Abstract
The introduction of cell‐free DNA screening has resulted in increased prenatal identification of sex chromosome aneuploidies (SCAs). This study aimed to evaluate genetic counselor experiences disclosing SCAs positive prenatal screening or testing results and genetic counselor‐reported parental questions regarding sex, gender, and sexual orientation. Forty‐eight prenatal genetic counselors completed the survey. When asked to quantify their experiences, 97.9% of counselors reported disclosing a SCAs positive screen result within the previous year, and 81.3% disclosed a diagnostic result. Of those counselors, 53.8% reported always or often receiving parental questions about sex, 33% always or often about gender, and 25% always or often regarding sexual orientation. Counselors were asked to share examples of parental questions following a positive screen or diagnostic testing for SCAs. Parental questions were stratified by karyotype and content analysis revealed questions about the fetus' sex, anatomy, reproduction, being cisgender, gender expression, behavior, being transgender, and sexual orientation. The examples of parental questions provided by genetic counselors suggested some parents may have misconceptions about the intersection of SCAs with sex, gender, and sexual orientation following prenatal screening or diagnostic testing. The majority of counselors (83.3%) agreed to some extent that they desired further education on responding to parental questions about SCAs. Findings from this research suggest a need for genetic counseling strategies that accurately and respectfully discuss SCAs in the context of sex, gender, and sexual orientation with prenatal patients.
Keywords: genetic counseling, genetic counselors, parents, prenatal diagnosis, prenatal genetic counseling, sex chromosome aneuploidies
What is known about this topic
The rate of prenatal identification of sex chromosome aneuploidies (SCAs) has increased with the introduction of noninvasive prenatal screening. SCAs present with variable phenotypes and there is minimal evidence that SCAs is associated with variations in sexuality or gender identity, despite common misconceptions regarding a connection.
What this paper adds to the topic
As rates of prenatal identification of SCAs increases, genetic counselors are fielding questions from parents related to assignment of fetal sex, fetal anatomy and the possibility of future variations in fertility, gender expression, behavior, and sexual orientation. Prenatal genetic counselors desire additional education on discussing SCAs with patients.
1. INTRODUCTION
Sex chromosome aneuploidies (SCAs) as well as other fetal chromosome anomalies are increasingly detected in the prenatal period with the advent of cell‐free DNA (cfDNA) screening. Noninvasive prenatal screening (NIPS) analyzes isolated, fragmented pieces of placental and maternal DNA found in maternal blood during pregnancy to determine risk for chromosomal aneuploidies. NIPS expanded to include screening for SCA in 2012 (Howard‐Bath et al., 2018; Petersen et al., 2017). SCA screening is available through many commercially available prenatal cfDNA screening tests and include analyses for 45,X (Turner syndrome), 47,XXY (Klinefelter syndrome), 47,XYY (Jacob syndrome), and 47,XXX (trisomy X or triple X syndrome). Prior to NIPS including screening options for SCA, approximately 10%–12% of fetuses with an SCAs were diagnosed prenatally and were typically diagnosed incidentally via invasive testing (Jaramillo et al., 2019; Lalatta & Tint, 2013; Pieters et al., 2011). The proportion of SCA among all prenatal diagnoses has increased since the introduction of NIPS (Howard‐Bath et al., 2018). Following widespread adoption of NIPS, nearly 20% of “increased risk” NIPS results in a large cohort were positive for SCA (Guy et al., 2019). Overall, it is estimated that incidence of SCA‐positive fetuses represent between 0.36% and 1.1% of all NIPS results (Bevilacqua et al., 2018; Bianchi et al., 2015; Deng et al., 2019; Guy et al., 2019).
When provided a choice, families have often elected to opt‐in to screening that includes X and Y chromosome analysis (Bevilacqua et al., 2018), indicating a desire by parents for prenatal sex chromosome analysis. The pursuit of diagnostic testing for SCA as the primary indication has also increased (Deng et al., 2019; Kornman et al., 2018). However, limited time is dedicated to pretest genetic counseling, sometimes as little as 2–4 min, contributing to reduced retention of knowledge about features of SCAs (Lalatta & Tint, 2013). Furthermore, parents receiving a prenatal diagnosis of SCA may not recall being informed that NIPS could identify SCAs (Riggan et al., 2021). These findings suggest a gap in counseling as well as patient knowledge about SCA in the prenatal setting.
This gap in counseling and knowledge may be impacted by limited awareness and misconceptions related to SCA in part due to limited research on the lived experiences of individuals with SCA. The terminology of “sex chromosome abnormality/aneuploidy” itself may cause confusion for the public and medical community due to the language conflating conceptions of gender and sexual orientation (Dennis et al., 2015; Linden et al., 2002; Tartaglia et al., 2010). Outdated terminology still used by medical professionals such as “hermaphrodite” along with inconsistent use of appropriate language to describe differences of sexual development may also contribute to a lack of accurate understanding of SCA diagnoses (Miller et al., 2018). Furthermore, medical research has perpetuated stigmatization of those with sex chromosome aneuploidies. Previous examinations of men with 47,XYY utilized biased sampling of the prison population, creating historical foundation of stigmatization related to sexual deviance, criminality, and institutionalization (Schiavi et al., 1988; Wiener et al., 1968; Witkin et al., 1976). Articles describing “lesbianism” in the Turner syndrome population were published in the 1980s, possibly artificially linking such findings early on and creating an early bias (Fishbain & Vilasuso, 1980). However, no evidence to date has suggested a significant association with SCA and an individual's sexuality or gender identity (Auer et al., 2013; Herlihy et al., 2011). Feminine gender identity and heterosexuality in Turner's syndrome have been noted to be consistent with the general population (McCauley et al., 1986; Pavlidis et al., 1995; Ross et al., 2000). Sexual orientation of individuals with Klinefelter syndrome (47,XXY) are comparable to the general population as well (Hayes et al., 2012; Herlihy et al., 2011; McConaghy et al., 2006). Pituitary‐gonadal hormonal function and sexual behaviors in men with SCA have no significant correlation (Schiavi et al., 1988). In many of these studies, sexuality and gender identity were pathologized and framed as phenotypes rather than personal identities, further contributing to stigmatization.
Counseling approaches for SCAs in the prenatal setting are not well‐described, despite the increased detection of SCA by NIPS. Therefore, this study aimed to explore the prevalence and nature of parental questions regarding assigned sex, gender, and sexual orientation related to SCAs following screening and diagnostic testing. Through analysis of parental questions about SCAs, misconceptions and gaps in knowledge are identified, which could in turn be used by healthcare professionals to better inform accurate and respectful education regarding sex chromosome aneuploidies.
2. METHODS
Prenatal genetic counselors were surveyed to determine the rates of SCAs screen positive results and diagnoses, as well as questions commonly asked by parents. This study was approved by the Institutional Review Board at the University of North Carolina Greensboro (IRB# 20‐0067).
2.1. Participant recruitment
The survey invitation was distributed electronically via the National Society of Genetic Counselors (NSGC) Student Research Listserv in November 2019. Inclusion criteria required participants to be currently practicing prenatal genetic counselors in the U.S. or Canada.
2.2. Instrumentation
Following an extensive review of the literature, the research team, which included a genetic counseling graduate trainee and three genetic counselors (a prenatal genetic counselor, a research genetic counselor with experience in survey development, and a counselor who supports a clinic for differences of sex development) developed a survey to capture genetic counselors' experiences disclosing sex chromosome aneuploidy results (Appendix A). The survey included closed‐ended questions about participant characteristics including years since graduation, years of experience in the prenatal genetic counseling subspecialty, and geographic location of work. Additional quantitative questions explored the prevalence of SCA screen positive disclosures, diagnostic positive disclosures, the prevalence of specific genotypes seen, and the proportion of the time parents had questions of sex, gender, or sexual orientation. Questions using a Likert scale assessed previous genetic counselor education on SCAs and counseling on sex, gender, or sexual orientation with parents. Participants were also asked to report interest in further education on the topics. Open‐ended questions elicited examples of parental questions asked, stratified by SCA condition (45,X; 47,XXY; 47,XYY; 47,XXX; 48,XXYY; other SCA) with space for up to five examples for each SCA. Definitions for sex, gender identity, and sexual orientation were provided throughout the survey as defined by the American Psychological Association (2015) (Appendix A).
Data were collected via the online survey platform Qualtrics for a period of 6 weeks.
2.3. Statistical analyses
Descriptive statistics were calculated for quantitative responses in the survey. Qualitative data were analyzed through a two‐step process. First, we used a process of inductive content analysis for responses stratified by chromosome karyotype. This step utilized a categorization approach similar to previous genetic counseling research on genetic counseling for LGBTQ+ patients (Glessner et al., 2012; VandenLangenberg et al., 2012). Responses of similar content for each SCA were grouped together, and categories and subcategories were identified. Frequency of responses involving each category identified were calculated and explanatory quotations were selected. Second, a process of inductive thematic coding identified themes present among all SCAs. For both steps of qualitative coding, the first author (SB) coded all of the examples of parental questions provided by the respondents as described. The second author (JL) also reviewed the data separately; any discrepancies between the two coders were discussed until a consensus was reached. The last author (RM) served as an additional reviewer and auditor to resolve discrepancies.
Of note, genetic counselor‐reported parental questions that included terms regarding chromosomes, “male,” or “female” were categorized as “sex” per the definitions provided to participants. Parental questions that used terminology such as “man,” “woman,” “girl,” and “boy” were categorized as “gender.” For some responses, it was difficult to determine if the use of terminology represented the true nature of the question posed, or if terminology was inaccurately used. For example, if the respondent reported a parental question using the word “male” which is typically related to questions about sex, but the question content was appeared to be about gender, it was unclear if it should be coded as a question about sex or gender. One such statement that was excluded from analysis due to this discrepancy was: “When disclosing a diagnosis of Turner syndrome (45,X), patients and/or their partners have asked me if their child won't be a woman or have typically physical female features;” in this case the word “female” may imply a question about sex, but the words “woman” and “features” may imply gender or gender expression. Utilizing this exclusion criteria, three responses were excluded from categorization.
3. RESULTS
Fifty‐six genetic counselors responded to the survey. Eight surveys were excluded from analysis because they were incomplete, resulting in a dataset of 48. The 2019 National Society of Genetic Counselors' Professional Status Survey (PSS) indicated the number of prenatal counselors involved in direct patient who responded to the PSS was 503 (National Society of Genetic Counselors, 2019). As the PSS captures only a subset of practicing genetic counselors in North America, a conservative response rate of 9.54% is estimated.
3.1. Genetic counselor demographic information
Twenty‐four U.S. states and Canadian provinces were represented by the respondents. The mean years of prenatal practice was 5.6 years (SD = 6.6 years), and median year of genetic counseling program graduation was 2016.
3.2. Genetic counselors experiences with SCA in clinic
When asked if they had ever disclosed a NIPS screen positive for a SCA in their career, 97.9% of respondents (n = 47) had done so with 46 reporting disclosing a SCA positive NIPS screen within the last year. Forty‐one respondents (85.4%) reported disclosing a SCA diagnosis in their career, and 39 (81.3%) reported disclosing a SCA diagnosis in the past year.
The respondents were asked to recall and estimate the number of screen positives and diagnoses they saw in the last year. The mean number of SCA NIPS screen positives and diagnoses counselors reported in the past year were 4.84 (SD = 3.56, range 1–15) and 4.54 (SD = 9.36, range 1–60), respectively. Excluding the maximum outlier, the average number of diagnoses in the past year was 3.07 (SD = 2.16, range 1–10). These estimates were further stratified by specific SCA (Table 1). The majority of genetic counselors reported returning screen positive and diagnosis results of 45,X (77.1% and 64.4% respectively) and 47,XXY (70.8% and 43.8% respectively).
TABLE 1.
Number of counselors who recalled disclosing a sex chromosome aneuploidy (SCA) result and their estimated number of cases seen in past year, stratified by indication.
| Indication | n (%) | Estimated number of cases |
|---|---|---|
| 45,X | ||
| NIPT | 37 (77.1%) | 116 ( = 3.14, SD = 2.20, 1–10) |
| Diagnosis | 31 (64.6%) | 72 ( = 2.23, SD = 1.53, 1–7) |
| 47,XXY | ||
| NIPT | 34 (70.8%) | 54 ( = 1.34 SD = 0.96, 1–5) |
| Diagnosis | 21 (43.8%) | 26 ( = 2.32, SD = 1.54, 1–3) |
| 47,XXX | ||
| NIPT | 18 (37.5%) | 25 ( = 1.39, SD = 0.78, 1–4) |
| Diagnosis | 12 (25.0%) | 14 ( = 1.17, SD = 0.39, 1–2) |
| 47,XYY | ||
| NIPT | 15 (31.3%) | 18 ( = 1.2, SD = 0.77, 1–4) |
| Diagnosis | 9 (18.8%) | 8 ( = 1.0, SD = 0) |
| 48,XXYY a | ||
| Diagnosis | 0 | 0 |
| Other SCA a | ||
| Diagnosis | 2 (4.2%) | 3 ( = 1.5, SD = 0.71, 1–2) |
These conditions are not detected via NIPT.
Counselors were asked to compare the number of SCA screen positives and diagnoses across 5 years. Of the counselors who were in practice 5 years prior to completion of the survey (n = 19): 52.6% (n = 10) said the number of screen positives had increased, 31.6% (n = 6) remained the same, and 15.8% (n = 3) reported a decrease. A similar distribution was noted when considering trends in SCA diagnoses: 31.6% (n = 6) stated the number of diagnoses increased, 47.4% (n = 9) remained the same, and 21.1% (n = 4) reported a decrease.
3.3. Parental questions
Participants were asked to consider how often they received questions from patients regarding sex, gender, and sexual orientation in SCA cases using a Likert scale (always, often, sometimes, never). Twenty‐five (52.8%) respondents reported that they always or often received questions about sex following a SCA disclosure (NIPS positive or diagnosis positive). Thirty‐three percent (n = 16) always or often received questions about gender, and 25% (n = 12) always or often received questions about sexual orientation. Eight (16.7%) reported they never received questions across all categories (Figure 1).
FIGURE 1.
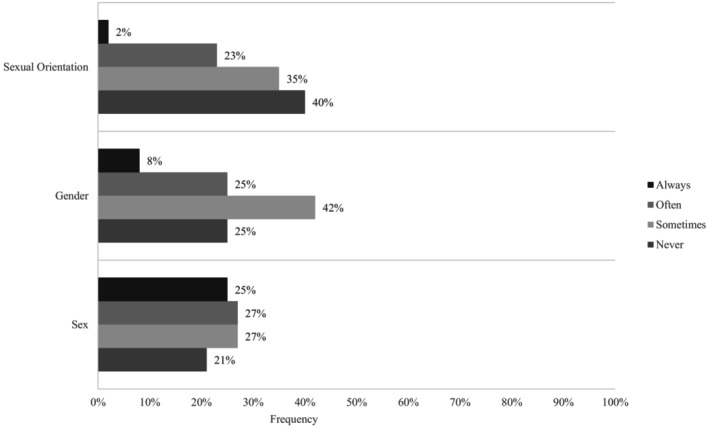
How often respondants received questions about sex, gender, and sexual orientation across all SCA disclosures.
Respondents were then asked to share questions they received from parents, stratified by karyotype. Twenty‐six (76.5%) genetic counselors who disclosed a 47,XXY result reported having received questions about sex, gender, or sexual orientation. Counselors reported receiving questions about sex, gender, or sexual orientation for other SCA genotypes as well: 39.5% (n = 15) for 45,X, 22.2% for 47,XYY, 14.3% (n = 3) for 47,XXX, and 50% (n = 1) for other SCAs.
3.4. Content analysis of parental questions
Parental questions reported by genetic counselors about sex, gender and sexual orientation were stratified by SCA and categorized as questions about sex, gender, and sexual orientation. These major categorizations were further subcategorized into questions regarding anatomy and hormones, intersex, reproduction, cisgender, behavior, gender expression, and transgender. Examples of these parental questions are described below.
3.4.1. Parental questions about sex
Genetic counselors reported receiving questions from parents about whether their child was “male” or “female” for all SCAs except 47,XXX. Counselors indicated receiving questions regarding the fetus' anatomy or hormones for all SCAs, but particularly for 47,XXY. One counselor noted that “…male partners seem to be generally more concerned about anatomical differences in boys with 47,XXY…they've asked whether the boys will be ‘less male’ because of their potentially smaller genitalia, lower testosterone, etc.” Another said that “…the patient asked if her child will have a penis” (45,X).
Counselors also indicated receiving questions about the chance of the child being intersex for 45,X and 47,XXY. For example, one such statement was “When disclosing a positive screen for Turner syndrome, a patient has asked me if this means their child is intersex….” Questions about reproduction and future fertility were reported from parents receiving a fetal diagnosis of 47,XXX and 47,XYY.
3.4.2. Parental questions about gender
Counselors reported parents asking questions to confirm gender. For example: “Will she be a normal girl?” (47,XXX), and “A patient wanted to know if a fetus with Turner syndrome could be a boy.” Questions regarding behavior primarily involved inquiries surrounding aggression and the 47,XYY genotype. One genetic counselor reported that a parent asked if a child with Klinefelter syndrome (47,XXY) will be able to play sports. Questions of gender expression focused on concepts of the masculinity or femininity of the future child, particularly during disclosures of 47,XXY. Examples included: “So she is only half girl? Will she be a tomboy?” (45,X), and “Patients will want to know if their child will be more feminine” (47,XXY).
Questions reported about transgender identity were also prevalent within our data set, particularly when reporting 47,XXY. Questions related to this theme were reported by nine of the 26 genetic counselors who reported parental questions about 47,XXY; one genetic counselor reported parental questions related to 45,X and transgender identity. Some parental questions used more definitive language like, “Are they transgender?” (47,XXY), while others reported statements using language associated with an increased likelihood, chance, or risk such as “Is he more likely to be transgender?” (47,XXY).
3.4.3. Parental questions about sexual orientation
Genetic counselors received questions from parents about sexuality when discussing 45,X, 47,XXY and 47,XYY. One respondent stated, “Patients wonder if this means their child will be gay” (47,XXY) or “…more likely to be attracted to the same sex” (45,X). The distribution of question types varied based on SCA. Questions about sexual orientation and 47,XXY were reported by 15 of 26 genetic counselors who reported parental questions about 47,XXY, compared to four genetic counselors that reported questions about sexual orientation of the 15 who received parental questions related to 45,X. Due to the small sample size, we were unable to conduct analyses to determine if this difference was statistically significant.
3.5. Thematic analysis across SCAs
One theme identified across all SCAs was parents associating qualifying language to sex or gender expression. These statements involved wording such as “less,” “more,” “half,” “extra,” and “neither.” Some examples of parental questions using qualifying language include: “So she is only half girl?” (45,X), “So babies with Turner syndrome aren't really male or female?,” “…boys will be ‘less male’”(47,XXY), and “People have asked if their baby will be ‘extra’ or ‘super’ male” (47,XYY).
Another theme noted, though not as frequently, were statements suggesting parental use of negatively coded language. One such statement was “Parents [were] concerned that son may be at risk of being transgender or homosexual” (47,XXY; emphasis ours). Another parental question asked about their child being a “hermaphrodite.” One counselor indicated that parents will use “older, inappropriate terms” when asking about their child being intersex, though this counselor did not report the exact terminology.
3.6. Genetic counselor education
Twenty‐two participants (45.8%) strongly agreed or agreed that their graduate program prepared them to answer parental questions about sex, gender, and sexual orientation; 35.4% (n = 17) somewhat agreed, 6.3% (n = 3) neither agreed nor disagreed, and 12.5% (n = 6) somewhat or strongly disagreed. Those who agreed or strongly agreed indicated that the type of training they received included clinical information about SCAs and differences in sex development (n = 9), working with the LGBTQ+ community (n = 3) or identifying misconceptions about SCAs (n = 2) through a variety of means including didactic presentation such as lectures (n = 17), clinical experiences (n = 4), research and literature review (n = 2) and observation of support groups (n = 1). Respondents were also asked if they received any continued education regarding SCA and parental questions of sex, gender, sexual orientation; 20.8% of participants (n = 10) reported they had. Examples of this continuing education provided in response to an open‐ended question included workshops and lectures at conferences, webinars, and journal publications.
Respondents were asked about their interest in additional education on how to respond to questions of sex, gender, and orientation in a prenatal setting. Most respondents (60.4%, n = 29) agreed or strongly agreed that they were interested in additional education; 22.9% (n = 11) somewhat agreed, 8.3% (n = 4) neither agreed nor disagreed, and the remaining 8.33% (n = 4) somewhat or strongly disagreed. Those who expressed interest in additional education desired education formats including webinars and CEU courses (n = 12), written materials and literature (n = 7), didactic lectures (n = 6), meeting workshops (n = 3), and discussion with other genetic counselors (n = 2). Specific topics of interest included more in‐depth information on SCAs across the lifespan and how to best respond to questions and misconceptions (n = 9). Other topic areas included information on discussing sex, gender, and sexuality with patients and information on the most up to date terminology (n = 7), hearing firsthand from physicians, families, and adults with SCA (n = 6), and education on working with the LGBTQ+ community (n = 1).
4. DISCUSSION
The results of this study indicate that most of the prenatal counselors surveyed have disclosed SCA positive NIPS or diagnostic results and received questions about sex, gender, or sexual orientation when discussing SCA with families. Additional support and education in counseling strategies were desired to prepare counselors to have these conversations with clients.
The number of counselors who reported seeing NIPS screen positive for SCA is comparable to previous reports (97.9% vs. 94%; Fleddermann et al., 2019), suggesting that counseling about SCA is a routine part of prenatal practice. Many of our participants also reported a higher incidence of SCA diagnosis prenatally compared to 5 years prior.
Although previous research has examined the rates of SCA screen positive and diagnoses, this is the first to explore common parental questions following a positive screen or diagnostic test to our knowledge. The examples of parental questions provided by genetic counselors reveal an apparent lack of clarity on the intersection of sex, gender, and sexual orientation with SCA. This may also suggest a general lack of understanding among patients about the etiology of sex, gender, or sexual orientation. Although it is unclear whether parental questions are rooted in curiosity or criticism, the presence of the questions themselves reveal a sense of ambiguity. Recent data suggests that many parents feel that SCA diagnoses were often delivered in a way that emphasize the negative attributes of the SCAs further increasing the ambiguity these prospective parents may feel (Riggan et al., 2021).
This uncertainty and ambiguity of SCA can influence parental decision‐making. Studies analyzing pregnancy outcomes in prenatally diagnosed SCA cases found that patients pursued elective termination due to fears of infertility, and abnormal sexual development (Mezei et al., 2004; Sagi et al., 2001). Potential concerns about the fetus' future sexual orientation and gender were not explicitly reported in previous studies but were suggested by parental questions reported by our study participants. Genetic counselors can clarify uncertainty related to etiology of gender and sexual orientation, and provide insight to the lived experience of patients with SCAs to ensure that parents are making informed decisions (Llorin & Zayhowski, 2021; Llorin & Zayhowski, 2023).
The most common parental questions reported by genetic counselors in our study were related to the sex of the fetus, including whether the fetus will be male or female, and what the fetus' physical anatomy would look like. Previous research indicates that genetic counselors commonly discuss sex in binary terms of males (XY) and females (XX) with little time dedicated to discussing SCA in pretest counseling conversations (Lalatta & Tint, 2013). Therefore, the parental desire for additional clarification of fetal sex is likely congruent with their experience in counseling. When the education of sex is framed as binary, parents are left to draw their own conclusions regarding how their child fits this model. This presents an opportunity for genetic counselors to engage in counseling that minimizes use of binary language and to provide clarification to parental misconceptions about sex while promoting inclusion alongside education. Indeed, genetic counselors have been called to correct misconceptions about sex, as well as gender, when counseling about NIPS and SCA (Llorin & Zayhowski, 2023).
Questions of sexual orientation were also revealed in the analysis which may be due to a generalized confounding of sex chromosomes with sexual orientation. The root of this confusion may be lack of clarity in counseling or education, or it may be reflective of personal or societal beliefs or misconceptions. One 2007 study exploring public perceptions of the etiology of homosexuality found that eight of its 86 participants believed genetics was the sole cause of homosexuality, and 25 thought that genetics played some role (Sheldon et al., 2007). The parents reported in our survey may hold similar beliefs of sexual orientation being of genetic origin and may process that a difference in what we label explicitly as “sex” chromosomes may be the cause of their genetic conception of sexual orientation.
Other misconceptions related to sex, gender, and sexual orientation may further influence how differences in sex chromosomes are interpreted. A majority (94%) of surveyed prenatal genetic counselors also reported patients using ‘sex’ and ‘gender’ interchangeably when discussing NIPS (Stevens et al., 2023). In the aforementioned study by Sheldon et al. (2007), 26 of their 86 participants “made statements that revealed potential confusion about the difference between sex or gender and sexual orientation” (p. 18) including misunderstanding that homosexual individuals have genetic material of the “other sex.” Our data also suggests that parents may perceive that sex chromosomes influence sexual orientation, as many parental questions were related to the potential sexual orientation of their fetus across 45,X, 47,XXY, and 47,XXX disclosures. Incorrect conceptions of sexual orientation can have negative impacts on the visibility, representation, and healthcare of LGBTQ+ individuals. Implicit biases against the LGBTQ+ community have been observed among healthcare providers (Sabin et al., 2015), including genetic counselors. Genetic counselors report a lack of experience working with LGBTQ+ patients and have exhibited implicit biases that often surpasses their expressed explicit biases (Glessner et al., 2012; Nathan et al., 2019; Valentine et al., 2023; VandenLangenberg et al., 2012). Genetic counselors' implicit biases may contribute to or affirm parental misunderstanding of the etiology of sexuality or gender identity and their association with SCA.
Although the tone of parental questions about gender identity and sexuality could not be captured through the methodology used in this study, it is interesting to consider possible motives for such statements, particularly those that use negatively coded language. Parents who are asking these questions may be doing so as a need to clarify and better understand what an SCA could mean for a child. Conversely, asking these questions could be reflective of negative associations or biases against the LGBTQ+ community, especially as this topic has become further politically charged. For example, one genetic counselor reported a parent expressing concern following a 47,XXY diagnosis that their son “may be at risk of being transgender or homosexual” (emphasis ours). The use of “risk” in medicine and health tends to connote the chance of negative outcomes (Hayes, 1992), perhaps suggesting the parents perceived being transgender or homosexual as negative as well. It raises additional questions: Are parents asking about their child's gender identity and sexual orientation out of concern of falling outside societal norms? Or perhaps, concern about having a child who would be in conflict with their own personal values and views? Our study was not intended to address “why” parents are asking these questions about SCA, but further research could address the motivations behind these questions. If discriminatory attitudes were elicited, it is important to consider how counselors can best advocate for the LGBTQ+ community when working with patients who hold such views.
This study also aimed to assess differences in questions posed between karyotypes. Although statistical analysis criteria were not met due to the sample size, striking differences in question were observed between 45,X and 47,XXY, from which the largest samples of questions were provided. Questions of a child's sexual orientation were considerably more prevalent in discussions of 47,XXY rather than 45,X. This difference may be reflective of expectations and norms held by the broader society. Sheldon et al. (2007) noted that participant examples of homosexuality and gender expression differences often were of gay males, which may be due to conceptualizations of homosexuality or differences in gender expression with that of the “gay male” more so than a “lesbian female.” Furthermore, the conflation of gender expression with transgender identity may be related to the higher prevalence of parental questions of being transgender in 47,XXY cases compared to 45,X reported by our participants.
This difference in reports of parental questions about 45,X compared to 47,XXY could also be reflective of a societal value of cisgender and heterosexual identity being more valued in males than in females. Cultural studies have suggested that masculine behaviors are valued over feminine behaviors (Schilt & Westbrook, 2009), which creates a power hierarchy where masculinity is valued over femininity, and normative expectations are designed to reinforce gender inequality (Connell, 1987; Schilt & Westbrook, 2009; Schippers, 2007; West & Zimmerman, 1987). Likewise, societies that value masculinity also tend to value heterosexuality (Schilt & Westbrook, 2009). Thus, when males with SCAs are perceived to be “not masculine” or “not heterosexual,” it could be interpreted to result in a loss of power, status, and privilege to much greater extent than their female counterparts due to these societal expectations. These values may also be reflected in parental questions that prioritized “maleness” first, such as questions about 45,X that suggested “lack of a Y chromosome” rather than lack of an X.
4.1. Genetic counselor education
Fleddermann et al. (2019) evaluated prenatal genetic counselor general comfort on counseling for SCAs (not specifically regarding sex, gender, or sexual orientation), and 81%–94% percent of counselors felt extremely or somewhat comfortable counseling on SCAs, stratified by indication. Though this illustrates counselors are prepared and comfortable counseling about SCA, over 80% of our respondents reported a desire for continued education on SCAs, considerations of current terminology, and how to counsel on concepts of sex, gender, and sexual orientation. Genetic counselors' understanding of the concepts of sex, gender and sexual orientation may be strengthened by additional education related to SCAs as well seeking to better understand the lived experiences of LGBTQ+ individuals. This knowledge may also empower genetic counselors to combat parental bias or misunderstanding and support informed decision‐making when discussing SCAs.
Stevens et al. (2023) also reported that many genetic counselors desire additional education on utilization of inclusive language when discussing sex and gender. These data suggest a desire to gain a more nuanced understanding and refine advanced counseling skills. It may also be reflective of counselors doubting their knowledge in this area or grappling with some level of discomfort potentially due to implicit biases when discussing associated topics of sex, gender, and sexual orientation (Glessner et al., 2012; Nathan et al., 2019; Valentine et al., 2023; VandenLangenberg et al., 2012). Educational opportunities provided by the National Society of Genetic Counselors and others have provided tools for counseling on SCAs, some of which have been presented or published since conducting this research (Ernst et al., 2023; Huser et al., 2022; Llorin & Zayhowski, 2021).
When evaluating how well participants felt graduate school prepared them to counsel about SCA, there was great variability in both the content and means of education. Over 12% of participants reported they did not feel prepared to some extent. Programs are not explicitly required to cover topics related to SCA (Standards of Accreditation: ACGC, 2019), which may contribute to the variability in the content, means, and extent of SCA education. Likewise, there are no explicit content requirements regarding counseling on topics of sex, gender, and sexual orientation, or working with the LGBTQ+ community. Without clear guidelines to include such topics in genetic counseling training program curriculum, student experiences are likely to continue to reflect this wide variation of methods for providing education to promote preparedness. Development of professional guidelines related to SCA disclosure may also influence structured education and best practices for counseling for SCAs, with consideration of transgender and intersex perspective in particular (Llorin & Zayhowski, 2023).
4.2. Limitations
The small sample size and response rate limited the ability to perform the statistical analysis and extrapolate our findings. It is difficult to assess the number of counselors that received and opened the survey, as well as account for counselors who are not members of NSGC. The survey captured currently practicing prenatal counselors, so it did not capture those who may have experience in prenatal genetic counseling who are now in a different specialty. Additionally, the survey was not formally validated which could have resulted in differing interpretations of survey questions. The survey was largely based on participant recall, limiting the accuracy of numerical cases provided. Language reported in the qualitative analysis may be more reflective of counselor language regarding sex, gender, and sexual orientation, than wording exactly used by patients. Finally, counselor understanding of the concepts of sex, gender, and sexual orientation were not accounted for in the study. As such, responses may reflect individual biases or misconceptions held by the genetic counselor respondent rather than their patients.
4.3. Practice implications
Overall, the results of this study report the prevalence of NIPS positive and diagnoses of SCA in prenatal settings and the types of questions asked of genetic counselors when returning SCA screening or test results. Given the wide variety of question categories reported across all indications, counselors must be prepared to address topics including biological sex, anatomy, cisgender and transgender identity, as well as sexual orientation in a prenatal setting. Genetic counselors desire additional education about SCAs to improve counselor preparedness to respond to such questions. Expanding research initiatives and literature on these topics to inform instructional content is equally important. Current recommendations for healthcare providers outlined by the National LGBT Health Education Center (2016), which could inform genetic counselor education on providing inclusive care, suggests providers use nongendered terminology, avoid asking unnecessary questions, maintain nonjudgmental attitudes, understand the diversity and fluidity of expression, and to create a work environment of accountability (Providing Inclusive Services and Care for LGBT People: A Guide for Health Care Staff). The parental questions reported in our study can further guide such instruction, increasing awareness of these possible parental concerns for counselors and other healthcare providers. Considering these parental questions can guide pretest counseling strategies, phenotypic content, word choice, and time dedicated to SCA to address misconceptions upfront (Lalatta & Tint, 2013). The reported parental questions may also be considered by professional organizations developing guidance on how to navigate these discussions with parents, which is desired by genetic counselors (Stevens et al., 2023). This could expand accurate, respectful, and inclusive education on SCAs as well as concepts of sex, gender, and sexual orientation across a broader scope of prenatal patients.
5. CONCLUSION
This survey of prenatal genetic counselors reported experiences disclosing SCAs positive prenatal screening or testing results including parental questions about SCAs. Counselors reported receiving parental questions about sex, gender and sexual orientation when discussing SCAs in the prenatal setting. Parental questions reported by genetic counselors suggest that some parents may have misconceptions about SCAs as it relates to sex, gender, and sexual orientation. Genetic counselors desire additional education on counseling about these issues in order to clarify misunderstanding, minimize bias, and support informed decision‐making.
AUTHOR CONTRIBUTIONS
S.B. contributed to study conceptualization; data collection and curation; investigation; methodology; qualitative and quantitative analysis; project administration; and writing of original draft and writing as a reviewer and editor. J.L. contributed to study conceptualization; qualitative data analysis; methodology; and writing as a reviewer and editor. C.C contributed to conceptualization; methodology; and writing as a reviewer and editor. J.P.A. contributed to conceptualization; methodology; and writing as a reviewer and editor. L.E.D. contributed to conceptualization; methodology; supervision; and writing as a reviewer and editor. R.M. contributed to conceptualization; investigation; methodology; project administration; supervision; and writing as a reviewer and editor. Authors S.B. and R.M. confirm that they had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All of the authors gave final approval of this version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
ETHICS STATEMENT
Human Subjects and Informed Consent: This study was reviewed and granted an exemption by the University of North Carolina Greensboro. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Implied informed consent was obtained for individuals who voluntarily completed the online survey and submitted their responses.
Animal Studies: No nonhuman animal studies were carried out by the authors for this article.
ACKNOWLEDGMENTS
This research study was completed in partial fulfillment of a second‐year capstone project for the University of North Carolina at Greensboro Genetic Counseling Program for the first author, S.B.
APPENDIX A. Survey
Helpful definitions for use during the survey
Sexual orientation refers to the sex of those to whom one is sexually and romantically attracted.
Gender Identity refers person's deeply‐felt, inherent sense of being a boy, a man, or male; a girl, a woman, or female; or an alternative gender.
Sex refers to a person's biological status and is typically categorized as male, female, or intersex. There are a number of indicators of biological sex, including sex chromosomes, gonads, internal reproductive organs, and external genitalia.
Key Terms and Concepts in Understanding Gender Diversity and Sexual Orientation Among Students: American Psychological Association (2015).
Q1 Years of clinical practice as a prenatal genetic counselor (rounded to the nearest year) _______
Q2 Year of graduation from genetic counseling education _______
Q3 In what state or province do you currently practice? _______
Q4 Have you received any additional training on counseling sex chromosome aneuploidies (SCAs) since graduating?
Yes (1)
No (2)
If yes: You have indicated that you received additional training. Can you describe this training? If possible, include where and by what means/method this additional SCA training was received
________________________________________________________________
________________________________________________________________
Q5 Have you discussed a NIPT screen positive for a sex chromosome aneuploidy to a patient or client directly, including in person, telephone, and telemedicine counseling.
Yes (1)
No (2)
Q6 Have you disclosed a prenatal sex chromosome aneuploidy diagnosis in clinic to a patient or client directly, including in person, telephone, and telemedicine counseling.
Yes (1)
No (2)
Q7 Approximately how many sex chromosome aneuploidy NIPT screen positives have you disclosed? Include in person, telephone, and telemedicine disclosures during in the past year. _______
Q8 How does the number of SCA NIPT screen positives you saw this past year compare to the number you saw the year before?
Significantly increased (1)
Slightly increased (2)
Remained the same (3)
Slightly decreased (4)
Significantly increased (5)
N/A – I was not practicing 2 years ago (6)
Q9 How does the number of SCA NIPT screen positives you saw this past year compare to the number you saw the 5 years before?
Significantly increased (1)
Slightly increased (2)
Remained the same (3)
Slightly decreased (4)
Significantly decreased (5)
N/A – I was not practicing 5 years ago (6)
Q10 Approximately how many SCA diagnoses have you disclosed? Include in person, telephone, and telemedicine disclosures during the past year. _______
Q11 How does the number of SCA diagnoses you saw this past year compare to the number you saw the year before?
Significantly increased (1)
Slightly increased (2)
Remained the same (3)
Slightly decreased (4)
Significantly decreased (5)
N/A – I was not practicing 2 years ago (6)
Q12 How does the number of SCA diagnoses you saw this past year compare to the number you saw 5 years before?
Significantly increased (1)
Slightly increased (2)
Remained the same (3)
Slightly decreased (4)
Significantly decreased (5)
N/A – I was not practicing 5 years ago (6)
Q13 Please check all the conditions that you have disclosed a NIPT screen positive in clinic in the past year. Include in person, telephone, and telemedicine disclosures.
45,X (Turner syndrome) (1)
47,XXY (Klinefelter syndrome) (2)
47,XXX (trisomy X) (3)
47,XYY (4)
If 45,X (Turner syndrome) selected:
Write the approximate number of 45,X (Turner syndrome) NIPT screen positives you have disclosed in the last year. _______
If 47,XXY (Klinefelter syndrome) selected:
Write the approximate number of 47,XXY (Klinefelter syndrome) NIPT screen positives you have disclosed in the last year. _______
If 47,XXX (trisomy X) selected:
Write the approximate number of 47,XXX (trisomy X) NIPT screen positives you have disclosed in the last year. _______
If 47,XYY selected:
Write the approximate number of 47,XYY NIPT screen positives you have disclosed in the last year. _______
Q14 Please check all the conditions that you have disclosed a SCA diagnosis in clinic in the past year. Include in person, telephone, and telemedicine disclosures.
45,X (Turner syndrome) (1)
47,XXY (Klinefelter syndrome) (2)
47,XXX (trisomy X) (3)
47,XYY (4)
48,XXYY (5)
Other (6)
If 45,X (Turner syndrome) selected:
Write the approximate number of 45,X (Turner syndrome) diagnoses you have disclosed in the last year. (Include mosaic versions as well). _______
If 47,XXY (Klinefelter syndrome) selected:
Write the approximate number of 47,XXY (Klinefelter syndrome) diagnoses you have disclosed in the last year. (Include mosaic versions as well). _______
If 47,XXX (trisomy X) selected:
Write the approximate number of 47,XXX (trisomy X) diagnoses you have disclosed in the last year. (Include mosaic versions as well). _______
If 47,XYY selected:
Write the approximate number of 47,XYY diagnoses you have disclosed in the last year. (Include mosaic versions as well). _______
If 48,XXYY selected:
Write the approximate number of 48,XXYY diagnoses you have disclosed in the last year. (Include mosaic versions as well). _______
If Other selected:
Write the approximate number of other SCA diagnoses you have disclosed in the last year. (Include mosaic versions as well). _______
Q15 Considering all cases seen regarding SCA screen positives and diagnoses, how often have parents expressed questions regarding sex, gender, or sexual orientation? Please use the definitions provided to delineate between the terms.
| Never (1) | Sometimes (2) | Often (3) | Always (4) | |
|---|---|---|---|---|
| Sex (1) | ||||
| Gender (2) | ||||
| Sexual Orientation (3) |
Q16 For the next set of questions, you will be asked to write examples of questions you have heard in clinic regarding different sex chromosome aneuploidies. When doing so, please refrain from providing any identifiable patient information. Include both specific examples (noting if it was a diagnosis or screen positive) as well as questions you have heard numerous times. Example responses could look like: “Following a specific 48,XXYY diagnosis, the parents asked whether their child will be a boy or girl” or “Many times, parents have thought that having Klinefelter syndrome means that their child will be gay.”
If disclosed NIPT screen positive or diagnosis of 45,X (Turner syndrome) in the past year:
In your discussions regarding 45,X (Turner syndrome) results, have questions regarding an association between sex, gender, and sexuality been posed by patients?
Yes (1)
No (2)
Please list any questions or misconceptions you have received about sex, sexual orientation, or gender in screens and diagnoses of 45,X (Turner syndrome).
____________________________________________________________
____________________________________________________________
____________________________________________________________
If disclosed a NIPT screen positive or diagnosis of 47,XXY (Klinefelter syndrome) in the past year:
In your discussions regarding 47,XXY (Klinefelter syndrome) results, have questions regarding an association between sex, gender, and sexuality been posed by patients?
Yes (1)
No (2)
Please list any questions or misconceptions you have received about sex, sexual orientation, or gender in screens and diagnoses of 47,XXY (Klinefelter's syndrome).
____________________________________________________________
____________________________________________________________
____________________________________________________________
If disclosed a NIPT screen positive or diagnosis of 47,XXX (trisomy X) in the past year:
In your discussions regarding 47,XXX (Trisomy X or Triple X syndrome) results, have questions regarding an association between sex, gender, and sexuality been posed by patients?
Yes (1)
No (2)
Please list any questions or misconceptions you have received about sex, sexual orientation, or gender in screens and diagnoses of 47,XXX (Trisomy X or Triple X syndrome).
____________________________________________________________
____________________________________________________________
____________________________________________________________
If disclosed NIPT screen positive or diagnosis of 47,XYY in the past year:
In your discussions regarding 47,XYY results, have questions regarding an association between sex, gender, and sexuality been posed by patients?
Yes (1)
No (2)
Please list any questions or misconceptions you have received about sex, sexual orientation, or gender in screens and diagnoses of 47,XYY.
____________________________________________________________
____________________________________________________________
____________________________________________________________
If disclosed NIPT screen positive or diagnosis of 48,XXYY in the past year:
In your discussions regarding 48,XXYY results, have questions regarding an association between sex, gender, and sexuality been posed by patients?
Yes (1)
No (2)
Please list any questions or misconceptions you have received about sex, sexual orientation, or gender in screens and diagnoses of 47,XYY.
____________________________________________________________
____________________________________________________________
____________________________________________________________
If disclosed a NIPT screen positive or diagnosis of Other SCA in the past year:
In your discussions regarding other sex chromosome aneuploidies not previously listed, have questions regarding an association between sex, gender, and sexuality been posed by patients?
Yes (1)
No (2)
Please list any questions or misconceptions you have received about sex, sexual orientation, or gender in screens and diagnoses for any other SCA. Please also include the specific SCA you are referencing for each example.
____________________________________________________________
____________________________________________________________
____________________________________________________________
Q17 I feel my graduate education prepared me well to respond to questions of sex, gender, and sexual orientation regarding SCA in a prenatal setting.
Strongly agree (1)
Agree (2)
Somewhat Agree (3)
Neither agree nor disagree (4)
Somewhat disagree (5)
Disagree (6)
Strongly disagree (7)
If strongly agree or agree:
You indicated that you received graduate education that prepared you to answer questions regarding sex, gender and sexual orientation. Can you describe that education? Please include information about content as well as method of instruction.
____________________________________________________________
____________________________________________________________
____________________________________________________________
Q18 I would be interested in receiving further education on how to respond to questions of sex, gender, and sexual orientation regarding SCA in a prenatal setting.
Strongly agree (1)
Agree (2)
Somewhat agree (3)
Neither agree nor disagree (4)
Somewhat disagree (5)
Disagree (6)
Strongly disagree (7)
If Strongly agree or agree:
You indicated that you would be interested in receiving additional education about how to respond to questions of sex, gender, and sexual orientation. What type of additional training would be useful to you? Please include your thoughts on both content and method of instruction.
____________________________________________________________
____________________________________________________________
____________________________________________________________
If you have not discussed a NIPT screen positive or diagnosis for a sex chromosome aneuploidy to a patient or client:
Even though you have not discussed a prenatal SCA diagnosis or screen positive SCA, have parental questions regarding any sex chromosome aneuploidy and a fetus' sex, gender, or sexual orientation ever been brought up to you otherwise in clinic?
Yes (1)
No (2)
If yes: Please describe the parental questions or misconceptions here. Please note the question or statement as well as if it was in regards to a specific SCA.
____________________________________________________________
____________________________________________________________
____________________________________________________________
Thank you for your participation in this survey.
Burzynski, S. , Leonard, J. , Albrecht, J. P. , Doyle, L. E. , & Mills, R. (2025). Parental questions about sex chromosome aneuploidies regarding sex, gender, and sexual orientation as reported by genetic counselors in a prenatal setting. Journal of Genetic Counseling, 34, e1897. 10.1002/jgc4.1897
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- American Psychological Association . (2015). Key terms and concepts in understanding gender diversity and sexual orientation among students .
- Auer, M. K. , Fuss, J. , Stalla, G. K. , & Athanasoulia, A. P. (2013). Twenty years of endocrinologic treatment in transsexualism: Analyzing the role of chromosomal analysis and hormonal profiling in the diagnostic work‐up. Fertility and Sterility, 100(4), 1103–1110. 10.1016/j.fertnstert.2013.05.047 [DOI] [PubMed] [Google Scholar]
- Bevilacqua, E. , Ordóñez, E. , Hurtado, I. , Rueda, L. , Mazzone, E. , Cirigliano, V. , & Jani, J. C. (2018). Screening for sex chromosome aneuploidy by cell‐free DNA testing: Patient choice and performance. Fetal Diagnosis and Therapy, 44(2), 98–104. 10.1159/000479507 [DOI] [PubMed] [Google Scholar]
- Bianchi, D. W. , Parsa, S. , Bhatt, S. , Halks‐Miller, M. , Kurtzman, K. , Sehnert, A. J. , & Swanson, A. R. (2015). Fetal sex chromosome testing by maternal plasma DNA sequencing: Clinical laboratory experience and biology. Obstetrics and Gynecology, 125(2), 375–382. 10.1097/AOG.0000000000000637 [DOI] [PubMed] [Google Scholar]
- Connell, R. W. (1987). Gender and power: Society, the person and sexual politics. Stanford University Press. [Google Scholar]
- Deng, C. , Zhu, Q. , Liu, S. , Liu, J. , Bai, T. , Jing, X. , Xia, T. , Liu, Y. , Cheng, J. , Li, Z. , Wei, X. , Xing, L. , Luo, Y. , & Liu, H. (2019). Clinical application of noninvasive prenatal screening for sex chromosome aneuploidies in 50,301 pregnancies: Initial experience in a Chinese hospital. Scientific Reports, 9(1), 1–8. 10.1038/s41598-019-44018-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis, A. , Howell, S. , Cordeiro, L. , & Tartaglia, N. (2015). “How should I tell my child?” disclosing the diagnosis of sex chromosome aneuploidies. Journal of Genetic Counseling, 24(1), 88–103. 10.1007/s10897-014-9741-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst, G. , Huser, N. , Koeller, D. R. , Hulswit, B. , Bender‐Bernstein, H. , Muir, S. , Brogdon‐Soster, E. , & Yashar, B. M. (2023). Learning from our patients: Utilizing the expertise of transgender and/or gender diverse educators to build an inclusive learning cycle. Journal of Genetic Counseling, 32(6), 1154–1160. 10.1002/jgc4.1762 [DOI] [PubMed] [Google Scholar]
- Fishbain, D. A. , & Vilasuso, A. (1980). Exclusive adult lesbianism associated with Turner's syndrome mosaicism. Archives of Sexual Behavior, 9(4), 349–353. 10.1007/BF01541360 [DOI] [PubMed] [Google Scholar]
- Fleddermann, L. , Hashmi, S. S. , Stevens, B. , Murphy, L. , Rodriguez‐Buritica, D. , Friel, L. A. , & Singletary, C. (2019). Current genetic counseling practice in the United States following positive non‐invasive prenatal testing for sex chromosome abnormalities. Journal of Genetic Counseling, 28(4), 802–811. 10.1002/jgc4.1122 [DOI] [PubMed] [Google Scholar]
- Glessner, H. , VandenLangenberg, E. , Veach, P. , & LeRoy, B. (2012). Are genetic counselors and GLBT patients “on the same page”? An investigation of attitudes, practices, and genetic counseling experiences. Journal of Genetic Counseling, 21(2), 326–336. 10.1007/s10897-011-9403-8 [DOI] [PubMed] [Google Scholar]
- Guy, C. , Haji‐Sheikhi, F. , Rowland, C. M. , Anderson, B. , Owen, R. , Lacbawan, F. L. , & Alagia, D. P. (2019). Prenatal cell‐free DNA screening for fetal aneuploidy in pregnant women at average or high risk: Results from a large US clinical laboratory. Molecular Genetics & Genomic Medicine, 7(3), e545. 10.1002/mgg3.545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, J. , Chakraborty, A. T. , McManus, S. , Bebbington, P. , Brugha, T. , Nicholson, S. , & King, M. (2012). Prevalence of same‐sex behavior and orientation in England: Results from a National Survey. Archives of Sexual Behavior, 41(3), 631–639. 10.1007/s10508-011-9856-8 [DOI] [PubMed] [Google Scholar]
- Hayes, M. V. (1992). On the epistemology of risk: Language, logic and social science. Social Science & Medicine, 35(4), 401–407. 10.1016/0277-9536(92)90332-K [DOI] [PubMed] [Google Scholar]
- Herlihy, A. S. , McLachlan, R. I. , Gillam, L. , Cock, M. L. , Collins, V. , & Halliday, J. L. (2011). The psychosocial impact of Klinefelter syndrome and factors influencing quality of life. Genetics in Medicine, 13(7), 632–642. 10.1097/GIM.0b013e3182136d19 [DOI] [PubMed] [Google Scholar]
- Howard‐Bath, A. , Poulton, A. , Halliday, J. , & Hui, L. (2018). Population‐based trends in the prenatal diagnosis of sex chromosome aneuploidy before and after non‐invasive prenatal testing. Prenatal Diagnosis, 38(13), 1062–1068. 10.1002/pd.5363 [DOI] [PubMed] [Google Scholar]
- Huser, N. , Hulswit, B. B. , Koeller, D. R. , & Yashar, B. M. (2022). Improving gender‐affirming care in genetic counseling: Using educational tools that amplify transgender and/or gender non‐binary community voices. Journal of Genetic Counseling, 31, 1102–1112. 10.1002/jgc4.1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaramillo, C. , Nyquist, C. , Riggan, K. A. , Egginton, J. , Phelan, S. , & Allyse, M. (2019). Delivering the diagnosis of sex chromosome aneuploidy: Experiences and preferences of parents and individuals. Clinical Pediatrics, 58(3), 336–342. 10.1177/0009922818817310 [DOI] [PubMed] [Google Scholar]
- Kornman, L. , Palma‐Dias, R. , Nisbet, D. , Scott, F. , Menezes, M. , da Silva Costa, F. , & McLennan, A. (2018). Non‐invasive prenatal testing for sex chromosome aneuploidy in routine clinical practice. Fetal Diagnosis and Therapy, 44(2), 85–90. 10.1159/000479460 [DOI] [PubMed] [Google Scholar]
- Lalatta, F. , & Tint, G. S. (2013). Counseling parents before prenatal diagnosis: Do we need to say more about the sex chromosome aneuploidies? American Journal of Medical Genetics Part A, 161(11), 2873–2879. 10.1002/ajmg.a.36226 [DOI] [PubMed] [Google Scholar]
- Linden, M. G. , Bender, B. G. , & Robinson, A. (2002). Genetic counseling for sex chromosome abnormalities. American Journal of Medical Genetics, 110(1), 3–10. 10.1002/ajmg.10391 [DOI] [PubMed] [Google Scholar]
- Llorin, H. , & Zayhowski, K. (2021). Degendering “the gender test”—Reframing gender conversations in prenatal genetics clinics. National Society of Genetic Counselors Perspectives. https://perspectives.nsgc.org/Article/degendering‐the‐gender‐test‐reframing‐gender‐conversations‐in‐prenatal‐genetics‐clinics
- Llorin, H. , & Zayhowski, K. (2023). The erasure of transgender and intersex identities through fetal sex prediction and genetic essentialism. Journal of Genetic Counseling Advance Online Publication, 32, 942–944. 10.1002/jgc4.1736 [DOI] [PubMed] [Google Scholar]
- McCauley, E. , Ito, J. , & Kay, T. (1986). Psychosocial functioning in girls with Turner's syndrome and short stature: Social skills, behavior problems, and self‐concept. Journal of the American Academy of Child Psychiatry, 25(1), 105–112. 10.1016/S0002-7138(09)60606-3 [DOI] [PubMed] [Google Scholar]
- McConaghy, N. , Hadzi‐Pavlovic, D. , Stevens, C. , Manicavasagar, V. , Buhrich, N. , & Vollmer‐Conna, U. (2006). Fraternal birth order and ratio of heterosexual/homosexual feelings in women and men. Journal of Homosexuality, 51(4), 161–174. 10.1300/J082v51n04_09 [DOI] [PubMed] [Google Scholar]
- Mezei, G. , Papp, C. , Tóth‐Pál, E. , Beke, A. , & Papp, Z. (2004). Factors influencing parental decision making in prenatal diagnosis of sex chromosome aneuploidy. Obstetrics and Gynecology, 104(1), 94–101. 10.1097/01.AOG.0000128171.14081.eb [DOI] [PubMed] [Google Scholar]
- Miller, L. , Leeth, E. , Johnson, E. , Rosoklija, I. , Chen, D. , Aufox, S. , & Finlayson, C. (2018). Attitudes towards ‘disorders of sex development’ (DSD) nomenclature among physicians, genetic counselors, and mental health clinicians. Journal of Pediatric Urology, 14, 418.e1–e7. 10.1016/j.jpurol.2018.08.009 [DOI] [PubMed] [Google Scholar]
- Nathan, M. L. , Ormond, K. E. , Dial, C. M. , Gamma, A. , & Lunn, M. R. (2019). Genetic Counselors' and genetic counseling Students' implicit and explicit attitudes toward homosexuality. Journal of Genetic Counseling, 28(1), 91–101. 10.1007/s10897-018-0295-8 [DOI] [PubMed] [Google Scholar]
- National LGBT Health Education Center . (2016). Providing inclusive services and care for LGBT people: A guide for health care staff . http://www.lgbtqiahealtheducation.org/publication/learning‐guide
- National Society of Genetic Counselors . (2019). Professional Status Survey. https://www.nsgc.org/Policy‐Research‐and‐Publications/Professional‐Status‐Survey
- Pavlidis, K. , McCauley, E. , & Sybert, V. (1995). Psychosocial and sexual functioning of adult women with turner syndrome. Clinical Genetics, 47, 85–89. [DOI] [PubMed] [Google Scholar]
- Petersen, A. K. , Cheung, S. W. , Smith, J. L. , Bi, W. , Ward, P. A. , Peacock, S. , Braxton, A. , Van Den Veyver, I. B. , & Breman, A. M. (2017). Positive predictive value estimates for cell‐free noninvasive prenatal screening from data of a large referral genetic diagnostic laboratory. American Journal of Obstetrics and Gynecology, 217(6), 691.e1–e6. 10.1016/j.ajog.2017.10.005 [DOI] [PubMed] [Google Scholar]
- Pieters, J. J. P. M. , Kooper, A. J. A. , van Kessel, A. G. , Braat, D. D. M. , & Smits, A. P. T. (2011). Incidental prenatal diagnosis of sex chromosome aneuploidies: Health, behavior, and fertility. ISRN Obstetrics and Gynecology, 2011, 807106. 10.5402/2011/807106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggan, K. A. , Gross, B. , Close, S. , Weinberg, A. , & Allyse, M. A. (2021). Prenatal diagnosis of a sex chromosome aneuploidy: Parent experiences. Journal of Genetic Counseling, 30(5), 1407–1417. 10.1002/jgc4.1407 [DOI] [PubMed] [Google Scholar]
- Ross, J. , Zinn, A. , & McCauley, E. (2000). Neurodevelopmental and psychosocial aspects of turner syndrome. Mental Retardation and Developmental Disabilities Research Reviews, 6(2), 135–141. 10.1002/1098-2779(2000)6:23.0.CO;2-K [DOI] [PubMed] [Google Scholar]
- Sabin, J. A. , Riskind, R. G. , & Nosek, B. A. (2015). Health care Providers' implicit and explicit attitudes toward lesbian women and gay men. American Journal of Public Health, 105(9), 1831–1841. 10.2105/AJPH.2015.302631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagi, M. , Meiner, V. , Reshef, N. , Dagan, J. , & Zlotogora, J. (2001). Prenatal diagnosis of sex chromosome aneuploidy: Possible reasons for high rates of pregnancy termination. Prenatal Diagnosis, 21(6), 461–465. 10.1002/pd.78 [DOI] [PubMed] [Google Scholar]
- Schiavi, R. C. , Theilgaard, A. , Owen, D. R. , & White, D. (1988). Sex chromosome anomalies, hormones, and sexuality. Archives of General Psychiatry, 45(1), 19–24. 10.1001/archpsyc.1988.01800250023004 [DOI] [PubMed] [Google Scholar]
- Schilt, K. , & Westbrook, L. (2009). Doing gender, doing heteronormativity: “Gender Normals,” transgender people, and the social maintenance of heterosexuality. Gender and Society, 23(4), 440–464. [Google Scholar]
- Schippers, M. (2007). Recovering the feminine other: Masculinity, femininity, and gender hegemony. Theory and Society, 36(1), 85–102. [Google Scholar]
- Sheldon, J. P. , Pfeffer, C. A. , Jayaratne, T. E. , Feldbaum, M. , & Petty, E. M. (2007). Beliefs about the etiology of homosexuality and about the ramifications of discovering its possible genetic origin. Journal of Homosexuality, 52, 111–150. 10.1300/J082v52n03_06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Standards of Accreditation: ACGC . (2019). Accreditation council for genetic counselling . Retrieved from https://www.gceducation.org/standards‐of‐accreditation/
- Stevens, C. , Llorin, H. , Gabriel, C. , Mandigo, C. , Gochyyev, P. , & Studwell, C. (2023). Genetic counseling for fetal sex prediction by NIPT: Challenges and opportunities. Journal of Genetic Counseling, 32, 945–956. 10.1002/jgc4.1703 [DOI] [PubMed] [Google Scholar]
- Tartaglia, N. R. , Howell, S. , Sutherland, A. , Wilson, R. , & Wilson, L. (2010). A review of trisomy X (47,XXX). Orphanet Journal of Rare Diseases, 5, 8. 10.1186/1750-1172-5-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine, R. , Mills, R. , Nichols, T. , & Doyle, L. (2023). Disclosure and comfort during genetic counseling sessions with LGBTQ+ patients: An updated assessment. Journal of Genetic Counseling, 32(4), 833–845. 10.1002/jgc4.1692 [DOI] [PubMed] [Google Scholar]
- VandenLangenberg, E. , Veach, P. M. , LeRoy, B. S. , & Glessner, H. D. (2012). Gay, lesbian, and bisexual patients' recommendations for genetic counselors: A qualitative investigation. Journal of Genetic Counseling, 21(5), 741–747. 10.1007/s10897-012-9499-5 [DOI] [PubMed] [Google Scholar]
- West, C. , & Zimmerman, D. H. (1987). Doing Gender. Gender and Society, 1(2), 125–151. http://www.jstor.org/stable/189945 [Google Scholar]
- Wiener, S. , Sutherland, G. , Bartholomew, A. A. , & Hudson, B. (1968). XYY males in a Melbourne Prisone. The Lancet, 291(7534), 150. 10.1016/S0140-6736(68)92770-0 [DOI] [PubMed] [Google Scholar]
- Witkin, H. A. , Mednick, S. A. , Schulsinger, F. , Bakkestrom, E. , Christiansen, K. O. , Goodenough, D. R. , & Stocking, M. (1976). Criminality in XYY and XXY men. Science, 193(4253), 547–555. 10.1126/science.959813 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


