Abstract
The World Health Organization (WHO) has added glass ionomer cement (GIC) to the WHO Model List of Essential Medicines since 2021, which represents the most efficacious, safe and cost-effective medicines for priority conditions. With the potential increase in the use of GIC, this review aims to provide an overview of the clinical application of GIC with updated evidence in restorative and preventive dentistry. GIC is a versatile dental material that has a wide range of clinical applications, particularly in restorative and preventive dentistry. It has unique properties, such as direct adhesion to tooth structures, minimal shrinkage or expansion, a similar coefficient of thermal expansion to natural tooth structure, biocompatibility, and long-lasting fluoride release. According to the chemical composition, GIC can be classified as conventional glass ionomer cement (CGIC) and resin-modified glass ionomer cement (RMGIC). It has been used as restorative materials, luting cement for indirect restorations, liner and base of restorations, and dental sealants. While its use as a base material and liner is debatable, the clinical application of GIC as restorative cement, luting cement, and dental sealant is supported by current research.
Keywords: Glass ionomer cement, Dental caries, Preventive dentistry, Restorative dentistry, Review
Introduction
Dental caries, also known as tooth decay, is a widespread dental disease that affects a significant portion of the global population. Untreated caries can be severe, leading to pain, infection, and tooth loss. Around half of the world's population suffers from untreated dental caries. Approximately 2.5 billion adults, which accounts for about 35% of the global population, are estimated to have untreated caries in their permanent teeth. Approximately 573 million children, constituting approximately 9% of the global child population, suffer from untreated caries in their deciduous teeth.1,2 Dental caries exerts a significant economic burden on the community. The Global Burden of Disease Study reported that the estimated worldwide expenditures due to dental diseases totalled $544.41 billion in 2015. These numbers indicate the substantial socio-economic impact of untreated caries, affecting individuals, families and the community.1,3
The management of dental caries constitutes a significant portion of restorative and preventive dentistry. The commonly used restorative materials for caries management include dental amalgam, resin composite, and glass ionomer cement (GIC).4 Dental amalgam has been widely used for dental restorations for many years due to its high mechanical strength and longevity.5 However, mercury is harmful to the environment, and mercury poisoning can cause long-term and sometimes permanent neurological damage in human beings.6 Concerns regarding the potential adverse health effects of mercury have led to a global initiative to stop the production and use of mercury-containing products. The Minamata Convention on Mercury is a multilateral environmental agreement that addresses specific human activities which are contributing to widespread mercury pollution. 128 signatories and 133 parties around the world have signed the convention by March 2021. With the implementation of this agreement, the phase-down and eventual phase-out of dental amalgam is expected in the coming decades. Resin composite is another common restorative material with great physical and aesthetic properties for caries management.7 The major limitation of resin composite is the polymerization shrinkage, which could cause microleakage between the tooth and the restoration and increase the possibility of secondary caries and repair failure.8,9 Besides, resin composites are moisture-sensitive and technique sensitive. These drawbacks limited the application of resin composite in some clinical scenarios.
GIC has been available since the early 1970s. The FDI World Dental Federation has released a policy document recommending the development and the use of alternative direct restorative materials, including glass ionomer cement, to dental amalgam.10 The World Health Organization (WHO) has recognized the importance of GIC in dental care by including it in the Model List of Essential Medicines in 2021.11 With the background, an increase in the use of GIC is plausible. Therefore, this review aims to provide an overview of the clinical application of GIC with updated evidence in restorative and preventive dentistry.
Classification of GIC based on chemical composition
GIC is derived from silicate and zinc polycarboxylate cements.12 It has powder and liquid counterparts and consists of polymeric matrices with ionic crosslinking around reinforcing glass particles after the mixture of powder and liquid. The powder is normally composed of three basic components: silica (SiO2), alumina (Al2O3) and calcium fluoride (CaF2). Some manufacturers also add amalgam alloy particles or silver particles into the basic powders to enhance the mechanical strength of the GIC materials. The liquid is an aqueous solution of polyalkenoic acids with or without the addition of resin components.13 Based on the chemical composition and set reactions, GIC can be generally classified into conventional glass ionomer cement and resin-modified glass ionomer cement.
Conventional glass ionomer cement (CGIC)
Conventional glass ionomer cement (CGIC) is composed of a powder and a liquid. The powder typically contains a basic ion-leachable glass, such as fluoro-aluminosilicate glass, while the liquid is a polymeric water-soluble acid and water. The setting reaction is an acid–base reaction and starts from the mixture of powder and liquid.14 Examples of the commercially available products of CGIC include Fuji I (GC Corporation, Tokyo, Japan), GC Fuji IX GP (GC Corporation), Equia Forte HT (GC Corporation), Equia Forte Fil (GC Corporation), 3M™ Ketac™ Cem (3M ESPE, St Paul, MN, USA), Ketac Universal (3M ESPE), Chemfil Rock (Dentsply Sirona, Konstanz, Germany), ChemFlex (Dentsply Sirona), Aqua Ionofil (VOCO, Cuxhaven, Germany) and Riva Self Cure (SDI, Bayswater, VIC, Australia).
High-viscosity GIC (HVGIC) is a type of CGIC which set by mixing with a high powder/liquid ratio. It was introduced in 1995.15 HVGIC has been used as a restorative material for Atraumatic Restorative Treatment (ART), which is a minimally invasive technique. HVGIC is preferred for ART application due to its superior mechanical properties, better marginal seal and longer clinical durability.16 Examples of the commercially available products of HVGIC include Fuji IX GP (GC Corporation), Equia Forte Fil (GC Corporation), Ketac Molar Easymix (3M ESPE), Ketac Universal (3M ESPE), Chemfil Rock (Dentsply Sirona) and Riva Self Cure (SDI).
Resin-modified glass ionomer cement (RMGIC)
To overcome the traditional problems including compromised mechanical strength, wear resistance and aesthetics associated with CGIC materials, a type of glass ionomer cement called resin-modified glass ionomer cement (RMGIC) was introduced in 1989. RMGIC maintains the clinical advantages of CGIC, such as fluoride release and simplicity in clinical operation, and is more aesthetically pleasing than CGIC. The powder composition of RMGIC is similar to CGIC, which contains a basic ion-leachable glass, while the liquid part contains a water-soluble resin monomer, a polymeric water-soluble acid and water. The setting reaction of RMGIC involves both resin polymerization and an acid–base reaction.18,19 The common resin added into RMGIC includes Bisphenol-A glycidylmethacrylate (Bis-GMA), urethane dimethacrylate (UDMA), dimethacrylate (TEGDMA), 2-hydroxyethyl methacrylate (HEMA). Examples of the commercially available products of RMGIC include Fuji II LC (GC Corporation), GC Fuji PLUS (GC Corporation), Fuji Lining LC (GC Corporation), RelyX™ Luting (3M ESPE), Ketac™ Cem Plus (3M ESPE), Vitremer (3M ESPE), Photac-Fil (3M ESPE), Vitrebond™ (3M ESPE) and Riva Light Cure (SDI).
Metal-reinforced GIC
Metal-reinforced GIC is a type of GIC containing metal powders. The liquid composition is similar to that of other GICs, while the powder consists of a mixture of conventional powder with amalgam alloy particles or silver particles sintered with the glass. These cements have arisen with the expectation of improved mechanical properties. The inclusion of metallic particles brought damage to materials in relation to fluoride release, and adhesion to tooth structure, as well as the aesthetic damage arising from the darkening of the edges of the cavities.17 Examples of the commercially available products of metal-reinforced GIC include Ketac-Silver (3M ESPE), Miracle Mix® (GC Corporation) and Hi-Dense XP (SHOFU, Kyoto, Japan).
Physical and chemical properties of GIC
GIC has unique advantages for clinical application, including direct adhesion to tooth structures, minimal shrinkage or expansion, similar coefficient of thermal expansion to natural tooth structure, biocompatibility, and long-lasting fluoride release.20, 21, 22 As shown in the scanning electron microscope images, the surfaces of Fuji IX GP (GC Corporation) and Fuji II LC (GC Corporation) have irregular glass-ceramic structure with uneven particle distribution (Fig. 1).
Figure 1.
Properties of glass ionomer cement (GIC). A) Surface morphology and elemental composition of the GIC; B) Surface topography in 2D (left) and 3D (right) with surface roughness value in Ra of GIC; C) The daily fluoride ion release in various groups for 720 days. CGIC: conventional GIC; RMGIC: resin-modified GIC.
GIC can directly adhere to tooth structures by forming an ionic bond with the calcium ions in the hydroxyapatite of the tooth structure.23 Direct adhesion allows the application of GIC without extra adhesive systems, which are normally expensive and can significantly increase the cost of clinical procedures. In addition, the waiver of the extra adhesive procedures makes the clinical operation simple and saves the chairside operation time.
GIC is biocompatible, as the pulp response to GIC is mild.24 Polyacrylic acid has macromolecule structures with high molecular weight and is prone to combine with the calcium ions of the tooth, making it difficult to move into the dentinal tubules. Generally, they are less irritating to the pulp tissues when compared to resinous adhesives.23 However, in some deep or very deep cavities close to the dental pulp, the acid portion of the ionomer might cause pulp irritation.12 The biocompatibility of GIC was observed not only in dental pulp tissues but also in periodontal tissues. GIC was capable of reducing subgingival biofilm attachment without irritating the gingiva tissues.25,26
GIC presents minimal shrinkage or expansion after setting. It has a linear thermal expansion coefficient which is close to that of the dental structures. This feature, combined with the direct chemical bonding with the dental structures, results in a reduced chance of marginal leakage clinically.12 The values of the thermal expansion coefficient in RMGIC are closer to those presented by the amalgam and resin composite.12,27
GICs are known for long-lasting fluoride release, which can be extended for up to 8 years.22 The fluoride release shows a pattern of an initial rapid release (“early burst”), followed by a sustained and lower level diffusion-based release.28,29 We detect the fluoride released of CGIC and RMGIC restoration for 720 days. The daily fluoride release in the CGIC and RMGIC Groups was highest on Day 1 and dropped to a lower level on Day 84. The stable low-level fluoride release was maintained until Day 720 (Fig. 1C). CGIC restoration released more fluoride compared to RMGIC restoration. Fluoride release from GIC increases in acidic conditions.30 This ability to release and store fluoride makes GIC an excellent choice in treating patients at high risk for caries.17
However, GIC also has disadvantages, such as lower compressive strength, lower flexural strength, compromised aesthetics and limited antimicrobial effects.31
GIC exhibits lower compressive strength and lower flexural strength compared to dental amalgam and resin composite. Its compressive strength ranges between 60 and 300 MPa and flexural strength ranges between 14 and 50 MPa.21 The mechanical strength of GIC varies largely among the products from different companies. The mechanical strength of GIC limits their extensive use in dentistry as a filling material in stress-bearing areas.27,32,33 In addition, GIC, particularly CGIC, showed lower wear resistance compared to resin composite and amalgam. The unsatisfactory wear resistance could reduce the longevity of the material when applied in areas bearing heavy abrasive wear.34
GIC has an opaque to translucent appearance. CGIC is opaque. RMGIC has a translucent appearance and matches dentin and enamel shade aesthetically.35 However, the shade range of GIC is limited and the aesthetic properties of GIC are generally inferior to that of resin composites.26
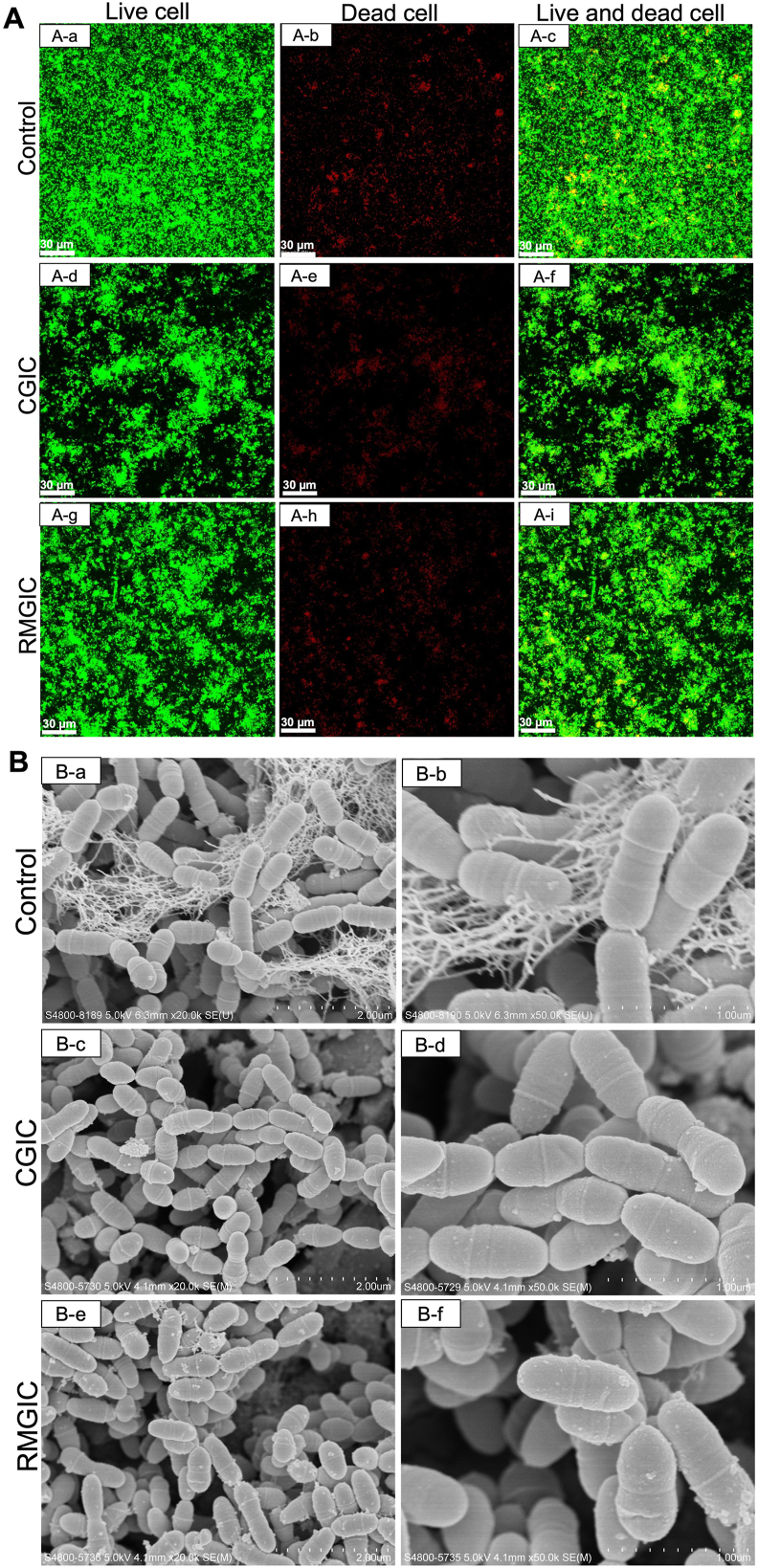
GIC shows limited antimicrobial effects. Although GIC can release fluoride release sustainably to prevent caries in the dental tissues,36,37 the influence of fluoride on the antimicrobial properties of GIC is limited, especially after the setting reaction is completed.38 When cultivating Streptococcus mutans (S. mutans) biofilms on CGIC and RMGIC include Fuji IX GP (GC Corporation) and Fuji II LC (GC Corporation) dentin surfaces and observing the biofilm with confocal laser scanning microscopy, a large proportion of green fluorescence, representing living cells, was found on the CGIC, RMGIC and dentin block surfaces (control). There were no differences in the proportion of dead cells among CGIC, RMGIC and control group (Fig. 2A). When observing the biofilm structure with scanning electron microscopy, CGIC, RMGIC and dentine surfaces were all fully covered by biofilm of normal structure with no significant differences (Fig. 2B). These assessments indicated that the antimicrobial effects of CGIC, RMGIC and dentine were similar. The Fuji IX GP (GC Corporation) and Fuji II LC (GC Corporation) were selected as examples of conventional glass ionomer cement (CGIC) and resin-modified glass ionomer cement (RMGIC), respectively to assess their physical and chemical properties. However, due to potential variations within each of these specific product lines, they may not fully capture the entire range of characteristics exhibited by all commercial products of CGIC and RMGIC. To obtain a more comprehensive understanding of the physical and chemical properties of GICs, testing a broader selection of GIC commercial products would be beneficial.
Figure 2.
Properties of glass ionomer cement (GIC). A) Representative confocal laser-scanning microscopy images of GIC; B) Representative scanning electron microscope images of glass ionomer cement. CGIC: conventional GIC; RMGIC: resin-modified GIC; control: dentin block.
Major clinical application of GICs
GIC have various applications in restorative and preventive dentistry. It has been commonly used as restorative materials, luting cements, liners and bases, and fissure sealants with different powder-to-liquid ratios. Understanding the properties, clinical indications and the clinical performance of GIC for different applications is essential to achieve optimal clinical outcomes when using the GIC material.
GIC as restorative cement
Suggested clinical uses of GIC restorations
Glass ionomer cements are a versatile direct restorative material with multiple clinical indications because of its chemical, mechanical and biological properties.17 For GIC restorative cements, a high powder-to-liquid ratio (at least 3:1, and up to 6.8:1) is employed, which ensures sufficient strength and durability of the restoration.14
Modification of GIC restorative materials has been made to enhance its biological, mechanical and antimicrobial properties to broaden its clinical applications. The most common modifications of GIC were to add functional filler components into GIC, such as silver-amalgam particles,39 spherical silica,40 zirconia,41 glass fibre,42 hydroxyapatite,43 bioactive glass particles as pre-reacted glass ionomer particles (PRG),44 etc.
GIC is excellent for interim restorations. They could be used for the repair of small defective margins of resin-based composite or silver amalgam restorations.17,45 GIC can be used for occlusal restorations in primary teeth.19 In the permanent dentition, small, minimally invasive preparations in the occlusal surface can be restored with RMGIC.46 RMGIC is good for occlusal-proximal restorations in primary molars.47 In addition, the self-adhesive and easy handling properties and acceptable tooth-coloured appearance of RMGIC greatly simplify restorative procedures for carious and non-carious lesions located in the cervical areas of the teeth, particularly for patients in high caries risk or teeth that cannot be isolated ideally.48
Clinical performance of GIC restoration
A study in 2018 included 1.6 million GIC restorations and evaluated their survivability. The survival to re-intervention rate of GIC was 81% at 1 year, 52% at 5 years, 36% at 10 years, 28% at 15 years in upper molars, and 81%, 49%, 34%, and 26% at 1, 5, 10, and 15 years in lower molars, respectively.49 GIC exhibited significantly lower values of secondary carious lesions (SCL) than resin composite in primary teeth.50
Teeth restored with atraumatic restorative treatment (ART) techniques using GIC have exhibited a wide range of survival rates, from 29.6 to 100%, over 4-month to 6-year follow-ups for single occlusal restorations, and 30.6–100% over 6-month to 2-year follow-ups for multi-surface restorations.51 Another study on the survival rate of Fuji IX GP Fast (GC Corporation) and Equia Fil (GC Corporation) restoration found that at a 3-month recall, the retention of RMGIC restorations was 97.06%. At a 6-month recall, the retention of GIC averaged 95.6%. At the 12-month recall, the retention of RMGIC averaged 93.35%. At a 2-year recall, the retention of GIC averaged 91.1%. At 3-year recall, the retention of GIC averaged 83.35%.52
Previous studies have proved the advantageous clinical performance of using GIC for caries restoration. A systematic review and meta-analysis compared the preventive effect of GIC restorations on new caries formation on other teeth of the dentition with other types of restorations. This study got the conclusion that CGIC restorations presented a better caries preventive effect on new caries than RMGIC and amalgam restorations did in primary dentitions. RMGIC restorations showed a similar preventive effect on new caries formation to resin composite restorations in both primary and permanent dentitions.53 The systematic review on the comparison of the preventive effect of secondary caries among different types of restorations found that GIC restorations showed a superior preventive effect against secondary caries compared to amalgam restorations and resin composite restorations in primary teeth. Meanwhile, GIC restorations showed a superior preventive effect against secondary caries compared to amalgam and a similar preventive effect against secondary caries compared to resin composite restorations in permanent teeth.22
GIC as luting cement
Suggested clinical uses of GIC luting cements
Luting cement is a material used to attach indirect restorations to prepared tooth surfaces by filling the minute voids between the restorations and the tooth structures, locking the restoration mechanically to prevent dislodgement.54 GIC's adhesive properties ensure a secure bond between the restoration and the tooth structure without the application of extra adhesive systems, as it chemically bonds to enamel, dentine, precious metals and porcelain restorations. It reduces the incidence of microleakage when used to cement resin composite inlays or onlays. It is easy to mix with good flowability. It sets fast with a low film thickness and low viscosity.55, 56, 57 It reaches the neutral pH rapidly after being placed on the prepared tooth.58 When using GIC as luting cement, a powder-to-liquid ratio ranging from 1.5:1 to 3.8:1 is commonly employed for cementation of inlays, onlays, crowns and bridges.14
Novel GIC luting cements are under development by modifying GIC materials. Nano-modifications of GIC by either reducing the size of the glass particles or the addition of nano-sized bioceramics were made to improve its mechanical and physical properties.59 Another modification was the addition of calcium sodium phosphosilicate bioactive glass to GIC to promote its remineralising effect on demineralized enamel lesions.60
CGIC luting cements are generally used for the cementation of full metallic and metal-ceramic crowns and fixed dental partial, metal-ceramic crowns with porcelain margins, slip-cast alumina crowns, metal posts, inlays, implant-supported crowns and bridges, and aesthetic post and core (fibre and ceramic).61,62 RMGICs are indicated to retain total crowns and bridges, metal–ceramic crowns and bridges, zirconia frameworks and restorations, metal posts, metal inlays, orthodontic appliances, and aesthetic post and core (fibre and ceramic).61, 62, 63
Clinical performance of GIC luting cement
Meron (VOCO) CGIC luting cement used on the veneered yttrium-stabilized tetragonal zirconia polycrystal zirconia crowns presented a 100% retention rate after 2 years and a 95.8% retention rate after 4 years.64 One study aimed to evaluate and compare the long-term clinical retention of prefabricated zirconia crowns (PZCs) in primary molar teeth cemented using different luting cements CGIC, RMGIC and resin composite, including Fuji I® (GC Corporation), BioCem™ (Nusmile, Houston, TX, USA) and Clearfil SA Luting (Kuraray, Okayama, Japan), respectively. The study found that the survival rate of PZCs was 76.7% when using CGIC cement, 50% when using RMGIC cement, and 70% when using resin cement after three years. The mean survival for PZC in the CGIC group (35.5 months) was significantly higher than for resin composite (34.7 months), and RMGIC (33 months; P = 0.019).65
GIC as liner and base
Suggested clinical uses of GIC liner or base
Liners and bases are materials placed between dentin (sometimes pulp) and the restoration to provide pulpal protection. GIC can be used as a liner or base to reduce sensitizing by protecting and insulating dental pulp. It is a good option for liners or bases because of their biomimetic nature and physical properties that are similar to those of dentin.66 GIC used as a liner in dental restorations was found to reduce the problems associated with microleakage. This might be attributed to the antimicrobial properties of GIC.67 Another advantage of using GIC is that the use of RMGIC as a liner can significantly reduce the volumetric polymerization contraction that occurs with light-cured resin-based restorations.68 GICs have advantages as cavity liners because they bond to dentin/enamel and release fluoride. These properties not only help in preventing decay and minimizing the chance of the appearance of secondary caries but also promote the formation of tertiary dentin.69 For GIC liner cement, a powder-to-liquid ratio of 1.5:1 is typically recommended to achieve good adaptation and provide a protective layer between the tooth structure and restorative materials. On the other hand, GIC bases require a higher powder-to-liquid ratio, ranging from 3:1 to 6.8:1, to provide adequate strength and support for the restoration.14
GIC can be used as a liner material between the tooth structure and the definitive restorative material including resin composite and amalgam.69,70 GIC can also be used as a base since it meets the characteristics of a base.71 Currently, GIC is usually not promoted as a base but rather as a core build-up material (eg, Fuji II LC Core Material, GC; Vitremer, 3M ESPE).72
Clinical performance of GIC liner or base
It should be noted that current evidence revealed a contradictory result regarding the necessity of the use of GIC liner for pulp protection. GIC might cause less pulpal damage compared to other restorative materials. In vivo studies on human teeth have shown that Vitrebond™ Plus (3M ESPE) and Vitrebond™ (3M ESPE) RMGIC liner caused only mild initial pulp damage when applied to deep dentin caries, which decreased over time, indicating its acceptable compatibility with the pulp.73 The pulpal response to CGIC and RMGIC including Riva Self Cure (SDI) and Riva Light Cure (SDI) were slightly different, with the latter potentially causing more damage.74 However, the initial pulp damage caused by GIC tends to decrease over time. Both CGIC and RMGIC were considered biocompatible after 30 days, suggesting that any adverse pulpal effects might be transient. When used as liners in very deep cavities, neither CGIC nor RMGIC resulted in post-operative sensitivity or persistent pulp damage.74 However, a study found no statistical difference in success rate on the pulpal outcome between the Fuji II Lining LC (GC Corporation) RMGIC liner group and the group without liner.75
Studies on the survival rate of the restorations with GIC liner or base showed that GIC liner or base did not have significant effects on the survival rate of the restorations. A study found that the application of Ionoseal (VOCO) RMGIC liner did not have a significant effect on the clinical performance of bulk-fill restorations, suggesting that GIC-based liner might be unnecessary for the bulk-filled resin composite.76 Another study on the effect of Fuji Lining LC (GC Corporation) RMGIC liner on the quality of posterior resin composite restorations found that the retention rate was 100% for restoration with and without RMGIC liner for 1 year. This study showed that the qualities of the restorations were not significantly affected by the placement of the RMGIC liner, regardless of the adhesive used.77 For the GIC base, a study on the influence of Ketac-Fil (3M ESPE) CGIC base in survival of posterior composite restorations found that the annual failure rate was 1.9% for restorations with CGIC base and 2.1% for restorations without intermediate material for up to 18 years follow-up. This study showed that CGIC base did not affect the survival of resin composite restorations.78
GIC as fissure sealant
Suggested clinical uses of dental sealant
Dental sealants are used to prevent dental caries in tooth surfaces, particularly those with pits and fissures.79 The mechanisms of dental sealant in preventing and arresting dental caries include creating a physical barrier, ease of cleaning and ion release.79, 80, 81 GIC sealants are fluoride-releasing, which can prevent caries by reducing demineralization and inhibiting cariogenic bacteria growth.82,83 Moreover, they can offer protection to both sealed teeth and adjacent teeth.84,85 The GIC sealant has a fluid consistency to allow its adaption into the pits and fissure area of the posterior teeth. GIC sealants normally have a powder-to-liquid ratio ranging from 1.1:1 to 1.8:1, which ensures proper flowability and allows for effective sealing of the pits and fissures.14
GIC sealants are indicated for patients at high caries risk in both permanent and primary teeth.86,87 Except for applying on occlusal fissure surfaces, current evidence also supports the application of GIC sealant on axial smooth surfaces. It can be used in preventing caries on sound tooth surfaces or arresting caries on carious tooth surfaces.88
Clinical performance of GIC dental sealant
GIC sealants was effective in preventing caries on sound tooth surfaces including occlusal fissure surfaces, decreasing the caries risk of sound teeth by 76% within 24–48 months, and 85% in 84 months compared to no treatment.89,90 GIC dental sealant was effective in arresting non-cavitated caries with 2–3 times higher when compared with no treatment.91,92 However, the effectiveness of dental sealant in arresting cavitated caries was controversial. Some studies showed its success in arresting initial to moderate stage caries,93,94,88 while others reported that dental sealant was ineffective for micro-cavitated caries lesions.95
However, the retention of GIC sealants was not satisfactory. A review reported that the retention rate for GIC sealant at different follow-up periods was 49–63% at 6 months, 21–78% at 12 months, and 14–24% at 24 months.88 More recently, a meta-analysis on the clinical retention of pit and fissure sealants in relation to observation time and material type found that the retention rates for high-viscosity GIC-based sealants were 5.2% at 5 years.96
Summary
Glass ionomer cement is a versatile dental material that has a wide range of applications in restorative and preventive dentistry. It has been used as restorative materials, luting cement for indirect restorations, liner and base of restorations, and dental sealants. While its use as a base material and liner is debatable, the clinical application of GIC as restorative cement, luting cement, and dental sealant is supported by current research.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The authors gratefully acknowledge the financial support from the Health and Medical Research Fund, Food and Health Bureau of Hong Kong SAR, China (No. 09200926).
References
- 1.Righolt A., Jevdjevic M., Marcenes W., Listl S. Global-, regional-, and country-level economic impacts of dental diseases in 2015. J Dent Res. 2018;97:501–507. doi: 10.1177/0022034517750572. [DOI] [PubMed] [Google Scholar]
- 2.Collaborators G.O.D., Bernabe E., Marcenes W., et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99:362–373. doi: 10.1177/0022034520908533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peres M.A., Macpherson L.M., Weyant R.J., et al. Oral diseases: a global public health challenge. Lancet. 2019;394:249–260. doi: 10.1016/S0140-6736(19)31146-8. [DOI] [PubMed] [Google Scholar]
- 4.Reza Rezaie H., Beigi Rizi H., Rezaei Khamseh M.M., Öchsner A. 2020. Dental restorative materials. A review on dental materials. Cham: Springer International Publishing AG 2020 1st Edition; pp. 47–171. [Google Scholar]
- 5.Flanders R.A. Mercury in dental amalgam-a public health concern? J Publ Health Dent. 1992;52:303–311. doi: 10.1111/j.1752-7325.1992.tb02293.x. [DOI] [PubMed] [Google Scholar]
- 6.Report of the informal global WHO consultation with policymakers in dental public health, 2021: monitoring country progress in phasing down the use of dental amalgam. https://www.who.int/publications/i/item/9789240038424 Available at:
- 7.Pratap B., Gupta R.K., Bhardwaj B., Nag M. Resin based restorative dental materials: characteristics and future perspectives. Jpn Dent Sci Rev. 2019;55:126–138. doi: 10.1016/j.jdsr.2019.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarrett D.C. Clinical challenges and the relevance of materials testing for posterior composite restorations. Dent Mater. 2005;21:9–20. doi: 10.1016/j.dental.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Li Z., Zhang H., Xiong G., et al. A low-shrinkage dental composite with epoxy-polyhedral oligomeric silsesquioxane. J Mech Behav Biomed Mater. 2020;103 doi: 10.1016/j.jmbbm.2019.103515. [DOI] [PubMed] [Google Scholar]
- 10.Alternative direct restorative materials to dental amalgam.Available at: https://www.fdiworlddental.org/alternative-direct-restorative-materials-dental-amalgam [Date accessed: Septemeber, 2023] [DOI] [PMC free article] [PubMed]
- 11.Global oral health status report: towards universal health coverage for oral health by 2030. World Health Organization; 2022. Licence: CC BY-NC-SA 3.0 IGO; Geneva: 2022. https://www.who.int/publications/i/item/9789240070868 Available at: [Google Scholar]
- 12.Rizzante F., Cunali R., Bombonatti J., Correr G., Gonzaga C., Furuse A. Indications and restorative techniques for glass ionomer cement. RSBO. 2016;12:70–79. [Google Scholar]
- 13.Nicholson J., Czarnecka B. Review paper: role of aluminum in glass-ionomer dental cements and its biological effects. J Biomater Appl. 2009;24:293–308. doi: 10.1177/0885328209344441. [DOI] [PubMed] [Google Scholar]
- 14.Sidhu S.K., Nicholson J.W. A review of glass-ionomer cements for clinical dentistry. J Funct Biomater. 2016;7:16. doi: 10.3390/jfb7030016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zecevic Culina M., Rajić V., Šalinović I., Klarić E., Marković L., Ivanisevic A. Influence of pH cycling on erosive wear and color stability of high-viscosity glass ionomer cements. Materials. 2022;15:923. doi: 10.3390/ma15030923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hegde D., Suprabha B.S., Rao A. Organic antibacterial modifications of high-viscosity glass ionomer cement for atraumatic restorative treatment: a review. Jpn Dent Sci Rev. 2024;60:22–31. doi: 10.1016/j.jdsr.2023.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Almuhaiza M. Glass-ionomer cements in restorative dentistry: a critical appraisal. J Contemp Dent Pract. 2016;17:331–336. doi: 10.5005/jp-journals-10024-1850. [DOI] [PubMed] [Google Scholar]
- 18.Agha A., Parker S., Patel M.P. Development of experimental resin modified glass ionomer cements (RMGICs) with reduced water uptake and dimensional change. Dent Mater. 2016;32:713–722. doi: 10.1016/j.dental.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Vaikuntam J. Resin-modified glass ionomer cements (RMGICs) implications for use in pediatric dentistry. ASDC (Am Soc Dent Child) J Dent Child. 1997;64:131–134. [PubMed] [Google Scholar]
- 20.Hoshika S., Ting S., Ahmed Z., et al. Effect of conditioning and 1 year aging on the bond strength and interfacial morphology of glass-ionomer cement bonded to dentin. Dent Mater. 2021;37:106–112. doi: 10.1016/j.dental.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 21.Lohbauer U. Dental glass ionomer cements as permanent filling materials?—properties, limitations future trends. Materials. 2010;3:76–96. [Google Scholar]
- 22.Ge K.X., Quock R., Chu C.H., Yu O.Y. The preventive effect of glass ionomer cement restorations on secondary caries formation: a systematic review and meta-analysis. Dent Mater. 2023;39:1–17. doi: 10.1016/j.dental.2023.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Sikka N., Brizuela M. Glass ionomer cement. StatPearls; 2024. [Google Scholar]
- 24.Khoroushi M., Keshani F. A review of glass-ionomers: from conventional glass-ionomer to bioactive glass-ionomer. Dent Res J. 2013;10:411–420. [PMC free article] [PubMed] [Google Scholar]
- 25.Santos V.R., Lucchesi J.A., Cortelli S.C., Amaral C.M., Feres M., Duarte P.M. Effects of glass ionomer and microfilled composite subgingival restorations on periodontal tissue and subgingival biofilm: a 6-month evaluation. J Periodontol. 2007;78:1522–1528. doi: 10.1902/jop.2007.070032. [DOI] [PubMed] [Google Scholar]
- 26.Sidhu S.K. Glass-ionomer cement restorative materials: a sticky subject? Aust Dent J. 2011;56(Suppl 1):23–30. doi: 10.1111/j.1834-7819.2010.01293.x. [DOI] [PubMed] [Google Scholar]
- 27.Davidson C.L. Advances in glass-ionomer cements. J Appl Oral Sci. 2006;14(Supp l):3–9. doi: 10.1590/s1678-77572006000700002. [DOI] [PubMed] [Google Scholar]
- 28.Forsten L. Fluoride release and uptake by glass ionomers. Scand J Dent Res. 1991;99:241–245. doi: 10.1111/j.1600-0722.1991.tb01891.x. [DOI] [PubMed] [Google Scholar]
- 29.De Witte A.M., De Maeyer E.A., Verbeeck R.M., Martens L.C. Fluoride release profiles of mature restorative glass ionomer cements after fluoride application. Biomaterials. 2000;21:475–482. doi: 10.1016/s0142-9612(99)00188-x. [DOI] [PubMed] [Google Scholar]
- 30.Lewis S.M., Coleman N.J., Booth S.E., Nicholson J.W. Interaction of fluoride complexes derived from glass-ionomer cements with hydroxyapatite. Ceramics. 2013;57:196–200. [Google Scholar]
- 31.Nantanee R., Santiwong B., Trairatvorakul C., Hamba H., Tagami J. Silver diamine fluoride and glass ionomer differentially remineralize early caries lesions, in situ. Clin Oral Invest. 2016;20:1151–1157. doi: 10.1007/s00784-015-1603-4. [DOI] [PubMed] [Google Scholar]
- 32.Forss H., Seppä L., Lappalainen R. In vitro abrasion resistance and hardness of glass-ionomer cements. Dent Mater. 1991;7:36–39. doi: 10.1016/0109-5641(91)90024-s. [DOI] [PubMed] [Google Scholar]
- 33.Reddy D.S., Kumar R.A., Venkatesan S.M., Narayan G.S., Duraivel D., Indra R. Influence of citric acid on the surface texture of glass ionomer restorative materials. J Conserv Dent. 2014;17:436–439. doi: 10.4103/0972-0707.139830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao J., Weng Y., Xie D. In vitro wear and fracture toughness of an experimental light-cured glass–ionomer cement. Dent Mater. 2009;25:526–534. doi: 10.1016/j.dental.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 35.Attaie A.B., Ouatik N. In: Esthetic dentistry. 3rd ed. Aschheim K.W., editor. Mosby; St. Louis: 2015. Esthetics and pediatric dentistry; pp. 423–439. [Google Scholar]
- 36.Wiegand A., Buchalla W., Attin T. Review on fluoride-releasing restorative materials--fluoride release and uptake characteristics, antibacterial activity and influence on caries formation. Dent Mater. 2007;23:343–362. doi: 10.1016/j.dental.2006.01.022. [DOI] [PubMed] [Google Scholar]
- 37.Ananda S.R., Mythri H. A comparative study of fluoride release from two different sealants. J Clin Exp Dent. 2014;6:497–501. doi: 10.4317/jced.51507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yesilyurt C., Er K., Tasdemir T., Buruk K., Celik D. Antibacterial activity and physical properties of glass-ionomer cements containing antibiotics. Operat Dent. 2009;34:18–23. doi: 10.2341/08-30. [DOI] [PubMed] [Google Scholar]
- 39.Bala O., Arisu H.D., Yikilgan I., Arslan S., Gullu A. Evaluation of surface roughness and hardness of different glass ionomer cements. Eur J Dermatol. 2012;6:79–86. [PMC free article] [PubMed] [Google Scholar]
- 40.Tjandrawinata R., Irie M., Suzuki K. Effect of 10 wt% spherical silica filler addition on the various properties of conventional and resin-modified glass-ionomer cements. Acta Odontol Scand. 2005;63:371–375. doi: 10.1080/00016350500206819. [DOI] [PubMed] [Google Scholar]
- 41.Gu Y.W., Yap A.U.J., Cheang P., Koh Y.L., Khor K.A. Development of zirconia-glass ionomer cement composites. J Non-Cryst Solids. 2005;351:508–514. [Google Scholar]
- 42.Bakhadher W. Modification of glass ionomer restorative material: a review of literature. EC Dent Sci. 2019;18:1001–1006. [Google Scholar]
- 43.Lucas M.E., Arita K., Nishino M. Toughness, bonding and fluoride-release properties of hydroxyapatite-added glass ionomer cement. Biomaterials. 2003;24:3787–3794. doi: 10.1016/s0142-9612(03)00260-6. [DOI] [PubMed] [Google Scholar]
- 44.Ikemura K., Tay F.R., Endo T., Pashley D.H. A review of chemical-approach and ultramorphological studies on the development of fluoride-releasing dental adhesives comprising new pre-reacted glass ionomer (PRG) fillers. Dent Mater J. 2008;27:315–339. doi: 10.4012/dmj.27.315. [DOI] [PubMed] [Google Scholar]
- 45.Pitel M.L. Reconsidering glass-ionomer cements for direct restorations. Comp Cont Educ Dent. 2014;35:26–31. [PubMed] [Google Scholar]
- 46.Croll T.P., Killian C.M. Glass-ionomer-silver-cermet interim Class I restorations for permanent teeth. Quintessence Int. 1992;23:731–733. [PubMed] [Google Scholar]
- 47.Dermata A., Papageorgiou S.N., Kotsanos N. Three-year performance of a nano-filled resin-modified glass ionomer cement in class II primary molar restorations. Eur Arch Paediatr Dent. 2021;22:425–432. doi: 10.1007/s40368-020-00574-2. [DOI] [PubMed] [Google Scholar]
- 48.Berg J.H., Croll T.R. Glass ionomer restorative cement systems: an update. Pediatr Dent. 2015;37:116–124. [PubMed] [Google Scholar]
- 49.Burke F.J.T., Lucarotti P.S.K. The ultimate guide to restoration longevity in England and Wales. Part 3: glass ionomer restorations - time to next intervention and to extraction of the restored tooth. Br Dent J. 2018;224:865–874. doi: 10.1038/sj.bdj.2018.436. [DOI] [PubMed] [Google Scholar]
- 50.Dias A.G.A., Magno M.B., Delbem A.C.B., Cunha R.F., Maia L.C., Pessan J.P. Clinical performance of glass ionomer cement and composite resin in Class II restorations in primary teeth: a systematic review and meta-analysis. J Dent. 2018;73:1–13. doi: 10.1016/j.jdent.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 51.Panetta A., Lopes P., Novaes T.F., Rio R., Fernandes G.V.O., Mello-Moura A.C.V. Evaluating glass ionomer cement longevity in the primary and permanent teeth-an umbrella review. J Funct Biomater. 2024;15:48. doi: 10.3390/jfb15020048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Heck K., Frasheri I., Diegritz C., Manhart J., Hickel R., Fotiadou C. Six-year results of a randomized controlled clinical trial of two glass ionomer cements in class II cavities. J Dent. 2020;97 doi: 10.1016/j.jdent.2020.103333. [DOI] [PubMed] [Google Scholar]
- 53.Ge K.X., Quock R., Chu C.H., Yu O.Y. The preventive effect of glass ionomer restorations on new caries formation: a systematic review and meta-analysis. J Dent. 2022;125 doi: 10.1016/j.jdent.2022.104272. [DOI] [PubMed] [Google Scholar]
- 54.Hill E.E., Lott J. A clinically focused discussion of luting materials. Aust Dent J. 2011;56(Suppl 1):67–76. doi: 10.1111/j.1834-7819.2010.01297.x. [DOI] [PubMed] [Google Scholar]
- 55.Rv Noort. 4th ed. 2013. Introduction to dental materials. [Google Scholar]
- 56.Craig R.G., Powers J.M., Wataha J.C. Mosby; 2000. Dental materials: properties and manipulation. [Google Scholar]
- 57.Kenneth J., Anusavice D., Shen C., Rawls H.R. Elsevier Health Sciences; 2012. Phillips' science of dental materials. [Google Scholar]
- 58.Christensen G.J. Why is glass ionomer cement so popular? J Am Dent Assoc. 1994;125:1257–1258. doi: 10.14219/jada.archive.1994.0156. [DOI] [PubMed] [Google Scholar]
- 59.Najeeb S., Khurshid Z., Zafar M.S., et al. Modifications in glass ionomer cements: nano-sized fillers and bioactive nanoceramics. Int J Mol Sci. 2016;17:1134. doi: 10.3390/ijms17071134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim D.A., Lee J.H., Jun S.K., Kim H.W., Eltohamy M., Lee H.H. Sol–gel-derived bioactive glass nanoparticle-incorporated glass ionomer cement with or without chitosan for enhanced mechanical and biomineralization properties. Dent Mater. 2017;33:805–817. doi: 10.1016/j.dental.2017.04.017. [DOI] [PubMed] [Google Scholar]
- 61.Ghazy M.H., Aboumadina M.M., Mahmoud S.H. Retentiveness of metal coping luted to teeth of uremic patients undergoing hemodialysis using five different luting cements. Operat Dent. 2014;39:101–108. doi: 10.2341/12-523-LR2. [DOI] [PubMed] [Google Scholar]
- 62.Lad P.P., Kamath M., Tarale K., Kusugal P.B. Practical clinical considerations of luting cements: a review. J Int Oral Health. 2014;6:116–120. [PMC free article] [PubMed] [Google Scholar]
- 63.Leevailoj C., Platt J.A., Cochran M.A., Moore B.K. In vitro study of fracture incidence and compressive fracture load of all-ceramic crowns cemented with resin-modified glass ionomer and other luting agents. J Prosthet Dent. 1998;80:699–707. doi: 10.1016/s0022-3913(98)70058-7. [DOI] [PubMed] [Google Scholar]
- 64.Torres C., Ávila D., Gonçalves L.L., et al. Glass ionomer versus self-adhesive cement and the clinical performance of zirconia coping/press-on porcelain crowns. Operat Dent. 2021;46:362–373. doi: 10.2341/20-229-C. [DOI] [PubMed] [Google Scholar]
- 65.Srinivasan S.R., Mathew M.G., Jayaraman J. Comparison of three luting cements for prefabricated zirconia crowns in primary molar teeth: a 36-month randomized clinical trial. Pediatr Dent. 2023;45:117–124. [PubMed] [Google Scholar]
- 66.Frencken J.E. The state-of-the-art of ART sealants. Dent Update. 2014;41:119–120. doi: 10.12968/denu.2014.41.2.119. [DOI] [PubMed] [Google Scholar]
- 67.Prati C., Fava F., Di Gioia D., Selighini M., Pashley D.H. Antibacterial effectiveness of dentin bonding systems. Dent Mater. 1993;9:338–343. doi: 10.1016/0109-5641(93)90053-s. [DOI] [PubMed] [Google Scholar]
- 68.Tolidis K., Nobecourt A., Randall R.C. Effect of a resin-modified glass ionomer liner on volumetric polymerization shrinkage of various composites. Dent Mater. 1998;14:417–423. doi: 10.1016/s0300-5712(99)00016-0. [DOI] [PubMed] [Google Scholar]
- 69.Mount G.J. Esthetics with glass-ionomer cements and the "sandwich" technique. Quintessence Int. 1990;21:93–101. [PubMed] [Google Scholar]
- 70.Sikka N.B.M. StatPearls [Internet]. Treasure Island (FL) StatPearls Publishing; 2024. Glass ionomer cement.https://www.ncbi.nlm.nih.gov/books/NBK582145/ Available from: [Updated 2024 Mar 4] [Google Scholar]
- 71.Ricketts D. Management of the deep carious lesion and the vital pulp dentine complex. Br Dent J. 2001;191:606–610. doi: 10.1038/sj.bdj.4801246. [DOI] [PubMed] [Google Scholar]
- 72.Weiner R. Liners, bases, and cements: material selection and clinical applications. Dent Today. 2005;24:66–72. [PubMed] [Google Scholar]
- 73.Costa C.A., Ribeiro A.P., Giro E.M., Randall R.C., Hebling J. Pulp response after application of two resin modified glass ionomer cements (RMGICs) in deep cavities of prepared human teeth. Dent Mater. 2011;27:158–170. doi: 10.1016/j.dental.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 74.Ribeiro A.P.D., Sacono N.T., Soares D.G., Bordini E.A.F., de Souza Costa C.A., Hebling J. Human pulp response to conventional and resin-modified glass ionomer cements applied in very deep cavities. Clin Oral Invest. 2020;24:1739–1748. doi: 10.1007/s00784-019-03035-3. [DOI] [PubMed] [Google Scholar]
- 75.Singh S., Mittal S., Tewari S. Effect of different liners on pulpal outcome after partial caries removal: a preliminary 12 months randomised controlled trial. Caries Res. 2019;53:547–554. doi: 10.1159/000499131. [DOI] [PubMed] [Google Scholar]
- 76.Torres C.R.G., Mailart M.C., Rocha R.S., et al. The influence of a liner on deep bulk-fill restorations: randomized clinical trial. J Dent. 2020;102 doi: 10.1016/j.jdent.2020.103454. [DOI] [PubMed] [Google Scholar]
- 77.Banomyong D., Harnirattisai C., Burrow M.F. Posterior resin composite restorations with or without resin-modified, glass-ionomer cement lining: a 1-year randomized, clinical trial. J Investig Clin Dent. 2011;2:63–69. doi: 10.1111/j.2041-1626.2010.00036.x. [DOI] [PubMed] [Google Scholar]
- 78.van de Sande F.H., Da Rosa Rodolpho P.A., Basso G.R., et al. 18-year survival of posterior composite resin restorations with and without glass ionomer cement as base. Dent Mater. 2015;31:669–675. doi: 10.1016/j.dental.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 79.Ahovuo-Saloranta A., Forss H., Walsh T., Nordblad A., Mäkelä M., Worthington H.V. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev. 2017;7 doi: 10.1002/14651858.CD001830.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ramamurthy P., Rath A., Sidhu P., et al. Sealants for preventing dental caries in primary teeth. Cochrane Database Syst Rev. 2022;2:CD012981. doi: 10.1002/14651858.CD012981.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Balian A., Campus G., Bontà G., et al. Long-term caries prevention of dental sealants and fluoride varnish in children with autism spectrum disorders: a retrospective cohort study. Sci Rep. 2022;12:8478. doi: 10.1038/s41598-022-12176-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Philip N. State of the art enamel remineralization systems: the next frontier in caries management. Caries Res. 2019;53:284–295. doi: 10.1159/000493031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Johnston N.R., Strobel S.A. Principles of fluoride toxicity and the cellular response: a review. Arch Toxicol. 2020;94:1051–1069. doi: 10.1007/s00204-020-02687-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Alsabek L., Al-Nerabieah Z., Bshara N., Comisi J.C. Retention and remineralization effect of moisture tolerant resin-based sealant and glass ionomer sealant on non-cavitated pit and fissure caries: randomized controlled clinical trial. J Dent. 2019;86:69–74. doi: 10.1016/j.jdent.2019.05.027. [DOI] [PubMed] [Google Scholar]
- 85.Cagetti M.G., Carta G., Cocco F., et al. Effect of fluoridated sealants on adjacent tooth surfaces: a 30-mo randomized clinical trial. J Dent Res. 2014;93:59–65. doi: 10.1177/0022034514535808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Akinlotan M., Chen B., Fontanilla T.M., Chen A., Fan V.Y. Economic evaluation of dental sealants: a systematic literature review. Community Dent Oral Epidemiol. 2018;46:38–46. doi: 10.1111/cdoe.12326. [DOI] [PubMed] [Google Scholar]
- 87.Griffin S., Wei L., Gooch B., Weno K., Espinoza L. Vital signs: dental sealant use and untreated tooth decay among U.S. school-aged children. MMWR Morb Mortal Wkly Rep. 2016;65:1141–1145. doi: 10.15585/mmwr.mm6541e1. [DOI] [PubMed] [Google Scholar]
- 88.Ng T.C.H., Chu C.H., Yu O.Y. A concise review of dental sealants in caries management. Front Oral Health. 2023;4 doi: 10.3389/froh.2023.1180405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wright J.T., Tampi M.P., Graham L., et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: a systematic review of randomized controlled trials- a report of the American dental association and the American academy of pediatric dentistry. J Am Dent Assoc. 2016;147:631–645. doi: 10.1016/j.adaj.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 90.Ahovuo-Saloranta A., Forss H., Walsh T., Nordblad A., Mäkelä M., Worthington H.V. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev. 2017;7 doi: 10.1002/14651858.CD001830.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jaafar N., Ragab H., Abedrahman A., Osman E. Performance of fissure sealants on fully erupted permanent molars with incipient carious lesions: a glass-ionomer-based versus a resin-based sealant. J Dent Res Dent Clin Dent Prospects. 2020;14:61–67. doi: 10.34172/joddd.2020.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Urquhart O., Tampi M.P., Pilcher L., et al. Nonrestorative treatments for caries: systematic review and network meta-analysis. J Dent Res. 2018;98:14–26. doi: 10.1177/0022034518800014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kasemkhun P., Nakornchai S., Phonghanyudh A., Srimaneekarn N. The efficacy of dental sealant used with bonding agent on occlusal caries (ICDAS 2-4): a 24-month randomized clinical trial. Int J Paediatr Dent. 2021;31:760–766. doi: 10.1111/ipd.12758. [DOI] [PubMed] [Google Scholar]
- 94.Muñoz-Sandoval C., Gambetta-Tessini K., Giacaman R.A. Microcavitated (ICDAS 3) carious lesion arrest with resin or glass ionomer sealants in first permanent molars: a randomized controlled trial. J Dent. 2019;88 doi: 10.1016/j.jdent.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 95.Beresescu L., Păcurar M., Bica C.I., et al. The assessment of sealants' effectiveness in arresting non-cavitated caries lesion—a 24-month follow-up. Healthcare. 2022;10:1651. doi: 10.3390/healthcare10091651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kühnisch J., Mansmann U., Heinrich-Weltzien R., Hickel R. Longevity of materials for pit and fissure sealing—results from a meta-analysis. Dent Mater. 2012;28:298–303. doi: 10.1016/j.dental.2011.11.002. [DOI] [PubMed] [Google Scholar]