ABSTRACT
Objective
Lamina‐implantation is gradually becoming the main surgical method for the treatment of intraspinal tumors. Traditional titanium (Ti) internal fixation not only produces artifacts, which affects the observation of tumors and dural sac closure, but also faces the problem of secondary surgical removal. In this study, absorbable material were used in lamina replantation for the first time and was evaluated for its efficacy and safety.
Methods
We retrospectively enrolled patients who underwent short‐segment lamina replantation for intraspinal tumors in our center from February 2020 to November 2022. After condition matching of the number of fixation segment and fixation position, the baseline information, complications, neurological function, quality of life, spinal mobility and bone healing rate of the absorbable group and the Ti group were compared. Fisher exact, Chi‐square, or rank sum test were used for categorical variables, and t‐test was used for continuous variables to distinguish differences between groups.
Results
Cerebrospinal fluid leak was the most common complication, with no difference between the two groups (12.9% vs. 19.4%, p = 0.366). The bone healing rates of the two groups at 3 months after surgery were 77.4% and 87.1%, respectively, and there was no significant difference (p = 0.508). At 1 year after surgery, the resorbable group showedlower levels of anxiety/depression (1.20 ± 0.41 vs. 1.61 ± 0.61, p = 0.050), however, it did not affect the overall quality of life of the patients at 1 year.
Conclusion
Both titanium and absorbable internal fixation have shown good clinical results in the treatment of intraspinal tumors by laminareplantation. Regardless of cost, absorbable screws and plates are also suitable options for patients undergoing lamina replantation, because it has no stress shielding effect and does not require secondary removal. In addition, there are no artifacts in the image, which is more conducive to observing the recurrence of the tumor and the closure of the dural sac.
Keywords: bioabsorbable materials, intraspinal tumor, lamina replantation
Bioresorbable plates and screws were used to perform lamina reimplantation in patients with short‐level intraspinal tumors, and compared with traditional titanium materials in clinical outcomes, bone healing and quality of life.
1. Introduction
Intraspinal tumors, including intramedullary, extramedullary subdural and epidural tumors, are common tumors of the spine. Early complete resection is the mainstay of treatment for most primary intraspinal tumors [1]. As most intraspinal tumors are located dorsally, laminectomy is unavoidable for the sake of providing a full field of view to facilitate tumor removal. According to the Dennis three‐column theory, the posterior column is subjected to about 24%–30% pressure and about 21%–54% rotational stress, and laminectomy destroys the structural integrity of the posterior column of the vertebral body, thus affecting the biomechanical stability of the spine [2]. Long‐term laminar defects can lead to severe kyphosis and nerve damage, which seriously affects the stability and daily life of patients [3, 4]. To avoid kyphotic deformity and maintain the stability of the spine, researchers have tried using screw fixation after laminectomy, which, however, cannot prevent the bone structure from being destroyed. In addition, it may increase the occurrence of adjacent segment disease and decrease the mobility of the fixed segments. In addition, the serious consequences of iatrogenic spinal stenosis, cerebrospinal fluid (CSF) leakage, and the possibility of piercing the fixation screws into the spinal cord. Raimondi et al. was the first to try lamina replantation for the treatment of intraspinal tumors with good outcomes [5]. Lamina‐implantation preserves the structure of the spinous ligament complex, thus maintaining the posterior tension band and protecting the bone tissue and dural sac from being damaged. Studies currently have demonstrated that lamina replantation for the treatment of intraspinal tumors not only reduces intraoperative blood loss, operative time, and the incidence of postoperative complications, but also preserves the mobility of spinal motor segments to the greatest extent compared with screw fixation [1, 6, 7].
Traditional surgical suture fixation and wire fixation in lamina replantation, are often associated with high incidences of laminar displacement and bone nonfusion [8, 9]. At present, titanium (Ti) plates and screws are commonly used, but metallic materials greatly increase the risk of bone tissue infection. In addition, Ti internal fixation materials are often difficult to remove after prolonged use and there is also a risk of falling off, which often requires further surgery to have them removed. Over the past few decades, new resorbable plates and screws have been introduced as a reliable alternative to the treatment of fractures [10]. Bioresorbable materials include a variety of polymers such as polylactic acid, polyl‐lactic acid, or polyglycolic acid, all of which are degradable and can be replaced by tissues over time, devoid of secondary material removal after fracture healing. These absorbable materials have been successfully applied in the field of spine surgery, such as anti‐dural adhesion films, bioabsorbable cages and bioabsorbable screws [11]. Animal experiments have demonstrated that absorbable materials have better resistance to infection than traditional Ti alloy materials [12]. However, there is no study reporting the application of resorbable materials in spinal oncology.
The aims of the present study were as follows: (i) evaluating the safety and effectiveness of absorbable plates and screws for the treatment of short‐segment intraspinal tumors in lamina reimplantation and (ii) exploring the benefits and disadvantages of resorbable material by comparing the overall clinical outcome between the absorbable and Ti fixation materials in lamina reimplantation.
2. Patients and Methods
2.1. Baseline Characteristics and Clinical Information
The relevant clinical data of all patients who underwent lamina reimplantation in our center from February 2020 to November 2022 for intraspinal tumors were reviewed and analyzed, including demographic data (age, gender, and duration of symptoms), tumor information (tumor‐involving segment and tumor type), perioperative data (operative time, internal fixation method, intraoperative blood loss, postoperative drainage volume, postoperative complications, and hospital stay), neurological function information [Oswestry Disability Index (ODI)/Neck Disability Index (NDI) and Frankel score and Frankel neurological score], and Quality of life (QoL) information [Visual Anolog Scale (VAS) score, EQ‐5D‐5L score and patient satisfaction].
All patients were observed by conventional X‐ray and CT before surgery to observe the degree of displacement and angulation of each level of each segment to exclude the spinal instability such as lumbar spondylolisthesis before surgery. Preoperative electromyography was performed to exclude peripheral neuropathy and spinal nervous system diseases. After routine scanning, all patients underwent preoperative contrast‐enhanced MRI to determine the tumor size and its relationship with the nerve root and spinal cord.
2.2. Surgical Treatment
After fully communicating the pros and cons of the two types of materials with the patients who were scheduled to undergo short‐segment lamina replantation, the patients and their families were free to choose either the absorbable material or the conventional Ti alloy material.
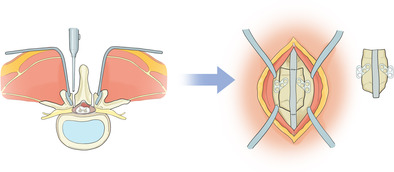
The surgical procedures were performed by the same surgical team in all patients of both groups. After successful tracheal intubation under general anesthesia, the patient was laid in a prone position. According to the three‐dimensional (3D) positioning of the tumor segment, the posterior median longitudinal incorporation was taken with the tumor segment as the center, followed by exposure of the bilateral muscles, bilateral lamina and spinous processes in sequence, during which special attention was paid to preserving the integrity of the superior spinous ligaments, and interspinous ligaments. The position of the absorbable or titanium alloy microplate was designed according to individual patients, and the microplate was bent in tailor to the need for cutting. The lamina was cut with an ultrasound bone knife about 2–3 mm medial to the facet joint, and spinous plate ligament complex was cut accordingly. The pre‐flexed microcompression locking plate was secured to the spinous plate ligament complex for later use. With the help of a microscope, the dural sac was cut open, the nerve tissue attached to the tumor was separated, and the tumor tissue was completely exposed and resected. CSF was supplemented with normal saline to maintain normal CSF pressure. The dural sac was sutured, the spinous process plate ligament complex was reduced and fixed with screws, and the supraspinous ligament and interspinous ligament were sutured. After placing the drain, the incision layer was sewed up (Figure 1). Postoperative CSF leakage was defined as postoperative postural orthostatic headache or discharge of clear fluid from a wet wound [13].
FIGURE 1.
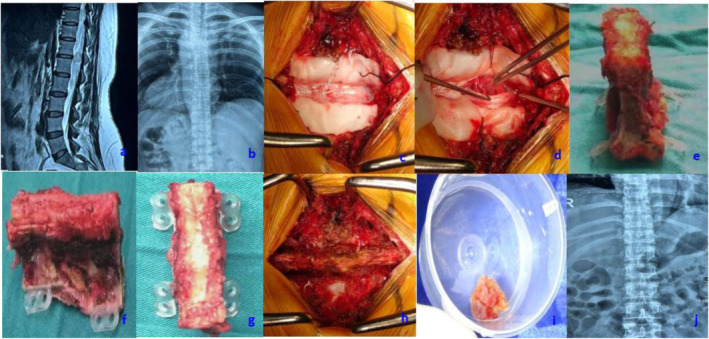
Perioperative data of patients with absorbable plates. Perioperative data of patients with absorbable plates. T12‐L1 intraspinal tumor was found in preoperative MRI (a) and preoperative X‐ray showed no bone destruction (b). In the operation, the lamina were removed, the dural sac was completely expose (c), and tumor was exposed completely resected (d). The excised laminas were connected with absorbable locking plates (e–g) and completely replanted into body (h). The rescted tumor tissue was sent for pathological examination (i). Postoperative X‐ray showed obvious laminae osteotomy line of T12‐L1 without internal fixation image (j).
2.3. Postoperative Follow‐Up
Imaging evaluation was performed in all patients after surgery. At 3 and 12 months after operation, posteroanterior and lateral X‐ray radiographies were performed to evaluate bone healing, postoperative adjacent segment degeneration (ASD), and spinal deformity. ASD was defined as new degenerative imaging findings in adjacent segments of the fusion segment after fusion accompanied by corresponding clinical symptoms [14]. The degree of bone fusion was judged by the presence of a trabecular bridge through the fracture segment without a transparent band on the X‐ray radiogram, which means that the fusion is successful [15]. If postoperative CSF leakage occurred persistently, MRI was repeated to observe the closure of the dural sac. MRI was followed up 3 months and 1 year after surgery to observe tumor recurrence. One year after surgery, X‐ray radiography was performed to measure the range of motion (ROM) of the cervical and lumbar spine in terms of flexion/extension.
In addition, the postoperative QoL information and neurological function were collected through physical examination and questionnaire investigation, including the postoperative Frankel score, postoperative VAS score, EQ‐5D‐5L score and patient satisfaction. NDI/ODI evaluation of the cervical and lumbar spine was performed. The EQ‐5D‐5L scale consists of five dimensions: mobility, usual activities, self‐care, anxiety/depression, and pain/discomfort, with five options for each dimension. The minimum score for each dimension is 5 points, with higher scores indicating better QoL in each dimension (0 points indicating no impairment at all, and 5 points indicating very severe impairment), and finally the total score of the 5 dimensions was calculated.
2.4. Inclusion and Exclusion Criteria
Inclusion criteria were patients (1) with single or adjacent multiple intraspinal tumors; (2) with complete clinicopathological data; (3) with no spinal instability or structural destroy; and (4) who underwent lamina replantation involving fewer than three segments.
The exclusion criteria were patients (1) whose tumors involved the vertebral body and appendages, (2) whose tumors grew inside and outside the spinal canal, (3) with recurrent intraspinal tumors, (4) with metastatic tumors in the spine, (5) with obvious osteoporosis (T < −2 g/cm2), (6) with a previous history of poor bone healing, and (7) who were lost to follow‐up.
2.5. Match of Patients
To better evaluate the effectiveness of the absorbable internal fixation materials on the bone healing rate and stability, we did 1:1 conditional matched in the Ti group with the absorbable group as the criterion. The matching conditions includedthe number of fixation segment and fixation position. This study was approved by the Institutional Review Board of Changzheng Hospital, Naval Medical University (IRB number: 2022‐143).
3. Statistical Methods
The informed consent was obtained from the patients or their guardians prior to surgery. Quantitative data are described in terms of mean, median (range), and qualitative data are described in terms of counts and percentages. The patients were divided into absorbable material group and Ti material group. Univariate difference analysis was performed on all factors. Fisher exact test, Pearson Chi‐square test, or Wilcoxon rank sum test was used for categorical variables, and student t test was used for continuous variables to distinguish differences between groups. p Value less than or equal to 0.05 was considered statistically significant. All statistical calculations were performed using SPSS Statistics, version26.0 (SPSS Inc., Chicago, IL, USA).
4. Results
4.1. Patient Features
During the 2‐year inclusion phase, 62 patients with spinal canal tumors were selected from 152 cases of intraspinal tumors in our center. The flow chart of enrollment, screening, and matching of patients is shown in Figure 2.
FIGURE 2.
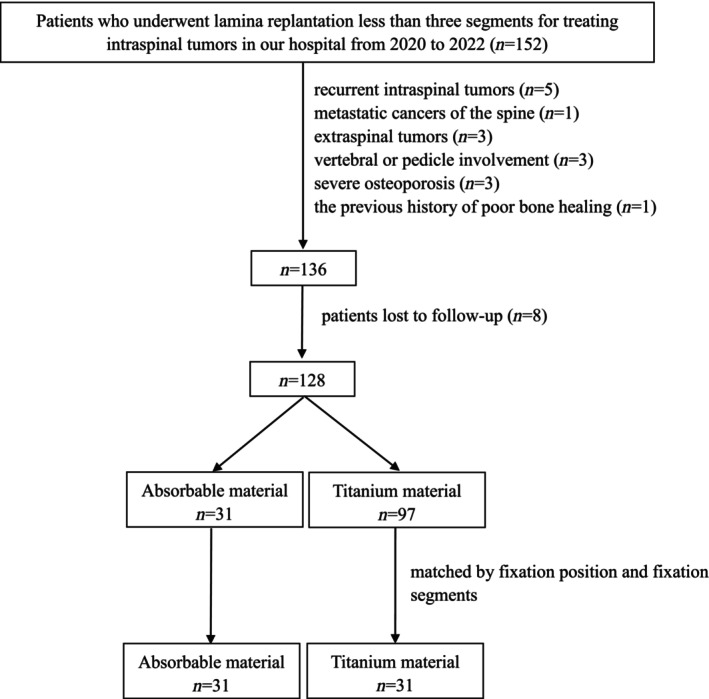
Flow chart of enrollment, screening, and matching of patients.
Schwannomas were found as the most common tumors in the spinal canal (31/62, 50.0%). A high proportion (52/62, 83.8%) of the intraspinal tumors had already exhibited a high rate of invasion by the time when the patient came to the doctor for the presenting symptoms, with the tumor occupying more than a half of the diameter of the spinal canal. There was no significant difference in baseline data and tumor information between the two groups (Table 1).
TABLE 1.
Baseline characteristics between the two group.
| Characteristic | Absorbable material (n = 31) | Titanium material (n = 31) | p |
|---|---|---|---|
| Age (y) | 51 ± 18 | 49 ± 17 | 0.721 |
| Sex (female) | 14 (45%) | 12 (39%) | 0.609 |
| Pathological diagnosis (schwannoma/meningioma/others) | 17/5/9 | 14/9/8 | 0.474 |
| Duration of symptoms (ms) | 8 ± 14 | 16 ± 35 | 0.249 |
| Fixation segments (single/two) | 10/21 | 10/21 | — |
| Fixation position (cervical/thoracic/lumbar) | 6/9/16 | 6/9/16 | — |
| Tumor diameter/spinal cord diameter (> 0.5/≤ 0.5) | 27/4 | 25/6 | 0.454 |
Abbreviations: ms, months; y, year.
4.2. Surgical Outcomes
The mean operative time in absorbable material group was longer than that in Ti material group (192.6 ± 25.4 min vs. 181.0 ± 17.4 min, p = 0.037), but there was no significant difference in intraoperative blood loss (208.1 ± 98.4 mL vs. 257.5 ± 114.1 mL, p = 0.064) and postoperative drainage (191.3 ± 85.6 mL vs. 185.5 ± 80.7 mL, p = 0.637) between the two groups (Table 2). CSF leakage was the most common complication in both groups, showing no significant difference between them (12.9% vs. 19.4%, p = 0.366). In addition, one patient in absorbable material group developed deep vein thrombosis of the lower extremities and was treated with the thrombosis filter, and one patient with cervical spinal canal tumor developed respiratory failure and was put on ventilator‐assisted ventilation. In Ti material group, one patient developed postoperative CSF infection and was treated with lumbar cistern drainage and meropenem.
TABLE 2.
Comparison of the surgical outcomes between the two groups.
| Group | Surgical time (min) | Intraoperative blood loss (mL) | Drainage volume 3 days postoperatively (mL) | Cerebrospinal fluid leakage | Other complications | Hospital stay (days) |
|---|---|---|---|---|---|---|
| Absorbable material (n = 31) | 192.6 ± 25.4 | 208.1 ± 98.4 | 191.3 ± 85.6 | 4 (12.9%) | 2 (6.4%) | 14.0 ± 2.3 |
| Titanium material (n = 31) | 181.0 ± 17.4 | 257.5 ± 114.1 | 185.5 ± 80.7 | 6 (19.4%) | 1 (3.2%) | 14.4 ± 2.6 |
| p | 0.032* | 0.064 | 0.637 | 0.366 | 0.500 | 0.624 |
p ≤ 0.05.
4.3. Follow‐Up Outcomes
At 1‐year follow‐up, ODI and NDI were significantly decreased in both groups compared with the baseline values before surgery (Table 3). There was no significant difference between the two groups in NDI and ODI. Although 83.8% of the intraspinal tumors occupied more than a half of the diameter of the spinal canal, only 25.8% (16/62) of patients exhibited severe neurological impairment (Frankel neurological grade below the C level), and they were admitted to the hospital with a flat car. We found a significant increase in the number of patients with Frankel D/E after surgery and the number of patients with Frankel E gradually increased over time (Figure 3). There was no significant difference in pre‐ and postoperative neurological function between the two groups.
TABLE 3.
Comparison of the follow‐up results between the two groups.
| Group | ODI (%) (n = 16) | NDI (%) (n = 6) | Frankel score (A‐C/D‐E) | Bone fusion | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | 3 ms p.o | 12 ms p.o | Preoperative | 3 ms p.o | 12 ms p.o | Preoperative | 3 ms p.o | 12 ms p.o | 3 ms p.o | 12 ms p.o | ||
| Absorbable material (n = 31) | 68.3 ± 13.4 | 25.8 ± 7.6 | 11.7 ± 3.6 | 26.0 ± 4.9 | 15.3 ± 2.7 | 9.5 ± 2.1 | 7/24 | 4/27 | 1/30 | 24 (77.4%) | 30 (96.8%) | 1 (3.2%) |
| Titanium material (n = 31) | 66.3 ± 14.0 | 24.8 ± 6.2 | 11.0 ± 2.5 | 25.7 ± 4.5 | 15.9 ± 2.2 | 10.6 ± 2.5 | 9/22 | 6/25 | 1/30 | 27 (87.1%) | 31 (100%) | 1 (3.2%) |
| p | 0.437 | 0.695 | 0.733 | 0.902 | 0.690 | 0.390 | 0.772 | 0.731 | 0.999 | 0.508 | 0.999 | 0.999 |
Abbreviations: ms, months; NDI, Neck disability index; ODI, Oswestry disability index; p.o, postoperative.
FIGURE 3.
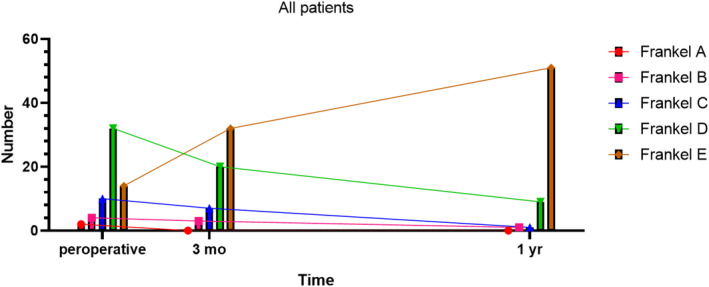
Changes of Frankel neurological function before and after operation.
The bone healing rate at 3 months after surgery was 77.4% in absorbable material group and 87.1% in Ti material group, showing no significant difference between the two groups (p = 0.508) (Figure 4). In addition, the number of fixed segments had no significant effect on the bone fusion rate (Table S1).
FIGURE 4.
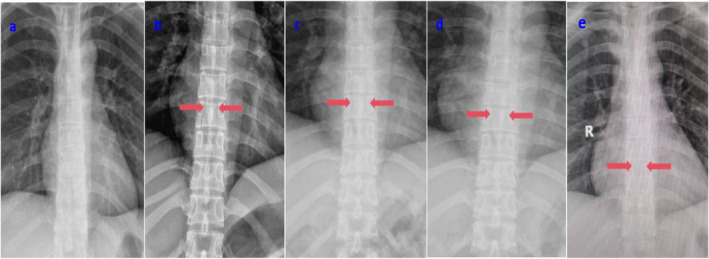
Bony fusion of the patient with absorbable materials. Preoperative X‐ray data showed no bone destruction (a). Postoperative X‐ray showed obvious fractures line of lamine, but no internal fixation images were observed (b). X‐ray showed that the fracture line was blurred and the callus was formed 3 months after surgery (c). X‐rays showed that the patient had healed bony 6 months after surgery (d). X‐rays 1 year postoperatively showed good fracture healing in patient (e).
One year after surgery, only one patient of absorbable material group had a fracture that did not fuse and was suggested to wear the brace for a long time. In resorbable material group, a patient with Schwannoma relapsed 6 months after surgery and received a second operation. In Ti material group, a patient with meningioma was admitted to the hospital 1 year after surgery because of chronic myelopathy recurrence, and underwent spinal canal exploration. Finally, the patient was found as having tumor cell relapse.
4.4. The Result of QoL
As shown in Table S2, pain/discomfort, usual activities and anxiety/depression were moderately limited (mean score ≥ 3), which became an important factor affecting preoperative QOL. Although the five dimensions of the EQ‐5D‐5L in both groups were significantly improved compared with those before surgery, there was no significant difference in any dimension at 3 months after surgery. At 1 year after surgery, the level of anxiety/depression in resorbable material group was lower than that in Ti material group (1.20 ± 0.41 vs. 1.61 ± 0.61, p = 0.050), but it did not affect the overall QoL of the patients at 1 year. In addition, 1 year after surgery, the mean of all dimensions of EQ‐5D‐5L of two group was between one and two.
4.5. ROM
The ROM of the spine was measured and recorded in 1 year after surgery. The ROMs for lumbar flexion and extension in the absorbable material group were79.6 ± 5.9 and 21.4 ± 4.1, respectivelyandthere was no statistical difference withtitanium materialgroup of 78.5 ± 4.0 and 22.3 ± 2.9 (p = 0.551 and p = 0.551). In addition, there was also no difference in cervical ROM between the two groups (39.2 ± 3.5 vs. 39.0 ± 3.7, p = 0.933; 37.0 ± 4.4 vs. 40.3 ± 2.6, p = 0.107). Therefore, thespine fixed with absorbent plates has the same good ROM with titanium plates.
5. Disscusion
In our study, we found no significant differences in postoperative complications, neurological function, bone healing rate, and spinal ROM despite the longer operative time of absorbable materials. However, patients in the resorbable material group had lower levels of anxiety 1 year after surgery. In addition, we found that, although there was one case of tumor recurrence in both groups, patients in the resorbable group were identified earlier and had milder symptoms.
5.1. Absorbable Internal Fixation for Lamina Replantation
Most intraspinal tumors are benign with insidious onset and atypical symptoms, and therefore are often confused with or comorbid with cervical spondylosis and lumbar disk herniation. With the gradual aggravation of the disease, the tumor can eventually compress the spinal cord and nerves, resulting in paralysis and/or bowel and urinary disorders, seriously affecting the QoL of patients. Deterioration of neurological function and incomplete resection have been shown by several studies as risk factors for poor prognosis after neuraxial tumor resection [16, 17]. Therefore, early and complete resection of intraspinal tumors and preservation of spinal anatomy and function are considered as the basic principles of intraspinal tumor surgery [18]. Post‐laminectomy lamina replantation with plate fixation is a popular practice in spine surgeons because it not only preserves the posterior bone structure and ligamentous complex of the spine, but also maximizes the mobility of the spine [19]. In addition, in the event of intraspinal tumor recurrence, revision surgery with laminoplasty is safer and easier than revision surgery with screw fixation after laminectomy because laminoplasty preserves relatively the normal posterior bone structure and prevents the epidural scar from adhering with the dural sac. Although the use of Ti plates for lamina implantation has been well documented, problems exist with Ti implants, including stress shielding, displacement, hyperesthesia, growth restriction, cold intolerance, and implant‐related infection [20]. Bioresorbable materials address many of these drawbacks. Most notably, there is no need to remove the implant and it does not hinder growth and development in the pediatric population. In addition, stress shielding is avoided, so that the bone plate can be more mechanically stimulated during the repair process. These benefits have encouraged the clinical application of bioresorbable internal fixation materials for fractures with good outcomes [21, 22]. For intraspinal tumors, resorbable materials will not produce artifacts, which facilitates observing dural sac healing and tumor recurrence. This is also a great temptation for patients with intraspinal tumors, because it attenuates the patient's worry about CSF leakage (the most common postoperative complication), tumor recurrence and reoperation. The use of resorbable materials has been shown to be reliable under low loads in the spine [11], so we use it for lamina reimplantation in cases involving less than three segments.
5.2. Clinical Outcomes
It was shown in our practice that the operative time of using absorbable plates was longer because there is a shaping phase. The incidence of complications was 19.4% (6/31), and the main cause was CSF leakage (12.9%). This is comparable to Ti implants. Our center and Ting et al. had reported that the occurrence of CSF leakage in laminoplasty with metal plates is 14.8% and 15.6%, respectively [1, 23]. Although some scholars have reported that absorbable materials exhibit a higher incidence of aseptic inflammation due to foreign body reactions to bioresorbable materials compared to traditional Ti alloy screws [24], this inflammation often occurs 2–3 months after surgery and is related to the type of absorbable materials [10]. No incisional and implant‐associated infection occurred in our study. Previous studies reported 21.7° ± 11.8° of ROM for screw fixation in lumbar lamina replantation [1], and our study showed that the ROM of lumbar lamina replantation was 36.4° ± 12.1° in Ti material group and 38.4° ± 15.1° in absorbable material group, showing no significant difference between the two groups.
In terms of QoL, anxiety was more pronounced in Ti material group 1 year after surgery, which may be related to patients' concerns about long‐term foreign body reactions. However, the gap between the two groups was small and did not affect the overall QoL. Our practice has shown that the overall clinical outcome is similar between bioabsorbable and Ti materials, and the latter offer more psychological benefits. However, more clinical data are necessary to substantiate this conclusion.
5.3. Bone Healing
Fracture healing is a topic of interest because of early low mechanical properties of biodegradable implants. A meta‐analysis including 25 clinical articles investigated the safety and effectiveness of bioresorbable materials in spinal fractures to answer the question about the low mechanical properties of biodegradable implants [25]. They reported that the overall mean bone healing rate was 89%, the mean bone healing rate was 92% for the cervical spine, and 83.6% for the lumbar spine. It was found in our study that the bone healing rate at 3 months and 1 year after surgery was 77.4% and 96.8%, respectively, in absorbable material group. Wang et al. analyzed the potential influencing factors of bone healing after lamina replantation, and found that age, gender, and surgical segment were not related to bone healing [23]. We performed the osteotomy with an ultrasonic osteotome, with neat osteotomy lines and narrow osteotomy space, which reduced bone loss and effectively promoted laminectomy bone healing. In addition, absorbable materials allow for small local movement at the broken end of the fracture, which is conducive to the growth of callus and fracture healing [10]. Although there was no significant difference in the fracture healing rate between the two groups and no correction of the fracture was required by secondary surgery, it has to be admitted that bioresorbable materials have greater instability in the first 4 weeks of fracture healing, so early undisturbed primary fracture healing is more needed [20]. By the fourth week the resorbable material is able to reduce the stress shielding effect, can better transfer the load to the fracture healing, promote bone healing under the fretting movement of small loads, and reduce the damage to bone tissue under high load activities, so as to better maintain the stability of bone healing [26]. It is generally believed that, 6–8 weeks after the fracture, the bony callus is formed, the fracture has basically healed, and therefore there is no need for fixation. Indeed, our postoperative fixation strategy is based on these studies, and we recommend that all patients wear a brace for 8 weeks.
5.4. Tumor Recurrence
Complete tumor resection is considered the most important strategy to prevent postoperative recurrence, but it is often troubled by adhesions between the tumor and the spinal cord and close relationship between the tumor and the key structures in the spinal cord, especially the spinal nerve roots and blood vessels. It is reported in the literature that the incomplete resection rate of intraspinal tumors can be as high as 14.5% [17]. Mahdy et al. reported a recurrence rate of 16% for extramedullary subdural tumors [27]. Asazuma et al. concluded that the recurrence rate of neuraxial tumors was 7.2% [28].
In this study, there was one recurrence in both groups (one was schwannoma and the other was meningioma), with an overall recurrence rate of 3.2% (2/62), and no death occurred in our series. Although there was no difference in recurrence rates between the two groups, one patient in Ti material group relapsed, accompanied with more severe neurological symptoms and a larger tumor diameter. Tumor recurrence is often associated with poorer neurological function outcomes and QoL [29], so early detection is crucial. This may be another advantage of absorbable materials.
5.5. Economic Burden of the Absorbable Material
It is understandable that the cost of internal fixation with absorbable materials is relatively high. One study showed even a three‐fold difference [20]. In spine surgery, there was a study comparing absorbable screws with plate fixation in anterior cervical surgery and the difference of average cost between the two groups was 70% [30]. In our experience, despite the cost of surgical operation in two group is basically same, the internal fixation cost of absorbable material is often about twice that of Ti material. The implant cost of both types are covered by Chinese National Health Insurance program.
Few previous studies had taken into account the long‐term burden of anxiety on patients and the cost of a second operation for Ti plate removal. In this case, the patient may be more inclined to choosing resorbable materials. In addition, it is not uncommon to have the metal plates and screws removed after bone healing, accounting for about 10% even in radius fractures with fewer loads [31]. But we believe that this economic gap will become smaller with the rapid development and wider application of biomaterials.
5.6. Strengths and Limitations
For the first time, we innovatively used absorbable plates and screws for the treatment of short‐segment intraspinal tumors during lamina reimplantation in this study, and compared them with Ti materials in terms of clinical outcomes and QoL. But as this is a single‐center retrospective study with a limited number of patients, and QoL data are influenced by day‐to‐day changes and the emotional state of the patient at the time. Therefore, the further prospective randomized trials are needed to verify the safety and effectiveness of bioresorbable plates and screws.
6. Conclusion
Both Ti and absorbable internal fixation materials have shown good clinical outcomes in the treatment of intraspinal tumors by laminar replantation. There was no significant difference in bone healing and complications between the two groups. The anxiety level in patients who used resorbable materials was lower than that in patients who used Ti materials at 1 year after surgery. Regardless of the cost, absorbable screws and plates are more suitable for patients undergoing lamina replantation due to the advantages of no stress shielding effect and requiring no secondary implant removal. In addition, they do not produce imaging artifacts, which is more conducive to observing tumor recurrence and closure of the dural sac.
Author Contributions
Conceptualization: Xinghai Yang. Data curation and formal analysis: Dingbang Chen, LuoSheng Zhang and Xin Gao. Writing – original draft: Dingbang Chen and Jinhan Song. Writing – review and editing: Xinghai Yang and Quan Huang.
Ethics Statement
The study was approved by the Institutional Review Board of Changzheng Hospital, Naval Medical University, for studies involving humans (IRB number: 2022–143).
Conflicts of Interest
The authors declare no conflicts of interest.
Supporting information
Table S1. The result of subgroup analysis of fixation segments.
Table S2. Comparison of the surgical outcomes between the two groups.
Acknowledgments
We would like to thank the editors, reviewers, and other persons for their assistance to improve the manuscript. Thanks to Dr. Xin Gao for his guidelines of editing. This work was supported by the National Natural Science Foundation of China (grant no. 82072961).
Funding: This work was supported by National Natural Science Foundation of China, 82072961.
Dingbang Chen and Jinhan Song contributed equally to this work and are co‐first authors.
References
- 1. Jiang L., Luo J., Gong H., et al., “Clinical and Biomechanical Study of Laminoplasty for Thoracic and Lumbar Intradural Tumors,” Journal of Clinical Medicine 12, no. 1 (2023): 355, 10.3390/jcm12010355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Denis F., “The Three Column Spine and Its Significance in the Classification of Acute Thoracolumbar Spinal Injuries,” Spine (Phila Pa 1976) 8, no. 8 (1983): 817–831, 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 3. Lee S. E., Chung C. K., Jahng T. A., and Kim H. J., “Long‐Term Outcome of Laminectomy for Cervical Ossification of the Posterior Longitudinal Ligament,” Journal of Neurosurgery. Spine 18, no. 5 (2013): 465–471, 10.3171/2013.1.SPINE12779. [DOI] [PubMed] [Google Scholar]
- 4. Abeloos L., De Witte O., Riquet R., Tuna T., and Mathieu N., “Long‐Term Outcome of Patients Treated With Spinal Cord Stimulation for Therapeutically Refractory Failed Back Surgery Syndrome: A Retrospective Study,” Neuro‐Chirurgie 57, no. 3 (2011): 114–119, 10.1016/j.neuchi.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 5. Raimondi A. J., Gutierrez F. A., and Di Rocco C., “Laminotomy and Total Reconstruction of the Posterior Spinal Arch for Spinal Canal Surgery in Childhood,” Journal of Neurosurgery 45, no. 5 (1976): 555–560, 10.3171/jns.1976.45.5.0555. [DOI] [PubMed] [Google Scholar]
- 6. Song Z., Zhang Z., Ye Y., Zheng J., and Wang F., “Efficacy Analysis of Two Surgical Treatments for Thoracic and Lumbar Intraspinal Tumours,” BMC Surgery 19, no. 1 (2019): 131, 10.1186/s12893-019-0602-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li H., Weng Y., Zhou D., Nong L., and Xu N., “Experience of Operative Treatment in 27 Patients With Intraspinal Neurilemmoma,” Oncology Letters 14, no. 4 (2017): 4817–4821, 10.3892/ol.2017.6799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yu L. X., Ping Z. Y., and Min L. J., “Laminoplasty for the Treatment of Extramedullary Intradural Tumors in the Thoracic and Lumbar Spine: Greater Than Two‐Year Follow‐Up,” Orthopaedic Surgery 1, no. 4 (2009): 275–279, 10.1111/j.1757-7861.2009.00050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dai G., Zhang M., Su W., et al., “Replantation of Lamina Spinous Process Ligament Complex and Miniature Titanium Plate Shaping Internal Fixation in the Treatment of Tumors in the Spinal Canal,” BMC Musculoskeletal Disorders 24, no. 1 (2023): 873, 10.1186/s12891-023-06984-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rokkanen P. U., Böstman O., Hirvensalo E., et al., “Bioabsorbable Fixation in Orthopaedic Surgery and Traumatology,” Biomaterials 21, no. 24 (2000): 2607–2613, 10.1016/s0142-9612(00)00128-9. [DOI] [PubMed] [Google Scholar]
- 11. Tomasino A., Gebhard H., Parikh K., Wess C., and Härtl R., “Bioabsorbable Instrumentation for Single‐Level Cervical Degenerative Disc Disease: A Radiological and Clinical Outcome Study,” Journal of Neurosurgery. Spine 11, no. 5 (2009): 529–537, 10.3171/2009.6.SPINE08838. [DOI] [PubMed] [Google Scholar]
- 12. Kitridis D., Savvidis P., Cheva A., Papalois A., Givissis P., and Chalidis B., “Are Absorbable Plates More Resistant to Infection Than Titanium Implants? An Experimental Pre‐Clinical Trial in Rabbits,” Journal of Functional Biomaterials 14, no. 10 (2023): 498, 10.3390/jfb14100498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dobrocky T., Nicholson P., Häni L., et al., “Spontaneous Intracranial Hypotension: Searching for the CSF Leak,” Lancet Neurology 21, no. 4 (2022): 369–380, 10.1016/S1474-4422(21)00423-3. [DOI] [PubMed] [Google Scholar]
- 14. Mimura T., Tsutsumimoto T., Yui M., Takahashi J., Kuraishi S., and Misawa H., “Adjacent Segment Pathology Following Posterior Lumbar Interbody Fusion for Lumbar Degenerative Spondylolisthesis: A Comparison Between Minimally Invasive and Conventional Open Approach,” Spine Journal 21, no. 8 (2021): 1297–1302, 10.1016/j.spinee.2021.03.027. [DOI] [PubMed] [Google Scholar]
- 15. Gruskay J. A., Webb M. L., and Grauer J. N., “Methods of Evaluating Lumbar and Cervical Fusion,” Spine Journal 14, no. 3 (2014): 531–539, 10.1016/j.spinee.2013.07.459. [DOI] [PubMed] [Google Scholar]
- 16. Brotchi J., “Intrinsic Spinal Cord Tumor Resection,” Neurosurgery 50, no. 5 (2002): 1059–1063, 10.1097/00006123-200205000-00021. [DOI] [PubMed] [Google Scholar]
- 17. Halvorsen C. M., Rønning P., Hald J., et al., “The Long‐Term Outcome After Resection of Intraspinal Nerve Sheath Tumors: Report of 131 Consecutive Cases,” Neurosurgery 77, no. 4 (2015): 585–593, 10.1227/NEU.0000000000000890. [DOI] [PubMed] [Google Scholar]
- 18. Samartzis D., Gillis C. C., Shih P., O'Toole J. E., and Fessler R. G., “Intramedullary Spinal Cord Tumors: Part II‐Management Options and Outcomes,” Global Spine Journal 6, no. 2 (2016): 176–185, 10.1055/s-0035-1550086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu Z., Zheng J. H., Yuan N., and Miao J., “Comparison of the Clinical Effects of Lamina Replantation and Screw Fixation After Laminectomy in the Treatment of Intraspinal Tumours,” Orthopaedic Surgery and Research 18 (2023): 617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Leno M. B., Liu S. Y., Chen C. T., and Liao H. T., “Comparison of Functional Outcomes and Patient‐Reported Satisfaction Between Titanium and Absorbable Plates and Screws for Fixation of Mandibular Fractures: A One‐Year Prospective Study,” Journal of Cranio‐Maxillo‐Facial Surgery 45, no. 5 (2017): 704–709, 10.1016/j.jcms.2017.01.034. [DOI] [PubMed] [Google Scholar]
- 21. Böstman O. M., “Absorbable Implants for the Fixation of Fractures,” Journal of Bone and Joint Surgery 73, no. 1 (1991): 148–153. [PubMed] [Google Scholar]
- 22. Simon J. A., Ricci J. L., and Di Cesare P. E., “Bioresorbable Fracture Fixation in Orthopedics: A Comprehensive Review. Part II. Clinical Studies,” American journal of orthopedics (Belle Mead, NJ) 26, no. 11 (1997): 754–762. [PubMed] [Google Scholar]
- 23. Wang Z. C., Li S. Z., Sun Y. L., et al., “Application of Laminoplasty Combined With ARCH Plate in the Treatment of Lumbar Intraspinal Tumors,” Orthopaedic Surgery 12, no. 6 (2020): 1589–1596, 10.1111/os.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weiler A., Helling H. J., Kirch U., Zirbes T. K., and Rehm K. E., “Foreign‐Body Reaction and the Course of Osteolysis After Polyglycolide Implants for Fracture Fixation: Experimental Study in Sheep,” Journal of Bone and Joint Surgery. British Volume (London) 78, no. 3 (1996): 369–376. [PubMed] [Google Scholar]
- 25. Koutserimpas C., Alpantaki K., Chatzinikolaidou M., Chlouverakis G., Dohm M., and Hadjipavlou A. G., “The Effectiveness of Biodegradable Instrumentation in the Treatment of Spinal Fractures,” Injury 49, no. 12 (2018): 2111–2120, 10.1016/j.injury.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 26. Liu C., Huang L., Zhang H., et al., “Biomechanical Comparison Between Bioabsorbable and Medical Titanium Screws in Distal Chevron Osteotomy of First Metatarsal in Hallux Valgus Treatment,” Journal of the Mechanical Behavior of Biomedical Materials 131 (2022): 105260, 10.1016/j.jmbbm.2022.105260. [DOI] [PubMed] [Google Scholar]
- 27. El‐Mahdy W., Kane P. J., Powell M. P., and Crockard H. A., “Spinal Intradural Tumours: Part I‐‐Extramedullary,” British Journal of Neurosurgery 13, no. 6 (1999): 550–557, 10.1080/02688699943042. [DOI] [PubMed] [Google Scholar]
- 28. Asazuma T., Toyama Y., Watanabe M., Suzuki N., Fujimura Y., and Hirabayashi K., “Clinical Features Associated With Recurrence of Tumours of the Spinal Cord and Cauda Equina,” Spinal Cord 41, no. 2 (2003): 85–89, 10.1038/sj.sc.3101394. [DOI] [PubMed] [Google Scholar]
- 29. R X., Ja M., Kg A., D L., Te M., and Ec B., “Quality of Life Outcomes Following Resection of Adult Intramedullary Spinal Cord Tumors,” Neurosurgery 78, no. 6 (2016): 821–828, 10.1227/NEU.0000000000001147. [DOI] [PubMed] [Google Scholar]
- 30. Qiu X., Zhao B., He X., Zhao C., and Leng Z., “Interface Fixation Using Absorbable Screws Versus Plate Fixation in Anterior Cervical Corpectomy and Fusion for Two‐Level Cervical Spondylotic Myelopathy,” Medical Science Monitor 26 (2020): e921507, 10.12659/MSM.921507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Meyer M. A., Benavent K. A., Chruscielski C. M., Janssen S. J., Blazar P. E., and Earp B. E., “The Impact of the Soong Index on Hardware Removal and Overall Reoperation Rates After Volar Locking Plate Fixation of Distal Radius Fractures,” Journal of Hand Surgery 47, no. 6 (2022): 584.e1–584.e9, 10.1016/j.jhsa.2021.06.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. The result of subgroup analysis of fixation segments.
Table S2. Comparison of the surgical outcomes between the two groups.


