Abstract
Background
Globally, healthcare institutions have seen a marked rise in workplace violence (WPV), especially since the Covid-19 pandemic began, affecting primarily acute care and emergency departments (EDs). At the University Health Network (UHN) in Toronto, Canada, WPV incidents in EDs jumped 169% from 0.43 to 1.15 events per 1000 visits (p < 0.0001). In response, UHN launched a comprehensive, systems-based quality improvement (QI) project to ameliorate WPV. This study details the development of the project’s design and key takeaways, with a focus on presenting trauma-informed strategies for addressing WPV in healthcare through the lens of health systems innovation.
Methods
Our multi-intervention QI initiative was guided by the Systems Engineering Initiative for Patient Safety (SEIPS) 3.0 framework. We utilized the SEIPS 101 tools to aid in crafting each QI intervention.
Results
Using the SEIPS 3.0 framework and SEIPS 101 tools, we gained a comprehensive understanding of organizational processes, patient experiences, and the needs of HCPs and patient-facing staff at UHN. This information allowed us to identify areas for improvement and develop a large-scale QI initiative comprising 12 distinct subprojects to address WPV at UHN.
Conclusions
Our QI team successfully developed a comprehensive QI project tailored to our organization’s needs. To support healthcare institutions in addressing WPV, we created a 12-step framework designed to assist in developing a systemic QI approach tailored to their unique requirements. This framework offers actionable strategies for addressing WPV in healthcare settings, derived from the successes and challenges encountered during our QI project. By applying a systems-based approach that incorporates trauma-informed strategies and fosters a culture of mutual respect, institutions can develop strategies to minimize WPV and promote a safer work environment for patients, families, staff, and HCPs.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12873-024-01144-1.
Keywords: Workplace Violence in Health Care, Quality Improvement, Emergency Department, Pandemic Recovery, Health Systems Innovation
Background
Problem description
Workplace violence (WPV) in hospitals is a multifaceted problem that impacts healthcare institutions globally [1, 2]. The definition of WPV in the healthcare setting is heterogeneous across different agencies and policy makers (see Table 1). However, following the onset of the COVID-19 pandemic, the rate of WPV has more than doubled in healthcare institutions around the world, especially in high-acuity and emergency department (ED) settings [3, 4]. Although there exist numerous attempts by hospitals to address WPV through various interventions, individual initiatives have encountered challenges in achieving a positive impact in part due to the complexity of WPV [5].
Table 1.
Comparing Workplace Violence and Code Whites, [2]
| Definition of Workplace Violence (World Health Organization) | Definition of Workplace Violence (Occupational Health and Safety Act,. R.S.O, 1990, c. O.1) | Definition of Code White (Public Services Health & Safety Association, Ontario, Canada) | Definition of Code White (University Health Network, Toronto, Canada) |
|---|---|---|---|
| Global Definition | Provincial Definition | Provincial Definition | Local Definition |
| " … incidents where staff are abused, threatened or assaulted in circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being or health." (Richards, 2003, p. 2) | a. The exercise of physical force by a person against a worker, in a workplace, that causes or could cause physical injury to the worker; b. An attempt to exercise physical force against a worker, in a workplace, that could cause physical injury to the worker; c. A statement or behaviour that it is reasonable for a worker to interpret as a threat to exercise physical force against the worker, in a workplace, that could cause physical injury to the worker. |
Definition: Code White is a coordinated and trained emergency response to a care recipient, worker, or visitor displaying violent behaviours that may cause harm or injury to others, themselves, and/or is damaging to property. Reasons: Worker perceives themselves or others in danger from a person’s behaviours; Person’s behaviours are harmful to self, others, or damaging to property; Person’s behaviours are escalating towards physical violence; Person’s behaviours are unmanageable for workers and resources. |
Definition: An emergency response for a violent person. Reasons: The person is verbally and/or physically threatening towards themselves, staff, patients/clients, and/or visitors; The person is not responding to verbal de-escalation techniques, negotiating, redirection, limit setting, and problem-solving techniques by the staff; The person may require restraint (chemical and/or physical) and is anticipated to be resistive to the restraining procedure; and/or, urgent assistance is required. |
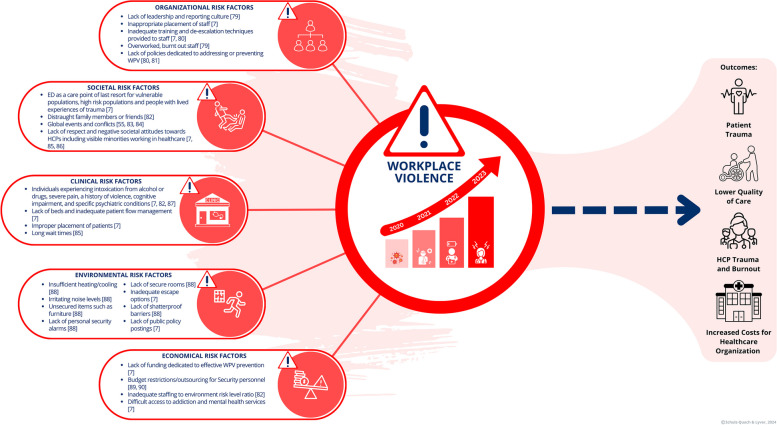
Ameliorating WPV-related outcomes requires complex interventions and a systems approach to change management in healthcare [5, 6]. To effectively design such interventions, a comprehensive understanding of the issue and contributing risk factors is required. Several category systems for WPV in healthcare settings have been proposed, such as the five risk factor categories suggested by Keith & Brophy [7]: (1) clinical risk factors, (2) environmental risk factors, (3) organizational risk factors, (4) societal risk factors, and (5) economic risk factors [7, 8]. Figure 1 illustrates the breadth of these factors, emphasizing the interdependence of variables contributing to WPV. A systematic framework and step-by-step guidance for the development and implementation of WPV prevention interventions is needed in healthcare to support organizations in making measurable impacts on this multifaceted problem.
Fig. 1.
This figure illustrates the complexity of WPV in healthcare, encompassing the escalation of WPV since the onset of the pandemic, the contributory risk factors, and the resultant outcomes for patients, HCPs, and healthcare organizations. References relating to [7, 9–21]
Available knowledge
A multitude of theories in scholarly research provide deep and varied understanding of the factors that drive WPV in healthcare environments [22]. These theories arise from a range of academic fields, such as psychology, biology, criminology, ecology, and sociology. Table 2 provides a summary of theoretical frameworks identified in a narrative review of the literature to describe WPV. Gaining insight from various theoretical standpoints is essential for a cross-disciplinary approach to effective WPV prevention strategies in healthcare settings and it was one of the early steps our team approached when initiating this project [22]. We believe that the practical application of these theories is key to understanding the subtle aspects relevant to intervention(s) implementation, which can greatly influence their success. For example, the efficacy of common practices such as education and training programs, commonly used in WPV prevention strategies, may hinge on how well these theories are integrated into their design. Theories such as the Minority Stress Model [23], Terror Management Theory [44], and the Struggle for Recognition theory [30], highlight the importance of adopting a trauma-informed perspective which has been linked to improved outcomes in healthcare settings [50, 51]. Without an in-depth understanding of these theories, training may prove to be inefficient or yield only temporary effects without the necessary impact on organizational culture change. However, research has demonstrated that well-structured training programs can reduce the impacts of WPV incidents [52]. Thus, good understanding of WPV theories is crucial for effectively addressing and ameliorating WPV in healthcare settings.
Table 2.
Summary of theoretical frameworks identified in our literature review for understanding WPV
| Theory | Theory description | Category of risk factor | Non-modifiable factors within hospitals | Modifiable factors within hospital | Quality improvement initiatives |
|---|---|---|---|---|---|
| Ecological occupational health model of workplace assault [23, 24] |
• A model depicting the factors and consequences of WPV in Long Term Care • It considers the complex interactions between individual worker, interpersonal, organizational environment, and societal factors. • Factors included the individual worker, the workplace, the external environment, and the assault situation • Assaults have an impact on the workers, workplace and quality of care |
• Clinical risk factors • Societal risk factors • Organizational risk factors |
• Societal changes • crime rates • substance abuse • lack of mental health care • Staffing levels • Global affairs/wars |
• Individual worker sense of safety in their workspace |
• Environmental indicators • Debriefing Improved • Incident Reporting • Interviews, pulse surveys |
| • Training and education | • Educational intervention | ||||
| Broken Windows Theory [25] |
• Criminology based • Tolerance of smaller crimes leads to more larger crimes occurring • Tolerance of verbal abuse can lead to more severe forms of abuse, such as physical abuse, being tolerated |
• Organizational risk factors |
• Societal changes • crime rates • substance abuse • lack of mental health care • world events |
• WPV Policies Managing • WPV Data and statistics |
• Identifying and implementing tailored quality indicators on WPV |
| Cultural care theory [26] |
• Uses Holistic Culture Care Theory • Identifies 4 subcultures of those involved in ED WPV • ED Nurses • Institution’s administration departments • Clients with violent behaviours • Clients without violent behaviours • Three prominent themes • Policies often lack sufficient contribution to a safe ED environment • Administration often value hospital/organizational reputation over ED staff well-being • Anxiety, fear, and negative emotions caused by WPV impact nurses’ quality of care |
• Clinical risk factors • Societal risk factors • Organizational risk factors |
• Clients with violent behaviours Clients without violent behaviours |
• WPV culture • Support for ED staff |
• Educational interventions • Environmental indicators • Debriefing • Improved Incident Reporting • Interviews, pulse surveys • Clinical representation in leadership decisions |
| Routine Activity Theory [27] |
• Criminology based • A person’s daily activities can increase or decrease the opportunities for victimization • A person with one or more of the following is likely to be a victim of WPV; • greater exposure to aggressor • lower levels of protection over possible targets • repeated engagement with potential aggressor • greater closeness to potential aggressor |
• Organizational risk factors • Societal risk factors • Clinical risk factors • Economical risk factors |
• Patient behaviour upon arrival • Staff exposure to patients with aggressive behaviours |
• Societal perspectives on hospital staff • Increased protection for staff |
• Environmental indicators • Increased security presence • Wearable devices such as body cameras • Personal alarm buttons • Environmental awareness training |
| Situational Crime Prevention Theory [28] |
• Criminology based • Situational crime prevention theory is based on rational choice theory • Offenders consider the perceived risks and rewards associated with crime • in healthcare, attacking a nurse could prevent the pain associated with medical interventions such as drawing blood • Need to emphasize the punishment and risk for violent behaviour in ED in environment to reduce the rewards |
• Organizational risk factors | • Emphasizing WPV policies in hospital |
• Environmental indicators • Policy review |
|
| Framework of cultural aspects of violence in the ED [29] |
• Cultural themes related to WPV in the ED were categorized into the following three groups; • Problems and solutions • Staffs perceptions of violence • Indicators or warning signs of violence • Diverse staff responses to violence • Them and us • Patient/relative behaviour • Nurses’ behaviour • Requests and demands • Rejected request of patients/relative • Long waiting times or waiting times perceived as long contributing to requests and demands of patients and relatives |
• Organizational risk factors • Societal risk factors • Clinical risk factors • Economical risk factors |
• Wait times • Patient and relative behaviour • Number of staff |
• Nurses behaviour • Perceptions of violence • Knowledge of violence • Response to violence • Patient/visitor requests |
• Education • Support • Outreach to staff • Trauma informed approach • Behavioural emergency response team |
| Honneth’s theory of struggle for recognition [30, 31] |
• Three themes that describe the experiences of patients in WPV situations; • Unmet needs • Involuntary assessment • Unsolicited touch • Violence felt as a demand for rights and recognition as a person |
• Societal risk factors • Clinical risk factors |
• Previous patient experiences and traumas | • Trauma-informed approach | • Education for staff |
| Psychological frameworks [32]: Psychoanalytical model [33], personality theories [34–39], frustration-aggression hypothesis [40] |
• Aggressive behaviours may be innate and unconscious forces due to certain personality types • Frustration when patient can’t get what they want • We have no control over who enters ED so nurses must be calm and prepared |
• Societal risk factors | • Patient population | • Calm and prepared HCPs |
• Education interventions • Support for staff • Pulse survey, check ins • Behavioural emergency response team |
| Environmental Stimuli theories [32] |
• Negative affect escape model [41] • Unpleasant environmental stimuli increasing in intensity can often lead to aggression • Excitation-transfer theory [42] • Stimuli add up and can result in triggering an aggressive behaviour |
• Environmental risk factors |
• Patient population with environmental triggers • Physical layout of hospital |
• Limiting stimuli • Comfortability of patients and visitors |
• Seclusion rooms • Limiting noise • Regulating temperature • Creating calm atmosphere |
| Rational Choice Theory [43] |
• Makes choice based on rational calculation of costs and benefits or pain versus enjoyment with the aim of maximizing pleasure • Perception and understanding of potential pain caused by the punishment drives the choice • If you don’t follow through with protecting you workers, then likely to commit more violence as no costs, only benefits |
• Clinical risk factors • Organization risk factors |
• Patient population with prior negative experiences and traumas with healthcare • Patient population with knowledge of medicine |
• Trauma-informed approach • Supported staff • Policy to protect staff |
• Education interventions • Debriefs • Improved culture with regards to WPV • Environmental indicators • Policy change |
| Terror Management Theory [44] |
• Addresses how individuals cope with anxiety and fear associated with their awareness of mortality • If a person consciously believes that a world event such as the • Covid-19 virus could result in death, fear of death will play a role in a person’s attitude and behaviours regarding the topic Covid-19 disrupts the feeling of calmness, causes a feeling of threat, terror management takes over and responds in distress or disorderly manners • Awareness of death creates a potential for existential terror to due survival instincts • Anxiety buffering systems related to cultural worldviews, self-esteem and close interpersonal relationships play a role in this • Fear of death may be conscious or unconscious |
• Clinical risk factors • Organization risk factors |
• Patient population with prior negative experiences and traumas with healthcare • Patient population with knowledge of medicine |
• Trauma-informed approach • Supported staff |
• Education interventions • Debriefs • Improved culture with regards to WPV • Increased security guard presence |
| Psychology Model for Understanding Violence [45] |
• Psychobiological theories of violence include brain dysfunction, autonomic functioning, hormones, neuropsychology, and temperament • Evolutionary psychology states that due to natural selection, humans have evolved adaptations enabling them to harm other humans in order to reproduce and survive, which still exists • The death instinct states that a defence system controls our anger but when we no longer feel like they keep us safe, we may react with violent behaviour |
• Societal risk factors | • Biological factors affecting patient population |
• Trauma-informed approach • Culture change |
• Education intervention • Environmental indicators |
| Sociological perspectives on WPV [46] |
• Violence is a resource used to obtain a result • Violence is a reaction to a crisis situation • Culture of violence from either, friends, family, community or society leads to more violence |
• Societal risk factors | • Patient population | • Trauma-informed approach | • Education intervention |
| Psychosocial Risk Factors [47] |
• Biological vulnerability for aggression in combination with psychosocial factors contribute to aggressive behaviours, factors include • Proximal factors, present psychological state • Developmental and environmental factors influencing an individual’s personality and cognition |
• Societal risk factors | • Patient population | • Agitation management | • Education Intervention |
| Minority Stress Model [48] |
• A model based on multiple sociological and social psychological theories that describes the stigma, prejudice, and discrimination that minority communities encounter and the impact that these negative experiences have on individuals’ physical and mental health • Negative encounters stemming from discrimination and stigmatization may lead individuals to anticipate rejection and discrimination in social contexts, prompting the development of defensive coping mechanisms that could be perceived as confrontational • Marginalized communities can include ethnic minorities, the 2SLGBTQIA+ community, individuals with disabilities • Model argues that minority stress can only be managed through systemic changes that address social inequalities and providing the necessary supports and resources that marginalized communities require |
• Societal risk factors | • Societal inequalities that result in marginalization, discrimination and stigma towards minority communities |
• Trauma-informed approach • Culture change within hospital |
• Education interventions • Improved culture with regards to WPV |
| Intersectional Identities [49] |
• Intersectional identities outlines the power and control individuals experience in society due to different intersecting aspects of their identity including sex, gender, age, sexual orientation, ethnicity, race, religion, language, culture, education, presence of disability, geography, income, marital status, immigration status and indigenous status • Whether an individual experiences power or discrimination in their society is determined through the way their different identities are interpreted by the society they live in and the way their identities intersect, for example a person that identifies with multiple marginalize communities is more likely to experience discrimination than a person that identifies mainly with the identities in power • Individuals with marginalized identities possess more lived experiences of trauma are likely to feel less safe in social situations |
• Societal risk factors | • Societal inequalities that result in marginalization of identities |
• Trauma-informed approach • Culture changes within hospital |
• Education interventions • Improved culture with regards to WPV |
Rationale
WPV in healthcare is an urgent issue that significantly impacts patients, chosen family members, healthcare providers (HCPs), and healthcare institutions (Fig. 1). The rising frequency and severity of WPV incidents, particularly in acute care settings, necessitate targeted interventions that address this pressing challenge [3, 4]. Research indicates that WPV not only harms individual well-being but also adversely affects overall quality of care, HCP morale and burnout, and contributes to an environment that compromises safety [53].
Previous attempts to address WPV have often fallen short due to the multifaceted nature of the problem [5, 7]. Research demonstrates that a multicomponent intervention utilizing a systems-based approach is necessary to effectively address WPV [5]. Consequently, a systematic framework outlining the identification and development of a complex WPV prevention intervention is essential in healthcare to assist organizations in creating comprehensive solutions to this complex issue.
Developing such interventions requires a robust QI initiative. QI projects in patient and staff safety often focus on the three categories derived from Donabedian’s Structure-Process-Outcome (SPO) model [54]; however, this approach omits a focus on the ‘human factor’ within the structure component and the individuals involved in the processes including patients, caregivers, chosen family members, HCPs and patient facing staff. To expand on the work developed by Donabedian, Carayon and colleagues released multiple iterations of the Systems Engineering Initiative for Patient Safety (SEIPS) [54–56]. With SEIPS, the “structure” component of Donabedian's framework is reimagined as a “work system”, where there are five main elements interacting: person, environment, organization, technology and tool, and task factors [54].
In this QI project, we incorporated the 3.0 iteration of the SEIPS framework to support us in developing a comprehensive, systems approach to address our multifaceted WPV challenges [56]. Further details on the operationalization of SEIPS 3.0 in our methods and interventions are provided in the Methods section.
Specific aims
WPV in healthcare is a complex systemic issue that requires a comprehensive solution. The aim of this article is to present the development of a large-scale multifaceted QI project tailored to a multi-site academic health science centre in Toronto, Ontario. Additionally, we present a stepwise framework that summarizes our initial approach and learning points to support other healthcare institutions in developing an approach to address WPV from a systems theory lens.
Methods
Context
The Security Operations Program at a multi-site academic health science centre established a QI team to address WPV in November 2022. Our organization is a complex healthcare network comprised of three acute-care hospitals, including a cancer centre, a multi-site rehabilitation network and an educational institution. In 2022, this organization had a care volume of approximately 98,000 inpatient weighted cases, 1.1 million ambulatory visits, and 158,000 ED patients. WPV incidents in the ED increased overall during the COVID-19 pandemic (1.15 reported incidents per 1000 ED visits) compared to 2019 (0.43 reported incidents per 1000 ED visits), an increase of 169% (p < 0.0001). This data is consistent with data from other EDs globally [3, 4, 57]. The QI team consisted of healthcare professionals, administrative leaders, and researchers who were sponsored by the organization’s executive leadership, to develop a comprehensive strategy for ameliorating WPV. The QI initiative received formal Research Ethics Board exemption and approval from the organization's Quality Improvement Review Board (QI ID: 22–0499). Our reporting followed the Revised Standards for Quality Improvement Reporting Excellence guideline [58].
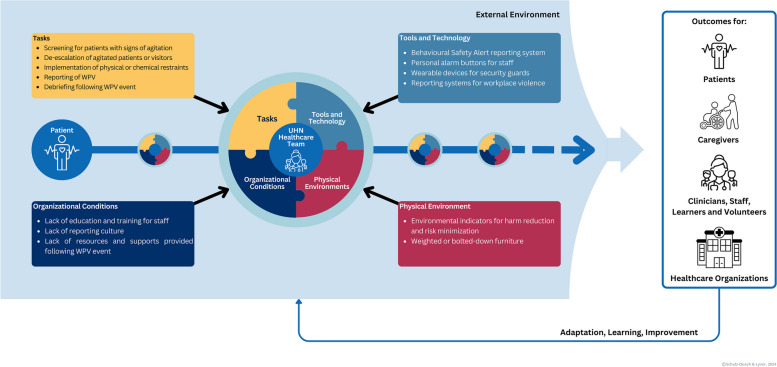
Interventions
The SEIPS 3.0 framework guided a systemic approach to investigating and understanding the configurations of work system elements and functional entities, interactions through processes, and patient, caregiver, HCP, and organizational outcomes. SEIPS 3.0 was also selected as compared to past iterations of SEIPS as this iteration recognizes that patients move through various and unique work systems in their patient journey. Thus, SEIPS 3.0 provided us with a structure to examine factors influencing and interacting with WPV across multiple care environments.
Recognizing the need for practical tools to implement SEIPS, the creators developed a set of tools referred to as “SEIPS 101” [59]. These tools provide a simplified version of the SEIPS model that includes seven unique tools for QI initiatives [59]. We employed the SEIPS 101 tools in a variety of ways to identify areas for improvement regarding WPV at our institution. These identified areas informed the development of the subprojects that constitute our WPV QI project.
The first tool, the People, Environment, Tools, Tasks (PETT) scan is a checklist used to investigate the work system and provide the researcher with the broader context of the interactions within a system, it’s facilitators, barriers, contributing factors and areas of improvement [59]. A PETT scan was performed by collaborating with key stakeholders to complete the PETT scan template. The next tool is the people map, which takes the people aspect of a PETT scan to a more in-depth level. A people map identifies people involved in a work system, their roles, interactions with others, as well as the proximity of interactions [59]. To perform a people map, researchers must identify and document the roles, responsibilities, and relationships of individuals within a specific area or process. This involved gathering information from stakeholders then visually mapping out the connections and interactions [59].
Additional SEIPS 101 tools involve the use of matrices including Tasks and Tools matrices. This matrix identifies the tools that are being used for tasks within a work system and allows researchers to identify opportunities to streamline process and design or redesign tools to better serve the task [59]. We performed a tools and tasks matrix by engaging with key stakeholders and completing the SEIPS 101 Task Matrix, Tools matrix, and the Tasks X Tools Matrix ([59], Supplementary file, page 3]). We analyzed the matrix to identify gaps, redundancies, and areas for improvement, subsequently developing QI initiatives to optimize efficiency and effectiveness. Another tool includes the outcomes matrix, for each task or QI initiative, an outcome matrix can be performed to identify project goals, determining measures to be collected or establish evaluation criteria. We performed this task by completing an outcome matrix ([59], Supplementary file, page 4]), identifying desirable and undesirable outcomes as well as means to evaluate the outcomes.
The SEIPS 101 Journey map investigates the journey of an individual or functional unit throughout a process and identifies the impact and interactions with the work systems and its outcomes. The tool is valuable in highlighting issues or considerations when modifying processes or systems. We performed a journey map by documenting the step-by-step experiences and interactions of users throughout a process or system of interest. This enabled us to visualize the journey of the user throughout a process. The interactions diagram highlights the interactions between people, environments, tools, and tasks to identify areas for improvement and enhance understanding of the work system. To perform an interactions diagram, we mapped out the interactions between people, environments, tools, and tasks to visualize relationships and identify areas for improvement within the work system. Lastly, the systems story tool serves as a frame of reference by illustrating how changes in the work system impact processes and subsequent outcomes. This tool effectively communicates complex concepts and can be used to advocate for change. Researchers developed a narrative using findings from a qualitative interview study and employed storytelling techniques to engage stakeholders effectively. Further details of these tools can be found in the SEIPS 101 Supplementary file [59].
Study of the Interventions
This article presents the development process of the 12 subprojects to provide a focused and detailed account of our QI interventions. For the purposes of this article, we will focus on presenting the development of the 12 subprojects, outlining how SEIPS 3.0 and SEIPS 101 tools informed the creation of these interventions. This approach provides a detailed account of the development process of the interventions. Future publications will provide a presentation of the effectiveness and outcomes of these interventions.
Results
Identifying where change is needed within UHN
The SEIPS 3.0 framework and SEIPS 101 tools guided our environmental scan and strategic planning with stakeholders in order to develop an initiative aiming to collectively understand, measure, and ameliorate WPV at our organization. A SEIPS 3.0 journey map was created by our QI team to outline the key factors and interactions related to WPV within the work system. The QI team collaborated with 48 stakeholders that were identified as experts who are involved in some aspect of WPV [60] to gather information on workflows and WPV related processes in 5 meetings, in addition the QI team reviewed existing data related to WPV. This information was used to map the patient journey as it relates to WPV, identifying the various people, tasks, tool and technologies, as well as organizational and environmental conditions related to WPV (Fig. 2). This map provided the foundation for our QI project, guiding the team in identifying necessary areas to investigate using the SEIPS 101 toolbox.
Fig. 2.
An illustration of the application of the SEIPS 3.0 journey map to identify the tasks, tools and technology, physical environment, and organizational conditions relevant to WPV in healthcare. Adapted from [56]
After identifying key intervention areas through the SEIPS 3.0 journey map, the QI team selected specific SEIPS 101 tools to further investigate these areas and guide the development of our QI interventions. Ultimately, a comprehensive QI initiative consisting of 12 subprojects was developed and implemented based on insights gained from the application of the SEIPS 101 tools (Table 3). To illustrate our approach, this article will focus on three example topic areas drawn from these subprojects.
Table 3.
Summary of the 12-subproject quality improvement initiative, including the application of SEIPS 101 tools and proposed outcome measures for each subproject. For additional information on the 12 subprojects, please refer to Appendix 1
| Subproject number | Subproject | Subproject description | SEIPS 101 tools utilized | Structural units responsible | Associated change implemented | Proposed outcome measure |
|---|---|---|---|---|---|---|
| 1 | Ongoing Literature Review of WPV-related topics | Ongoing literature reviews of current research pertaining to WPV in healthcare were performed to provide UHN Security with the most up to date information necessary to make informed decisions. | • Outcomes Matrix | • UHN Security WPV QI Team |
Ongoing literature reviews on the following topics related to WPV: • WPV in healthcare settings during the pandemic • Agitation Management • De-escalation Techniques • Code White Simulation Training |
• number of hot debriefs since implementation • number of cold debriefs logged since implementation • number of Code White/WPV requests for escalation |
| 2 | Identifying quality indicators for measuring change in quality of care related to Code White and WPV incidences | Based on a rapid review, a collated list of quality indicators will be condensed to the top relevant, impactful and feasible indicators through an anonymous modified Delphi process. This process will utilize experts from UHN and Toronto Academic Health Science Network. | • Outcomes Matrix | • UHN Security WPV QI Team |
• Rapid review of quality indicators to measure WPV-related processes in healthcare • Modified Delphi process to select top indicators |
• number of governance committee meetings • number of annual progress reports |
| 3 | Implementing quality indicators to an organization-wide WPV dashboard | A WPV dashboard with the top evidence-based quality indicators identified from the modified Delphi process will be created to measure WPV at UHN and be used to inform leadership decision making. |
• Outcomes Matrix • Journey Map |
• UHN Security WPV QI Team | • WPV dashboard creation |
• number of hot debriefs since implementation • number of cold debriefs logged since implementation • number of Code White/WPV requests for escalation |
| 4 | Changing the perception of safety and support in HCPs during Code White and WPV incidences | A longitudinal qualitative approach to capture ED staff’s perception of safety, support, clinical guidance relating to managing and learning from WPV incidence, security and personal expectations for organizational change. Additionally, measuring change over time in sense of preparedness to handle WPV situations using Bandura’s self-efficacy theory. | • Systems Story | • UHN Security WPV QI Team | • Performing semi-structured qualitative interviews with all staff, learners and volunteers in the ED on an ongoing basis | • number of meetings regarding community outreach |
| 5 | Implementation of educational intervention I | An ad-hoc training program focused on situational and environmental awareness was implemented as a pilot training program for ED staff. The program would provide staff with additional training methods and skills for safety and self-protection while determining whether a need for additional training was evident. |
• Outcomes Matrix • Systems Story |
• UHN WPV Education Collaboration • UHN Safety Services • Code White Governance Committee • UHN Security WPV QI Team |
• Implementation of a pilot WPV skills training session | • number of meetings regarding reporting systems |
| 6 | Implementation of a dedicated UHN Code White Governance Committee |
A governance committee dedicated to Code Whites at UHN that will be responsible for the following tasks: • establishing a streamlined approach and response to Code White incidents • overseeing implementation of high complexity Code White simulation training that uses a trauma-informed lens • optimize Code White incident reporting, including a user-centred and trauma-informed reporting approach • optimizing of auditing statistics and quality indicators for Code White clinical care at UHN |
• PETT Scan • People Map • Journey map • Interactions Diagram |
• UHN WPV Prevention Advisory Committee • Code White Governance Committee |
• Implementation of an interdisciplinary Code White Governance Committee |
• number of hot debriefs since implementation • number of cold debriefs logged since implementation • number of Code White/WPV requests for escalation |
| 7 | Reviewing, updating and implementing incident reporting for WPV and Code White incidents | A working group made up of multiple functional units at UHN are reviewing the incident reporting processes and reporting systems at UHN. The working group will update UHN’s reporting system to develop a streamlined, user-centred and trauma-informed reporting approach. | • Tools and Tasks Matrix |
• UHN Quality and Safety • UHN Safety Services • UHN Emergency Preparedness • Code White Governance Committee |
• Development of Safety Event Reporting and Review System (SERRS) Project | • number of meetings on physical restraint systems |
| 8 | Implementation of educational intervention II (UHN TIDES) | The development of a trauma-informed WPV prevention education program centred around agitation management, de-escaltion techniques, physical safety, self-protection and code white simulation. The training must be specific to staff’s environment, provide the opportunity for different positions to work together and provide refresher training. |
• Outcomes Matrix • Systems Story |
• UHN WPV Education Collaboration • UHN Safety Services • Code White Governance Committee • UHN Security WPV QI Team • External Collaboration partner |
• Implementation of UHN TIDES | • number of articles related to WPV in healthcare that were reviewed |
| 9 | Implementing Environmental Indicators for harm reduction and risk minimization | Environmental signage using trauma-informed language to communicate a message of mutual respect between hospital staff and visitors to create an environmental and cultural change surrounding WPV in EDs. | • Interactions Diagram | • UHN Security WPV QI Team | • Implementation and evaluation of environmental indicators for mutual respect in UHN EDs |
• number of quality indicators identified from the literature • number of unique quality indicators operationalized for UHN • number of unique quality indicators selected through the Delphi Process |
| 10 | Code White hot and cold debriefing process and debriefing escalation algorithm | A new approach to debriefing following Code White and WPV events will be implemented using hot and cold debriefs. Additionally, an algorithm for escalating a Code White or WPV event will be developed. |
• PETT Scan • People Map • Tools and Tasks Matrix • Journey Map • Interactions Diagram |
• UHN Emergency Preparedness • Code White Governance Committee • UHN Security WPV QI Team |
• Implementation of hot and cold debrief guidelines • Implementation of new communication strategy for entities requesting cold debriefs |
• number of quality indicators implemented • number of databases used to provide data |
| 11 | Physical restraint systems | Currently no guidelines or policies on physical restraints are provided on a provincial or national level. A descriptive physical restraint system is required for a universal approach to applying physical restraints. | • Tools and Tasks Matrix |
• Code White Governance Committee • UHN Security WPV QI Team |
• Development of physical restraint system |
• number of staff that completed training program • evidence of staff satisfaction with training |
| 12 | Patient partners and community outreach | Connecting with patients, caregivers and (chosen) family members and providing them with the opportunity to connect and talk about their experience during Code White or WPV events. |
• People Map • Systems Story |
• Code White Governance Committee • UHN Security WPV QI Team |
• Implementing a town hall style meeting with patients, caregivers and (chosen) family members involved in Code White or WPV events |
• evidence of new training program • number of trainers hired |
Code white interventions: subprojects 6 and 10
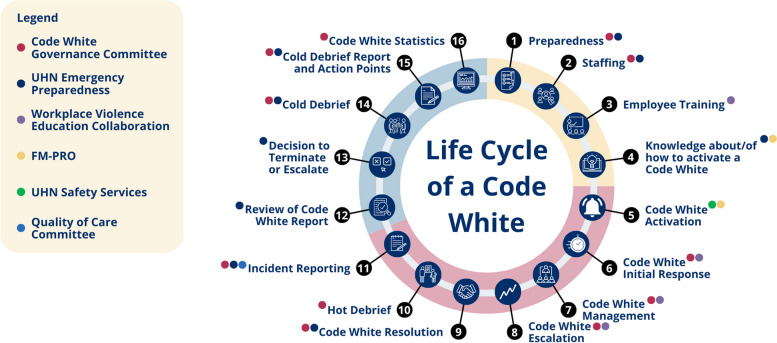
Multiple SEIPS 101 tools were employed to investigate Code White incidents and related processes at UHN, including a PETT scan, people map, tools and task matrix, journey map, and interactions diagram. These tools facilitated a comprehensive understanding of the Code White process and informed the development of targeted interventions.
In collaboration with 10 key stakeholders, including representatives from Safety Services, the Emergency Department, and the Centre for Mental Health, we conducted a PETT scan using the PETT scan template to identify the people, environments, tools, and tasks involved in a Code White incident. Following this, a people map was created to further examine the roles of individuals and functional units engaged during a Code White (Table 4).
Table 4.
Functional units at UHN addressing or involved in processes related to WPV and Code White incidents within UHN [2]
| Code White Governance Committee (CWGC) | • Composed of clinical and academic experts in the field of agitation management |
| • Provide guidance and structure required to streamline and optimize CW management | |
| Workplace Violence Prevention Advisory Committee (WPVPAC) | • Put in place by the UHN executive leadership forum to address WPV across UHN |
| Workplace Violence Education Collaboration (WPVEC) | • Collaboration between Safety Services and Security that is providing staff, learners and volunteers with education related to WPV and CWs |
| Quality of Care Committee | • Involved in reviewing and improving the quality of care provided at the healthcare institution |
| Safety Services | • Prioritizes and monitors the safety of UHN staff and patients |
| Emergency Preparedness (EP) | • Supports UHN in preventing, mitigating, preparing for and recovering from emergency events that impact staff, patient and visitor safety and the delivery of critical services |
| Facilities Management-Planning, Redevelopment and Operations (FM-PRO) | • Responsible for a wide range of tasks related to maintaining the physical environment at the healthcare institution |
| Security Operations | • Responsible for providing UHN staff and patients with protection, security and support |
We then combined an interactions diagram with a journey map to develop the Life Cycle of a Code White (LCCW) (2). The information gathered from the PETT scan and people map was used to outline all steps in a Code White and identify the functional units involved at each stage (2). The LCCW revealed 16 distinct steps and the participation of 6 functional units, highlighting the complexity of Code White incidents (Fig. 3). This comprehensive understanding underscored the need for a governance committee to evaluate and streamline Code White processes. As a result, these SEIPS 101 tools collectively identified the need to implement a Code White Governance Committee (CWGC) (subproject 6).
Fig. 3.
The Life Cycle of a Code White, a journey map that outlines the steps involved in a Code White and the functional units involved [2]
Furthermore, the LCCW identified the need to streamline our organization’s debriefing approach. Our QI team collaborated with Emergency Preparedness to perform a tools and task matrix for the debriefing process. Following this task, a new Code White hot and cold debriefing process and debriefing escalation algorithm would be developed (subproject 10).
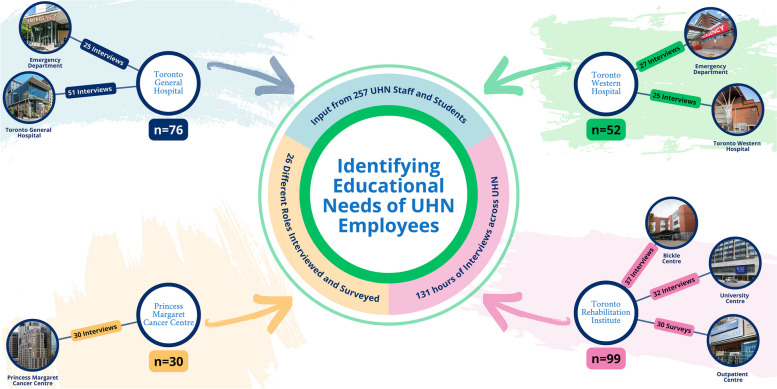
Education interventions: subprojects 5 and 8
A need for education interventions was identified and developed using an outcome matrix and the systems story tool. Both tools were informed by qualitative data (Appendices 2 and 3), which was collected through semi-structured interviews conducted by our QI team at both UHN EDs (n = 52) and by the CWGC, which conducted 175 interviews and 30 surveys across all UHN sites (Fig. 4). All interviews and surveys underwent a thematic analysis performed by our QI team and the CWGC. The findings of the analysis frequently were related to staff feeling unsafe, unsupported and emphasized a need for education related to WPV prevention. A detailed summary of the findings will be presented in a separate publication.
Fig. 4.
Overview of the educational needs assessment conducted at UHN. The assessment collected input from 257 UHN staff and students from 26 different roles across all sites. The data collected was used to create a systems story
An outcome matrix was developed by our QI team based upon the findings of the thematic analysis. Project goals included improving staff’s sense of safety, support and confidence in de-escalation. The matrix allowed us to identify that education interventions across the organization were needed, however, implementing such a project in a large organization would require executive level support. Consequently, the thematic analysis was utilized to illustrate a systems story that effectively advocated the need for WPV prevention education to UHN leadership. The systems story helped advocating with leadership to implement an ad-hoc education initiative (subproject 5) was implemented as a pilot project, in addition to supporting implementation and rollout of an organization-wide WPV prevention education program (subproject 8).
Environmental interventions: subproject 9
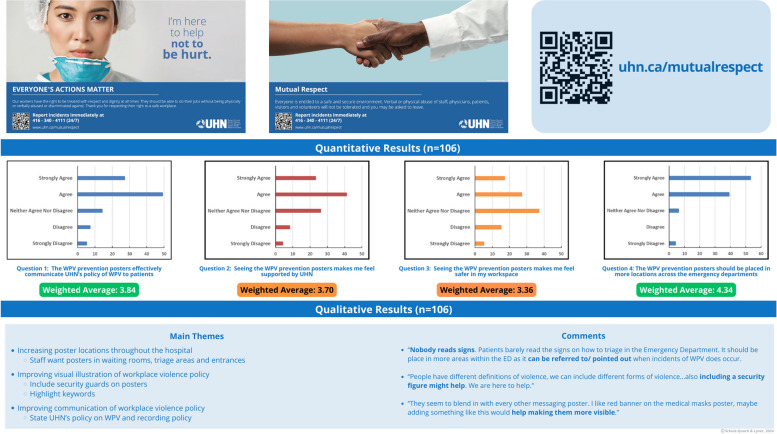
An interactions diagram was utilized to explore the relationships between people, environments, tools, and tasks during a WPV incident, with the aim of identifying areas for improvement within the work system. Utilizing the lived experiences of our QI team members as clinicians, code white respondents, and security personnel, we mapped these interactions to better understand the dynamics involved. The diagram revealed the absence of an environmental component that actively advocated for WPV prevention. Utilizing findings from an environmental scan of other healthcare and public service institutions, such as public transit, we identified posters as an effective tool for communicating messages of mutual respect and hospital policies related to WPV. In response, five posters were developed using trauma-informed language to promote mutual respect between patients and HCPs (Fig. 5). Feedback was gathered from 106 staff members through surveys (Appendix 4) using a convenience sampling method. Although staff voiced that the posters were not enough to prevent WPV, they supported the project and requested that more posters be placed throughout the hospital (Fig. 5). Further details from these surveys will be shared in a future publication.
Fig. 5.
An overview of the Environmental Indicators Project, featuring samples of the posters utilized, alongside qualitative and quantitative feedback obtained from staff through surveys
Discussion
Summary
In summary, a large-scale QI initiative was developed using SEIPS methodology to arrive at 12 subprojects at our large multi-site academic health sciences centre in November 2022 with the objective of addressing WPV from a systemic perspective. The project consisted of various literature-based, community, educational, and organizational interventions that were identified and informed using the SEIPS 3.0 framework and SEIPS 101 tools.
Interpretation
Systematic framework to address WPV in healthcare institutions
The following framework was created to provide guidance on how to approach WPV in a healthcare institution. Although, there is an abundant amount of literature on WPV-related topics and interventions, in addition to frameworks for QI projects, there is limited guidance on how to address WPV in hospital settings. Therefore, we created a 12-step framework which was also used to guide our WPV QI initiative at UHN (Table 5).
Table 5.
Summary of the 12 Steps in our systematic framework for addressing WPV in healthcare institutions, including the associated subprojects implemented at our healthcare institution for each step
| Framework step number | Framework step | Step description | Evidence | Corresponding subproject |
|---|---|---|---|---|
| 1 | Define the Problem and Find the Data | WPV quality improvement projects should begin by clearly defining the problem and reviewing available data. Tools like the SEIPS 101 PETT scan help identify key elements and interactions within the work system, including barriers, risk factors, and facilitators, providing a comprehensive understanding of the WPV problem. This method is particularly useful for organizations that lack sufficient data due to issues like underreporting. |
• Holden & Carayon, 2021 • Chung et al., 2014 • Cumbler et al., 2013 • Bokhoven et al., 2003 • Mento et al., 2020 |
SP1. Ongoing Literature Review of WPV-related topics SP3. Implementing quality indicators to an organization-wide WPV dashboard SP4. Changing the perception of safety and support in HCPs during Code White and WPV incidences |
| 2 | Assemble a WPV QI team | Addressing WPV is a complex task that will require a well-rounded interdisciplinary team. The team should include individuals with diverse perspectives, skill sets, and backgrounds and should emphasize collaboration and creativity in order to have effective WPV quality improvement. |
• Chung et al., 2014 • Kaplan et al., 2012 • Hulscher et al., 2013 |
This relates to the approach taken for the systems level QI project. |
| 3 | Listen to Frontline Staff | Collecting qualitative data from frontline staff is crucial for WPV initiatives. WPV contributes to HCP burnout, high turnover rates, and reduced quality of care; ensuring HCPs feel heard fosters a sense of organizational support and yields valuable insights. Integrating both qualitative and quantitative data through interviews and surveys enables organizations to better understand WPV, support staff, and guide QI efforts. A mixed-methods approach, including longitudinal data, enhances intervention effectiveness and secures key collaborators' buy-in. |
• Schulz-Quach et al., 2022 • Shanafelt et al., 2020 • Crowe et al., 2017 • Calman et al., 2013 • Sachdeva et al., 2007 • Franco et al., 2011 |
SP4. Changing the perception of safety and support in HCPs during Code White and WPV incidences |
| 4 | Key Collaborator Engagement | Active engagement with key collaborators, especially organizational leadership, is essential for the success of WPV QI projects. Leadership buy-in ensures resource availability, fosters cultural change, and supports the sustainability of ongoing WPV initiatives like training. Early involvement, clear communication, and including key collaborators in decision-making are critical to maintaining their long-term support. |
• Kaplan et al., 2012 • Fryer et al., 2007 • Kaplan et al., 2010 • Brandrud et al., 2011 • Guise et al., 2013 |
This relates to the approach taken for the systems level QI project. |
| 5 | Bringing Organizational Entities Together | Addressing WPV requires collaboration beyond the QI team, involving representatives from all functional units to ensure a comprehensive understanding of the problem. However, siloed operations in healthcare institutions often hinder efficiency and can undermine organization-wide initiatives like WPV prevention. Effective communication between departments must be established early, as demonstrated in our case, where eight distinct functional units addressing WPV were identified and brought together before initiating change. |
• Chung et al., 2014 • Alves et al., 2018 • Akmal et al., 2021 |
This relates to the approach taken for the systems level QI project. |
| 6 | Implement an Effective Governance Structure | An effective WPV governance structure is vital to project success, providing leadership, preventing conflicts, managing resources, and ensuring sustainability. In our large organization, multiple governance structures were developed alongside existing departments to support the WPV QI initiative. The governance framework should include leadership from all relevant functional units, with a clear charter outlining roles, budgeting, goal alignment, and data sharing. Additionally, presenting to senior executives is essential for securing full organizational endorsement. |
• Kaplan et al., 2012 • Fryer et al., 2007 • Derakhshan et al., 2019 • Jones et al., 2017 |
SP6. Implementation of a dedicated UHN Code White Governance Committee |
| 7 | Assess Project viability and Monitor Progress and Engagement of Functional Units | Assessing viability and monitoring project execution are crucial for multi-level WPV initiatives to achieve successful outcomes. The DICE framework, developed by the Boston Consulting Group, evaluates key factors such as project duration, team integrity, commitment of senior executives and frontline collaborators, and the additional effort required from staff. Continuous monitoring helps maintain engagement and commitment, particularly in the face of delays and resource constraints, ensuring the sustained progress of WPV initiatives. |
• Hughes, 2021 • Sirkin et al., 2005 • Day et al., 2017 • Raza et al., 2023 • Ziółkowski et al., 2006 |
This relates to the approach taken for the systems level QI project. |
| 8 | Connect with the Community | In addressing WPV, it was crucial to include patients, chosen family members, and visitors, as they experience various stressors during healthcare visits that can trigger stress responses, minority stress, and responsive behaviour, potentially leading to WPV incidents. A trauma-informed and inclusive approach is necessary to create a safe environment for these groups. Engaging with these groups through surveys, advisory boards, and involvement in developing initiatives offers valuable perspectives on WPV. It is essential to foster meaningful and authentic engagement to avoid feelings of under appreciation or tokenism among patients. |
• Muskett, 2014 • Beattie et al., 2019 • Schulz-Quach et al., 2023 • Ashworth et al., 2023 • Armstrong et al., 2013 • Baker et al., 2016 • McNeill et al., 2020 |
SP12. Patient partners and community outreach |
| 9 | Implement a Cohesive and Clear Communication Strategy | Effective organizational communication is crucial for the success of WPV QI initiatives. Clear and cohesive communication from leadership helps staff understand the organization's direction, which enhances HCP buy-in and engagement. Inconsistent communication can lead to rumours and create divisions that undermine cohesiveness and trust. Successful WPV initiatives can be shared through various channels, including newsletters, emails, websites, meetings, and leadership updates. Utilizing existing communication strategies increases effectiveness, and establishing a communication channel between site managers and the WPV QI team allows for valuable site-specific feedback. |
• Boan & Funderburk, 2003 • Brown, 2020 • Seijts & Crim, 2006 • Simmonds, 2006 • Agency for Healthcare Research and Quality, 2017 • Kellogg et al., 2017 |
SP9. Implementing Environmental Indicators for harm reduction and risk minimization |
| 10 | Implement Data Monitoring and Utilize Statistics for Planning/Management Decisions | Measuring changes in regions of interest related to WPV over time is essential for assessing the impact of WPV QI initiatives. However, current WPV metrics in healthcare often focus solely on outcome indicators, such as the frequency of documented incidents, which are problematic due to the historical underreporting of WPV. To effectively monitor WPV, healthcare institutions need a broader set of quality indicators that encompass structure, process, and outcome measures, providing a comprehensive view of WPV within the organization. |
• Keith & Brophy, 2021 • Lyver et al., 2024 • Sethi et al., 2024 • Byon et al., 2022 • Itri et al., 2017 |
SP2. Identifying quality indicators for measuring change in quality of care related to Code White and WPV incidences SP3. Implementing quality indicators to an organization-wide WPV dashboard |
| 11 | Improve Debriefing and Reporting | Improving debriefing and reporting protocols in healthcare institutions enhances HCP well-being and organizational culture, which are vital for increasing buy-in and incident reporting. Effective debriefing minimizes adverse outcomes by providing support and validation without placing blame. Addressing the underreporting of WPV, a consistent issue in healthcare, requires a robust, accessible reporting system that minimizes staff workload and includes follow-up communication. Education and debriefing interventions should promote these reporting systems to foster a culture of reporting, ensuring staff feel supported and cared for. |
• Shanafelt et al., 2020 • Antai-Otong, 2001 • Fricke et al., 2023 • Juarez, 2021 • Rodrigues et al., 2021 • Arnetz, 2022 • Johnson, n.d. • Thomas et al., 2021 |
SP7. Reviewing, updating and implementing incident reporting for WPV and Code White incidents SP10. Code White hot and cold debriefing process and debriefing escalation algorithm |
| 12 | Implement Comprehensive Training Plan based on HCP’s Environmental Risks | Implementing a new or updated training plan tailored to staff needs is essential for addressing WPV in healthcare. Effective training enhances WPV management, increases staff safety, and fosters a culture of safety within the organization. Training should encompass simulation and education programs focused on WPV awareness, de-escalation, agitation management, decision-making, crisis intervention, and conflict resolution. Since factors such as department, patient interaction frequency, and WPV concerns influence the likelihood of involvement in incidents, training should be based on risk profiles rather than solely on profession. This approach fosters interdisciplinary understanding, enhances interprofessional communication, and improves teamwork. |
• Keith & Brophy, 2021 • Beech & Leather, 2006 • Martinez, 2017 • Alafean & Dalahmeh, 2022 • Liu et al., 2020 • Walton et al., 2019 |
SP5. Implementation of educational intervention I SP8. Implementation of educational intervention II |
Step 1: define the problem and find the data
WPV quality improvement projects begin with properly defining the problem and finding reviewing the available data. Identifying the root causes of problems is critical to preventing issues from reoccurring. There are multiple problem-analysis methods to define problems such as the Ishikawa fishbone diagram or root cause analysis [61, 62]. Regardless of the method used, it is important to define the WPV problem, identify barriers, risk factors, contextual factors and facilitators of change [62, 63]. The PETT scan from the SEIPS 101 toolbox provided us with an effective method of investigating the people, environment, tools, tasks and the interactions between them in a work system to assist with defining our WPV problem [59]. The PETT scan is a checklist that encourages users to identify a comprehensive understanding of key elements interacting within the work system, as well as the barriers and facilitators of each work system component. Using these data excavation tools will assist healthcare organizations in identifying where WPV interventions are required. Utilizing SEIPS 101 tools at the commencement of a WPV QI initiative can further be helpful if healthcare institutions lack the data necessary to demonstrate an increase in WPV due to common barrier factors such as underreporting [64].
Step 2: assemble a WPV QI team
An important preliminary step in WPV QI is assembling an effective team. An interdisciplinary team approach supports leveraging diverse perspectives, skillsets, and knowledge of team members with various backgrounds while fostering opportunities for collaboration and creativity necessary for effective WPV quality improvement [61]. When forming a QI team, it's important to consider contextual factors that have been shown to contribute to success including team diversity, physician involvement, subject matter experts, team members with a history of working together, prior experiences and skills with QI, leadership and a sound decision-making process [65, 66]. Assembling a well-rounded QI team mindful of these factors sets the foundation for a successful and collaborative QI initiative addressing WPV in healthcare.
Step 3: listen to frontline Staff
While it is always essential to ensure voices of frontline staff are heard, this becomes particularly crucial when addressing WPV in healthcare. WPV is a demoralizing issue contributing to undesirable patient outcomes, HCP burnout and high turnover rates, thus, making HCPs feel heard on this subject by their own organization can have a positive impact on staff engagement with the WPV QI process [67]. Performing qualitative interviews and collecting data through pulse surveys with frontline staff throughout the project is crucial. HCPs need to be heard, supported, and cared for, and prepared for the envisioned change, and ultimately, be protected within their healthcare settings, as has been discussed in a recent study in the context of the collective impact of the COVID-19 pandemic [68]. WPV-related qualitative data, complementing quantitative data, proves pivotal in addressing intricate issues and guiding WPV QI initiatives [69]. Employing a longitudinal approach supports the identification of lived experience of change, impact or lack thereof overtime [70]. Lastly, meaningful integration of both qualitative and quantitative data enhances the probability of securing key collaborators buy-in [71, 72]. By employing a mixed-methods methodology, teams can combine both quantitative and qualitative data which is often needed to pragmatically address WPV challenges.
Step 4: key collaborator engagement
A critical phase in QI projects involves active engagement with key collaborators. Securing organizational leadership buy-in is a prerequisite for any project success, as it ensures the availability of resources [73]. This includes funding and protected time for team members which is crucial for success in WPV QI projects [74]. Involving leadership is pivotal in creating a cultural change that fosters supportive behaviours of WPV QI initiatives within the organization [65]. Additionally, many WPV QI initiatives, such as training, are ongoing and require ongoing funding commitment. Maintaining engagement of key collaborators is crucial to ensure that these WPV QI initiatives are sustained [75]. Research demonstrates that engaging key collaborators early, maintaining ongoing clear communication with key collaborators and involving key collaborators in project decision making are effective means of maintaining key collaborators involvement and support [76].
Step 5: bringing organizational entities together
With WPV being a systemic concern, collaboration must continue beyond the QI team. In most healthcare institution, several functional units are likely to be involved in processes related to WPV, collaborating with representatives from all functional units involved in these processes is necessary to gain comprehensive problem understanding [61]. Unfortunately, functional units in healthcare institutions often operate with silo effects that compromise efficiency and promote conflict, repeated initiatives and sometimes ineffective use of resources [77]. Silo mentality is particularly harmful to organization-wide QI initiatives such as addressing WPV [78], thus proper communication between hospital departments needs to be established from the start. In our case, when investigating functional units addressing WPV using a people map, eight separate functional units involved in WPV were identified (Table 4). It was imperative that these organizational entities were brought together first before initiating change processes.
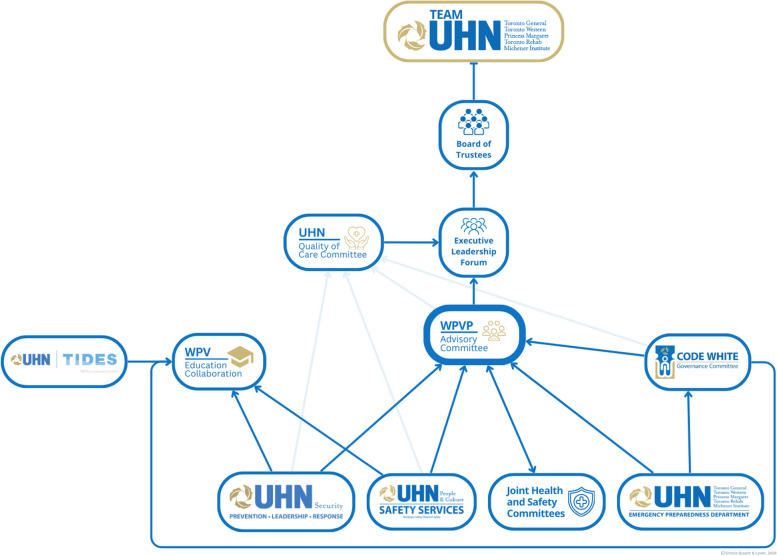
Step 6: implement an effective governance structure
Once all involved partners are identified, an effective WPV governance structure is crucial to project success [79]. This offers the leadership and management essential to prevent conflicts in project implementation, resource management, and ensure sustainability [65]. Given the size and complexity of our organization, multiple governance structures were developed in conjunction with existing departments and committees to ensure the success of a large-scale WPV QI initiative (Fig. 6). The governance structure should include leadership representation from all functional units involved in WPV initiatives or related processes. A charter for rules and roles of each member should include budgeting analysis, goal alignment and prioritization, data sharing for QI, as well as the timeline of projects [80]. Furthermore, it is imperative that the governance framework has the opportunity to present to the senior most executive level of the organization to ensure securing comprehensive organizational endorsement for its initiatives [73].
Fig. 6.
The WPV governance structure implemented at our organization to orchestrate a systemic approach to addressing WPV
Step 7: assess project viability and monitor progress and engagement of functional units
It is imperative to assess viability and monitor project execution by a governance team for multi-level projects to reach successful outcomes [81]. A validated tool can reduce resource waste [82], which is crucial for assessing the viability of a WPV initiative. Additionally, continuous project monitoring is necessary to maintain employee engagement and commitment, factors that can be influenced by burnout [83, 84]. The Boston Consulting Group has developed an efficacious four-element model known as Duration, Integrity, Commitment and Effort (DICE), [82, 85]. This framework can highlight important determinants of program viability such as the duration of the initiative or sub-projects, the integrity and skills of the team, the commitment level of senior executives and front-line key collaborators, and the additional effort required from the workforce. As subprojects will have natural delays and competing resources, strategic resource allocation and monitoring of functional units is crucial to the continuous progression of WPV initiatives.
Step 8: connect with the community
In addition to placing a focus on HCPs and frontline staff, it was important to us to include patients, (chosen) family members and visitors when addressing WPV. Each group is subjected to numerous stressors during visits to a healthcare institution, a multitude of factors that impact their experience at the healthcare institution can trigger stress responses, minority stress and responsive behavior which can increase the probability of WPV events [86]. Trauma-informed care and inclusive lens is a requirement to ensure that patients, (chosen) family members and visitors can feel as safe as possible [9, 87, 88]. Engaging with patients involved in past WPV or Code White incidents provides a different and often complementing perspective of WPV events. However, there exists challenges in reaching out to patients and visitors such as patients feeling underappreciated, unheard and that the gesture is tokenistic [89]. Research has demonstrated that including patient advisors in the development of initiatives, collecting information from patients and visitors on their experiences via surveys and developing patient and visitor advisory boards are effective methods of engaging with patients, (chosen) family members and visitors [90, 91].
Step 9: implement a cohesive and clear communication strategy
Ensuring organizational communication regarding WPV QI initiatives is imperative to project success [92]. Clear and cohesive communication from organizational leadership is essential for ensuring staff members understand the organization's direction, leading to increased HCP buy-in and engagement [93, 94]. A lack of consistency in intra-organizational communication can result in rumours and a divide between individuals or groups with knowledge and without that negatively impacts cohesiveness and organizational trust [95]. WPV QI initiatives and successes can be communicated through organization-wide newsletters, emails, websites, office computer screens, meetings, in-person handouts and leadership communication [96]. Researchers demonstrate utilizing pre-existing organization communication strategies improves effectiveness [97]. Developing a communication stream between site managers and WPV QI team members is another valuable tool that provides the opportunity for managers to provide site-specific feedback on WPV initiatives [97].
Step 10: implement data monitoring and utilize statistics for planning/management decisions
Measuring changes in regions of interest pertaining to WPV overtime is pivotal to monitoring the impact of WPV QI initiatives. However, WPV metrics at healthcare institutions often place an emphasis exclusively on outcome indicators including the frequency of documented WPV incidents [98]. These indicators are problematic as WPV is historically underreported in healthcare [7]. Consequently, healthcare institutions will require a larger set of WPV quality indicators that do not rely solely on staff reporting of incidents to successfully monitor WPV [60]. These quality indicators must include structure, process and outcome measures to capture a comprehensive and systemic perspective on WPV within an organization [8, 99]. In our case example, we performed a rapid review and Delphi process to determine quality indicators that would provide the quantitative data imperative to monitoring WPV QI impact and for informing decision making [60].
Step 11: improve debriefing and reporting
Enhancing debriefing and reporting protocols in healthcare institutions has been demonstrated to improve HCP well-being, and organizational culture [100, 101] both of which are pivotal to increasing HCP buy in and reporting of WPV incidents. Debriefing after WPV incidents minimizes adverse outcomes to staff and provide them with a sense of support, connectedness, and relief following the event [100, 102]. However, debriefing must not leave HCPs feeling blamed or criticized, a positive debrief checks in with staff, validates their feelings and encourages help-seeking when needed [103]. Utilizing a protocol for debriefing after WPV events enhances quality and consistency of debriefs in order to meet the support needs of HCPs [100].
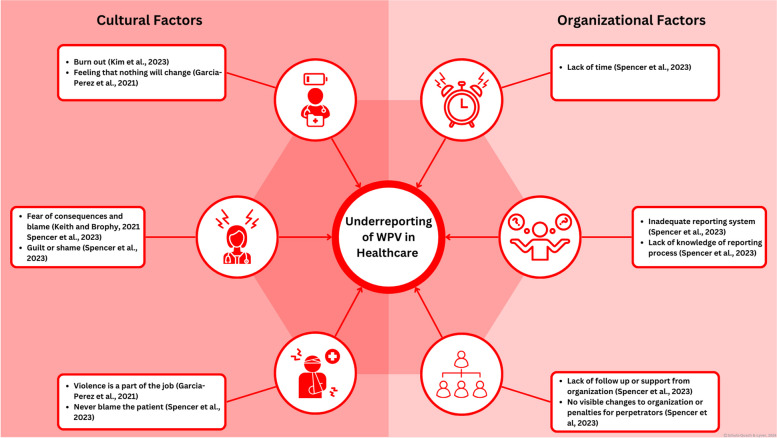
The underreporting of WPV is a culturally and structurally rooted problem faced by healthcare institutions. Research has documented that as many as 88% of HCPs that experienced WPV did not report the event [104]. WPV reporting is crucial to identifying WPV trends and informing decision making processes. A wide array of cultural and organizational factors contributes to underreporting (Fig. 7), many of which can be addressed through an updated WPV reporting system. Staff require a convenient, accessible reporting system that minimizes added workload, provides staff with follow up messages to demonstrate a course of action was taken and provides WPV support resources to ensure that staff feel seen, heard, supported, protected, and cared for [68, 105]. Education interventions and debriefs must encourage the use of WPV reporting systems to create a culture of reporting.
Fig. 7.
This figure depicts the numerous cultural and organizational factors contributing to the underreporting of WPV in healthcare. References related to [7, 53, 106, 107]
Step 12: implement comprehensive training plan based on HCP’s environmental risks
Implementing a new or updated training plan that meets the needs of their staff is a crucial step in addressing WPV in healthcare [108]. Effective WPV prevention training improves the management of WPV situations, increases staff’s sense of safety and promotes a culture of safety within the organization [109]. Training must include simulation and education programs that focus on WPV awareness, verbal and physical de-escalation, agitation management, decision making, critical thinking, crisis intervention training and conflict resolution to be effective [7, 110]. Research indicates that factors such as an employee's department, frequency of patient interactions, and concerns regarding WPV are key contributors to the likelihood of their involvement in a WPV incident [111]. Consequently, staff’s training requirements need to be determined by generating risk profiles that consider these factors rather than relying solely on professions as a determining factor of needs. Utilizing risk profiles for training will lead to interdisciplinary cohorts that will enhance staff’s understanding of other roles, interprofessional communication and teamwork [112]. In our case example at our organizations, criteria for risk level stratification were based upon an environmental assessment of each unit.
Limitations
Although the development of our QI project emphasized the utilization of a systemic, methodological approach, there are several limitations that require acknowledgement. It is important to note that the objective of this paper is to illustrate the development of a systemic WPV QI project, rather than its success. Consequently, this article lacks data to demonstrate the effectiveness of the interventions. Our team is in the process of publishing findings of the individual subprojects.
An additional limitation of the framework is its limited generalizability. The subprojects are specific to our healthcare institution, shaped by resources and processes unique to our situation. For example, not all healthcare institutions utilize the Code White response protocol or manage WPV incidents using physical restraint systems. Furthermore, the timing of this project’s initiation during the COVID-19 pandemic recovery phase may have influenced our findings. The global surge in WPV during this period created a distinctive environment [3, 4], which may limit the applicability of the framework in other healthcare settings. Moreover, sustainability of large-scale QI projects is difficult due to interventions, such as education and training, requiring ongoing funding and key collaborators support.
Conclusions
In conclusion, WPV is a multifactorial and complex phenomenon in healthcare which ought to be addressed through complex interventions and a systems approach. Through the utilization of the SEIPS 3.0 framework and SEIPS 101 tools, our team developed such an approach to address WPV at a multi-site academic health sciences centre in Toronto, Ontario. In addition, we have developed a framework outlining the necessary steps that we undertook in developing our own project. This framework can be utilized by healthcare institutions to aid in establishing a comprehensive WPV QI project within their own settings. Future research should focus on factors that optimize WPV QI engagement and intervention impact on the organizational level.
Supplementary Information
Acknowledgements
We would like to thank our colleagues for their contribution to the content of this article: the members of the Workplace Violence Prevention Advisory Committee, the members of the Code White Governance Committee and the members of the Workplace Violence Education Collaboration.
Abbreviations
- WPV
Workplace violence
- ED
Emergency Department
- QI
Quality improvement
- SPO
Structure-Process-Outcome
- HCP
Healthcare Provider
- SEIPS
System Engineering Imitative for Patient Safety
- PETT
People, Environment, Tools, Tasks
- SP
Subproject
- DICE
Duration, Integrity, Commitment and Effort
Authors’ contributions
C. S.-Q. provided substantial contributions to the conception and design of the quality improvement project, the acquisition, analysis and interpretation of the quality improvement subprojects, and the conception and design of the framework. C.S.-Q. contributed to drafting the work and preparing all figures and tables. C.S.-Q. reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work; C.S.-Q. has shared first authorship. B.L. provided substantial contributions to the conception and design of the quality improvement project, the acquisition, analysis and interpretation of the quality improvement subprojects, and the conception and design of the framework. B.L. contributed to drafting the work and preparing all figures and tables. B.L. reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work; B.L. has shared first authorship. C.R. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. T.H. provided substantial contributions to the conception of the quality improvement project, the acquisition, analysis and interpretation of the quality improvement subprojects, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. J.H. provided substantial contributions to the conception of the quality improvement project, the acquisition, analysis and interpretation of the quality improvement subprojects, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. J.S. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. L.D.P. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. J.G. provided substantial contributions to the conception of the quality improvement project, the analysis and interpretation of the quality improvement subprojects, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. B.S. provided substantial contributions to the conception of the quality improvement project, the acquisition, analysis and interpretation of the quality improvement subprojects, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. Y.S. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. S.S. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. S.E. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. N.B. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. L.B.C. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. M.E. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. D.E. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. M.T. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. B.H. provided substantial contributions to the conception of the quality improvement project, reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. R.S. provided substantial contributions to the conception and design of the quality improvement project, the acquisition, analysis and interpretation of the quality improvement subprojects, and the conception and design of the framework. R.S. contributed to drafting the work. R.S. reviewed the framework manuscript critically for important intellectual content, provided final approval of the version to be published and agreed to be accountable for all aspects of the work. All authors have read and approved the final manuscript.
Funding
This work was supported by the UHN Quality Improvement Physicians Grant.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
C.S.-Q. has received education scholarship support from Academic Scholars Award, Department of Psychiatry, University of Toronto, and Young Leaders Program and Cancer Experience Program, Princess Margaret Cancer Center, University Health Network and the Quality Improvement Physicians Grant, University Health Network. He is on the board of directors for the Canadian Academy for Consultation and Liaison Psychiatry. He is the Provincial Quality Lead Psychiatry – Psychosocial Oncology at Ontario Health, Ontario, Canada. B. L. has received support from the Quality Improvement Physicians Grant, University Health Network. C. R. has nothing to declare. T. H. has nothing to declare. J. H. has nothing to declare. J.S. has nothing to declare. L.D.P. has nothing to declare. Y.S. has nothing to declare. S.S. has nothing to declare. S.E. has nothing to declare. N.B. has nothing to declare. J.G. has received support from the Quality Improvement Physicians Grant, University Health Network. B. S. has received support from the Quality Improvement Physicians Grant, University Health Network. L.B.C. has nothing to declare. M.E. has nothing to declare. D.E. has nothing to declare. M.T. is on the board of Health Insurance Reciprocal of Canada. B.H. has nothing to declare. R.S. has received support from the Quality Improvement Physicians Grant, University Health Network.
B. L. has received support from the Quality Improvement Physicians Grant, University Health Network.
C. R. has nothing to declare.
T. H. has nothing to declare.
J. H. has nothing to declare.
J.S. has nothing to declare.
L.D.P. has nothing to declare.
Y.S. has nothing to declare.
S.S. has nothing to declare.
S.E. has nothing to declare.
N.B. has nothing to declare.
J.G. has received support from the Quality Improvement Physicians Grant, University Health Network.
B. S. has received support from the Quality Improvement Physicians Grant, University Health Network.
L.B.C. has nothing to declare.
M.E. has nothing to declare.
D.E. has nothing to declare.
M.T. is on the board of Health Insurance Reciprocal of Canada.
B.H. has nothing to declare.
R.S. has received support from the Quality Improvement Physicians Grant, University Health Network.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Christian Schulz-Quach and Brendan Lyver share the first Authorship.
References
- 1.Caruso R, Toffanin T, Folesani F, Biancosino B, Romagnolo F, Riba MB, et al. Violence against physicians in the workplace: trends, causes, consequences, and strategies for intervention. Curr Psychiatry Rep. 2022;24(12):911–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schulz-Quach C, Gorla J, Reynolds C, Sethi R, Lyver B. The life cycle of a code white: a framework for managing workplace violence. NEJM Catalyst. 2024;5(3):CAT.23.0352. [Google Scholar]
- 3.McGuire SS, Gazley B, Majerus AC, Mullan AF, Clements CM. Impact of the COVID-19 pandemic on workplace violence at an academic emergency department. Am J Emerg Med. 2022;53:285.e1–e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brigo F, Zaboli A, Rella E, Sibilio S, Canelles MF, Magnarelli G, et al. The impact of COVID-19 pandemic on temporal trends of workplace violence against healthcare workers in the emergency department. Health Pol. 2022;126(11):1110–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Somani R, Muntaner C, Hillan E, Velonis AJ, Smith P. A systematic review: effectiveness of interventions to de-escalate workplace violence against nurses in healthcare settings. Saf Health Work. 2021;12(3):289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim MC, Jeffree MS, Saupin SS, Giloi N, Lukman KA. Workplace violence in healthcare settings: The risk factors, implications and collaborative preventive measures. Ann Med Surg (Lond). 2022;78:103727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keith M, Brophy J. Code white: sounding the alarm on violence against healthcare workers. Toronto, Ontario: Between the Lines. 2021.
- 8.Lyver B, Gorla J, Schulz-Quach C, Anderson M, Singh B, Hanagan T, et al. Identifying quality indicators to measure workplace violence in healthcare settings: a rapid review. BMC Emerg Med. 2024;24(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashworth H, Lewis-O’Connor A, Grossman S, Brown T, Elisseou S, Stoklosa H. Trauma-informed care (TIC) best practices for improving patient care in the emergency department. Int J Emerg Med. 2023;16(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flowerdew L, Brown R, Russ S, Vincent C, Woloshynowych M. Teams under pressure in the emergency department: an interview study. Emerg Med J. 2012;29(12):e2–e. [DOI] [PubMed] [Google Scholar]
- 11.Sanders J, Thomas L, Kerr T, Benita T, Abela K, Ulrich B. Interventions to prevent and mitigate workplace violence: teaming up for a safer environment. Nurs Manage. 2023;54(8):20–30. [DOI] [PubMed] [Google Scholar]
- 12.Oztermeli AD, Oztermeli A, Şancı E, Halhallı HC. Violence in the emergency department: What can we do? Curēus (Palo Alto, CA). 2023;15(7):e41909–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartley D, Ridenour M, Craine J, Morrill A. Workplace violence prevention for nurses on-line course: program development. Work (Reading, Mass). 2015;51(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abbas M, Aloudat T, Bartolomei J, Carballo M, Durieux-Paillard S, Gabus L, et al. Migrant and refugee populations: a public health and policy perspective on a continuing global crisis. Antimicrob Resist Infect Control. 2018;7(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chirico F, Afolabi AA, Ilesanmi O, Nucera G, Ferrari G, Szarpak L, et al. Workplace violence against healthcare workers during the COVID-19 pandemic: a systematic review. J Health Soc Sci. 2022;7(1):14–35. [Google Scholar]
- 16.He Y, Holroyd E, Koziol-McLain J. Understanding workplace violence against medical staff in China: a retrospective review of publicly available reports. BMC Health Serv Res. 2023;23(1):660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.UçAr YG, Kuş C, Gümüştakim RŞ, Eryilmaz ME. The approach of society regarding the violence against healthcare providers. Interdiscipl Med J. 2023;14(49):117–25. [Google Scholar]
- 18.Joyce A, Pellatt R, Ranse J, Doumany A, Hall E, Sweeny A, et al. Occupational violence in a tertiary emergency department: a retrospective descriptive study. Australas Emerg Care. 2023;26(4):346–51. [DOI] [PubMed] [Google Scholar]
- 19.McPhaul KM, London M, Murrett K, Flannery K, Rosen J, Lipscomb J. Environmental evaluation for workplace violence in healthcare and social services. J Safety Res. 2008;39(2):237–50. [DOI] [PubMed] [Google Scholar]
- 20.Morphet J, Griffiths D, Beattie J, Innes K. Managers’ experiences of prevention and management of workplace violence against health care staff: a descriptive exploratory study. J Nurs Manag. 2019;27(4):781–91. [DOI] [PubMed] [Google Scholar]
- 21.Blando JD, Ridenour ML, Hartley D. Surveys of workplace violence perceptions, prevention strategies, and prevalence of weapons in healthcare facilities. J Healthc Protect Manag. 2020;36(2):76–87. [PMC free article] [PubMed] [Google Scholar]
- 22.Ramacciati N, Ceccagnoli A, Addey B, Lumini E, Rasero L. Violence towards emergency nurses: a narrative review of theories and frameworks. Int Emerg Nurs. 2018;39:2–12. [DOI] [PubMed] [Google Scholar]
- 23.Levin PF, Hewitt JB, Misner ST. Insights of nurses about assault in hospital-based emergency departments. Image J Nurs Schol. 1998;30(3):249–54. [DOI] [PubMed] [Google Scholar]
- 24.Levin PF, Hewitt JB, Misner ST, Reynolds S. Assault of long-term care personnel. J Gerontol Nurs. 2003;29(3):28–35. [DOI] [PubMed] [Google Scholar]
- 25.Hesketh KL, Duncan SM, Estabrooks CA, Reimer MA, Giovannetti P, Hyndman K, et al. Workplace violence in Alberta and British Columbia hospitals. Health Pol. 2003;63(3):311–21. [DOI] [PubMed] [Google Scholar]
- 26.Early MR, Hubbert AO. Violence in the emergency department: a culture care perspective. J Nurs Theory. 2006;15(3):3–10. [Google Scholar]
- 27.Landau SF, Bendalak Y. Personnel exposure to violence in hospital emergency wards: a routine activity approach. Aggr Behav. 2008;34(1):88–103. [DOI] [PubMed] [Google Scholar]
- 28.Henson B. Preventing interpersonal violence in emergency departments: practical applications of criminology theory. Violence Vict. 2010;4:553–65. [DOI] [PubMed] [Google Scholar]
- 29.Lau JBC, Magarey J, Wiechula R. Violence in the emergency department: an ethnographic study (part II). Int Emerg Nurs. 2012;20(3):126–32. [DOI] [PubMed] [Google Scholar]
- 30.Honneth A. The struggle for recognition: The moral grammar of social conflicts. Cambridge: MIT Press; 1996.
- 31.Morken T, Alsaker K, Johansen IH. Emergency primary care personnel’s perception of professional-patient interaction in aggressive incidents – a qualitative study. BMC Fam Pract. 2016;17(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ferns T. Considering theories of aggression in an emergency department context. Accid Emerg Nurs. 2007;15(4):193–200. [DOI] [PubMed] [Google Scholar]
- 33.Freud S. Beyond the pleasure principle. London (UK). Psychoanalysis and History. 2015;17(2):151–204.
- 34.Glass DC. Behavior patterns, stress, and coronary disease. Oxford, England: Lawrence Erlbaum; 1977. xi, 217-xi, p.
- 35.Holmes DS, Will MJ. Expression of interpersonal aggression by angered and nonangered persons with the type A and type B behavior patterns. J Pers Soc Psychol. 1985;48(3):723–7. [DOI] [PubMed]
- 36.Snyder M. Self-monitoring of expressive behavior. J Pers Soc Psychol. 1974;30(4):526–37. [Google Scholar]
- 37.Dodge KA, Coie JD. Social-information-processing factors in reactive and proactive aggression in children’s peer groups. J Pers Soc Psychol. 1987;53(6):1146–58. [DOI] [PubMed] [Google Scholar]
- 38.Eysenck HJ, Gudjonsson GH. The causes and cures of criminality. New York: Plenum Press; 1989. Available from: 10.1007/978-1-4757-6726-1.
- 39.Harrower J. Applying psychology to crime. Abingdon: Hodder & Stoughton; 1998. p. 239.
- 40.Berkowitz L. On the formation and regulation of anger and aggression: a cognitive-neoassociationistic analysis. Am Psychol. 1990;45(4):494–503. [DOI] [PubMed] [Google Scholar]
- 41.Baron RA, Bell PA. Sexual arousal and aggression by males: Effects of type of erotic stimuli and prior provocation. J Pers Soc Psychol. 1977;35(2):79. [DOI] [PubMed] [Google Scholar]
- 42.Zillermann D. Cognitive excitation interdependencies in aggressive behaviour. Aggr Behav. 1988;14:51–64. [Google Scholar]
- 43.Elster J. Rational choice. New York: NYU Press; 1986.
- 44.Pyszczynski T, Lockett M, Greenberg J, Solomon S. Terror management theory and the COVID-19 pandemic. J Humanist Psychol. 2021;61(2):173–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.King B. Psychological theories of violence. J Hum Behav Soc Environ. 2012;22(5):553–71. [Google Scholar]
- 46.Wieviorka M. The sociological analysis of violence: new perspectives. Sociol Rev. 2014;62(2_suppl):50–64. [Google Scholar]
- 47.Bhattacharjee D. Workplace violence in healthcare: Towards a psychosocial perspective. Aggress Violent Beh. 2021;58:101573. [Google Scholar]
- 48.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chavis AZ, Hill MS. Integrating multiple intersecting identities: a multicultural conceptualization of the power and control wheel. Women Ther. 2008;32(1):121–49. [Google Scholar]
- 50.Borckardt JJ, Madan A, Grubaugh AL, Danielson CK, Pelic CG, Hardesty SJ, Hanson R, Herbert J, Cooney H, Benson A, Frueh BC. Systematic investigation of initiatives to reduce seclusion and restraint in a state psychiatric hospital. Psychiatr Serv. 2011;62(5):477–83. [DOI] [PubMed] [Google Scholar]
- 51.Hales TW, Nochajski TH, Green SA, Hitzel HK, Woike-Ganga E. An association between implementing trauma-informed care and staff satisfaction. Adv Soc Work. 2017;18(1):300–12. [Google Scholar]
- 52.Yosep I, Mardhiyah A, Hendrawati H, Hendrawati S. Interventions for reducing negative impacts of workplace violence among health workers: a scoping review. J Multidiscip Healthc. 2023;31:1409–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim S, Lynn MR, Baernholdt M, Kitzmiller R, Jones CB. How does workplace violence-reporting culture affect workplace violence, nurse burnout, and patient safety? J Nurs Care Qual. 2023;38(1):11–8. [DOI] [PubMed] [Google Scholar]
- 54.Carayon P, Hundt AS, Karsh B, Gurses AP, Alvarado C, Smith M, et al. Work system design for patient safety: the SEIPS model. BMJ Qual Saf. 2006;15(suppl 1):i50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carayon P, Wooldridge A, Hoonakker P, Hundt AS, Kelly MM. SEIPS 3.0: Human-centered design of the patient journey for patient safety. Appl Ergon. 2020;84:103033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dopelt K, Davidovitch N, Stupak A, Ben Ayun R, Lev Eltsufin A, Levy C. Workplace violence against hospital workers during the COVID-19 pandemic in Israel: implications for public health. Int J Environ Res Public Health. 2022;19(8):4659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. Standards for QUality Improvement Reporting Excellence 2.0: revised publication guidelines from a detailed consensus process. J Surg Res. 2016;200(2):676–82. [DOI] [PubMed] [Google Scholar]
- 59.Holden RJ, Carayon P. SEIPS 101 and seven simple SEIPS tools. BMJ Qual Saf. 2021;30(11):901–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sethi R, Lyver B, Gorla J, Singh B, Hanagan T, Haines J, Toppings M, Schulz-Quach C. Developing a customised set of evidence-based quality indicators for measuring workplace violence towards healthcare workers: a modified Delphi method. BMJ open quality. 2024;13(3):e002855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chung PJ, Baum RA, Soares NS, Chan E. Introduction to quality improvement part one: defining the problem, making a plan. J Dev Behav Pediatr. 2014;35(7):460–6. [DOI] [PubMed] [Google Scholar]
- 62.Cumbler EU, Simpson JR, Rosenthal LD, Likosky DJ. Inpatient falls: defining the problem and identifying possible solutions. Part II: application of quality improvement principles to hospital falls. Neurohospitalist. 2013;3(4):203–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bokhoven MAv, Kok G, Weijden T. Designing a quality improvement intervention: a systematic approach. Qual Saf Health Care. 2003;12(3):215–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mento C, Silvestri MC, Bruno A, Muscatello MRA, Cedro C, Pandolfo G, et al. Workplace violence against healthcare professionals: A systematic review. Aggress Violent Beh. 2020;51:101381. [Google Scholar]
- 65.Kaplan HC, Provost LP, Froehle CM, Margolis PA. The Model for Understanding Success in Quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf. 2012;21(1):13–20. [DOI] [PubMed] [Google Scholar]
- 66.Hulscher ME, Schouten LM, Grol RP, Buchan H. Determinants of success of quality improvement collaboratives: what does the literature show? BMJ Qual Saf. 2013;22(1):19–31. [DOI] [PubMed] [Google Scholar]
- 67.Schulz-Quach C, Lyver B, Li M. Healthcare provider experiences during COVID-19 redeployment. Curr Opin Support Palliat Care. 2022;16(3):144–50. [DOI] [PubMed] [Google Scholar]
- 68.Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133–4. [DOI] [PubMed] [Google Scholar]
- 69.Crowe S, Brown K, Tregay J, Wray J, Knowles R, Ridout DA, et al. Combining qualitative and quantitative operational research methods to inform quality improvement in pathways that span multiple settings. BMJ Qual Saf. 2017;26(8):641–52. [DOI] [PMC free article] [PubMed]
- 70.Calman L, Brunton L, Molassiotis A. Developing longitudinal qualitative designs: lessons learned and recommendations for health services research. BMC Med Res Methodol. 2013;13(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sachdeva R, Williams T, Quigley J. Mixing methodologies to enhance the implementation of healthcare operational research. J Operat Res Soc. 2007;58(2):159–67. [Google Scholar]
- 72.Franco LA, Lord E. Understanding multi-methodology: Evaluating the perceived impact of mixing methods for group budgetary decisions. Omega. 2011;39(3):362–72. [Google Scholar]
- 73.Fryer KJ, Antony J, Douglas A. Critical success factors of continuous improvement in the public sector. TQM Mag. 2007;19(5):497–517. [Google Scholar]
- 74.Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Brandrud AS, Schreiner A, Hjortdahl P, Helljesen GS, Nyen B, Nelson EC. Three success factors for continual improvement in healthcare: an analysis of the reports of improvement team members. BMJ Qual Saf. 2011;20(3):251–9. [DOI] [PubMed] [Google Scholar]
- 76.Guise J-M, O’Haire C, McPheeters M, Most C, LaBrant L, Lee K, et al. A practice-based tool for engaging stakeholders in future research: a synthesis of current practices. J Clin Epidemiol. 2013;66(6):666–74. [DOI] [PubMed] [Google Scholar]
- 77.Alves J, Meneses R. Silos mentality in healthcare services. In 11th Annual Conference of the EuroMed Academy of Business 2018 (Vol. 2018).
- 78.Akmal A, Podgorodnichenko N, Foote J, Greatbanks R, Stokes T, Gauld R. Why is quality improvement so challenging? A viable systems model perspective to understand the frustrations of healthcare quality improvement managers. Health Pol. 2021;125(5):658–64. [DOI] [PubMed] [Google Scholar]
- 79.Derakhshan R, Turner R, Mancini M. Project governance and stakeholders: a literature review. Int J Project Manage. 2019;37(1):98–116. [Google Scholar]
- 80.Jones L, Pomeroy L, Robert G, Burnett S, Anderson JE, Fulop NJ. How do hospital boards govern for quality improvement? A mixed methods study of 15 organisations in England. BMJ Qual Saf. 2017;26(12):978–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hughes R. Chapter 44 tools and strategies for quality improvement and patient safety. Pat Saf Qual Evid-Based Handb Nurs. 2021;3:1–4. [Google Scholar]
- 82.Sirkin HL, Keenan P, Jackson A. The hard side of change management. Harv Bus Rev. 2005;83(10):108. [PubMed] [Google Scholar]
- 83.Day A, Crown SN, Ivany M. Organisational change and employee burnout: the moderating effects of support and job control. Saf Sci. 2017;100:4–12. [Google Scholar]
- 84.Raza MA, Imran M, Rosak-Szyrocka J, Vasa L, Hadi NU. Organizational change and workplace incivility: mediated by stress, moderated by emotional exhaustion. Int J Environ Res Public Health. 2023;20(3):2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ziółkowski B, Drake G, editors. Rolling the DICE® for agile software projects. Extreme Programming and Agile Processes in Software Engineering: 7th International Conference, XP 2006, Oulu, Finland, June 17–22, 2006 Proceedings 7; 2006: Springer.
- 86.Muskett C. Trauma-informed care in inpatient mental health settings: A review of the literature. Int J Ment Health Nurs. 2014;23(1):51–9. [DOI] [PubMed] [Google Scholar]
- 87.Beattie J, Griffiths D, Innes K, Morphet J. Workplace violence perpetrated by clients of health care: A need for safety and trauma-informed care. J Clin Nurs. 2019;28(1–2):116–24. [DOI] [PubMed] [Google Scholar]
- 88.Schulz-Quach C, Kennedy M, Lyver B. Sexual and gender diversity in cancer care and survivorship. Curr Opin Support Palliat Care. 2023;17(1):55–69. [DOI] [PubMed] [Google Scholar]
- 89.Armstrong N, Herbert G, Aveling EL, Dixon-Woods M, Martin G. Optimizing patient involvement in quality improvement. Health Expect. 2013;16(3):e36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Baker GR, Fancott C, Judd M, O’Connor P. Expanding patient engagement in quality improvement and health system redesign: Three Canadian case studies. Healthc Manage Forum. 2016;29(5):176–82. [DOI] [PubMed] [Google Scholar]
- 91.McNeill LH, Wu IHC, Cho D, Lu Q, Escoto K, Harris C. Community outreach and engagement strategies to address breast cancer disparities. Curr Breast Cancer Reports. 2020;12(4):209–15. [Google Scholar]
- 92.Boan D, Funderburk F. Healthcare quality improvement and organizational culture. Delmarva Foundation. 2003;5:1–18. [Google Scholar]
- 93.Brown A. Communication and leadership in healthcare quality governance: findings from comparative case studies of eight public hospitals in Australia. J Health Organ Manag. 2020;34(2):144–61. [DOI] [PubMed] [Google Scholar]
- 94.Seijts GH, Crim D. What engages employees the most or, the ten C’s of employee engagement. Ivey Bus J. 2006;70(4):1–5. [Google Scholar]
- 95.Simonds RJ. Together we can: Strategies for developing cohesive leadership groups in the fire service of New Brunswick: Royal Roads University; 2006.
- 96.Agency for Healthcare Research and Quality. The CAHPS Ambulatory Care Improvement Guide Practical Strategies for Improving Patient Experience; 2017 Available from: https://www.ahrq.gov/sites/default/files/wysiwyg/cahps/quality-improvement/improvement-guide/4-approach-qi-process/cahps-section-4-ways-to-approach-qi-process.pdf
- 97.Kellogg KC, Gainer LA, Allen AS, O’Sullivan T, Singer SJ. An intraorganizational model for developing and spreading quality improvement innovations. Health Care Manage Rev. 2017;42(4):292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Byon HD, Sagherian K, Kim Y, Lipscomb J, Crandall M, Steege L. Nurses’ experience with type II workplace violence and underreporting during the COVID-19 pandemic. Workplace Health Saf. 2022;70(9):412–20. [DOI] [PubMed] [Google Scholar]
- 99.Itri JN, Bakow E, Probyn L, Kadom N, Duong P-AT, Gettle LM, et al. The science of quality improvement. Acad Radiol. 2017;24(3):253–62. [DOI] [PubMed] [Google Scholar]
- 100.Antai-Otong D. Critical incident stress debriefing: a health promotion model for workplace violence. Perspect Psychiatr Care. 2001;37(4):125–32. [DOI] [PubMed] [Google Scholar]
- 101.Fricke J, Siddique SM, Douma C, Ladak A, Burchill CN, Greysen R, et al. Workplace violence in healthcare settings: a scoping review of guidelines and systematic reviews. Trauma Viol Abuse. 2023;24(5):3363–83. [DOI] [PubMed] [Google Scholar]
- 102.Juarez LA. Addressing emergency department nurses’ experiences of workplace violence through the development of a peer-based, post-Code Gray support tool [dissertation on the Internet]. University of California, Davis; 2021. [cited 2024 Dec 3]. Available from: https://escholarship.org/uc/item/70m1z9qj.
- 103.Rodrigues NC, Ham E, Kirsh B, Seto MC, Hilton NZ. Mental health workers’ experiences of support and help-seeking following workplace violence: a qualitative study. Nurs Health Sci. 2021;23(2):381–8. [DOI] [PubMed] [Google Scholar]
- 104.Arnetz JE. The joint commission’s new and revised workplace violence prevention standards for hospitals: a major step forward toward improved quality and safety. Jt Comm J Qual Patient Saf. 2022;48(4):241–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Thomas B, McGillion A, Edvardsson K, O’Meara P, Van Vuuren J, Spelten E. Barriers, enablers, and opportunities for organisational follow-up of workplace violence from the perspective of emergency department nurses: a qualitative study. BMC Emerg Med. 2021;21(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.García-Pérez MD, Rivera-Sequeiros A, Sánchez-Elías TM, Lima-Serrano M. Workplace violence on healthcare professionals and underreporting: Characterization and knowledge gaps for prevention. Enfermería Clínica (English Edition). 2021;31(6):390–5. [DOI] [PubMed] [Google Scholar]
- 107.Spencer C, Sitarz J, Fouse J, DeSanto K. Nurses’ rationale for underreporting of patient and visitor perpetrated workplace violence: a systematic review. BMC Nurs. 2023;22(1):134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Beech B, Leather P. Workplace violence in the health care sector: a review of staff training and integration of training evaluation models. Aggress Violent Beh. 2006;11(1):27–43. [Google Scholar]
- 109.Martinez AJS. Implementing a workplace violence simulation for undergraduate nursing students: a pilot study. J Psychosoc Nurs Ment Health Serv. 2017;55(10):39–44. [DOI] [PubMed] [Google Scholar]
- 110.Aladwan M, Dalahmeh E. Prevention of workplace violence in ED nursing using the implementation of an educational program and a new reporting tool. Clinical Journal of Nursing Care and Practice 2022 6(1);1-8
- 111.Liu Y, Zhang M, Li R, Chen N, Huang Y, Lv Y, et al. Risk assessment of workplace violence towards health workers in a Chinese hospital: a cross-sectional study. BMJ Open. 2020;10(12):e042800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Walton V, Hogden A, Long JC, Johnson JK, Greenfield D. How do interprofessional healthcare teams perceive the benefits and challenges of interdisciplinary ward rounds. J Multidiscip Healthc. 2019;12(null):1023–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its supplementary information files].