Graphical Abstract
To the Editor:
Lymphangioleiomyomatosis (LAM) is a rare neoplasm, predominantly seen among young women, involving proliferation and metastatic infiltration of the lungs by atypical smooth muscle-like cells. LAM is caused by mutations in the tuberous sclerosis complex (TSC) genes that lead to constitutive activation of the mechanistic target of rapamycin (mTOR) pathway.1 Sirolimus, an oral mTOR inhibitor, has been shown to stabilize lung function decline in patients with LAM2 and has become the first-line treatment option for qualifying patients.3
Spontaneous pneumothorax (SP) is a frequent source of morbidity for patients with LAM; more than 50% of patients with LAM experience at least one SP, with an approximately 70% chance of recurrence.4,5 Pleurodesis can reduce the recurrence risk to approximately 30% and is recommended for all patients with LAM after the first episode of SP.4,5 Whether treatment with mTOR inhibitors can reduce the risk of recurrent SPs is not well established. The objectives of our study were to determine (1) the relationship between age and menopausal status on the risk of development of SP and (2) the impact of mTOR inhibitors on the incidence of recurrent SPs.
Methods
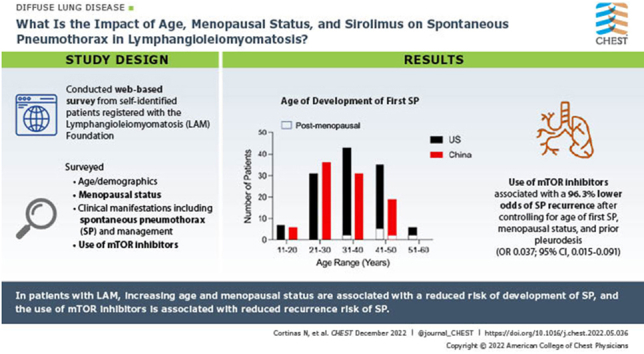
We conducted a web-based survey of patients self-identified with LAM and registered with the LAM Foundation. The survey included questions regarding demographics, menopausal status, clinical manifestations including details of SPs and the treatments received for the management of SPs, and the use of mTOR inhibitors. Responses were collected and managed with the Research Electronic Data Capture (REDCap) tools hosted at the University of Cincinnati. The questionnaire was subsequently translated into Chinese to obtain independent external validation of the results. A similar web-based approach to data gathering was used to gather information from patients with LAM seen at the Guangzhou Institute of Respiratory Health in China. The study was reviewed and approved by the University of Cincinnati Institutional Review Board (IRB No. 2018-1324).
Respondent characteristics and data are reported descriptively, using frequencies, percentages, central tendency (median), and interquartile range (IQR). The statistical significance of the difference in proportions was estimated by χ2 test. Data from the US and Chinese cohorts were combined to perform multivariable logistic regression to examine the association between SP recurrence and mTOR inhibitor use after controlling for the following variables: age at first SP, menopausal status, and prior pleurodesis. All analyses were conducted with a prespecified significance threshold of .05. Data analysis was performed with Microsoft Excel and Stata 17 (StataCorp).
Results
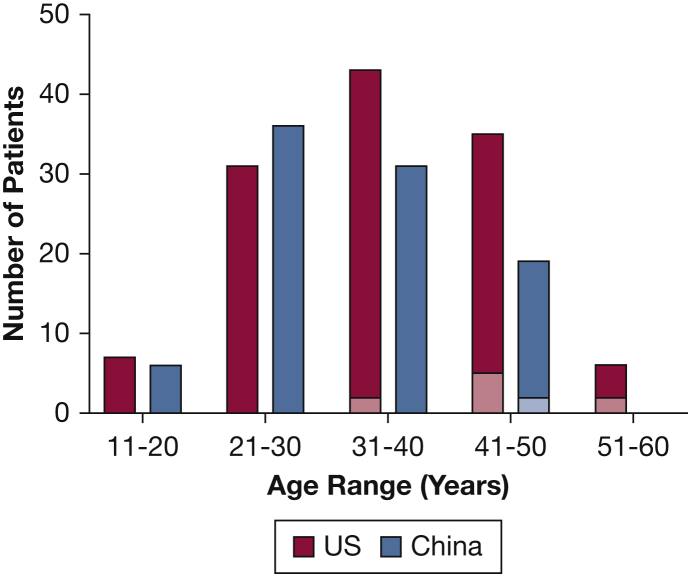
Our cohort consisted of 251 patients from the United States and 206 from China (Table 1). Of the US responders, 108 (43%) were premenopausal, 103 (41%) were postmenopausal, and 40 (16%) were unsure of their menopausal status. One hundred twenty-three patients (49%) had experienced at least one SP, with 70% experiencing at least one additional SP. The median (IQR) age at development of SP was 36 (29-43) years (Fig 1). There were 65 postmenopausal patients with LAM who had not experienced a prior SP. Nine patients (13.8%) reported that their first SP occurred after menopause, in contrast to 55 premenopausal patients (51%) with at least one SP (P < .001). Among those with a history of SP, 71 patients (58%) reported receiving mTOR inhibitors, with three patients (4.2%) experiencing a recurrent SP after the initiation of mTOR inhibitors, compared with 33 untreated patients (63.4%) with a recurrent SP (P < .001). The proportion of patients who underwent pleurodesis was similar among patients taking mTOR inhibitors compared with patients not taking mTOR inhibitors (32 of 71 [45%] taking mTOR inhibitors vs 21 of 52 [40%] not taking mTOR inhibitors; P = .60).
Table 1.
Key Demographic and Clinical Features of Cohorts
| Variable | Data, No. (%) or Median (IQR) |
|
|---|---|---|
| US Patients With LAM (n = 251) | Chinese Patients With LAM (n = 206) | |
| Race | ||
| White | 228 (90%) | 8 (4%) |
| Asian | 10 (4%) | 172 (83%) |
| Black | 5 (2%) | 26 (13%) |
| Preferred not to answer | 8 (3%) | |
| LAM subtype | ||
| Sporadic LAM | 196 (78%) | 134 (65%) |
| TSC-LAM | 30 (12%) | 23 (11%) |
| Unsure/unknown | 25 (10%) | 49 (24%) |
| Menopausal status | ||
| Premenopausal | 108 (43%) | 152 (74%) |
| Postmenopausal | 103 (41%) | 33 (16%) |
| Unsure/unknown | 40 (16%) | 21 (10%) |
| Age at menarche, y | 13 (11-20) | 14 (13-15) |
| Age at menopause, y | 47 (35-53) | 47 (43-50) |
| Age at LAM diagnosis, y | 42 (29-56) | 35 (30-42) |
| Age at symptom onset, y | 35 (32-45) | 33 (28-41) |
| mTOR inhibitor use | 119 (47%) | 154 (75%) |
| History of SP | 123 (49%) | 95 (46%) |
| Age at first SP, y | 36 (29-43) | 31 (25-38) |
| Age at last SP, y | 37 (30-47) | 32 (27-39) |
| Among patients with a history of SP, No. with pleurodesis | 53 (42%) | 49 (52%) |
| Among patients with a history of SP, No. treated with mTOR inhibitors | 71 (58%) | 77 (81%) |
| No. of patients with recurrent SP following initiation of mTOR inhibitors | 3 (4%) | 11 (14%) |
| Among patients with a history of SP, No. with multiple SPs | 86 | 74 |
| Ipsilateral recurrence | 58 (67%) | 37 (50%) |
| Contralateral occurrence | 26 (30%) | 34 (46%) |
| Unsure/unknown | 2 (2%) | 3 (4%) |
IQR = interquartile range; LAM = lymphangioleiomyomatosis; mTOR = mechanistic target of rapamycin; SP = spontaneous pneumothorax; TSC = tuberous sclerosis complex.
Figure 1.
Bar graph depicting the age at development of first spontaneous pneumothorax in US and Chinese patients with lymphangioleiomyomatosis. Dark colored areas in each bar represent premenopausal patients, and lighter areas represent postmenopausal patients.
Of the Chinese responders, 152 (74%) were premenopausal, 33 (16%) were postmenopausal, and 21 (10%) were unsure of their menopausal status. Ninety-five patients (46%) had experienced at least one SP, with 76% experiencing at least one additional SP. The median (IQR) age at development of SP was 31 (25-38) years. There were 13 postmenopausal patients with LAM who had not experienced a prior SP. Two patients (15%) reported their first SP following menopause, as opposed to 82 premenopausal patients (54%) with at least one SP (P = .008). Among those with a history of SP, 77 patients (81%) reported receiving mTOR inhibitors, with 11 patients (14%) experiencing a recurrent SP following initiation of mTOR inhibitors, compared with 14 untreated patients (78%) with a recurrent SP (P < .001). The proportion of patients who underwent pleurodesis was similar among patients taking mTOR inhibitors compared with patients not taking mTOR inhibitors (38 of 77 patients taking mTOR inhibitors [49%] vs 11 of 18 patients not taking mTOR inhibitors [61%]; P = .37).
Finally, the results of multivariable logistic regression revealed that the use of mTOR inhibitors is associated with 96.3% lower odds of SP recurrence after controlling for age at first SP, menopausal status, and prior pleurodesis (OR, 0.037; 95% CI, 0.015-0.091; P < .001).
Discussion
The major findings of our analysis are that in patients with LAM, increasing age and menopausal status are associated with a reduced risk of development of SP, and the use of mTOR inhibitors is associated with reduced recurrence risk of SP.
In our analysis, the median age at development of SP in the US and Chinese cohorts was 36 and 31 years, respectively, and the majority of first SPs occurred before the age of 50 years, consistent with the prior literature on LAM.4 A recent machine learning-based cluster analysis conducted on two large LAM cohorts identified a distinct LAM subgroup composed of older patients with reduced risk of SP.6 A role for female sex hormones in the pathogenesis of LAM has long been speculated,1 and menopausal status has been associated with a differential natural history of disease progression as well as response to treatment with mTOR inhibitors.7,8 Our findings further highlight the importance of menopausal status as a useful variable that portends a different clinical course for women with LAM. At present, all patients with LAM receive similar counseling regarding their risk of developing SP as well as the consideration of early pleurodesis to reduce future recurrence risk. Our findings suggest a more nuanced approach toward counseling and treatment of patients with LAM regarding SPs, taking into account their age and menopausal status.
Although the role of mTOR inhibitors in stabilizing lung function decline in LAM is clear, the benefit of mTOR inhibitors in reducing the risk of future SPs is not well established. Two small case series from China and Japan have suggested a potential beneficial role for sirolimus in reducing the risk of recurrent SPs in patients with LAM.9,10 The results from our analysis are in keeping with the findings from these reports and lend further credence to the potential beneficial role of mTOR inhibitors in reducing the burden of SPs in patients with LAM. Current clinical practice guidelines for LAM recommend treatment with mTOR inhibitors for patients with abnormal and/or declining lung function and for patients with problematic chylous effusions.3 We submit that recurrent SPs should be considered an additional criterion for potential initiation of mTOR inhibitors in LAM. However, the optimal trigger and the timing of mTOR inhibitor initiation for the primary purpose of reducing the burden of SPs in LAM need to be better defined.
Several limitations of our analysis should be noted. The study design is associated with the possibility of selection as well as recall bias. However, these biases are mitigated to a large extent by the inclusion of an independent Chinese LAM cohort that revealed remarkably similar results compared with the US LAM cohort. We were unable to account for pulmonary function as an independent variable while assessing the association between mTOR inhibitor use and SP recurrence. Lastly, age and menopause are not mutually exclusive and we are unable to differentially examine the independent effect of these variables.
In conclusion, age and menopausal status are important factors determining the risk of SP; they should be taken into account when counseling patients with LAM and might assist in devising individualized management strategies. mTOR inhibitors might be useful in mitigating the risk of recurrent SPs, and this aspect of pharmacotherapy in LAM warrants further investigation.
Acknowledgments
Author contributions: N. G. has full access to all the data in this study and had final responsibility for the decision to submit for publication. N. G. conceived the study design. E. K. and N. G. developed the data collection instrument. J. L. translated the data collection survey into Chinese and helped distribute the survey to the Chinese LAM population. N. C., H. M., R. B., and N. G. performed the data analysis. N. C. and N. G. wrote the initial draft of the manuscript that was subsequently edited and approved by all listed authors.
Role of sponsors: The sponsors had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: The authors thank Dr Zulma Swank, MD, for assistance in the creation of the study questionnaire. The authors also express sincere gratitude to the patients with LAM who took the time to complete the survey and for their constant support and commitment to research.
Footnotes
FUNDING/SUPPORT: J. L. was supported by the following grants: the Natural Science Foundation of Guangdong Province (No. 2021A1515011352), the National Key Research and Development Program of China (No. 2016YFC0901502), and the Zhongnanshan Medical Foundation of Guangdong Province (No. ZNSA-2020013).
FINANCIAL/NONFINANCIAL DISCLOSURES: None declared.
References
- 1.McCarthy C., Gupta N., Johnson S.R., Yu J.J., McCormack F.X. Lymphangioleiomyomatosis: pathogenesis, clinical features, diagnosis, and management. Lancet Respir Med. 2021;9(11):1313–1327. doi: 10.1016/S2213-2600(21)00228-9. [DOI] [PubMed] [Google Scholar]
- 2.McCormack F.X., Inoue Y., Moss J., et al. National Institutes of Health Rare Lung Diseases Consortium; MILES Trial Group Efficacy and safety of sirolimus in lymphangioleiomyomatosis. N Engl J Med. 2011;364:1595–1606. doi: 10.1056/NEJMoa1100391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCormack F.X., Gupta N., Finlay G.R., et al. ATS/JRS Committee on Lymphangioleiomyomatosis Official American Thoracic Society/Japanese Respiratory Society clinical practice guidelines: lymphangioleiomyomatosis diagnosis and management. Am J Respir Crit Care Med. 2016;194(6):748–761. doi: 10.1164/rccm.201607-1384ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Almoosa K.F., Ryu J.H., Mendez J., et al. Management of pneumothorax in lymphangioleiomyomatosis: effects on recurrence and lung transplantation complications. Chest. 2006;129(5):1274–1281. doi: 10.1378/chest.129.5.1274. [DOI] [PubMed] [Google Scholar]
- 5.Gupta N., Finlay G.A., Kotloff R.M., et al. ATS Assembly on Clinical Problems Lymphangioleiomyomatosis diagnosis and management: high-resolution chest computed tomography, transbronchial lung biopsy, and pleural disease management. an official American Thoracic Society/Japanese Respiratory Society clinical practice guideline. Am J Respir Crit Care Med. 2017;196(10):1337–1348. doi: 10.1164/rccm.201709-1965ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chernbumroong S., Johnson J., Gupta N., et al. Machine learning can predict disease manifestations and outcomes in lymphangioleiomyomatosis. Eur Respir J. 2021;57(6) doi: 10.1183/13993003.03036-2020. [DOI] [PubMed] [Google Scholar]
- 7.Gupta N., Lee H.S., Ryu J.H., et al. NHLBI LAM Registry Group The NHLBI LAM Registry: prognostic physiologic and radiologic biomarkers emerge from a 15-year prospective longitudinal analysis. Chest. 2019;155(2):288–296. doi: 10.1016/j.chest.2018.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta N., Lee H.S., Young L.R., et al. NIH Rare Lung Disease Consortium Analysis of the MILES cohort reveals determinants of disease progression and treatment response in lymphangioleiomyomatosis. Eur Respir J. 2019;53(4) doi: 10.1183/13993003.02066-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sakurai T., Arai T., Hirose M., et al. Reduced risk of recurrent pneumothorax for sirolimus therapy after surgical pleural covering of entire lung in lymphangioleiomyomatosis. Orphanet J Rare Dis. 2021;16(1):466. doi: 10.1186/s13023-021-02081-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou L., Ouyang R., Luo H., et al. Efficacy of sirolimus for the prevention of recurrent pneumothorax in patients with lymphangioleiomyomatosis: a case series. Orphanet J Rare Dis. 2018;13(1):168. doi: 10.1186/s13023-018-0915-2. [DOI] [PMC free article] [PubMed] [Google Scholar]