Abstract
Introduction
Unstable pelvic fractures cause significant bleeding, morbidity, and mortality. Commercially available Pelvic Circumferential Compression Devices (PCCDs) are used in the initial resuscitation and management of these cases. In the trauma-burdened, resource limited setting of Southern Africa, the available alternative is a pelvic sheet binder (PSB). For optimal results placement should be at the greater trochanters (GTs). Prior studies have shown that practitioners are inaccurate in their placement. This study aimed to describe placement of PSBs by doctors and factors influencing placement.
Methods
This was a multicentre, prospective, observational, simulation-based study. Doctors working in Emergency Departments (EDs) and Trauma Emergency Units (TEUs) in Johannesburg were asked to place a PSB on two healthy male models of differing body mass index (BMI), as simulated patients (SPs). Outcomes were based on PSB position relative to the GTs, marked using an ultraviolet pen, and photographed under ultraviolet light. Data on techniques of placement, as well as practitioner factors, were also collected to investigate their influence on accuracy.
Results
In this study 147/176 (83.5 %) of the PSBs placed were correct (trochanteric). Of those placed on the normal BMI SP 71/88 (81 %) were correct and 76/88 (86 %) of those on the increased BMI SP. BMI did not appear to influence accuracy of placement. Practitioner factors that had statistically significant association with accurate placement included the following: Working in the TEU, work experience of ≥6 years, a diploma in primary emergency care (DipPEC, College of emergency medicine, South Africa), all methods of placing the PSB and inspecting to find the GTs.
Conclusion
The overall accuracy of PSBs placement was high (83.5 %). Additional postgraduate training (DipPEC) and work experience improved placement accuracy. This study highlighted the importance of additional trauma training and areas of possible future research, such as optimal binder width and method of securing PSBs.
Key words: Pelvic binder, Pelvic fracture, Unstable pelvis, Trauma
African relevance
● Africa's high trauma burden requires optimal initial resuscitation and management of severely injured patients. South Africa has a higher overall incidence of pelvic fractures compared to global numbers.
● Unstable pelvic fractures cause significant bleeding, morbidity and mortality, and early stabilisation improves outcomes, especially without ready access to theatre and definitive surgical care.
● Pelvic binding is the only option to mitigate pelvic haemorrhage from unstable fractures pre-hospital and in the ED, making the correct application vital.
● Commercial binders are not readily available in most centres in Africa due to cost, hence the use of sheet binders.
Background
Unstable pelvic fractures can lead to significant haemorrhage, morbidity, and mortality [1]. The trauma burden associated with blunt pelvic injury is high despite the lower incidence compared to other injuries. Unstable fractures imply a large force of impact and usually have multi-system involvement, leading to mortality rates of >40 % [2]. Pelvic circumferential compression devices (PCCDs) are used during the initial management and resuscitation of patients with these injuries to reduce, compress, and stabilise the pelvic ring. This minimises blood loss by decreasing venous and bony bleeding, aiding clot formation, and reducing the potential space in the pelvis, possibly leading to a tamponade effect [2].
The correct placement at the level of the greater trochanters (GTs) is crucial to achieve the desired effect [3]. This ensures reduction of the true pelvic ring. When placed correctly, PCCDs have been shown to decrease the need for blood transfusion, improve haemodynamic parameters acutely and shortens the length of stay in the intensive care unit [4]. This also allows for ongoing resuscitation and transport to definitive surgical care.
There are several commercially available devices, the most common being the T-POD®, SAM-Sling® and Pelvic Binder®. The T-POD requires the least amount of force to achieve reduction, but all the devices demonstrate effective reduction of unstable pelvic fractures [5]. A South African product, the PelviGrip®, is locally available, measuring 39 cm wide.
Many emergency departments (EDs) and trauma emergency units (TEUs) in South Africa do not have access to commercial pelvic binders, hence the need to make use of an improvised pelvic sheet binder (PSB). The use of both are core skills taught in Advanced Trauma Life Support® (ATLS) [1]. The T-POD® has been compared to a PSB and was found to offer no difference in pelvic stability [6].
Previous studies have demonstrated that practitioners do not place PCCDs accurately [[7], [8], [9], [10]]. A South African review of 129 blunt pelvic trauma patients requiring pelvic binders showed that 66 % of patients did not have a binder applied at all [11]. No studies have looked at PSB placement technique in South Africa. The aim of this study was to assess the accuracy of PSB placement by doctors working in the trauma setting, as well as factors that influence it.
Methods
This was a multicentre, prospective, observational, simulation-based study.
The study was approved by the University of the Witwatersrand Human Research Ethics Committee (M230747). Written informed consent was obtained from all participants and simulated patients.
Data collection
Data collection took place from November 2023 to April 2024. Doctors working in mixed EDs at Helen Joseph Hospital, Tambo Memorial Hospital and Thelle Mogoerane Hospital, as well as the Trauma Emergency Unit in Chris Hani Baragwanath Hospital, were enrolled. Every unit has a high trauma burden. They were asked to place a PSB on two healthy male models of differing body mass index (BMI), as simulated patients (SPs). The enrolled participants were community service medical officers, medical officers, registrars and consultants, i.e. Post-Graduate Year 3 and above.
The same SPs were recruited and used at all study sites. Their BMIs were calculated as 21.2 (normal, Model 1) and 28.5 (overweight, Model 2). The models were placed supine on an examining bed and participants were asked to place a PSB on each model using a hospital sheet. Participants also completed a short, self-administered questionnaire.
Under normal ambient light, participants were instructed to place the PSBs as they normally would in clinical practice. Participants could perform the procedures in any order, using their preferred techniques of determining the level of the GTs, placing and securing the PSBs.
Outcomes were measured using the GTs, marked with an 8280 Special Securitas UV Marker (Edding, Germany), and photographed from anterior after placement using an iPhone 13 (Apple, USA) under ambient and ultraviolet (UV) light. The Zartek ZA-490 UV Flashlight (Zartek, SA) was used to illuminate the UV pen markings. The GTs were first palpated and marked by the study supervisors, both with significant trauma experience, then photographed for reference when setting up in subsequent sites. The ink was not visible to the naked eye without use of the UV light (Fig. 1).
Fig. 1.
A-E. A: Control photograph of normal BMI simulated patient (SP) (Model 1). B: Control photograph of increased BMI SP (Model 2). GTs were palpated by study supervisors, marked with ultraviolet (UV) ink and photographs taken under UV light. C: Correctly placed pelvic sheet binder, secured with surgical clamps, 7 cm wide, under ambient light and D: under ultraviolet light. Please note the outlined UV markings are covered by the PSB. E: Incorrectly placed pelvic sheet binder, completely cephalad to the outlined range. Considered high in terms of outcome.
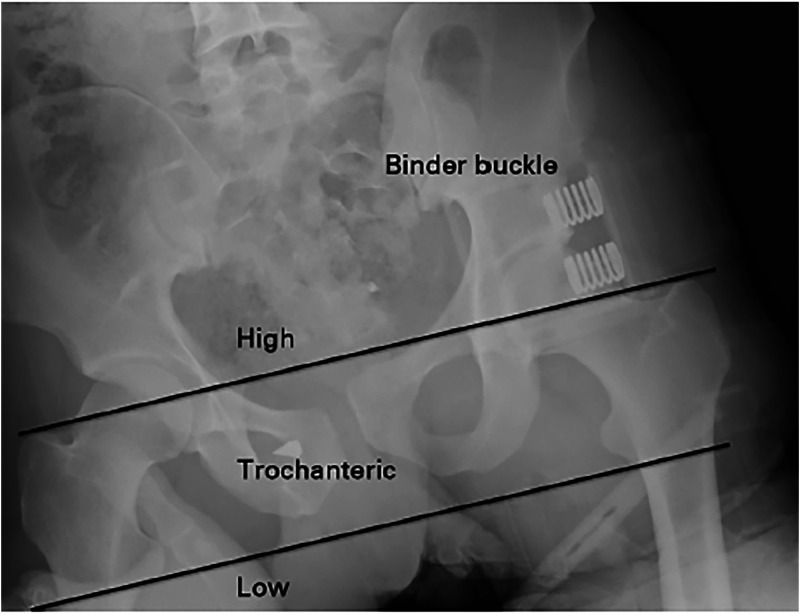
PSB position was determined relative to the outlined landmarks, adapted from Bonner et al. [7]. (Fig. 2). Outcomes were determined as ‘Trochanteric’, ‘High’ or ‘Low’. Placement was considered trochanteric if ≥50 % of the outlined range was covered by the PSB. Placement was considered high if the PSB was completely cephalad to or included <50 % of the range. Placement was considered low if the PSB was completely caudal to or included <50 % of the range. Model 1′s GTs measured 5 cm and Model 2′s, 4cm (Fig. 1).
Fig. 2.
Figure from Bonner et al. [7] illustrating outcomes based on a commercial binder buckle relative to radiographic outline of the GTs. Note the lines drawn from the upper margin of the greater trochanters and the inferior margins of the lesser trochanters.
Techniques of placement (method of determining the level of GTs, method of placing PSB under SP, width of applied sheet) were documented during the procedure. Practitioner factors (age, gender, ED work experience, practice level, place of work, diploma and course qualifications, number of PCCDs placed in preceding 6 months) were obtained from the questionnaire.
The population size was 104 doctors as derived from the rosters of the study sites at the time of protocol submission. A minimum of 84 participants was calculated to achieve confidence intervals of 95 % and a 5 % margin of error. Convenience sampling was used. A total 88 participants were enrolled.
Statistical analysis
Continuous variables were described using means and standard deviation. Categorical variables were described using percentages. Comparison between SPs and factors influencing accuracy of placement were described using the Chi-squared test. A p value of <0.05 was considered statistically significant. R® software package was used to calculate all statistical values.
Results
In total 88 doctors participated, each placing 2 PSBs resulting in 176 placements. Participant information is shown in Table 1.
Table 1.
Participant information. Total N = 88.
| Mean | (Standard deviation) | |
|---|---|---|
| Age (years) | 31.83 | (4.87) |
| ED Work Experience (years) | 3.44 | (2.63) |
| N | (%) | |
| Male | 40 | (45) |
| Female | 48 | (55) |
| Workplace: ED | 81 | (92) |
| Workplace: TEU | 7 | (8) |
| Sheet Binders placed in preceding 6 months | ||
| 0 | 44 | (50) |
| 1–5 | 37 | (42) |
| >5 | 7 | (8) |
| Commercial Binders placed in preceding 6 months (any) |
24 |
(27) |
| Level of practice: | N | (%) |
| Community Service | 17 | (19) |
| Registrar | 30 | (34) |
| Medical Officer | 39 | (44) |
| Consultant | 2 | (3) |
| Post-grad training: | N | (%) |
| ATLS Trained | 64 | (73) |
| ATLS Instructor | 3 | (3) |
| DipPEC Qualified | 48 | (55) |
| ITLS Trained | 6 | (7) |
ED = Emergency Department; TEU = Trauma Emergency Unit, ATLS = Advanced Trauma Life Support® DipPEC = Diploma in Primary Emergency Care (College of Emergency Medicine; South Africa), ITLS = International Trauma Life Support®.
Most participants were medical officers 39 (44 %), and the mean ED work experience was 3.44 years. Half of the participants had not placed a PSB in the preceding 6 months, while 37 (42 %) had placed 1–5 and only 7 (8 %) had placed >5. Only 24 (27 %) had placed a commercial binder in the preceding 6 months. Most of the participants worked in EDs, 81/88 (92 %) as opposed to TEUs 7/88 (8 %). A significant number of participants 64/88 (73 %) had attended an ATLS course, of which 50/64 (78 %) had certificates that had not expired. Fewer participants had the diploma in primary emergency care (DipPEC, College of emergency medicine, South Africa) 48/88 (55 %). Very few participants had attended International Trauma Life Support® (ITLS) 6/88 (7 %).
Accuracy of placement
A total of 176 PSBs were placed with an accuracy rate of 83.5 % (147/176). In this study accurate placement was described as Trochanteric. Of those placed on model 1, 71/88 (81 %) were trochanteric and on model 2, 76/88 (86 %). Of note 61/176 (69 %) participants placed both their PSBs correctly. High placements were more likely on model 1 [12/88 (13.6 %) versus 2/88 (2.3 %)]. Low placements were more likely on model 2 [10/88 (11.3 %) versus 5/88 (5.7 %)]. There was better overall accuracy on model 2 with 86.4 % versus 80.7 % on model 1. However, there was no statistically significant difference between the models (p = 0.42). Methods and accuracy of placement shown in Table 2.
Table 2.
Methods and accuracy of placement.
| Level of placement N (%) | ||||
|---|---|---|---|---|
| Trochanteric | High | Low | ||
| Model 1 | 71 (80.7) | 12 (13.6) | 5 (5.7) | |
| Model 2 | 76 (86.4) | 2 (2.3) | 10 (11.3) | |
| Method of determining the level of the greater trochanters N (%) | ||||
|---|---|---|---|---|
| Palpations | Inspection | None | ||
| Model 1 | 59 (67) | 6 (7) | 23 (26) | |
| Model 2 | 59 (67) | 6 (7) | 23 (26) | |
| Method of placement N (%) | ||||
|---|---|---|---|---|
| Log Roll | Shimmy | Pre-Placed | Supine maneuver | |
| Model 1 | 44 (50) | 33 (38) | 2 (2) | 9 (10) |
| Model 2 | 42 (48) | 34 (39) | 2 (2) | 10 (11) |
Model 1: Normal BMI. Model 2: Increased BMI.
Methods of determining the level of the GTs were similar between models, with 67 % using palpation, 7 % using inspection, and 26 % using no observable method.
Methods of placing the PSB under the SP remained consistent between models with 49 % of participants utilising a log roll, 38 % placing the sheet under the legs and pulling the sheet proximally and under the pelvis, described as shimmying, 12 % manoeuvring a folded PSB from lateral under the pelvis of the supine SP and 2 % utilising a pre-placed PSB.
The average width of the PSBs was 17 cm on Model 1 and 18 cm on Model 2. Very few binders were >30cm [5 on Model 1 and 6 on Model 2].
Factors influencing accuracy of placement
Practitioner factors that had statistically significant associations with accurate placement included the following: Working in the TEU, work experience of ≥6 years, a diploma in primary emergency care (DipPEC, College of emergency medicine, South Africa), every method of placing the PSB and inspecting to find the GTs. Associations with accurate placement are shown in Table 3.
Table 3.
Participant variables and accurate placement.
| Model 1 N (%) | p-value | Model 2 N (%) | p-value | |
|---|---|---|---|---|
| Place of work: | ||||
| ED | 66 (81) | 0.0481 | 70 (86) | 0.3312 |
| TEU | 5 (71) | <0.0001 | 6 (86) | <0.0001 |
| Age (years): | ||||
| 25–29 | 26 (87) | <0.0001 | 26 (87) | <0.0001 |
| 30–34 | 32 (76) | <0.0001 | 36 (86) | <0.0001 |
| 35–39 | 7 (70) | <0.0001 | 9 (90) | <0.0001 |
| ≥40 | 6 (100) | <0.0001 | 5 (83) | <0.0001 |
| Work experience (years): | ||||
| 1–5 | 58 (82) | 1 | 62 (87) | 0.4164 |
| ≥6 | 13 (76) | <0.0001 | 14 (82) | <0.0001 |
| Level of practice: | ||||
| Community Service | 15 (88) | <0.0001 | 14 (82) | <0.0001 |
| Registrar | 22 (73) | <0.0001 | 25 (83) | <0.0001 |
| Medical Officer | 32 (82) | <0.0001 | 35 (90) | <0.0001 |
| Consultant | 2 (100) | <0.0001 | 2 (100) | <0.0001 |
| Post-grad training: | ||||
| ATLS Trained | 53 (83) | 0.2847 | 57 (89) | 0.03982 |
| DipPEC Qualified | 38 (79) | 0.0004 | 41 (85) | <0.0001 |
| PSBs placed in preceding 6 months: | ||||
| 0 | 37 (84) | <0.0001 | 38 (86) | <0.0001 |
| 1–5 | 29 (78) | <0.0001 | 32 (86) | <0.0001 |
| >5 | 5 (71) | <0.0001 | 6 (86) | <0.0001 |
| Method of placing PSB under SP: | ||||
| Log Roll Method | 34 (77) | <0.0001 | 35 (83) | <0.0001 |
| Shimmy Method | 27 (82) | <0.0001 | 31 (91) | <0.0001 |
| Supine maneuver | 8 (89) | <0.0001 | 8 (80) | <0.0001 |
| Pre-Placed Method | 2 (100) | <0.0001 | 2 (100) | <0.0001 |
| Method of determining the level of GTs: | ||||
| Palpation Method | 45 (76) | 0.05914 | 50 (85) | 0.0043 |
| Inspection Method | 5 (83) | <0.0001 | 5 (83) | <0.0001 |
| No method | 21 (91) | <0.0001 | 21 (91) | <0.0001 |
Model 1: Normal BMI. Model 2: Increased BMI, ED = Emergency Department; TEU = Trauma Emergency Unit, ATLS = Advanced Trauma Life Support® DipPEC = Diploma in Primary Emergency Care (College of Emergency Medicine; South Africa.
Discussion
During the initial management of patients with unstable pelvic fractures and shock, it is crucial that a PCCD is placed accurately to obtain reduction in bleeding, morbidity and mortality [1]. The clear benefit and relatively rare complications have led to PCCD placement becoming the standard of care.
In this study, the overall accuracy of placement was higher as compared to similar studies (range 39–50 %) [[7], [8], [9], [10]]. Bonner et al. found that the most incorrect placements were too high [7]. They contributed their inaccurate placement to difficulty in identifying the GTs as well as the way the PCCD was applied, sliding under the lumbar spine and then down to the pelvis. Others also determined that major contributing factors were lack of knowledge and training [8]. Our study found that most doctors do not apply PSBs regularly, however the rate of accurate placement was still high.
We found that participants with less experience were associated with lower accuracy. The sample size might have been too small to fully evaluate the differences between practice levels, especially between consultants (N = 2). Of note the doctors working in the TEU were all registrars and consultants and are exposed to this procedure more regularly working in a level 1 trauma centre. This likely contributed to a higher accuracy compared to the ED. This could be further investigated in larger cohorts.
Our study showed that further trauma training from the DipPEC leads to more accurate placement, though surprisingly ATLS training was only associated with accurate placement with Model 2. This could possibly be due to multiple factors including infrequent practice, inadequate training or the lack of skill refreshing from expired courses. Also, surprisingly, palpating for the GTs as emphasised in courses like ATLS did not show as strong of an association with accurate placements (p = 0.059 for Model 1 and 0.0043 for Model 2) compared to inspection and no method (p ≤ 0.0001).
There is a paucity of evidence regarding the methods of applying PSBs [2,[12], [13], [14]]. The case studies that first suggested this technique all varied in terms of the specific methods (width of PSB, method of placing under the patient, method of securing) and there is no randomised control trial that supports one method. This study only looked at individual aspects of performing this clinical procedure. We allowed practitioners to perform the procedure as they would in clinical practice, allowing for and looking at variation of technique. We did not find any difference between techniques.
In practice, the method of placing the PSB under a patient is subject to variation depending on clinical presentation. In this study the SPs were already on the examination bed, leading to fewer candidates using a pre-placed PSB. When accepting a patient in the ED practitioners might pre-place the sheet in anticipation of applying it. The sequence of events during the primary and secondary survey would also dictate at what stage the log roll would happen [1]. Hence, applying the PSB might have to happen before a log roll can be safely performed, for example in the case of a patient needing simultaneous airway management. In such a case one would have to use a method other than log rolling like sliding it under the legs and shimmying proximally or manoeuvring a folded PSB from lateral under the pelvis.
The width of the PSB is a significant factor to consider for the effective application of a PSB. An extensive literature search found no studies that have investigated the ideal width of a PSB, with the studies referencing actual numbers doing so without clearly adapting for patient size and habitus. Routt et al. used a sheet as wide as above the anterior superior iliac spine (ASIS) until below the GTs [12]. White et al. advocated for placement between the ASIS and GTs [2]. Nunn et al. suggested 15 cm [13]. Higgens et al. did not suggest any width but focused on the level of the GTs [14]. ATLS also does not specify a width [1]. One must consider that the same method described by Routt et al. was used when Prasarn et al. compared the T-POD® with a PSB, suggesting that a wider binder might be effective [6,12]. This is a possible area of future research.
In our study, we allowed participants to perform the procedure as they would in normal practice, and this showed how much variation there is in our clinical setting. We noted that only 11/176 of the PSBs placed were wider than 30cm. Many of the PSBs in this study encompassed the correct target range, being the GTs, however it is unclear how much force a wider PSB exerts on the GTs. These factors need to be investigated in future studies.
Many other factors could not be investigated in this study, for example the amount of force used to reduce the pelvis. The accuracy of placement is one measure of how well this skill is performed and should be considered when interpreting these results.
No study has identified any one superior method of securing the PSB once placed. This was not an outcome in this study but would possibly be a topic for future research as it influences the stability of a PSB, especially during moving and transferring patients. Notably, some PSBs were applied but not secured during this study.
In all the available literature there have been very few adverse outcomes related to the application of a PCCD [4]. Care must still be taken to avoid prolonged application, excess reduction and force, as well as avoiding creases or too narrow binders due to risk of pressure necrosis. Ideally a patient with an unstable pelvic fracture needs expeditious transfer and definitive surgical management once appropriately resuscitated, allowing for timely release of the PSB.
Limitations
This study had a small sample size in a limited setting and findings may not be representative of practices in other settings. The SPs were both male, which limits the generalisability of the findings. The Hawthorne effect may have played a role in the accuracy and method of placement [15].
Conclusion
The accurate placement of a PSB is essential to reduce bleeding, morbidity and mortality from unstable pelvic fractures. The overall accuracy of PSB placement in this study was high (83.5 %). Practitioner factors that had statistically significant associations with accurate placement included the following: working in the TEU, work experience of ≥6 years, a diploma in primary emergency care (DipPEC, College of emergency medicine, South Africa), every method of placing the PSB and inspecting to find the GTs. More research is needed in larger cohorts. There are multiple areas identified for future research, including the ideal width of a PSB and its pressure mechanics, studying SPs with higher BMIs and including female SPs. We hope that future studies will identify the most reliable method of securing a PSB.
This was the first study of this kind in our setting and the first to look at different levels of qualification as well as ED work experience. We hope that this will lead to quality improvement and more training, resulting in better patient outcomes.
Dissemination of results
Results from this study were shared with the Division of Emergency Medicine of the University of the Witwatersrand. The study and its findings may be presented at local, national or international academic meetings in the future.
Authors contributions
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: MK 60 %, LD 20 %, PM 20 %. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors have no conflicts of interest to declare.
References
- 1.Stewart R.M., Rotondo M.F., Henry S.M., et al. 10th ed. 2018. Student course manual atls ® advanced trauma life support®. Chicago. [Google Scholar]
- 2.White C.E., Hsu J.R., Holcomb J.B. Haemodynamically unstable pelvic fractures. Injury. 2009;40(10):1023–1030. doi: 10.1016/j.injury.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 3.Bottlang M., Simpson T., Sigg J., et al. Noninvasive reduction of open-book pelvic fractures by circumferential compression. J Orthop Trauma. 2002;16(6):367–373. doi: 10.1097/00005131-200207000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Bakhshayesh P., Boutefnouchet T., Tötterman A. Effectiveness of non invasive external pelvic compression: a systematic review of the literature. Scand J Trauma Resusc Emerg Med. 2016;24(1):73. doi: 10.1186/s13049-016-0259-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knops S.P., Schep N.W.L., Spoor C.W., et al. Comparison of three different pelvic circumferential compression devices: a biomechanical cadaver study. J Bone Joint Surg. 2011;93(3):230–240. doi: 10.2106/JBJS.J.00084. [DOI] [PubMed] [Google Scholar]
- 6.Prasarn M.L., Conrad B., Small J., et al. Comparison of circumferential pelvic sheeting versus the T-POD on unstable pelvic injuries: a cadaveric study of stability. Injury. 2013;44(12):1756–1759. doi: 10.1016/j.injury.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Bonner T.J., Eardley W.G.P., Newell N., et al. Accurate placement of a pelvic binder improves reduction of unstable fractures of the pelvic ring. J Bone Joint Surg Br. 2011;93(11):1524–1528. doi: 10.1302/0301-620X.93B11.27023. [DOI] [PubMed] [Google Scholar]
- 8.Gowda S.R., Mitchell C.J., Higgs D.R., et al. Pelvic binders in trauma patients - are we doing it right? J Clin Med Res. 2021;3(6):1–9. doi: 10.37191/Mapsci-2582-4333-3(6)-101. [DOI] [Google Scholar]
- 9.McCreesh S. In a simulated adult trauma patient, can pelvic binders be applied accurately by paramedics and HEMS paramedics? A pilot observational study. Br Paramed J. 2021;6(1):23–29. doi: 10.29045/14784726.2021.6.6.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tiziani S., Janett A., Alkadhi H., et al. Does the accuracy of prehospital pelvic binder placement affect cardiovascular physiological parameters during rescue? A clinical study in patients with pelvic ring injuries. OTA Int. 2022;5(2S):e186. doi: 10.1097/OI9.0000000000000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ashkal A., Kong V., Blodgett J., et al. A review of blunt pelvic injuries at a major trauma centre in South Africa. S Afr J Surg. 2021;59(1):26. doi: 10.17159/2078-5151/2021/v59n1a3200. [DOI] [PubMed] [Google Scholar]
- 12.Routt M.L.C., Falicov A., Woodhouse E., et al. Circumferential pelvic antishock sheeting: a temporary resuscitation aid. J Orthop Trauma. 2002;16(1):45–48. doi: 10.1097/00005131-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Nunn T., Cosker T.D.A., Bose D., et al. Immediate application of improvised pelvic binder as first step in extended resuscitation from life-threatening hypovolaemic shock in conscious patients with unstable pelvic injuries. Injury. 2007;38(1):125–128. doi: 10.1016/j.injury.2006.06.026. [DOI] [PubMed] [Google Scholar]
- 14.Higgins T.F., Swanson E.R. Pelvic antishock sheeting. Air Med J. 2006;25(2):88–90. doi: 10.1016/j.amj.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 15.Sedgwick P., Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351:h4672–h4673. doi: 10.1136/bmj.h4672. [DOI] [PubMed] [Google Scholar]