Abstract
BACKGROUND:
Helminthic infections are a major health burden worsened by inadequate health education and awareness among schoolchildren. This study aims to reduce helminthic infection by increasing awareness and knowledge through school nurse-led health education among primary schoolchildren in Bangladesh.
MATERIALS AND METHODS:
This was a prospective, open-label, parallel-group (1:1), cluster non-randomized controlled trial conducted on 5- to 12-year-old school-going children from September 2021 to September 2022 in rural Bangladesh. Trained school nurses provided evidence-based health education to the children from the intervention group (IG) for 9 months to improve awareness and knowledge regarding helminthic infection, whereas another group did not receive any health education during intervention periods, except for usual care. Data were analyzed by the Chi-square test and regression analysis.
RESULTS:
Overall, 455 children (control group (CG), n = 220; IG, n = 235) completed the entire study. Changes in the prevalence of helminthic infection—the primary outcome—were significant (P < 0.001). Concerning the secondary outcome, the adjusted endline data with baseline and sociodemographic data, the children’s health-related hygiene behavior (P < 0.001) and awareness and knowledge regarding helminthic infection (P < 0.001) were improved significantly in the IG than the CG.
CONCLUSION:
The school nurse-led health education program encouragingly reduced helminthic infection and improved primary schoolchildren’s awareness and knowledge of helminthic infection according to the World Health Organization (WHO) health policy. In the future, health policymakers may take initiatives to recruit school nurses to sustainably establish child health education programs.
Keywords: Awareness, child, health education, hygiene, knowledge, school nursing
Introduction
Helminthic infection is the worst infectious infestation among children worldwide which is aggravated by nutritional disorders.[1] In many countries, children are at high risk of helminthic infection posing a vital threat.[2,3] Controlling and/or eliminating helminthic infection till now remains a part of the global health challenge.[4,5] However, this health issue is preventable by drug administration and ensuring high-quality care for children. Subsequently, the World Health Organization (WHO) is working to diminish helminthic infection by addressing the quality and primary care services for children.[6] Several developed countries have controlled helminthic infection through effective public sanitation practices and various primary healthcare programs[7,8]; however, these infections are still widespread in low- and middle-income countries (LMICs),[9] and often, drug administration program does not cover the whole population to protect against rapid re-infection. Besides, children are more vulnerable and exposed to unhygienic environments due to unsafe water supplies, poor sanitation, and lack of adequate health facilities, which increases their risk of suffering from helminthic infection.[2,10,11,12] The WHO stated that around 46 million children between 1 and 14 years are at risk of helminthic infection, whereas the highest prevalence of helminthic infection infected (Ascaris 25%; Trichuris 22%) school-aged children from Southeast Asia.[13] Although, since 2008, Bangladesh has implemented nationally biannual mass drug administration for helminthic infection, however, evidence from this country shows that nationally both in urban (41.7%)[14] and in rural (39.2%)[15] of school-aged children between the ages of 5–13 were infested with a minimum of one species of helminth, and this issue reflects that deworming program was not fully successful[16] due to overpopulation, lack of proper health assessment, laboratory investigation, case detection, and health education by a healthcare professional.[2,11]
Furthermore, children who are suffering from helminthic infection develop the risk of recurrent infections which leads to poorer academic performance.[17] Besides, the considerable reasons are socioeconomic status, poor personal hygiene, unsanitary/unhygienic food, water treatment in daily life, movement toward development, and low health literacy.[10,11,18] In addition, it is globally revealed that to minimize child helminthic infection, health promotion, prevention, and healthcare services are significant requirements for children.[12] The previous research states that evidence-based educational intervention in school areas by school nurses is particularly significant, for developing longer-term sustainable, positive behavioral changes, and improving awareness among school-going children.[12,19] Furthermore, the risk of child infection is also associated with parental educational determinants which are very crucial.[20] Health education to minimize the knowledge gap among the children, including their parents, is significant, especially in the school areas.[19] In contrast, in Bangladesh, hygiene and sanitation conditions in households (48.8%) and schools (21.4%) of school-aged children are poor, and school health services are remarkably deprived.
Besides, in Bangladesh, school health services are very deprived, especially regarding the improvement of awareness among children, including their parents, about their health status to prevent helminthic infection. For educating, assessing, and screening the health status of the school-aged children, school nurse placement in the school is crucial. Thus, we developed a Health Awareness Program for Primary Schoolchildren (HAPSC) with scientific recommendations and implemented an interventional study involving the pilot placement of trained school nurses in a school setting in Bangladesh to provide evidence-based health education to primary schoolchildren and their parents. This research finding magnificently evaluated the significant effects of the intervention which can influence the school nurse-led health services in Bangladesh. Therefore, for the first time, we developed a project to introduce trained school nurses into the primary school environment in Bangladesh. This study aims to reduce helminthic infection by increasing awareness and knowledge through school nurse-led health education among primary schoolchildren in Bangladesh. Thus, we hypothesized that the placement of school nurses and evidence-based health education will have a significant impact on the increasing health awareness and knowledge of primary schoolchildren to prevent helminthic infection.
Materials and Methods
Study design and setting
This is a prospective, open-label, parallel-group (1:1), cluster non-randomized controlled trial (NRCT), with pre- and post-test design study, and registered by the Clinical Trial Registry. The study outline and outcomes are shown in Figure 1. This study was conducted from September 2021 to September 2022 in four governmental primary schools in the rural North Matlab, Chandpur District, Bangladesh. Those schools were selected purposively from two Unions called Ekhlaspur and Jahirabad, and the distance between those Unions was around 5.4 kilometers.
Figure 1.
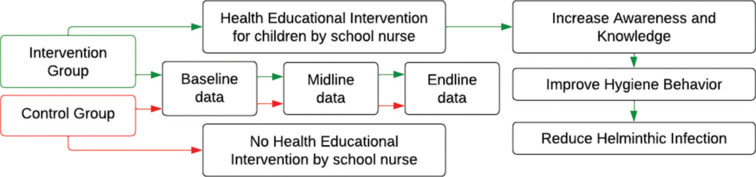
Study outline and outcomes
Study participants and sampling
The study participants were primary schoolchildren (1 to 5 grades). The researcher was introduced to the children and collected their basic information through schools’ authorities. Then, the community health workers (CHWs) visited their houses, described study details, checked the eligibility criteria, and enrolled children based on their interests to participate actively, including their parents’ consent. The details regarding the study procedure and quality control were documented elsewhere.[21]
The study sample size was 110 for both groups, which was calculated by G*Power software (version 3.1.9.4), considering that the effect size and confidence level were 0.70 and 0.95, respectively. However, the researcher invited all the children to participate and the sample size was 604. In addition, the children from grade 5 were not available after baseline data collection because during this period, they completed their primary education and had to move to different schools. Therefore, the total sample size was 455, the intervention group (IG) had 235, and the control group (CG) had 220 children from 1 to 4 grades.
Health education
Intervention group
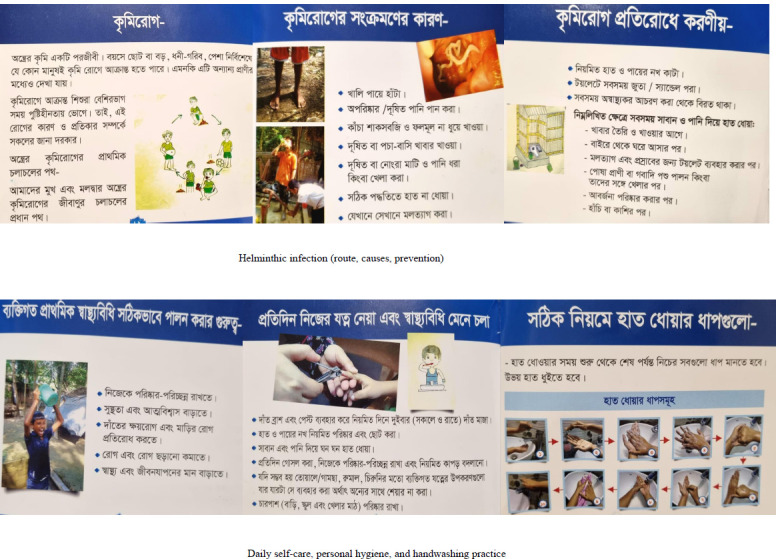
The IG received 9 months (one session per week except for vacations) of health education through various methods in the children’s classroom. All the sessions were organized based on playing and having fun for the children which were effective ways to provide health education among the children. The face-to-face sessions were conducted, such as asking questions, small group discussions, roleplay, group work, and hands-on practical sessions during the intervention period. Each session was conducted for a maximum of 45 minutes. Health education was evidence-based and conducted through a HAPSC regarding helminthic infection which was developed by researchers. The educational content was prepared by following the WHO guidelines for helminthic infection control. The educational contents related to helminthic infection (route, causes, prevention) included daily self-care, personal hygiene, and handwashing practice.[16] Demonstration and practice of handwashing was performed followed by the poster developed by WHO, patient safety, and saving lives together.[22] Based on this, the researcher developed a few health education materials (booklet, health record notebook, short message leaflet, and poster) [Supplementary Appendix 1] for the children. Additionally, other educational materials were used, such as pictures, soap, and the light-emitting diode (LED) handwashing checker machine with lotion (Saraya Co., Ltd, Japan). This handwashing checker with lotion is an advanced technology that was invented in Japan and used to ensure proper handwashing techniques for confirming handwash. The child’s parents (parents/legal guardians) were involved in the health education twice during the first month and once a month throughout interventional periods by CHWs.
The health education was conducted by trained school nurses and their assistants who were specially trained for this study. The skilled registered nurses (faculty members) from a reputed nursing college in Bangladesh have conducted training sessions among undergraduate nursing students. Then, they were allocated on a part-time basis at the IG to be performed as assistants to the school nurse and the CHWs received training for this study from the school nurses.
Control group
The CG attended health assessment at baseline and endline and provided survey information at baseline, midline, and endline. Educational materials were shared and briefly explained to them after the completion of endline data collection.
Data collection tool and technique
Stool examination
The child’s parent or legal guardian was informed about the way to collect their child’s morning fresh stool samples at home, and for that, one separate and individually labeled container with tight covers was provided to them 1 day before data collection during both baseline and endline. Then, they requested to bring the samples to the school area on specific days, and after receiving the stool sample, CHWs put it into the cooler box and transferred it to the diagnostic center for laboratory tests. If necessary, the parents received reminder telephone calls from the CHWs. If they were not able to bring it back within the requested days and the CHWs were not able to communicate with them, the researcher was classified as non-respondent.
Research instruments
The researcher developed a survey form that was pretested and used to collect data from the children. They were asked about their hygiene-related behavior in the past 7 days of practice using a 5-point Likert scale running from 1 = never to 5 = every time. The higher scores represented better hygiene behavior, and Cronbach’s alpha was 0.874. It included the frequency of brushing teeth (in the morning and night) using toothbrush and toothpaste, using personal self-care items (such as towel, handkerchief, and comb), noticing the expiration date/rotten or quality when eating food, washing hands with soap and water before eating food, after defecation and coming home from outside, washing fruits/vegetables before eating, using sandal at while playing outdoors and go to the toilet, and the habit of biting nails by teeth. Awareness and knowledge regarding helminthic infection (10 questions) were asked through a quiz test questionnaire for the children. The response was categorized into, 0 = do not know, 1 = no, and 2 = yes. Therefore, the minimum score and maximum score were 0 and 10, whereas the higher score indicates better knowledge and Cronbach’s alpha was 0.856.
Data analysis
In this study, the per-protocol set analysis was used. The independent and categorical variables were expressed in frequencies and percentages through a suitable test, such as descriptive analysis and Chi-square (χ2) test. To explore the changes between groups regarding helminthic infection, the Chi-square test was performed by the statistical software package SPSS for Windows (version 26.0, Armonk IBM Co.). To compare the intervention effects between groups, regression analysis was used, whereas groups as independent variables, data related to child’s awareness and knowledge regarding helminthic infection, and hygiene behavior at the endline as dependent variables, baseline data were considered as the covariate. For non-normally distributed data, a gamma distribution was used and the link function was log with added 0.5 before calculation. These analyses were performed using the software R version 4.2 (R Foundation). The significance level was set at ˂ 0.05.
Ethical consideration
This study was approved by the Institutional Review Board (2021/OR-NSU/IRB/0701) of North South University in Bangladesh. Before enrollment, we obtained verbal assent from all the children and written informed consent from their parents (or legal guardian). All the children and their parents were informed sincerely about the research purpose, privacy, anonymity, no/minimal risk to participate in this study, and their right to withdraw from the study at any point without explanation.
Results
A total of 455 children participated till the endline data collection, and among them, 235 children from the IG and 220 children from the CG completed the entire study. During baseline, 140 and 123 children were female in the IG and CG, respectively. Most of the children’s monthly family income was 10,000–20,000 BDT (100 USD–200 USD), and tin shades and mud were used in their house walls and floors in both groups, respectively. Furthermore, in baseline, >50% of the children did not take any treatment medicine for helminthic infection [Table 1]. Although health-related hygiene behavior among the children was improved gradually at each time point in both groups, however, the children from the IG improved their hygiene behavior better than the CG [Figure 2]. Moreover, the children’s hygiene behavior related to the prevention of helminthic infection (handwashing practice, using footwear in the toilet, and brushing teeth) was improved more at the endline.
Table 1.
Sociodemographic data of the children with the prevalence of helminthic infection at each time point in the groups (n=455)
| Variables | Intervention group=235 | Control group=220 | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||||||||||||||||
| Helminthic infection | Baseline, n=(%) | P | Endline, n=(%) | P<0.001§ | Baseline, n=(%) | P | Endline, n=(%) | P 0.284§ | ||||||||||||||||||
|
|
|
|
|
|||||||||||||||||||||||
| Positive (n=25 (10.6)) | Negative | Positive (n=13 (5.5)) | Negative | Positive (n=17 (7.7)) | Negative | Positive (n=52 (23.6)) | Negative | |||||||||||||||||||
| Gender | Male | 8 (32.0) | 87 (41.4) | 0.364 | 1 (7.7) | 94 (42.3) | 0.013* | 11 (64.7) | 86 (42.4) | 0.075 | 19 (36.5) | 78 (46.4) | 0.209 | |||||||||||||
| Female | 17 (68.0) | 123 (58.6) | 12 (92.3) | 128 (57.7) | 6 (35.3) | 117 (57.6) | 33 (63.5) | 90 (53.6) | ||||||||||||||||||
| Age | 5 | 0.790 | 1 (5.9) | 0 (0.0) | 0.023* | 0 (0.0) | 1 (0.6) | 0.647 | ||||||||||||||||||
| 6 | 2 (8.0) | 13 (6.2) | 0.740 | 2 (15.4) | 13 (5.9) | 5 (29.4) | 28 (13.8) | 8 (15.4) | 25 (14.9) | |||||||||||||||||
| 7 | 5 (20.0) | 45 (21.4) | 3 (23.1) | 47 (21.2) | 3 (17.6) | 40 (19.7) | 10 (19.2) | 33 (19.6) | ||||||||||||||||||
| 8 | 7 (28.0) | 50 (23.8) | 2 (15.4) | 55 (24.8) | 2 (11.8) | 49 (24.1) | 10 (19.2) | 41 (24.4) | ||||||||||||||||||
| 9 | 3 (12.0) | 50 (23.8) | 2 (15.4) | 51 (23.0) | 3 (17.6) | 45 (22.2) | 10 (19.2) | 38 (22.6) | ||||||||||||||||||
| 10 | 6 (24.0) | 41 (19.5) | 3 (23.1) | 44 (19.8) | 2 (11.8) | 29 (14.3) | 11 (21.2) | 20 (11.9) | ||||||||||||||||||
| 11 | 1 (4.0) | 9 (4.3) | 1 (7.7) | 9 (4.1) | 1 (5.9) | 8 (3.9) | 3 (5.8) | 6 (3.6) | ||||||||||||||||||
| 12 | 1 (4.0) | 2 (1.0) | 0 (0.0) | 3 (1.4) | 0 (0.0) | 4 (2.0) | 0 (0.0) | 4 (2.4) | ||||||||||||||||||
| Monthly family income | <10,000 BDT | 9 (36.0) | 92 (43.8) | 4 (30.8) | 97 (43.7) | 3 (17.6) | 83 (40.9) | 20 (38.5) | 66 (39.3) | |||||||||||||||||
| 10,000 – 20,000 BDT | 11 (44.0) | 91 (43.3) | 7 (53.8) | 95 (42.8) | 8 (47.1) | 103 (50.7) | 24 (46.2) | 87 (51.8) | ||||||||||||||||||
| > 20,000 BDT | 5 (20.0) | 27 (12.9) | 2 (15.4) | 30 (13.5) | 6 (35.3) | 17 (8.4) | 8 (15.4) | 15 (8.9) | ||||||||||||||||||
| Material used for house wall | Mud | 1 (4.0) | 4 (1.9) | 0.507 | 0 (0.0) | 5 (2.3) | 0.195 | 0 (0.0) | 1 (0.5) | 0.933* | 0 (0.0) | 1 (0.6) | 0.468 | |||||||||||||
| Tin shade/tin house | 23 (92.0) | 185 (88.1) | 10 (76.9) | 198 (89.2) | 16 (94.1) | 187 (92.1) | 50 (96.2) | 153 (91.1) | ||||||||||||||||||
| Others (cement/concrete or brick and wooden) | 1 (4.0) | 21 (10.0) | 3 (23.1) | 19 (8.6) | 1 (5.9) | 15 (7.4) | 2 (3.8) | 14 (8.3) | ||||||||||||||||||
| Material used for house floor | Mud | 19 (76.0) | 149 (71.0) | 0.499 | 8 (61.5) | 160 (72.1) | 0.692 | 14 (82.4) | 139 (68.5) | 0.382 | 44 (84.6) | 109 (64.9) | 0.013* | |||||||||||||
| Cement/concrete or brick | 6 (24.0) | 50 (23.8) | 4 (30.8) | 52 (23.4) | 3 (17.6) | 50 (24.6) | 8 (15.4) | 45 (26.8) | ||||||||||||||||||
| Others (tiles or wooden) | 0 (0.0) | 11 (5.2) | 1 (7.7) | 10 (4.5) | 0 (0.0) | 14 (6.9) | 0 (0.0) | 14 (8.3) | ||||||||||||||||||
| Type of toilet use | Open toilet | 0 (0.0) | 5 (2.4) | 0.517 | 1 (7.7) | 4 (1.8) | 0.294 | 0 (0.0) | 3 (1.5) | 0.886 | 1 (1.9) | 2 (1.2) | 0.418 | |||||||||||||
| Own sanitary latrine inside home | 2 (8.0) | 34 (16.2) | 3 (23.1) | 33 (14.9) | 4 (23.5) | 36 (17.7) | 10 (19.2) | 30 (17.9) | ||||||||||||||||||
| Own sanitary latrine outside home | 15 (60.0) | 122 (58.1) | 5 (38.5) | 132 (59.5) | 8 (47.1) | 107 (52.7) | 31 (59.6) | 84 (50.0) | ||||||||||||||||||
| Shared sanitary latrine | 8 (32.0) | 49 (23.3) | 4 (30.8) | 53 (23.9) | 5 (29.4) | 57 (28.1) | 10 (19.2) | 52 (31.0) | ||||||||||||||||||
| Accessibility of handwashing with soap and water in the toilet | Inside the toilet | 3 (12.0) | 67 (31.9) | 0.024* | 7 (53.8) | 63 (28.4) | 0.278 | 4 (23.5) | 37 (18.2) | 0.913 | 9 (17.3) | 32 (19.0) | 0.945 | |||||||||||||
| Near to the toilet’s outside | 10 (40.0) | 76 (36.2) | 3 (23.1) | 83 (37.4) | 6 (35.3) | 86 (42.4) | 23 (44.2) | 69 (41.1) | ||||||||||||||||||
| Far from the toilet | 6 (24.0) | 16 (7.6) | 1 (7.7) | 21 (9.5) | 1 (5.9) | 15 (7.4) | 3 (5.8) | 13 (7.7) | ||||||||||||||||||
| Not available | 6 (24.0) | 51 (24.3) | 2 (15.4) | 55 (24.8) | 6 (35.3) | 65 (32.0) | 17 (32.7) | 54 (32.1) | ||||||||||||||||||
| Have any cattle or pets in house | Yes | 18 (72.0) | 137 (65.2) | 0.500 | 9 (69.2) | 146 (65.8) | 0.798 | 14 (82.4) | 148 (72.9) | 0.396 | 44 (84.6) | 118 (70.2) | 0.040* | |||||||||||||
| No | 7 (28.0) | 73 (34.8) | 4 (30.8) | 76 (34.2) | 3 (17.6) | 55 (27.1) | 8 (15.4) | 50 (29.8) | ||||||||||||||||||
| Dispose of household wastes | Anywhere near to house | 20 (80.0) | 143 (68.1) | 0.293 | 9 (69.2) | 154 (69.4) | 0.342 | 12 (70.6) | 142 (70.0) | 0.880 | 38 (73.1) | 116 (69.0) | 0.580 | |||||||||||||
| Anywhere far from the house | 4 (16.0) | 63 (30.0) | 3 (23.1) | 64 (28.8) | 5 (29.4) | 58 (28.6) | 14 (26.9) | 49 (29.2) | ||||||||||||||||||
| Appropriate place | 1 (4.0) | 4 (1.9) | 1 (7.7) | 4 (1.8) | 0 (0.0) | 3 (1.5) | 0 (0.0) | 3 (1.8) | ||||||||||||||||||
| Child take any treatment medicine for intestinal worm infestation (during the last 6 months) | Do not know | 0 (0.0) | 3 (1.4) | 0.439 | 0 (0.0) | 1 (0.5) | 0.953 | |||||||||||||||||||
| Yes | 5 (20.0) | 64 (30.5) | 6 (35.3) | 74 (36.5) | ||||||||||||||||||||||
| No | 20 (80.0) | 143 (68.1) | 11 (64.7) | 128 (63.1) | ||||||||||||||||||||||
§=P value evaluated by the Chi-square test between the groups at baseline and endline. *=P<0.05
Figure 2.
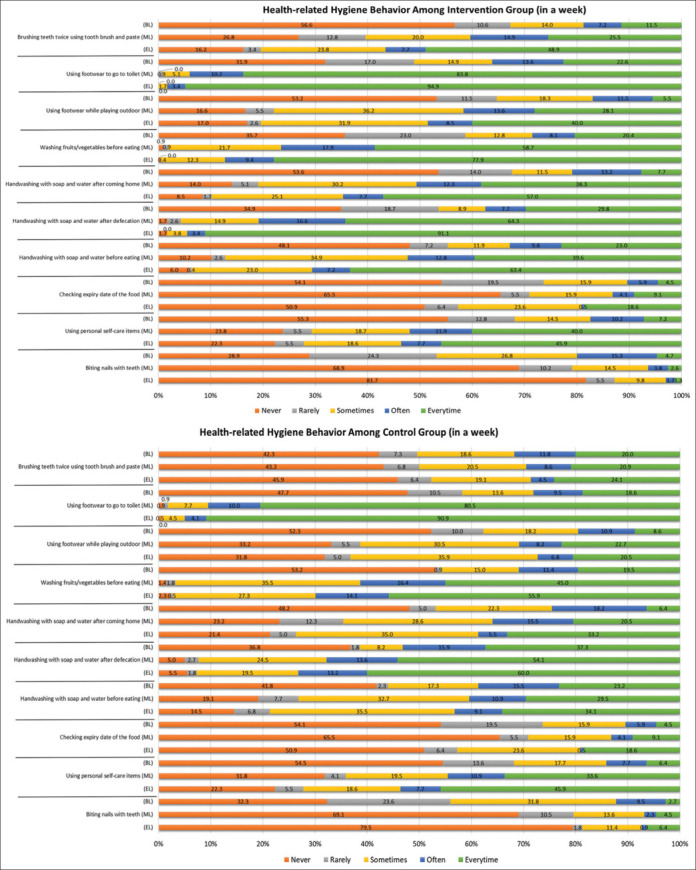
Changes in the frequency of health-related hygiene behaviors among the children at baseline, midline, and endline in both groups (n = 455)
The prevalence of helminthic infection was reduced compared with baseline 25 (10.6%) to endline 13 (5.5%) in the IG, whereas during baseline 17 (7.1%) to endline 52 (23.6%) in the CG, it was statistically significant (P < 0.001) [Table 1]. Subsequently, the female children were more vulnerable to getting infected by the helminthic infection within each group, except in the CG at baseline; however, in the IG, the total number of helminth-infected children was reduced significantly (P = 0.013) among both male and female participants [Table 1].
Regarding awareness and knowledge concerning helminthic infection, the gamma regression analysis revealed that the IG had a significant positive effect at both midline (Exp(β) = 1.858, SE = 0.044, t = 14.246, P < .001) and endline (Exp(β) = 2.592, SE = 0.044, t = 21.684, P < .001), after adjusting with the baseline [Table 2].
Table 2.
Awareness and knowledge changes regarding hygiene between the groups (n=455)
| Outcome variable | 95% CI |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficients | Exp β (Estimate) | Low | High | Std. error | t | P | ||||||||
| Awareness and knowledge related to hygiene | ||||||||||||||
| Midline | (Intercept) | 3.985 | 3.665 | 4.336 | 0.042 | 32.734 | <0.001*** | |||||||
| Group | 1.858 | 1.706 | 2.024 | 0.044 | 14.246 | <0.001*** | ||||||||
| Baseline | 1.006 | 0.990 | 1.021 | 0.008 | 0.722 | 0.471 | ||||||||
| Endline | (Intercept) | 3.558 | 3.277 | 3.872 | 0.043 | 29.775 | <0.001*** | |||||||
| Group | 2.592 | 2.377 | 2.823 | 0.044 | 21.684 | <0.001*** | ||||||||
| Baseline | 0.997 | 0.981 | 1.013 | 0.008 | -0.363 | 0.717 | ||||||||
General liner model: family=Gamma (link=log). Note, CI=confidence interval; Std. error=standard error, *<0.05, **<0.01, ***<0.001
Regarding hygiene behavior, the gamma regression analysis indicated that the IG had significant positive effects on the midline (Exp(β) = 1.105, SE = 0.018, t = 5.585, P < 0.001) and endline (Exp(β) =1.164, SE = 1.164, t = 10.058, P < 0.001) after adjusting with the baseline [Table 3].
Table 3.
Hygiene behavior changes between groups (n=455)
| Outcome variable | Coefficients | Exp β (Estimate) | 95% CI |
Std. error | t | P | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low | High | |||||||||||||
| Hygiene behavior | ||||||||||||||
| Midline | (Intercept) | 33.691 | 32.008 | 35.481 | 0.026 | 133.859 | <0.001*** | |||||||
| Group | 1.105 | 1.067 | 1.146 | 0.018 | 5.585 | <0.001*** | ||||||||
| Baseline | 1.000 | 0.998 | 1.002 | 0.001 | 0.059 | 0.953 | ||||||||
| Endline | (Intercept) | 36.439 | 34.883 | 38.054 | 0.015 | 244.032 | <0.001*** | |||||||
| Group | 1.164 | 1.129 | 1.198 | 1.164 | 10.058 | <0.001*** | ||||||||
| Baseline | 1.000 | 1.002 | 1.001 | 0.003 | -0.012 | 0.551 | ||||||||
General liner model: family=Gamma (link=log). Note, CI=confidence interval; Std. error=standard error, *<0.05, **<0.01, ***<0.001
Discussion
The purpose of this study was to reduce helminthic infection by increasing awareness and knowledge through school nurse-led health education among primary schoolchildren in Bangladesh. The school nurse-led evidence-based health educational intervention was conducted first time in Bangladesh.
The study results exposed the satisfactory changes in the prevalence of child helminthic infection between the groups at the endline which was statistically significant. We conducted the educational intervention in the school area according to prior several successful school-based interventional research.[19,23] In this study, during endline, the total number of helminth-infected children was increased (23.6%) in the CG; however, in the IG the total number of helminth-infected children was reduced (5.5%) successfully. We found that the majority of the helminth-infected children from both groups were female. Besides, the previous studies had contradictory findings, whereas male children are more affected by helminthic infection than females.[24,25] According to the expert opinion, the prevalence of soil-transmitted helminths among school-aged children was reduced from 79.8% to 14.0% in Bangladesh.[26]
However, in 2018, the prevalence of helminth-infected children was 41.7% and 39.2% among school-aged children in Bangladesh.[14,15] Furthermore, currently a large number of children (36.78%–60.7%) from LMICs, particularly in poor resource settings, suffer from the high prevalence of helminthic infection which impacts child growth and development.[27,28] Subsequently, the evidence states that helminth-infected children had poor academic performance which was unmeasured in our study.[17]
Household socioeconomic status, including proper housing conditions with basic amenities, is essential and a strong confounder for healthy hygiene practices.[29,30] Our study findings could be influenced by the children’s socioeconomic status and housing conditions, such as household flooring materials and the practice of household waste disposal. According to this study result, most of the helminth-infected children were within 10 years old with cattle or pets in their houses. Although they had their sanitary latrine outside of their home and had handwashing accessibility with soap and water near the toilets outside, however, they disposed of household waste anywhere near their house. The previous study had similar findings that children within 8 years old were infected by helminthic and the factors were significantly associated with age, poverty, maternal educational level, household overcrowding, and having a latrine and presence of infected siblings or members in the household.[31] Furthermore, we found that not all the children from this study area were able to get anthelminthic treatment according to the mass drug administration, whereas the previous researcher suggested to evaluate the critical gaps and actions required with strong collaborations among different field experts to control and/or elimination of child helminthic infection.[4]
This study result showed that correspondingly, the health-related hygiene behavior improved by the educational intervention among the children from the IG compared with the CG at each time point. The previous studies state that, less fingernail hygiene, using an open latrine, not practicing wearing shoes, no habit of washing fruits and vegetables, and irregular handwashing practice were considered as the focus area to minimize helminthic infection,[10,25] while we found that 37.4% of children improved their teeth brushing practice twice a day, and correspondingly, all the health-related hygiene behavior did improve by the educational intervention. Those improvements and significant differences were detected in the IG compared with the CG in midline and endline. The previous articles stated that improving hygiene behavior was vital with appropriate health awareness and knowledge to boost the prevention practice and reduce helminthic infection, especially for school-aged children,[8] whereas children’s parental educational determinants parents are essential to improving the children’s health and reducing the risk of child mortality.[11] Correspondingly, oral hygiene and proper handwashing practice had great effectiveness in reducing child helminthic infection.[32,33]
We exposed positive changes among the helminth-infected children at each time point (midline and endline) in the enhancement of hygiene behavior and improvement of awareness and knowledge regarding helminthic infection in the IG compared with the CG. Magnificently, health education is considered crucial in the healthcare system for children by healthcare personnel, especially in the school area.[34] According to prior research, school nurses are professionally unique healthcare provider with dynamic roles, their placement in the school setting shows in improving health behavior among the children,[35] and significant collaboration to promote health with other healthcare providers.[36,37] It also benefits the school by creating a healthy, supportive environment and positive child educational development. However, LMICs had poor resources to ensure sanitation in the school due to low socioeconomic conditions. This study’s outcomes revealed the improvement of the child’s awareness and knowledge related to health behavior from their early stages of life and the effectiveness of the school nurse placement system for all school settings.
Limitations and recommendations
This study has some limitations. The study site and schools were selected non-randomly and purposively. The study was conducted among four primary schools from a rural sub-district which did not represent the whole population in Bangladesh. Although the results of the prevalence of helminthic infection were significant, however, the results were affected by other possible factors:
When the baseline data were collected, the coronavirus disease 2019 (COVID-19) outbreak happened in Bangladesh, so every institute was closed and people were asked to stay home strictly.
During the intervention, the schools’ authorities and some parents became more aware of their child’s laboratory tests and the children might have medicine (antihelminthic) by them following Bangladesh government rules. The researcher did not get the actual information regarding the child’s medication and the time of medication in each group from the school authorities.
Conclusion
The school nurses-led evidence-based health education had a significant impact on reducing helminthic infection and increasing health awareness and knowledge of primary schoolchildren based on WHO guidelines for helminthic infection control. Those significant findings pointed to the effectiveness of school nurses’ placement and demand to health policymaker to expand the school nurse-led health education program for the children in the future.
Ethical approval statement
This study followed the ethical standards of the 1975 Helsinki Declaration (revised version 2013) and was approved by the Institutional Review Board (2021/OR-NSU/IRB/0701) of North South University in Bangladesh.
Clinical Trial Registration
NCT number: NCT05012592 (https://www.clinicaltrails.gov)
Participant’s consent statement
Written informed consent to publish this study was obtained from the children’s parents (or legal guardians) to publish this paper.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors cordially acknowledge all the participants for their active participation in the study. The authors thank all the institutes (Grameen Caledonian College of Nursing, Grameen Communications, and Jadur Kathi Bangladesh), including their staff, school nurses, school staff, and study members for their support.
Supplementary Appendix 1
Booklet
Funding Statement
This study was funded by the Grants-in-Aid for Scientific Research Program (KAKENHI), Japan (Kiban B, N0. 21H03250).
References
- 1.Degarege A, Erko B, Negash Y, Animut A. Intestinal Helminth infection, anemia, undernutrition and academic performance among schoolchildren in Northwestern Ethiopia. Microorganisms. 2022;10:1353. doi: 10.3390/microorganisms10071353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang D, Yang Y, Wang Y, Yang Y, Dong S, Chen Y, et al. Prevalence and risk factors of Ascaris lumbricoides, Trichuris trichiura and Cryptosporidium infections in elementary schoolchildren in southwestern China: A school-based cross-sectional study. Int J Environ Res Public Health. 2018;15:1–16. doi: 10.3390/ijerph15091809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chelkeba L, Mekonnen Z, Emana D, Jimma W, Melaku T. Prevalence of soil-transmitted helminths infections among preschool and school-age children in Ethiopia: A systematic review and meta-analysis. Glob Health Res Policy. 2022;7:1–23. doi: 10.1186/s41256-022-00239-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Specht S, Keiser J. Helminth infections: Enabling the World Health Organization road map. Int J Parasitol. 2023;53:411–4. doi: 10.1016/j.ijpara.2022.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Gonza'lez Quiroz DJ, Agudelo Lopez SdP, Arango CM, Acosta JEO, Bello Parias LD, Alzate LU, et al. Prevalence of soil transmitted helminths in school-aged children, Colombia, 2012–2013. PLoS Negl Trop Dis. 2020;14:e0007613. doi: 10.1371/journal.pntd.0007613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Montresor Id A, Mupfasoni D, Mikhailov A, Mwinzi P, Lucianez A, Jamsheed M, et al. The global progress of soil-transmitted helminthiases control in 2020 and World Health Organization targets for 2030. PLoS Negl Trop Dis. 2020;14:e0008505. doi: 10.1371/journal.pntd.0008505. doi: 10.1371/journal.pntd.0008505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hasegawa M, Pilotte N, Kikuchi M, Means AR, Papaiakovou M, Gonzalez AM, et al. What does soil-transmitted helminth elimination look like? Results from a targeted molecular detection survey in Japan. Parasit Vectors. 2020;13:1–11. doi: 10.1186/s13071-019-3875-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puspita WL, Khayan K, Hariyadi D, Anwar T, Wardoyo S, Ihsan BM. Health education to reduce helminthiasis: Deficits in diets in children and achievement of students of elementary schools at Pontianak, West Kalimantan. J Parasitol Res. 2020;2020:4846102. doi: 10.1155/2020/4846102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Budi Satria F. Stunting, micronutrient deficiencies, and worm infections among primary schoolchildren at low and lower-middle income countries in Asia and Africa: A systematic review. Cent African J Public Health. 2018;4:102. [Google Scholar]
- 10.Assemie MA, Shitu Getahun D, Hune Y, Petrucka P, Abebe AM, Telayneh AT, et al. Prevalence of intestinal parasitic infection and its associated factors among primary school students in Ethiopia: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2021;15:e0009379. doi: 10.1371/journal.pntd.0009379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sujan MSH, Islam MS, Naher S, Banik R, Gozal D. Predictors associated with knowledge and practice of helminthic infection prevention among rural school-aged children’s parents in Bangladesh: A cross-sectional study. Front Public Health. 2020;8:484. doi: 10.3389/fpubh.2020.00484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alharazi T, Aa Bamaga O, Al-Abd N, Alcantara JC. Intestinal parasitic infection: Prevalence, knowledge, attitude, and practices among schoolchildren in an urban area of Taiz city, Yemen. AIMS Public Health. 2019;7:769–77. doi: 10.3934/publichealth.2020059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Silver ZA, Kaliappan SP, Samuel P, Venugopal S, Kang G, Sarkar R, et al. Geographical distribution of soil transmitted helminths and the effects of community type in South Asia and South East Asia – A systematic review. PLoS Negl Trop Dis. 2018;12:e0006153. doi: 10.1371/journal.pntd.0006153. doi: 10.1371/journal.pntd.0006153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nath TC, Eom KS, Choe S, Mukutmoni M, Khanum H, Bhuiyan JU, et al. An update of intestinal helminth infections among urban slum communities in Bangladesh. IJID Reg. 2022;5:7. doi: 10.1016/j.ijregi.2022.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Afroz S, Debsarma S, Dutta S, Rhaman MM, Mohsena M. Prevalence of helminthic infestations among Bangladeshi rural children and its trend since mid-seventies. IMC J Med Sci. 2019;13:004. [Google Scholar]
- 16.Nath TC, Adnan MR, Sultana N, Husna A, Ndossi BA, Kang Y, et al. Integration of health education intervention to improve the compliance to mass drug administration for soil-transmitted helminths infection in Bangladesh: An implementation research. Parasite Epidemiol Control. 2020;11:e00165. doi: 10.1016/j.parepi.2020.e00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donkoh ET, Berkoh D, Fosu-Gyasi S, Ofori Boadu WI, Raji AS, Asamoah S, et al. Evidence of reduced academic performance among schoolchildren with helminth infection. Int Health. 2023;15:309–17. doi: 10.1093/inthealth/ihac044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rasoul R, Khalesi N, Safavi M, Mirzaei A, Alimohammadzadeh K. Identifying the outcomes of healthy lifestyles in the post-COVID era. Archives of Advances in Biosciences. 2023;14:1–14. [Google Scholar]
- 19.Karki P, Prabandari YS, Probandari A, Banjara MR. Feasibility of school-based health education intervention to improve the compliance to mass drug administration for lymphatic Filariasis in Lalitpur district, Nepal: A mixed methods among students, teachers and health program manager. PLoS One. 2018;13:e0203547. doi: 10.1371/journal.pone.0203547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Balaj M, York HW, Sripada K, Besnier E, Vonen HD, Aravkin A, et al. Parental education and inequalities in child mortality: A global systematic review and meta-analysis. Lancet. 2021;398:608–20. doi: 10.1016/S0140-6736(21)00534-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aivey SA, Rahman MM, Fukushima Y, Ahmed A, Prihanto JB, Sarker MHR, et al. Nutritional status and prevalence of helminthic infection among primary schoolchildren in Bangladesh: A cross-sectional study. Japan J Nurs Sci. 2024;21:e12568. doi: 10.1111/jjns.12568. [DOI] [PubMed] [Google Scholar]
- 22.Tengku Jamaluddin TZM, Mohamed NA, Mohd Rani MD, Ismail Z, Ramli S, Faroque H, et al. Assessment on hand hygiene knowledge and practices among pre-schoolchildren in Klang Valley. Glob Pediatr Health. 2020;7:2333794X2097636. doi: 10.1177/2333794X20976369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ponnambalam S, Palanisamy S, Singaravelu R, Janardhanan HA. Effectiveness of a school-based nutrition education program on waist circumference and dietary behavior among overweight adolescents in Puducherry, India. J Educ Health Promot. 2022;11:323. doi: 10.4103/jehp.jehp_413_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rahimi BA, Rafiqi N, Tareen Z, Kakar KA, Wafa MH, Stanikzai MH, et al. Prevalence of soil-transmitted helminths and associated risk factors among primary schoolchildren in Kandahar, Afghanistan: A cross-sectional analytical study. PLoS Negl Trop Dis. 2023;17:e0011614. doi: 10.1371/journal.pntd.0011614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tolera A, Dufera M. The prevalence of soil-transmitted helminths and associated risk factors among schoolchildren at Sekela Primary School, Western Ethiopia. J Parasitol Res. 2020;2020:8885734. doi: 10.1155/2020/8885734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhakal S, Karim MJ, Al Kawsar A, Irish J, Rahman M, Tupps C, et al. Post-intervention epidemiology of STH in Bangladesh: Data to sustain the gains. PLoS Negl Trop Dis. 2020;14:e0008597. doi: 10.1371/journal.pntd.0008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hernandez-Castro C, Agudelo-Lopez S del P, Medina-Lozano AP, Lopez-Garcia D, Garcia-Tuberquia LA, Botero-Garces JH, et al. The burden of intestinal parasitic infections in Antioquia, Colombia: Impact in childhood growth development and nutritional status. Acta Trop. 2024;251:107119. doi: 10.1016/j.actatropica.2024.107119. [DOI] [PubMed] [Google Scholar]
- 28.Aemiro A, Menkir S, Tegen D, Tola G. Prevalence of soil-transmitted helminthes and associated risk factors among people of Ethiopia: A systematic review and meta-analysis. Infect Dis Res Treat. 2022;15:117863372110554. doi: 10.1177/11786337211055437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong LW, Ong KS, Goh CBS, Dwiyanto J, Reidpath DD, Lee SWH, et al. Extremely low prevalence in soil-transmitted helminth infections among a multi-ethnic community in Segamat, Malaysia. J Parasit Dis. 2021;45:313–8. doi: 10.1007/s12639-020-01334-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Benjamin-Chung J, Crider YS, Mertens A, Ercumen A, Pickering AJ, Lin A, et al. Household finished flooring and soil-transmitted helminth and Giardia infections among children in rural Bangladesh and Kenya: A prospective cohort study. Lancet Glob Health. 2021;9:e308. doi: 10.1016/S2214-109X(20)30523-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ster IC, Niaz HF, Chico ME, Oviedo Y, Vaca M, Cooper PJ. The epidemiology of soil-transmitted helminth infections in children up to 8 years of age: Findings from an Ecuadorian birth cohort. PLoS Negl Trop Dis. 2021;15:1–20. doi: 10.1371/journal.pntd.0009972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seid M, Yohanes T, Goshu Y, Jemal K, Siraj M. The effect of compliance to Hand hygiene during COVID-19 on intestinal parasitic infection and intensity of soil transmitted helminthes, among patients attending general hospital, southern Ethiopia: Observational study. PLoS One. 2022;17:e0270378. doi: 10.1371/journal.pone.0270378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goel S, Chandrashekar BR. Evaluating the efficacy of handwashing demonstration on hand hygiene among school students – An interventional study. J Educ Health Promot. 2020;9:226. doi: 10.4103/jehp.jehp_94_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rizvi DS. Health education and global health: Practices, applications, and future research. J Educ Health Promot. 2022;11:262. doi: 10.4103/jehp.jehp_218_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pawils S, Heumann S, Schneider SA, Metzner F, Mays D. The current state of international research on the effectiveness of school nurses in promoting the health of children and adolescents: An overview of reviews. PLoS One. 2023;18:e0275724. doi: 10.1371/journal.pone.0275724. doi: 10.1371/journal.pone.0275724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goldberg L, Rankine J, Devlin B, Miller E, Ray KN. School nurse perspectives on collaboration with primary care providers. J Sch Health. 2023;93:717–25. doi: 10.1111/josh.13325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Raesi R, Shaye ZA, Saghari S, Sheikh Beig Goharrizi MA, Raei M, Hushmandi K. The impact of education through nurse-led telephone follow-up (telenursing) on the quality of life of COVID-19 patients. J Egypt Public Health Assoc. 2021;96:30. doi: 10.1186/s42506-021-00093-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


