Abstract
Background/purpose
Computer-assisted implant surgery (CAIS) is increasingly performed to reduce deviations in implant position. Dynamic CAIS or navigation systems provide instant display of implant drilling instruments and patient positions directly on the computer monitor. Augmented reality (AR) technology allows operators to visualize real-time information projected onto the lenses of AR glasses. Although AR is being used in medical applications, there are few clinical studies on applying AR glasses to dental implants. The purpose of this randomized clinical study was to compare the accuracy of implant position using the dynamic CAIS with and without AR glasses.
Materials and methods
Twenty patients who needed a single dental implant were randomly divided into two groups: combined dynamic CAIS with AR glasses (AR glasses group, n = 10) and dynamic CAIS without AR glasses (non-AR glasses group, n = 10). Three-dimensional (3D) deviations of implant platform, apex and angular deviations were measured and analyzed using independent t-tests (P < 0.05).
Results
The 3D angular deviations in the AR glasses and non-AR glasses groups were 1.47 ± 1.01° and 2.42 ± 0.76°, respectively. Mean 3D entry point and apical deviations were 0.75 ± 0.45 mm and 0.87 ± 0.45 mm in the AR glasses group, whereas the non-AR glasses group were 1.11 ± 0.44 mm and 1.18 ± 0.50 mm, respectively. There was no statistically significant difference between the two groups.
Conclusion
Implant position accuracy using dynamic CAIS with AR glasses was similar to dynamic CAIS without AR glasses during a single implant placement.
Keywords: Computer-assisted implant surgery (CAIS), Dynamic system, Navigation, Accuracy, Augmented reality (AR)
Introduction
The goal of implant placement is to place a restoration that provides function, esthetic and maintenance of oral health. Optimal implant position is an important factor for successful implant supported prosthetic restorations.1 Malposition of implants, caused by improper treatment planning and/or improper surgical procedures, may lead to biologic failure, esthetic failure and/or mechanical failure. These complications can be prevented by proper treatment planning, proper site development and a good understanding of the restorative aspects of implantology.2,3
Computer-assisted implant surgery (CAIS) technologies are increasingly incorporated into various sectors of dentistry. Several studies have shown that these technologies can decrease the deviation between planned and placed position of dental implants. The two major techniques currently use are the static and dynamic systems.4 Static CAIS, or guided surgery, uses laboratory guided templates to fix implant position. This system composes of CT-generated CAD/CAM guide stents with metal tube. The dynamic CAIS system, or navigation system, is a technology that allows direct visualization of the implant drilling instruments and the patient position on a computer monitor in real time. Current navigation system is empowered by optical tracking technology, which continuously registers the position of the handpiece and the position of the patient and display them on the monitor, superimpose with preoperative CBCT image.5, 6, 7 The ideal implant position is planned digitally by the surgeon using 3D implant planning software. While the surgeon performs implant placement, tracking sensors attached on patient's jaw and handpiece will transfer 3D positional information to an overhead tracking camera or camera standing unit.8 The signal pathway is shown in Fig. 1. Subsequently, the system immediately calculates and displays the actual position of the surgical instruments in the surgical area superimpose on the preoperative CBCT image on a screen throughout the implant placement procedure. This system uses a mobile screen positioned near the dental chair, which requires the surgeon to monitor both the screen and the surgical site in the oral cavity, which may result in possible errors.9 Thus, the operator must pay attention to both the patient and navigation display at the same time.
Figure 1.
Signal path of the dynamic computer-assisted implant surgery (CAIS) system tracking sensors attached to the patient's target jaw. The handpiece transmits three-dimensional (3D) positional information to a camera standing unit.
Augmented reality (AR) is a type of technology that enhances an environment by superimposing computer-generated virtual material onto real structures. AR is a new development in field of medicine, and its applications are focused on specialties such as neurosurgery, laparoscopic, and plastic surgery.10, 11, 12 Medical education and training also make extensive use of AR technologies. Dentists may use AR when performing oral and maxillofacial surgery, or with dental implant placement and orthognathic procedures.13, 14, 15 AR allows the operator to visualize in real-time information projected onto the lenses of AR glasses via wireless technology.9,16 Benefits of AR included shortened surgery times, enhanced outcomes and reduced complications. However, there are some of the AR-related concerns. The most common risk of AR is cybersickness that be caused by a mismatch between the motion perceived visually in AR and the real-motion perceived with physical surrounding. Next, the minor side effects associated with AR glasses are disorientation, misjudgment of distanced and confusion between real and AR images.17,18
The application of AR when combined with navigation system might improve this issue and decrease the possibility of implant deviation. The AR system recognizes computer hardware and instantly displays current navigation images on the AR lens. Previous studies also showed that intraoperative visual assistance achieved successful implant positions and reduced the risk of iatrogenic damage to nearby anatomic structures such as the mandibular nerve or the maxillary sinus floor.19,20
Many studies reported the advantages of using CAIS in dental implant placement over freehand approach7,21,22 and conventional surgical guide stent.1,23, 24, 25 Some in vitro and clinical studies1,26, 27, 28 compared the deviation of implant position from virtual planning position using static CAIS system and dynamic CAIS system and reported that there are no significant differences between the two methods. However, there are few clinical studies that compare the implant deviation in dynamic CAIS systems with and without AR glasses. The purpose of this randomized clinical study was to compare the accuracy of implant position (i.e., deviation at entry point, apex, and the angulation of implant or the divergence of axis) between the implant placement using the dynamic CAIS system (navigation system) with and without AR glasses.
Materials and methods
Patient selection and study design
This prospective randomized clinical study was approved by the Human Research Ethics Committee of the Faculty of Dentistry Chulalongkorn University (study code: HREC-DCU 2022-042) and was also registered at the Thai Clinical Trials Registry (TCTR20210709003). The Clinical Trial Registration included two clinical protocols, with this manuscript reporting the results of Intervention Arm 3, while the outcomes of other intervention arms have been reported in a previous publication.29
The study followed the CONSORT statements. Patients who required a dental implant and eligible for surgical implant placement will be enrolled in this study. All implant surgeries were performed at Department of Oral and Maxillofacial Surgery, Chulalongkorn University between July 2022 to January 2024. The inclusion criteria required as (a) single tooth space which completely extracted at least 3 months prior and required single implant restoration at upper or lower arch, (b) adults aged 20–70 years, (c) ASA Physical Status Class I or II. The exclusion criteria were as followed: (a) uncontrolled systemic diseases, (b) taking anti-rejection medicine or osteoporosis drugs for long-term use, (c) immunodeficiency or history of malignancy within the past 5 years; (d) the case with filled bone graft, (e) the case of multiple missing teeth, (f) the case of dental bridge or dentures required. The required sample size was calculated based on a previous study of Block et al.8 using G∗power version 3.1 software with significance level (α) of 0.05 and power (1-β) of 0.95. The calculated sample size was 10 implants in each group.
The participating patients who met the inclusion criteria have signed informed consent and randomly divided into two groups equally: dynamic CAIS combined with AR glasses (AR glasses group, n = 10) and dynamic CAIS without AR glasses (non-AR glasses group, n = 10) using computer-generated random numbers within opaque sealed envelopes handling by one researcher (T.Y) who is not involved for surgery. All implants were operated by one expert surgeon (A.P) who familiar with CAIS and AR technologies, and performed approximately 1000 dental implants per year.
Presurgical preparation
Each patient received pre-operative cone-beam computed tomography (CBCT) image (X-mind® trium, Acteon, Varese, Italy) and visual planning for 3D implant position using a navigation system (Iris–100 version 6.8, EPED Inc., Kaohsiung, Taiwan).
Surgical procedure
The surgical procedures were operated under local anesthesia using the navigation system machine and components (Iris–100 version 6.8, EPED Inc.). Registration of the dynamic navigation system was done for the handpiece and patient's jaw position that is shown in Fig. 2. The operator performed implant placement with using AR glasses (Epson® Moverio BT-300, Seiko Epson Corporation, Tokyo, Japan) in the AR glasses group. The AR glasses were connected with the navigation system via bluetooth settings that is shown in Fig. 3. The operator could see the navigated images and monitor the drilling movement on the AR glasses. The bone level implants were placed following the protocol of the manufacturer (Straumann®, Institute Straumann AG, Basel, Switzerland). However, this surgery in which neither the participants nor the examiners knew which treatment or intervention participants were receiving until the clinical trial was over.
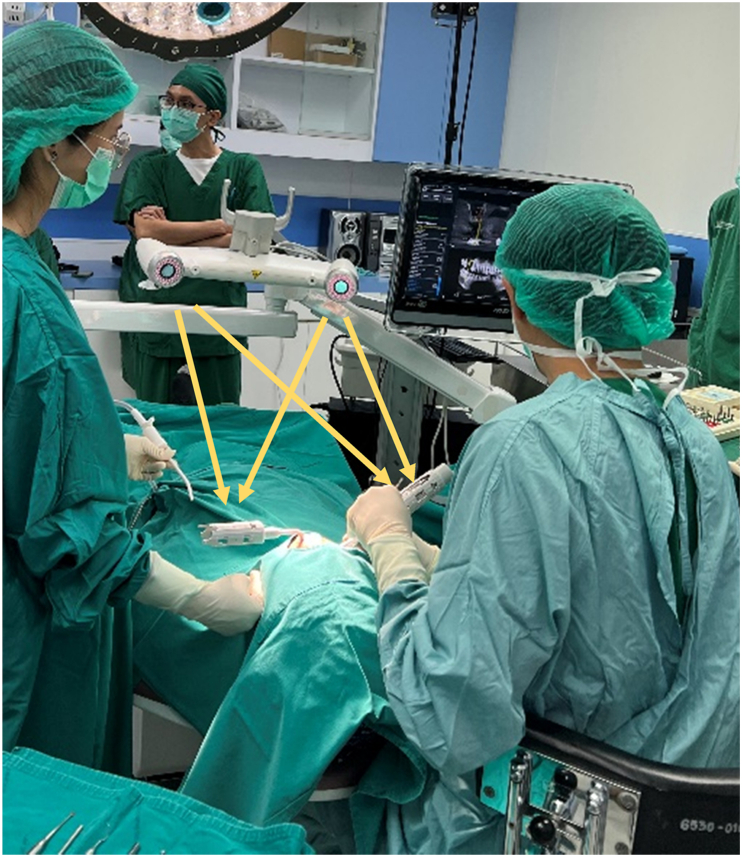
Figure 2.
Registration of the dynamic navigation system was done for the handpiece and the patient's jaw position.
Figure 3.
The operator performed implant placement using dynamic computer-assisted implant surgery (CAIS) combined with augmented reality (AR) glasses in the AR glasses group. The AR glasses were connected with the navigation system via bluetooth settings.
Postsurgical evaluation and measurement
All patients were prescribed systemic antibiotics (1 g amoxicillin twice a day) and analgesic (400 mg ibuprofen three times a day) for 5 days post-operatively. In patients with a reported allergy to penicillin, 300 mg clindamycin was administered three times a day for five days. Post-operative care instructions were given to all patients and suture removal took place 2 weeks later. The patients received post-operative CBCT (X-mind® trium, Acteon) with the similar setting to pre-operative image. Postoperative 3D implant position was superimposed onto the preoperative planning using treatment evaluation tool in the coDiagnostiX® software version 9.7 (Dental Wings Inc, Montreal, Canada) to evaluate the accuracy of implant placement via global implant deviations.
Accuracy evaluation
After image superimposition, the implant deviations were examined as defined below:
-
-
3D entry point deviation: displacement between the virtual planned and real placed implant at the implant platform in total direction, measuring at the center of the implant platform.
-
-
3D apical deviation: displacement between the virtual planned and real placed implant at the implant apex in total direction, measuring at the center of implant apex.
-
-
3D angular deviation/divergence of implant axis: angle difference of the implant axis that using an imaginary line crossed the center of the implant platform and the center of the implant apex between the virtual planned and real placed implant.
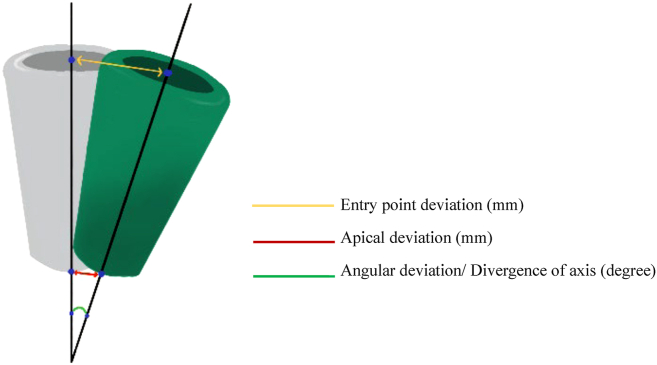
The two reference points of each deviation was shown in Fig. 4 and measured by one investigator (S.A) who was blinded to the group assignment of the patient's allocation.
Figure 4.
Implant deviations were measured using two reference points, including three-dimensional (3D) entry point deviation, apical deviation and angular deviation.
Statistical analysis
All measured data was gathered and analyzed using Statistical Package for Social Science version 22.0 (SPSS Inc., Chicago, IL, USA). The normality of distribution of all data was tested with Shapiro-Wilk test. The mean of 3D deviation at entry point, apex and axis of implants was compared between dynamic CAIS with and without AR glasses using independent t-test if the data was normally distributed or Mann-Whitney U test if the data was not normally distributed. P value < 0.05 was considered statistically significant.
Results
Twenty patients who needed a single implant and met the inclusion criteria were recruited in this study. The sex ratio (male:female) was 0.43 (6:14), aged range from 21 to 70 years old. All implants achieved primary stability with 25 Ncm insertion torque or more. The Implants used in this study were only Straumann bone level implants with the proper implant diameter and length depending on each patient's alveolar ridge dimensions (3.3BLT 10 and 12 mm, 4.1BLT 10 mm, 4.8BLT 8, 10 mm, and 12 mm, 5.0BLT 8 and 10 mm). All patients voluntarily participated throughout in this study without drop out and all measurements were conducted. The sample characteristics showed no significant differences between the two groups. The distribution of implants including type of arch, implant locations and sizes is presented in Table 1.
Table 1.
The distribution of implants including type of arch, implant locations and sizes in dynamic computer-assisted implant surgery (CAIS) with augmented reality glasses (AR glasses) and without augmented reality glasses (non-AR glasses).
| Variables | AR glasses (n = 10) | non-AR glasses (n = 10) |
|---|---|---|
| Type of arch | ||
| Maxilla | 6 | 7 |
| Mandible | 4 | 3 |
| Implant location | ||
| Anterior | 0 | 2 |
| Posterior | 10 | 8 |
| Implant diameter (mm) | ||
| 3.3 | 4 | 4 |
| 4.1 | 1 | 3 |
| 4.8 | 3 | 3 |
| 5.0 | 2 | 0 |
| Implant length (mm) | ||
| 8 | 2 | 2 |
| 10 | 5 | 6 |
| 12 | 3 | 2 |
The implant deviations including between the virtual planed and the actual placed positions for the AR glasses group and non-AR glasses group are presented in Table 2. Briefly, the 3D angular deviations in the AR glasses and non-AR glasses groups were 1.47 ± 1.01° and 2.42 ± 0.76°, respectively. Mean 3D entry point and apical deviations in the AR glasses group were 0.75 ± 0.45 mm and 0.87 ± 0.45 mm, respectively. Mean 3D entry point and apical deviations in the non-AR glasses group were 1.11 ± 0.44 mm and 1.18 ± 0.50 mm, respectively. A normal distribution was observed in all data; therefore, an independent t-test was applied. There were no significant differences between two groups; however, the results revealed a tendency of lower deviation of all aspects in the AR glasses group. All implant sites healed uneventfully with no major complications. Only post-operative mild pain and swelling were found.
Table 2.
The three-dimensional (3D) deviations at entry point, apex and axis of implants in dynamic computer-assisted implant surgery (CAIS) with augmented reality glasses (AR glasses) and without augmented reality glasses (non-AR glasses).
| Group | AR glasses (n = 10) | non-AR glasses (n = 10) | P value (independent t-test) |
|---|---|---|---|
| 3D Angular deviation (degree) | |||
| Mean ± SD | 1.47 ± 1.01 | 2.42 ± 0.76 | 0.50 |
| Median | 1.68 | 2.48 | |
| Min-Max | 0.00–2.90 | 1.15–3.79 | |
| 3D Entry point deviation (mm) | |||
| Mean ± SD | 0.75 ± 0.45 | 1.11 ± 0.44 | 0.96 |
| Median | 0.65 | 1.09 | |
| Min-Max | 0.12–1.61 | 0.53–1.97 | |
| 3D Apical deviation (mm) | |||
| Mean ± SD | 0.87 ± 0.45 | 1.18 ± 0.50 | 0.84 |
| Median | 0.82 | 1.14 | |
| Min-Max | 0.14–1.79 | 0.61–2.10 |
Independent t-test was performed at P value < 0.05; SD, standard deviation; Min, minimum value; Max, Maximum value.
Discussion
CAIS approaches in implant dentistry have been proofed relatively effective outcomes in terms of the accuracy of implant placement. Block et al.7 studied the implant placement deviation obtained by three operators using the dynamic navigation system in 100 partially edentulous patients. For the dynamic navigation group, the mean error of 0.87 ± 0.42 mm at the entry point, 1.56 ± 0.69 mm at the tip, and 3.62 ± 2.73° for angular deviations were showed. The similar results were reported with another study.4 The entry point, apical, and angular deviations had concordant mean values of 1.15 ± 0.59 mm, 2.51 ± 0.86 mm, and 7.69 ± 4.92°, for non-dynamically guided group, respectively. Stefanelli et al.30 stated the mean deviations of 0.71 ± 0.40 mm at the entry point, 1 ± 0.49 mm at the tip and also the mean angular deviation of 2.26 ± 1.62° in a retrospective study on 231 implants. Kaewsiri et al.26 studied the accuracy of the implant placement using static system compared to dynamic systems for 60 implants. The deviations were reported with 0.97 ± 0.44 mm at the entry point, 1.28 ± 0.46 mm at the tip, and 2.84 ± 1.71 degrees of the angular deviation in static system group. Whereas, the deviations were found 1.05 ± 0.4 mm at the entry point, 1.29 ± 0.50 mm at the tip, and the angular deviation of 3.06 ± 1.37° in the dynamic system group. They concluded that accuracy of implant placement in single implant case using dynamic CAIS appear to be the same to that of static CAIS.
Although the dynamic navigation shows some advantages, the operators are required to monitor and coordinate their vision of the screen along with the hand movements when using this system. Turning the head to view the navigation screen and look away from the operative field could result in accidental surgical instrument shifting or unexpected patient movement, especially in complex implant procedure. The usage of AR could solve these problems. Moreover, the AR using could also shorten the operating time.9,31
In our study, the implant position was mainly deviated depending on the drilling sequence and hand-eye coordinate by using the optical tracking of navigation system. There is no documentation of implant placements with simultaneous bone augmentation that subsequently affected implant deviation. Previous studies32,33 have mentioned that available bone and surrounding bone can also affect implant stability, but this was not specifically assessed and analyzed in our study.
A previous in vitro study,20 using stereolithographic stents integrated with AR-based surgical simulations, the mean deviations between planned and placed sites at the entry point, tip, angle, depth, and lateral locations were 0.50 ± 0.33 mm, 0.96 ± 0.36 mm, 2.70 ± 1.55°, 0.33 ± 0.27 mm, and 0.86 ± 0.34 mm for the fully edentulous mandibles, respectively. While, the mean deviations of 0.46 ± 0.20 mm, 1.23 ± 0.42 mm, 3.33 ± 1.42°, 0.48 ± 0.37 mm, and 1.1 ± 0.39 mm were reported for the partially edentulous maxilla, respectively. They concluded that the deviations of implant placement from planned position were significantly decreased by using surgical stents integrated with AR technology.
The recent in vitro study,15 compared the accuracy of dental implant placement using dynamic and AR-based dynamic navigation for 242 dental implants. They reported that AR-based dynamic navigation demonstrates a comparable accuracy to the conventional dynamic navigation system regarding coronal and apical deviations without any significant differences. However, the angular deviation showed significantly higher in the AR-based dynamic navigation group.
Dental implant procedures require biomechanical, functional, phonetic, and esthetic outcomes. Precise implant placement and accurate orientation are necessary, especially in complex cases.5,34,35 Our prospective clinical study confirmed the beneficial outcomes that AR can provide by eradicating hand-eye coordination obstacles. A dynamic navigation system and static guided approach with AR glasses allowed the operator to view both the surgical site and the virtual navigation system monitor, which displays the implant planning and virtual drilling onto the same field. Using the AR glasses, the operator could perform the implant surgery and clearly see the implant position without interference. In addition, AR glasses might also reduce the risk of overlay errors. This study showed that implant placement using AR glasses tended to present superior results to those without AR glasses. However, there was no statistically significant difference between two manners. All implant placements in this study were performed by one experienced operator to avoid any operator effect. To extend the utilizing of AR technology, the further studies should magnify a range of trained AR users with both experienced dentists and non-experienced operators such as dental students, and general practitioner.
The limitations of AR technology including an uncomfortable virtual screen positioning and orientation results in the necessary for the operator to tilt the head at ungraceful position. However, this inconvenience did not impact the study outcomes.36,37 The expense of the AR technology, setting time, and the additional software required for AR still are disadvantages. Moreover, the dilatory of the device's wireless connection and the degeneration of battery storage are also possible occurred. Although they were not mentioned in this investigation, these issues could be solved by improving and updating the implant software applications, and also upgrading the related hardware.
In addition, this study did not analyze the implant dimension, type of arch, nor whether they affected outcomes. These might be interesting for future research. Therefore, further studies including the placement of multiple implants in partially or fully edentulous patients are recommended. Moreover, further studies should evaluate the time restriction, cost-benefits, cost-effectiveness, and learning curve required for training.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgments
This study was supported by a research fund from Southern Taiwan Science Park Precision Health Cluster of National Science and Technology Council (grant number BX-03-11-15-111). N.M was supported by the Second Century Fund (C2F), Chulalongkorn University.
References
- 1.Somogyi-Ganss E., Holmes H.I., Jokstad A. Accuracy of a novel prototype dynamic computer-assisted surgery system. Clin Oral Implants Res. 2015;26:882–890. doi: 10.1111/clr.12414. [DOI] [PubMed] [Google Scholar]
- 2.Cooper L.F. In: Dental implant complications: etiology, prevention, and treatment. 2nd ed. Froum S.J., editor. Wiley-Blackwell; New Jersey: 2015. Prosthodontic complications related to non-optimal dental implant placement; pp. 539–558. [Google Scholar]
- 3.Chee W., Jivraj S. Failures in implant dentistry. Br Dent J. 2007;202:123–129. doi: 10.1038/bdj.2007.74. [DOI] [PubMed] [Google Scholar]
- 4.Block M.S., Emery R.W. Static or dynamic navigation for implant placement-choosing the method of guidance. J Oral Maxillofac Surg. 2016;74:269–277. doi: 10.1016/j.joms.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 5.Ewers R., Schicho K., Undt G., et al. Basic research and 12 years of clinical experience in computer-assisted navigation technology: a review. Int J Oral Maxillofac Surg. 2005;34:1–8. doi: 10.1016/j.ijom.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 6.Casap N., Wexler A., Eliashar R. Computerized navigation for surgery of the lower jaw: comparison of 2 navigation systems. J Oral Maxillofac Surg. 2008;66:1467–1475. doi: 10.1016/j.joms.2006.06.272. [DOI] [PubMed] [Google Scholar]
- 7.Block M.S., Emery R.W., Lank K., Ryan J. Implant placement accuracy using dynamic navigation. Int J Oral Maxillofac Implants. 2017;32:92–99. doi: 10.11607/jomi.5004. [DOI] [PubMed] [Google Scholar]
- 8.Jung R.E., Schneider D., Ganeles J., et al. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2009;24(Suppl):92–109. [PubMed] [Google Scholar]
- 9.Pellegrino G., Mangano C., Mangano R., Ferri A., Taraschi V., Marchetti C. Augmented reality for dental implantology: a pilot clinical report of two cases. BMC Oral Health. 2019;19:158. doi: 10.1186/s12903-019-0853-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sakellariou E., Alevrogiannis P., Alevrogianni F., et al. Single-center experience with Knee+™ augmented reality navigation system in primary total knee arthroplasty. World J Orthoped. 2024;15:247–256. doi: 10.5312/wjo.v15.i3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naito Y., Hasegawa M., Tone S., Wakabayashi H., Sudo A. Accuracy of cup placement and pelvic motion in total hip arthroplasty in the lateral decubitus position using a new computed tomography-based navigation system with augmented reality technology. Arch Orthop Trauma Surg. 2024;144:2381–2389. doi: 10.1007/s00402-024-05284-8. [DOI] [PubMed] [Google Scholar]
- 12.Kong H., Wang S., Zhang C., Chen Z., Wu Z., Wang J. A novel pedicle screw placement surgery based on integration of surgical guides and augmented reality. J Neurol Surg Cent Eur Neurosurg. 2023 doi: 10.1055/a-2200-3585. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 13.Fan X., Feng Y., Tao B., Shen Y., Wu Y., Chen X. A hybrid robotic system for zygomatic implant placement based on mixed reality navigation. Comput Methods Progr Biomed. 2024;249 doi: 10.1016/j.cmpb.2024.108156. [DOI] [PubMed] [Google Scholar]
- 14.Engelschalk M., Al Hamad K.Q., Mangano R., Smeets R., Molnar T.F. Dental implant placement with immersive technologies: a preliminary clinical report of augmented and mixed reality applications. J Prosthet Dent. 2024 doi: 10.1016/j.prosdent.2024.02.017. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 15.Tao B., Fan X., Wang F., Chen X., Shen Y., Wu Y. Comparison of the accuracy of dental implant placement using dynamic and augmented reality-based dynamic navigation: an in vitro study. J Dent Sci. 2024;19:196–202. doi: 10.1016/j.jds.2023.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwon H.B., Park Y.S., Han J.S. Augmented reality in dentistry: a current perspective. Acta Odontol Scand. 2018;76:497–503. doi: 10.1080/00016357.2018.1441437. [DOI] [PubMed] [Google Scholar]
- 17.Caserman P., Garcia-Agundez A., Gámez Zerban A., Göbel S. Cybersickness in current-generation virtual reality head-mounted displays: systematic review and outlook. Virtual Real. 2021;25:1153–1170. [Google Scholar]
- 18.Condino S., Carbone M., Piazza R., Ferrari M., Ferrari V. Perceptual limits of optical see-through visors for augmented reality guidance of manual tasks. IEEE Trans Biomed Eng. 2020;67:411–419. doi: 10.1109/TBME.2019.2914517. [DOI] [PubMed] [Google Scholar]
- 19.Ng F.C., Ho K.H., Wexler A. Computer-assisted navigational surgery enhances safety in dental implantology. Ann Acad Med Singapore. 2005;34:383–388. [PubMed] [Google Scholar]
- 20.Lin Y.K., Yau H.T., Wang I.C., Zheng C., Chung K.H. A novel dental implant guided surgery based on integration of surgical template and augmented reality. Clin Implant Dent Relat Res. 2015;17:543–553. doi: 10.1111/cid.12119. [DOI] [PubMed] [Google Scholar]
- 21.Nickenig H.J., Wichmann M., Hamel J., Schlegel K.A., Eitner S. Evaluation of the difference in accuracy between implant placement by virtual planning data and surgical guide templates versus the conventional free-hand method - a combined in vivo - in vitro technique using cone-beam CT (Part II) J Cranio-Maxillo-Fac Surg. 2010;38:488–493. doi: 10.1016/j.jcms.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 22.Behneke A., Burwinkel M., Behneke N. Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin Oral Implants Res. 2012;23:416–423. doi: 10.1111/j.1600-0501.2011.02337.x. [DOI] [PubMed] [Google Scholar]
- 23.Sarment D.P., Sukovic P., Clinthorne N. Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants. 2003;18:571–577. [PubMed] [Google Scholar]
- 24.Farley N.E., Kennedy K., McGlumphy E.A., Clelland N.L. Split-mouth comparison of the accuracy of computer-generated and conventional surgical guides. Int J Oral Maxillofac Implants. 2013;28:563–572. doi: 10.11607/jomi.3025. [DOI] [PubMed] [Google Scholar]
- 25.Amorfini L., Migliorati M., Drago S., Silvestrini-Biavati A. Immediately loaded implants in rehabilitation of the maxilla: a two-year randomized clinical trial of guided surgery versus standard procedure. Clin Implant Dent Relat Res. 2017;19:280–295. doi: 10.1111/cid.12459. [DOI] [PubMed] [Google Scholar]
- 26.Kaewsiri D., Panmekiate S., Subbalekha K., Mattheos N., Pimkhaokham A. The accuracy of static vs. dynamic computer-assisted implant surgery in single tooth space: a randomized controlled trial. Clin Oral Implants Res. 2019;30:505–514. doi: 10.1111/clr.13435. [DOI] [PubMed] [Google Scholar]
- 27.Ruppin J., Popovic A., Strauss M., Spüntrup E., Steiner A., Stoll C. Evaluation of the accuracy of three different computer-aided surgery systems in dental implantology: optical tracking vs. stereolithographic splint systems. Clin Oral Implants Res. 2008;19:709–716. doi: 10.1111/j.1600-0501.2007.01430.x. [DOI] [PubMed] [Google Scholar]
- 28.Kang S.H., Lee J.W., Lim S.H., Kim Y.H., Kim M.K. Verification of the usability of a navigation method in dental implant surgery: in vitro comparison with the stereolithographic surgical guide template method. J Cranio-Maxillo-Fac Surg. 2014;42:1530–1535. doi: 10.1016/j.jcms.2014.04.025. [DOI] [PubMed] [Google Scholar]
- 29.Yotpibulwong T., Arunjaroensuk S., Kaboosaya B., et al. Accuracy of implant placement with a combined use of static and dynamic computer-assisted implant surgery in single tooth space: a randomized controlled trial. Clin Oral Implants Res. 2023;34:330–341. doi: 10.1111/clr.14043. [DOI] [PubMed] [Google Scholar]
- 30.Stefanelli L.V., DeGroot B.S., Lipton D.I., Mandelaris G.A. Accuracy of a dynamic dental implant navigation system in a private practice. Int J Oral Maxillofac Implants. 2019;34:205–213. doi: 10.11607/jomi.6966. [DOI] [PubMed] [Google Scholar]
- 31.Jiang W., Ma L., Zhang B., et al. Evaluation of the 3D augmented reality-guided intraoperative positioning of dental implants in edentulous mandibular models. Int J Oral Maxillofac Implants. 2018;33:1219–1228. doi: 10.11607/jomi.6638. [DOI] [PubMed] [Google Scholar]
- 32.Putra R.H., Yoda N., Iikubo M., et al. Influence of bone condition on implant placement accuracy with computer-guided surgery. Int. J. Implant Dent. 2020;6:62. doi: 10.1186/s40729-020-00249-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Juodzbalys G., Kubilius M. Clinical and radiological classification of the jawbone anatomy in endosseous dental implant treatment. J Oral Maxillofac Res. 2013;4 doi: 10.5037/jomr.2013.4202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma L., Jiang W., Zhang B., et al. Augmented reality surgical navigation with accurate CBCT-patient registration for dental implant placement. Med Biol Eng Comput. 2019;57:47–57. doi: 10.1007/s11517-018-1861-9. [DOI] [PubMed] [Google Scholar]
- 35.Ewers R., Schicho K., Truppe M., et al. Computer-aided navigation in dental implantology: 7 years of clinical experience. J Oral Maxillofac Surg. 2004;62:329–334. doi: 10.1016/j.joms.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 36.Wang F., Bornstein M.M., Hung K., et al. Application of real-time surgical navigation for zygomatic implant insertion in patients with severely atrophic maxilla. J Oral Maxillofac Surg. 2018;76:80–87. doi: 10.1016/j.joms.2017.08.021. [DOI] [PubMed] [Google Scholar]
- 37.Pellegrino G., Tarsitano A., Taraschi V., Vercellotti T., Marchetti C. Simplifying zygomatic implant site preparation using ultrasonic navigation: a technical note. Int J Oral Maxillofac Implants. 2018;33:e67–e71. doi: 10.11607/jomi.6270. [DOI] [PubMed] [Google Scholar]