ABSTRACT
Hepatitis B (Hep B) remains a critical public health issue globally, particularly in Tibet, where vaccination rates and influencing factors among college students are yet understudied. This study applies a cross-sectional design to investigate the Hep B vaccination rate among 1,126 college students in Tibet and utilizes the expanded theory of planned behavior (ETPB) to identify vaccination behavior intention (BI) and vaccination behavior (VB). Stratified cluster sampling across three universities was used to assess behavioral attitudes (BA), subjective norms (SN), perceived behavioral control (PBC), past vaccination history (PVH) and vaccination knowledge (VK), and used structural equation modeling (SEM) for model validation and multi-group comparison. Results indicated that 16.3% of students had received the Hep B vaccine. VK notably improved BA toward vaccination (β = 0.518, p < .001). BA (β = 0.232, p < .001), PBC (β = 0.239, p < .001), SN (β = 0.385, p < .001) positively influenced BI. However, PVH failed to predict BI. BI (β = 0.448, p < .001) and PVH (β = 0.127, p < .001) were significant predictors of VB. Significant ethnic variations were noted. The positive effect of PVH on VB (β = 0.151, p < .001) and the mediating role of PBC in VB (β = 0.076, p < .05) were significant among Tibetan students. The effect of VK on BA was stronger among Tibetans (β = 0.503, p < .05),while the impact of attitude on BI was more pronounced among Han students (β = 0.366, p < .05). The vaccination rate for Hep B among college students in Tibet is relatively low, and the ETPB model effectively explains their vaccination intentions and behaviors. Tailored intervention strategies for Tibetan and Han students are recommended to boost vaccination rates effectively.
KEYWORDS: Expanded theory of planned behavior (ETPB), Tibetan college students, hepatitis B vaccination, structural equation modeling (SEM), vaccination behavior determinants
Introduction
Hepatitis B (Hep B), caused by the hepatitis B virus (HBV), is a major global health issue, with 1.2 million new infections and 1.1 million deaths reported in 2022.1–3 The World Health Organization (WHO) aims to eliminate the public health risks associated with viral hepatitis by 2030, recognizing vaccination as a cost-effective prevention strategy.4 In China, the introduction of the Hep B vaccine into the National Immunization Program(NIP)for children has reduced HBsAg prevalence from high to moderate. Despite this progress, high HBsAg prevalence in adults and ongoing mother-to-child transmission challenges remain significant5,6 Furthermore, the overall coverage of hepatitis B vaccination in adults remains low.7 Tibet, the westernmost part of China, faces particularly severe economic and medical challenges, with higher rates of Hep B incidence and mortality compared to the national average and a high prevalence of non-immuno-protected adults at 43.8%.8,9
Given the immunological efficacy and cost-effectiveness of Hep B vaccination, existing research suggests promoting hepatitis B vaccination among young adults aged 20–39.10,11 Since many college students fall within this age range, increasing their vaccination rate is essential to achieving greater cost-effectiveness. However, surveys conducted in the Xizang Autonomous Region in 2014 and 2020 revealed a full-course National Immunization Program (NIP) Hep B vaccination rate of 52.8% among university students, with an antibody positivity rate of only 37.7%.8,9 Both figures are well below the other provinces,12–14 highlighting that a significant portion of university students in Tibet missed the Hep B vaccination(NIP), creating a considerable immunity gap in this population. This low vaccination rate increases transmission risk, and insufficient antibody levels among female students pose additional challenges for preventing mother-to-child transmission. Understanding the adult Hep B vaccination rate in this population and implementing targeted strategies to improve their uptake is a valuable and impactful effort. Despite the importance of improving vaccination rates, there is a lack of comprehensive research in this field.15
The theory of planned behavior (TPB), proposed by Ajzen, provides a framework for understanding health behaviors through behavioral attitude (BA), subjective norms (SN), and perceived behavioral control (PBC).16 These factors influence behavioral intention (BI) as well as actual behavior.17 The TPB model has been widely adopted across various disciplines,18–20 and has been successfully applied to predict vaccination intentions for various diseases, including COVID-19, influenza, and pertussis.21–23
BA refers to an individual’s positive or negative evaluation of a specific behavior.16 Empirical studies further highlight its role as a strong predictor of vaccination intentions for vaccines like COVID-19 and influenza.24,25 These previous studies indicated that positive attitudes toward vaccines significantly increase the likelihood of vaccination, underscoring the critical role of behavioral attitude in shaping vaccination intentions and behaviors.
SN reflect an individual’s perception of others’ attitudes toward their behavior.16 Empirical research consistently shows their influence on vaccine uptake, including HPV and hepatitis B vaccines. For example, research indicates that recommendations from healthcare professionals can increase individuals’ motivation and intent to receive the hepatitis B vaccine,26,27 and Yang et al. found that subjective norms significantly impact influenza vaccine hesitancy.24 Thus, subjective norms are a crucial factor in shaping vaccination intentions and behaviors.
PBC refers to an individual’s confidence in their ability to successfully perform a specific behavior.17 In Yang et al.‘s study on influenza, perceived behavioral control was shown to contribute to explaining vaccine hesitancy.24 Similarly, Guidry et al. identified perceived behavioral control as one of the predictive factors for the intention to receive the COVID-19 vaccine.28
However, there is limited research on applying the TPB to Hep B vaccination intention and behavior among adults. Accordingly, we aimed to address the gap in the literature by utilizing the TPB model to explore the factors influencing Hep B vaccination intention and behavior among adults.
The flexibility of TPB allows for enhancements by incorporating additional variables to better predict specific behaviors.16 Ajzen and Conner suggested that past behaviors could significantly influence future behavioral intention.29,30 Prior influenza vaccination increases the likelihood of receiving a COVID-19 vaccine,25 and individuals with previous preventive strategies are more inclined to continue such behavior.31 These facts raise the question of whether prior vaccinations that are non- NIP vaccine can predict Hep B vaccination intention and behavior.
Knowledge, typically viewed as a foundational factor influencing attitude and behavior,32 plays a crucial role in vaccination intention. Knowledge about the benefits of COVID-19 vaccination directly correlates with a positive attitude and indirectly influences vaccination intention.25 A recent review highlighted that a lack of awareness about the benefits of Hep B vaccination contributes to high hesitancy rates.33 A French study found that perceptions of vaccine benefits and effectiveness influence the acceptance of vaccines like varicella and HPV. Recognizing the benefits of a vaccine increases the likelihood of its acceptance.34 Thus, this study integrates past vaccination history (PVH) and vaccination knowledge (VK) into the TPB model to assess their impact.
Additionally, previous research has underscored the role of racial and cultural factors in shaping vaccination intention and hesitancy.35–37 In China, ethnic minorities’ religious beliefs and traditional cultures have been linked to vaccine hesitancy.38 To address this matter, we conducted a multi-group analysis to compare decision-making processes regarding Hep B vaccination among Tibetan and Han students for following reasons. Research has highlighted the unique challenges faced by ethnic minorities in accessing and understanding vaccine information due to socio-economic, cultural, and geographic factors, which can negatively influence vaccination attitudes and rates.39,40 Lower education levels and limited trust in media sources make healthcare professionals the primary sources of vaccine information for these populations,41 suggesting that subjective norms may have different effects on ethnic minorities compared to the Han population. Additionally, lower health literacy, often linked to reduced self-efficacy, is more prevalent among ethnic minorities, potentially impacting perceived behavioral control and vaccination behavior.42 While ethnicity’s role in vaccination behavior has been acknowledged, few studies have systematically examined its differential impacts across model pathways.
In summary, the overall objective of this study is to investigate the status of adult hepatitis B vaccination among students in Tibetan universities who have not received the NIP Hep B vaccine. Employing the expanded theory of planned behavior (ETPB) and structural equation modeling (SEM), we investigated the determinants of Hep B vaccination among college students in Tibet, and aimed to address this gap by conducting a multi-group analysis to compare decision-making processes regarding Hepatitis B vaccination between Tibetan and Han students, providing insights for targeted interventions to improve vaccination rates in minority communities.
Thus, based on the theoretical framework and empirical evidence outlined above, we propose the following ten hypotheses:
H1:
BA toward Hep B vaccination is positively associated with BI
H2:
SN are positively associated with BI.
H3:
PBC is positively associated with BI.
H4:
PBC is positively associated with VB.
H5:
Hep B BI is positively associated with VB.
H6:
VK concerning Hep B vaccination is positively associated with BA toward vaccination.
H7:
PVH is positively associated with BI.
H8:
PVH is positively associated with VB.
H9:
BI mediates the relationship between SN (H9a), PBC (H9b), PVH (H9c), and VB; BA and BI mediate the relationship between VK (H9d) and VB.
H10:
Path coefficients in the mediation model vary by ethnic identity.
Methods
Participants and recruitment procedure
We collected data from March to June 2024 using stratified cluster sampling at three comprehensive colleges under the jurisdiction of the Xizang Autonomous Region: Xizang Minzu University (located in Xianyang, Shaanxi), Tibet University (located in Lhasa, Xizang), and Xizang Agricultural and Animal Husbandry University (located in Nyingchi, Xizang). We categorized the participants by their school and major, with 3–4 classes randomly selected from each major.
The inclusion criteria for participants were (1) household registration in Tibet and (2) voluntary participation in the questionnaire survey. The exclusion criteria were (1) unable to read the questionnaire independently, (2) Hep B patient, and (3) individuals who had received the Hep B Vaccine through NIP or the Supplemental Immunization Program for NIP before the age of 15. We calculated the sample size estimation for the cross-sectional survey using the following formula:
where d represents the permissible error, set at 0.03 based on expert experience; α is the type I error, set at 0.05 as per standard practice; and P is the adult Hep B vaccination rate in ethnic autonomous area, which is 13.9% according to Xu et al .43 We set the design effect (deff) at 2, considering both international research practices and the specific context of China.
The estimated minimum sample size was 1,022 individuals. After accounting for factors such as the rate of lost visits and refusal of visits, an additional 10%-20% was added to the estimated sample size, and the final sample size was around 1,200 individuals.
To ensure the quality of the questionnaire and prevent missing data, the questionnaire was administered on-site via an online e-questionnaire link and completed class by class, under the supervision of a teacher. At least one member of the research team was present to handle any questions from participants. Counselors and classroom teachers provided support and assistance to ensure the smooth execution of the project. Additionally, the project received ethical approval from the Ethics Committee of the Faculty of Medicine at Xizang Minzu University (No. 23MDY04). Prior to the survey, participants were given a comprehensive explanation of the study, with assurances of voluntary participation and confidentiality.
Measures
We adapted the measures used in this study from the basic framework of TPB, incorporating additional dimensions for VK and PVH. The questionnaire items were based on Franceis’ scale and included questions from other scholars’ surveys to develop a suitable set of questions.24,25,44 (show in Appendix A)
Behavior measure
We defined Hep B VB as receiving the Hep B vaccine after reaching the age of 16. We measured it using a dichotomous entry: “Did you receive the non-NIP Hep B vaccine?” (yes/no).
Behavior attitude measure
We assessed BA toward the TPB using a scale with four items using the prompt “I think that the Hep B vaccine is … ” The participants could choose from the following answers, we used five-point Likert scale: useless/risky/unnecessary/has serious side effects was score as 1 and useful/not risky/necessary/has no side effects was score as 5. Participants were instructed to score from 1–5 according to their personal views.
Subjective norms measure
We assessed SN using four items on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree): “The attitudes of (1) online media or netizens/(2) parents and family members/(3) classmates and friends/(4) doctors influenced my decision to receive the non-NIP Hep B vaccine.”
Perceived behavioral control measure
We assessed PBC using four items ranging from 1 (strongly disagree) to 5 (strongly agree): “I think I am able to follow through with the plan and put it into action, if I decide to get the non-NIP Hep B vaccine.” “I think the decision to get the non-NIP Hep B vaccine or not was an easy decision to make,” “I think I made the right decision.” and “I think I can make an independent decision about whether to get the non-NIP Hep B vaccine or not.”
Behavior intention measure
We measured BI using three items scale: “After reaching the age for the non-NIP Hep B vaccine (16 years and older), I think I would (1) considering to get/(2) trying to get/(3) actually getting the non-NIP Hep B vaccine.” We assessed this using a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree).
Vaccination knowledge measure
We assessed the knowledge dimension using four items ranging from 1 (strongly disagree) to 5 (strongly agree), focusing on the participants’ understanding of the benefits of Hep B vaccination: “I am highly aware of how the Hep B vaccine protects me from Hep B,” “I am highly aware of the Hep B vaccine’s role in reducing the serious consequences of the disease,” “I am highly aware of the Hep B vaccine’s role in creating an immune barrier for the population.” and “I am highly aware of the importance of Hep B vaccine for social activities (e.g.: travel, job hunting, learning) provides convenience .”
Past vaccination history measure
Participants were asked whether they had received the influenza vaccine, rabies vaccine, HPV vaccine, hemorrhagic fever vaccine, and an open-ended question was included to allow participants to list any additional non-NIP vaccines they had received beyond those mentioned above. If participants had received the non-NIP Hep B vaccine, we ensure that these non-NIP vaccines were administered prior to the Hep B vaccination. The results were recorded as follows: “never received” for those with no vaccinations, and “received” for those who had received at least once vaccination.
We also collected data on socio-demographic traits such as sex, age, ethnicity, place of residence, school, grade, profession, and parents’ education level.
Data analysis
We analyzed the data descriptively using SPSS 26.0 software. We assessed the reliability of the questionnaire by calculating the Cronbach’s alpha coefficient. Additionally, we evaluated the component reliability and convergent validity of the scales using composite reliability (CR) and average variance extracted (AVE) tests, calculated with AMOS 24.0 software.45 The analysis involved comparing the root value of AVE with Pearson correlation coefficients between latent variables to determine their validity. We estimated the structural equation models using the maximum likelihood method, with model fit assessed using the minimum discrepancy of confirmatory factor analysis/degrees of freedom (CMIN/df), the goodness-of-fit index (GFI), the adjusted GFI (AGFI), the comparative fit index (CFI), and the root mean square of error of approximation (RMSEA).46 We employed a bias-corrected percentile Bootstrap test with 5,000 replicate extractions to calculate 95% confidence intervals (CIs) to validate the mediating effects of the models,47 with the test level set at 0.05.
Data were analyzed using AMOS 24.0 software to conduct a multi-group analysis. This analysis aims to examine differences in the structural model across groups by using nested models with constraints to test for structural invariance.48,49 The primary objective of this multi-group analysis was to assess whether ethnic factors moderate the model and to explore the mechanisms influencing vaccination intentions and behaviors in different ethnic groups. The process involves several steps:
Measurement Invariance: A measurement weight equality constraint was applied to the baseline model to assess whether the measurement structure is consistent across groups. If the test was passed, it indicated that the measurement model is invariant and suitable for both groups.
Structural Invariance: Next, based on the previous step, we further imposed equality constraints on the structural weights to assess whether differences exist in the structural models (i.e., path coefficients) between the groups. This step evaluated whether the relationships between variables are consistent across the Tibetan and Han groups. The main goal is to evaluate whether ethnic factors moderate the model and if further exploration is needed to understand the mechanisms influencing vaccination intentions and behaviors in different groups.
Results
Characteristics of the participants
We included a total of 1,126 participants (92.0% response rate) in the study after excluding questionnaires that were completed in under 4 minutes, did not meet the inclusion criteria, or exhibited highly patterned responses. The sample comprised 66.4% female (747) and 33.7% male (379) students. Over half of the students were Tibetan, accounting for 77.3% of the total. Additionally, 74.8% of the students came from rural areas, while 9.4% were involved in the medical profession. Most respondents were sophomores (41.7%) and juniors (31.2%). Furthermore, 12.2% reported having a family member employed in a medical-related occupation, such as in the Department of Health, hospitals, or the Center for Disease Control and Prevention (CDC). Most participants’ parents had an education level of elementary school or lower, at 55.6% and 69.5% for fathers and mothers respectively. Family incomes were either below ¥10,000 per year (33.0%) or between ¥10,000 and ¥50,000 per year (35.7%) (Table 1).
Table 1.
Participants’ information and univariate analysis.
| Variable | N (%) | Hep B vaccination |
Univariate analysis |
|||
|---|---|---|---|---|---|---|
| Yes (n = 184) |
No (n = 942) |
x2 | P value | |||
| Sex | Male | 379 (33.7%) | 61 | 318 | 0.025 | 0.874 |
| Female | 747 (66.3%) | 123 | 624 | |||
| Ethnicity | Tibetan | 870 (77.3%) | 135 | 735 | 1.900 | 0.168 |
| Han | 256 (22.7%) | 49 | 207 | |||
| Locality | Rural | 916 (81.3%) | 140 | 776 | 4.015 | 0.045 |
| Urban | 210 (18.7%) | 44 | 166 | |||
| Medical professional | Yes | 106 (9.4%) | 24 | 82 | 3.398 | 0.065 |
| No | 1020 (90.6%) | 160 | 860 | |||
| College | Xizang Minzu University | 351 (31.2%) | 50 | 301 | 1.641 | 0.440 |
| Xizang Agricultural and Animal Husbandry University | 525 (46.6%) | 91 | 434 | |||
| Tibet University | 250 (22.2%) | 43 | 207 | |||
| Grade | Freshman | 158 (14.0%) | 23 | 135 | 5.841 | 0.120 |
| Sophomore | 470 (41.7%) | 74 | 396 | |||
| Junior | 351 (31.2%) | 53 | 298 | |||
| Senior | 147 (13.1%) | 34 | 113 | |||
| Family with a medical background | Yes | 137 (12.2%) | 24 | 113 | 0.158 | 0.691 |
| No/Unknown | 989 (87.8%) | 160 | 829 | |||
| Father’s education level | Primary | 626 (55.6%) | 87 | 539 | 12.925 | 0.012 |
| Secondary | 276 (24.5%) | 45 | 231 | |||
| High school | 95 (8.4%) | 24 | 71 | |||
| College | 79 (7.0%) | 20 | 59 | |||
| Unknown | 50 (4.4%) | 8 | 42 | |||
| Mother’s education level | Primary | 783 (69.5%) | 114 | 669 | 11.180 | 0.025 |
| Secondary | 186 (16.5%) | 31 | 155 | |||
| High school | 71 (6.3%) | 20 | 51 | |||
| College | 36 (3.2%) | 8 | 28 | |||
| Unknown | 50 (4.4%) | 11 | 39 | |||
| Annual household income | <10,000 | 372 (33.0%) | 59 | 313 | 3.260 | 0.515 |
| 10,000–50,000 | 402 (35.7%) | 58 | 344 | |||
| 50,000–100,000 | 131 (11.6%) | 26 | 105 | |||
| >100,000 | 86 (7.6%) | 17 | 69 | |||
| Unknown | 135 (12.0%) | 24 | 111 | |||
The survey indicated that 16.3% (184/1126) of the respondents had received the Hep B vaccine. Univariate analysis identified a significant association between VB and factors such as locality, parents’ education level, and the presence of relatives studying medicine (p<0.05). However, these demographic factors did not significantly predict Hep B VB when included in the logistic regression model. Consequently, we excluded demographic variables from the SEM analysis.
Measurement model reliability and fit
We removed items from the scale based on their factor loadings, excluding those having loadings below 0.6.50 The CR and Cronbach’s alpha coefficients for all dimensions exceeded 0.7, while the AVE surpassed 0.5. These findings indicate that the scales demonstrated strong internal consistency and solid convergent validity (Table 2). In terms of discriminant validity, the square roots of the AVE values for each construct were greater than the correlations between the latent variables, except for the correlation between SN and VK, which was slightly higher. Despite this result, the discriminant validity was generally acceptable (Appendix B). Furthermore, the measurement model showed satisfactory fit indices: χ2/df = 2.983, RMSEA = 0.042, GFI = 0.968, AGFI = 0.954, CFI = 0.978, all of which met the recommended criteria.46 These results suggest that the data fit the model well (Appendix C).
Table 2.
Unstandardized coefficients (unstd), standard errors (SE), test of significant deviation from zero (Z, p-value), standard deviations (std) of items, reliability (Cronbach’s α), composite reliability (CR), and average variance extracted (AVE) for the measurement scales.
| Dimension | Question | Unstandardized coefficients (Unstd.) | Standard error (SE) | Z-value | P-value | standard deviation (Std.) | Cronbach alpha (α) | Composite Reliability (CR) | Average Variance Extracted (AVE) |
|---|---|---|---|---|---|---|---|---|---|
| BA | BA1 | 1.000 | 0.824 | 0.818 | 0.822 | 0.607 | |||
| BA2 | 0.910 | 0.040 | 22.699 | <0.001 | 0.694 | ||||
| BA3 | 0.987 | 0.039 | 25.569 | <0.001 | 0.813 | ||||
| SN | SN1 | 1.000 | 0.809 | 0.853 | 0.854 | 0.594 | |||
| SN2 | 0.968 | 0.034 | 28.120 | <0.001 | 0.780 | ||||
| SN3 | 0.932 | 0.034 | 27.190 | <0.001 | 0.759 | ||||
| SN4 | 0.930 | 0.036 | 26.058 | <0.001 | 0.733 | ||||
| PBC | PBC1 | 1.000 | 0.714 | 0.774 | 0.775 | 0.535 | |||
| PBC2 | 1.030 | 0.051 | 20.301 | <0.001 | 0.721 | ||||
| PBC3 | 1.116 | 0.053 | 20.949 | <0.001 | 0.759 | ||||
| VK | VK1 | 1.000 | 0.755 | 0.795 | 0.798 | 0.569 | |||
| VK2 | 1.007 | 0.045 | 22.594 | <0.001 | 0.710 | ||||
| VK3 | 1.127 | 0.045 | 25.157 | <0.001 | 0.795 | ||||
| BI | BI1 | 1.000 | 0.744 | 0.800 | 0.802 | 0.574 | |||
| BI2 | 1.021 | 0.045 | 22.526 | <0.001 | 0.756 | ||||
| BI3 | 1.037 | 0.045 | 22.851 | <0.001 | 0.772 |
AVE = average variance extracted, BA = behavioral attitude, BI = behavioral intention, CR = composite reliability, PBC = perceived behavioral control, SE = standard error, SN = subjective norms, Std. = standard deviation, Unstd. = unstandardized coefficients, VK = vaccination knowledge, α = Cronbach’s alpha reliability coefficient.
Analysis of SEM
The fit of the structural model was tested before the path analysis and the model fit indices of the structural model indicated a good fit(χ2/df = 2.634, RMSEA = 0.038, GFI = 0.976, AGFI = 0.955, CFI = 0.976), as show in Appendix C. For the entire sample, the results (Appendix D) showed that most hypothesized paths were significant, except for the paths between PBC and VB (p=0.300) and between PVH and BI (p=0.184). The comprehensive model accounted for 50.1% of the variance in BI and 20.1% of the variance in VB. Specifically, VK was positively associated with BA (β=0.518, p< 0.001). BA (β=0.232, p<0.001), SN (β=0.385, p<0.001), and PBC (β=0.239, p<0.001) were positively correlated with BI. Additionally, BI (β=0.448, p<0.001) and PVH (β=0.127, p<0.001) were positively associated with VB (Figure 1a).
Figure 1.
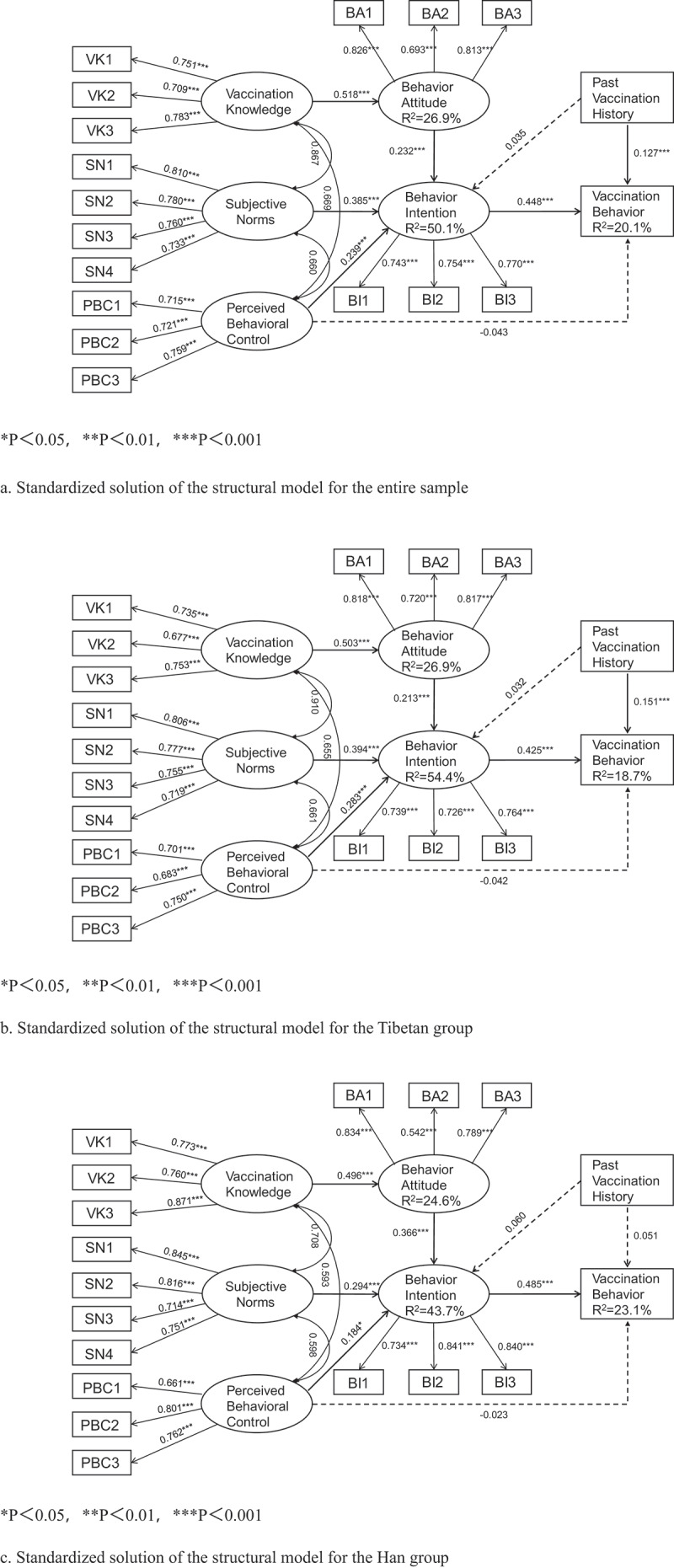
Standardized solution of the structural model.
Among the four proposed pathways to explain the mediating effects, the results from the SEM supported the mediating effects for H9a, H9b, and H9d, except for the pathway involving PVH → BI → VB. Specifically, the relationships between SN, PBC, and VB were mediated by BI. The effect sizes were as follows: SN (β=0.096, 95% CI: [0.066,0.133]) and PBC (β=0.066, 95% CI: [0.036,0.106]). Additionally, BA and BI served as chain mediators between VK (β=0.032, 95% CI: [0.022,0.045]) and VB.
A comparative analysis of the mediating effects for different pathways revealed no statistically significant difference between the mediating effects of the two paths: SN→BI→VB and PBC→BI→VB (p > 0.05). However, the mediating effects of both paths were higher than the pathway from VK→BA→BI→VB (Bpathway 1=0.065, Bpathway 2=0.035, p<0.05), as shown in Table 3.
Table 3.
Results of the mediation effect in the proposed model.
| Pathway | Point estimate (Unstd.) |
Z-value | Bootstrapping 95% |
P-value | ||||
|---|---|---|---|---|---|---|---|---|
| Standard error (SE) | Bias-corrected |
Percentile |
||||||
| Lower | Upper | Lower | Upper | |||||
| The mediation effect test of the entire sample | ||||||||
| SN → BI → VB (1) | 0.096 | 0.017 | 5.647 | 0.066 | 0.133 | 0.065 | 0.131 | <0.01 |
| PBC → BI → VB (2) | 0.066 | 0.018 | 3.667 | 0.036 | 0.106 | 0.035 | 0.103 | <0.01 |
| PVH → BI → VB (3) | 0.012 | 0.009 | 1.333 | −0.005 | 0.030 | −0.006 | 0.030 | >0.05 |
| VK → BA → BI → VB (4) | 0.032 | 0.006 | 5.333 | 0.022 | 0.045 | 0.021 | 0.044 | <0.01 |
| Comparison of the mediation effect | ||||||||
| 1 vs 2 | 0.030 | 0.028 | 1.071 | −0.025 | 0.085 | −0.025 | 0.084 | >0.05 |
| 1 vs 4 | 0.065 | 0.017 | 3.824 | 0.034 | 0.101 | 0.033 | 0.101 | <0.01 |
| 2 vs 4 | 0.035 | 0.018 | 1.944 | 0.002 | 0.074 | 0.001 | 0.073 | <0.05 |
| Mediation effect test of the Tibetan group | ||||||||
| SN → BI → VB | 0.092 | 0.019 | 4.842 | 0.059 | 0.135 | 0.057 | 0.131 | <0.001 |
| PBC → BI → VB | 0.076 | 0.023 | 3.304 | 0.039 | 0.133 | 0.038 | 0.129 | <0.001 |
| PVH → BI → VB | 0.010 | 0.009 | 1.111 | −0.008 | 0.030 | −0.008 | 0.029 | >0.05 |
| VK → BA → BI → VB | 0.028 | 0.006 | 4.667 | 0.018 | 0.041 | 0.017 | 0.040 | <0.001 |
| Mediation effect test of the Han group | ||||||||
| SN → BI → VB | 0.080 | 0.031 | 2.581 | 0.030 | 0.153 | 0.027 | 0.149 | <0.01 |
| PBC → BI → VB | 0.068 | 0.038 | 1.789 | 0.000 | 0.155 | −0.005 | 0.146 | >0.05 |
| PVH → BI → VB | 0.023 | 0.022 | 1.045 | −0.018 | 0.072 | −0.020 | 0.069 | >0.05 |
| VK→ BA → BI → VB | 0.050 | 0.019 | 2.632 | 0.022 | 0.103 | 0.021 | 0.099 | <0.001 |
BA = behavioral attitude, BI = behavioral intention, PBC = perceived behavioral control, PVH = past vaccination history, SE = standard error, SN = subjective norms, Unstd. = unstandardized coefficients, VB = vaccination behavior, VK = vaccination knowledge.
Comparison of the Tibetan and Han groups
The comparison between the two-group constraint models yielded the following findings: After imposing the equality constraint on the measurement weights of the baseline model, no significant difference was observed between the two groups (χ2 =13.958, df=11, p > 0.05). The small absolute increment in the fit indices further supported the conclusion that the measurement model is invariant across the two groups. However, when we further applied equality constraints on the structural weights of the model based on this foundation, significant differences between the two groups were identified (χ2 =18.137, df =8, P<0.05). This suggests that ethnicity may moderate the structural influence on vaccination behavior. These findings warrant further exploration of the differences in path coefficients between the two group models, as detailed in Appendix E. For the Tibetan group, the model explained 18.7% of the variance in VB and 54.4% in BI. VK positively influenced BA (β=0.503, p<0.001), and BA, SN, and PBC were positively correlated with BI. However, no statistically significant relationship between PBC and VB was observed.
In the Han group, the model explained 23.1% of the variance in VB and 43.7% in BI. We noted similarly positive relationships between VK, BA, and BI, but unlike the Tibetan group, PVH was not significantly linked to VB. The mediation effect of PBC on VB was also non-significant (β=0.068, p>0.05), as shown in Table 3.
We analyzed the paths of the Tibetan and Han groups to assess potential differences between the models. By comparing the critical ratios of the path coefficients, a significant difference was indicated if the absolute value of the critical ratio was exceeded 1.96 (p < 0.05). The analysis revealed two significantly different paths: BA → BI (critical ratio=2.942) and VK→BA (critical ratio=-2.432). Although we observed no significant difference between PVH and VB, the direction of the path coefficients differed between the groups, suggesting possible variability in this relationship. These findings support Hypothesis 10 (see Table 4).
Table 4.
The critical ratio of path coefficients between the Tibetan and han groups.
| Hypothesis | Pathway | Path coefficient |
Critical ratio | |
|---|---|---|---|---|
| Tibetan group | Han group | |||
| H1 | BA → BI | 0.213*** | 0.366*** | 2.942** |
| H2 | SN → BI | 0.394*** | 0.294*** | −0.603 |
| H3 | PBC → BI | 0.283*** | 0.184* | −0.340 |
| H4 | PBC → VB | −0.042 | −0.023 | 0.135 |
| H5 | BI → VB | 0.425*** | 0.485*** | 0.217 |
| H6 | VK → BA | 0.503*** | 0.496*** | −2.432** |
| H7 | PVH → BI | 0.032 | 0.060 | 0.545 |
| H8 | PVH→VB | 0.151*** | 0.051 | −1.399 |
BA = behavioral attitude, BI = behavioral intention, CI = confidence interval, PBC = perceived behavioral control, PVH = past vaccination history, SE = standard error, SN = subjective norms, VB = vaccination behavior, VK = vaccination knowledge.
*P<0.05,**P<0.01,***P<0.001.
Discussion
Our study found that among university students in Tibet, only 16.3% of students who missed the NIP Hep B vaccine received the adult Hep B vaccine. This rate aligns with findings from other ethnic minority regions in China but is notably lower than vaccination rates in economically developed areas.7,43 This result underscores the urgent need for public health initiatives to enhance vaccination rates in this region.
The primary aim of this study was to develop an ETPB model to assess its efficacy in explaining Hep B vaccination intention and behavior among unvaccinated university students in Tibet, considering ethnic differences. Our results support the hypotheses that VK (H6) positively influences BA, and that BA (H1), SN (H2), and PBC (H3) positively impact BI. Additionally, PVH (H8) and BI (H5) were found to positively impact VB. Nevertheless, PVH (H7) did not substantially impact BI, and PBC (H4) did not significantly influence VB. Furthermore, the model was able to differentiate between different ethnic identities through multi-group analysis, suggesting that the ETPB extension model can be utilized to shed light on BI and subsequent VB.
ETPB model analysis
We found that Tibetan university students with positive attitudes toward Hep B vaccination were more likely to intend to get vaccinated. Additionally, higher levels of positive attitudes were associated with stronger intentions to vaccinate. The perceptions of vaccine-related knowledge of participants had an indirect effect on VB, mediated by BA and BI. These findings align with those of previous studies.25,51,52 When individuals understand the efficacy and advantages of the Hep B vaccine, their favorable attitudes toward the vaccine are enhanced, leading to increased intention to get vaccinated and ultimately promoting VB.27 Hep B vaccination efforts should prioritize highlighting the necessity and advantages of vaccination to potentially enhance vaccination rates.
The participants’ intention to get vaccinated against Hep B was more strongly influenced by SN compared to other factors. Additionally, our findings provide evidence that BI mediates the promotion of VB. This result suggests that students are more susceptible to the influence of expectations surrounding their social relationships on their intention and choice to get vaccinated. This finding aligns with previous research,24,26 Indicating that students prefer to receive recommendations for Hep B vaccination from individuals. For instance, a study conducted by Afolabi et al. revealed that health worker recommendations effectively motivated participants to receive the Hep B vaccine.27
Certain studies examining COVID-19 vaccination intention imply that SN do not play a significant role in predicting BI. This finding appears to contradicts our results.25,53 However, whether this discrepancy is directly comparable is worth further investigation. A study by Emily et al. suggested that the empirical relationship between the COVID-19 vaccine and the Hep B vaccine lacks peer-reviewed evidence.54 On one hand, this difference may stem from the distinct characteristics of the COVID-19 vaccine and disease compared to Hep B, which may render direct comparisons inappropriate. On the other hand, it suggests that different vaccines may raise different concerns, and applying the same reasoning from COVID-19 to Hep B could lead to flawed conclusions. This suggests the need for solid empirical research to verify the relationship between these two vaccines and confirm their comparability
Moreover, the influence of online communication (as opposed to traditional social relationships) is a matter of greater concern than the influence of doctors, parents, or classmates. The emergence of “online communities” transcends conventional geographic constraints. The vast amount and quick spread of information online facilitate the development of vaccine hesitancy among students through negative public opinion on social media, more so than in traditional face-to-face interactions. It is crucial not to overlook the impact of social media on vaccination intention and behaviors41,55,56
We found that PBC positively influenced BI. However, PBC did not directly predict behavior but rather influenced it through the intention to vaccinate. This finding aligns with the discoveries found by O’Neal et al.,31 though it contradicts the initial framework proposed by Ajzen et al.16 This phenomenon may be attributed to the fact that while some university students perceive vaccination decisions as individually autonomous, the practical execution of VB is not exempt from the impact and restrictions imposed by the family model. Parental involvement curtails students’ autonomy in making decisions regarding healthcare. This pattern may also influence the relationship between PVH and both vaccination intention and behavior.
While past vaccination experiences can serve as a reference for students’ future vaccination experiences, these past behaviors may have been decided upon by the students’ parents rather than by the students. As a result, the influence of PVH on their current choices may be diminished. This situation may clarify our findings, wherein PVH did not emerge as a significant predictor of BI and exhibited a relatively weak association with VB. These results are comparable to the outcomes of a study on flu vaccination.24
Multi-group analysis
The path correlation results of the structural model in the analysis of multi-group effects showed distinct patterns in the Tibetan and Han groups, partially supporting the conclusion that the attributes of ethnic group have a moderating effect on the model. Specially, the analysis, found that PVH did not significantly impact VB in the Han group, which differed from the Tibetan group.
We have argued that past VB is likely influenced by surrogate parental decision-making due to parental and family model in the vaccination process for students. This influence leads to a difference between individuals’ perceptions of the situation and their sense of control over their own behavior. Parents of Chinese minority students are influenced by factors such as culture, educational level, ethnic religion, and cultural disparities, leading to a limited pattern of parental involvement in their children’s health choices.38,57 Consequently, Han individuals may be more likely to be influenced by family patterns compared to Tibetan students. Additionally, the correlation between PVH and VB was no longer significant in the Han group. Moreover, the influence of PBC on VB through BI is not significant in the Han group, possibly due to the presence of this phenomenon. Hence, the impact of PVH on VB and the underlying process by which PBC affects VB through BI may not be suitable for this specific subgroup of the study’s population.
Our analysis of the variations in path coefficients indicates that the impact of BA on BI is more evident in the Han group. When Han participants held favorable views toward the vaccine, their inclination to get vaccinated increased significantly. In contrast, the ability of Tibetan group to promote positive attitudes was stronger when they believed they had a greater understanding of the Hep B vaccine and held more favorable opinions about it. Previous studies have reached similar conclusions.39,40 These variations may stem from the impact of diverse traditional cultures and religious beliefs on the decision-making process regarding healthcare options among different ethnic groups.57 Medical anthropology asserts that the delivery of healthcare should not solely rely on modern medicine but should also consider social, cultural, psychological, spiritual, and other variables. This assertion implies that it is important to consider ethnic-cultural disparities when striving to encourage adult VB among Tibetan college students. Enhancing cultural caregiving competence and improving the ability to handle cultural differences are crucial steps in this direction.58,59 This phenomenon suggests that further research could be conducted to validate the impact of ethnic differences on decision-making processes and behaviors within a more balanced sample size.
Limitations
This study has several limitations. First, the cross-sectional design limits the ability to establish causal relationship, although the findings offer valuable directions for future research. Second, vaccination behavior (VB) was self-reported through retrospective recall, which may introduce recall bias.
However, a preliminary survey was conducted to refine the questionnaire, and in the subsequent community-based trial, a subset of participants underwent serological testing, which demonstrated high accuracy and good quality in self-reports. Additionally, we assessed students’ understanding of Hep B vaccination based on subjective perceptions rather than objective knowledge. The sample was also limited to three universities in Tibet, excluding junior colleges. Future studies should consider expanding the sample size to improve representativeness and generalizability. Finally, the sample was imbalanced, with 77.3% (N = 870) from the Tibetan group and 22.7% (N = 256) from the Han group. In addition,81.3% of participants were from rural areas (N = 916), while only 18.7% were from urban areas (N = 210); 87.8% of participants came from families without a medical background (N = 989), and 12.2% came from families with a medical background (N = 137). This imbalance, resulting from random sampling, suggests the need for future research to ensure more balanced representation, possibly using matching techniques to better explore the factors influencing Hepatitis B vaccination in these populations and account for potential socio-demographic differences.
Conclusion
This study offers valuable insights and strategies for Hep B prevention, vaccine promotion, and health education and promotion, particularly in universities with ethnic minority students. In general, the Hep B vaccination rate of college students is low. The model analysis results suggest that we need for tailored interventions based on cultural background. For Tibetan students, the focus was on improving practical knowledge of the Hep B vaccine to encourage vaccination uptake rather than merely promoting the vaccine. In contrast, Han students benefited from strategies aimed at enhancing positive attitudes through educational campaigns, leading to increased VB. By leveraging medical advice and positive online public sentiment, societal expectations and perceived control over VB were strengthened, particularly among Tibetan university students.
Supplementary Material
Acknowledgments
We would like to thank Xizang Minzu University, Tibet University, and Xizang Agricultural and Animal Husbandry University, all college students who participated in this survey, and Editage (www.editage.cn) for English language editing.
Biography
Jin Hui is a professor and doctoral supervisor at Southeast University. He has been a visiting scholar at The Chinese University of Hong Kong and the University of California, Berkeley. He serves as an expert in Jiangsu Province’s COVID-19 prevention and control team. Jinhui is a reviewer for the Ministry of Education talent programs, National Natural Science Foundation projects, and university laboratory safety. He is the Deputy Chair of the Pharmaceutical Division of the Chinese Society of Systems Engineering and an editorial board member for journals such as “Environmental and Occupational Medicine,” as well as a peer reviewer for “The Lancet” and “Nature Human Behaviour.” He has led and participated in 12 major national projects, including Natural Science Foundation projects, and has published 85 papers in SCI journals. He has received three ministerial awards and seven provincial awards.
Funding Statement
This work was supported by: Research Projects of Xizang Minzu University [Grant No. 23MDY04]. The National Natural Science Foundation of China [Grant No. 82460671].
Disclosure statement
No potential conflict of interest was reported by the author(s).
Author contributions
Conceptualization, Hui Jin; methodology, Hui Jin; software, Jun Ma and Qi Chen; formal analysis, Qi Chen and Jun Ma; survey, Xiaoxin Ma and Xiaolei Zheng; resources, Ruipeng Wu; data curation, Ruipeng Wu,Yingting Wang, Jun Ma, Qi Chen; writing – original draft preparation,Qi Chen. All authors have read and agreed to the published version of the manuscript.
Data availability
Data available on request due to restrictions (e.g., privacy, legal or ethical reasons).
Institutional review board statement
Our study protocol was approved by the Ethics Committee of the Faculty of Medicine at Xizang Minzu University (No. 2023–25; data 26 June 2023).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2025.2452026
References
- 1.Hsu YC, Huang DQ, Nguyen MH.. Global burden of hepatitis B virus: current status, missed opportunities and a call for action. Nat Rev Gastroenterol Hepatol. 2023;20(8):524–11. doi: 10.1038/s41575-023-00760-9. [DOI] [PubMed] [Google Scholar]
- 2.Cui F, Blach S, Mingiedi CM, Gonzalez MA, Alaama AS, Mozalevskis A, Séguy N, Rewari BB, Chan P-L, Le L-V, et al. Global reporting of progress towards elimination of hepatitis B and hepatitis C. Lancet Gastroenterol Hepatol. 2023;8(4):332–342. doi: 10.1016/S2468-1253(22)00386-7. [DOI] [PubMed] [Google Scholar]
- 3.Devarbhavi H, Asrani SK, Arab JP, Nartey YA, Pose E, Kamath PS.. Global burden of liver disease: 2023 update. J Hepatol. 2023;79(2):516–537. doi: 10.1016/j.jhep.2023.03.017. [DOI] [PubMed] [Google Scholar]
- 4.Sheena BS, Hiebert L, Han H, Ippolito H, Abbasi-Kangevari M, Abbasi-Kangevari Z, Abbastabar H, Abdoli A, Abubaker Ali H, Adane MM, et al. Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Gastroenterol Hepatol. 2022;7(9):796–829. doi: 10.1016/S2468-1253(22)00124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang H, Wei C. How to address vaccine hesitancy? Lessons from national hepatitis B immunization program in China. Front Public Health. 2024;12:1286801. doi: 10.3389/fpubh.2024.1286801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lazarus JV, Picchio CA, Nayagam S, Ratzan S, Thursz M. Strengthening vaccine confidence during the COVID-19 pandemic: a new opportunity for global hepatitis B virus elimination. J Hepatol. 2020;73(3):490–492. doi: 10.1016/j.jhep.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bai X, Chen L, Liu X, Tong Y, Wang L, Zhou M, Li Y, Hu G. Adult hepatitis B virus vaccination coverage in China from 2011 to 2021: a systematic review. Vaccines. 2022;10(6):900. doi: 10.3390/vaccines10060900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tian T, Dunzhu D, Hu Y, Zhao W, Qiong Z, Ciren D, Jin M. A seroepidemiological survey of hepatitis B markers in people aged 1-69 years in Xizang Autonomous Region in 2020. Chin J Vaccines Immun. 2024;30:174–178. doi: 10.19914/j.CJVI.2024027. [DOI] [Google Scholar]
- 9.Zhao W, Tian T, Hu Y, Nimaciren, Bianbacangjue,Zhuoma,Ye X, Ciwang, Dunzhuduoji. Analysis of the epidemiological characteristics of hepatitis Bvirus and the current status of hepatitis Bvaccination in the population aged 1 to 69 in Tibet Autonomous Region in 2014.Chin JIntegr Trad West Med Liver Dis.2023;33:504–508. doi: 10.3969/j.issn.1005-0264.2023.006.007. [DOI] [Google Scholar]
- 10.Zheng H, Wang FZ, Zhang GM, Cui FQ, Wu ZH, Miao N, Sun X-J, Liang X-F, Li L. An economic analysis of adult hepatitis B vaccination in China. Vaccine. 2015;33(48):6831–6839. doi: 10.1016/j.vaccine.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Wan Y, Wang F, Zheng H, Zhang G, Zhang W, Yao J, Cui Fet al. eImmunogenicity of hepatitis B vaccines in 20-49-year-old adults vaccinated using varying immunization schedules. Chin J Vacc Immun. 2020;26:19–24. doi: 10.19914/j.cjvi.2020.01.004. [DOI] [Google Scholar]
- 12.Dou Q, Yang K, Wang W, Yang J, Lyu W, Liu Q, Kong J, Feng D, Seng M, Guo Y, et al. Surveillance of hepatitis B surface antibody levels among people aged 1- 79 years in Henan in 2021. Henan J Prev Med. 2023;34:60–80.doi: 10.13515/j.cnki.hnjpm.1006-8414.2023.01.006. [DOI] [Google Scholar]
- 13.Shen JC, Feng HY, Shao TY. Analysis of the seroepidemiological survey of viral hepatitis B in the coastal area of Zhoushan City from 2017 to 2020. Chin J PHM. 2022;38:258–261. doi: 10.19568/j.cnki.23-1318.2022.02.0030. [DOI] [Google Scholar]
- 14.Luo JJ, Wang SQ, Wang L, Zhao MJ. Surveillance on hepatitis B immunization level among population in Hubei Province, 2015-2018. Pract Prev Med. 2021;28:66–69. doi: 10.3969/j.issn.1006-3110.2021.01.016. [DOI] [Google Scholar]
- 15.Kong H, Cui X, Zhang Y, Xue Q, Shi J, Yao T, Guo Y, Xu X, Wang S, Feng Y, et al. Occurrence and reduction of hepatitis B vaccine hesitancy among medical university students — Shanxi Province, China, 2020. China CDC Weekly. 2024;6(19):431–436. doi: 10.46234/ccdcw2024.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 17.Ajzen I. The theory of planned behavior: Frequently asked questions. Hum Behav Emerg Technol. 2020;2(4):314–324. doi: 10.1002/hbe2.195. [DOI] [Google Scholar]
- 18.León-Jariego JC, Parrado-González A, Ojea-Rodríguez FJ. Behavioral intention to gamble among adolescents: differences between gamblers and non-gamblers—prevention recommendations. J Gambl Stud. 2020;36(2):555–572. doi: 10.1007/s10899-019-09904-6. [DOI] [PubMed] [Google Scholar]
- 19.Mehdizadeh M, Shariat-Mohaymany A. Who are less likely to vote for a low emission charging zone? Attitudes and adoption of hybrid and electric vehicles. Transp Res A Policy Pract. 2021;146:29–43. doi: 10.1016/j.tra.2021.02.001. [DOI] [Google Scholar]
- 20.Cheng EWL, Chu SKW. Students’ online collaborative intention for group projects: evidence from an extended version of the theory of planned behaviour. Int J Psychol. 2016;51:296–300. doi: 10.1002/ijop.12159. [DOI] [PubMed] [Google Scholar]
- 21.Hossain MB, Alam M, Islam M, Sultan S, Faysal M, Rima S, Hossain MA, Mamun AA. Health belief model, theory of planned behavior, or psychological antecedents: What predicts COVID-19 vaccine hesitancy better among the Bangladeshi adults? Front Public Health. 2021;9:711066. doi: 10.3389/fpubh.2021.711066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ryan M, Marlow LAV, Forster A. Countering vaccine hesitancy among pregnant women in England: The case of Boostrix-IPV. Int J Environ Res Public Health. 2020;17(14):4984. doi: 10.3390/ijerph17144984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shah SFA, Ginossar T, Bentley JM, Zimet G, McGrail JP. Using the theory of planned behavior to identify correlates of HPV vaccination uptake among college students attending a rural university in Alabama. Vaccine. 2021;39(51):7421–7428. doi: 10.1016/j.vaccine.2021.10.082. [DOI] [PubMed] [Google Scholar]
- 24.Yang L, Yang G, Wang Q, Cui T, Shi N, Xiu S, Zhu L, Xu X, Jin H, Ji L, et al. Understanding drivers of influenza vaccine hesitancy among pregnant women in China: Evidence from an extended theory of planned behavior. Expert Rev Vaccines. 2022;21(11):1655–1665. doi: 10.1080/14760584.2022.2117695. [DOI] [PubMed] [Google Scholar]
- 25.Fan CW, Chen IH, Ko NY, Yen CF, Lin CY, Griffiths MD, Pakpour AH. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: An online survey study. Hum Vaccines Immunother. 2021;17(10):3413–3420. doi: 10.1080/21645515.2021.1933687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masserey Spicher V, Weiss MG. Policy and socio-cultural differences between cantons in Switzerland with high and low adolescent vaccination coverage for hepatitis B and HPV. Vaccine. 2019;37(52):7539–7546. doi: 10.1016/j.vaccine.2019.09.085. [DOI] [PubMed] [Google Scholar]
- 27.Afolabi IB, Aremu AB, Maidoki LA, Atulomah NO. Dynamics of hepatitis B infection prevention practices among pregnant women attending antenatal care at Lubaga Hospital Kampala, Uganda using the constructs of information-motivation-behavioural skills model. BMC Public Health. 2022;22(1):2243. doi: 10.1186/s12889-022-14723-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guidry JPD, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, Ryan M, Fuemmeler BF, Carlyle KE. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ajzen I. Residual effects of past on later behavior: Habituation and reasoned action perspectives. Pers Soc Psychol Rev. 2002;6(2):107–122. doi: 10.1207/S15327957PSPR0602_02. [DOI] [Google Scholar]
- 30.Conner M, Armitage CJ. Extending the theory of planned behavior: A review and avenues for further research. J Appl Soc Psychol. 1998;28(15):1429–1464. doi: 10.1111/j.1559-1816.1998.tb01685.x. [DOI] [Google Scholar]
- 31.Malcolm O, Nelson A, Modeste NN, Gavaza P. Factors influencing implementation of personalized prevention plans among annual wellness visit patients using the theory of planned behavior: A quantitative study. Res Soc Adm Pharm. 2021;17(9):1636–1644. doi: 10.1016/j.sapharm.2021.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Pelto PJ, Pelto GH. Studying knowledge, culture, and behavior in applied medical anthropology. Med Anthropol Q. 1997;11(2):147–163. doi: 10.1525/maq.1997.11.2.147. [DOI] [PubMed] [Google Scholar]
- 33.Pujol FH, Toyé RM, Loureiro CL, Jaspe RC, Chemin I. Hepatitis B eradication: vaccine as a key player. Am J Transl Res. 2023;15(8):4971–4983. [PMC free article] [PubMed] [Google Scholar]
- 34.Brosset E, Fressard L, Cogordan C, Bocquier A, Velter A, Annequin M, Bourrelly M, Constance J, Michels D, Mora M, et al. Gradient of vaccine hesitancy among French men having sex with men: An electronic cross-sectional survey in 2022. Hum Vaccines Immunother. 2023;19(3):2293489. doi: 10.1080/21645515.2023.2293489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Momplaisir FM, Kuter BJ, Ghadimi F, Browne S, Nkwihoreze H, Feemster KA, Frank I, Faig W, Shen AK, Offit PA, et al. Racial/ethnic differences in COVID-19 vaccine hesitancy among health care workers in 2 large academic hospitals. JAMA Network Open. 2021;4(8):e2121931. doi: 10.1001/jamanetworkopen,2021.21931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Truong J, Bakshi S, Wasim A, Ahmad M, Majid U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot Int. 2022;37(1):daab105. doi: 10.1093/heapro/daab105. [DOI] [PubMed] [Google Scholar]
- 37.Morgan KM. Medical mistrust, perceived discrimination, and race: A longitudinal analysis of predictors of COVID-19 vaccine hesitancy in US adults. J Racial Ethn Health Disparities. 2023;10(4):1846–1855. doi: 10.1007/s40615-022-01368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang S, Pan J, Wang Z. A cross-sectional survey to evaluate knowledge, attitude and practice (KAP) regarding measles vaccination among ethnic minorities-all databases. Ethn Dis. 2015;25:98–103. [PubMed] [Google Scholar]
- 39.Zhao X, Wang Y, Liu Z, Duan X, Hu S, Wang Y, Remila R, Xu X, Zhao S, Zhang Y, et al. Knowledge and its influencing factors of cervical cancer screening and human papillomavirus vaccines among 19201 Chinese population. Chin J Cancer Prev Treat. 2022;29:623–649. doi: 10.16073/j.cnki.cjcpt.2022.09.02. [DOI] [Google Scholar]
- 40.Qi H, Zhang H, Kang Y, Hou C, Wang X, Fan Y, Ma X. Survey on Knowledge-Attitude-Practice of immunization among parents of children from Linxia Hui autonomous prefecture of Gansu Province. Chin J Health Educ. 2015;31:362–366. doi: 10.16168/j.cnki.issn.1002-9982.2015.04.006. [DOI] [Google Scholar]
- 41.Luan M, Qi Q, Shi W, Tao Z, Bao Y, Zhou J. Differential impacts of vaccine scandal by ethnic and socioeconomic factors: Evidence from China. PLOS ONE. 2023;18(7):e0288841. doi: 10.1371/journal.pone.0288841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mai J, Lin L, Zhou L, Wu Y, Sun X. The influence of self-efficacy on health literacy among Chinese residents. Chin J Health Educ. 2022;38:579–588. doi: 10.16168/j.cnki.issn.1002-9982.2022.07.001. [DOI] [Google Scholar]
- 43.Xu C. Analysis on the situation and influencing factors of hepatitis B vaccination among adults in Yulin city. Preventative Med. 2020;16:27–34. doi: 10.19347/j.cnki.2096-1413.202016010. [DOI] [Google Scholar]
- 44.Francis JJ, Eccles MP, Johnston M, Walker A. Constructing questionnaires based on the theory of planned behaviour: A manual for health services researchers. Newcastle upon Tyne (UK): Centre for Health Services Research, University of Newcastle upon Tyne; 2004. https://openaccess.city.ac.uk/id/eprint/1735/. [Google Scholar]
- 45.Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39–50. doi: 10.2307/3151312. [DOI] [Google Scholar]
- 46.Jackson DL, Gillaspy JA, Purc-Stephenson R. Reporting practices in confirmatory factor analysis: An overview and some recommendations. Psychol Methods. 2009;14(1):6–23. doi: 10.1037/a0014694. [DOI] [PubMed] [Google Scholar]
- 47.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- 48.Xie H, Cui K. Peer victimization, environmental and psychological distress, and academic performance among children in China: A serial mediation model moderated by migrant status. Child Abuse Negl. 2022;133:105850. doi: 10.1016/j.chiabu.2022.105850. [DOI] [PubMed] [Google Scholar]
- 49.Rongsheng T. Muilt-group analysis. In: Lin J, Li J, editors. Amos and research methods. Chongqing: Chongqing Publishing Inc; 2010. p. 154–165. [Google Scholar]
- 50.Hooper D, Coughlan J, Mullen MR. Structural equation modelling: Guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60. doi:https://www.researchgate.net/publication/373874397. [Google Scholar]
- 51.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Health – Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Siu JY, Fung TKF, Leung LH. Social and cultural construction processes involved in HPV vaccine hesitancy among Chinese women: A qualitative study. Int J Equity Health. 2019;18(1):147. doi: 10.1186/s12939-019-1052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alshagrawi SS. Examining health sciences students’ intention to uptake COVID-19 vaccination using the theory of planned behavior. Hum Vaccine Immunother. 2023;19(2):2256044. doi: 10.1080/21645515.2023.2256044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vraga EK, Brady SS, Gansen C, Khan EM, Bennis SL, Nones M, Tang R, Srivastava J, Kulasingam S. A review of HPV and HBV vaccine hesitancy, intention, and uptake in the era of social media and COVID-19. eLife. 2023;12:e85743. doi: 10.7554/eLife.85743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Van Der Linden S. We need a gold standard for randomised control trials studying misinformation and vaccine hesitancy on social media. BMJ. 2023;381:1007. doi: 10.1136/bmj.p1007. [DOI] [PubMed] [Google Scholar]
- 56.Quon CM, Walker M, Graves L. The influence of mass media on the COVID-19 vaccination decision-making process: Prospective survey-based study. J Med Internet Res. 2023;25:e45417. doi: 10.2196/45417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang L. Anthropological analysis of Tibetan people’s medical choice practice under the background of pluralistic medical care: A case study of C Village in Ganzi Tibetan Autonomous Prefecture. J Ethnol. 2021;12:80–88+119. doi: 10.3969/j.issn.1674-9391.2021.04.010. [DOI] [Google Scholar]
- 58.Betsch C, Airhihenbuwa CO, Butler R, Chapman GB, Haase N, Herrmann B, Igarashi T, Kitayama S, Korn L, Nurm ÜK. Improving medical decision making and health promotion through culture-sensitive health communication: An agenda for science and practice. SMDM. 2015;36(7):811–833. doi: 10.1177/0272989X15600434. [DOI] [PubMed] [Google Scholar]
- 59.Tjoflåt I, Karlsen B. Challenges in sharing knowledge: Reflections from the perspective of an expatriate nurse working in a South Sudanese hospital. Int Nurs Rev. 2012;59(4):489–493. doi: 10.1111/j.1466-7657.2012.01020.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data available on request due to restrictions (e.g., privacy, legal or ethical reasons).


