Abstract
Background
Osteoarthritis (OA) is prevalent, yet its management remains challenging. This meta-analysis aims to evaluate the efficacy of acupuncture combined with moxibustion versus other standard treatments in patients with knee osteoarthritis (KOA) based on randomized controlled trials (RCTs).
Methods
Searches were conducted in Ovid MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials to retrieve relevant RCTs. Data on baseline characteristics, treatment efficacy, and adverse events were extracted. The analysis utilized pooled weighted mean differences (WMD) and risk ratios (RR) with 95% confidence intervals (CIs) to assess the superior treatment modality.
Results
A total of 18 RCTs were included. Acupuncture combined with moxibustion demonstrated significant improvement in the visual analog scale (VAS) for pain and the long-term (> 60 weeks) Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores for pain, stiffness, and physical function compared to other treatments. In contrast, short- (< 4 weeks) and mid-term (6–60 weeks) WOMAC outcomes for pain, stiffness, and physical function indicated varied results. The overall efficacy rate also favored the combined therapy significantly in the short- and mid-term evaluations. Notably, this therapy was associated with fewer adverse events.
Conclusion
The meta-analysis reveals that acupuncture combined with moxibustion is notably more effective and safer than other treatment modalities for KOA, particularly during mid- and long-term follow-up periods.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13643-025-02762-x.
Keywords: Acupuncture, Moxibustion, Knee osteoarthritis, Meta-analysis, Treatment, Adverse events
Background
Osteoarthritis (OA) is a prevalent and progressive disorder characterized by pain and dysfunction in the affected joint [1]. It impacts approximately 10% of men and 18% of women over 60 [2]. OA can involve multiple peripheral joints, both small (such as those in the hands) and large (including the knee and hip joints), which may be affected either simultaneously or asynchronously [1]. The treatment of OA remains challenging as understanding its classifications, risk factors, and pathophysiology continues evolving [3]. Symptoms such as pain, transient morning stiffness, and crepitus during joint movement—a grating sound or sensation—indicate a severe condition that can deteriorate quality of life (QOL) and lead to joint instability [4].
OA is treated with pharmacotherapy, physical therapy, rehabilitation therapy, acupuncture, and massage [5–7]. However, long-term use of pharmacotherapy has a risk of several negative consequences, such as hypertension, kidney damage, gastrointestinal problems, congestive heart failure, and heart attacks [8]. Moreover, surgery is not necessary for early-stage OA, and physical therapy is not appropriate for end-stage OA. Therefore, exploring a well-tolerated treatment modality is essential for OA patients.
According to traditional Chinese medicine’s (TCM) holistic theory, an organism can only remain vibrant and vigorous when there is harmony between its body and soul. With the integration of ancient Chinese philosophy, TCM has progressively developed into a unique method that blends movement and quiet, dredges meridians, controls qi and blood, and focuses on strengthening, feeding, and managing the body to avoid illnesses [9]. Among all the TCM modalities, acupuncture and moxibustion have demonstrated substantial efficacy with minimal adverse reactions [10]. Often used in conjunction with acupuncture to treat musculoskeletal issues, moxibustion is a TCM technique that increases blood circulation by burning wormwood at acupuncture sites [11, 12], and the evidence about acupuncture combined with moxibustion in treating OA was almost all reported in knee OA (KOA). Moreover, there are various acupuncture techniques for treating OA. However, systematic evidence comparing the efficacy of various acupuncture techniques combined with moxibustion in terms of recovery or pain reduction in the treatment of KOA is lacking.
Hence, this meta-analysis aims to compare the efficacy of acupuncture combined with moxibustion with other standard treatment modalities in enhancing recovery and reducing pain among KOA patients with randomized controlled trial (RCT) studies included.
Methods
Search strategy
This meta-analysis aligned with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Searches were performed on Ovid MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL) from the inception of each database until June 30, 2024. Reference lists from relevant articles were scrutinized to assess eligibility. The detailed search strategy employed for MEDLINE is documented in Appendix Material 1. Our study protocol was also registered on the PROSPERO website under the registration number CRD42024562008.
Selection criteria and data extraction
Inclusion criteria
RCTs focusing on OA affecting any peripheral or extremity joints, with no restrictions regarding the duration or severity of OA, included any acupuncture techniques combined with moxibustion, as were studies comparing these techniques to other interventions. Articles in all languages were considered.
Exclusion criteria
Studies were excluded if they involved animal or laboratory research, had unclear outcomes, or involved OA that did not affect the extremities (e.g., the neck or lumbar spine). Studies employing the small needle knife technique as the intervention were also excluded.
Working in pairs, two reviewers independently conducted titles and abstracts screening, full-text screening, data extraction, and risk of bias (RoB) assessment for included studies using a piloted electronic data extraction form (the Excel sheet). Reviewers resolved disagreement by discussion and, when necessary, consulting a third reviewer and clinical experts. Data extracted include the author’s name, year of publication, countries, study registry ID, patient characteristics (age, sex, location of OA, severity of condition, and length of disease, etc.), intervention information (type of acupuncture and moxibustion, length of treatment, and co-intervention, etc.), and efficacy and safety outcomes (measure name, type of data, timepoint of follow-up, and outcome values, etc.). The RoB of the included studies will be assessed using the Cochrane RoB 2.0 tool for RCTs [13]. The combination of acupuncture and moxibustion group was considered the experimental group for all the included studies. When a study had more than three arms, the patients in the group without any intervention were excluded from the meta-analysis.
Statistical analysis
Information regarding the characteristics of included studies, patients, and interventions was comprehensively summarized. For each direct comparison, the risk ratio (RR) and associated 95% CIs were calculated for dichotomous outcomes, while weighted mean differences (WMDs) and corresponding 95% CIs were determined for continuous outcomes. The random-effects model was used to conduct statistical analysis due to the high heterogeneity in our study.
Prior to pooling, scales for continuous outcomes were standardized. For instance, most studies employed the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) to assess treatment efficacy. The WOMAC subscales include pain (score range: 0–20), stiffness (0–8), and physical function (0–68). Conversely, some studies utilized a 0–100 scoring system for these subscales, which required mathematical conversion to WOMAC scales. A pairwise meta-analysis using a random-effects model was conducted. The certainty of the evidence was evaluated using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach. Sensitivity analyses were performed to evaluate the stability of the results by systematically excluding studies and observing any significant alterations in the outcomes, as well as a funnel plot to examine the possibility of publication bias.
Results
Study selection
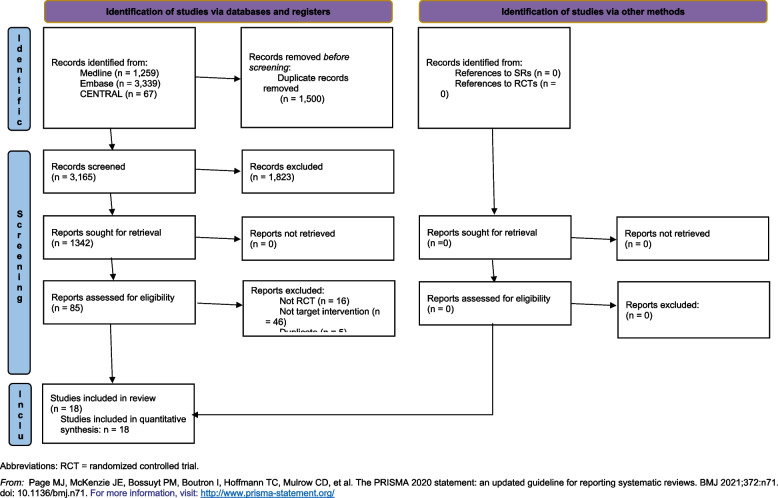
The PRISMA flowchart of study selection is presented in Fig. 1 [14]. In total, 4565 studies (Medline = 1259, Embase = 3339, and CENTRAL = 67) were identified. After the duplicate and abstract screening, 85 studies were included in the full-text screening. Eventually, 18 papers satisfied the inclusion criteria and were included in the meta-analysis [15–32].
Fig. 1.
PRISMA flowchart of literature selection
Study characteristics
All the RCT studies were conducted in China to evaluate the treatment efficacy for KOA. Among them, 18 studies were published, 2 in English, and 16 in Chinese. No studies were registered on National ClinicalTrials.gov.
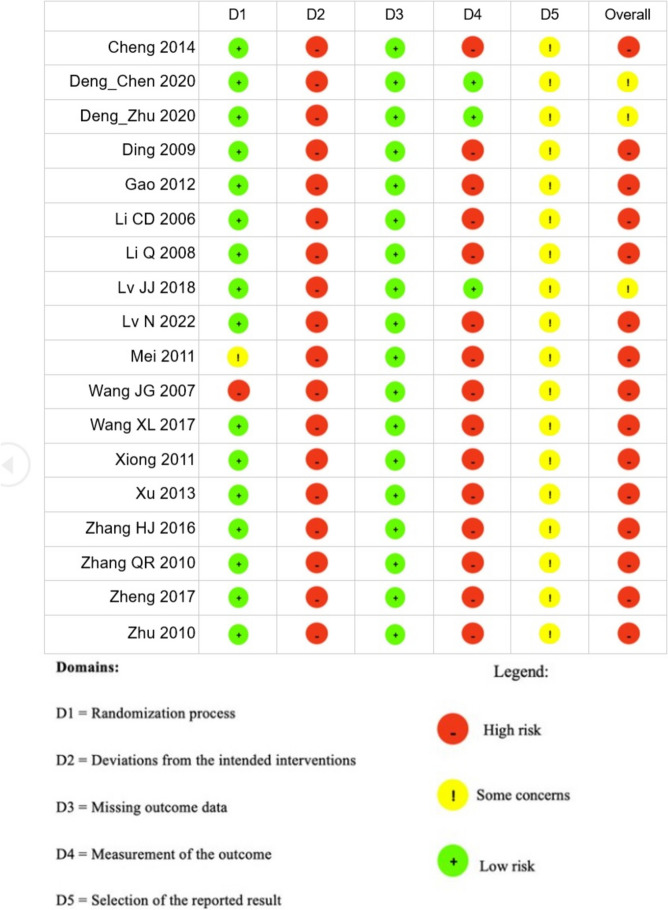
Among the 18 studies, 15 were identified as having a high risk of bias, and the other 3 were identified as having a medium risk of bias (Fig. 2). The summary of blinding in the included studies is summarized in Appendix Material 2.
Fig. 2.
Risk of bias based on Cochrane 2.0 tool for each study
In total, 736 patients were enrolled in the experimental group, and 696 patients were enrolled in the control group. The study characteristics for the included patients were presented in Table 1, and the intervention details for the enrolled patients were summarized in Appendix Material3.
Table 1.
The characteristics of included studies
| Study | N (intervention/ control) | Indication | Age, mean (SD), years | Sex (Male/Female) | Disease duration, mean (SD), months | Severity | Treatment duration | Follow-up |
|---|---|---|---|---|---|---|---|---|
| Cheng 2014 | 30/29 | KOA | 60.0 (5.0) | 28/31 | 50.5 (11.7) | NR | 44d (30d + two 1w rest in between 3 treatment cycles) | 1w |
| Deng_Chen 2020 | 35/37 for efficacy outcomes, 38/38 for safety outcome | KOA of cold-dampness type | 60.1 (7.7) | 30/42 (sex information was missing for 4 patients) | 58.8 (17.2) | Kellgren-Lawrence grade 0-III | 30d (28d + 2d of rest in between) | 1 m |
| Deng_Sheng 2020 | 35/33 for efficacy outcomes, 36/36 for safety outcome | KOA of cold-damp type | 52.9 (8.5) | 35/37 | 49.2 (17.4) | NR | 30d (28d + 2d of rest in between) | 4 m |
| Ding 2009 | 30/30 | KOA | 55.7 (14.6) | 17/43 | 56.2 (46.6) | VAS score of 7 cm or lower | 2w | 10w |
| Gao 2012 | 35/34 | KOA of kidney deficiency and marrow insufficiency pattern/syndrome | 58.2 (8.8) | 28/41 | 38.1 (11.4) | NR | 4w, 8w | NA |
| Li CD 2006 | 56/54 | KOA of kidney-yang deficiency and cold syndrome | 59.4 (5.2) | 65/55 | NR | VAS pain score 4 or greater, Lequesne Index of 6 or higher | 7d, 15d (14d + 1d of rest in between 2 cycles) | NA |
| Li Q 2008 | 30/30 (54/50 knees) | KOA of Yang-deficiency pattern | 64.1 (5.6) | 16/44 | 105.6 (86.4) | Kellgren-Lawrence grade II-IV | 10d | 1 m |
| Lü JJ 2018 | 30/28 | KOA of Yang-deficiency pattern | 53.0 (8.5) | 33/25 | 18.9 (5.0) | NR | 22d (20d + 2d of rest in between) | 1 m |
| Lü N 2022 | 48/48 | KOA | 63.9 (11.0) | 40/56 | 79.2 (21.8) | Kellgren-Lawrence grade I-III | 4w | NA |
| Mei 2011 | 68/69 | KOA | 60.9 (6.9) | 48/89 | 20.5 (5.3) | NR | 42d (20*2 + 2; once every other day 10 times, over 2 courses of treatment with a 2-day interval between courses) | 2w |
| Wang JG 2007 | 40/40 | KOA | 59.4 (5.3) | 37/43 | Value NR, shorter than 120 months as one of the inclusion criteria | NR | 20d, 43d (40d + 3d of rest in between of 2 cycles) | NA |
| Wang XL 2017 | 25/21 | KOA | 59.6 (6.6) | 10/36 | range, 24 to 360 months | Kellgren-Lawrence grade II or greater, and VAS score of 3 cm or greater | 3w | NA |
| Xiong 2011 | 30/30 | KOA | 55.3 (8.6) | 13/47 | 0.9 (0.4) | NR | 20d | NA |
| Xu 2013 | 80/80 | KOA | 58.0 (13.8) | 82/78 | 56.5 (44.6) | Kellgren-Lawrence grade I-III, and VAS score of 70 mm or lower | 5w | 3 m, 6 m |
| Zhang HJ 2016 | 40/10 | KOA with cold-damp stagnation | 50.5 (10.5) | 47/33 | 27.6 (15.8) | NR | 20d | 6 m but only for recurrence rate |
| Zhang QR 2010 | 32/30 | KOA | 59.7 (6.9) | 31/31 | 54.0 (42.7) | NR | 22d (20d + 2d of rest in between) | NA |
| Zheng 2017 | 30/30 | KOA with yang-deficiency and cold-stagnation syndrome | 53.0 (10.5) | 31/29 | 14.3 (5.7) | NR | 22d (20d + 2d of rest in between) | NA |
| Zhu 2010 | 62/62 | KOA of cold-damp type | 53.4 (2.8) | 48/76 | 66.0 (45.5) | NR | 4w | 10w |
SD standard deviation, EA electroacupuncture, KOA knee osteoarthritis, NA not applicable, NR not reported,
OA osteoarthritis, d day, m month, w week
Treatment efficacy
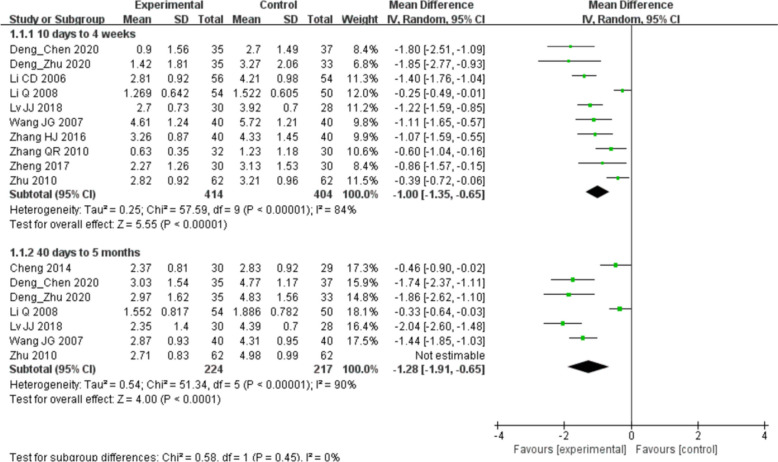
Regarding pain scores evaluated by visual analog scales (VAS), ten studies reported short-term (< 4 w) outcomes; the pooled WMD was − 1.00 (95% CI: − 1.35 to − 0.65; I2 = 84.0%, p 0.00001). Seven studies reported middle-term (6–60w) outcomes; the pooled SMD was − 1.28 (95% CI: 1.91 to − 0.65; I2 = 90.0%, p = 0.0001) (Fig. 3). These results indicated that the patients undergoing acupuncture combined with moxibustion treatment significantly reduced the VAS pain score compared to patients undergoing other treatments.
Fig. 3.
Forest plot showing the difference in visual analog scale pain scores between moxibustion combined with acupuncture and other treatments for osteoarthritis knee
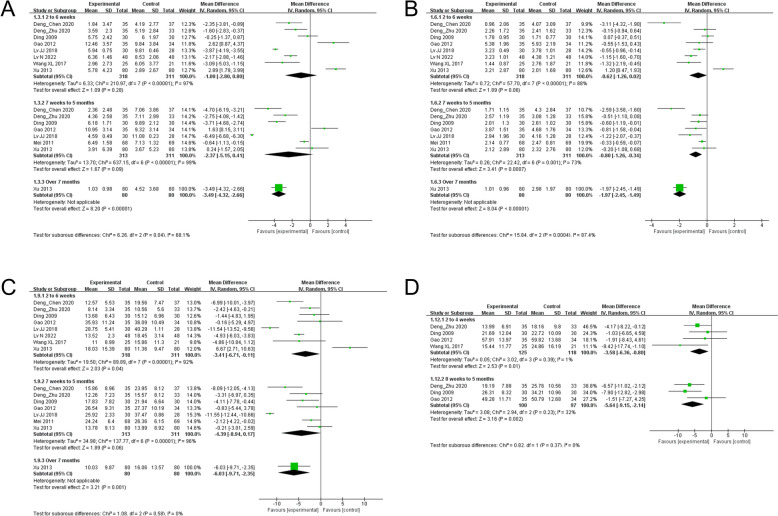
Regarding WOMAC, eight studies reported short-term treatment (2–6w) outcomes, seven studies reported middle-term (7w–5 months) treatment outcomes, and one study reported long-term (> 7 months) treatment outcomes. For pain score, the WMD was − 1.00 (95% CI: − 2.80 to 0.8; I2 = 97.0%, p = 0.28) for short-term outcomes, the WMD was −2.37 (95% CI: −5.15 to 0.41; I2 = 99.0%, p = 0.09) for middle-term treatment outcomes, and the WMD was − 3.49 (95% CI: − 4.32 to − 2.66; p = 0.0001) for long-term treatment outcomes (Fig. 4A).
Fig. 4.
Forest plot showing the difference in Western Ontario McMasters University Osteoarthritis Index between moxibustion combined with acupuncture and other treatments for osteoarthritis knee. A pain; B stiffness; C physical function; D total score
For stiffness, the WMD was − 0.62 (95% CI: − 1.26 to 0.02; I2 = 88.0%, p = 0.06) for short-term outcomes, the WMD was − 0.08 (95% CI: − 1.26 to − 0.34; I2 = 73.0%, p = 0.0007) for middle-term treatment outcomes, and the WMD was − 1.97 (95% CI: − 2.45 to − 1.49; p = 0.0001) for long-term treatment outcomes (Fig. 4B).
For physical function, the WMD was − 3.41 (95% CI: − 6.71 to − 0.11; I2 = 92.0%, p = 0.04) for short-term outcomes, − 4.39 (95% CI: − 8.94 to 0.17; I2 = 93.0%, p = 0.06) for middle-term treatment outcomes, and − 6.03 (95% CI: − 9.71 to − 2.35; p = 0.001) for long-term treatment outcomes (Fig. 4C). Moreover, four studies reported short-term (2–4w) changes in WOMAC total scores; the WMD was − 3.58 (95% CI: − 6.36 to − 0.80; I2 = 1.0%, p = 0.01). Three studies reported middle-term (2–4w) change in WOMAC total scores; the WMD was − 5.64 (95% CI: − 9.15 to − 2.14; I2 = 32.0%, p = 0.002) (Fig. 4D). These results indicated the heterogeneity advantages of acupuncture combined with moxibustion over other treatments in improving WOMAC.
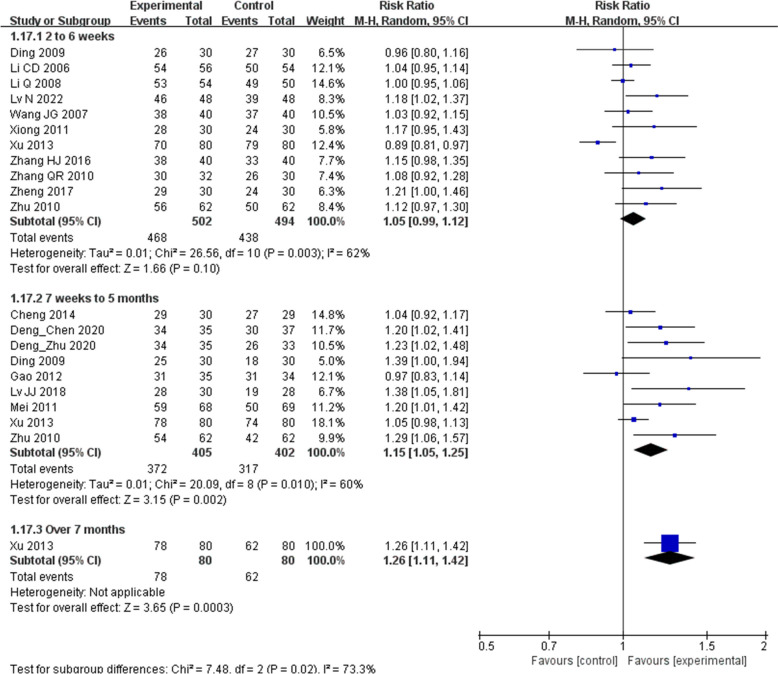
Finally, the overall efficacy rate was analyzed. Eleven studies reported short-term treatment (2–6w) outcomes; the RR was 1.05 (95% CI: 0.99 to 1.12; I2 = 62.0%, p = 0.10). In 9 studies of middle-term treatment (7w–5 m) outcomes, the RR was 1.15 (95% CI: 1.05 to 1.25; I2 = 62.0%, p = 0.002). One study reported long-term (> 7 months) treatment outcome; the RR was 1.26 (95% CI: 1.11 to 1.42, p = 0.0003) (Fig. 5). These results indicated that the advantages of acupuncture combined with moxibustion over other treatments were evident in middle and long-term periods.
Fig. 5.
Forest plot showing the difference in the overall efficacy rate between moxibustion combined with acupuncture and other treatments for osteoarthritis knee
Treatment-related adverse events
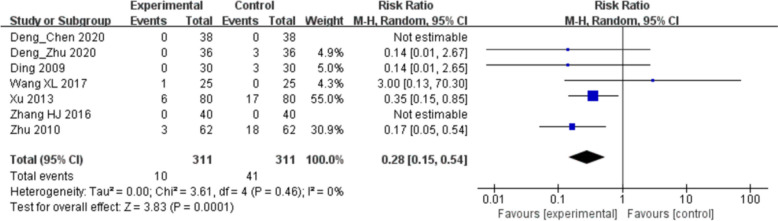
Seven studies reported treatment-related AEs. In total, thirteen adverse events were reported in the acupuncture combined with the moxibustion group. Among them, ten cases developed redness and pain in the local skin, two cases developed faintness, and one developed scald during treatments. All the AEs were mild and resolved with proper treatments. No severe AEs were reported in any studies. Meanwhile, 38 AEs were reported in other treatment groups. The RR was 0.28 (95% CI: 0.15 to 0.54; I2 = 0%, p = 0.001). The result indicated that acupuncture combined with moxibustion was safer than other treatments (Fig. 6).
Fig. 6.
Forest plot showing the difference in adverse events between moxibustion combined with acupuncture and other treatments for osteoarthritis knee
Sensitivity analyses
Sensitivity analyses covered all evaluated outcomes except the WOMAC total scores and adverse events, as detailed in Supplementary Tables 1–4. The analysis revealed no single study that markedly affected the direction or magnitude of the outcomes. The I2 statistic for these outcomes consistently remained above 50%, indicating a moderate to high level of heterogeneity.
Publication bias
We used a funnel plot to examine the possibility of publication bias. The short-term and middle-term VAS score (Supplementary Fig. 1), WOMAC pain score (Supplementary Fig. 2), WOMAC stiffness (Supplementary Fig. 3), and physical function (Supplementary Fig. 4). The overall efficacy rate (Supplementary Fig. 5) had no publication bias.
Discussion
Two of the most widely utilized TCM modalities in China are moxibustion and acupuncture [32, 33]. They are commonly applied in clinical settings, with an expanding evidence base, including case reports, longitudinal studies, and randomized controlled trials, supporting their use in OA treatment. However, evidence was previously insufficient for the efficacy of combining moxibustion with acupuncture in managing KOA. Our meta-analysis is the first to demonstrate that the combination of moxibustion and acupuncture is superior to other treatments (acupuncture alone, moxibustion alone, or pharmaceuticals), particularly showing more pronounced benefits during middle-term and long-term follow-ups.
Moxibustion enhances blood circulation at the knee joint, reduces cartilage degradation, and decreases macrophage infiltration. It also inhibits the production of inflammatory mediators such as interleukin-6, mast cell cyclooxygenase, and tumor necrosis factor, contributing to the restoration of articular chondrocytes [34, 35]. Additionally, moxibustion has been shown to regulate insulin-like and transforming growth factors, strengthening the knee joint’s limb pedal strength [36]. The efficacy of various moxibustion techniques has been explored, with fire needle moxibustion potentially showing the most remarkable efficacy [37]. Future research is needed to ascertain the most effective moxibustion technique.
Acupuncture, another fundamental component of TCM, operates on the principle of enhancing qi flow through specific acupoints and meridians. Selecting acupoints is critical for effective treatment [38, 39]. In KOA model rabbits, acupuncture has been shown to decrease the anaerobic glycolytic metabolism rate and levels of metabolites, potentially protecting the cartilage [40]. It may also alleviate cartilage hypoxia and improve oxygen levels through enhanced synovial microcirculation and fluid PO2. Furthermore, He et al. [41] revealed significant upregulation of miR-214 and its targets, TRPV4 and BAX, in damaged articular cartilage following acupuncture, suggesting a therapeutic mechanism for KOA recovery. Research into various acupuncture modalities is encouraged to further understand their specific effects on KOA [42].
Although the individual benefits of moxibustion and acupuncture are well-documented, comprehensive reviews comparing these combined therapies to other treatments are scarce. Qu et al.’s meta-analysis, which included 10 RCTs, found that combining acupotomy, acupuncture, and moxibustion offers superior therapeutic benefits for KOA, reducing postoperative pain and enhancing clinical efficacy [43]. Similarly, Park et al. reported significant pain reduction in KOA patients treated with single or integrated oriental medicine modalities (acupuncture, herbal medicine, pharmaco-acupuncture, and moxibustion) [44]. These findings align with our results, suggesting that combined TCM modalities may offer enhanced treatment efficacy.
However, significant heterogeneities were identified in most results. The reason was complicated. First, the disease condition of KOA was challenging to balance among all the studies. Different doctors judged the severity of KOA, and the standard may be inconsistent among different studies. Second, the improvements in KOA after treatments were measured using subjective evaluation tools. Potential biases may exist among different studies. Third, the follow-up period was varied. The short-term, middle-term, and long-term results were analyzed from different studies. Therefore, the interpretations of the results in our study should be cautious due to the high heterogeneity.
In our study, using different evaluation tools resulted in different outcomes. It suggested that the assessment tool selected may impact how well moxibustion and acupuncture are considered to work together. While WOMAC did not reveal a significant difference in short-term or middle-term outcomes, other evaluation tools identified better treatment outcomes with the combination approach. A plausible rationale for these disparities might be the variation of pain measures. It is also essential to consider the pain score as a proportion of the overall score. For instance, the VAS offers a more comprehensive evaluation of pain, whereas the WOMAC scale emphasizes on physical functions more. The difference in measurement tools could explain some of the heterogeneity in our study.
Moreover, the results of the GRADE analysis, which revealed highly low-quality evidence, underscore the necessity for more rigorous and standardized research in this field. The significant risk of bias and inconsistency among studies cannot be overlooked despite including RCTs, which are considered the gold standard for evaluating therapy efficacy. The variability in treatment modalities in the control groups, the differing durations of therapy, and the diverse techniques of moxibustion combined with acupuncture contribute to an elevated risk of publication bias. Future research should focus on designing RCTs with robust methodologies to minimize bias and ensure consistency across studies. Additionally, establishing standardized treatment guidelines in this field and using advanced techniques, such as artificial intelligence systems [45], to help select the preferred treatment modality for KOA are essential.
The strength of this meta-analysis lies in its aggregation of a significant number of RCTs, each with considerable sample sizes (18 studies involving over 1400 participants). However, our review has notable limitations. Firstly, the quality of most included studies was low. Significant publication bias and heterogeneity among the studies were observed, which could influence the interpretation of results. Secondly, implementing blinding methods was challenging, and subjective assessments might have increased the risk of bias, potentially leading to overestimating the efficacy of combined therapy. Thirdly, the follow-up periods were generally short, making it difficult to assess long-term treatment efficacy. Future studies should aim to conduct well-designed, blinded trials with extended follow-up periods to more accurately determine the outcomes of our findings.
Conclusion
A meta-analysis of RCT studies found that combining acupuncture and moxibustion treatment was significantly more effective and safer than other treatments. The benefits were particularly pronounced during the middle-term and long-term follow-up periods.
Supplementary Information
Supplementary Material 1. Appendix 1. The detailed search strategy.
Supplementary Material 2. Appendix 2. Summary of Blinding in the Included Studies
Supplementary Material 3. Appendix 3. Intervention details for the experimental and control groups.
Supplementary Material 4. Figure S1. Funnel plot for visual analog scale pain outcome.
Supplementary Material 5. Figure S2. Funnel plot for Western Ontario McMasters University Osteoarthritis Index pain outcome.
Supplementary Material 6. Figure S3. Funnel plot for Western Ontario McMasters University Osteoarthritis Index stiffness outcome.
Supplementary Material 7. Figure S4. Funnel plot for Western Ontario McMasters University Osteoarthritis Index physical function outcome.
Supplementary Material 8. Figure S5. Funnel plot for overall efficacy rate outcome.
Acknowledgements
We thank Medjaden Inc. for the scientific editing of this manuscript.
Abbreviations
- OA
Osteoarthritis
- QOL
Quality of life
- TCM
Traditional Chinese medicine
- KOA
Knee osteoarthritis
- RCT
Randomized controlled trial
- RR
Risk ratio
- WMDs
Weighted mean differences
- WOMAC
Western Ontario and McMaster Universities Osteoarthritis Index
- GRADE
Grading of Recommendations, Assessment, Development, and Evaluation
Authors’ contributions
Conceptualization: Xing Li, Wei Zhai, Cheng Chen, Mi Liu, Ge-Shu Du. Data curation: Zhao-Bo Yan, Cheng Chen, Wei Zhai. Formal analysis: Rui-Xin Zhu, Xing Li. Funding acquisition: Xing Li, Wei Zhai, Cheng Chen, Mi Liu, Ge-Shu Du. Investigation: Heng-Cai Zhang, Wen-Juan Ma, Kun-Fu Wang. Methodology: Zhao-Bo Yan, Cheng Chen, Wei Zhai, Heng-Cai Zhang, Wen-Juan Ma, Fu-Kun Wang. Project administration: Mi Liu, Ge-Shu Du. Resources: Heng-Cai Zhang, Wen-Juan Ma, Fu-Kun Wang. Software: Zhao-Bo Yan, Heng-Cai Zhang, Wen-Juan Ma, Fu-Kun Wang. Supervision: Mi Liu, Ge-Shu Du. Validation: Mi Liu, Ge-Shu Du. Visualization: Mi Liu, Ge-Shu Du. Writing - original draft: Rui-Xin Zhu, Xing Li. Writing - review & editing: Mi Liu, Ge-Shu Du
Funding
The following funding sources funded this study:
(1) Natural Science Foundation of Changsha City, grant number: Kq 2,208,492, Ge-Shu Du.
(2) Natural Science Foundation of Changsha City, grant number: Kq 2,208,489, Xing Li.
(3) Scientific Research Foundation of Administration of Traditional Chinese Medicine of Hunan Province, grant number: A2024048, Xing Li.
(4) Scientific Research Foundation of Administration of Traditional Chinese Medicine of Hunan Province, grant number: B2023113, Ge-Shu Du.
(5) Scientific Research Foundation of Administration of Traditional Chinese Medicine of Hunan Province, grant number: B2024129, Wei Zhai.
(6) Scientific Research Foundation of Administration of Traditional Chinese Medicine of Hunan Province, grant number: B2024130, Cheng Chen.
(7) Natural Science Foundation of Hunan Province, grant number: 2023JJ6075, Ge-Shu Du.
(8) The Science and Technology Innovation Program of Hunan Province, grant number: 2024JK2132, Mi Liu.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article. Further inquiries can be directed to the corresponding author.
Declarations
Ethics approval and consent to participate
Institutional Review Board approval was not required because this is a meta-analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mi Liu, Email: newmean@hnucm.edu.cn.
Ge-Shu Du, Email: dgsmmcc@163.com.
References
- 1.Martel-Pelletier J, Barr AJ, Cicuttini FM, Conaghan PG, Cooper C, Goldring MB, et al. Osteoarthritis Nat Rev Dis Primers. 2016;2:16072. [DOI] [PubMed] [Google Scholar]
- 2.Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646–56. [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang Y. Osteoarthritis year in review 2021: biology. Osteoarthritis Cartilage. 2022;30:207–15. [DOI] [PubMed] [Google Scholar]
- 4.Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, Weinans H, et al. Osteoarthritis Lancet. 2015;386:376–87. [DOI] [PubMed] [Google Scholar]
- 5.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, et al. Knee replacement. Lancet. 2012;379:1331–40. [DOI] [PubMed] [Google Scholar]
- 6.Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012;380:1768–77. [DOI] [PubMed] [Google Scholar]
- 7.Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377:2115–26. [DOI] [PubMed] [Google Scholar]
- 8.Singh JA. Making the current non-surgical treatments for knee osteoarthritis more effective: Solutions from a diverse patient group. Joint Bone Spine. 2023;90: 105535. [DOI] [PubMed] [Google Scholar]
- 9.Tao T, Shi MP, Tan BY, Zhang XS, Sun FL, Liu BR, et al. Evaluation of traditional Chinese exercise for knee osteoarthritis (KOA): an overview of systematic reviews. Syst Rev. 2024;13:187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang M, Jiang L, Wang Q, Chen H, Xu G. Traditional Chinese medicine for knee osteoarthritis: an overview of systematic review. PLoS ONE. 2017;12: e0189884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deng H, Shen X. The mechanism of moxibustion: ancient theory and modern research. Evid Based Complement Alternat Med. 2013;2013: 379291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim MY, Huang J, Zhao B, Ha L. Current status of acupuncture and moxibustion in China. Chin Med. 2015;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng G, Cheng W. Jiang YG [Controlled observation of clinical efficacy on knee osteoarthritis treated with auricular electroacupuncture and the isolated moxibustion with Lingxian herbal paste]. Zhongguo Zhen Jiu. 2014;34:230–4. [PubMed] [Google Scholar]
- 16.Deng KF, Chen RL, Zhu SW, Wei XC, Zhang LJ, Zhu Y. Electroacupuncture combined with thunder-fire moxibustion in the treatment of cold-dampness knee osteoarthritis: a randomized controlled clinical trial. Chinese Journal of Tissue Engineering Research. 2020;24:4638. [DOI] [PubMed] [Google Scholar]
- 17.Deng KF, Sheng FF, Wei XC, Jiang Y, Zhu Y, Liao ZL, et al. Electroacupuncture combined with thunder-fire moxibustion for knee osteoarthritis of cold-damp type: a randomized controlled trial. World Journal of Acupuncture-Moxibustion. 2020;30:33–8. [Google Scholar]
- 18.Ding MH, Zhang H, Li Y. A randomized controlled study on warming needle moxibustion for treatment of knee osteoarthritis. Zhongguo Zhen Jiu. 2009;29:603–7. [PubMed] [Google Scholar]
- 19.Gao J, Ouyang BS, Zhang Y, Li J, Yang HZ, Ji LL, et al. Comparison of the clinical therapeutic effects between electroacupuncture and warming needle moxibustion for knee osteoarthritis of kidney deficiency and marrow insufficiency pattern/syndrome. Zhongguo Zhen Jiu. 2012;32:395–8. [PubMed] [Google Scholar]
- 20.Li CD, Huang XY, Yang XG, Wang QF, Huang SQ. Observation on therapeutic effect of warming needle moxibustion on knee osteoarthritis of deficiency-cold type. Zhongguo Zhen Jiu. 2006;26:189–91. [PubMed] [Google Scholar]
- 21.Li Q. [Observation on therapeutic effect of moxibustion at Shenque (CV 8) combined with electroacupuncture on gonarthritis of type of accumulation of pathogenic cold due to yang deficiency]. Zhu J Zhongguo Zhen Jiu. 2008;28:565–8. [PubMed] [Google Scholar]
- 22.Lü JJ, Yang XC, Ji TT, Xue MX. Randomized controlled clinical trials of treatment of knee osteoarthritis of yang-deficiency pattern by acupuncture plus moxibustion. Zhen Ci Yan Jiu. 2018;43:661–5. [DOI] [PubMed] [Google Scholar]
- 23.Lü N, Cheng P, Xia JX. Yuan YP [Effect of acupuncture combined with moxibustion on serum matrix metalloproteinase-9 and matrix metalloproteinase inhibitor-1 in patients with knee osteoarthritis]. Zhen Ci Yan Jiu. 2022;47:262–7. [DOI] [PubMed] [Google Scholar]
- 24.Mei ZG, Cheng CG, Zheng JF. Observations on curative effect of high-frequency electric sparkle and point-injection therapy on knee osteoarthritis. J Tradit Chin Med. 2011;31:311–5. [DOI] [PubMed] [Google Scholar]
- 25.Wang JG. He LJ [Observation on the therapeutic effect of warming needle moxibustion on knee osteoarthritis]. Zhongguo Zhen Jiu. 2007;27:191–2. [PubMed] [Google Scholar]
- 26.Wang X, Wang X, Hou M, Wang H, Ji F. [Warm-needling moxibustion for knee osteoarthritis:a randomized controlled trial]. Zhongguo Zhen Jiu. 2017;37:457–62. [DOI] [PubMed]
- 27.Xiong GP, Huang Q. Dong YF [Thirty cases of knee osteoarthritis treated by acupuncture and warming needle moxibustion]. Zhongguo Zhen Jiu. 2011;31:551–2. [PubMed] [Google Scholar]
- 28.Xu L, Jing L, He K, Wang JL. Wang Y [Treatment of knee osteoarthritis with acupuncture and moxibustion: a randomized controlled trial]. Zhongguo Zhen Jiu. 2013;33:871–6. [PubMed] [Google Scholar]
- 29.Zhang H, Xu H, Liu T, Li P. [Clinical study of the electroacupuncture combined with thunder-fire moxibustion in treatment of degenerative knee osteoarthritis with cold-damp stagnation]. Zhongguo Zhen Jiu. 2016;36:1266–70. [DOI] [PubMed]
- 30.Zhang QR. Fu WB [Osteoarthritis of knee joint treated with acupuncture and moxibustion]. Zhongguo Zhen Jiu. 2010;30:375–8. [PubMed] [Google Scholar]
- 31.Zheng J, Zhang H. [Different acupuncture and moxibustion methods at Heding (EX-LE 2) for knee osteoarthritis with yang-deficiency and cold-stagnation syndrome]. Liu J Zhongguo Zhen Jiu. 2017;37:594–8. [DOI] [PubMed] [Google Scholar]
- 32.Zhu Y, Chen RL, Miao FR, Ji L. [Clinical observation on the therapeutic effect of drugs-paste separated moxibustion combined with electroacupunture for knee osteoarthritis patients of cold-damp type]. Zhen Ci Yan Jiu. 2010;35:293–7. [PubMed]
- 33.Xu J, Yang Y. Traditional Chinese medicine in the Chinese health care system. Health Policy. 2009;90:133–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu L, Wang L, Wei J, Ryszard G, Shen X, Wolfgang S. Heat induces adenosine triphosphate release from mast cells in vitro: a putative mechanism for moxibustion. J Tradit Chin Med. 2015;35:323–8. [DOI] [PubMed] [Google Scholar]
- 35.Liu D, Wu YL, Li C, Wang ML, Ma XX, Liu JW, et al. Warming moxibustion attenuates inflammation and cartilage degradation in experimental rabbit knee osteoarthriti. J Tradit Chin Med. 2021;41:959–67. [DOI] [PubMed] [Google Scholar]
- 36.Lin JG, Lin SZ, Lin LH, Wu CC, Tsai WT, Harn HJ, et al. Effects of Moxibustion on the Levels of Insulin-Like Growth Factor 1: A Pilot Study. Cell Transplant. 2018;27:551–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xin S, Liu J, Yang Z, Li C. Comparative effectiveness of moxibustion and acupuncture for the management of osteoarthritis knee: a systematic review and meta-analysis. Heliyon. 2023;9: e17805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cao BQ, Tan F, Zhan J, Lai PH. Mechanism underlying treatment of ischemic stroke using acupuncture: transmission and regulation. Neural Regen Res. 2021;16:944–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ha L, Yu M, Yan Z, Rui Z, Zhao B. Effects of moxibustion and moxa smoke on behavior changes and energy metabolism in APP/PS1 mice. Evid Based Complement Alternat Med. 2019;2019:9419567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiwei M, Mei D, Juan L, Longfei X, Xilin C, Tingyao H, et al. Electroacupuncture improves articular microcirculation and attenuates cartilage hypoxia in a male rabbit model of knee osteoarthritis. J Tradit Complement Med. 2024;14:414–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.He J, Zuo J, Fan X, Li Z. Electro-acupuncture modulated miR-214 expression to prevent chondrocyte apoptosis and reduce pain by targeting BAX and TRPV4 in osteoarthritis rats. Braz J Med Biol Res. 2024;57: e13238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chang Y, Wu N, Zhang Z, Zhang Z, Ren B, Liu F, et al. Efficacy of manual acupuncture, electro-acupuncture, and warm acupuncture for knee osteoarthritis: study protocol for a randomized controlled trial. Trials. 2022;23:700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Qu B, Wu X, Liu H, Cai W, Wang G, Song H, et al. Meta-analysis and systematic review of acupotomy combined with puncture and moxibustion in the treatment of knee osteoarthritis. Ann Palliat Med. 2021;10:6637–49. [DOI] [PubMed] [Google Scholar]
- 44.Park YC, Park KJ, Goo BH, Kim JH, Seo BK, Baek YH. Oriental medicine as collaborating treatments with conventional treatments for knee osteoarthritis: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2023;102: e34212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Omotunde H, Mouhamed MR. The modern impact of artificial intelligence systems in healthcare: a concise analysis. mesopotamian journal of artificial intelligence in healthcare. 2023;2023:66–70.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1. Appendix 1. The detailed search strategy.
Supplementary Material 2. Appendix 2. Summary of Blinding in the Included Studies
Supplementary Material 3. Appendix 3. Intervention details for the experimental and control groups.
Supplementary Material 4. Figure S1. Funnel plot for visual analog scale pain outcome.
Supplementary Material 5. Figure S2. Funnel plot for Western Ontario McMasters University Osteoarthritis Index pain outcome.
Supplementary Material 6. Figure S3. Funnel plot for Western Ontario McMasters University Osteoarthritis Index stiffness outcome.
Supplementary Material 7. Figure S4. Funnel plot for Western Ontario McMasters University Osteoarthritis Index physical function outcome.
Supplementary Material 8. Figure S5. Funnel plot for overall efficacy rate outcome.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article. Further inquiries can be directed to the corresponding author.