Abstract
This study aims to evaluate the efficacy of selective laser trabeculoplasty in improving the intraocular pressure in patients diagnosed with open-angle glaucoma. A comprehensive search was performed across electronic databases, including PubMed, Scopus, and Web of Science, until June 2024, using keywords related to “selective laser trabeculoplasty” and “open-angle glaucoma.” Studies were chosen based on set eligibility criteria. Data extraction was carried out by two independent reviewers, and statistical analyses were performed using a random-effects model to calculate the pooled mean differences in IOP reduction and overall success rates. The initial search yielded 3111 articles, with 23 studies included in the systematic review and 22 in the meta-analysis. The pooled MD in IOP reduction between the SLT and control groups was -1.44 mm Hg (95% CI: -2.19 to -0.70, p <0.01). Subgroup analyses revealed a MD of -0.76 mm Hg (95% CI: -1.31 to -0.21, p <0.01) when comparing SLT to medication, and -0.42 mm Hg (95% CI: -0.64 to -0.19, p <0.01) when comparing 180-degree SLT to 360-degree SLT. The pooled success rate favored SLT with an odds ratio (OR) of 0.71 (95% CI: 0.51 to 0.99, p=0.05). There was significant heterogeneity among the studies (I²=71%). SLT is effective in lowering IOP in OAG patients, demonstrating significant efficacy compared to medication and different SLT protocols. The findings underscore SLT’s potential as a reliable treatment option. However, the observed heterogeneity underscores the necessity for standardized protocols in future research to improve comparability and verify SLT’s long-term effectiveness.
Key Words: open-angle glaucoma, selective laser trabeculoplasty, intraocular pressure, meta-analysis, laser trabeculoplasty, glaucoma treatment
Open-Angle Glaucoma (OAG) is one of the most common forms of glaucoma, leading to irreversible blindness globally by affecting millions of individuals. This condition is marked by progressive optic neuropathy, resulting in the degeneration of retinal ganglion cells and subsequent visual field loss.1,2 Elevated Intraocular Pressure (IOP) is the main risk factor for OAG progression, necessitating effective management strategies to prevent further optic nerve damage. Conventional treatments primarily involve topical IOP-lowering medications, which, although effective, come with challenges such as patient adherence, systemic side effects, and financial costs.3,4
Laser trabeculoplasty has become an essential intervention in OAG management, providing an alternative or complement to medication. ALT was initially the standard laser treatment but had significant complications, including thermal damage to the Trabecular Meshwork (TM) and IOP spikes.5,6 To address these issues, Selective Laser Trabeculoplasty (SLT) was introduced in the mid-1990s. SLT targets pigmented TM cells with a lower-energy laser, minimizing collateral damage and offering a safer profile while effectively lowering IOP. However, the recurrence of elevated IOP and the necessity for retreatment remain significant challenges in the long-term management of OAG.7,8 Recent advancements in laser technology have positioned SLT as a promising method with fewer side effects and similar efficacy to traditional approaches. SLT employs a frequency-doubled, Q-switched Nd laser to deliver precise energy bursts that selectively target pigmented cells in the trabecular meshwork, enhancing aqueous humor outflow without causing substantial thermal damage.9,10 This technique has proven effective in lowering IOP and is particularly beneficial for patients who find it difficult to adhere to pharmacological treatments. Despite the increasing use of SLT, comprehensive assessments of its long-term efficacy and safety across various patient populations are needed. This systematic review and meta-analysis aim to consolidate existing evidence on SLT’s role in treating OAG, comparing its outcomes to other treatment modalities to provide a clearer understanding of its clinical utility.
Materials and Methods
The present study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline.11
Systematic search
A comprehensive search was performed across Web of Science, Scopus, and PubMed, covering all available records up to June 2024. We used relevant Medical Subject Headings (MeSH) and relevant keywords, specifically targeting (“selective laser trabeculoplasty” OR “SLT”) AND (“open-angle glaucoma” OR “OAG”).
Inclusion and eligibility
The eligibility criteria was defined based on the PICO framework: Population (P): Clinical studies on human patients diagnosed with OAG. Intervention (I): SLT. Comparison (C): Medication, argon laser therapy, and 180 vs. 360-degree SLT. Outcome (O): IOP reduction and success rate of SLT. The exclusion criteria were defined as: animal studies, case reports, studies on other types of glaucoma, studies not involving SLT, unclear or undefined SLT protocols, absence of clear clinical outcomes, lack of sufficient data, and histologic and in vitro studies.
Data extraction and outcome measures
Data was extracted independently by two authors using a standardized data collection sheet. Any disagreements were resolved and discussed with a third author. The collected variables included: Authors’ names, publication year, design, size, demographics (age, gender), SLT protocols (including laser settings and treatment parameters), Follow-up periods, Mean and standard deviation of IOP measurements, Success rates, Comparison groups (medication, argon laser therapy, 180 vs. 360-degree SLT).
Statistical analysis and data synthesis
The pooled Mean Differences (MD) in IOP reduction between SLT and control groups was calculated using a random-effects model, with Hedges’ g and standard deviation estimation. The pooled success rate and Odds Ratio (OR) were determined using the meta package in R. we used the I² test to evaluate the heterogeneity. The Mantel-Haenszel method and random-effects model were applied for pooling effect sizes and calculating standard deviations. A z-test was conducted to evaluate the overall significance of the random model and the significance between subgroups. Publication bias was assessed by creating funnel plots for each group. Statistical analyses and the creation of forest and funnel plots were performed using R (R Foundation for Statistical Computing, Vienna, Austria) and RStudio (RStudio Inc., Boston, MA).
Results
Our initial search yielded 3,111 articles from PubMed, Scopus, and Web of Science, from which we eliminated 338 duplicates. After reviewing the titles and abstracts of the remaining 2,493 records, we retrieved 94 full-text articles for further evaluation. Ultimately, 23 studies met our eligibility criteria and were included in the systematic review,3,9,12-32 with 22 of these studies also included in the meta-analysis (Figure 1). Detailed characteristics of the included studies are summarized in Table 1.
The main focus of the included studies was to evaluate the effectiveness of SLT in lowering IOP in patients with open-angle glaucoma. The studies made several comparisons: SLT versus medication, SLT versus argon laser trabeculoplasty, and 180-degree SLT versus 360-degree SLT. Variations in laser settings and treatment protocols among the studies contributed to the heterogeneity of the outcomes.
Pooled mean difference
The pooled MD in IOP reduction between the SLT and control groups was assessed using a random-effects model. The overall MD was -1.44 mm Hg (95% CI: -2.19 to -0.70, p <0.01), demonstrating a significant decrease in IOP in the SLT groups compared to the control groups (Figures 2 and 3). There was considerable heterogeneity among the studies (I²=71%, τ²=0.6742, p <0.01).
Figure 1.

PRISMA flow diagram of the included studies.
Further subgroup analysis revealed varying MDs: For SLT versus medication, the MD was -0.76 mm Hg (95% CI: -1.31 to -0.21, p <0.01), indicating a statistically significant IOP reduction. For SLT versus ALT, the MD was -1.30 mm Hg (95% CI: -3.77 to 1.17, p=0.14), which was not statistically significant. For 180-degree SLT versus 360-degree SLT, the MD was -0.42 mm Hg (95% CI: -0.64 to -0.19, p <0.01), also showing a statistically significant reduction in IOP.
Pooled success rate
The overall success rate of SLT was evaluated, and the pooled odds ratio (OR) was calculated. The random-effects model indicated an OR of 0.71 (95% CI: 0.51 to 0.99, p=0.05), signifying a statistically significant higher success rate for SLT compared to control treatments (Figures 4 and 5). Significant heterogeneity was observed among the studies (I²=73%, τ²=0.3277, p <0.01). Subgroup analyses provided the following ORs.
For SLT versus medication, the OR was 1.46 (95% CI: 0.88 to 2.40, p=0.14), which was not statistically significant. For SLT versus ALT, the OR was 1.34 (95% CI: 0.73 to 2.45, p=0.33), also not statistically significant. For 180-degree SLT versus 360-degree SLT, the OR was 0.56 (95% CI: 0.20 to 2.51, p=0.43), which was not statistically significant.
Table 1.
Detailed characteristics of the included studies.
| Author | Year | Country | Design | Eyes | FD | Age | M/F | Comparison | Control |
|---|---|---|---|---|---|---|---|---|---|
| Lai et al.20 | 2004 | China | RCT | 58 | 60 | 51.9 | 13/16 | SLT vs M | Various |
| Nagar et al.25 | 2004 | UK | RCT | 167 | 10.3 | 63 | 77/90 | SLT vs M | Latanoprost |
| Nagar et al.21 | 2008 | UK | RCT | 40 | 4-6 | 66.4 | 21/19 | SLT vs M | Latanoprost |
| Goyal et al.15 | 2009 | UK | RCT | 37 | 1 | 57-67 | - | 180 vs 360 | 360 as control |
| Prasad et al.3 | 2009 | USA | ROS | 41 | 1-24 | 65 | 18/23 | 180 vs 360 | 360 as control |
| Bovell et al.23 | 2011 | Canada | RCT | 176 | 36-50 | 69.5 | 72/104 | SLT vs ALT | ALT as control |
| Katz et al.31 | 2012 | USA | RCT | 127 | 9-12 | - | 28/41 | SLT vs M | Various |
| Rosenfeld et al.18 | 2012 | Israel | RCT | 52 | 12 | 71.9 | 25/27 | SLT vs ALT | ALT as control |
| Shibata et al.12 | 2012 | Japan | ROS | 69 | 17.9-19.5 | 66.4-70.2 | 35/34 | 180 vs 360 | 360 as control |
| Kent et al.26 | 2015 | Canada | RCT | 76 | 6 | 73 | - | SLT vs ALT | ALT as control |
| Kaplowitz et al.27 | 2016 | USA | RCT | - | 24 | 62.8-70.3 | 13/24 | SLT vs TLT | TLT as control |
| Gazzard et al.30 | 2019 | UK | RCT | 1230 | 36 | 62.7-63.4 | 397/321 | SLT vs M | Various |
| Ozen et al.14 | 2020 | Turkey | POS | 52 | 6 | 62.3 | 28/24 | 180 vs 360 | 360 as control |
| Nirappel et al.16 | 2021 | USA | RCS | 258 | 1.5-24 | 18-97 | 215/238 | 180 vs 360 | 360 as control |
| Philippin et al.29 | 2021 | Tanzania | RCT | 339 | 12 | 65.09 | 118/83 | SLT vs M | Timolol |
| Wong et al.17 | 2021 | Hong Kong | RCT | 132 | 12 | - | - | SLT vs PS-SLT | SLT as control |
| Christie et al.24 | 2023 | Denmark | RCT | 144 | 12 | 60 | 77/67 | SLT vs M | Bimatoprost as control |
| Dahlgren et al. (i)9 | 2023 | Sweden | RCT | 199 | 6 | 70-73 | - | 180 vs 360 | 360 as control |
| Dahlgren et al. (ii)9 | 2023 | Sweden | RCT | 201 | 6 | 70-73 | - | 180 vs 360 | 360 as control |
| Michaelov et al.28 | 2022 | Australia | RCT | 80 | 12 | 66.5 | - | 180 vs 360 | 360 as control |
| Pimentel et al.32 | 2023 | Brazil | ROS | 98 | 12 | 61.-62.7 | 42/56 | SLT vs MLT | MLT as control |
| Robin et al.13 | 2023 | USA | RCS | 131 | 6-12 | 65.2 | 63/68 | SLT vs MLT | MLT as control |
| Schmidl et al.19 | 2023 | Austria | RCCS | 25 | 3 | 72-73 | 16-Sep | SLT vs ALT | ALT as control |
| Martini et al.22 | 2024 | France | ROS | 73 | 12 | 77.7 | 29/44 | SLT vs M | iStent as control |
Potential publication bias was assessed through funnel plots for the included studies. The observed asymmetry in the funnel plots suggests the presence of publication bias, which may affect the reliability of the pooled estimates.
Discussion
We aimed at evaluating the efficacy of SLT in improving IOP in patients with OAG. We analyzed multiple studies that compared SLT with other treatments, including medication, ALT, and varying SLT protocols (180-degree versus 360-degree). Our findings indicated that SLT significantly reduces IOP, with an overall MDof -1.44 mm Hg (95% CI: -2.19 to -0.70, p <0.01) compared to control groups. Subgroup analyses showed a statistically significant IOP reduction for SLT versus medication and for 180-degree versus 360-degree SLT. However, the comparison between SLT and ALT did not reach statistical significance. Furthermore, the pooled success rate demonstrated a higher success rate for SLT relative to control treatments, despite substantial heterogeneity among the included studies.
A prospective randomized clinical trial compared the effectiveness of SLT and ALT in pseudophakic glaucoma patients. Over a 12-month period, the study observed no significant differences in IOP-lowering effects between SLT and ALT. At the final checkup, the mean IOP reduction was 3.23 mm Hg for ALT and 4.30 mm Hg for SLT, supporting our findings that SLT effectively reduces IOP.9,28,30 However, unlike our meta-analysis, which found a statistically significant IOP reduction with SLT compared to controls, Rosenfeld et al. did not find a significant difference between SLT and ALT. This suggests that while SLT is effective, its relative advantage over ALT may vary based on patient populations and study designs.9,28,30,33,34
A randomized controlled trial compared the efficacy of 180-degree and 360-degree SLT in patients with OAG and glaucoma suspects. The results indicated that 360-degree SLT was more effective in lowering IOP, with reductions of 21.5 mm Hg for 180-degree SLT and 19.9 mm Hg for 360-degree SLT at a 1-year follow-up. This finding is in line with our subgroup analysis, which also demonstrated a statistically significant greater IOP reduction with 360-degree SLT compared to 180-degree SLT. Gazzard et al. conducted two studies on the efficacy of SLT for OAG treatment. In their 2019 study, they found that SLT was as effective as medication in reducing IOP over a 3-year period.3,18 Their 2023 study further confirmed these results, showing sustained IOP reduction with SLT over an extended follow-up period. These findings are consistent with our meta-analysis, which showed a MD in IOP reduction of -0.76 mm Hg (95% CI: -1.31 to -0.21, p <0.01) for SLT compared to medication. The agreement across various studies underscores the reliability of SLT as a treatment option for OAG, particularly for patients who struggle with medication adherence.9,28,30 When comparing our results to previous meta-analyses, we observe both similarities and differences. One comprehensive network meta-analysis evaluated the effectiveness of various laser trabeculoplasty techniques, including SLT and ALT, for treating OAG. This study found no statistically significant differences in IOP reduction between any pairs of interventions, consistent with our finding of no significant difference between SLT and ALT (MD -1.30 mm Hg, 95% CI: -3.77 to 1.17, p=0.14). However, the study reported that 180-degree SLT significantly reduced medication use compared to ALT at 12 months (MD -0.28, 95% CI: -0.50 to -0.06, p=0.014), which aligns with our subgroup analysis findings.35-38
Figure 2.

The pooled mean difference between SLT and alternative treatments.
Figure 3.
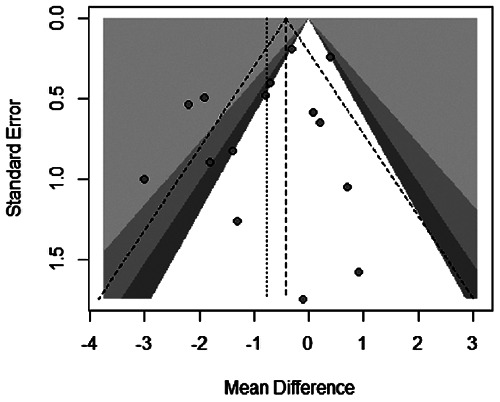
Funnel plot of the mean difference between SLT and alternative treatments.
Figure 4.

Forest plot of the succus rate and ORs between SLT and alternative treatments.
Figure 5.

Funnel plot of ORs between SLT and alternative treatments.
Another study by Sun et al. similarly supported the equivalence of SLT to medication in terms of IOP reduction. This consistency is demonstrated in our findings, where SLT versus medication showed a statistically significant IOP reduction (MD -0.76 mm Hg, 95%CI: -1.31 to -0.21, p <0.01). They also explored the efficacy of newer laser technologies, such as MLT and PSLT, which were not specifically addressed in our analysis. Their results suggested these newer forms of LT are comparable in effectiveness to traditional SLT, indicating potential alternatives for clinical practice. Both studies underscored significant heterogeneity among included studies, a factor also noted in our systematic review (I²=71%). This variability can be attributed to differences in study designs, patient populations, laser settings, and follow-up durations. The two studies emphasized the need for standardized protocols in future research to minimize heterogeneity and enhance comparability. The consistency of findings across our study and these meta-analyses confirms SLT’s role as a reliable and effective treatment for OAG, while highlighting areas for further investigation, particularly regarding the long-term efficacy and optimal treatment parameters of newer LT techniques.35,36,39-41
The inclusion of multiple subgroup analyses allowed for a detailed understanding of SLT’s relative efficacy against various treatments and protocols. However, the study also had limitations, such as the significant heterogeneity. It can be explained by the variability of study designs, sample size, laser settings, and follow-up durations. Additionally, potential publication bias, as suggested by asymmetry in funnel plots, may have influenced the robustness of the pooled estimates. Future research should aim to standardize study protocols and address potential biases to further validate SLT’s efficacy.
Conclusions
Our systematic review and meta-analysis study aimed at evaluating the effectiveness of laser trabeculoplasty in the treatment of glaucoma. Based on our results, SLT is leads to reliable treatment outcomes reducing IOP among those with OAG. SLT demonstrates significant IOP reduction compared to control treatments, with 360-degree SLT showing greater efficacy than 180-degree SLT. These findings are consistent with individual studies and other metaanalyses, reinforcing SLT’s role as a reliable treatment option. However, the significant heterogeneity among studies highlights the need for standardized protocols in future research. Despite these limitations, our study supports the use of SLT in managing OAG.
Acknowledgement
We would like to extend our sincere thanks to Dr. Baseer Khan, MD, Ophthalmologist, FRCS(C), and the team at Clarity Eye Institute, Vaughan, ON, Canada, for their invaluable support and contributions to this study.
List of abbreviations
- IOP
Elevated Intraocular Pressure
- SLT
selective laser trabeculoplasty
- OAG
Open-Angle Glaucoma
- TM
Trabecular Meshwork
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- MD
Mean Differences
- OR
Odds Ratio
Footnotes
The authors declare no potential conflict of interest, and all authors confirm accuracy.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
- 1.Tawfique K, Khademi P, Quérat L, Khadamy JChen EP. Comparison between 90-degree and 360-degree selective laser trabeculoplasty (SLT): A 2-year follow-up. Acta Ophthalmologica 2019;97:427-9. [DOI] [PubMed] [Google Scholar]
- 2.Ayala M, Chen E. Comparison of selective laser trabe-culoplasty (SLT) in primary open angle glaucoma and pseudoexfoliation glaucoma. Clin Ophthalmol 2011;5: 1469-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasad N, Murthy S, Dagianis JJ, Latina MA. A comparison of the intervisit intraocular pressure fluctuation after 180 and 360 degrees of selective laser trabeculo-plasty (SLT) as a primary therapy in primary open angle glaucoma and ocular hypertension. J Glaucoma 2009;18:157-60. [DOI] [PubMed] [Google Scholar]
- 4.Ong K, Ong L, Ong LB. Corneal endothelial abnormalities after selective laser trabeculoplasty (SLT). J Glaucoma 2015;24:286-90. [DOI] [PubMed] [Google Scholar]
- 5.Mucciolo JT, Frenkel REP. The effect of selective laser trabeculoplasty (SLT) in open angle glaucoma patients with previous 360 degree argon laser trabeculoplasty (ALT) treatment. Investigative Ophthalmol Visual Sci 2003;44:U375-U. [Google Scholar]
- 6.Klamann MK, Gonnermann J, Maier AK, et al. Influence of Selective Laser Trabeculoplasty (SLT) on combined clear cornea phacoemulsification and Trabectome outcomes. Graefes Arch Clin Exp Ophthalmol 2014;252:627-31. [DOI] [PubMed] [Google Scholar]
- 7.Maier AKB, Arani P, Pahlitzsch M, et al. Influence of Selective Laser Trabeculoplasty (SLT) on the iStent inject® outcomes. BMC Ophthalmol 2020;20:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayala M. Intraocular pressure reduction after initial failure of selective laser trabeculoplasty (SLT). Graefes Arch Clin Experimental Ophthalmol 2014;252:315-20. [DOI] [PubMed] [Google Scholar]
- 9.Dahlgren T, Ayala M, Zetterberg M. Optimal Performance of Selective Laser Trabeculoplasty: Results from the Swedish Optimal SLT Multicenter Randomized Controlled Trial. Ophthalmol Glaucoma 2023;7:105-15. [DOI] [PubMed] [Google Scholar]
- 10.Lee JW, Wong MO, Liu CC, Lai JS. Optimal selective laser trabeculoplasty energy for maximal intraocular pressure reduction in open-angle glaucoma. J Glaucoma 2015;24:e128-31. [DOI] [PubMed] [Google Scholar]
- 11.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shibata M, Sugiyama T, Ishida O, et al. Clinical results of selective laser trabeculoplasty in open-angle glaucoma in Japanese eyes: comparison of 180 degree with 360 degree SLT. J Glaucoma 2012;21:17-21. [DOI] [PubMed] [Google Scholar]
- 13.Robin AZ, Syar P, Darwish D, et al. Comparison of success rate and intraocular pressure spikes between selective laser trabeculoplasty and micropulse laser trabeculoplasty in African American and Hispanic patients. Int J Ophthalmol 2023;16:75-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Özen B, Öztürk H, Yüce B. Comparison of the effects of 180° and 360° applications of selective laser trabeculoplasty on intraocular pressure and cornea. Int Ophthalmol 2020;40:1103-10. [DOI] [PubMed] [Google Scholar]
- 15.Goyal S, Beltran-Agullo L, Rashid S, et al. Effect of primary selective laser trabeculoplasty on tonographic outflow facility: a randomised clinical trial. Br J Ophthalmol 2010;94:1443-7. [DOI] [PubMed] [Google Scholar]
- 16.Nirappel A, Klug E, Ye R, et al. Effectiveness of selective laser trabeculoplasty applied to 360° vs. 180° of the angle. J Ophthalmol 2021;2021:8860601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong MOM, Lai ISW, Chan PP, et al. Efficacy and safety of selective laser trabeculoplasty and pattern scanning laser trabeculoplasty: a randomised clinical trial. Br J Ophthalmol 2021;105:514. [DOI] [PubMed] [Google Scholar]
- 18.Rosenfeld E, Shemesh G, Kurtz S. The efficacy of selective laser trabeculoplasty versus argon laser trabeculoplasty in pseudophakic glaucoma patients. Clinical Ophthalmol 2012:1935-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schmidl D, Hommer N, Hommer A. An exploratory retrospective data analysis comparing the outcomes of selective laser trabeculoplasty and argon laser trabeculoplasty in patients with open-angle glaucoma or ocular hypertension in Vienna, Austria, from the year 2012 to 2022. Medicina (Kaunas) 2023;59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai JS, Chua JK, Tham CC, Lam DS. Five-year follow up of selective laser trabeculoplasty in Chinese eyes. Clin Experimental Ophthalmol 2004;32:368-72. [DOI] [PubMed] [Google Scholar]
- 21.Nagar M, Luhishi E, Shah N. Intraocular pressure control and fluctuation: the effect of treatment with selective laser trabeculoplasty. Br J Ophthalmol 2009; 93:497. [DOI] [PubMed] [Google Scholar]
- 22.Martini K, Baillif S, Nahon-Esteve S, et al. Intraoperative iStent versus postoperative selective laser trabeculoplasty in early glaucoma patients undergoing cataract surgery: A retrospective comparative study. J Francais D Ophtalmol 2024;47. [DOI] [PubMed] [Google Scholar]
- 23.Bovell AM, Damji KF, Hodge WG, et al. Long term effects on the lowering of intraocular pressure: selective laser or argon laser trabeculoplasty? Can J Ophthalmol 2011;46:408-13. [DOI] [PubMed] [Google Scholar]
- 24.Christie WC, Basha MM, Ho QC, et al. Phase 3, randomized study comparing intracameral bimatoprost implant 15 μg and selective laser trabeculectomy in patients with open-angle glaucoma or ocular hypertension. Clin Ophthalmol 2023;17:3023-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nagar M, Ogunyomade A, O’Brart DPS, et al. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol 2005;89:1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kent SS, Hutnik CM, Birt CM, et al. A randomized clinical trial of selective laser trabeculoplasty versus argon laser trabeculoplasty in patients with pseudoexfoliation. J Glaucoma 2015;24:344-7. [DOI] [PubMed] [Google Scholar]
- 27.Kaplowitz K, Wang S, Bilonick R, Oatts JT, Grippo T, Loewen NA. Randomized Controlled Comparison of Titanium-Sapphire Versus Standard Q-Switched Nd: YAG Laser Trabeculoplasty. J Glaucoma 2016;25: e663-7. [DOI] [PubMed] [Google Scholar]
- 28.Michaelov E, Sachdeva R, Raniga A, Lin T Y. A randomized, controlled comparison of 180 versus 360 degrees selective laser trabeculoplasty in open angle glaucoma and glaucoma suspects. J Glaucoma 2023;32:252-6. [DOI] [PubMed] [Google Scholar]
- 29.Philippin H, Matayan E, Knoll KM, et al. Selective laser trabeculoplasty versus 0·5% timolol eye drops for the treatment of glaucoma in Tanzania: a randomised controlled trial. Lancet Global Health 2021;9: e1589-e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet 2019;393:1505-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Katz LJ, Steinmann WC, Kabir A, et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma 2012;21:460-8. [DOI] [PubMed] [Google Scholar]
- 32.Pimentel RL, Alves RRA, Lima W, et al. Selective laser trabeculoplasty versus micropulse laser trabeculoplasty for intraocular pressure control in patients with primary open angle glaucoma: a 12-month retrospective comparative study. Lasers Med Sci 2023;38. [DOI] [PubMed] [Google Scholar]
- 33.Landim DFC, Neto CAD, Sabino LRD, et al. Selective Laser Trabeculoplasty (SLT) for IOP Control in a Patient with Bilateral Acute Iris Transillumination (BAIT). Ocular Immunology and Inflammation. 2023. [DOI] [PubMed] [Google Scholar]
- 34.Pillunat KR, Kretz FTA, Koinzer S, Ehlken C, Pillunat LE, Klabe K. Effectiveness and safety of VISULAS(®) green selective laser trabeculoplasty: a prospective, interventional multicenter clinical investigation. Int Ophthalmol 2023;43:2215-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou RX, Sun Y, Chen HY, et al. Laser trabeculo-plasty for open-angle glaucoma: a systematic review and network meta-analysis. Am J Ophthalmol 2020; 229:301-13. [DOI] [PubMed] [Google Scholar]
- 36.Zhu D, Shah P, Wong A, et al. 180° versus 360° Selective Laser Trabeculoplasty in Open Angle Glaucoma and Ocular Hypertension: A Systematic Review and Meta-Analysis. J Glaucoma 2024;33:566-75. [DOI] [PubMed] [Google Scholar]
- 37.Narayanaswamy A, Sood SR, Thakur S. Selective laser trabeculoplasty: An updated narrative review. Indian J Ophthalmol 2024;72:312-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Takusagawa HL, Hoguet A, Sit AJ, et al. Selective laser trabeculoplasty for the treatment of glaucoma a report by the American Academy of Ophthalmology. Ophthalmology 2024;131:37-47. [DOI] [PubMed] [Google Scholar]
- 39.Dendumrongsup W. Identifying baseline predictors of selective laser trabeculoplasty effectiveness: an alternative mathematical approach. Cureus 2024;16:e54116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hallaj S, Sinha S, Mehran NA, et al. Intraocular pressure profile following selective laser trabeculoplasty in pigmentary and primary open-angle glaucoma. Eur J Ophthalmol 2024. doi: 10.1177/11206721241237305. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 41.Kurnaz E. Selective laser trabeculoplasty in the treatment of juvenile open angle glaucoma patients under 25 years of age. Int Ophthalmol 2024;44:201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


