Abstract
Long segment ureteral reconstruction has always posed a challenge for surgeons. We report the case of a 49 years male patient with a right ureteral obstruction between the ileal orthotopic bladder and the ureter. The patient underwent a 12cm ureteral reconstruction with the prepuce. One month after the surgery, anterograde angiography through the nephrostomy tube showed ureteral patency. After one year of postoperative follow-up, the patient's ureteral stricture did not recur. Using the prepuce as a free graft for ureteral reconstruction is one of the available options.
Keywords: Ureteral reconstruction, Prepuce, Ureteral stricture
1. Introduction
Surgical repair of long-segment proximal ureteral strictures (LPUS) is challenging. Ureteroureterostomy alone is generally contraindicated in this setting given the difficulty in obtaining a tension-free anastomosis.1. Usually, we have to select other materials to reconstruct the ureter, such as Boari flap, appendix, intestine, oral mucosa, etc., to achieve tension-free anastomosis.2,3. However, for some complex cases, where Boari flap, appendix, intestine, or oral mucosa are inaccessible, what other methods can replace and reconstruct the ureter? Therefore, it is highly necessary to develop safe, effective and new surgical techniques for ureteral reconstruction. Circumcision has been carried out for thousands of years, and it can be considered the most commonly performed surgical procedure in the world.4. Usually, the removed prepuce is treated as medical waste. In this case we reported, because the patient needed materials for ureteral reconstruction, we performed circumcision on the patient and obtained the prepuce as a free graft to reconstruct the ureter.
2. Case presentation
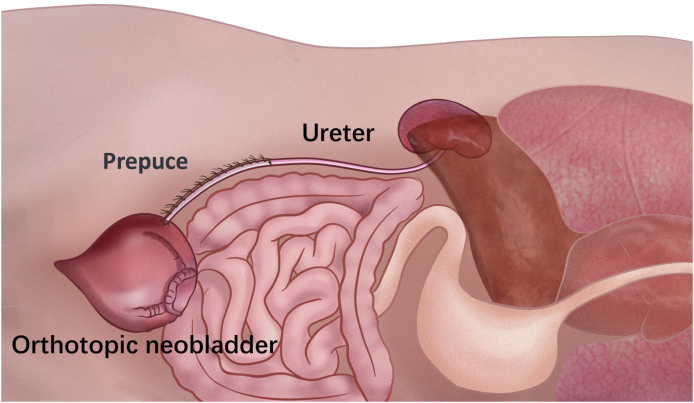
The patient, male, 49 years old, underwent radical cystectomy and ileal orthotopic bladder for bladder cancer one year ago. Three months after the surgery, the patient developed right-sided hydronephrosis and was given nephrostomy. Through antegrade and retrograde angiography, we found that there was a distance of about 8cm between the dilated ureteral end and the new bladder (Fig. 1). Because the patient had an ileal orthotopic bladder, it was not possible to reconstruct the ureter with a Boari flap. The patient had extensive adhesions in the intestine after radical cystectomy, and it was almost impossible to reconstruct the ureter with the intestine. The patient also did not agree to reconstruct the ureter with oral mucosa. Finally, we asked the patient whether he had undergone circumcision and whether the patient had a redundant prepuce. The patient answered that he had not undergone circumcision and had a redundant prepuce. So we designed this surgical procedure for him(Fig. 2). It seemed that reconstructing the ureter with the prepuce was the only choice.
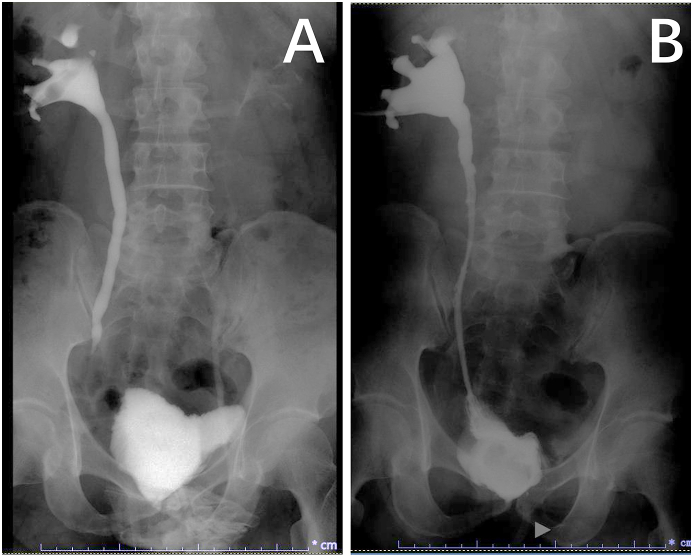
Fig. 1.
A Preoperative angiography revealed a defect of approximately 8cm between the distal ureter and the ileal orthotopic bladder. B Postoperative angiography showed no leakage of contrast material throughout the ureter and ureteral patency.
Fig. 2.
Surgical scheme design. Free prepuce was taken and rolled into a tube, one end was anastomosed with the ureter, and the other end was anastomosed with the ileal orthotopic bladder. The reconstructed ureter was wrapped with mesentery.
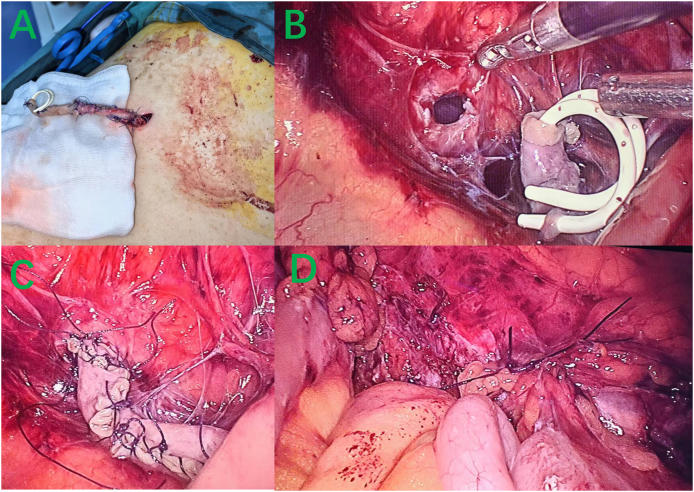
Intraoperatively, the patient was found to have severe intra-abdominal adhesions. We completely disengaged the ureter and found that there was a distance of about 12cm between the ileal orthotopic bladder and the ureter to achieve tension-free anastomosis, rather than the 8cm evaluated by preoperative imaging. We took the end of the ureter out of the body, and then we performed a circumcision. We reconstructed about 12cm ureteral segment with a prepuce coil(Fig. 3A). The ureter is then returned to the body, achieving a tension-free anastomosis with the ileal orthotopic bladder (Fig. 3BC). The ureteral part of the reconstruction with the prepuce was wrapped with omentum (Fig. 3D). The surgery time was about 3 hours, and blood loss was about 100ml. The abdominal drainage tube was removed 5 days after the surgery, and the renal fistula was kept. One month after the surgery, the patient returned to the hospital for antegrade angiography through the renal fistula, which showed that the ureteral reconstruction with free prepuce was unobstructed (Fig. 1), and the renal fistula was removed. After one year of postoperative follow-up, the patient's ureteral stricture did not recur.
Fig. 3.
Long ureteral reconstruction with the free prepuce. A After the ureteral was disengaged, the ureteral end was extracted from the body, and approximately 12cm of the ureter was reconstructed with the free prepuce. B The sutured ureter was then introduced back into the body, and laparoscopic anastomosis between the ureter and the ileal orthotopic bladder was performed. C The ureter and the ileal orthotopic bladder anastomosis was completed. D The ureteral part reconstructed with the free prepuce was wrapped with omentum.
3. Discussion
Orthotopic neobladder (ONB) reconstruction is a continent urinary diversion procedure that may be performed in a patient with bladder cancer following a radical cystectomy.5. According to a cross-sectional study in China that included 2304 patients undergoing radical cystectomy, the orthotopic neobladder was the predominant choice for diversion (44 %), followed by the ileal conduit (31 %).6. The reported incidence of ureteroileal anastomosis stricture (UIAS) was about 10 % (range from 3 % to 18 %).7. Although the incidence of UIAS is not high, once satisfactory reconstruction repair cannot be performed, patients will face long-term survival with nephrostomy tube, which will greatly reduce the quality of life of patients. Therefore, repair and reconstruction of the stricture segment is very necessary.
During radical cystectomy, certain tension exists at the anastomosis between the terminal ureteral end and the orthotopic neobladder due to the invasion of bladder tumor to the terminal ureteral end or the incomplete dissociation of the terminal ureteral end caused by adhesion. Tension anastomosis is easy to cause UIAS. Although UIAS may show a shorter narrow segment in the angiogram. However, when the narrow segment is reconstructed, the length of the ureteral segment that needs to be reconstructed is often much longer than the length evaluated before surgery. In this case, the preoperative evaluation of the ureteral defect was 8cm, but it was found during the surgery that a 12cm ureteral segment needed to be reconstructed to achieve tension-free anastomosis between the ureteral end and the orthotopic neobladder. Therefore, the length of the ureteral defect should be fully evaluated before surgery. In such cases, the reconstruction of the ureteral segment is often very difficult. Because this kind of secondary surgery is often accompanied by extensive adhesion of the intestine, it is extremely difficult to take the intestine again for ureteral reconstruction surgery. Because the patient has an intestinal bladder, it is also impossible to take the Boari flap for ureteral reconstruction. There have been some recent reports on the long-segment ureteral reconstruction with oral mucosa, with good results,8,9, but this requires the consent of the patient. The patient in this case did not agree to take oral mucosa for ureteral reconstruction, which limited the choice of ureteral reconstruction materials. Therefore, long-segment ureteral reconstruction with prepuce became the optimal choice in this patient.
The skin tissue is currently referred to as a reservoir of cells with therapeutically relevant functions. Historically considered biological waste, prepuce is increasingly used to provide immunotherapeutic MSCs for medicinal products.10. In circumcision, the prepuce is generally discarded as medical waste. In fact, in urethral reconstruction, the prepuce is an excellent material for urethral reconstruction and widely used.11. We chose the prepuce as the material for ureteral reconstruction of patients, based on the long-term experience of using the prepuce to reconstruct the urethra in the past. Using the prepuce as a free graft to reconstruct the ureter could make this type of surgery more definitive. Taking oral mucosa can cause oral complications, and may be difficult for some patients to accept. When taking the intestine or appendix, it is often difficult to know before surgery whether the intestine or appendix has adhesions and inflammation in the abdomen. The prepuce allows for a full evaluation of condition and length before surgery. After the reconstruction of the ureteral with the free prepuce, we used the omentum to wrap the prepuce, because the free prepuce had no blood supply. The angiography results one month after the surgery also showed that the prepuce survived well without the leakage of contrast agent. The excellent characteristics of the prepuce in urethral reconstruction give us reason to believe that the prepuce may play a greater role in ureteral reconstruction.
4. Conclusion
Complex ureteral stenosis remains clinically challenging, often requiring long-term nephrostomy. When ureteral reconstruction is carried out with intestinal and oral mucosa, it often brings new pains such as intestinal obstruction, oral pain, articulation difficulty and so on to patients while treating the disease. Repair and reconstruction of ureteral stricture with prepuce offers a potential new treatment option for these patients.
CRediT authorship contribution statement
Xiaoyong Zeng: Writing – review & editing, Data curation, Conceptualization. Zhenliang Qin: Methodology, Formal analysis, Data curation. Xing Li: Project administration, Data curation. Jun Zhou: Visualization, Data curation. Shuai Lu: Data curation. Weiwu Liu: Data curation. Ying Zhan: Investigation. Ruibao Chen: Writing – original draft, Data curation, Conceptualization.
Declaration of competing interest
No conflict of interest to be noted.
References
- 1.Lee M., Lee Z., Koster H., et al. Collaborative of Reconstructive Robotic Ureteral Surgery (CORRUS). Intermediate-term outcomes after robotic ureteral reconstruction for long-segment (≥4 centimeters) strictures in the proximal ureter: a multi-institutional experience. Investig Clin Urol. 2021 Jan;62(1):65–71. doi: 10.4111/icu.20200298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang C., Wang J., Hai B., et al. Lingual mucosal graft ureteroplasty for long proximal ureteral stricture: 6 Years of experience with 41 cases. Eur Urol. 2022 Aug;82(2):193–200. doi: 10.1016/j.eururo.2022.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Wang X., Chen S., Li X., et al. Robotic-assisted laparoscopic Bilateral ileal ureter replacement with extracorporeal ileal segment preparation for bilateral extensive ureteral strictures: the initial experience. Urology. 2023 Jun;176:213–218. doi: 10.1016/j.urology.2023.03.026. [DOI] [PubMed] [Google Scholar]
- 4.Timmermans F.W., Mokken S.E., Poor Toulabi S.C.Z., Bouman M.B., Özer M. A review on the history of and treatment options for foreskin reconstruction after circumcision. Int J Impot Res. 2022 Aug;34(5):424–433. doi: 10.1038/s41443-021-00438-3. [DOI] [PubMed] [Google Scholar]
- 5.Qu L.G., Lawrentschuk N. Orthotopic neobladder reconstruction: patient selection and perspectives. Res Rep Urol. 2019 Dec 11;11:333–341. doi: 10.2147/RRU.S181473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang Y., Bai Y., Wang X., Tang Y., Han P., Wei X. Internal double-J stent was associated with a lower incidence of ureteroileal anastomosis stricture than external ureteral catheter for patients undergoing radical cystectomy and orthotopic neobladder: a systematic review and meta-analysis. Int J Surg. 2019 Dec;72:80–84. doi: 10.1016/j.ijsu.2019.10.023. [DOI] [PubMed] [Google Scholar]
- 7.Peng Y.L., Ning K., Wu Z.S., et al. Ureteral stents cannot decrease the incidence of ureteroileal anastomotic stricture and leakage: a systematic review and meta-analysis. Int J Surg. 2021 Sep;93 doi: 10.1016/j.ijsu.2021.106058. [DOI] [PubMed] [Google Scholar]
- 8.Drain A., Jun M.S., Zhao L.C. Robotic ureteral reconstruction. Urol Clin North Am. 2021 Feb;48(1):91–101. doi: 10.1016/j.ucl.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Zhao L.C., Yamaguchi Y., Bryk D.J., Adelstein S.A., Stifelman M.D. Robot-Assisted ureteral reconstruction using buccal mucosa. Urology. 2015 Sep;86(3):634–638. doi: 10.1016/j.urology.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Najar M., Lagneaux L. Foreskin as a source of immunotherapeutic mesenchymal stromal cells. Immunotherapy. 2017 Jan;9(2):207–217. doi: 10.2217/imt-2016-0093. [DOI] [PubMed] [Google Scholar]
- 11.Rampersad R., Nyo Y.L., Hutson J., O'Brien M., Heloury Y. Foreskin reconstruction vs circumcision in distal hypospadias. Pediatr Surg Int. 2017 Oct;33(10):1131–1137. doi: 10.1007/s00383-017-4151-y. [DOI] [PubMed] [Google Scholar]