ABSTRACT
Introduction
Evidence highlights the importance of social isolation as a critical yet underserved treatment target for individuals managing psychosis. Schizotypal traits represent a useful model of psychosis, facilitating the assessment of contributors to social isolation without the confounds associated with schizophrenia. This study utilised structural equation modelling to examine the unique predictive capacity of schizotypal traits for subjective and objective indices of social isolation. In addition, the potentially mediating role of negative core schemas and dysfunctional attitudes was assessed.
Methods
Structural equation modelling was used to measure and compare the relationships between the constructs of interest simultaneously.
Results
Satisfactory fit indices were attained with separate models predicting loneliness and social engagement. Results support the partial mediation of the relationships between positive and negative traits, internalising symptoms and loneliness. While all three direct pathways were significant, all three were partially mediated. Of note, these mediated effects were not observed in the model predicting social engagement, with the only significant pathways being those directly from positive and negative schizotypal traits.
Conclusions
Schizotypal traits directly predict loneliness and social engagement above that accounted for by internalising symptoms. Cognitive factors partially mediate the relationships between schizotypy and loneliness but not the size of an individual's social network. Cognitive interventions may be well suited for reducing loneliness; however, other approaches may be required to increase social networks for individuals with high levels of schizotypy.
Keywords: cognitive schemas, dysfunctional attitudes, schizotypy, social isolation
1. Introduction
Social functioning impairment is often observed in schizophrenia‐spectrum disorders (SSDs), with social isolation a frequent manifestation (Badcock, Adery, and Park 2020). An estimated 80% of individuals managing an SSD experience chronic isolation (Stain et al. 2012) and report social networks approximately half the size of individuals without psychosis (Gayer‐Anderson and Morgan 2013). Evidence suggests social isolation is strongly associated with increased instances of suicide and substance use within the SSD population (Barrantes‐Vidal, Lewandowski, and Kwapil 2010; Bornheimer et al. 2023) and may have a bidirectional relationship (Fulford and Mueser 2020) with psychosis onset (Chau, Zhu, and So 2019) and maintenance (Michalska da Rocha et al. 2018). As such, isolation has become recognised as a critical issue impacting well‐being within the SSD population (Michalska da Rocha et al. 2018).
Unfortunately, examining the manifestation of social isolation within the SSD population is complicated by a variety of illness‐related factors, including iatrogenic effects of medical treatment and societal stigmatisation that are unrelated to the psychopathology of schizophrenia itself. One method of examining the psychopathology of schizophrenia without these confounds is to examine subclinical schizotypal traits. Schizotypy is conceptualised as an underlying vulnerability for developing schizophrenia (Lenzenweger 2018), occurs on a continuum in the general population and is organised according to positive, negative and disorganised subtypes characterised by a range of social and affective abnormalities present in individuals with SSDs (Fonseca‐Pedrero et al. 2018). Evidence has similarly supported the prevalence of social isolation with non‐clinical individuals endorsing high levels of both negative for example, reduced social functioning (Wang et al. 2013), reduced social engagement (Kwapil et al. 2020), and elevated loneliness (Christensen et al. 2022) and positive (e.g., greater isolation (Barrantes‐Vidal, Lewandowski, and Kwapil 2010), and elevated loneliness (Chau, Zhu, and So 2019)) traits. What remains unknown are the unique contributions of negative versus positive traits when shared variance between the dimensions are accounted for. Additionally, research consistently demonstrates the high co‐occurrence of social isolation with affective symptoms such as anxiety and depression (Beutel et al. 2017). When shared variance between the dimensions and affective symptoms are controlled, different relationships may emerge with social isolation.
Importantly, social isolation can be operationalised through objective and subjective indicators. Social network size is a relatively objective indicator of the quantity of social relationships. In contrast, loneliness is recognised as a subjective construct representing perceived social isolation (Käll et al. 2020), manifesting from a disconnect between an individual's expectations regarding social relationships and their realities (Cacioppo and Hawkley 2009). Evidence suggests that these constructs are not strongly correlated despite the conceptual similarities between social network size and loneliness (e.g., r = ~0.201; 1), suggesting their distinctiveness. Feelings of loneliness may not always be present when an individual reports low quantities of social relationships. The unique relationships between schizotypy and perceived social isolation (i.e., subjective loneliness) versus objective social isolation (i.e., social engagement) have yet to be examined.
Furthermore, despite associations observed between schizotypal traits and indices of social isolation, little is known regarding underlying mechanisms. One hypothesis proposes a bidirectional relationship between the presence of psychosis/psychotic‐like experiences and social isolation (Badcock, Adery, and Park 2020). In this, the presence of psychosis‐like experiences results in the development of negative beliefs regarding the self and others. Such beliefs increase social withdrawal to minimise the threat of social rejection, contributing to the manifestation of social isolation. Subsequently, as social isolation increases, psychotic‐like experiences may similarly increase, potentially leading to the onset of psychosis, a pattern observed with paranoid delusions (Fett et al. 2022). Two relevant negative beliefs are negative core schemas and dysfunctional beliefs. According to the cognitive model, schemas are conceptualised as underlying cognitive structures that develop based on previous life experience and guide how future events are processed (Beck 1979). In contrast, dysfunctional beliefs are conceptualised as situation‐specific beliefs that guide behaviour when relevant stimuli are present. (Beck et al. 2013). Cognitive theories of both psychotic and non‐psychotic disorders highlight the importance of schemas and beliefs in guiding ongoing appraisals of events, moods and mental states, potentially maintaining functional impairment (Beck, Himelstein, and Grant 2019), such as chronic social isolation.
Maladaptive beliefs and negative schemas are prominent in samples of individuals with psychosis (Beck et al. 2018) and elevated schizotypal traits (Fervaha et al. 2015). Elevated total schizotypal traits predict lower indices of positive schemas and higher indices of negative schemas regarding the self and others (Zahid and Best 2023). Both positive and negative schizotypal traits independently predict increased endorsement of negative self/other schemas (Barrantes‐Vidal et al. 2013; Devoe et al. 2022) and dysfunctional beliefs (Campellone et al. 2019; Devoe et al. 2022). Uniquely, negative schizotypy more consistently demonstrates associations with decreased positive schemas (Barrantes‐Vidal et al. 2013). Of note, endorsement of negative self schemas, negative other schemas and dysfunctional attitudes have been shown to significantly correlate with indices of social network size (Sorenson, Rossell, and Sumner 2021), loneliness (Chau et al. 2022b) and consummatory social pleasure (Campellone et al. 2019) in samples of non‐clinical individuals endorsing elevated schizotypal traits, supporting for their characterisation as a psychological underlying mechanism (Chau et al. 2022a). Given the existing literature, further examining these relationships is important to help identify a broader model of schizotypy, social functioning and maladaptive cognitive structures.
Thus, this study aimed to test a comprehensive model of the interrelationships between schizotypal traits, indices of social isolation and maladaptive schemas/beliefs. We hypothesised that positive and negative schizotypal traits would directly predict social engagement and loneliness. Furthermore, we hypothesised that maladaptive schemas and dysfunctional attitudes would partially mediate these effects. Given noted relevance, we also examined these relationships with internalised symptoms.
2. Methods
2.1. Participants
All participants were recruited using Amazon Mechanical Turk (MTurk; (Cheung et al. 2017) for a larger study on coping strategies (Rumas et al. 2021)). Survey access was permitted if the participant used a Canadian or American Internet Protocol address. Participants were required to have a 99% approval rating based on previous MTurk task completions. Survey data were collected at two time points approximately 1 month apart (M = 30.03 days, Mdn = 30 days, SD = 1.69, Max = 35, Min = 27). One thousand participants were recruited between April 21st and 25th, 2020 (Time 1). All participants who passed embedded validity measures were re‐contacted to complete the follow‐up survey approximately 1 month later, between May 21st and 27th, 2020 (Time 2). Participants were compensated with $2 (USD), with the passing of all effort questions embedded in both surveys being awarded a bonus of $2 (USD).
3. Measures
3.1. UCLA Loneliness Scale (Russell 1996)
The UCLA Loneliness Scale is a 20‐item self‐report measure designed to assess subjective feelings of loneliness at the time of assessment. Each item on the scale is rated on a 4‐point scale from 0 (I never feel this way) to 3 (I often feel this way). Higher scores are indicative of greater subjective feelings of loneliness. Internal consistency on this measure was α = 0.96.
3.2. Lubben Social Network Scale‐6 (LSNS‐6; (Lubben et al. 2006)
The LSNS‐6 is a 6‐item self‐report measure assessing the degree of social engagement with family and friends endorsed by the participant at the time of assessment. Items are rated on a 6‐point Likert scale from 0 (none) to 5 (nine or more) with higher scores indicating greater social engagement (e.g., more frequent social interactions, a greater quantity of relationships, a greater quantity of high‐quality relationships). Internal consistency on this measure was α = 0.84.
3.3. Wisconsin Schizotypy Scales—Short Forms (WSS‐SF; (Winterstein et al. 2011)
The WSS‐SF is composed of four subscales (magical ideation [MIS], perceptual aberration [PeAS], physical anhedonia [PhAS] and revised social anhedonia [RSAS]) comprised of 15 items each. The MIS and PAS assess positive symptom aspects of schizotypy, while the PhAS and the RSAS assess negative symptoms. All items on the WSS‐SF are designed to assess the participant's agreement with the item at the time of assessment using a true/false binary format, where false responses are scored as a 0 and true responses a 1. Internal consistency on this measure was α = 0.92.
3.4. The Brief Core Schema Scale (BCSS; Fowler et al. 2006)
The BCSS is a self‐report measure used to assess self and other schemas at the time of assessment. It contains 24 items that query beliefs regarding the self and others assessed on a 5‐point scale (0–4). Four subscale scores are derived from the BCSS, each based on responses to six items. These scales reflect the strength of beliefs regarding negative self, positive‐self, negative others and positive‐others. Internal consistency on this measure was α = 0.80.
3.5. The Dysfunctional Attitudes Scale (DAS; Beck et al. 1991)
The DAS is a 40‐item measure designed to assess depressive attitudes at the time of assessment. Ratings reflecting the degree to which the participant agrees or disagrees with a statement are provided on a 7‐point scale ranging from Totally Agree to Disagree Totally. Internal consistency on this measure was α = 0.86.
3.6. Patient Health Questionnaire (PHQ‐9; (Kroenke, Spitzer, and Williams 2001)
The PHQ‐9 is a 9‐item self‐report measure of depression. Items are scored on a scale of 0 (not at all) to 3 (nearly every day) and reflect the participant's experiences over the last 2 weeks. Internal consistency on this measure was α = 0.90.
3.7. Generalised Anxiety Disorder (GAD‐7; (Spitzer et al. 2006)
The GAD‐7 is a 7‐item self‐report measure assessing the presence and severity of anxiety symptoms. Items query the frequency with which responders have been bothered by anxiety‐related problems on a 4‐point scale, ranging from 0 (Not At All) to 3 (Nearly Every Day). Higher scores reflect more severe anxiety symptoms over the past 2 weeks. Internal consistency on this measure was α = 0.90.
3.8. Effort Items
The validity of the responses provided by the participants was assessed via four embedded effort questions adapted from Huang et al. (2015). Participants were excluded if they failed more than one effort question.
3.9. Statistical Analyses
Correlational analyses between all variables of interest were conducted using Pearson correlation coefficients using R Core Team (2021). Tests were two‐tailed and Bonferroni corrected (i.e., 0.05/72 = 0.0007,0.001/72 = 0.0001; (Bland and Altman 1995)).
Structural equation modelling (SEM) used the Lavann package in R Core Team (2021) to test correlation and mediation effects. Models were comprised of three latent exogenous variables (i.e., positive schizotypal traits, negative schizotypal traits, internalising symptoms), three mediating manifest variables of negative self schema, negative other schema and dysfunctional attitudes and a predicted manifest variable of either subjective loneliness or social engagement. Each model was evaluated using the chi‐squared statistic (good fit indicated by an insignificant result at a 0.05 threshold; Barrett 2007), the root mean square error of approximation (RMSEA; < 0.07 indicating good fit; Steiger 2007), the Comparative Fit Index (CFI; > 0.95 indicative of good fit; Hu and Bentler 1999) and the standardised root mean square residuals (SRMR; < 0.05 indicating good fit, < 0.08 indicating adequate fit; Hu and Bentler 1999). The primary theoretical model hypothesised a direct relationship between positive and negative schizotypal traits to the indices of social isolation (e.g., loneliness or social engagement) and mediated relationships through negative self schemas, negative others schemas and dysfunctional attitudes. Competing models varied based on including internalising symptoms and the constraining of non‐significant pathways. The model demonstrating the best fit was tested using data from Time 2 to determine whether a satisfactory fit was replicated.
4. Results
4.1. Sample Characteristics
Sample characteristics are reported in Table 1. A total of 203 participants at Time 1 were excluded (20.3%) based on effort item responses, resulting in a sample of 797 participants at Time 1. Of these, 408 (51%) completed the survey at Time 2, of which 13 were excluded based on effort item response, resulting in a final sample of 395 at Time 2.
TABLE 1.
Demographic characteristics of the baseline and longitudinal sample.
| Time 1 (N = 797) | Time 2 (n = 395) | |
|---|---|---|
| Age, M years (SD) | 32.2 (11.5) | 33.7 (12.6) |
| Country of residence, n (%) | ||
| USA | 755 (94.7) | 366 (92.7) |
| Canada | 42 (5.3) | 29 (7.3) |
| Gender, n (%) | ||
| Male | 357 (44.8) | 173 (43.8) |
| Female | 435 (54.6) | 220 (55.7) |
| Non‐binary | 3 (0.4) | 2 (0.5) |
| Two‐spirit | 2 (0.3) | 0 (0.0) |
| Ethnicity, n (%) | ||
| White | 538 (67.5) | 274 (69.4) |
| Black | 66 (8.3) | 28 (7.1) |
| Multiracial | 52 (6.5) | 26 (6.6) |
| Latin American | 49 (6.1) | 21 (5.3) |
| South Asian | 36 (4.5) | 20 (5.1) |
| Chinese | 22 (2.8) | 11 (2.8) |
| Southeast Asian | 11 (1.4) | 7 (1.8) |
| Filipino | 8 (1.0) | 3 (0.8) |
| Korean | 4 (0.5) | 1 (0.3) |
| West Asian | 3 (0.4) | 1 (0.3) |
| Indigenous | 2 (0.3) | 1 (0.3) |
| Arab | 2 (0.3) | 1 (0.3) |
| Japanese | 2 (0.3) | 1 (0.3) |
| Other | 2 (0.3) | 0 (0.0) |
4.2. Correlations
Correlations between the measures of interest at Time 1 and Time 2 are reported in Table 2.
TABLE 2.
Intercorrelations among schizotypal traits, maladjusted cognitions, loneliness, social network and internalising symptoms at baseline and follow‐up.
| Time 1 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| 1. MIS | 1 | ||||||||||
| 2. PeAS | 0.72** | 1 | |||||||||
| 3. RSAS | 0.27** | 0.35** | 1 | ||||||||
| 4. PhAS | 0.23** | 0.32** | 0.40** | 1 | |||||||
| 5. DAS | 0.34** | 0.38** | 0.18** | 0.14** | 1 | ||||||
| 6. Negative self | 0.20** | 0.35** | 0.33** | 0.23** | 0.40** | 1 | |||||
| 7. Negative other | 0.21** | 0.14** | 0.18** | 0.06 | 0.21** | 0.31** | 1 | ||||
| 8. LSNS | −0.08 | −0.13* | −0.47** | −0.26** | −0.09 | −0.28** | −0.17** | 1 | |||
| 9. UCLA | 0.25** | 0.30** | 0.39** | 0.16** | 0.46** | 0.58** | 0.29** | −0.39** | 1 | ||
| 10. PHQ | 0.28** | 0.34** | 0.29** | 0.20** | 0.35** | 0.52** | 0.20** | 21** | 0.56** | 1 | |
| 11. GAD | 0.24** | 0.28** | 0.24** | 0.11 | 0.31** | 0.48** | 0.25** | −0.20** | 0.51** | 79** | 1 |
| Time 2 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| 1. MIS | 1 | ||||||||||
| 2. PeAS | 0.72** | 1 | |||||||||
| 3. RSAS | 0.27** | 0.34** | 1 | ||||||||
| 4. PhAS | 0.19* | 0.30** | 0.40** | 1 | |||||||
| 5. DAS | 0.29** | 0.32** | 0.08 | 0.10 | 1 | ||||||
| 6. Negative self | 0.21** | 0.37** | 0.30** | 0.18* | 0.39** | 1 | |||||
| 7. Negative other | 0.21** | 0.18* | 0.27** | 0.10 | 0.19** | 0.30** | 1 | ||||
| 8. LSNS | −0.12 | −0.19* | −0.54** | −0.29** | −0.03 | −0.26** | −0.15 | 1 | |||
| 9. UCLA | 0.26** | 0.28** | 0.34** | 0.10 | 0.43** | 0.62** | 0.35** | −0.38** | 1 | ||
| 10. PHQ | 0.24** | 0.36** | 0.32** | 0.16 | 0.33** | 0.63** | 0.30** | −0.24** | 0.60** | 1 | |
| 11. GAD | 0.24** | 0.29** | 0.26** | 0.05 | 0.31** | 0.53** | 0.32** | −0.21** | 0.57** | 0.82** | 1 |
Note: p values adjusted for multiple comparison (i.e., 0.05/66 = 0.0007, 0.01/66 = 0.0001).
Abbreviations: DAS: Dysfunctional Attitudes Scale Total; GAD: Generalized Anxiety Disorder‐7 Total Score; LSNS: Lubben Social Network Scale Total Score; MIS: Magical Ideation Scale Total; Negative other: Negative other schema total; Negative self: Negative self schema total; PeAS: Perceptual Aberration Scale Total; PHQ: Patient Health Questionnaire‐9 Total Score; RSAS: Revised Social Anhedonia Scale Total; UCLA: UCLA Loneliness Scale Total Score.
p < 0.0007.
p < 0.0001.
5. Structural Equation Model
5.1. Subjective Loneliness—Time 1
The final model demonstrating the best fit is illustrated in Figure 1 (x 2 = 99.05, RMSEA = 0.06, SRMR of 0.03, CFI = 0.97). This model assessed the hypothesised relationships between schizotypal traits, symptoms, maladjusted cognitions and subjective loneliness. Non‐significant pathways were observed between positive schizotypal traits and negative self schemas (p = 0.053), positive schizotypal traits and negative other schemas (p = 0.339) and negative schizotypal traits and dysfunctional attitudes (p = 0.617). For parsimony and based on fit indices, these pathways were constrained to zero in the final model.
FIGURE 1.
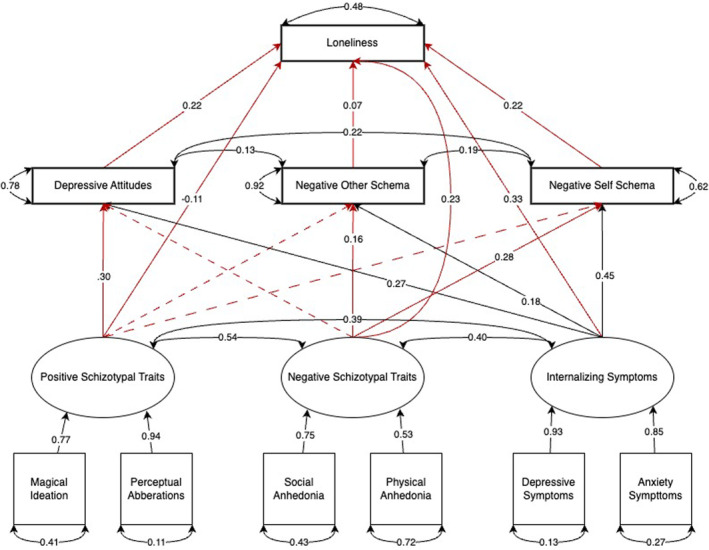
Structural equation model (SEM) with schizotypal traits, internalising symptoms, dysfunctional attitudes, maladaptive schemas and subjective loneliness. Primary pathways of interest are presented in red.
The SEM revealed significant direct pathways from internalising symptoms (β = 0.33, p < 0.001), positive schizotypal traits (β = −0.11, p = 0.004) and negative schizotypal traits (β = 0.23, p < 0.001) to subjective loneliness. A significant pathway was also observed between positive schizotypal traits and dysfunctional attitudes (β = 0.30, p < 0.001). The associations observed between negative schizotypal traits, negative other schemas β = 0.16 (β = 0.16, p = 0.001) and negative self schemas (β = 0.28, p < 0.001) were statistically significant. Internalising symptoms were demonstrated to have significant relationships with dysfunctional attitudes (β = 0.27, p < 0.001), negative other schemas (β = 0.18, p < 0.001) and negative self schemas (β = 0.45, p < 0.001). Similar significant pathways were observed between dysfunctional attitudes (β = 0.22, p < 0.001), negative other schemas (β = 0.06, p = 0.017), negative self schemas (β = 0.22, p < 0.001) and subjective loneliness.
Indirect pathways were also observed to be significant. The impact of internalising symptoms on subjective loneliness through dysfunctional attitudes (β = 0.06, p < 0.00), negative other schemas (β = 0.01, p = 0.040) and negative self schemas (β = 0.10, p < 0.001) were all statistically significant. The relationship between negative schizotypal traits and subjective loneliness through negative self schemas (β = 0.06, p < 0.001) and negative other schemas (β = 0.01, p < 0.040) was also statistically significant. Only the indirect effect of positive schizotypal traits on subjective loneliness through dysfunctional attitudes (β = 0.06, p < 0.001) was shown to be statistically significant.
5.2. Subjective Loneliness—Time 2
To test the temporal stability of the final subjective loneliness model, it was retested for fit using the Time 2 data. As depicted in Figure S3 (available in Supporting Information), satisfactory fit indices were again observed (x 2 = 74.76, RMSEA = 0.08, SRMR of 0.04, CFI = 0.97). Non‐significant pathways were again constrained to zero for parsimony.
The SEM for Time 2 revealed significant direct pathways from positive traits (β = −0.09, p = 0.038), negative traits (β = 0.15, p = 0.005) and internalising symptoms (β = 0.31, p < 0.001) to subjective loneliness. Positive traits again demonstrated a significant association with dysfunctional attitudes (β = 0.22, p < 0.001). While the relationship between positive traits and negative others schema was non‐significant and thus constrained, a statistically significant association between positive traits and negative self schemas was observed (β = 0.12, p = 0.007). As at Time 1, negative schizotypal traits demonstrated a statistically significant association with negative self (β = 0.11, p = 0.038) and negative others (β = 0.23, p < 0.001) schemas. Internalising symptoms were demonstrated to have a significant relationship with negative self schemas (β = 0.57, p < 0.001), negative others schemas β = 0.23 (β = 0.33, p < 0.001) and dysfunctional attitudes (β = 0.26, p < 0.001). Significant pathways were also observed from negative self schemas (β = 0.29, p < 0.001), negative others schemas (β = 0.09, p = 0.022) and dysfunctional attitudes (β = 0.21, p < 0.001) to subjective loneliness.
The indirect pathways from internalising symptoms to subjective loneliness through dysfunctional attitudes (β = 0.06, p < 0.00), negative other schemas (β = 0.02, p = 0.048) and negative self schemas (β = 0.16, p < 0.001) were all statistically significant. The relationship between negative schizotypal traits and subjective loneliness through negative self schemas (β = 0.03, p = 0.046) and negative other schemas (β = 0.02, p = 0.045) was also statistically significant. Finally, the indirect effect of positive schizotypal traits on subjective loneliness through dysfunctional attitudes (β = 0.05, p = 0.001) and negative self schemas (β = 0.04, p = 0.016) was shown to be statistically significant.
5.3. Social Engagement—Time 1
The model demonstrating the best fit is illustrated in Figure 2 (x 2 = 87.67, RMSEA = 0.06, SRMR of 0.03, CFI = 0.98). The final model included a latent construct of internalising symptoms and non‐significant pathways constrained to zero. Non‐significant pathways were observed between positive schizotypal traits and negative self schema (p = 0.114), positive schizotypal traits and negative other schema (p = 0.592) and negative schizotypal traits and dysfunctional attitudes (p = 0.585). Of note, the direct pathways to social engagement from negative self schema (β = 0.33, p = 0.282), negative other schema (p = 0.181), dysfunctional attitudes (p = 0.725) and internalising symptoms (p = 0.667) were all statistically non‐significant. For parsimony and based on model fit indices, these pathways were constrained to zero for the final model.
FIGURE 2.
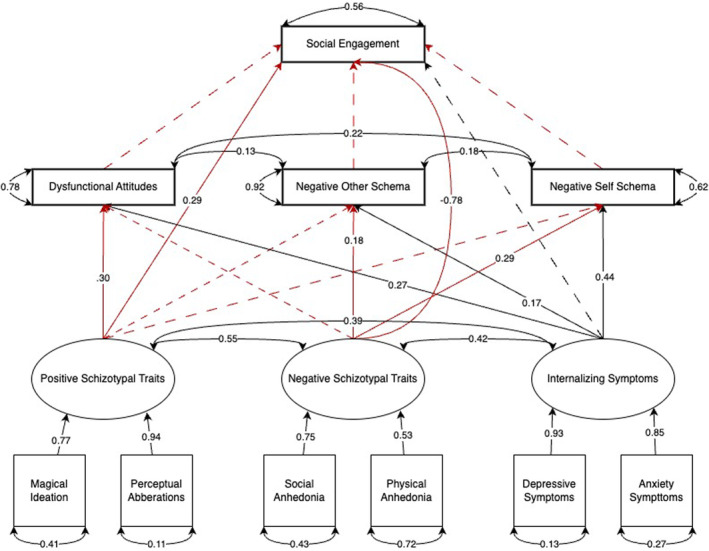
Structural equation model (SEM) with schizotypal traits, internalising symptoms, dysfunctional attitudes, maladaptive schemas and social engagement. Primary pathways of interest are presented in red.
The SEM revealed only two significant direct pathways from the variables of interest and social network/engagement. Of those tested, only the direct pathways from negative (β = −0.78, p < 0.001) and positive (β = 0.29, p < 0.001) schizotypal traits to social network/engagement were significant. The latent construct of internalising symptoms demonstrated significant associations with negative self schema (β = 0.44, p < 0.001), negative other schema (β = 0.17, p < 0.001) and dysfunctional attitudes (β = 0.27, p < 0.001). Negative schizotypal traits demonstrated significant relationships with negative self schema (β = 0.29, p < 0.001) and negative other schema (β = 0.18, p < 0.001). Only the pathway from positive schizotypal traits to dysfunctional attitudes (β = 0.30, p < 0.001) was statistically significant. No indirect pathways were significant.
5.4. Social Engagement—Time 2
Model 2 was similarly tested using Time 2 data to assess its temporal stability. As depicted in Figure S4 (available in Supporting Information), satisfactory fit indices were observed (x 2 = 64.13, RMSEA = 0.07, SRMR of 0.03, CFI = 0.97). Non‐significant pathways were constrained to zero.
Two significant direct pathways from the variables of interest and social engagement were observed. The direct pathways from negative (β = −0.72, p < 0.001) and positive (β = 0.12, p = 0.022) schizotypal traits to social engagement were significant. Internalising symptoms demonstrated significant associations with negative self schema (β = 0.55, p < 0.001), negative other schema (β = 0.22, p < 0.001) and dysfunctional attitudes (β = 0.25, p < 0.001). Negative schizotypal traits demonstrated significant relationships with negative self schema (β = 0.14, p = 0.006) and negative other schema (β = 0.22, p < 0.001). The pathway from positive schizotypal traits to dysfunctional attitudes (β = 0.23, p < 0.001) and negative self schemas β = 0.11 (β = 0.33, p = 0.014) was statistically significant. No indirect pathways were significant.
6. Discussion
This study examined the relationships between schizotypal traits, maladaptive schemas and dysfunctional attitudes with subjective loneliness and social engagement. Both dimensions of schizotypy demonstrated significant associations with subjective loneliness and social engagement. All pathways remained significant despite controlling for shared variance between schizotypy traits and internalising symptoms. These results highlight the association of schizotypy with loneliness and social engagement beyond that already accounted for by internalising symptoms. Additionally, dysfunctional attitudes and maladaptive schemas mediated these relationships for loneliness but not for social engagement.
Previous studies have supported medium to large positive associations between positive schizotypy and loneliness (Chau, Zhu, and So 2019). Similarly sized positive correlations at both Time 1 and Time 2 were observed; however, when incorporated into the full model, a significant, although small, negative association (Time 1: r = −0.11, Time 2: −0.09) was observed. These results suggest that previously identified positive associations between positive schizotypal traits and loneliness may be better explained by factors such as comorbid negative schizotypal traits, maladaptive attitudes/schemas, or internalising symptoms, unaccounted for in previous models. When such relationships are statistically accounted for, the direction of effect is reversed, suggesting positive traits predict less subjective loneliness. This is consistent with a recent study analysing the associations between loneliness and positive, negative and disorganised schizotypal traits, where it was observed that when negative traits, disorganised symptoms and depression were accounted for, the relationship between positive traits and loneliness reversed from positive to negative (Christensen et al. 2022). Similar patterns have been observed in studies using experience sampling (Kwapil et al. 2020) and cluster analysis methodology (Chau et al. 2022a). Together, these results suggest positive schizotypal traits can negatively correlate with loneliness within non‐clinical samples. One possible explanation for this finding with supporting evidence is that positive traits offer some form of a protective effect against loneliness (Crespi et al. 2019; Mohr and Claridge 2015; Polner, Simor, and Kéri 2018). While the exact process by which positive traits would facilitate this protective effect is unknown, some have hypothesised that it may reflect a cognitive defence mechanism through which life uncertainties are rationalised (Williams and Irwin 1991).
It has been previously predicted that elevated levels of negative schizotypy traits are associated with reduced levels of self‐reported loneliness (Christensen et al. 2022; Silvia and Kwapil 2011), attributable to the greater endorsement of a reduced need for social interactions captured by the negative trait of asociality (Kwapil et al. 2018). While studies have supported this hypothesis by reporting negative associations between negative symptoms and social functioning in at‐risk populations (Corcoran et al. 2011; Schlosser et al. 2015), others have failed to replicate such effects (Chau et al. 2022a; Christensen et al. 2022; Tan, Shallis, and Barkus 2020). Our findings highlighted a medium positive association between negative schizotypal traits and subjective loneliness. Correlation coefficients reflecting the relationship between negative schizotypal traits and loneliness were consistently positive with no change in direction when multiple relationships and shared variance were accounted for. This suggests that individuals who endorse negative schizotypal traits, specifically those falling within the dimensions of social and physical anhedonia, do not necessarily have divergent perceptions of the need for social interactions and similarly experience subjective loneliness.
The current results also demonstrate the importance of dysfunctional attitudes and maladaptive schemas in understanding the association between schizotypy and social functioning. In alignment with previous findings, significant positive associations between negative schizotypal traits and negative schemas regarding the self and others were consistently observed across the time points. In contrast, the association between negative traits and dysfunctional attitudes never reached significance. In contrast to these findings, positive schizotypy was never significantly associated with endorsing negative other schemas while demonstrating a consistently significant association with dysfunctional attitudes across Time 1 and Time 2. The only association which demonstrated a notable change from Time 1 and 2 was between positive traits and negative self schemas, which were non‐significant at Time 1 and significant at Time 2.
Of the indirect effects assessed between schizotypal traits and loneliness, the pathway from positive schizotypy through dysfunctional beliefs to loneliness returned the largest effect (r = 0.064) at Time 1. Negative traits demonstrated a similarly strong indirect effect through negative self schemas at Time 1 (r = 0.062), while the indirect effect from negative traits to loneliness through negative other schemas was comparatively weaker (r = 0.010). A similar pattern was observed at Time 2, with the positive traits to dysfunctional attitudes pathway demonstrating the largest effect (r = 0.045) and the indirect effect through positive self‐schemas having an effect size of r = 0.035. The indirect pathways from negative traits through the schemas assessed demonstrated a similar pattern of effects (Negative Traits—Negative Other: r = 0.020; Negative Traits—Negative Self: r = 0.032). In contrast, based on the pattern of the observed effects, no indirect pathways were demonstrated as significant in the model predicting social engagement. This is the first time these relationships have been assessed within a schizotypy sample using an SEM methodology. These results suggest that the impact of schizotypal traits on loneliness is partially mediated by schema and belief content, with some evidence suggesting a trait‐specific pattern of effects regarding the relevance of schemas or dysfunctional beliefs.
Finally, several noteworthy results emerged when the relationship between schizotypal traits and social engagement was examined. Negative schizotypal traits demonstrated a large negative (r = −0.78) direct association with social engagement. Conversely, positive schizotypal traits demonstrated a positive medium association (r = 0.29). Unlike the results observed within the subjective loneliness model, all three cognitive constructs assessed failed to demonstrate significant associations with endorsed social engagement. Previous research has demonstrated weak correlations between social engagement and subjective loneliness (Coyle and Dugan 2012), suggesting a more complex relationship between the constructs. While both constructs were measured using self‐report questionnaires, it is arguable that social engagement represents a more objective measurement of social experience than subjective loneliness, which reflects a perception. Thus, dysfunctional attitudes and maladaptive schemas appear to serve an important mediating role with the subjective experience of loneliness but not with the nature of someone's social relationships. Further research is needed to assess what factors may better explain the relationship between schizotypal traits and social engagement, such as external factors (e.g., stigmatising attitudes or societal exclusion; (Best and Bowie 2022)).
6.1. Limitations
The primary strength of this study is its use of a model which allowed for the simultaneous assessment of various factors and their links to loneliness and social engagement. Despite this, several limitations must be acknowledged. The sample was recruited via MTurk, which may have limited generalisability since participation necessitated familiarity with the platform. However, research has suggested that MTurk samples may better represent community‐based demographics than typical sampling techniques (Cheung et al. 2017; Clifford, Jewell, and Waggoner 2015). The cross‐sectional analysis limited our ability to examine causal inferences. However, the consistency of the models was observed at Time 2, supporting the temporal reliability of the model (Boyer et al. 2012). Additionally, this study relied upon self‐report measures to assess various indices of mental health, cognition and social functioning. While the measures used have been validated with the relevant populations, results may have differed if behavioural or interview‐based assessments had been used. Future studies should seek to replicate the pattern of findings observed using a longitudinal design in addition to more detailed and objective measures of the constructs of interest.
7. Conclusion
The results of the current study support an association between both positive and negative schizotypal traits and both loneliness and social engagement after controlling for the effect of internalising symptoms. Dysfunctional attitudes and maladaptive cognitive schemas mediated the association between schizotypy and loneliness; however, they were unrelated to social engagement. These results highlight the importance of considering the presence of schizotypal traits in understanding loneliness and social engagement. Future research may consider the implications such findings have on developing interventions targeting loneliness and social engagement for individuals with high levels of schizotypy to improve the overall quality of life effectively.
Supporting information
Data S1. Figures.
Funding: The authors received no specific funding for this work.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Badcock, J. C. , Adery L. H., and Park S.. 2020. “Loneliness in Psychosis: A Practical Review and Critique for Clinicians.” Clinical Psychology: Science and Practice 27, no. 4: 50. 10.1111/cpsp.12345. [DOI] [Google Scholar]
- Barrantes‐Vidal, N. , Gross G. M., Sheinbaum T., Mitjavila M., Ballespí S., and Kwapil T. R.. 2013. “Positive and Negative Schizotypy Are Associated With Prodromal and Schizophrenia‐Spectrum Symptoms.” Schizophrenia Research 145, no. 1–3: 50–55. 10.1016/j.schres.2013.01.007. [DOI] [PubMed] [Google Scholar]
- Barrantes‐Vidal, N. , Lewandowski K. E., and Kwapil T. R.. 2010. “Psychopathology, Social Adjustment and Personality Correlates of Schizotypy Clusters in a Large Nonclinical Sample.” Schizophrenia Research 122, no. 1–3: 219–225. 10.1016/j.schres.2010.01.006. [DOI] [PubMed] [Google Scholar]
- Barrett, P. 2007. “Structural Equation Modelling: Adjudging Model Fit.” Personality and Individual Differences 42, no. 5: 815–824. 10.1016/j.paid.2006.09.018. [DOI] [Google Scholar]
- Beck, A. T. 1979. Cognitive Therapy of Depression. New York, NY: Guilford Press. [Google Scholar]
- Beck, A. T. , Grant P. M., Huh G. A., Perivoliotis D., and Chang N. A.. 2013. “Dysfunctional Attitudes and Expectancies in Deficit Syndrome Schizophrenia.” Schizophrenia Bulletin 39, no. 1: 43–51. 10.1093/schbul/sbr040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. T. , Himelstein R., Bredemeier K., Silverstein S. M., and Grant P.. 2018. “What Accounts for Poor Functioning in People With Schizophrenia: A Re‐Evaluation of the Contributions of Neurocognitive v. Attitudinal and Motivational Factors.” Psychological Medicine 48, no. 16: 2776–2785. 10.1017/S0033291718000442. [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Himelstein R., and Grant P. M.. 2019. “In and out of Schizophrenia: Activation and Deactivation of the Negative and Positive Schemas.” Schizophrenia Research 203: 55–61. 10.1016/j.schres.2017.10.046. [DOI] [PubMed] [Google Scholar]
- Beck, A. T. , Weissman A. N., Brown G., and Steer R.. 1991. “Factor Analysis of the Dysfunctional Attitude Scale in a Clinical Population.” Psychological Assessment 3, no. 3: 478–483. [Google Scholar]
- Best, M. W. , and Bowie C. R.. 2022. “Social Exclusion in Psychotic Disorders: An Interactional Processing Model.” Schizophrenia Research 244: 91–100. 10.1016/j.schres.2022.05.016. [DOI] [PubMed] [Google Scholar]
- Beutel, M. E. , Klein E. M., Brähler E., et al. 2017. “Loneliness in the General Population: Prevalence, Determinants and Relations to Mental Health.” BMC Psychiatry 17, no. 1: 97. 10.1186/s12888-017-1262-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bland, J. M. , and Altman D. G.. 1995. “Statistics Notes: Multiple Significance Tests: The Bonferroni Method.” British Medical Journal 310, no. 6973: 170. 10.1136/bmj.310.6973.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornheimer, L. A. , Wastler H., Li Verdugo J., et al. 2023. “Depression, Suicide Intent, and Plan Among Adults Presenting in an Emergency Department After Making a Suicide Attempt: Exploratory Differences by Psychosis Symptom Experience.” Journal of Psychiatric Research 157: 197–201. 10.1016/j.jpsychires.2022.11.033. [DOI] [PubMed] [Google Scholar]
- Boyer, L. , Cermolacce M., Dassa D., et al. 2012. “Neurocognition, Insight and Medication Nonadherence in Schizophrenia: A Structural Equation Modeling Approach.” PLoS One 7, no. 10: e47655. 10.1371/journal.pone.0047655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo, J. T. , and Hawkley L. C.. 2009. “Perceived Social Isolation and Cognition.” Trends in Cognitive Sciences 13, no. 10: 447–454. 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campellone, T. R. , Sanchez A. H., Fulford D., and Kring A. M.. 2019. “Defeatist Performance Beliefs in College Students: Transdiagnostic Associations With Symptoms and Daily Goal‐Directed Behavior.” Psychiatry Research 272: 149–154. 10.1016/j.psychres.2018.12.045. [DOI] [PubMed] [Google Scholar]
- Chau, A. K. C. , So S. H., Sun X., et al. 2022a. “A Network Analysis on the Relationship Between Loneliness and Schizotypy.” Journal of Affective Disorders 311: 148–156. 10.1016/j.jad.2022.05.057. [DOI] [PubMed] [Google Scholar]
- Chau, A. K. C. , So S. H., Sun X., et al. 2022b. “The Co‐Occurrence of Multidimensional Loneliness With Depression, Social Anxiety and Paranoia in Non‐clinical Young Adults: A Latent Profile Analysis.” Frontiers in Psychiatry 13: 931558. 10.3389/fpsyt.2022.931558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau, A. K. C. , Zhu C., and So S. H.‐W.. 2019. “Loneliness and the Psychosis Continuum: A Meta‐Analysis on Positive Psychotic Experiences and a Meta‐Analysis on Negative Psychotic Experiences.” International Review of Psychiatry 31, no. 5–6: 471–490. 10.1080/09540261.2019.1636005. [DOI] [PubMed] [Google Scholar]
- Cheung, J. H. , Burns D. K., Sinclair R. R., and Sliter M.. 2017. “Amazon Mechanical Turk in Organizational Psychology: An Evaluation and Practical Recommendations.” Journal of Business and Psychology 32, no. 4: 347–361. 10.1007/s10869-016-9458-5. [DOI] [Google Scholar]
- Christensen, R. , Haenschel C., Gaigg S. B., and Fett A.‐K. J.. 2022. “Loneliness, Positive, Negative and Disorganised Schizotypy Before and During the COVID‐19 Pandemic.” Schizophrenia Research: Cognition 29: 100243. 10.1016/j.scog.2022.100243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford, S. , Jewell R. M., and Waggoner P. D.. 2015. “Are Samples Drawn From Mechanical Turk Valid for Research on Political Ideology?” Research and Politics 2, no. 4: 205316801562207. 10.1177/2053168015622072. [DOI] [Google Scholar]
- Corcoran, C. M. , Kimhy D., Parrilla‐Escobar M. A., et al. 2011. “The Relationship of Social Function to Depressive and Negative Symptoms in Individuals at Clinical High Risk for Psychosis.” Psychological Medicine 41, no. 2: 251–261. 10.1017/S0033291710000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyle, C. E. , and Dugan E.. 2012. “Social Isolation, Loneliness and Health Among Older Adults.” Journal of Aging and Health 24, no. 8: 1346–1363. 10.1177/0898264312460275. [DOI] [PubMed] [Google Scholar]
- Crespi, B. , Dinsdale N., Read S., and Hurd P.. 2019. “Spirituality, Dimensional Autism, and Schizotypal Traits: The Search for Meaning.” PLoS One 14, no. 3: e0213456. 10.1371/journal.pone.0213456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devoe, D. J. , Cadenhead K. S., Cornblatt B., Granholm E., and Addington J.. 2022. “Negative Symptoms: Associations With Defeatist Beliefs, Self‐Efficacy, and Maladaptive Schemas in Youth and Young Adults At‐Risk for Psychosis.” Behavioural and Cognitive Psychotherapy 50, no. 3: 298–311. 10.1017/S1352465821000461. [DOI] [PubMed] [Google Scholar]
- Fervaha, G. , Zakzanis K. K., Foussias G., Agid O., and Remington G.. 2015. “Distress Related to Subclinical Negative Symptoms in a Non‐clinical Sample: Role of Dysfunctional Attitudes.” Psychiatry Research 230, no. 2: 249–254. 10.1016/j.psychres.2015.09.002. [DOI] [PubMed] [Google Scholar]
- Fett, A.‐K. J. , Hanssen E., Eemers M., Peters E., and Shergill S. S.. 2022. “Social Isolation and Psychosis: An Investigation of Social Interactions and Paranoia in Daily Life.” European Archives of Psychiatry and Clinical Neuroscience 272, no. 1: 119–127. 10.1007/s00406-021-01278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca‐Pedrero, E. , Debbané M., Ortuño‐Sierra J., et al. 2018. “The Structure of Schizotypal Personality Traits: A Cross‐National Study.” Psychological Medicine 48, no. 3: 451–462. 10.1017/S0033291717001829. [DOI] [PubMed] [Google Scholar]
- Fowler, D. , Freeman D., Smith B., et al. 2006. “The Brief Core Schema Scales (BCSS): Psychometric Properties and Associations With Paranoia and Grandiosity in Non‐clinical and Psychosis Samples.” Psychological Medicine 36, no. 6: 749–759. 10.1017/S0033291706007355. [DOI] [PubMed] [Google Scholar]
- Fulford, D. , and Mueser K. T.. 2020. “The Importance of Understanding and Addressing Loneliness in Psychotic Disorders.” Clinical Psychology: Science and Practice 27, no. 4: 12383. 10.1111/cpsp.12383. [DOI] [Google Scholar]
- Gayer‐Anderson, C. , and Morgan C.. 2013. “Social Networks, Support and Early Psychosis: A Systematic Review.” Epidemiology and Psychiatric Sciences 22, no. 2: 131–146. 10.1017/S2045796012000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, L. , and Bentler P. M.. 1999. “Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria Versus New Alternatives.” Structural Equation Modeling: A Multidisciplinary Journal 6, no. 1: 1–55. 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huang, J. L. , Bowling N. A., Liu M., and Li Y.. 2015. “Detecting Insufficient Effort Responding With an Infrequency Scale: Evaluating Validity and Participant Reactions.” Journal of Business and Psychology 30, no. 2: 299–311. 10.1007/s10869-014-9357-6. [DOI] [Google Scholar]
- Käll, A. , Shafran R., Lindegaard T., et al. 2020. “A Common Elements Approach to the Development of a Modular Cognitive Behavioral Theory for Chronic Loneliness.” Journal of Consulting and Clinical Psychology 88, no. 3: 269–282. 10.1037/ccp0000454. [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer R. L., and Williams J. B. W.. 2001. “The PHQ‐9: Validity of a Brief Depression Severity Measure.” Journal of General Internal Medicine 16, no. 9: 606–613. 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwapil, T. R. , Gross G. M., Silvia P. J., Raulin M. L., and Barrantes‐Vidal N.. 2018. “Development and Psychometric Properties of the Multidimensional Schizotypy Scale: A New Measure for Assessing Positive, Negative, and Disorganized Schizotypy.” Schizophrenia Research 193: 209–217. 10.1016/j.schres.2017.07.001. [DOI] [PubMed] [Google Scholar]
- Kwapil, T. R. , Kemp K. C., Mielock A., et al. 2020. “Association of Multidimensional Schizotypy With Psychotic‐Like Experiences, Affect, and Social Functioning in Daily Life: Comparable Findings Across Samples and Schizotypy Measures.” Journal of Abnormal Psychology 129, no. 5: 492–504. 10.1037/abn0000522. [DOI] [PubMed] [Google Scholar]
- Lenzenweger, M. F. 2018. “Schizotypy, Schizotypic Psychopathology, and Schizophrenia: Hearing Echoes, Leveraging Prior Advances, and Probing New Angles.” Schizophrenia Bulletin 44, no. suppl_2: S564–S569. 10.1093/schbul/sby083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubben, J. , Blozik E., Gillmann G., et al. 2006. “Performance of an Abbreviated Version of the Lubben Social Network Scale Among Three European Community‐Dwelling Older Adult Populations.” Gerontologist 46, no. 4: 503–513. 10.1093/geront/46.4.503. [DOI] [PubMed] [Google Scholar]
- Michalska da Rocha, B. , Rhodes S., Vasilopoulou E., and Hutton P.. 2018. “Loneliness in Psychosis: A Meta‐Analytical Review.” Schizophrenia Bulletin 44, no. 1: 114–125. 10.1093/schbul/sbx036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr, C. , and Claridge G.. 2015. “Schizotypy—Do Not Worry, It Is Not All Worrisome.” Schizophrenia Bulletin 41, no. suppl 2: S436–S443. 10.1093/schbul/sbu185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polner, B. , Simor P., and Kéri S.. 2018. “Insomnia and Intellect Mask the Positive Link Between Schizotypal Traits and Creativity.” PeerJ 6: e5615. 10.7717/peerj.5615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . 2021. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. https://www.R‐project.org/. [Google Scholar]
- Rumas, R. , Shamblaw A. L., Jagtap S., and Best M. W.. 2021. “Predictors and Consequences of Loneliness During the COVID‐19 Pandemic.” Psychiatry Research 300: 113934. 10.1016/j.psychres.2021.113934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, D. W. 1996. “UCLA Loneliness Scale (Version 3): Reliability, Validity, and Factor Structure.” Journal of Personality Assessment 66, no. 1: 20–40. 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Schlosser, D. A. , Campellone T. R., Biagianti B., et al. 2015. “Modeling the Role of Negative Symptoms in Determining Social Functioning in Individuals at Clinical High Risk of Psychosis.” Schizophrenia Research 169, no. 1–3: 204–208. 10.1016/j.schres.2015.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvia, P. J. , and Kwapil T. R.. 2011. “Aberrant Asociality: How Individual Differences in Social Anhedonia Illuminate the Need to Belong: Social Anhedonia.” Journal of Personality 79, no. 6: 1315–1332. 10.1111/j.1467-6494.2010.00702.x. [DOI] [PubMed] [Google Scholar]
- Sorenson, R. P. , Rossell S. L., and Sumner P. J.. 2021. “Exploring the Associations Between Dimensions of Schizotypy and Social Defeat.” Psychosis 1–11: 306–316. 10.1080/17522439.2021.2014943. [DOI] [Google Scholar]
- Spitzer, R. L. , Kroenke K., Williams J. B. W., and Löwe B.. 2006. “A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD‐7.” Archives of Internal Medicine 166, no. 10: 1092. 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stain, H. J. , Galletly C. A., Clark S., et al. 2012. “Understanding the Social Costs of Psychosis: The Experience of Adults Affected by Psychosis Identified Within the Second Australian National Survey of Psychosis.” Australian and New Zealand Journal of Psychiatry 46, no. 9: 879–889. 10.1177/0004867412449060. [DOI] [PubMed] [Google Scholar]
- Steiger, J. H. 2007. “Understanding the Limitations of Global Fit Assessment in Structural Equation Modeling.” Personality and Individual Differences 42, no. 5: 893–898. 10.1016/j.paid.2006.09.017. [DOI] [Google Scholar]
- Tan, M. , Shallis A., and Barkus E.. 2020. “Social Anhedonia and Social Functioning: Loneliness as a Mediator.” PsyCh Journal 9, no. 2: 280–289. 10.1002/pchj.344. [DOI] [PubMed] [Google Scholar]
- Wang, Y. , Neumann D. L., Shum D. H. K., et al. 2013. “Cognitive Empathy Partially Mediates the Association Between Negative Schizotypy Traits and Social Functioning.” Psychiatry Research 210, no. 1: 62–68. 10.1016/j.psychres.2013.03.015. [DOI] [PubMed] [Google Scholar]
- Williams, L. M. , and Irwin H. J.. 1991. “A Study of Paranormal Belief, Magical Ideation as an Index of Schizotypy and Cognitive Style.” Personality and Individual Differences 12, no. 12: 1339–1348. 10.1016/0191-8869(91)90210-3. [DOI] [Google Scholar]
- Winterstein, B. P. , Silvia P. J., Kwapil T. R., Kaufman J. C., Reiter‐Palmon R., and Wigert B.. 2011. “Brief Assessment of Schizotypy: Developing Short Forms of the Wisconsin Schizotypy Scales.” Personality and Individual Differences 51, no. 8: 920–924. 10.1016/j.paid.2011.07.027. [DOI] [Google Scholar]
- Zahid, A. , and Best M. W.. 2023. “Examining Cognitive Biases Uniquely Associated With Schizotypy.” Psychopathology 1–11: 462–472. 10.1159/000529742. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Figures.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


