Abstract
Background
Blood is a vital medical resource that is sourced from primarily nonremunerated donations. As Taiwan faces an aging population, increasing medical demands pose new challenges to blood resource management. Trend analysis can improve blood supply chain management and allocate blood resources more efficiently and cost-effectively.
Methods
A retrospective review was conducted from 2011–2023 in a teaching hospital to examine the utilization and wastage of blood products. Data were collected from hospital information system and blood wastage reports, categorized by cause, and analyzed via SAS software version 9.3.
Results
The hospital released 424,197 units of blood products, with leukocyte-reduced red blood cells accounting for 140,971 units. The highest annual wastage rate was 0.29% in 2011, and the annual average was 0.08%. Fresh frozen plasma (36.3%), platelet concentrates (15.2%), and cryoprecipitate (14.3%) were the most frequently discarded. Major causes of wastage included excessive or inappropriate orders (22.3%), inability to reissue blood before expiration (16.7%), and incorrect orders (14.6%). Platelet wastage was caused primarily by improper storage, while thawed plasma could not be repurposed. Utilization of leukocyte-reduced blood products has increased, leading to a significant reduction in transfusion reactions from 1.8% in 2011 to 0.6% in 2023.
Conclusions
The study highlights that blood wastage often stems from human error or improper storage conditions. The leading cause of platelet product disposal is incorrect storage temperatures, along with the inability to repurpose thawed plasma for plasma products. Importantly, the increased adoption of prestorage leukocyte-reduced blood products has significantly mitigated transfusion-related reactions. We emphasize that continuous education for healthcare professionals and enhanced inventory monitoring are critical to minimize wastage and enhance transfusion quality.
Keywords: Blood utilization, Aging, Leukocyte reduction, Platelet, Plasma, Wastage
Background
Blood is an essential component of human survival, and blood transfusion plays an indispensable role in life-saving medical intervention. Because blood is perishable, developing nontoxic anticoagulants and preservatives can improve the practicality and safety of blood transfusion for patients who are at risk of life-threatening blood loss. Researchers have yet to identify a substitute for blood; and therefore, blood has high value and is a limited substance. According to the literature, demographic changes are often associated with blood supply shortages [1–3]. Increases in older population and substantial decreases in the annual number of newborns have led to a considerable rise in the proportion of older adults and a decline in the number of blood donors, resulting in a blood supply shortage. Additionally, the global fertility rate has declined from 4.84 in 1950 to 2.23 in 2021 and is expected to further decrease to 1.59 by 2100, leading to a significant shift in age demographics [4]. According to the 2024 global fertility statistics released by the Central Intelligence Agency, Taiwan ranks last worldwide in terms of fertility, with a fertility rate of only 1.11. By 2025, the proportion of older adults in Taiwan is projected to reach 20%, making Taiwan a superaged society. As stated by the Taiwan Blood Services Foundation, the number of individuals aged 17–64 years who are capable of donating blood is projected to decrease by nearly 0.9 million by 2030, and the number of individuals older than 65 years is expected to increase by more than 1 million. These factors are likely to lead to insufficient of blood for transfusions, suggesting a potential blood shortage crisis. As indicated by the 2011–2020 annual report released by the Taiwan Blood Services Foundation, the number of first-time blood donors aged under 24 years has decreased from 117,932 to 69,098, representing a reduction from 15.65% to 11.63% in the proportion of individuals donating decreased [5].
During the COVID-19 pandemic, a substantial increase in blood wastage was observed, which was the result of the cancelation of elective surgeries and other nonurgent medical procedures (Association for the Advancement of Blood and Biotherapies) [6, 7]. This wastage results in a shortage of blood supply, significantly affecting various blood supply services [8] and transfusion procedures, such as massive transfusion protocols, in many hospitals [9]. Given the imbalance between increased blood demands and blood supply shortages, hospitals and health-care facilities should focus on reducing their blood wastage and should establish effective policies for blood component utilization. There is also an ethical dimension to limiting wastages, out of respect for the altruistic gesture of donors. If donors perceive a lack of effort in waste reduction, they may be discouraged from giving, which could heighten the risk of shortages. Worldwide, blood wastage has been reported to range between 0% and 6.7% [10, 11]. Therefore, avoiding blood wastage should be considered a medical, economic, and patient safety challenge in hospital blood bank management. Reducing the amount of wasted blood can reduce costs and save blood products that can be used for patients in need, and identifying the causes of blood wastage can enhance blood management and increase the safety of blood transfusion. The aim of this study is to analyze and explore the causes of blood product wastage, with the primary objective of improving blood product management.
Methods
Steps and regulations for blood supply
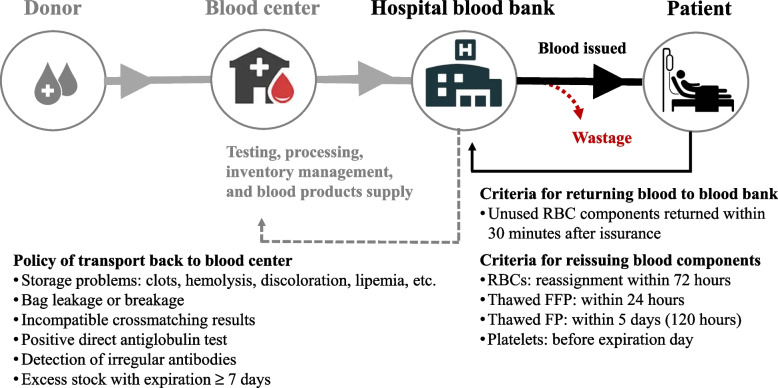
Blood is a valuable resource that is donated by volunteers for use in transfusions to patients in need. Figure 1 depicts the primary blood supply chain and retunes blood policy and criteria in Taiwan. Blood products pass from donors to patients through four steps: donor → blood center → hospital blood bank → patient. The Blood Center of the Taiwan Blood Services Foundation is the only blood provider in Taiwan; it supplies all blood components to Taiwanese hospitals. Among the major blood products supplied by the blood center are: (1) red blood cell (RBC) components, including whole blood (WB), packed RBCs (pRBCs), washed RBCs, and leukocyte-reduced RBCs (LR-RBCs); (2) platelet components, including platelet concentrates, apheresis platelets (phPLTs), and leukocyte-reduced phPLTs (LR-phPLTs); and (3) plasma components, including fresh frozen plasma (FFP), frozen plasmas (FP), and cryoprecipitate (CRYO). In addition, the Blood Center fulfills uncommon blood requests, such as those for human leukocyte antigen or human platelet antigen–matched RBC and platelet products.
Fig. 1.
Blood supply chain and policies for blood return and reissue in the healthcare system
In scenarios in which blood transfusion is not feasible, blood is immediately returned to the blood bank and reassigned to another patient to prevent blood wastage [12]. If these conditions are not met, the blood products should be discarded and should not be reassigned to other patients. When blood products are returned to the blood bank, all bags and containers should be intact and undamaged. For returned blood products to be assigned to other patients, the following conditions must be met. First, unused RBC products should be allowed to settle for 24 h at a controlled temperature (1 °C to 6 °C) and undergo visual inspection before they are reassigned. Second, thawed FFP (4 °C) should be reassigned within 24 h. Third, thawed FP (4 °C) should be reassigned within 5 days. Fourth, platelets (20 °C to 24 °C) should be reassigned before their expiry date.
Key milestones in blood transfusion practice improvement
2012: Updated blood return and re-issuance criteria.
2014: Established temperature monitoring and safety audit protocols.
2016: Promoted pre-storage leukocyte-reduced blood products.
2017: Initiated biannual transfusion safety training for nurses.
2018: Revised emergency and massive transfusion guidelines.
2019: Adopted a one-to-one blood delivery policy.
Data collection
This quantitative, retrospective, cross-sectional, descriptive study was conducted between 2011 and 2023 at Taichung Tzu-Chi Hospital (1,126 beds). All the data collected from the hospital information system (HIS) were deidentified to ensure patient privacy. In this study, we analyzed the trends of utilization for all blood components and explored the primary causes of blood wastage. The hospital’s blood bank is responsible for supplying blood to various departments and units, including the emergency department, internal wards, surgery wards, intensive care units, gynecology and obstetrics wards, chemotherapy and cancer wards, and outpatient clinics. All blood components are requested and documented through the HIS. This information includes the blood group, type of blood component, requested units, issued units, time of issuance, time of blood transfer to the ward or department, and time of transfusion. After laboratory technicians receive a blood transfusion order, they must conduct cross-matching or blood type check procedures in accordance with standard protocols. In the present study, blood wastage was defined as the delivery of nontransfused blood that was not reassigned to another patient or recipient. This information includes the blood group, type of blood components, requested units, issued units, time of issuance, time of blood transfer to the ward or department, and time of transfusion.
Wastage percentage
The following equation was used to calculate the percentage of wastage for each blood product:
Wastage as a percentage of issued products (WAPI) was calculated for each component as follows [11]:
Results
Trend of total blood supply during the study period
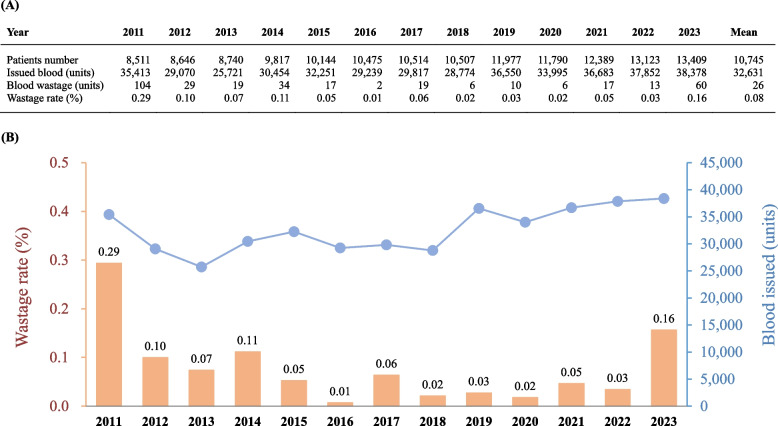
Figure 2A presents the total number of blood components issued and wasted between 2011 and 2023 at Taichung Tzu-Chi Hospital. The number of patients who received blood transfusions increased from 8,511 in 2011 to 13,409 in 2023, with an average of 10,745 patients every year. The average number of blood units issued every year was 32,631, and the average number of wasted blood units every year was 26. Figure 2B depicts blood wastage trends and key milestones in practice improvement.
2012: A notable drop in the wastage rate was observed after reviewing the criteria for blood return and updating re-issuance guidelines. The wastage rate decreased significantly from 0.29% in 2011 to 0.10% in 2012.
2014: The establishment of temperature monitoring systems and transfusion safety audit protocols further contributed to a sustained reduction in blood wastage, reaching 0.05% in 2015.
2016: The promotion of pre-storage leukocyte-reduced blood products maintained the wastage rate at a minimal level, achieving 0.01% in 2016.
2017: The introduction of biannual blood transfusion safety training for nursing staff coincided with a stable low wastage rate.
2019: A one-to-one blood delivery policy was implemented, further supporting wastage reduction. The wastage rates remained around 0.02% in both 2019 and 2020.
Fig. 2.
Trends in blood supply and wastage rates at Taichung Tzu-Chi Hospital from (2011–2023). A Annual data includes patient numbers, blood units issued, blood units wasted, and wastage rate (%). B The chart combines a line graph (right y-axis) for blood units issued and a bar graph (left y-axis) for wastage rates
These measures collectively demonstrate a proactive and data-driven approach to minimizing blood wastage. Despite a slight increase in recent years, with the wastage rate rising to 0.16% in 2023, likely due to increased demand and utilization, the overall trend underscores the effectiveness of these targeted interventions. Efforts to further optimize strategies are ongoing to address emerging challenges.
Utilization and wastage of blood products
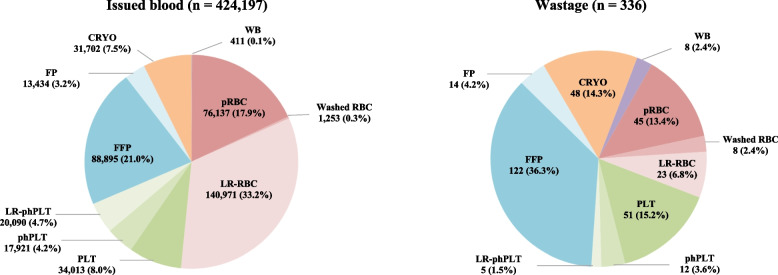
During the study period, 424,197 units of blood products were released by the hospital’s blood bank (Table 1). These blood components included RBC components (411 units of WB, 76,137 units of pRBCs, 1,253 units of washed RBCs, and 140,971 units of LR-RBCs), platelet components (34,013 units of platelet concentrates, 17,921 units of phPLT, and 20,090 units of LR-phPLT), and plasma components (88,895 units of FFP, 13,434 units of FP, and 31,072 units of CRYO). The rates of blood component wastage (WAPI) were expressed as the ratio of discarded blood components to issued blood components. Wastage rates of 0.04%, 0.09%, and 0.14% were recorded for RBC, platelet, and plasma components, respectively. Among them, plasma components have the highest waste rate of blood components (0.14%), and whole blood has the highest waste rate (1.95%) of blood products.
Table 1.
Total number of blood components issued and the wastage of blood units during this study
| Blood products | RBC components | Platelet components | Plasma components | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 218,772 | n = 72,024 | n = 133,401 | |||||||||
| WB | pRBC | Washed RBC | LR-RBC | Platelets | phPLT | LR-phPLT | FFP | FP | CRYO | ||
| Blood issue (unit) | 411 | 76,137 | 1,253 | 140,971 | 34,013 | 17,921 | 20,090 | 88,895 | 13,434 | 31,072 | 424,197 |
| Blood wastage (unit) | 8 | 45 | 8 | 23 | 51 | 12 | 5 | 122 | 14 | 48 | 336 |
| Wastage of blood product (%) | 1.95 | 0.06 | .06 | 0.01 | 0.15 | 0.07 | 0.02 | 0.14 | 0.10 | 0.15 | |
| WAPI (%) | 0.04 | 0.09 | 0.14 | 0.08 | |||||||
One unit of whole blood contains 250 mL
WB Whole blood, pRBC Packed red blood cells, LR Leukocyte-reduced, phPLT Apheresis platelets, LR-phPLT Leukocyte-reduced apheresis platelets, FFP Fresh-frozen plasma, FP Frozen plasma, CRYO Cryoprecipitate
Figure 3 illustrates the utilization and wastage percentages of various blood components. Among the issued blood components (n = 424,197), leukocyte-reduced red blood cells (LR-RBC) were the most utilized (33.2%, 140,971 units), followed by fresh frozen plasma (FFP, 21.0%, 88,895 units) and packed red blood cells (pRBC, 17.9%, 76,137 units). Platelet components collectively accounted for 16.9%, while cryoprecipitate (CRYO), fresh plasma (FP), washed red blood cells (washed RBC), and whole blood (WB) made up smaller proportions. In terms of wastage (n = 336), FFP had the highest rate (36.3%, 122 units), followed by platelet concentrates (PLT, 15.2%, 51 units), CRYO (14.3%, 48 units), and pRBC (13.4%, 45 units). LR-RBC (6.8%, 23 units) and pooled platelets (phPLT, 3.6%, 12 units) had moderate wastage rates, while washed RBC, WB (2.4% each, 8 units), and leukocyte-reduced apheresis platelets (LR-phPLT, 1.5%, 5 units) had the lowest rates. These findings underscore the predominance of LR-RBC in utilization and the high wastage of FFP, highlighting the need for strategies to minimize wastage of frequently used components.
Fig. 3.
Blood component utilization and wastage distribution in the teaching hospital (2011–2023). The left chart shows the proportions of issued blood components by category (n = 424,197), while the right chart presents the wastage rates of different blood components (n = 336). Abbreviations: WB, whole blood; pRBC, packed red blood cells; LR-RBC, leukocyte-reduced red blood cells; PLT, platelet concentrate; phPLT, apheresis platelets; LR-phPLT, leukocyte-reduced apheresis platelets; FFP, fresh frozen plasma; FP, frozen plasma; CRYO, cryoprecipitate
Causes of blood wastage
In this study, we analyzed the clinical utilization and wastage rates of all the blood components. Table 2 lists the 111 events that resulted in 336 units of blood wastage. Our analysis shows that excessive ordering due to inaccurate assessments of patient conditions was the primary cause of blood wastage, responsible for 75 units (22.3%) across 18 events (16.2%). This was followed by the inability to reissue blood units to other patients before their usability period expired, which led to 56 wasted units (16.7%) across 19 events (17.1%). Other significant causes included ordering errors (49 units, 14.6%) and cases where patients died or were discharged before transfusion (32 units, 9.5%). When examining individual blood components, we found that platelet units were particularly vulnerable to wastage due to improper storage temperatures, with 29 units (8.6%) lost for this reason. Additionally, accidental piercing of blood bags led to the wastage of 26 units (7.7%) across 19 events (17.1%), and 28 units (8.3%) were discarded due to expiration before use. These findings suggest that focusing on reducing specific types of events—such as excessive ordering and improper storage—could significantly impact overall blood wastage, as a smaller proportion of events accounted for a large portion of wasted units. This highlights the need for targeted improvements in inventory control, ordering accuracy, and storage compliance to prevent unnecessary wastage.
Table 2.
Analysis of blood component wastage: causes, frequency, and distribution across blood components
| Causes of blood wastage | Events n (%) | RBC components | Platelet components | Plasma components | Total units | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WB | pRBC | Washed RBC | LR-RBC | Platelets | phPLT | LR-phPLT | FFP | FP | CRYO | n (%) | |||
| Excessive ordering/inappropriate patient evaluation | 18 (16.2%) | 0 | 12 | 2 | 0 | 27 | 0 | 0 | 30 | 4 | 0 | 75 (22.3%) | |
| Unable to reissue before usability period | 19 (17.1%) | 0 | 11 | 6 | 0 | 0 | 0 | 1 | 26 | 2 | 10 | 56 (16.7%) | |
| Blood component order errors | 12 (10.8%) | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 22 | 0 | 24 | 49 (14.6%) | |
| Patient death/discharge before transfusion | 7 (6.3%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 18 | 2 | 12 | 32 (9.5%) | |
| Incorrect platelet storage temperature | 7 (6.3%) | 0 | 0 | 0 | 0 | 24 | 5 | 0 | 0 | 0 | 0 | 29 (8.6%) | |
| Expired blood | 10 (9.0%) | 8 | 5 | 0 | 0 | 0 | 2 | 2 | 11 | 0 | 0 | 28 (8.3%) | |
| Accidental blood bag puncture | 19 (17.1%) | 0 | 14 | 0 | 3 | 0 | 5 | 2 | 0 | 2 | 0 | 26 (7.7%) | |
| Excessive warming of blood components | 10 (9.0%) | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 14 | 4 | 2 | 21 (6.3%) | |
| Accidental blood bag breakage | 5 (4.5%) | 0 | 0 | 0 | 8 | 0 | 0 | 0 | 1 | 0 | 0 | 9 (2.7%) | |
| Blood kept at room temperature for over 4 hours | 1 (0.9%) | 0 | 0 | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 6 (1.8%) | |
| No intravenous access | 1 (0.9%) | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 (0.6%) | |
| Partial clotting of blood | 1 (0.9%) | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 2 (0.6%) | |
| Incorrect transfusion procedure | 1 (0.9%) | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (0.3%) | |
| Total | 111 (100.0%) | 8 | 45 | 8 | 23 | 51 | 12 | 5 | 51 | 12 | 5 | 336 (100.0%) | |
One unit of whole blood contains 250 mL
WB Whole blood, pRBC Packed red blood cells, LR Leukocyte-reduced, phPLT Apheresis platelets, LR-phPLT Leukocyte-reduced apheresis platelets, FFP Fresh-frozen plasma, FP Frozen plasma, CRYO Cryoprecipitate
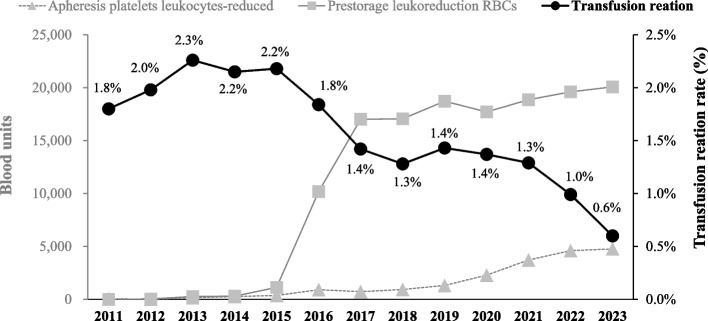
Utilization trends of prestorage leukocyte-reduced blood products
Since 2014, the Blood Center of the Taiwan Blood Services Foundation has been responsible for supplying leukocyte-reduced blood components to all medical facilities. In 2017, our hospital began utilizing LR-RBCs for clinical use. Since 2016, many facilities have transitioned from using pRBCs to prestorage LR-RBCs and LR-phPLTs. The shift was accompanied by a significant decline in transfusion reactions in our hospital, particularly between 2015 and 2017. Figure 4 illustrates the trends in transfusion reaction rates alongside the utilization of prestorage LR-RBCs and LR-phPLTs from 2011 to 2023. During this period, transfusion reaction rates decreased markedly, from 1.8% in 2011 to 0.6% in 2023. The decline became more pronounced after 2015, aligning with the increased implementation of prestorage leukoreduction for RBCs. By 2023, the use of prestorage LR-RBCs had exceeded 20,000 units annually. Similarly, the utilization of LR-phPLTs steadily increased, reflecting the growing adoption of this practice. These findings underscore the role of leukoreduction in improving transfusion safety and reducing adverse reactions.
Fig. 4.
Trends in transfusion reaction rates and leukocyte-reduced blood component utilization (2011–2023)
Discussion
In this study, we analyzed trends in blood utilization and identified the causes of blood wastage in clinical practice in Taiwan. The management of the blood supply chain is considered vital. Over the past decade, we have implemented several management approaches and education courses that have led to a low rate of blood wastage. To effectively utilize blood products and reduce their wastage, the Blood Center and hospital blood banks jointly established several criteria for inventory management (Fig. 1). These criteria ensure that excess or nontransfused blood products are returned to the blood bank for reassignment to other patients. We examined the utilization trends of blood products in a hospital between 2011 and 2023 and explored the causes of blood product wastage. As indicated in Fig. 2, our hospital had an annual average wastage rate of 0.08%, which is relatively low. Previous studies have reported blood wastage rates ranging from 0.2% to 7% [13, 14]. The rate of blood wastage decreased from 0.29% in 2011 to 0.10% in 2012, reaching 0.01% in 2016.
The Blood Transfusion Management Committee is responsible for ensuring safe transfusion practices and implementing patient management initiatives. The committee plays a key role in guaranteeing the safety and appropriateness of blood transfusions for patients at our hospital. In addition to routinely monitoring blood wastage as an indicator of quality, proactive measures should be implemented to identify the factors contributing to such wastage. This can aid in establishing an effective blood management system for reducing blood wastage. Over the past decade, our hospital has established several protocols for blood management, including (1) inviting clinical physicians who have misused or discarded blood products to present reports and engage in discussions with the committee, helping to strengthen blood product management; (2) limiting the transfer of RBC products from the blood bank to the ward to one bag at a time, preventing excessive requests, incorrect orders, or unnecessary rewarming; and (3) using cooling containers or tote bags to transport various blood products, accompanied by a portable thermometer to monitor storage temperature throughout the journey. This prevents these products from being exposed to room temperature for too long, thereby safeguarding their integrity.
Disseminating information on transfusion practices and educating medical staff and nurses may reduce blood wastage [10, 15]. At our hospital, blood wastage is caused in part by nurses inadvertently piercing blood bags during transfusion procedures. To address this issue, we conduct transfusion courses for all clinicians and nurses at least twice a year and provide them with information on how to avoid piecing blood bags. Although limited evidence is available regarding the effectiveness of continuing education in reducing blood wastage, at our institution, such education has led to a reduction in blood wastage rates over the past decade. This suggests that raising awareness about blood wastage and providing ongoing education on transfusion practices to clinicians and nurses can increase vigilance and help prevent it.
Good inventory management is essential for ensuring that the supply of blood components and products meets patients’ transfusion needs while minimizing wastage. Blood inventory management is a complex process that requires coordination between a central blood supply center and blood banks to balance supply and demand. The main goal of the blood bank is to reduce blood wastage while maintaining a sufficient inventory of blood products for patients. Blood product management involves various aspects, including external factors such as communication between the blood donation center and the hospital, delays in blood product delivery, and insufficient blood supply at the blood donation center. Internal factors include delayed delivery of blood products, insufficient inventory in the hospital, incorrect temperatures, improper rewarming of blood products, excessive blood orders, and personnel unfamiliar with blood transfusion operations. Striking a balance between blood component utilization and storage in the hospital blood bank is essential [16]. Excessive stock of blood products can lead to expiration and is one of the causes of blood wastage [6, 17]. To avoid stock excess and shortages, our blood bank uses fixed stock units of blood products to maintain its inventory. In our hospital, the maximum number of stock units of RBC components (LR-RBCs) is 1.5–2 times the amount of blood issued. Because platelet products rapidly degenerate, we request these products from the blood bank daily and transfuse them in the evening. For surgical patients or patients admitted to the intensive care unit, physicians are asked to order the required platelet products one day before transfusion. This strategy reduces the turnaround time of platelet components in our blood bank, helping to prevent wastage.
After the implementation of LR products (LR-phPLTs, LR-RBCs), the frequency of transfusion reactions decreased in our hospital (Fig. 4). By reducing white blood cells in RBC components before storage, the levels of IL-1, IL-6, IL-8, and TNF-α may be lowered, enhancing transfusion safety [16] and mitigating advanced transfusion reactions and allergies in recipients [18]. In 2014, the Taiwan Blood Services Foundation began providing LR-RBCs to all medical facilities. When prestorage LR-RBC products are adequately supplied for clinical transfusions, the frequency of transfusion reactions, such as febrile nonhemolytic transfusion reactions, significantly decreases [16, 19]. Although this provision offers numerous benefits, the cost of LR-RBCs is approximately double that of non-LR-RBC products (pRBCs) (US$30.8 vs. US$15.80, US$1 = NT$30). Given the high cost, physicians may be inclined to use these valuable blood components more appropriately. Additionally, owing to Taiwan’s health insurance policy and transfusion guidelines, our hospital did not fully incorporate LR-RBCs into clinical use until 2017. From 2015 to 2017, the rate of blood wastage at our hospital decreased, which coincided with a substantial reduction in the frequency of transfusion reactions due to the use of prestorage LR-RBC products.
Furthermore, improving blood management can help reduce healthcare expenses. Physicians must administer blood components appropriately during or after transfusions to avoid complications, such as volume overload or transfusion reactions. Blood transfusions are a crucial aspect of modern medical care. Over the past decade, the demand for blood components has risen, likely owing increasing life expectancy and an aging global population. In Taiwan, a significant reduction in blood donations among younger generations has been observed, which is attributed to the declining birth rate. Currently, the supply of blood products nearly matches, or at times even falls short of, the demand. With the increasing demand for blood transfusions in Taiwan’s rapidly aging society, a shortage of blood donations is expected in the near future [17]. To prevent a potential blood shortage crisis, minimizing wastage and ensuring the effective and appropriate use of all blood products are crucial [20]. Under Taiwan’s National Health Insurance system, a single unit of pRBCs costs only US$15.8 (US$1 = NT$30), which is considerably lower than that in the United States (US$200–US$300) [21] and the United Kingdom (approximately US$38) [22]. The cost of blood products typically includes various operational and maintenance expenses, such as equipment depreciation and personnel salaries at blood centers, as well as utility costs. Other services, including donor recruitment, blood collection, testing, storage, and delivery to hospitals, are also factored into the overall cost. Despite Taiwan’s lower blood product costs than those of other countries, physicians and healthcare staff must strive to avoid inappropriate transfusions and minimize wastage.
Conclusions
In this study, we explored the patterns of blood component utilization and developed several strategies to mitigate blood product wastage. Disseminating information about blood wastage among clinicians and technicians in blood banks, as well as providing continuing education for all medical staff, are essential for enhancing the safety of blood transfusions. Physicians should use blood components carefully to minimize wastage, especially given the anticipated blood shortage in Taiwan due to its rapidly aging population.
Acknowledgements
This study was extracted and analyzed from Taichung Tzu-Chi Hospital. We thank all the members of the blood bank in the hospital. We would also like to express our appreciation to Ms. Hsuan-Hui Wang of Taichung Blood Center of the Taiwan Blood Services Foundation for the consultation of blood supply and utilization.
Abbreviations
- WB
Whole blood
- pRBC
Packed red blood cell
- LR-RBC
Leukocyte-reduced RBC
- PLT
Platelet concentration
- phPLT
Apheresis platelet
- LR-phPLT
Leukocyte-reduced apheresis platelet
- FFP
Fresh frozen plasma
- FP
Frozen plasma
- CRYO
Cryoprecipitate
Authors’ contributions
Chien JH contributed to study conceptualization, investigation, formal analysis, and writing–original draft. Yao CY contributed to study supervision and writing–review & editing. Chen HF participated in data collection analysis of the manuscript. Ho TF contributed to project administration, supervision, funding acquisition, conceptualization, methodology, and writing–review & editing.
Funding
This work was supported by grants from the Central Taiwan University of Science and Technology, Taichung, Taiwan (CTU113-P-101) and from the Education of Taiwan, Taiwan (PMN1122369).
Data availability
The authors confirm that all data generated and analyzed during this study are included in this published article. The datasets analyzed during the current study contain patient medical information and are not publicly available due to the patient protection policy of Tzu-Chi Hospital. Inquiries about the study data and protocol can be directed sent to the corresponding author.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki, and applicable local regulations. Ethics approval was obtained from the Taichung Tzu-Chi Hospital, Buddhist Tzu-Chi Medical Foundation Research Ethics Committee (REC111-36: Protocol Version 1.0, and REC113-51: Protocol Version 2.0). As this study analyzed blood bank data and records without involving direct interventions or experimental procedures with participants, the Ethics Committee waived the requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Roh J, Choi SJ, Kim S, Min H, Kim HO. Blood supply and demand in Korea: what is in store for the future? Yonsei Med J. 2020;61:400–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greinacher A, Fendrich K, Brzenska R, Kiefel V, Hoffmann W. Implications of demographics on future blood supply: a population-based cross-sectional study. Transfusion. 2011;51:702–9. [DOI] [PubMed] [Google Scholar]
- 3.Ali A, Auvinen MK, Rautonen J. The aging population poses a global challenge for blood services. Transfusion. 2010;50:584–8. [DOI] [PubMed] [Google Scholar]
- 4.GBD 2021 Fertility and Forecasting Collaborators. Global fertility in 204 countries and territories, 1950–2021, with forecasts to 2100: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet (London, England). 2024;403:2057–99.
- 5.2011–2020 annual report released by the Taiwan Blood Services Foundation. Bing. https://www.bing.com/search?q=2011-2020+annual+report+released+by+the+Taiwan+Blood+Services+Foundation&form=ANNH01&refig=d8f56c3a6036409caf5a336bb43180c5&pc=NMTS. Accessed 6 Sep 2024.
- 6.Ngo A, Masel D, Cahill C, Blumberg N, Refaai MA. Blood banking and transfusion medicine challenges during the COVID-19 pandemic. Clin Lab Med. 2020;40:587–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen A, Burnett-Greenup S, Riddle D, Enderle J, Carman C, Rajendran R. Blood usage and wastage at an academic teaching hospital before the initial wave of COVID-19 and during and after its quarantine periods. Lab Med. 2024;55:198–203. [DOI] [PubMed] [Google Scholar]
- 8.Chiem C, Alghamdi K, Nguyen T, Han JH, Huo H, Jackson D. The impact of COVID-19 on blood transfusion services: a systematic review and meta-analysis. Transfusion medicine and hemotherapy : offizielles Organ der Deutschen Gesellschaft fur Transfusionsmedizin und Immunhamatologie. 2021;30:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobs JW, Booth GS. Blood shortages and changes to massive transfusion protocols: Survey of hospital practices during the COVID-19 pandemic. Transfusion and apheresis science : official journal of the World Apheresis Association : official journal of the European Society for Haemapheresis. 2022;61:103297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zoric L, Daurat G, Demattei C, Macheboeuf M, Boisson C, Bouix O, et al. Blood wastage reduction: a 10-year observational evaluation in a large teaching institution in France. Eur J Anaesthesiol. 2013;30:250–5. [DOI] [PubMed] [Google Scholar]
- 11.Amini Kafi-Abad S, Omidkhoda A, Pourfatollah AA. Analysis of hospital blood components wastage in Iran (2005–2015). Transfusion and apheresis science : official journal of the World Apheresis Association : official journal of the European Society for Haemapheresis. 2019;58:34–8. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Manual on the management, maintenance and use of blood cold chain equipment. 2005.
- 13.Yazer MH, Dunbar NM, Cohn C, Dillon J, Eldib H, Jackson B, et al. Blood product transfusion and wastage rates in obstetric hemorrhage. Transfusion. 2018;58:1408–13. [DOI] [PubMed] [Google Scholar]
- 14.Chong D, Lam JCM, Feng XYJ, Heng ML, Mok YH, Chiang LW, et al. Blood lost: a retrospective review of blood wastage from a massive transfusion protocol in a tertiary paediatric hospital. Children (Basel, Switzerland). 2022;9(12):1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heitmiller ES, Hill RB, Marshall CE, Parsons BJ, Berkow LC, Barrasso CA, et al. Blood wastage reduction using Lean Sigma methodology. Transfusion. 2010;50:1887–96. [DOI] [PubMed] [Google Scholar]
- 16.Wang RR, Triulzi DJ, Qu L. Effects of prestorage vs poststorage leukoreduction on the rate of febrile nonhemolytic transfusion reactions to platelets. Am J Clin Pathol. 2012;138:255–9. [DOI] [PubMed] [Google Scholar]
- 17.Yazer M. The Pittsburgh centralized transfusion model: less is more. Transfusion. 2007;7(2 Suppl):164S-168S. discussion 182S-183S. [Google Scholar]
- 18.Stanger SH, Yates N, Wilding R, Cotton S. Blood inventory management: hospital best practice. Transfus Med Rev. 2012;26:153–63. [DOI] [PubMed] [Google Scholar]
- 19.Rajesh K, Harsh S, Amarjit K. Effects of prestorage leukoreduction on the rate of febrile nonhemolytic transfusion reactions to red blood cells in a tertiary care hospital. Ann Med Health Sci Res. 2015;5:185–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jadwin DF, Fenderson PG, Friedman MT, Jenkins I, Shander A, Waters JH, et al. Determination of unnecessary blood transfusion by comprehensive 15-hospital record review. Jt Comm J Qual Patient Saf. 2023;49:42–52. [DOI] [PubMed] [Google Scholar]
- 21.Toner RW, Pizzi L, Leas B, Ballas SK, Quigley A, Goldfarb NI. Costs to hospitals of acquiring and processing blood in the US: a survey of hospital-based blood banks and transfusion services. Appl Health Econ Health Policy. 2011;9:29–37. [DOI] [PubMed] [Google Scholar]
- 22.Cataife G, Pagano MB. How much does a blood transfusion cost? Transfusion. 2018;58:833–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that all data generated and analyzed during this study are included in this published article. The datasets analyzed during the current study contain patient medical information and are not publicly available due to the patient protection policy of Tzu-Chi Hospital. Inquiries about the study data and protocol can be directed sent to the corresponding author.