Abstract
Purpose
To evaluate and summarize the best evidence of home enteral tube feeding (HETF) care management in the elderly to provide an evidence-based basis for caregivers to implement care interventions.
Patients and Methods
Evidence on HETF care management in the elderly was retrieved from Chinese and international databases, guidelines, and websites of professional associations, including systematic reviews and expert consensuses, using the keywords of home enteral nutrition, home tube feeding, old, elder, home care, etc. The literature considered in this study was published from April 2019 to April 2024. Two trained researchers independently evaluated the quality of the included literature, graded the literature using the JBI evidence pre-grading system, classified and summarized the extracted evidence.
Results
A total of 15 articles were included, including 1 clinical decision, 1 guideline, 3 best evidence summaries, 4 systematic reviews, 2 randomized controlled trials, and 4 quasi-experimental studies. 18 pieces of the best evidence were summarized in 3 aspects, including the NST administration, education of caregivers, and selection of nutrition formulas.
Conclusion
This study comprehensively summarized the best evidence of home enteral tube feeding care management in the elderly and provided a scientific basis for caregivers to implement care interventions. In home care settings, using evidence-based practices requires developing a comprehensive care management system based on the trinity of hospital, community and home, in order to reduce the incidence of HETF-related complications, improve the quality of life of the elderly with HETF, and provide a practical reference for NST members and caregivers.
Keywords: enteral nutrition, nutritional support, quality of life, complication prevention, patient education
Introduction
Due to the reality of high incidence of cancers, high requirements of Enteral Nutrition (EN) support and high prevalence of home health-care, older patients make up the majority of Home Enteral Nutrition (HEN).1–5 Home Enteral Tube Feeding (HETF) is a viable option for people needed HEN when oral intake is insufficient to meet nutritional needs, and the types of tubes generally consists of nasogastric tubes, nasojejunal tubes, gastronomy fistulas, and jejunostomy fistulas, etc.6
Studies have reported that older patients with HETF had a higher incidence of HEN-related complications as the gradual decline of various organ functions and poor general condition,7,8 and the incidence related to home care for disabled elders is 16.46%, with caregivers’ competence being one of the major influencing factors for this rate.9,10 Cross-sectional studies in China have reported low awareness of caring knowledge of HETF carers, with poor knowledge of feeding tube care, HEN preparations, HEN support devices, and how to prevent and deal with HETF complications.11–13 As much as 40% to 80% of the medical information received by the elderly and their caregivers is forgotten immediately after discharge, and nearly half of the retained information is incorrect.14 The poor caring quality of caregivers is mainly due to their older age, lower cultural level, or lack of caring experience.15
There is also a phenomenon of discontinuity between hospitals, communities, and HETF users. One of the major problems is a lack of specific assessment tools for elderly with HETF. The Mini Nutritional Assessment (MNA) has been designed and validated to provide a single, rapid assessment of nutritional status in elderly patients home care settings,16 but it lacks contents of tube-related questions, thus we are unable to get information about tube feeding.
While limited medical resources cannot meet the whole and continuous guidance of the elderly with HETF,12,17–19 systematic and comprehensive evidence has not yet been formed, which is not conducive to the standardized management of HETF care for the elderly. Therefore, this study summarizes the best evidence of HETF care management for the elderly to provide a basis for constructing a scientific HETF care plan.
Materials and Methods
Establishment of the Problem
The PIPOST method was employed to determine the research questions: (I) Population (P): The elderly undergoing HETF; (II) Intervention (I): Management of HETF care; (III) Profession (P): Nutritional support team (NST), including geriatric specialists, dietitians, rehabilitation therapists, psychologists, nutritional support pharmacists (NSP), nursing administrators, geriatric nurses, and community healthcare personnel; (IV) Outcome (O): Incidence of HETF-related complications, nutritional status, and quality of life; (V) Setting (S): Home, nursing homes, retirement communities; (VI) Type of Evidence (T): Guidelines, systematic reviews, expert consensus, evidence summaries, meta-analysis, best practices, randomized controlled trials (RCTs), and quasi-experimental studies.
Search Strategy
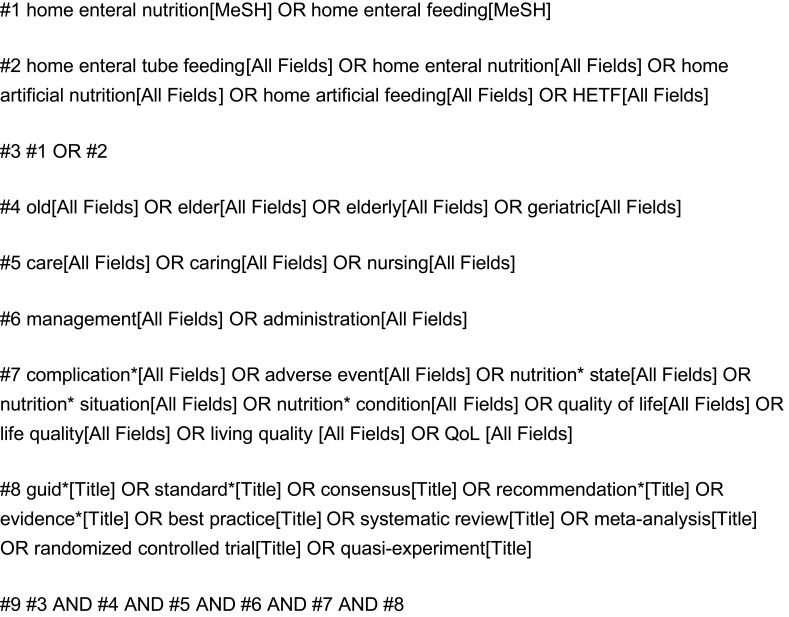
We conducted a comprehensive search according to the 6S pyramid through databases and websites as below: BMJ best practice, Up to Date, National Guideline Clearinghouse(NGC), Scottish Intercollegiate Guidelines Network(SIGN), National institute for Health and Care Excellence(NICE), Canadian Medical Association(CMA) Infobase, Registered Nurses’ Association of Ontario(RNAO), American Society for Parenteral and Enteral Nutrition(ASPEN), the European Society for Clinical Nutrition and Metabolism(ESPEN), Chinese Society for Parenteral and Enteral Nutrition(CSPEN), Joanna Briggs Institute(JBI) EBP database, EBSCO, Cochrane Library, Embase, PubMed, Web of Science, CINAHL, Yimaitong, China National Knowledge Infrastructure(CNKI), China Biology Medicine Disc(CBM), Wanfang, VIP and Chinese Medical Ace Base. Among them, BMJ best practice and Up to Date were selected as they rank the highest in 6S pyramid as “clinical decision support systems”, which cover a wide range of evidence-based practices including HETF. JBI and Cochrane Library were selected due to their high-quality, independent evidence relevant to HETF. ASPEN, ESPEN, CSPEN are authoritative institutions of enteral nutrition, which collect guidelines and consensus specifically related to HEN and HETF. EBSCO, Embase, PubMed, Web of Science, CINAHL and other Chinese databases provide comprehensive results of HETF-related original researches. English search terms included “home enteral tube feeding/home tube feeding/home enteral nutrition/home artificial nutrition/home artificial feeding/HETF”, “old/elder/elderly/geriatric”, “care/caring/nursing”, “management/administration”, “complication/adverse event/nutrition state/nutritional state/nutrition situation/quality of life/life quality/living quality/QoL”, “guideline/consensus/recommendation/evidence summary/systematic review/best practice/meta-analysis/randomized controlled trial/quasi-experiment.” The search was limited to articles published between April 1, 2019, and April 1, 2024. The detailed steps for searching English databases, using PubMed as an example, can be found in Figure 1.
Figure 1.
Literature search strategy of PubMed.
Inclusion and Exclusion Criteria
Inclusion criteria: (I) Study type: clinical decision, guideline, expert consensus, systematic review, recommended practice, evidence summary, meta-analysis, randomized controlled trial, quasi-experimental study published in English and Chinese; (II) Subjects: the elderly with HETF who are older than 65 years old; (III) Outcomes: Incidence of HETF-related complications, nutritional status, and quality of life.
Exclusion criteria: (I) Repeated published or translated literature; (II) Research proposal or report; (III) Conference abstracts; (IV) articles without access to the full text.
Literature Quality Evaluation
Four experts who had systematically studied evidence-based methodology independently evaluated the quality of the Guidelines according to the Appraisal of Guidelines for Research and Evaluation II (AGREE II) updated in 2017.20 The intraclass correlation coefficient (ICC) was used to test the consistency of the evaluation results. Clinical decision, expert consensus, systematic review, randomized controlled trial, and quasi-experiment studies were independently evaluated by two researchers according to the JBI literature quality assessment tool. Critical Appraisal for Summaries of Evidence (CASE)21 was used to evaluate clinical decision-making and evidence summaries. If there was a disagreement on the quality of the literature, a consensus was reached after consultation with the third researcher with higher qualifications. In case of conflicts between different sources of evidence, the principle of evidence-based, high-quality, and the latest published evidence should be given priority.
Evidence Extraction and Classification
The evidence was summarized by two nursing postgraduate students who had studied evidence-based nursing according to the following principles: (I) If the content was consistent, choose the evidence that was concise and easy to understand; (II) If the contents are complementary, they will be combined to form evidence according to linguistic logic; (III) If the content is in conflict, we adhere to the principles of prioritizing evidence based on its quality, credibility, and the latest authoritative publications. According to the JBI evidence pre-ranking system (2014),22 the included evidence was divided into grade 1 to 5, with grade 1 being the highest and 5 the lowest. After the extraction of the evidence, two researchers independently graded the evidence. In case of disagreement, the third researcher participated in the discussion and finally reached a consensus conclusion.
Results
Literature Search Results
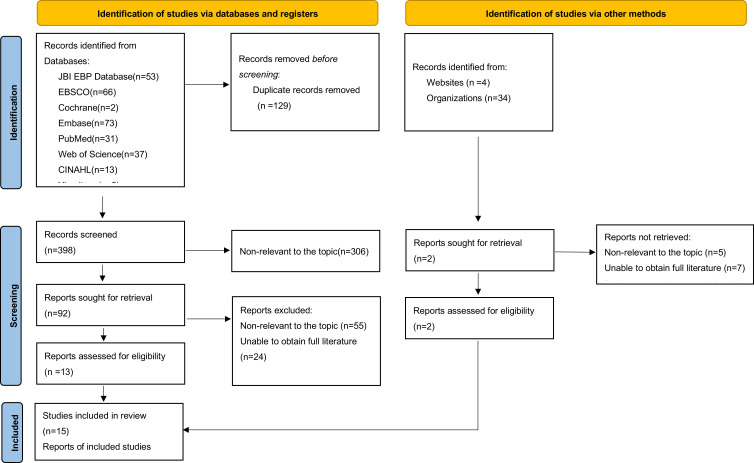
A total of 565 relevant literature were obtained by preliminary retrieval, 400 were left after eliminating duplicate literature, 94 literatures were obtained after initial screening, and 15 literatures were finally included after reading the full text, including 1 clinical decision, 1 guideline, 3 evidence summaries, 4 systematic reviews, 2 randomized controlled trials, and 4 quasi-experimental studies. The literature screening process is shown in Figure 2, and the general characteristics of the included literature are shown in Table 1.
Figure 2.
PRISMA flow chart of literature search and screening.
Notes: PRISMA figure adapted from Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology. 2009;62(10). Creative Commons.37
Table 1.
Characteristics of Included Studies
| No. | Included articles | Publication year | Source | Topic | Patterns | Type of articles |
|---|---|---|---|---|---|---|
| 1 | CROWLEY K. et al23 | 2024 | UpToDate | Patient education: Enteral (tube) feeding (The Basics) | A brief introduction about enteral tube feeding to patients | Clinical decision |
| 2 | Bischoff S. C. et al24 | 2022 | ESPEN | ESPEN practical guideline: Home enteral nutrition | Informing professionals and other HEN providers in a concise way about the indications and contraindications for HEN, as well as its implementation and monitoring | Guideline |
| 3 | Queiroz A. B. et al25 | 2023 | JBI | Enteral Tube Feeding (Adults): Blenderized vs Commercial Formula | Comparing the characteristics of blenderized formula and commercial formula, and provide recommendations for enteral tube feeding adults | Evidence summary |
| 4 | Mi Y. et al26 | 2019 | CBM | Prevention and management of enteral feeding intolerance in critically ill patients | Summarizing the best evidence and standardizing the implementation on the prevention and management of enteral nutrition feeding intolerance in critically ill patients for ICU nurses | Evidence summary |
| 5 | Niu Y. et al27 | 2023 | CBM | Safety management of long-term home tube feeding in the elderly | A guidance for safety management of long-term home tube feeding for the elderly in home setting | Evidence summary |
| 6 | Uniat K. C. et al28 | 2022 | Web of Science | Microbiological quality of enteral formulations handled at home | Reviewing the unsatisfactory microbiological quality of home-prepared enteral formulations | Systematic review |
| 7 | Mou J. et al29 | 2022 | Web of Science | Experiences and needs of home caregivers for enteral nutrition | Systematically identifying, evaluating and synthesizing the qualitative evidence on HEN of caregivers | Systematic review |
| 8 | Byrnes C. et al30 | 2022 | Web of Science | A scoping review of best practices in home enteral tube feeding | Reporting the importance of initial education to enable service users to adapt to HEN and the need for support from knowledgeable healthcare professionals. | Systematic review |
| 9 | Li C. et al31 | 2021 | CBM | Effect of semi-solid enteral nutrition on gastrointestinal tolerance in patients with tube feeding | Semi-curing enteral nutrition is helpful to reduce the incidence of diarrhea, abdominal distension and vomiting, and reduce the length of hospital stay for tube feeding patients | Meta-analysis |
| 10 | Kaźmierczak-Siedlecka et al32 | 2020 | CINAHL | The use of Lactobacillus plantarum 299v (DSM 9843) in cancer patients receiving home enteral nutrition | Administration of Lactobacillus plantarum 299v may be effective in improvement of nutritional status, enteral nutrition tolerance, and quality of life of cancer patients receiving HEN | Randomized controlled trial |
| 11 | Lei Z.33 | 2023 | CBM | Application of semi⁃cured homogenate diet with food thickener in senile patients with nasal feeding | Semi-cured homogenate diet can improve the nutritional status, reduce the incidence of gastroesophageal reflux, vomiting and diarrhea, and help achieve the nutritional target intake in senile patients | Randomized controlled trial |
| 12 | Chen Y. et al18 | 2019 | CNKI | Application of nutrition support team in elderly patients with home enteral nutrition | Through education of NST, the HEN caregivers can master the relevant knowledge and skills and improve the quality of HEN care for the elderly | Quasi-experimental study |
| 13 | Chen Y. et al34 | 2020 | Wanfang | The application of daily goal health education in caregivers of elderly patients with home nutrition | Daily targeted health education and skill training for caregivers of elderly HEN patients can reduce the incidence of complications, relieve the mental stress of caregivers, and optimize the use of limited medical resources | Quasi-experimental study |
| 14 | Zhu R. et al35 | 2020 | VIP | Effect of nasal feeding nursing training on caregivers of patients with nasal feeding at home | Targeted training of nasal tube feeding knowledge and skills of caregivers can reduce the incidence of complications | Quasi-experimental study |
| 15 | Madrid-Paredes A. et al36 | 2023 | Pubmed | Impact of nutritional and educational support on home enteral nutrition | The nutritional assessment to prescribe individualized HEN to each patient, together with educational measures and training for both patients and trainers, improves nutritional status and reduces the onset of adverse events | Quasi-experimental study |
Abbreviations: ESPEN, the European Society for Parenteral and Enteral Nutrition; JBI, the Joanna Briggs Institute; CNKI, China National Knowledge Infrastructure; CBM, China Biology Medicine Disc; HETF, home enteral tube feeding; HEN, home enteral nutrition.
Results of Literature Quality Evaluation
Quality Evaluation of Clinical Decision-Making
A total of one clinical decision was included in this study,23 and all items were evaluated as “yes” and approved for inclusion. The quality evaluation results are shown in Table 2.
Table 2.
Quality Evaluation of Clinical Decision
| I | II | III | IV | V | VI | |
|---|---|---|---|---|---|---|
| Patient education: Enteral (tube) feeding (The Basics)23 | Yes | Yes | Yes | Yes | Yes | Yes |
Quality Evaluation of Guidelines
A total of one guideline24 was included in this study, and the ICC value was 0.785, with good evaluation consistency. The quality evaluation results are shown in Table 3, and the inclusion was approved.
Table 3.
Quality Evaluation of Guidelines
| Included articles |
Percentage of standardization by area (%) | Domain scores≥60% | Domain scores≥30% | Recommendation level | |||||
|---|---|---|---|---|---|---|---|---|---|
| Scope and purpose | Stakeholder involvement | Rigor of development | Clarity of presentation | Applicability | Editorial independence |
||||
| Bischoff S. C. et al24 | 95.83 | 81.94 | 75.52 | 87.50 | 45.83 | 95.83 | 5 | 6 | B |
Notes: Recommendation level: A, the score for each domain is ≥60%; B, ≥3 domains have scores ≥30% and at least one <60%.
Quality Evaluation of Systematic Reviews
A total of four systematic reviews were included in this study,28–31 and the evaluation results are shown in Table 4, all of which were approved for inclusion.
Table 4.
Quality Evaluation of Systematic Review
Quality Evaluation of Evidence Summaries
A total of three evidence summaries were included in this study.25–27 The evaluation of research items 3 and 4 of Queiroz25 was “no”, the assessment of items 2 and 5 was “incomplete”, and the evaluation of the remaining items was “yes”, which was approved for inclusion. In the study of Mi et al26 the assessment of item 2 was “incomplete”, the evaluation of item 3 was “no”, and the evaluation of other items was “yes”, which was approved for inclusion. In the study of Niu et al27 the assessment of item 2 was “incomplete”, the evaluation of items 3 and 9 was “no”, and the assessment of the rest of the items was “yes”, and the inclusion was granted.
Quality Evaluation of Randomized Controlled Trials
A total of two randomized controlled trials were included in this study.32,33 In the study of Kaźmierczak-Siedlecka et al32 the evaluation of items 3 and 11 was “unclear”, and the assessment of other items was “yes”, and the inclusion was granted. The evaluation of item 2 of Lei33 was “no”, the evaluation of item 6, 8, 9, and 12 was “yes”, and the evaluation of the remaining items was “unclear”, so it was not included.
Quality Evaluation of Experimental Studies
A total of four quasi-experimental studies were included in this study,18,34–36 and the evaluation results are shown in Table 5, all of which were approved for inclusion.
Table 5.
Quality Evaluation of Quasi-Experimental Study
Summary of Evidence
Finally, 18 pieces of evidence were extracted from 15 articles. Through extraction and summary, the best evidence for the management of home care for tube feeding in the elderly is divided into three aspects- nutrition support team (NST) management, training of caregivers, and selection of nutrition formulas. The evidence is shown in Table 6.
Table 6.
Best Evidence for Management of Home Care for Tube Feeding in the Elderly
| Category | Evidence Content | Evidence Level | |
|---|---|---|---|
| NST management | The establishment of NST | 1. Establish NST, including geriatricians, dietitians, nutrition support pharmacists, nursing managers, geriatricians, and community health care workers24,29,30,36 | 2c |
| 2. Community and hospital to form follow-up teams to establish timely communication, operating standards, and procedures to avoid duplication of work or inconsistent information29 | 1 | ||
| NST assessment and personalized management | 3. All the elderly with HETF should get a professional evaluation and adequate intervention, especially in case of complications or emergencies24 | 5b | |
| 4. NST should prescribe personalized HETF according to the evaluation results24,29,32,36 | 1 | ||
| Indicators of nutritional status, complications, and quality of life | 5. Indicators of nutritional status are mainly based on weight, body composition, and hydration status, but may also include laboratory measurements, such as serum albumin or transthyretin (prealbumin)24 | 5b | |
| 6. Complications monitoring should include tube-related complications and respiratory and digestive tolerance24 | 5b | ||
| 7. The NutriQoL® questionnaire should be used regularly to evaluate the quality of life of the elderly during HETF24 | 5b | ||
| Training of caregivers | Training methods should be diversified and individualized | 8. Mutual support and help between home caregivers can not only provide psychological comfort and reduce the burden but also allow them to learn from each other and share experiences29 | 1 |
| 9. Daily targeted health education, skill training, and workshops combined with a food model can be used for caregivers34 | 2c | ||
| 10. Education methods include oral education, graphic explanation, chatting Apps follow-up, Internet platform, etc.24 | 2c | ||
| Training on the prevention and solution of complications | 11. Apply daily cleaning, disinfection, drying, and preservation of dietary appliances. The prepared homemade blenderized admixtures should be stored in the refrigerator at 4°C for 24 hours, and it is better to use right after preparation18 | 2c | |
| 12. For the elderly with diarrhea, the temperature of the nutrition solution should be maintained at 38–42°C26 | 5b | ||
| 13. Elevate the head of the bed to 30–45° before feeding. After feeding, keep the original position for 30–60 minutes before laying down18,26 | 2c | ||
| 14. The diameter of the feeding tube should be at least 14Fr, and the homemade blenderized admixtures should be sieved with gauze to ensure that there are no large particles and avoid blockage18,24,25 | 5b | ||
| 15. Regularly flush the tube before and after feeding with at least 30mL of water of drinking quality in case of bolus administration or 4 hours if continuous feeding18,24,25 | 5b | ||
| 16. Call a doctor if the elderly have any of the following: tube blockage, prolapse or leakage; Signs of wound infection (if a gastrostomy tube is inserted) such as a fever of 100.4°F (38°C) or higher; Or if the place where the tube enters your body is red or swollen, feels warm to the touch, has discharge or pus, smells terrible, is very painful when touched, bleeds, or does not seem to be healing; Inability to defecate or pass gas, or have loose or hard stools; Stomach pain or cramping; Vomiting23 | 5b | ||
| Selection of nutrition formulas | The risk of homemade blenderized admixtures is higher than that of commercial formulas | 16. The elderly without diarrhea, constipation, or special diseases should use standard commercial formulas under the guidance of NST25,28 | 1c |
| To standardize the preparation process of homemade blenderized admixtures | 17. If there are special reasons to use homemade blenderized admixtures, dietitians can determine the formula, list standardized food combinations, regulate energy supply, and establish hygiene standards to prevent microbial contamination and infectious complications24,25,28 | 5b | |
| Semi-solid enteral nutrition can reduce the incidence of complications of gastric tube feeding | 18. Semi-solid enteral nutrition can improve the nutritional status of the elderly with gastric tube feeding and reduce the incidence of diarrhea, abdominal distension, reflux, and vomiting31 | 2a | |
Discussion
The Administration of NST
The Establishment of NST Can Improve the Quality of HETF Care Management
One guideline,24 one scoping review30 and one quasi-experimental study18 all mentioned the establishment of NST, indicating the importance of NST in the care and management of HETF in the elderly. It is showed that the blood indexes and body surface indexes of elderly with NST support were significantly improved, and the improvement was more significant over time.18
The composition of NST may differ according to different scenarios and local conditions, but the core includes doctors, dietitians, and nurses.24 Since this study focuses on the elderly who live at home, geriatricians and geriatric nurses are included in NST, which helps the team make decisions on the specific nutritional status and problems of the elderly. The close cooperation between NST and community medical staff can make the information interconnected and facilitate the unified operation standard, which plays a vital role in the follow-up of the nutritional status and the prevention of complications of the elderly.24 In particular, community dietitians can deal with common complications of HETF and issue prescriptions, thus reducing the need for the elderly to go to the hospital and relieving the economic burden.30 In addition, nutritional support pharmacists (NSP) can provide comprehensive and detailed drug information for medical staff, the elderly, and caregivers to reduce drug-related problems, improve compliance, and increase the qualified rate of HETF prescription.38 NST members work together to form an H2H (Hospital to Home) management model, which can improve the management level of home tube feeding care.39
NST Assessment and Personalized Management of HETF in the Elderly
NST should prescribe personalized HETF for the elderly based on careful consideration of the diseases of the elderly, the type of feeding tube, nutritional tolerance, personal preferences, and cultural background.18,24,29,32,36 (Table 7) For example, for the elderly with diarrhea and constipation, a nutritional solution containing fiber should be used, which can reduce blood glucose and increase albumin and hemoglobin without aggravating diarrhea.40–42 The elderly with diabetes can use modified formulas that are lower in sugar, contain slowly digestible carbohydrates, and are rich in unsaturated fatty acids, primarily monounsaturated fatty acids, which improve blood glucose control.43,44 The elderly with cancer can use the nutrient solution supplemented with Lactobacillus plantarum 299v, which can effectively improve the nutritional status, tolerance, and quality of life of the elderly.32 Regular intake of specific protein-enriched enteral formula can enhance protein synthesis and reduce protein degradation, which is effective to prevent Sarcopenia.45
Table 7.
Nutritional Solutions Associated with Common Diseases in the Elderly
| Diseases | Nutritional solutions |
|---|---|
| Standard situation (patients without diarrhea, constipation or diabetes) | Standard commercial formula |
| Diarrhea/constipation | Fiber-containing feeds |
| Diabetes | Lower sugar content, containing slowly digestible carbohydrates and a fat content enriched in unsaturated fatty acids, especially monounsaturated fatty acids |
| Sarcopenia | Essential amino acid-enriched enteral diet |
| Cancer | Nutrient solution supplemented with Lactobacillus plantarum 299v |
For the monitoring of nutritional indicators, in addition to body mass index (BMI)/calf circumference (CC), ADL, and IADL, laboratory indicators such as prealbumin and albumin are surrogate markers for the adequacy of short-term and long-term dietary intake, respectively.46 Among them, the half-life of prealbumin is about 1.9 days, which is a good predictor of whether the dietary energy and protein of the elderly are sufficient in the days before the test.47 The normal range of serum prealbumin in most laboratories is 20–40 mg/dL, with a cut-off value of 16–20mg/dL and a low level of less than 16mg/dL.48
NST evaluates the elderly with HETF and decides on intervention measures. However, due to the disparity of assessment standards across China and the lack of assessment tools specifically for the elderly with HETF, it is challenging to complete standardized and comprehensive evaluation and care of HETF, resulting in a high incidence of complications and a low quality of life for the elderly with HETF.49 Therefore, it is necessary to develop an assessment tool specifically suitable for the elderly with HETF in the future to guide community medical staff and caregivers in carrying out more standardized care for this population.
NST Monitoring of Quality of Life
World Health Organization (WHO) defines quality of life (QoL) as an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns. As HETF has a considerable physical, social, and psychological effect on the elderly, assessment of QoL is one of the important methods to qualify the effects of HEN. Support during and after tube insertion helps to reduce the impact on both, enabling them to make full use of their daily lives, sleep better, and enjoy an overall higher quality of life.50 Spanish scholars have developed NutriQoL, a life quality assessment scale specifically for HEN, which supports self-evaluation or peer evaluation and has good reliability and validity. It has been included in ESPEN guidelines and has become the main scale for quality of life with HEN.24,51
It seems that a standardized care coordination model involving a multidisciplinary team could improve outcomes.52 Studies suggested that care coordination including education of HETF users and professionals, proper assessment, timely follow-ups, and continuous auditing and feedback by NSTs is positively associated with improved outcomes in HETF users.53,54 However, the effectiveness of a particular intervention or team composition needs further research.
Training of Caregivers
Education and Training Methods Should Be Diversified and Individualized
Due to the shortage of community nursing resources and high cost, home caregivers are mainly informal caregivers who often lack care knowledge and skills.55 At the same time, the current HETF system in China is incomplete, and caregivers lack monitoring, follow-up, and guidance, resulting in a high incidence of HETF-related adverse events.56 Considering the characteristics of most non-professional caregivers, education models of HETF can be diversified and carried out as early as possible to ensure caregivers have sufficient time to understand, such as the workshop plus food model, daily goal health education model, etc.15,34 Training methods can be individualized according to the education level of caregivers, including graphic explanation, chatting Apps follow-up, Internet management platforms, and communication between caregivers.29,54,57,58 So that the communication of hospitals, communities, and tube feeding families can break through the limitations of time and space, and realize the intelligence and humanization of care services. Targeted and diversified education methods can help caregivers consolidate their knowledge of tube feeding, acquire care abilities, and improve compliance with tube feeding care to reduce the incidence of complications of enteral nutrition for the elderly with tube feeding at home, relieve the psychological burden of caregivers, and optimize the use of limited medical resources to achieve continuous, whole process and systematic tube feeding care management.34,54
Training on Prevention and Solution of Complications Related to HETF
A prospective, observational, multicenter real-life study showed educational support for both patients and trainers led to a significant reduction in all HEN-related adverse effects between the 3-month and 6-month visits.36 Therefore, it is necessary to improve the basic knowledge of caregivers.
To prevent blockage, feeding tubes with a diameter of at least 14Fr must be selected, the blenderized admixtures must be sieved, and the tubes must be regularly flushed.18,24 It is helpful to raise the head of the bed during tube feeding and maintain it after tube feeding to prevent aspiration.18,24 The homemade blenderized admixtures were prepared and stored according to the schedule, and the dietary appliance was cleaned daily to prevent infection.28 Heating the homemade blenderized admixtures to the appropriate temperature before use can prevent the occurrence of feeding intolerance, such as diarrhea and abdominal distension. Medical staff provide caregivers with educational content such as operation methods, daily care norms, and complication management, which is conducive to promoting caregivers’ adaptation to HETF and enhancing the safety of HETF.30
Selection of Nutrition Formulas
Commercial Formula is Better Than Homemade Blenderized Admixture
Currently, the typical formula of nutrient solutions for HETF in China are primarily homemade blenderized admixtures, that is, a paste thick fluid diet made from ordinary dishes. Dieticians should decide on the formula, list the standardized food combinations, normalize the supply of energy density, establish health standards to prevent microbial contamination and infectious complications, and adjust the formula at any time according to the condition of the elderly. However, studies have pointed out that the risk of using homemade blenderized admixtures is higher than that of commercial formulas, which not only have a higher rate of bacteria disqualification and lower nutrient content, but also have a higher risk of tube blockage.25,28,59,60 Therefore, the elderly without gastrointestinal-related complications or specific diseases should use standard commercial formulas under the guidance of experts.
To Standardize the Preparation Process of Homemade Blenderized Admixtures
Considering the advantages of low cost, convenient access, and high acceptance of homemade blenderized admixtures for the elderly,60 the current status is hard to change in a short time, so it is necessary to strengthen the standardization of homemade blenderized admixtures preparation at this stage. Scientific and reasonable preparation can significantly improve the nutritional status, reduce the economic burden, and improve the quality of life of the elderly.15
The application of semi-solid enteral nutrition can reduce the incidence of gastric tube feeding complications
Semi-solid enteral nutrition refers to the mixing of pectin and liquid nutrient solution into semi-cured chyle in the stomach by injecting pectin and other substances through a feeding tube, which is close to the state of gastric grinding chyme and more in line with the needs of the human body. After the semi-solid nutrient solution enters the stomach, it will cause the relaxation of the proximal part of the stomach and promote the secretion of digestive juice, thus inhibiting the occurrence of reflux, vomiting, abdominal distension, and diarrhea, to improve the nutritional status of the elderly.61 Now, the application of semi-solid enteral nutrition is widely carried out in Japan, while in China, a liquid homogenized diet or nutrient solution is mainly used, and there are few research studies and practices on semi-solid enteral nutrition. Moreover, the amount of pectin used, feeding speed, and time are inconsistent. In addition, some scholars have applied semi-solid enteral nutrition to post-pyloric feeding and proposed that such formulas can reduce diarrhea and constipation caused by post-pyloric feeding, improve nutritional indicators, and reduce inflammatory response. Still, no high-quality research has been conducted.62 Therefore, large-scale samples and high-quality randomized controlled trials are still needed to further explore the application and safety of semi-solid enteral nutrition.31
Limitations
The literature included in this study was only in Chinese and English, and literature in other languages was not included. And the quality of the included quasi-experimental studies needs to be improved.
Future Perspectives
1. Development of Specific Assessment Tools:
Future research should focus on developing and validating specific assessment tools tailored for elderly patients with HETF. These tools should address various aspects of care, including nutritional status, tube feeding-related complications and quality of life.
2. Standardization of Care Practices:
Studies are needed to establish standardized care protocols and guidelines for HETF in the elderly. This includes the formulation of personalized HETF plans based on individual patient characteristics, regular monitoring and evaluation of nutritional status, and prevention and management of complications.
3. Enhancement of Caregiver Education and Training:
Future studies should evaluate various education and training programs aimed at improving caregivers’ knowledge, skills, and compliance with HETF care protocols. The effectiveness of different teaching methods, such as face-to-face training, online courses, and mobile health applications, should be explored.
4. Exploration of New Technologies and Interventions:
Research should investigate the potential of new technologies and interventions to improve HETF care management in the elderly. This includes the use of telemedicine, remote monitoring, and artificial intelligence to support caregivers and patients in real-time.
Conclusion
This study summarizes the best evidence of HETF care management in the elderly, involving three aspects: NST administration, education of caregivers, and selection of enteral formulas. These aspects were subdivided into eight sections, which elaborate the necessity of developing a comprehensive care management system based on the trinity of hospital, community and home, aiming at providing evidence-based guidance for HETF care management of the elderly, reducing the incidence of complications, improving the quality of life, and providing a practical reference for NST members and caregivers.
It is recommended that evidence users consider the specific background and environment in the process of evidence transformation, select evidence according to local conditions, experience of carers, allocation of medical staff, and demands of the elderly, to make appropriate modifications, and develop personalized care management plans for the elderly with HETF.
Strengths
This research has a small starting point and is close to the current situation of home care, which has important social significance. A rigorous, evidence-based approach was used to identify high-quality literature in the field from comprehensive data sources. The extracted evidence is close to the actual problems of home care settings, which provides a basis for improving the quality of HETF care, reducing complications of the elderly, and improving their quality of life.
Acknowledgments
This work was supported by National Clinical Research Center for Geriatric Diseases, Chinese PLA General Hospital, Beijing, China (NCRCG-PLAGH-2024013).
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. Ca a Cancer J Clini. 2024;74(1):12–49. doi: 10.3322/caac.21820 [DOI] [PubMed] [Google Scholar]
- 2.Han BF, Zheng RS, Zeng HM, et al. Cancer incidence and mortality in China, 2022. J National Cancer Center. 2024;4(1):47–53. doi: 10.1016/j.jncc.2024.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mundi MS, Mohamed EO, Olson DA, et al. Home enteral nutrition: a descriptive study. JPEN J Parenter Enteral Nutr. 2023;47(4):550–562. doi: 10.1002/jpen.2498 [DOI] [PubMed] [Google Scholar]
- 4.Bulletin on the Basic Data of the Fifth Sampling Survey of the Living Conditions of the Elderly in China’s Urban and Rural Areas. Ageing China National Committee on; 2024. [Google Scholar]
- 5.Folwarski M, Kłęk S, Zoubek-Wójcik A, et al. Home Enteral Nutrition in Adults-Nationwide Multicenter Survey. Nutrients. 2020;12(7). doi: 10.3390/nu12072087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.David S. Nutrition support in intubated critically ill adult patients: enteral nutrition; 2024. Available from: https://lib.plagh.cn/s/cn/uptodate/www/G.https/contents/nutrition-support-in-intubated-critically-ill-adult-patients-enteral-nutrition. Accessed December 31, 2024
- 7.Sandhu R, Saran D, Ho G, Vandop K, Hussain W. High costs and limited dietitian services for home enteral nutrition users: a Canadian study. Nutr Clin Pract. 2022;37(1):167–175. doi: 10.1002/ncp.10649 [DOI] [PubMed] [Google Scholar]
- 8.Mohamed Elfadil O, Shah RN, Hurt RT, Mundi MS. Peptide-based formula: clinical applications and benefits. Nutr Clin Pract Apr. 2023;38(2):318–328. doi: 10.1002/ncp.10961 [DOI] [PubMed] [Google Scholar]
- 9.Zeng QW, Wang FF, Tang L, Li XL. Current situation and hotspot analysis of home care safety research for the elderly. Geriatrics Rese. 2022;3(01):22–28. [Google Scholar]
- 10.Qi MS, Wang XJ. Analysis on the status of home care adverse events and influence factors of the elderly incapacitated patients. J Mod Medi Health. 2019;35(4):494–498. [Google Scholar]
- 11.Chen YW, Jiang LL. Current Status of Enteral Nutrition Related Knowledge of Caregivers at Home. Nurs J Chin PLA. 2018;35(10):37–40. [Google Scholar]
- 12.Chen YW, Sun WG, Xi CH. Analysis of health education demand of family enteral nutrition caregivers. Chin Nurs res. 2017;31(24):3030–3032. [Google Scholar]
- 13.Deng XL, Peng XQ, Liang XJ. Analysis of health education needs of home enteral nutrition providers in stroke patients. J Nursi. 2011;18(12):74–76. [Google Scholar]
- 14.Farris C. The Teach Back Method Definition and Uses of the Teach-Back Method. Home Healthcare Nurse. 2015;33:344–345. doi: 10.1097/NHH0000000000000244 [DOI] [PubMed] [Google Scholar]
- 15.Xiao T, Zhou XM, Zhou JP, Lu MM. Using meticulous management to improve home enteral nutrition support for elderly patients with esophageal cancer. Nursin Integr Traditio Chin Medi. 2019;5(01):136–138. [Google Scholar]
- 16.J. KM, M. BJ, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–788. doi: 10.1007/s12603-009-0214-7 [DOI] [PubMed] [Google Scholar]
- 17.Li P, Zhang L, Yu ZQ, Chen ZQ, Wang Y. Present situation of home enteral nutrition. J Nurs Sci. 2017;32(11):105–109. [Google Scholar]
- 18.Chen Y, Sun Y, Huang DQ. Application of nutrition support team in elderly patients with home enteral nutrition. J Mod Medi Health. 2019;35(15):2376–2378. [Google Scholar]
- 19.S. MM, I. MJ, Mohamed Elfadil O, et al. Optimizing the nutrition support care model: analysis of survey data. JPEN J Parenter Enteral Nutr. 2022;46(7):1709–1724. doi: 10.1002/jpen.2326 [DOI] [PubMed] [Google Scholar]
- 20.AGREE Next Steps Consortium.The Agree II Instrument. 2024. Available from: https://www.agreetrust.org/wp-content/uploads/2017/12/AGREE-II-Users-Manual-and-23-item-Instrument-2009-Update-2017.pdf. Accessed December 31, 2024.
- 21.Foster MJ, Shurtz S. Making the Critical Appraisal for Summaries of Evidence (CASE) for evidence-based medicine (EBM): critical appraisal of summaries of evidence. J Med Libr Assoc. 2013;101(3):192–198. doi: 10.3163/1536-5050.101.3.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.JBI Levels of Evidence. The Joanna Briggs Institute. Available from: https://jbi.global/sites/default/files/2019-05/JBI-Levels-of-evidence_2014_0.pdf#:~:text=JBI%20Levels%20of%20Evidence.%20Developed%20by%20the%20Joanna%20Briggs%20Institute. Accessed December 31, 2024.
- 23.Crowley K, Hume K, Martin KA, McLaurin M Patient education: enteral (tube) feeding (The Basics). Available from: https://www.uptodate.com/contents/zh-Hans/enteral-tube-feeding-The-basics?topicRef=142296&source=related_link#H492000931. Accessed December 31, 2024
- 24.Bischoff SC, Austin P, Boeykens K, et al. ESPEN practical guideline: home enteral nutrition. Article Clin Nutr. 2022;41(2):468–488. doi: 10.1016/j.clnu.2021.10.018 [DOI] [PubMed] [Google Scholar]
- 25.Queiroz AB Enteral Tube Feeding (Adults): blenderized vs Commercial Formula; 2023. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=jbi&NEWS=N&AN=JBI19644. Accessed December 31, 2024.
- 26.Mi YY, Huang PP, Dong J, et al. Best evidence summary for prevention and management of enteral feeding intolerance in critically ill patients. Best evidence summary for prevention and management of enteral feeding intolerance in critically ill patients. Chin J Nurs. 2019;54(12):1868–1876.2020289440. [Google Scholar]
- 27.Niu YR, Lin QR, Wang L, Huang RY, Yang X, Hou M. Evidence summary on safety management of long-term home tube feeding in the elderly. J Nurs Sci. 2023;38(20):101–105. [Google Scholar]
- 28.Uniat KC, Stangarlin-Fiori L, Kruger JF, Madalosso Schieferdecker ME, Rabito EI. Microbiological quality of enteral formulations handled at home: a systematic review. Review J Paren Enteral Nutri. 2022;46(8):1787–1796. doi: 10.1002/jpen.2432 [DOI] [PubMed] [Google Scholar]
- 29.Mou JJ, Sun JN, Zhang R, Yang Y, Yang WW, Zhao XS. Experiences and needs of home caregivers for enteral nutrition: a systematic review of qualitative research. Review Nurs Open. 2022;9(1):11–21. doi: 10.1002/nop2.990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Byrnes C, Mockler D, Lyons L, Loane D, Russell E, Bennett AE. A scoping review of best practices in home enteral tube feeding. Review. Prim Health Care Res Devel. 2022;23:e43. doi: 10.1017/s1463423622000366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li CX, Shen MF. Effect of semi-solid enteral nutrition on gastrointestinal tolerance in patients with tube feeding: a meta-analysis. J Nursi. 2021;28(9):43–47.2021349680. [Google Scholar]
- 32.Kaźmierczak-Siedlecka K, Folwarski M, Skonieczna-żydecka K, Ruszkowski J, Makarewicz W. The use of Lactobacillus plantarum 299v (DSM 9843) in cancer patients receiving home enteral nutrition - study protocol for a randomized, double-blind, and placebo-controlled trial. Nutr J. 2020;19(1):98. doi: 10.1186/s12937-020-00598-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lei Z. Application of semi⁃cured homogenate diet with food thickener in senile patients with nasal feeding. Application of semicured homogenate diet with food thickener in senile patients with nasal feeding. Chin Nurs res. 2023;37(9):1653–1655.2023295635. [Google Scholar]
- 34.Chen Y, Huang DQ, Sun Y. The application of daily goal health education in caregivers of elderly patients with home nutrition. Practical Geria. 2020;34(4):400–401. [Google Scholar]
- 35.Zhu RM, Zhou JM. Effect of nasal feeding nursing training on caregivers of patients with nasal feeding at home. Electronic J Pract Clin Nu Scie. 2020;15(5):168–168,188. [Google Scholar]
- 36.Madrid-Paredes A, Leyva-Martínez S, Ávila-Rubio V, et al. Impact of nutritional and educational support on home enteral nutrition. J Health Popul Nutr. 2023;42(1):1–8. doi: 10.1186/s41043-023-00384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10). [DOI] [PubMed] [Google Scholar]
- 38.Chen QT, Zhong MR, Li JH, Wan YJ. Research progress on the status quo and intervention measures of standardized tube feeding by nurses. Chin Gene Pract Nur. 2023;21(01):42–45. [Google Scholar]
- 39.Zhou J, Wang L, Xin ZH. Application effect of ”H2H” nutrition management mode in patients with esophageal cancer undergoing nasal feeding at home. Chin J Mod Nurs. 2021;27(28):3858–3862. [Google Scholar]
- 40.Zarling EJ, Edison T, Berger S, Leya J, DeMeo M. Effect of dietary oat and soy fiber on bowel function and clinical tolerance in a tube feeding dependent population. J Am Coll Nutr. 1994;13(6):565–568. doi: 10.1080/07315724.1994.10718448 [DOI] [PubMed] [Google Scholar]
- 41.Kagansky M, Rimon E. Is there a difference in metabolic outcome between different enteral formulas? J Parenteral Enteral Nutr. 2007;31(4):320–323. doi: 10.1177/0148607107031004320 [DOI] [PubMed] [Google Scholar]
- 42.Elia M, Engfer MB, Green CJ, Silk DB. Systematic review and meta-analysis: the clinical and physiological effects of fibre-containing enteral formulae. Aliment Pharmacol Ther. 2008;27(2):120–145. doi: 10.1111/j.1365-2036.2007.03544.x [DOI] [PubMed] [Google Scholar]
- 43.Elia M, Ceriello A, Laube H, Sinclair AJ, Engfer M, Stratton RJ. Enteral nutritional support and use of diabetes-specific formulas for patients with diabetes: a systematic review and meta-analysis. Diab Care. 2005;28(9):2267–2279. doi: 10.2337/diacare.28.9.2267 [DOI] [PubMed] [Google Scholar]
- 44.Craig LD, Nicholson S, SilVerstone FA, Kennedy RD. Use of a reduced-carbohydrate, modified-fat enteral formula for improving metabolic control and clinical outcomes in long-term care residents with type 2 diabetes: results of a pilot trial. Nutrition. 1998;14(6):529–534. doi: 10.1016/s0899-9007(98)00062-8 [DOI] [PubMed] [Google Scholar]
- 45.Olza J, Mesa MD, Poyatos RM, et al. A specific protein-enriched enteral formula decreases cortisolemia and improves plasma albumin and amino acid concentrations in elderly patients. Nutr Metab. 2010;7:58. doi: 10.1186/1743-7075-7-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Measurement of visceral protein status in assessing protein and energy malnutrition: standard of care. Nutrition. 1995;11(2):169–171. [PubMed] [Google Scholar]
- 47.Elhasid R, Laor A, Lischinsky S, Postovsky S, Weyl Ben Arush M. Nutritional status of children with solid tumors. Cancer. 86(1999):119–125. [DOI] [PubMed] [Google Scholar]
- 48.Arcara K. Blood Chemistries and Body Fluids. In: Anderson C, Kapoor S, Mark T, editors. The Harriet Lane Handbook. Elsevier; 2012:639–650. [Google Scholar]
- 49.Xie JL, Huang HH, Li XL, Lin HX. IPE Applied to the Training of Home Enteral Nutrition for Community Medical Staff. Chinese Health Standard Management. 2021;12(17):93–96. [Google Scholar]
- 50.Day T. Home enteral feeding and its impact on quality of life. Brit J Comm Nur. 2017;22(Sup7):S14–S16. doi: 10.12968/bjcn.2017.22.Sup7.S14 [DOI] [PubMed] [Google Scholar]
- 51.Cuerda MC, Apezetxea A, Carrillo L, et al. Development and validation of a specific questionnaire to assess health-related quality of life in patients with home enteral nutrition: nutriQoL(®) development. Patient Prefe Adhe. 2016;10:2289–2296. doi: 10.2147/ppa.S110188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Excellence National Institute for Health and Care Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition. Available from: https://www.nice.org.uk/guidance/cg32. Accessed December 31, 2024. [PubMed]
- 53.Majka AJ, Wang Z, Schmitz KR, et al. Care Coordination to Enhance Management of Long-Term Enteral Tube Feeding. J Parenteral Enteral Nutr. 2014;38(1):40–52. doi: 10.1177/0148607113482000 [DOI] [PubMed] [Google Scholar]
- 54.Ling HF, Sun LK. Home enteral nutrition management for the elderly under the medical and elderly care combination service mode. J Nurs Sci. 2020;35(24):87–89. [Google Scholar]
- 55.Jukic PN, Gagliardi C, Fagnani D, Venturini C, Orlandoni P. Home Enteral Nutrition therapy: difficulties, satisfactions and support needs of caregivers assisting older patients. Clin Nutr. 2017;36(4):1062–1067. doi: 10.1016/j.clnu.2016.06.021 [DOI] [PubMed] [Google Scholar]
- 56.Li J. Influencing factors and countermeasures of maintenance compliance in discharged patients with nasal feeding tube. J Pract Med Tech. 2009;16(10):843–844. [Google Scholar]
- 57.Lv Y, Ding YF, Li PF, Sun Y. Application of discharge planning model in home care of elderly long⁃term tube feeding patients. Chin Nurs res. 2022;36(15):2693–2697. [Google Scholar]
- 58.Cai XC, Wang RY, Chen XZ. Construction and empirical study of home care model for elderly stroke patients with indwelling gastric tube in the Internet background. Chin Scie Techn J databa. 2023;4:0134–0137. [Google Scholar]
- 59.Ojo O, Adegboye ARA, Ojo OO, Wang X, Brooke J. An Evaluation of the Nutritional Value and Physical Properties of Blenderised Enteral Nutrition Formula: a Systematic Review and Meta-Analysis. Nutrients. 2020;12(6):1840. doi: 10.3390/nu12061840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yu FM, Shi L, Li K, Ning N, Chen MJ, Hu W. Comparison of nutrients between self-made homogenate diet and industcialigod enteral nutrition. Comparison of nutrients between self-made homogenate diet and industcialigod enteral nutrition product. Chinese J Clin Nutr. 2019;27(3):173–178. [Google Scholar]
- 61.Kong F, Singh RP. Disintegration of solid foods in human stomach. J Food Scie. 2008;73(5):R67–80. doi: 10.1111/j.1750-3841.2008.00766.x [DOI] [PubMed] [Google Scholar]
- 62.Zhu JH, Zhou ML, Sun HC, Fan YW. Application of semi-solidified enteral nutrition via pylorus in critically ill patients of neurosurgery. Application of semi-solidified enteral nutrition via pylorus in critically ill patients of neurosurgery. Jiangsu Med J. 2019;45(3):235–238.2019281620. [Google Scholar]