Abstract
Objective
This study presents a novel odontoid parameter, the odontoid incidence (OI), to examine the correlation between OI on preoperative cervical sagittal radiographs and 2-year clinical outcomes following short-segment anterior cervical discectomy and fusion (ACDF) in patients with cervical spondylotic myelopathy (CSM).
Methods
A retrospective analysis of the clinical data of 87 patients with CSM who underwent ACDF surgery from January 2018 to December 2023 was conducted. The patients were categorized into a larger OI group (44 patients, OI > 12.62°) and a smaller OI group (43 patients, OI ≤ 12.62°) on the basis of the median cervical sagittal OI prior to surgery. The postoperative follow-up duration was 2 years. Cervical sagittal parameters were assessed on lateral cervical spine radiographs both preoperatively and postoperatively. Additionally, the Japanese Orthopedic Association (JOA), neck disability index (NDI), and visual analog scale (VAS) scores were documented for each patient before surgery and at the final 2-year postoperative follow-up.
Results
Compared with those in the preoperative period, the T1 slope, C2‒C7 Cobb angle, sagittal segmental angle (SSA), and C0‒C2 Cobb angle significantly improved in 87 patients with cervical spondylosis (P < 0.05). At the 2-year postoperative follow-up, all patients exhibited significant improvements in JOA, NDI, and VAS scores compared with the preoperative values (P < 0.05). No statistically significant difference was observed in the preoperative or baseline data between the larger OI group and the smaller OI group (P > 0.05); however, a statistically significant difference was noted in the postoperative SSA between the two groups (P < 0.05). A statistically significant difference was observed in the VAS score and NDI score at the final follow-up between the two groups (P < 0.05), as well as in the improvement in the JOA score and VAS score (preoperative score minus the final follow-up score), between the two groups (P < 0.05). The results of the Pearson correlation analysis indicated a negative correlation between the preoperative OI score and the VAS and NDI scores at the final postoperative follow-up (P = 0.012, r = − 0.268) (P = 0.028, r = − 0.236).
Conclusion
In ACDF, the preoperative OI of patients with CSM was negatively correlated with the VAS and NDI scores at the final postoperative follow-up; Larger preoperative OI corresponded to lower VAS and NDI scores at the final follow-up, leading to comparatively improved 2-year clinical outcomes.
Keywords: Odontoid incidence, Anterior cervical discectomy and fusion, Cervical spondylotic myelopathy, Sagittal parameters
Introduction
The prevalence of cervical spondylosis is increasing annually due to population aging and lifestyle alterations [1]. The pathogenesis primarily results from compression of the spinal cord, blood vessels, and nerves by degenerated cervical intervertebral discs, hyperplastic bone, and the ligamentum flavum, leading to various symptoms and signs [2]. Cervical spondylotic myelopathy (CSM) is a prevalent and severe variant of cervical spondylosis and represents the most frequent form of spinal cord injury in adults [3]. It frequently manifests as cervical pain, paresthesia, limb weakness, diminished hand dexterity, and a sensation of cotton in the feet. It may subsequently result in urinary and fecal incontinence, potentially leading to chronic disability, pain, financial strain, and a decline in quality of life [4].
Anterior cervical discectomy and fusion (ACDF) is the standard minimally invasive technique for addressing cervical spondylosis. ACDF has demonstrated substantial improvements in pain and dysfunction in patients with cervical spondylosis, as indicated by improvements in the neck disability index (NDI), Japanese Orthopedic Association (JOA) score, and visual analog scale (VAS) score for pain [5, 6]. Recently, interest in the influence of cervical sagittal alignment on postoperative clinical outcomes in patients undergoing cervical spine surgery has increased [7, 8]. The significance of cervical sagittal balance has been increasingly acknowledged since a study indicated a substantial correlation between sagittal balance and patients' quality of life scores [9]. Cervical sagittal imbalance is a primary contributor to degenerative cervical diseases [10]. Cervical spine parameters are essential for analyzing cervical sagittal alignment, assisting spine specialists in evaluating the clinical symptoms of cervical spondylosis, developing diagnostic and treatment strategies, choosing suitable surgical protocols, and forecasting postoperative clinical outcomes [11, 12]. The cervical sagittal balance parameters that are extensively analyzed include the C0–2 angle (C0–2), C2–C7 cervical lordosis (CL), C2 slope (C2S), T1 slope (T1S), and T1 slope minus cervical lordosis (T1S-CL) [13]. Nonetheless, these parameters are deficient because they are not invariant anatomical metrics, and the measurements may contain substantial inaccuracies. Consequently, identifying new, relatively stable anatomical parameters of the cervical spine is essential for a comprehensive evaluation of cervical alignment [14].
Lee et al. introduced a novel cervical sagittal parameter, the odontoid incidence (OI), an autonomous anatomical metric unaffected by external influences [15]. The OI can be distinctly demonstrated on cervical sagittal X-ray. Moreover, OI is a clinically relevant parameter, which significantly correlated with postoperative health-related quality of life (HRQOL) [16]. This study aimed to determine the correlation between preoperative OI and clinical outcomes in patients with CSM who underwent short-segment ACDF to facilitate the preoperative prediction of postoperative functional recovery.
Materials and methods
Participants
This study included eighty-seven patients with short-segment CSM who underwent ACDF surgery at the First Affiliated Hospital of Guangzhou University of Chinese Medicine from January 2018 to December 2023. The mean postoperative follow-up duration was 2 years. The inclusion criteria were as follows: (1) definitive diagnosis of cervical spondylosis in two or fewer segments; (2) inadequate conservative treatment significantly impairing daily activities; and (3) all participants underwent ACDF surgery, utilizing endoprostheses such as the Zero-P, Skyline, and ZEVO anterior cervical spine endoprosthesis systems. The exclusion criteria were as follows: (1) congenital cervical spine deformities; (2) neck trauma or injury; (3) prolonged use of aspirin, polivir, or similar medications; (4) severe comorbidities (e.g cardiovascular, cerebrovascular, pulmonary, or renal diseases) who could not endure surgery; and (5) prior history of cervical spine surgery. The study protocol received approval from the Clinical Trial Review Committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine (NO. K[2020] 104), and written informed consent was obtained from all participants prior to the study. The participants in this study provided consent for the publication of their images.
Surgical procedure
The identical surgeon and their team conducted the operations. The patients were directed to perform tracheal tube pushing training for 1 to 2 d prior to the operation. Following tracheal intubation under general anesthesia, the patients were positioned supine, the head was stabilized, the shoulders were retracted inferiorly, and a transverse incision was executed on the right side of the neck. The skin was incised and subcutaneously excised, bluntly dissected to the anterior intervertebral space with the trachea and esophagus retracted to the left side, while the longissimus cervical muscle and anterior vertebral fascia were separated to expose the anterior longitudinal ligament. The designated intervertebral space was identified with a locator pin and verified with a C-arm machine. The intervertebral space was accessed using a Caspar spreader, the intervertebral disc was excised, the dural sac was explored and decompressed until it resumed its bulging form, the cartilage from the upper and lower endplates was abraded, and bone fragments were implanted into the intervertebral space. The remaining intervertebral gaps were addressed similarly, and the plates were secured with screws The C-arm machine apparatus was utilized once more for fluoroscopy to verify the properpositioning of the plates and screws, followed by washing. Hemostasis was achieved with anelectrosurgical knife, a drainage tube was inserted, and the site was sutured, cleaned, and wrappedwith sterile gauze. Postoperatively, patients were monitored, antibiotics were administered consistently for 24 h, the drainage tube was withdrawn after 1 to 2 d, a neck brace was utilized for 8 to 12 weeks, and functional exercises were conducted based on the patient's condition.
Radiographic analyses and data collection
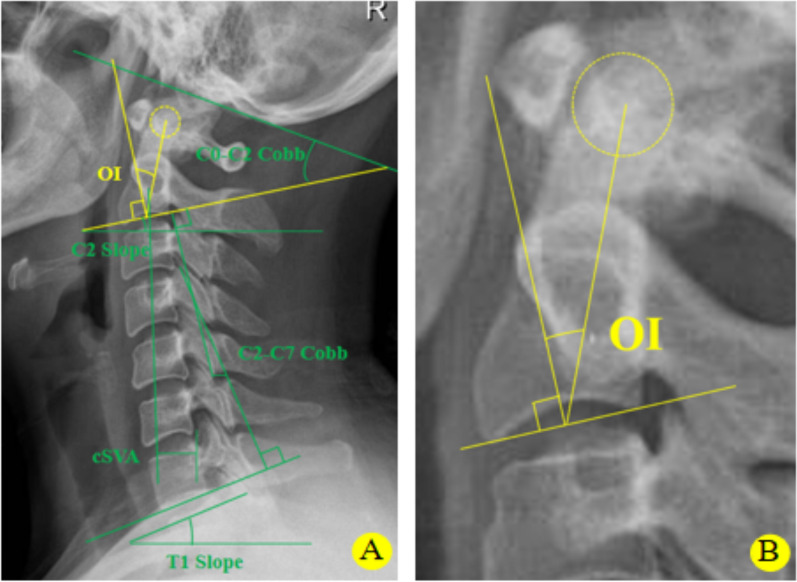
All patients were categorized into two groups according to the median preoperative OI, which served as the critical threshold [17]. Data regarding age, sex, surgical duration and intraoperative hemorrhage were gathered for both cohorts; preoperative and postoperative lateral, hyperextension and hyperflexion X-rays of the cervical spine were obtained. OI was defined as the angle formed between the line that is exactly perpendicular to the midpoint of the C2 endplate and the line that runs from this very point to the center of the odontoid process [15]. The C2-C7 Cobb's angle is defined as the angle between two lines perpendicular to the lower endplates of C2 and C7. The C0‒C2 Cobb angle represents the intersection angle between the McGregor line and the parallel line of the C2 lower endplate. The C2‒C7 sagittal vertical axis measures the horizontal distance from the perpendicular line passing through the geometric center of the C2 (or the odontoid process) to the perpendicular line passing through the posterior superior angle of the C7. The T1 slope is the angle between a horizontal line and a line parallel to the upper endplate of the T1. The C2 slope is the angle between the C2 lower endplate and the horizontal line. The specific measurements of these indices are illustrated in Fig. 1. The anterior convexity angle of the surgical segment was defined as the angle formed between the upper endplate of the superior vertebra and the lower endplate of the inferior vertebra of the surgical segment (SSA), whereas the curvatures of the superior and inferior vertebrae of the surgical segment were recorded in the power position film (upper and lower-SSA-ROMs). The JOA, VAS, and NDI scores were used to evaluate the patients' postoperative results. The JOA, NDI, and VAS scores were assessed preoperatively and at the final follow-up, and the results were evaluated by two senior physicians. Figure 2 depicts a quintessential case follow-up.
Fig. 1.
Measurement of odontoid parameters and cervical spine parameters on cervical spine X-ray sagittal images. A Measurement of the OI and other cervical spine parameters on an X-ray image; B High-resolution view of the OI shown on an X-ray image
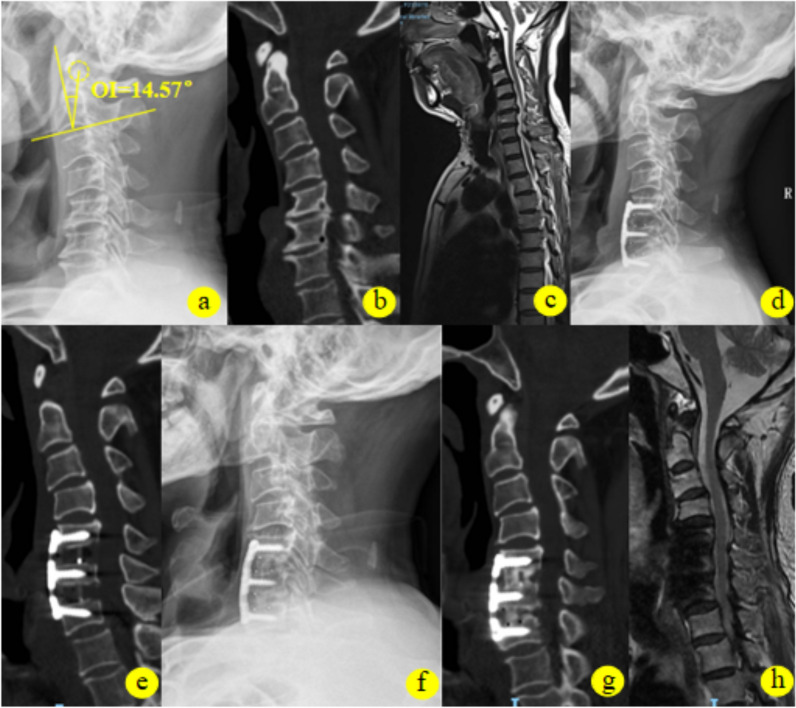
Fig. 2.
Patient presentation: This is a 72-year-old male patient with cervical spondylosis. a–c Preoperative imaging data suggest C5–7 disc herniation with corresponding spinal stenosis. The preoperative OI value was 14.57°, and the patient's main symptom was unsteady walking with numbness in both hands. d, e Immediate postoperative review revealed that the patient underwent C5–7 ACDF surgery, which presented postoperative changes in the cervical spine. f–h Postoperative review 2 years after surgery revealed that C5–7 had been fused, and the corresponding spinal canal did not show any significant narrowing. Walking instability, neck pain and hand numbness significantly improved
Statistical analysis
We conducted the data analysis via SPSS version 21.0. Continuous variables are presented as the means ± standard deviations. Qualitative data were analyzed via the chi-square test. Paired samples t-tests were employed to assess significant differences between preoperative and postoperative parameters. Statistical comparisons of the cervical sagittal parameters and different score types between the two groups were conducted via the independent samples t test. Pearson correlation analysis was used to examine the relationships between preoperative OI and postoperative follow-up scores. P values less than 0.05 were considered statistically significant.
Results
Patient demographics
This study enrolled 87 patients with CSM who underwent ACDF and categorized them into two groups on the basis of the median preoperative OI (12.62°): the larger OI group and the smaller OI group (Table 1). The larger OI group comprised 44 patients with a mean age of 50.68 ± 12.35 years, whereas the smaller OI group included 43 patients with a mean age of 54.88 ± 9.84 years. No statistically significant differences (P > 0.05) were detected between the larger OI group and the smaller OI group in terms of age, sex, duration of surgery, intraoperative bleeding, Range of motion (ROM), mobility of the upper segment of the operated segment (Upper-SSA-ROM), or mobility of the lower segment of the operated segment (Lower-SSA-ROM) (Table 2).
Table 1.
Grouping is based on the median OI
| Parameters (n = 87) | OI |
|---|---|
| Median OI | 12.62 |
| Larger OI (OI > 12.62°) | 16.93 ± 4.13 |
| Smaller OI (OI ≤ 12.62°) | 10.24 ± 1.67 |
Larger OI (OI > 12.62°), smaller OI (OI ≤ 12.62°), larger OI (16.93 ± 4.13), and smaller OI (10.24 ± 1.67°)
Table 2.
Demographic and clinical data for both the larger OI group and the smaller OI group
| Parameters | Larger OI (n = 44) | Smaller OI (n = 43) | P value |
|---|---|---|---|
| Age | 50.68 ± 12.35 | 54.88 ± 9.84 | 0.083 |
| Sex (male/female) | 14/30 | 20/23 | 0.160 |
| Operation time (min) | 124.66 ± 32.13 | 130.65 ± 32.76 | 0.392 |
| Blood loss (mL) | 35.00 ± 33.38 | 39.30 ± 34.67 | 0.557 |
| ROM (°) | 33.48 ± 14.64 | 32.41 ± 18.19 | 0.764 |
| Upper-SSA-ROM (°) | 7.74 ± 5.55 | 8.92 ± 5.76 | 0.332 |
| Lower-SSA-ROM (°) | 8.45 ± 4.24 | 9.12 ± 5.34 | 0.514 |
ROM, cervical spine mobility; ROM, Range of motion; SSA, sagittal segmental angle
Pre- and postoperative imaging results and scores at follow-up for all patients
A comparison of the preoperative and postoperative cervical sagittal parameters of all patients in this study revealed that all the cervical sagittal parameters, with the exception of the cSVA (P = 0.563), significantly improved postoperatively relative to preoperatively (P < 0.05) (Table 3). Additionally, the JOA, VAS, and NDI scores of all patients at the final follow-up were significantly greater (P< 0.05) than those at the preoperative (Table 4). These findings suggest that ACDF surgery effectively improves the physiological curvature of the cervical spine, restores sagittal balance, and significantly alleviates followed-up clinical symptoms in patients.
Table 3.
Comparison of preoperative and postoperative parameters for all patients
| Parameters (n = 87) | Preoperation | Postoperation | P value |
|---|---|---|---|
| T1 slope (°) | 21.51 ± 7.64 | 25.48 ± 7.18 | 0.000 |
| C2–C7 Cobb (°) | 7.42 ± 7.35 | 13.03 ± 8.15 | 0.000 |
| SSA (°) | 5.64 ± 5.25 | 8.75 ± 5.32 | 0.000 |
| C0–C2 Cobb (°) | 31.26 ± 6.92 | 23.84 ± 8.16 | 0.000 |
| cSVA (mm) | 21.33 ± 11.02 | 20.63 ± 10.81 | 0.563 |
| C2 slope (°) | 7.92 ± 4.71 | 10.45 ± 6.07 | 0.001 |
cSVA, cervical sagittal vertical axis; SSA, sagittal segmental angle
Table 4.
Efficacy scores at the final follow-up and preoperative follow-up for all patients
| Parameters (n = 87) | Preoperation | Final follow-up | P value |
|---|---|---|---|
| JOA | 13.25 ± 2.70 | 15.25 ± 1.46 | 0.000 |
| NDI | 21.90 ± 8.02 | 3.86 ± 1.95 | 0.000 |
| VAS | 5.08 ± 1.56 | 1.14 ± 1.11 | 0.000 |
Imaging parameters in the larger OI group and the smaller OI group
Aside from the C2 slope (P < 0.01), no statistically significant differences were observed in the preoperative baseline indicators between the larger OI group and the smaller OI group (P > 0.05). Given that OI = OT + C2 slope, it can be inferred that the preoperative C2 slope of the larger OI group exceeded that of the smaller OI group. A statistically significant difference in postoperative segmental curvature was observed between the two groups (P < 0.05), whereas the remaining postoperative parameters were not statistically significantly different (P> 0.05). Patients exhibiting reduced preoperative OI demonstrated increased postoperative surgical segmental curvature (P = 0.027), indicating that those with lower preoperative OI possess a greater capacity to rectify the physiological curvature of the surgically affected segment (Table 5).
Table 5.
Comparison of preoperative and postoperative parameters between the larger OI group and the smaller OI group
| Parameters | Larger OI (n = 44) | Smaller OI (n = 43) | P value |
|---|---|---|---|
| C2–C7cobb (°) | |||
| Preoperation | 6.29 ± 7.96 | 8.58 ± 6.56 | 0.148 |
| Postoperation | 13.26 ± 8.75 | 12.80 ± 7.58 | 0.795 |
| C0-C2cobb (°) | |||
| Preoperation | 32.28 ± 6.31 | 30.21 ± 7.41 | 0.164 |
| Postoperation | 23.99 ± 8.14 | 23.68 ± 8.27 | 0.858 |
| cSVA (mm) | |||
| Preoperation | 22.34 ± 12.55 | 20.29 ± 9.22 | 0.390 |
| Postoperation | 20.38 ± 11.82 | 20.89 ± 9.80 | 0.827 |
| Tl slope (°) | |||
| Preoperation | 21.70 ± 7.83 | 21.32 ± 7.51 | 0.820 |
| Postoperation | 24.87 ± 8.30 | 26.10 ± 5.85 | 0.425 |
| C2 slope (°) | |||
| Preoperation | 9.73 ± 5.45 | 6.07 ± 2.84 | 0.000 |
| Postoperation | 9.95 ± 6.14 | 10.96 ± 6.02 | 0.441 |
| SSA (°) | |||
| Preoperation | 5.53 ± 5.92 | 5.75 ± 4.54 | 0.850 |
| Postoperation | 7.51 ± 4.55 | 10.02 ± 5.78 | 0.027 |
cSVA, cervical sagittal vertical axis; SSA, sagittal segmental angle
Comparison of scores in the larger OI group and the smaller OI group
No statistically significant differences in preoperative JOA, VAS, or NDI scores were observed between the two groups (P> 0.05). Except for the JOA score (P = 0.149), a statistically significant difference (P < 0.05) was observed in the NDI and VAS scores at the final follow-up between the two groups (Table 6). Compared with the smaller OI group, the larger OI group presented lower NDI and VAS scores at the final follow-up (P < 0.05). A greater preoperative OI was correlated with reduced NDI and VAS scores during final postoperative follow-up and was more likely to enhance final postoperative pain status and axial symptoms. To facilitate a precise comparison and assessment of the clinical efficacy between the two groups during final follow-up, we evaluated the difference between the preoperative and final follow-up scores. The results indicated that the ∆JOA and ∆VAS scores were significantly greater in the larger OI group than in the smaller OI group (P < 0.05) (Table 7), implying that the larger OI group exhibited superior improvement rates in the JOA score and VAS score, thereby enhancing final postoperative spinal cord function and alleviating pain conditions.
Table 6.
Comparison of efficacy scores preoperatively and at the final follow-up between the larger OI group and the smaller OI group
| Score | Larger OI (n = 44) | Smaller OI (n = 43) | P value |
|---|---|---|---|
| JOA | |||
| Preoperation | 12.91 ± 3.14 | 13.60 ± 2.14 | 0.232 |
| Final follow-up | 15.48 ± 1.42 | 15.02 ± 1.49 | 0.149 |
| NDI | |||
| Preoperation | 21.70 ± 8.03 | 22.09 ± 8.10 | 0.823 |
| Final follow-up | 3.25 ± 0.81 | 4.49 ± 2.52 | 0.003 |
| VAS | |||
| Preoperation | 5.25 ± 1.18 | 4.91 ± 1.88 | 0.309 |
| Final follow-up | 0.75 ± 0.92 | 1.53 ± 1.16 | 0.001 |
Table 7.
Comparison of efficacy score improvement values between the larger and smaller OI groups (Preop minus final follow-up)
| Parameters | Larger OI (n = 44) | Smaller OI (n = 43) | P value |
|---|---|---|---|
| ∆JOA | − 2.57 ± 2.95 | − 1.42 ± 2.22 | 0.043 |
| ∆NDI | 18.45 ± 7.91 | 17.60 ± 8.44 | 0.629 |
| ∆VAS | 4.50 ± 1.52 | 3.56 ± 2.28 | 0.026 |
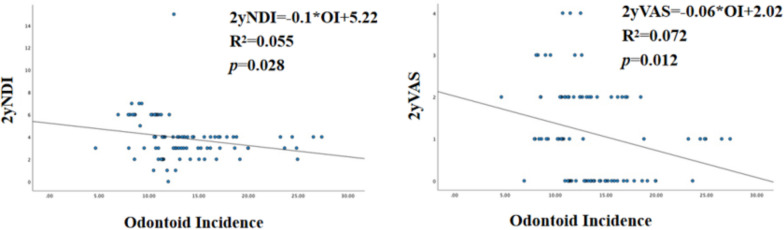
Correlation between preoperative OI and scores
Pearson correlation analysis was performed between the preoperative OI score and the VAS, NDI, and JOA scores at the final follow-up for all patients. The results revealed a negative correlation between preoperative OI and the NDI and VAS scores at the final follow-up (P = 0.012, r = − 0.268), (P = 0.028, r = − 0.236). There was no correlation between the preoperative OI and any other parameter. The above results indicated that the larger the preoperative OI was (Table 8), the smaller the NDI and VAS scores were during 2-year postoperative follow-up. Linear regression analysis also revealed that preoperative OI was correlated with postoperative NDI and VAS scores (Fig. 3).
Table 8.
Correlation analysis between preoperative OI and final follow-up scores
| Parameters (n = 87) | Final follow-up | ||
|---|---|---|---|
| Pre-OI | JOA | NDI | VAS |
| r | 0.119 | − 0.236 | − 0.268 |
| p value | 0.274 | 0.028 | 0.012 |
Fig. 3.
Linear regression analysis between preoperative OI and NDI and VAS scores at the 2-year postoperative follow-up
Complications
Three patients exhibited dysphagia during the immediate postoperative period: one from the larger OI group and two from the smaller OI group, with no statistically significant difference observed between the groups (χ2 = 3.357, P = 0.325). Their severity was moderate, and none of the patients experienced dysphagia at the final follow-up. No instances of adjacent spondylosis, implant failure, cage subsidence, plate or screw loosening, or dislocation were observed in any patient.
Discussion
In recent years, clinical studies concerning cervical sagittal balance have garnered significant attention [18], and research has established a close association between the onset of cervical spondylosis and imbalance in the cervical sagittal sequence. Prior biomechanical research has indicated that the cervical spine exhibits the most extensive sagittal range of motion. The head's center of gravity progressively shifts forward as the cervical curvature develops from normal physiological anterior convexity to the loss of this convexity or even cervical retroversion. Consequently, the moment that the arm in the cervical spine activities relative to the neck's center of rotation increases, leading to heightened compensatory work by the muscles, ligaments, and intervertebral joints in the posterior cervical region. This, in turn, exacerbates degeneration in the cervical spine, particularly in intervertebral joints affected by hyperplasia and other degenerative conditions [19]. ACDF has emerged as a standard procedure for addressing cervical spondylosis, effectively excising the affected disc and adequately decompressing the spinal cord. Various interbody fusion devices, including titanium plates combined with cage internal fixation and the Zero-P fusion system, have been employed in ACDF. These devices can restore the height of the intervertebral space and enhance the physiological curvature of the cervical spine, thereby effectively reinstating the cervical spine's localization and sagittal balance, and their efficacy is widely acknowledged [20]. The findings of this study align with the previous results, indicating that the T1 slope, C2‒C7 Cobb angle, SSA, and C0‒C2 Cobb angle of 87 patients were significantly improved compared with those in the preoperative period (P< 0.05). Additionally, the JOA, VAS, and NDI scores at the 2-year postoperative follow-up were significantly greater than those at the preoperative follow-up (P < 0.05).
Surgical intervention for cervical spondylosis should prioritize not only effective decompression of the spinal nerves in the affected segment but also reconstruction of the local sagittal balance [21]. The frequently utilized clinical parameters for evaluating cervical sagittal balance include the C0‒C2 Cobb angle, C2‒C7 Cobb angle, cSVA, T1S and T1S‒CL, which serve as critical references in the selection of surgical interventions and the evaluation of postoperative cervical sagittal balance [14, 22], however, these parameters have certain limitations. The anatomical alignment parameters of the cervical spine are not assessed in a fixed position. Furthermore, when assessing cervical spine sagittal parameters on radiographs, the cervicothoracic junction is frequently inadequately delineated, and the obscured T1 and C7 vertebrae are difficult to identify, complicating the measurement of conventional sagittal position parameters [23]. Furthermore, T1S and C2S are assessed solely along horizontal lines, which may consequently result in measurement inaccuracies [24]. The identification of novel, independent, and consistent anatomical parameters of the cervical spine is essential for a comprehensive evaluation of cervical alignment and sagittal balance.
Lee et al. studied cervical spine sagittal radiographs from 42 subjects and proposed a new cervical spine sagittal parameter, the OI. The OI adds measurements in the vertical axis direction to those in the horizontal axis direction to analyze the degree of cervical spine alignment in both directions. Unlike C7 and T1, which are sometimes not visible in some patients, the OI is easy to measure on plain cervical radiographs [15]. Notably, the data in the above study were based only on healthy asymptomatic adults, which limits the clinical relevance and utility of the study in patients with cervical spondylosis. In addition, few studies related to odontoid parameters. Many previous studies have reported the relationships between other cervical balance parameters and health-related quality of life (HRQOL) [25]. Nevertheless, these studies have focused mainly on patient prognosis and postoperative cervical alignment, and few studies have systematically evaluated the relationships between preoperative cervical sagittal parameters and cervical symptoms in patients with degenerative cervical spine disease. Therefore, this study investigated the relationships between preoperative cervical sagittal OI parameters and clinical scores at 2-year postoperative follow-up.
The OI, a critical parameter in cervical sagittal balance, is defined as the sum of the angle of inclination of the odontoid process (OT) and the C2 slope (OI = OT + C2S) [15]. The OI is intricately connected to the CL via C2S, significantly influencing various cervical spine disorders and the pathomechanisms underlying cervical spine degeneration [15]. It is essential to investigate the impact of OI on cervical sagittal balance and select surgical approaches to rectify cervical kyphosis. The OT denotes the spatial orientation of the odontoid process, which may rely on the equilibrium of cranial and horizontal vision and aid in assessing cervical alignment and sagittal balance [26]. The use of odontoid parameters facilitates a comprehensive examination of cervical alignment and the compensatory condition of the patient. A biomechanical study confirmed that the extension potential of the upper cervical spine is related to the anatomical characteristics of the odontoid process and that an odontoid process with a greater posterior inclination or a larger OI results in an increased ROM of C1 relative to C2 [27]. The OI, akin to the pelvic angle of incidence (PI), pertains to the compensatory reserve of cervical extension, thereby facilitating an evaluation of the patient's compensatory status and meticulous planning for optimal cervical alignment correction. The OI pertains to the cervical spine anatomy and remains unaffected by external factors [15], whereas additional benefits of the odontoid parameter are continually being investigated and revealed. Lee et al. reported that patients with a higher OI were significantly correlated with enhanced NDI scores (r = − 0.40, P < 0.05) [16]. The findings of the present study revealed a negative correlation between preoperative OI and VAS and NDI scores at the final postoperative follow-up (P = 0.012, r = − 0.268), (P = 0.028, r = − 0.236), indicating that patients with greater preoperative odontoid incidence angles presented lower VAS and NDI scores at the final follow-up. We also discovered that patients with a reduced preoperative OI exhibited, conversely, enhanced postoperative mobility of the operated segment. Our analysis suggested a correlation between the morphology of the odontoid process, which varies among individuals, and the observed cervical alignment inconsistencies. Specifically, when the odontoid axis—defined as the line extending from the midpoint of the inferior endplate of C2 to the center of the odontoid process—tilts anteriorly beyond the vertical axis, it indicates a misalignment in the cervical spine. Furthermore, the spatial orientation of the odontoid process significantly influences the overall alignment of the cervical spine [16], subsequently impacting postoperative segmental mobility.
This study has certain limitations. This was a retrospective study, and minor variations in the positioning of radiographs obtained from the patients may have resulted in selection bias. Second, the sample size was limited, and we could not conduct a retrospective analysis of the imaging parameters at the final follow-up. Our study revealed that the internal fixation devices utilized for patients who underwent ACDF surgery were inconsistent and included both Zero-P plates and conventional plates. Potential confounders may have influenced the correlation between preoperative OI and postoperative follow-up scores, undermining the validity of the results. Consequently, the findings of this study must be regarded with prudence.
Conclusion
In summary, ACDF is a traditional minimally invasive cervical spine procedure that effectively alleviates symptoms of spinal cord compression and preserves the sagittal alignment of the cervical spine in patients with CSM. The preoperative OI of patients with spinal cervical spondylosis was negatively correlated with the VAS and NDI scores at the final postoperative follow-up. These findings indicate that a larger preoperative OI is correlated with smaller VAS and NDI scores at the final follow-up, leading to improved final clinical outcomes while also serving as an effective preoperative predictor of postoperative functional recovery.
Acknowledgements
We would like to thank all the medical and nursing staff of the Department of Spine and Orthopedics, The First Affiliated Hospital of Guangzhou University of Chinese Medicine.
Abbreviations
- OI
Odontoid incidence
- ACDF
Anterior cervical discectomy and fusion
- JOA
Japanese Orthopedic Association
- NDI
Neck Disability Index
- VAS
Visual Analogue Scale
- SSA
Sagittal Segmental Angle
- SVA
Sagittal Vertical Axis
- CSM
Cervical spondylotic myelopathy
- HRQOL
Health-related quality of life
- OT
Odontoid tilt
- T1S
T1 slope
- C2S
C2 slope
- PI
Pelvic angle of incidence
- ROM
Range of motion
Author contributions
All the authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by YG, HL, YG, JH, ZZ, HZ, and YL, and the research design was performed by ZC, DL, HR and XJ. The first draft of the manuscript was written by YG, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The data used to support the findings of this study are included within the article.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Clinical Trial Review Committee of the First Affiliated Hospital of Guangzhou University of Chinese Medicine (No. K [2020] 104).
Consent for publication
The authors affirm that the human research participants provided informed consent for the publication of the images in Figs. 1 and 2.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yan Gong, Hao Liu and Yanchi Gan have contributed equally to this work.
Contributor Information
Xiaobing Jiang, Email: spinedrjxb@sina.com.
Zhaojun Cheng, Email: czjspine@163.com.
References
- 1.Theodore N. Degenerative cervical spondylosis. N Engl J Med. 2020;383(2):159–68. 10.1056/NEJMra2003558. [DOI] [PubMed] [Google Scholar]
- 2.Takagi I, Eliyas JK, Stadlan N. Cervical spondylosis: an update on pathophysiology, clinical manifestation, and management strategies. Dis Mon. 2011;57(10):583–91. 10.1016/j.disamonth.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Williams J, D’Amore P, Redlich N, et al. Degenerative cervical myelopathy: evaluation and management. Orthop Clin N Am. 2022;53(4):509–21. 10.1016/j.ocl.2022.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Corey DL, Comeau D. Cervical radiculopathy. Med Clin N Am. 2014;98(4):791–xii. 10.1016/j.mcna.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Kapetanakis S, Thomaidis T, Charitoudis G, Pavlidis P, Theodosiadis P, Gkasdaris G. Single anterior cervical discectomy and fusion (ACDF) using self- locking stand-alone polyetheretherketone (PEEK) cage: evaluation of pain and health-related quality of life. J Spine Surg. 2017;3(3):312–22. 10.21037/jss.2017.06.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spanos SL, Siasios ID, Dimopoulos VG, et al. Correlation of clinical and radiological outcome after anterior cervical discectomy and fusion with a polyetheretherketone cage. J Clin Med Res. 2018;10(3):268–76. 10.14740/jocmr3326w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iyer S, Nemani VM, Nguyen J, et al. Impact of cervical sagittal alignment parameters on neck disability. Spine. 2016;41(5):371–7. 10.1097/BRS.0000000000001221. [DOI] [PubMed] [Google Scholar]
- 8.Villavicencio AT, Babuska JM, Ashton A, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery. 2011;68(5):1309–16. 10.1227/NEU.0b013e31820b51f3. [DOI] [PubMed] [Google Scholar]
- 9.Zhou S, Li W, Su T, et al. Does lumbar lordosis minus thoracic kyphosis predict the clinical outcome of patients with adult degenerative scoliosis? J Orthop Surg Res. 2019;14(1):290. 10.1186/s13018-019-1339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu S, Lafage R, Smith JS, et al. Impact of dynamic alignment, motion, and center of rotation on myelopathy grade and regional disability in cervical spondylotic myelopathy. J Neurosurg Spine. 2015;23(6):690–700. 10.3171/2015.2.SPINE14414. [DOI] [PubMed] [Google Scholar]
- 11.Heidt ST, Louie PK, Khan JM, et al. Comparing allografts to autografts for maintenance of cervical sagittal parameters and clinical outcomes following anterior cervical discectomy and fusion with anterior cervical plating. Neurospine. 2019;16(3):618–25. 10.14245/ns.1836202.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ling FP, Chevillotte T, Leglise A, Thompson W, Bouthors C, Le Huec JC. Which parameters are relevant in sagittal balance analysis of the cervical spine? A literature review. Eur Spine J. 2018;27(Suppl 1):8–15. 10.1007/s00586-018-5462-y. [DOI] [PubMed] [Google Scholar]
- 13.Xu S, Liang Y, Yu G, Zhu Z, Wang K, Liu H. Exploration on sagittal alignment and clinical outcomes after consecutive three-level hybrid surgery and anterior cervical discectomy and fusion: a minimum of a 5-year follow-up. J Orthop Surg Res. 2020;15(1):79. 10.1186/s13018-020-01589-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qin H, Chen W, Huang L, Xiao X, Yang Q, Jiang H. The significance of odontoid incidence in patients with cervical spondylotic myelopathy. Glob Spine J. 2023. 10.1177/21925682231182342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee JK, Hyun SJ, Kim KJ. Odontoid incidence: a novel cervical parameter influencing cervical alignment from top to bottom. Neurospine. 2022;19(2):463–71. 10.14245/ns.2244220.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JK, Hyun SJ, Yang SH, Kim KJ. Clinical impact and correlations of odontoid parameters following multilevel posterior cervical fusion surgery. Neurospine. 2022;19(4):912–20. 10.14245/ns.2244604.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine. 2013;38(16):E992–7. 10.1097/BRS.0b013e3182972e1b. [DOI] [PubMed] [Google Scholar]
- 18.Lin T, Wang Z, Chen G, Liu W. Is cervical sagittal balance related to the progression of patients with cervical spondylotic myelopathy? World Neurosurg. 2020;137:e52–67. 10.1016/j.wneu.2019.12.148. [DOI] [PubMed] [Google Scholar]
- 19.Reddy RS, Tedla JS, Dixit S, Abohashrh M. Cervical proprioception and its relationship with neck pain intensity in subjects with cervical spondylosis. BMC Musculoskelet Disord. 2019;20(1):447. 10.1186/s12891-019-2846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu Z, Rao H, Zhang L, Li G, Xu Z, Xu W. Anterior cervical discectomy and fusion versus hybrid decompression and fusion for the treatment of 3-level cervical spondylotic myelopathy: a comparative analysis of cervical sagittal balance and outcomes. World Neurosurg. 2019;132:e752–8. 10.1016/j.wneu.2019.08.022. [DOI] [PubMed] [Google Scholar]
- 21.Yang X, Bartels RHMA, Donk R, Arts MP, Goedmakers CMW, Vleggeert-Lankamp CLA. The association of cervical sagittal alignment with adjacent segment degeneration. Eur Spine J. 2020;29(11):2655–64. 10.1007/s00586-019-06157-0. [DOI] [PubMed] [Google Scholar]
- 22.Park MS, Moon SH, Lee HM, et al. The effect of age on cervical sagittal alignment: normative data on 100 asymptomatic subjects. Spine. 2013;38(8):E458–63. 10.1097/BRS.0b013e31828802c2. [DOI] [PubMed] [Google Scholar]
- 23.Singhatanadgige W, Kang DG, Luksanapruksa P, Peters C, Riew KD. Correlation and reliability of cervical sagittal alignment parameters between lateral cervical radiograph and lateral whole-body EOS stereoradiograph. Glob Spine J. 2016;6(6):548–54. 10.1055/s-0035-1569462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine [published correction appears in Eur Spine J. 2019 Nov;28(11):2631. 10.1007/s00586-019-06128-5]. Eur Spine J. 2019;28(9):1889–1905. 10.1007/s00586-019-06083-1 [DOI] [PubMed]
- 25.Du Y, Chen W, Xu H, et al. Variation of odontoid incidence according to age in asymptomatic children. World Neurosurg. Published online July 30, 2024. 10.1016/j.wneu.2024.07.162 [DOI] [PubMed]
- 26.Machino M, Yukawa Y, Imagama S, et al. Age-related and degenerative changes in the osseous anatomy, alignment, and range of motion of the cervical spine: a comparative study of radiographic data from 1016 patients with cervical spondylotic myelopathy and 1230 asymptomatic subjects. Spine. 2016;41(6):476–82. 10.1097/BRS.0000000000001237. [DOI] [PubMed] [Google Scholar]
- 27.Werne S. Spontaneous atlas dislocation. Acta Orthop Scand. 1955;25(1):32–43. 10.3109/17453675508998922. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.