evaluated post SIJ fixation stiffness in experimental subjects at four-weeks (T1) and eight-weeks (T2). Visual analog scales were used to collect subjective pain scores at each time point.
Results
Healthy subject VECDI values suggested good intra-rater reliability (ICC = 0.819; CI 95% = 0.405–0.945). No significant differences in SIJ stiffness (ΔTU) were observed between healthy and experimental subjects at both time points (p > .05). Pearson correlation coefficients highlighted relationships between current pain at T1 and T2 (p = .004, r = .879), and Oswestry Disability Index (ODI) values at T1 and T2 (p = .003, r = .890).
Conclusions
Asymmetric laxity through the SIJ can be associated with pain resulting from either trauma or inherent physiologic variations. Prior to this study, the mainstay of evaluation was subjective indexes, such as the ODI. Here we propose VECDI as a potentially objective tool in SIJ assessment. Following surgical fixation necessitated by trauma, fixation using SI screws demonstrated similar stiffness values through the SIJ at four- and eight-weeks post-operatively when compared to healthy controls. Direct inferences regarding VECDI’s exact sensitivity to SIJ dysfunction cannot be concluded from our investigation due to small sample sizes. Future investigations should include a larger sample size to enhance our understanding of stiffness measurements obtained using VECDI, validate the technique, and determine the time-course of healing from SIJ surgical stabilization.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-024-05331-5.
Keywords: (MeSH terms) Ultrasonography, Doppler, color; Joint diseases; Joint diseases; Sacroiliac joint
Introduction
Pelvic ring disruptions are often the result of high-energy trauma and can have devastating outcomes such as high rates of chronic pain and disability [1–6]. Injuries to the posterior pelvic ring encompass a spectrum of injury patterns with varying degrees of bony and joint instability. Sacroiliac screw fixation accompanied by an open or closed reduction is a widely accepted method for surgically stabilizing posterior pelvic ring injuries [2, 7]. Typically, screws traversing the sacroiliac articulation remain in place indefinitely, but the long-term consequences of screw fixation through the sacroiliac joint (SIJ) are not well documented.
The sacroiliac joints are highly specialized, stable, and flexible articulations designed for transferring loads between the spine and lower extremities [8]. The osseous aspects of the sacroiliac joint (SIJ) with corresponding ligamentous connections contribute to stability and resistance to shear forces that enable load transfer through the pelvis during standing and gait. The flexible stability necessary for bipedal gait has been attributed to the interdigitating articular surfaces of the SIJ, which are supported by ligamentous and myofascial structures [8]. This configuration produces the highest friction coefficient of any diarthrodial joint, which contributes to pelvic ring stability.
The dysfunctional SIJ has been implicated as a potential pain source in both the non-traumatic and post-traumatic populations with persistent low back pain [8–10]. Trauma history is present in 40–50% of all SIJ pain cases, with most occurring due to motor vehicle accidents and falls [10, 11]. Sacroiliac joint pain is described as gluteal or paraspinal (lateral to the midline, below the 5th lumbar vertebra) and can be exacerbated with transitional movements, such as moving in bed or rising from a chair [10]. Several investigators have reported an association between SIJ pain and joint laxity [8, 12, 13]. Asymmetric forces on the joint may result in increased or decreased compression and force closure leading to SIJ dysfunction [8]. This theory is supported by evidence of reduced pain and increased stiffness with the application of an external compressive force across the pelvis (such as with belt fixation) among subjects with SIJ pain [14]. Therefore, examining the effect of screw fixation on SIJ stiffness and pain is relevant for guiding clinical decision-making with respect to SIJ screw management.
Sacroiliac dysfunction may also portend functional impairment and disability. Although no measurement instrument specific to SIJ pain and dysfunction has been reported, the Oswestry Disability Index (ODI) has been validated as a subjective tool capable of identifying disability caused by SIJ pain [15]. The ODI is a self-reporting instrument for patients with low back pain (LBP) and is widely accepted as a reference standard [15–17]. Despite differences in the clinical presentations of LBP and SIJ pain patients, ODI scores have been correlated with pain improvement and being sensitive to the changes in disability following fusion of the SIJ. The minimum clinically important difference (MCID) in ODI scores following SIJ treatment was calculated as 13–15, similar to values previously reported for LBP [15].
Measurement of sacroiliac joint motion has been a widely disputed topic. A variety of methods such as accelerometers, goniometers and manual pelvic compression have been used, albeit inconsistently, in attempts to measure joint stability and classify pathologic progression [18, 19]. Recent investigations have suggested Vibration Energy Color Doppler Imaging (VECDI) as a reproducible means of measuring stiffness at the SIJ in cadavers [19], healthy populations [20–23], and pelvic pain patients [13, 22, 24–26]. This technique was initially explored using physical models to measure differences in tissue sonoelasticity, which directly correlates with stiffness [27]. Investigators have now successfully demonstrated its efficacy by differentiating stiffness of the first tarsometatarsal joint in healthy versus hypermobile subjects [11], as well as in ankylosing spondylitis patients [26]. We sought to evaluate the abilities of VECDI in gauging SIJ stability after post-operative screw fixation, which may be an important parameter in clinical evaluations of patients with pelvic ring disruptions.
The purpose of this investigation is to examine the effect of screw fixation on the SIJ in patients who have undergone surgical repair for traumatic injury. This pilot study first aims to determine the intra-rater reliability of VECDI on SIJ stiffness. Secondly, this study will operationalize VECDI to compare SIJ stiffness in patients who have undergone surgical stabilization after joint trauma with age- and sex-matched control subjects. Third, this study will examine the relationship between data regarding post-stabilization SIJ stiffness, pain, and self-reported disability, for post-operative experimental subjects. The findings will objectively assess the degree of stiffness that screw fixation offers to provide evidence behind this surgical management strategy. This is the first study to use VECDI to examine the effect of screw fixation on SIJ stiffness.
Methods
Subjects
This study received approval from our Institutional Review Board. Thirty-two participants (13 reliability subjects without known medical problems, 11 experimental subjects with screw fixation, and 8 age- and sex-matched controls) volunteered for this study. All individuals were between the ages of 18- and 65 years old and could maintain a side-lying position for 15 minutes. Experimental subjects were selected a priori based on the inclusion criteria of previously undergoing SIJ screw fixation, which included trans-iliac or trans-sacral screw fixation. These subjects were recruited through the trauma division of the Department of Orthopedic Surgery at our midsized level 1 trauma center. The recruitment period started on September 1st, 2016 and ended July 1st, 2021. Any subject was excluded if: (1) the investigator was unable to confidently discriminate between the individual’s sacrum and posterior superior iliac spine (PSIS) during VECDI; (2) pregnancy by self-report; (3) open wounds around the SIJ; (4) and any pelvic screw fixations other than the SIJ. Additionally, reliability and control subjects were excluded if they: (1) experienced active spinal or pelvic pain requiring professional health-care management within the past 12-months; (2) had known, unhealed pelvic or sacral fracture; or (3) had known neuromuscular or musculoskeletal disorders. All participants read and signed the informed consent.
Instrumentation
An example setup of the required instrumentation can be seen in Fig. 1. Vibration energy was transmitted to the pelvic ring using a shaker apparatus (Labworks Inc. ET-139 75lb shaker, Costa Mesa, California). The device was positioned under the measurement table and extended up through an opening in the tabletop to a height sufficient to maintain contact against the subject’s ilium, applying a force in the lateral direction. High frequency (200 Hz, acceleration 2 g-pk), low amplitude (< 0.05 mm) vibrational energy was initiated at the shaker calibrator and transmitted to the top plate of the shaker apparatus, which was secured under the bony prominence of the test side lateral iliac crest. An investigator then applied a hypo-allergenic, water-based ultrasound gel over the interface between the dorsal sacrum and PSIS on the test side. Vibrations were detected using a linear ultrasound transducer (General Electric LOGIQ. GE Healthcare, Milwaukee, Wisconsin). The ultrasound transducer (12 MHz) was rested across the test side SIJ region spanning from the PSIS to the dorsal sacrum, parallel to the skin surface (Fig. 2). Anatomic landmarks visible on ultrasound included the ilium, PSIS, and SI joint (Fig. 3). Color Doppler was turned on, with the region of interest box capturing the PSIS and SIJ. Optimal pulse repetition and initial gain settings varied per patient. An example of these settings can be seen in Supplemental Video 1.
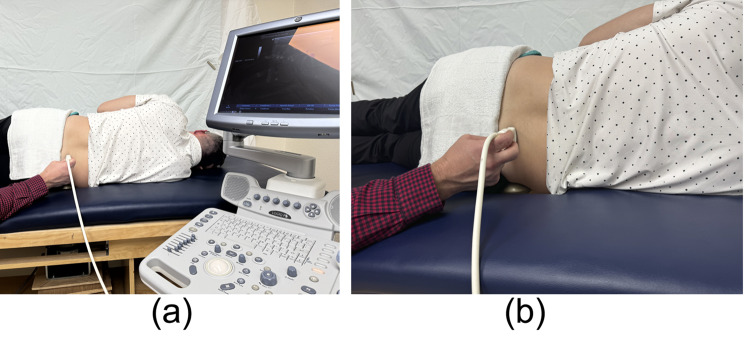
Fig. 1.
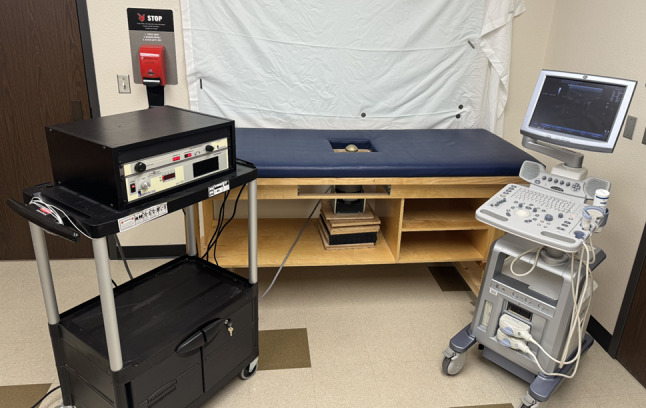
The instrumentation required: shaker calibrator (left), shaker apparatus positioned under a modified measurement table (center), ultrasound device and transducer (right)
Fig. 2.
(a) Vibrations were detected using a linear ultrasound transducer positioned across the test side SIJ region spanning from the PSIS to the dorsal sacrum. (b) A closer view demonstrating the shaker apparatus positioned under the bony prominence of the test side lateral iliac crest and placement of the ultrasound transducer
Fig. 3.
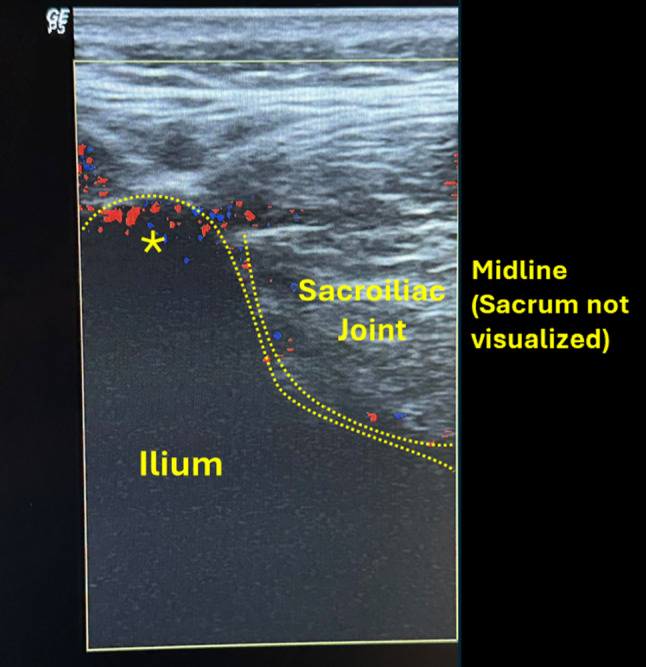
Vibration energy presented on the color Doppler monitor as pixels, where incrementally decreasing the ultrasound gain leads to color moving from both the SIJ and PSIS to the PSIS only. * = Posterior superior iliac spine
Vibration energy was presented on the color Doppler monitor as pixels, where the intensity of vibration pixels from the PSIS and SIJ appeared simultaneously on the monitor at sufficiently high threshold values (Fig. 3).The minimum threshold unit (TU) levels were determined for both the PSIS and SIJ by lowering the color Doppler image registry to a level where vibration from each structure was minimally detectable (where the image turns from color to gray). At a certain TU value of the color Doppler image, both the PSIS and SIJ vibrated with energy sufficient to display color on the monitor. The ultrasound gain setting was decreased until the sensitivity of the Doppler fell below the color threshold on the screen for each structure (TUSIJ and TUPSIS).
Because of an expected decline in the transfer of vibration energy across the ilium, the SIJ reached a minimum threshold unit level first, followed by the PSIS when the threshold unit level was further decreased (Supplemental Video 1). The PSIS (TUPSIS) threshold units were subtracted from the SIJ (TUSIJ) threshold units, which resulted in vibration threshold differences at the two structures (ΔTU). The relationship between the TU values of the PSIS and SIJ are represented by the following formula:
 |
1 |
ΔTU represents joint stiffness. A smaller value equates to a stiffer joint, while a larger value corresponds to increased joint laxity [28].
Preparatory procedures
Following reading and signing the informed consent, each subject completed a background health history questionnaire and was measured for height and weight with a subsequent body mass index (BMI; kg/m2) calculation. Experimental subjects additionally completed the ODI as well as a visual analog pain scale (VAS) to determine symptom severity. Next, all subjects attained a side-lying position with approximately 15˚ of knee flexion on top of a custom-built table with a square cut-out for the shaker apparatus. Complete contact of the ilium was confirmed to ensure optimal vibration energy transmission through the SIJ.
Experimental procedures
Thirteen asymptomatic subjects were measured for SIJ stiffness to assess intra-rater reliability. The dominant-side SIJ was measured three times by one investigator while an assistant recorded the ΔTU, effectively blinding the rater. Subjects returned 48 hours later and were measured using the same procedure to establish intra-rater reliability.
Following acceptable intra-rater reliability statistics, the same investigator measured 11 experimental subjects (1 with left, 2 with right, and 8 with bilateral fixation, respectively) at four-weeks (T1), and eight-weeks (T2). Three measurements were recorded for both SIJs with the shaker apparatus contacting the tested side. 8 age- and sex-matched control subjects were measured on their dominant side for between-group comparison of SIJ stiffness. Lastly, Visual analog scales (VAS) were used to collect subjective patient pain scores at each time point.
Statistical analysis
Measures of central tendency, standard deviation and gain unit (ΔTU) value distributions were used to describe the data. Data normality was established through assessing the values for skewness and kurtosis (from − 2 to 2), along with Shapiro-Wilk test outcomes (p > .05). A Levene’s test was used to test for data homogeneity of variance (p > .05). Intraclass correlation coefficients (ICC3, k) representing relative agreement were calculated in the initial 13 control subjects to determine intra-rater reliability of stiffness measurements using the previously described VECDI measurement model. Intra-rater reliability was calculated using each rater’s three repeated measurements between the two testing days. Independent and dependent sample t-tests were calculated to analyze between- and within-group SIJ stiffness. Pearson product-moment correlations were calculated between ΔTU, ODI, and VAS current pain score for both time points in experimental subjects. All statistics were calculated using SPSS Statistics 24.0 software (Statistical Package for the Social Sciences, IBM SPSS Inc., Chicago, IL).
Results
Intraclass correlation values suggested good intra-rater reliability (ICC = 0.819; CI 95% = 0.405–0.945). Differences in anthropometric variables between test subjects and controls (age, gender, BMI) were non-significant across experimental and control groups (Table 1).
Table 1.
Mean (standard deviation) of the anthropometric characteristics
| Experimental Group (n = 11) | Control Group (n = 8) | p value | |
|---|---|---|---|
| Age | 37.5 (13.0) | 40.3 (10.1) | 0.62 |
| Sex | Male = 8, Female = 3 | Male = 6, Female = 2 | |
| Height (m) | 1.7 (0.1) | 1.8 (0.1) | 0.18 |
| Weight (kg) | 75.5 (22.6) | 81.4 (12.0) | 0.52 |
| BMI (kg/m2) | 25.5 (5.4) | 25.2 (2.5) | 0.91 |
No significant differences for ΔTU were observed between healthy subjects and experimental subjects at both time points (p > .05; Table 2). A qualitative observation revealed increased SIJ stiffness within the unilaterally fixated group (N = 3) at T1 between the involved (mean = 3.67 ± 4.2 SD) and uninvolved side (mean = 10.13 ± 2.8 SD). Pearson correlation coefficients highlighted relationships between current pain at T1 and T2 (p = .004, r = .879), and ODI values at T1 and T2 (p = .003, r = .890). A non-significant negative correlation trend was observed for right side ΔTU at T1 and current pain at T1 (p = .458, r = − .25), and T2 (p = .158, r = − .550).
Table 2.
Mean joint stiffness (ΔTU) among healthy and experimental subjects
| Side – Time Point | ||||||
|---|---|---|---|---|---|---|
| Right – T1 | Right – T2 | p value* | Left – T1 | Left - T2 | p value* | |
| Healthy subjects | 5.6 (3.7) | 5.3 (2.1) | ||||
| Experimental subjects | 4.8 (3.1) | 5.4 (3.9) | 0.17 | 7.9 (6.5) | 7.4 (6.0) | 0.38 |
| p value** | 0.82 | 0.74 | ||||
ΔTU Values represented as: Mean (SD)
* = Paired samples t-test
** = Independent samples t-test
T1 = Time point one (4 weeks)
T2 = Time point two (8 weeks)
Discussion
The sacroiliac joints (SIJ) allow for upper and lower body load transference via highly specialized articulations. Traumatic disruptions of these articulations may result in surgical fixation to at least one of these joints. SIJ pain can be a significant source of low back pain, with cited etiologic rates of 4–15% [8, 29]. Thus, this pilot study attempted to elucidate whether VECDI can be a potential tool for objectively assessing the SIJ. This was done by including intra-rater reliability testing and examining those who had undergone prior posterior pelvic ring fixation. Lastly, subjective perceptions of SIJ pain were correlated with objective stiffness data to evaluate relationships regarding laxity across the SIJ.
Objective 1: to establish vibration energy color Doppler imaging (VECDI) SIJ intra-rater reliability
The use of doppler imaging of vibrations (DIV) has been investigated since the early 90’s. Buyruk et al. used DIV to characterize the SIJ in order to better understand peripartum pelvic pain [20]. This was accomplished through examination of healthy volunteers to validate the technique’s reproducibility and reliability. DIV has continued to be used as a research tool in studying pelvic pain in women but has yet to be validated in men or patients who have traumatic disruption of their posterior pelvic elements. Our study demonstrated good reproducibility and intra-rater reliability (ICC = 0.819) through repeated measurements over multiple testing days.
Prior to the work done with doppler imaging, the most common ways of analyzing the SIJ objectively were through: radiography, static images incapable of dynamically evaluating the SIJ in real time, or by using tantalum beads. The latter is notable for being invasive and difficult to measure small changes in position with. On physical examination, multiple provocation maneuvers (distraction test, compression test, thigh thrust test, Gaenslen test, sacral thrust, and FABER) and their associated sensitivities for SIJ dysfunction have been evaluated. Telli et al. found that when assessed individually, the sensitivities of these tests were 68.3%, 78.5%, 71.8%, 56.4%, 70.95%, and 91.4%, respectively [30]. Despite these good to excellent sensitivities, a multitest physical exam regimen was still recommended given that intraexaminer reliability and agreement remained questionable [30]. The preliminary data from our study revealed that VECDI has good intrarater reliability as determined by using an intraclass correlation coefficient analysis. Given the nature of the pilot study, our methodology did not examine the sensitivity of VECDI. Future studies should employ a larger population size with a blinded investigator to determine accuracy in diagnosing SIJ dysfunction using joint stiffness (ΔTU) found through utilization of VECDI.
Objectives 2 and 3: measuring SIJ stiffness in post SIJ fixation patients and comparison with healthy control subjects
It has been suggested that asymmetric hyperlaxity across the bilateral SIJ could play a role in LBP. Damen et al. reported asymmetric laxity during pregnancy is associated with a three-fold increase in postpartum pelvic pain in comparison to those who had symmetric laxity [13]. To assess SIJ laxity in our study, we used a measurement of stiffness, ΔTU, to examine whether post fixation patients may have asymmetric joint laxity across the SIJ that could be indicative of SIJ dysfunction. It is important to realize that ΔTU is only a reflection of the amount of mobility of the ilium relative to the sacrum and not the absolute rigidity of the pelvis. In our measurements, our study revealed there was no statistical difference in SIJ stiffness (ΔTU) between the fixation group versus the healthy controls. Care had been taken to eliminate potential confounders by approximating characteristics between experimental subjects and the controls as much as possible, with no statistical differences found (Table 1). This meant that the SIJ fixations received by the experimental subjects were demonstrative of restoration of near anatomic parameters (i.e. stiffness) of the joint. It is important to note that the degree of ligamentotaxis in each SIJ fixation was also likely contributory to the observed stiffness values seen among experimental subjects. By carefully molding fracture fragments back into alignment using an SIJ screw, anatomic alignment could be better achieved. This likely equated to higher than expected stiffness values at each time interval as the surrounding soft tissues further helped reinforce the fixation construct during healing.
A post hoc power analysis completed using statistical analysis in R (R Core Team (2021), R: A language and environment for statistical) assumed an alpha value of 0.05 with a power of 0.8 to calculate a sample size estimate from the pilot data. This included a mean of 3.67 ± 4.2 SD compared to the uninvolved mean of 10.13 ± 2.8 SD. An r number of 0.88 was derived, indicative of a large effect size. Using these variables, we calculated that a sample size of 40 patients would require SIJ examination using VECDI in order to find a statistically significant difference between SIJ stiffness among experimental and control subjects, with 20 patients in each group.
Objective 4: to evaluate the relationship between stiffness data and self-reported pain and disability scores
The lack of difference in SIJ stiffness/restoration of anatomic joint stiffness was also reflective of a reduction in pain as seen by the negative correlations with subjective pain measured at different time points in fixation. There was a statistically non-significant difference between the SIJ of the three patients with unilateral fixation. This was interesting as there did not appear to be any correlation with subjective pain for this asymmetry as would have been previously suggested based on the findings of Damen et al. [13]. Collectively, these results can be interpreted that the use of SIJ fixation, be it through transiliac-transsacral or sacroiliac screws, can restore near anatomic levels of mobility through a traumatically disrupted joint. As our investigation indicates, the restoration of anatomic parameters, specifically joint stiffness, can potentially be measured using VECDI in a reliably replicative manner among different technicians. However, the exact sensitivity of this technique to SIJ dysfunction and its ability to find a significant difference in SIJ stiffness need to be determined using large scale blinded studies. Our posthoc power analysis using the data from this pilot study has helped reveal the necessary number of subjects required to accomplish this.
Limitations
First, the small sample size of this pilot study is a limitation to the general applicability of the results. As previously noted, large scale studies are the next step in evaluating the sensitivity of VECDI for joint dysfunction and validating the technique. Second, only one researcher collected all the measurements. Multiple studies have indicated that there can be a steep learning curve to using VECDI, which could limit the potential for it to be adapted as a tool for objective measurements [2]. Third, multiple parameters can influence VECDI measurement results. These include differences in patient positioning, pelvic tilt, alignment, muscle status and activation, hydration status, extent of ligamentous injury, etc. Fourth, VECDI uses the relative difference of threshold units across the joint rather than the absolute value, which could confound measurements comparing those with and without fixation in future studies as well as anatomic variations between participants. Fifth, other pathologies contributing to postoperative low back pain may have confounded our assessment of SIJ stiffness and pain. For example, reported incidence rates of cluneal nerve entrapment have ranged from 1.6 to 14% [31, 32]. In the postoperative setting, trauma patients may develop cluneal neuralgia from scarring which may be difficult to distinguish from SIJ dysfunction [32].
Conclusion
The use of VECDI can serve as a reliably reproducible tool for measuring the stability of the SIJ before and after fixation. Asymmetric laxity through this joint can be associated with pain and be the result of either trauma or inherent physiologic variations. Prior to this study, the mainstay of evaluation was subjective indexes, such as the ODI. Here we propose VECDI as a potentially objective tool in SIJ assessment. Following surgical fixation necessitated by trauma, fixation using SI screws demonstrated similar stiffness values through the SIJ at four- and eight-weeks post-operatively when compared to healthy controls. Direct inferences regarding VECDI’s exact sensitivity to SIJ dysfunction cannot be concluded from our investigation due to small sample sizes. Future investigations should include a larger sample size of at least 40 patients total (20 experimental, 20 controls) to enhance our understanding of stiffness measurements obtained using VECDI, validate the technique, and determine the time-course of healing from SIJ surgical stabilization.
Future studies
As this study had a small overall sample size, we continue to add to our data in investigating patients with either unilateral or bilateral fixation after traumatic disruption of the posterior pelvic ring. We aim to collect long term follow-up data on patients who have symptomatic implants of the SIJ necessitating hardware removal and use this cohort for further subset analysis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: Video 1: A real-time video capture of VECDI performed on a volunteer. The intensity of vibration pixels from the PSIS and SIJ appear simultaneously on the monitor at sufficiently high threshold values. As ultrasound gain is decreased, it falls below the minimum threshold unit level of the SIJ first, followed by the PSIS.
Acknowledgements
None.
Abbreviations
- SIJ
Sacroiliac joint
- VECDI
Vibration energy color Doppler imaging
- ODI
Oswestry disability index
- PSIS
Posterior superior iliac spine
Author contributions
All authors have contributed equally with Dr. Cyrus Caroom and Dr. Phil Sizer aiding in data collection, concept development, manuscript revisions. Dr. Caleb Gottlich contributed with data collection and analysis as well as manuscript preparation and revisions. Dr. Thomas Githens contributed to IRB approval and concept development. Dr. Alex Drusch contributed with data collection, data analysis, manuscript preparation, and revisions. Dr. Neil Jain contributed with data analysis, manuscript preparation, and revisions. All authors have read and agree with the final manuscript preparation.
Funding
This research received no funds, grants, or other support from agencies in the public, commercial, or not-for-profit sectors.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was approved under the Texas Tech University Health Sciences Center Institutional Review Board IRB #L16-179. To participate in this investigation, patients read and signed the informed consent.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cole JD, Blum DA, Ansel LJ. Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res. 1996(329):160–79. [DOI] [PubMed]
- 2.Iorio JA, Jakoi AM, Rehman S. Percutaneous sacroiliac screw fixation of the posterior pelvic Ring. Orthop Clin North Am. 2015;46(4):511–21. [DOI] [PubMed] [Google Scholar]
- 3.Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989;242:83–97. [PubMed] [Google Scholar]
- 4.Riemer BL. Outcomes of pelvic ring injuries. Oper Tech Orthop. 1997;7(3):256–9. [Google Scholar]
- 5.Salari P, Cannada LK, Moed BR. Do asymptomatic patients have normal function after percutaneous fixation of the posterior pelvic ring? A case-control pilot study. J Orthop Surg Res. 2015;10:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70(1):1–12. [DOI] [PubMed] [Google Scholar]
- 7.Routt MLC, Meier M, Kregor PJ, Mayo KA. Percutaneous iliosacral screws with the patient supine technique. Oper Tech Orthop. 1993;3:35–45. [Google Scholar]
- 8.Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manjoo A, Sanders DW, Tieszer C, MacLeod MD. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma. 2010;24(1):2–6. [DOI] [PubMed] [Google Scholar]
- 10.Hooten WM, Cohen SP. Evaluation and treatment of low back pain: A clinically focused review for primary care specialists. Mayo Clin Proc. 2015;90(12):1699 – 718. [DOI] [PubMed]
- 11.Chou LH, Slipman CW, Bhagia SM, Tsaur L, Bhat AL, Isaac Z, et al. Inciting events initiating injection-proven sacroiliac joint syndrome. Pain Med. 2004;5(1):26–32. [DOI] [PubMed] [Google Scholar]
- 12.Mens JM, Damen L, Snijders CJ, Stam HJ. The mechanical effect of a pelvic belt in patients with pregnancy-related pelvic pain. Clin Biomech (Bristol Avon). 2006;21(2):122–7. [DOI] [PubMed] [Google Scholar]
- 13.Damen L, Buyruk HM, Güler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand. 2001;80(11):1019–24. [DOI] [PubMed] [Google Scholar]
- 14.Damen L, Spoor CW, Snijders CJ, Stam HJ. Does a pelvic belt influence sacroiliac joint laxity? Clin Biomech (Bristol Avon). 2002;17(7):495–8. [DOI] [PubMed] [Google Scholar]
- 15.Copay AG, Cher DJ. Is the Oswestry Disability Index a valid measure of response to sacroiliac joint treatment? Qual Life Res. 2016;25(2):283–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Polly D, Cher D, Whang PG, Frank C, Sembrano J. Does level of response to SI Joint Block Predict Response to SI Joint Fusion? Int J Spine Surg. 2016;10:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Do KH, Ahn SH, Jones R, Jang SH, Son SM, Lee DG, et al. A New Sacroiliac Joint Injection technique and its short-term effect on chronic Sacroiliac Region Pain. Pain Med. 2016;17(10):1809–13. [DOI] [PubMed] [Google Scholar]
- 18.Beales DJ, O’Sullivan PB, Briffa NK. The effects of manual pelvic compression on trunk motor control during an active straight leg raise in chronic pelvic girdle pain subjects. Man Ther. 2010;15(2):190–9. [DOI] [PubMed] [Google Scholar]
- 19.Buyruk HM, Stam HJ, Snijders CJ, Vleeming A, Laméris JS, Holland WP. The use of color Doppler imaging for the assessment of sacroiliac joint stiffness: a study on embalmed human pelvises. Eur J Radiol. 1995;21(2):112–6. [DOI] [PubMed] [Google Scholar]
- 20.Buyruk HM, Snijders CJ, Vleeming A, Laméris JS, Holland WP, Stam HJ. The measurements of sacroiliac joint stiffness with colour Doppler imaging: a study on healthy subjects. Eur J Radiol. 1995;21(2):117–21. [DOI] [PubMed] [Google Scholar]
- 21.Damen L, Stijnen T, Roebroeck ME, Snijders CJ, Stam HJ. Reliability of sacroiliac joint laxity measurement with Doppler imaging of vibrations. Ultrasound Med Biol. 2002;28(4):407–14. [DOI] [PubMed] [Google Scholar]
- 22.de Groot M, Spoor CW, Snijders CJ. Critical notes on the technique of Doppler imaging of vibrations (DIV). Ultrasound Med Biol. 2004;30(3):363–7. [DOI] [PubMed] [Google Scholar]
- 23.van Wingerden JP, Vleeming A, Buyruk HM, Raissadat K. Stabilization of the sacroiliac joint in vivo: verification of muscular contribution to force closure of the pelvis. Eur Spine J. 2004;13(3):199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buyruk HM, Stam HJ, Snijders CJ, Laméris JS, Holland WP, Stijnen TH. Measurement of sacroiliac joint stiffness in peripartum pelvic pain patients with Doppler imaging of vibrations (DIV). Eur J Obstet Gynecol Reprod Biol. 1999;83(2):159–63. [DOI] [PubMed] [Google Scholar]
- 25.Damen L, Buyruk HM, Güler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine (Phila Pa 1976). 2002;27(24):2820–4. [DOI] [PubMed] [Google Scholar]
- 26.Mohammadi A, Ghasemi-rad M, Aghdashi M, Mladkova N, Baradaransafa P. Evaluation of disease activity in ankylosing spondylitis; diagnostic value of color Doppler Ultrasonography. Skeletal Radiol. 2013;42(2):219–24. [DOI] [PubMed] [Google Scholar]
- 27.Parker KJ, Lerner RM. Sonoelasticity of organs: shear waves ring a bell. J Ultrasound Med. 1992;11(8):387–92. [DOI] [PubMed] [Google Scholar]
- 28.Wilhelm MP, Hooper TL, Seeber GH, Browne KL, Sargent E, Gilbert KK, et al. The relationship between measures of foot mobility and subtalar joint stiffness using vibration energy with color doppler imaging-A clinical proof-of-concept validation study. PLoS ONE. 2020;15(8):e0237634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Foley BS, Buschbacher RM. Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2006;85(12):997–1006. [DOI] [PubMed] [Google Scholar]
- 30.Telli H, Telli S, Topal M. The validity and reliability of provocation tests in the diagnosis of Sacroiliac Joint Dysfunction. Pain Physician. 2018;21(4):E367–76. [PubMed] [Google Scholar]
- 31.Anderson D, Szarvas D, Koontz C, Hebert J, Li N, Hasoon J, et al. A Comprehensive Review of Cluneal Neuralgia as a cause of Lower Back Pain. Orthop Rev (Pavia). 2022;14(4):35505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paracha U, Hendrix JM. Cluneal neuralgia. StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: Video 1: A real-time video capture of VECDI performed on a volunteer. The intensity of vibration pixels from the PSIS and SIJ appear simultaneously on the monitor at sufficiently high threshold values. As ultrasound gain is decreased, it falls below the minimum threshold unit level of the SIJ first, followed by the PSIS.
Data Availability Statement
No datasets were generated or analysed during the current study.