Abstract
Background
The influence of femoroacetabular (FA) impingement has been implied in early hip osteoarthritis, particularly in young patients who enjoy athletics. The purpose of this meta-analysis is to assess the effectiveness and safety of hip arthroscopy compared to open surgical dislocation for the treatment of femoroacetabular impingement (FAI), based on clinical trials that have been published.
Methods
A comprehensive literature search was conducted through PUBMED, EMBASE, and the Cochrane Central Register of Controlled Trials for studies evaluating coxoscopy and open surgical dislocation as treatment modalities for femoroacetabular impingement syndrome (FAI).
Results
Ultimately 9 studies were added in this meta-analysis. 9 studies reported the Improvement of alpha angle of the Hip Arthroscopy treatment group and the surgical treatment group, which was no remarkable statistical significance(SMD: -5.54; 95% Cl: -12.45,1.38; P = 0.117) compared to the surgical treatment group, Modified Harris Hip Score (mHHS) after 12 months of follow-up(SMD: 0.94; 95% Cl: -2.87,4.75; P = 0.629), Nonarthritic Hip Score (NAHS) after 12 months of follow-up (SMD:6.31; 95% Cl: 0.53,12.09; P = 0.032), rate of recurrence (OR: 0.48; 95% Cl: 0.29,0.82; P < 0.01), and rate of Complication (OR: 0.66; 95% Cl: 0.26,1.65; P = 0.372).
Conclusion
Alpha angle improvement, mHHS, NAHS after 12 months of follow-up, rate of recurrence, and rate of Complication are some of the indicators of the study’s results point to the possibility that hip arthroscopy may be effective for patients with FA impingement; hence, these conclusions required to be corroborated by additional superior-quality studies.
Keywords: Hip arthroscopy, Open surgical dislocation, FA impingement, Meta analysis
Introduction
Femoroacetabular impingement (FAI) is considered to be one of the most common causes of hip pain in young adults [1]. FAI is associated with abnormal mechanical contact between the acetabular rim and the upper end of the femur, where there is a femur-based (cam), acetabular-based (pincer), or combined impingement deformity [2]. FAI is considered to be the main etiologic factor in the pathophysiology of secondary hip osteoarthritis FA impingement can occur at any stage of life, but is most common in people between 20 and 40 years of age, with a prevalence between 10% and 15% [3, 4]. In addition, FA impingement has the potential to increase cartilage degeneration and ultimately lead to the development of osteoarthritis of the hip. Early intervention, either prophylactic or therapeutic, can prevent the progression of osteoarthritis and the need for artificial hip replacement [5, 6]. Despite its considerable impact, many clinicians are unfamiliar with FA impingement, largely due to its relatively low profile and unclear etiology, which can lead to misdiagnosis.
The symptoms of FAI include hip pain, limited mobility and joint damage [7]. Operations are performed when symptoms are severe or when non-operative treatment fails [8]. Open surgical dislocation has traditionally been considered the primary surgical treatment option for FAI [9]. Hip arthroscopy is a relatively new surgical procedure that uses small incisions and an arthroscope (small camera) to repair any damage, and is therefore much less invasive than open surgical dislocation.
Surgical interventions to treat FA impingement include surgical dislocation and hip arthroscopy [10, 11]. Hip arthroscopy is popular because it has fewer complications, better outcomes, less bleeding, and shorter recovery periods. However, patients require a period of immobilization after surgery, and patients with acetabular tears must avoid hyperflexion of the hip for six weeks [12, 13]. Several reviews have compared the efficacy of arthroscopic and open surgical dislocation of the hip. The results showed that the arthroscopic approach had fewer complications and a faster recovery rate. Recently, some controlled clinical trials on hip arthroscopy versus open surgical dislocation have been reported. These quantitative analyses were not included in previous reviews. Therefore, the aim of this study was to investigate and evaluate the efficacy of hip arthroscopy and open surgical dislocation in the treatment of FA impingement.
Materials and methods
This meta-analysis was reported in English, according to the guidelines of the Preferred Reporting Items for Systemic Reviews and Meta-analyses. And the ethical approval was deemed unnecessary because our meta-analysis was based on data derived from previously published studies.
Study strategy and selection
Three review authors independently searched the Cochrane Central Register of Controlled Trials (CENTRAL), PUBMED (from 1980 to August 2016), and EMBASE (from May 1995 to September 2023) databases, utilizing the key words in English: femoroacetabular impingement, surgery, adverse effects, randomized controlled trials, and clinical trials. Multiple combinations of these search terms were executed using the Boolean operators “AND” and “OR”. Furthermore, the following MeSH (Medical Subject Headings) term titles/subtitles were also employed: femoral acetabular impingement/complications, femoral acetabular impingement/surgery, and femoral acetabular impingement/treatment. In our meta-analysis, we mainly included randomized controlled trials and clinical trials of femoral acetabular impingement and surgery.
Inclusion and exclusion criteria
Inclusion criteria
Studies that meet the following criteria may be included in our analysis process: randomized controlled trials (RCTS) and controlled clinical trials, studies comparing open surgical dislocation with hip arthroscopy, reports of efficacy or safety of the two procedures, and studies that include patients with a clinical diagnosis of FAI.
Exclusion criteria
The following categories of studies were excluded, case reports, and cohort studies, including studies of FAI patients who had prior surgery for the affected hip, and studies that underwent open surgery without surgical dislocation (such as an improved Smith-Petersen approach) Differences in study selection were resolved by discussion and consensus among the authors.
Research grouping
Hip Arthroscopy treatment group received hip arthroscopy in the treatment of patients with FA impingement, and the surgical treatment group received open surgical dislocation in the treatment of FA impingement patients.
Types of outcome measures
Outcome Measures patients with FA impingement; Based on research, the assessment tools for FA impingement in patients, the following outcomes are associated with hip arthroscopy and open surgical dislocation: ①alpha angle Improvement; ②after 12 months of follow-up of Modified Harris Hip Score (mHHS); ③after 12 months follow-up of Nonarthritic Hip Score (NAHS); ④ Recurrence rate; ⑤ Complication rate. At least one of the aforementioned scales was used in the literature reviewed for this study to assess outcome measures.
Extraction of data and quality evaluation
The NOS is a well-established and widely used instrument that allows for a systematic and comprehensive assessment of study quality across various dimensions [14]. Two independent review authors evaluated the quality of each study employing the Newcastle-Ottawa Scale (NOS), which comprises three quality criteria: selection (with a maximum score of 4), comparability (with a maximum score of 2), and assessment of exposure or outcome (with a maximum score of 3). A score of 9 indicates a study of the highest quality, while a score of 5 or less signifies a study of lower quality. Any disagreements on the assessment of study quality were resolved through discussion.
Statistical analysis
Using Review Manager (RevMan), this meta-analysis was carried out. Combined Effects are: (1) All of the study’s outcome measures were measured data, and various evaluation techniques were employed. As a result of the variations in scores, the standardized mean difference (SMD) and 95% confidence interval (CI) are utilized as effect indicators. (2) Heterogeneity test: If P > 0.1 and I2 < 50%, the included studies were considered to be more homogeneous. Chi-square tests are performed to assess whether there is heterogeneity between studies. Carry out a fixed-effects model meta analysis; if P < 0.1, I2 > = 50%, and the included studies indicated heterogeneity, Examine a variety of sources, A random-effects model is used for meta analyses in the absence of clinical heterogeneity. Furthermore, a subgroup analysis was carried out to investigate possible differences in the qualitative attributes.
Results
Study characteristics and quality
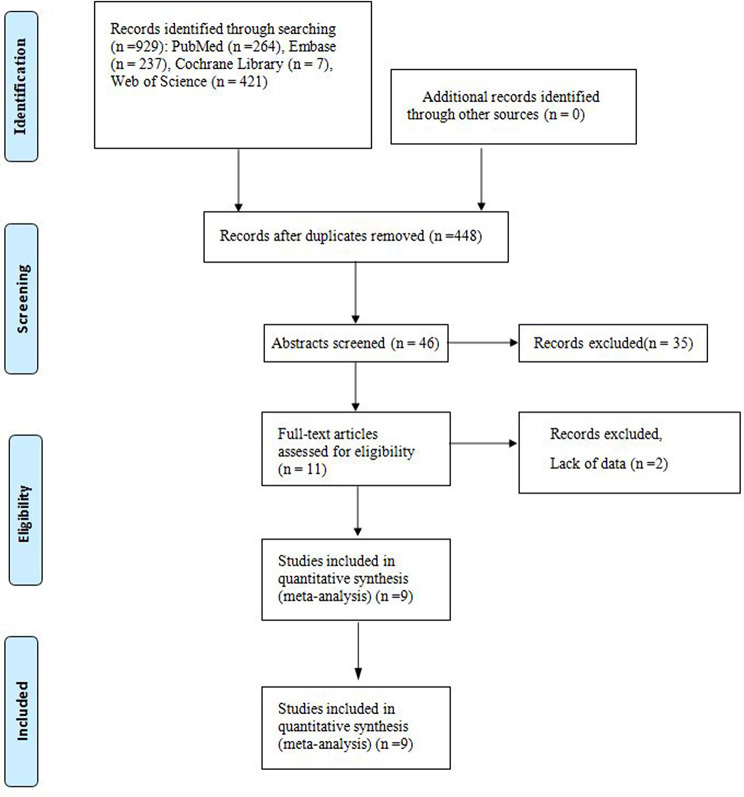
A total of 929 references were found using the search method. Based on the abstract and title, 46 studies were scanned after duplicate studies were eliminated. 11 studies were then assessed in depth. 2 records were removed after full text review for the following reasons Missing information (n = 2). In the end, this meta-analysis included 9 studies [18–26] (Table 1). This procedure is shown in the PRISMA statement flowchart. (Fig. 1).
Table 1.
The basic characteristics of the included studies
| Study(ref.) | Sample Size(T/C) | Man/Woman | Age (years)(Mean ± SD)(T/C) | T | C | Main Outcomes |
|---|---|---|---|---|---|---|
| Büchler, 2013 | 66/135 | 123/78 | 33.8 (11.9–62.7)/31.2 (16–54) | HA | OSD | ①④ |
| Bedi, 2011 | 30/30 | 60/0 | None | HA | OSD | ① |
| Botser, 2014 | 18/5 | 0/23 | 19(14–26) | HA | OSD | ①②③④⑤ |
| Domb, 2013 | 20/10 | 6/24 | 19.6/19 | HA | OSD | ①②③④ |
| González, 2020 | 31/26 | 39/18 | 41.23 ± 11.56/37.96 ± 7.09 | HA | OSD | ①④⑤ |
| Nepple, 2020 | 128/128 | 128/128 | 24.9 ± 9.2/24.9 ± 9.0 | HA | OSD | ②④⑤ |
| Rego, 2017 | 102/96 | 23/17 | 64.1 ± 7. 5/66.3 + 6.8 | HA | OSD | ⑤ |
| Roos, 2017 | 40/16 | 47/9 | 36.12 ± 8.7/35.76 ± 9.5 | HA | OSD | ①②③⑤ |
| Zingg, 2013 | 23/15 | 29/9 | 27.6 ± 8.4/28.9 ± 8.0 | HA | OSD | ①④⑤ |
Note T: trial group; C: control group. HA: Hip arthroscopy; OSD: Open Surgical Dislocation. ① Improvement of alpha angle; ② Modified Harris Hip Score (mHHS) after 12 months of follow-up; ③ Nonarthritic Hip Score (NAHS) after 12 months of follow-up; ④ Recurrence rate; ⑤ Complication rate
Fig. 1.
Flow chart of the article screening and selection process is shown. Based on the defined criteria, 9 studies were selected for this meta-analysis
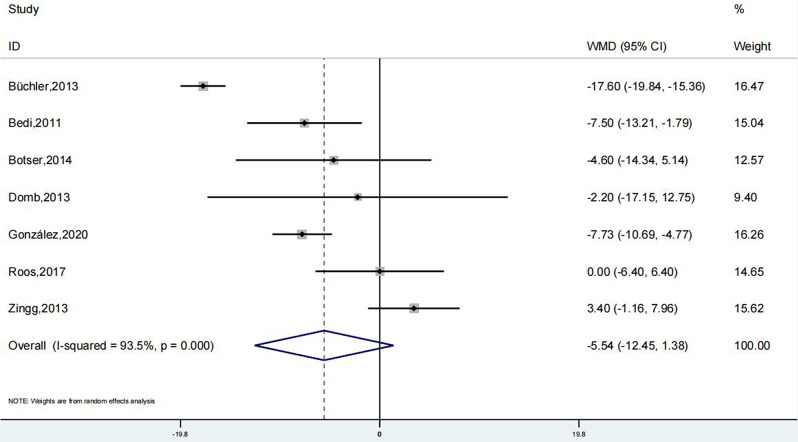
Alpha angle improvement by the Dunn view in patients with cam impingement from preoperation to postoperation
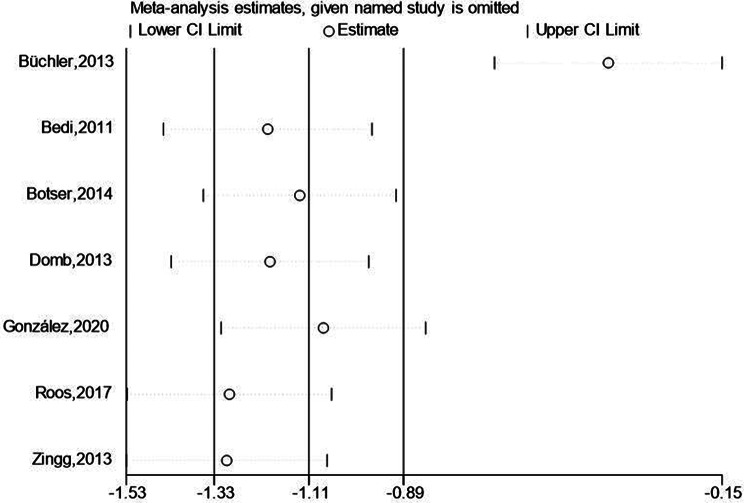
The findings of 7 studies showed that the alpha angle improvement of the hip arthroscopy treatment group and the surgical treatment group. Meta-analysis showed that the alpha angle improvement of the treatment group was lack of remarkable statistical significance (SMD: -5.54; 95% Cl: -12.45, 1.38; P = 0.117, Fig. 2) compared to the surgical treatment group. The study results were highly heterogeneous and sensitivity analysis was performed (Fig. 3). Patients with FA impingement treated with hip arthroscopy did not have a greater improvement in the alpha angle compared to the surgical treatment group. The Begg’s test is 1.000 and the Egger’s test is 0.129, so this study’s results are relatively stable and there is no obvious publication bias.
Fig. 2.
Forest illustration of the Improvement of alpha angle
Fig. 3.
Sensitivity analysis of the Improvement of alpha angle
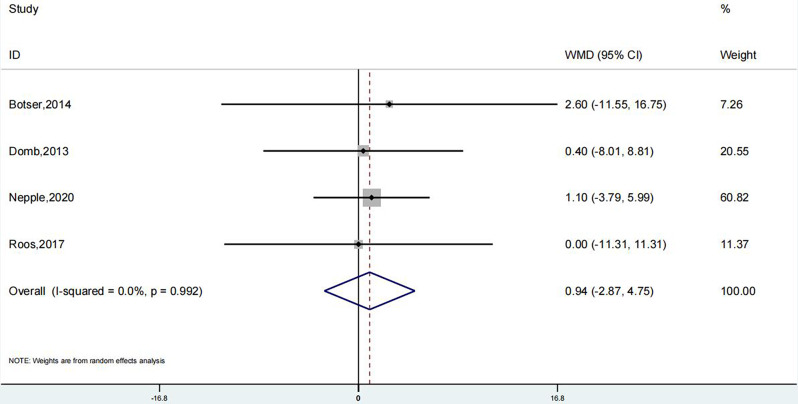
Meta-analysis of the modified Harris Hip Score (mHHS) after 12 months of follow-up
The results of 4 studies suggested that the mHHS after 12 months of follow-up of the Hip Arthroscopy treatment group and the surgical treatment group. Meta-analysis showed that the mHHS after 12 months of follow-up of the test group was no remarkable statistical significance (SMD: 0.94; 95% Cl: -2.87, 4.75; P = 0.629, Fig. 4) than the surgical treatment group. The trials results showed low heterogeneity, and a sensitivity analysis was conducted (Fig. 5). Compared with the surgical treatment group, hip arthroscopy in the treatment of patients with FA impingement did not increase the level of mHHS. The Begg’s Test is 1.000 and the Egger’s test is 0.979, so this research results are relatively stable and there is no obvious publication bias.
Fig. 4.
Forest illustration of the Modified Harris Hip Score (mHHS) after 12 months of follow-up
Fig. 5.
Sensitivity analysis of the Modified Harris Hip Score (mHHS) after 12 months of follow-up
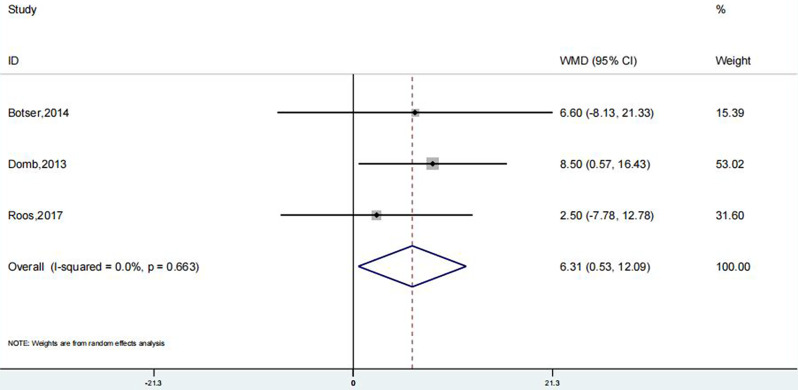
Nonarthritic hip score (NAHS) after 12 months of follow-up
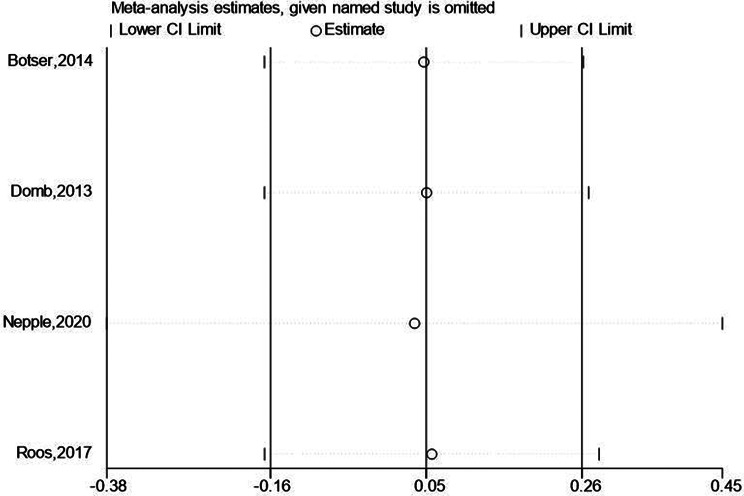
The results of 3 studies suggested that the NAHS of the Hip Arthroscopy treatment group and the surgical treatment group. Meta-analysis showed that the NAHS of the Hip Arthroscopy treatment group was remarkably greater compared to surgical treatment group (SMD: 6.31; 95% Cl: 0.53, 12.09; P = 0.032, Fig. 6).The trials results showed low heterogeneity, and a sensitivity analysis was conducted (Fig. 7). In comparison to the surgical treatment group, hip arthroscopy in the treatment of patients with FA impingement increase the level of NAHS. The Begg’s Test is 1.000 and the Egger’s test is 0.740, so this research results are relatively stable and there is no obvious publication bias.
Fig. 6.
Forest illustration of the Nonarthritic Hip Score (NAHS) after 12 months of follow-up
Fig. 7.
Sensitivity analysis of the Nonarthritic Hip Score (NAHS) after 12 months of follow-up
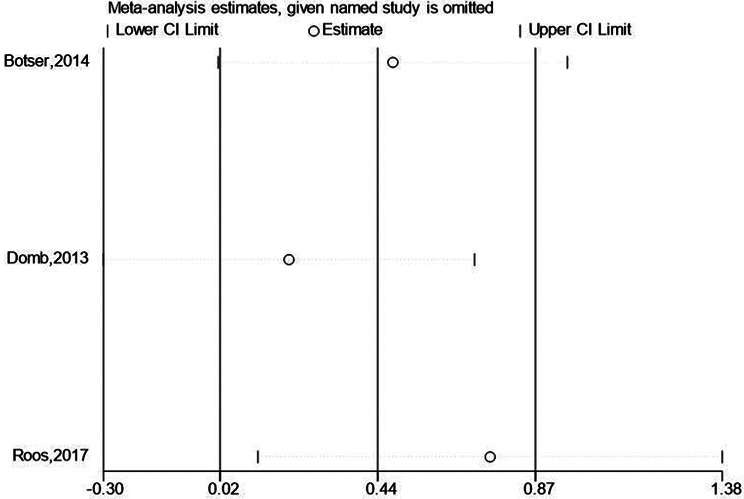
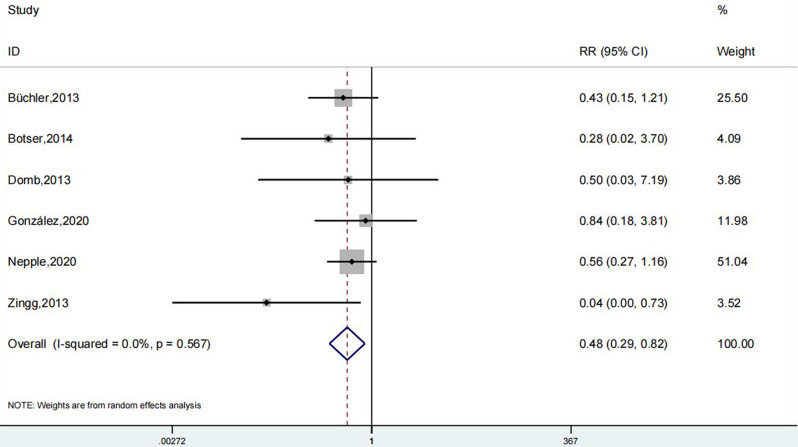
Recurrence rate
The results of 6 studies suggested that the recurrence rate of the Hip Arthroscopy treatment group and the surgical treatment group. Meta-analysis showed that the rate of recurrence of the Hip Arthroscopy treatment group was remarkably lesser compared to the surgical treatment group (OR: 0.48; 95% Cl: 0.29, 0.82; P < 0.01, Fig. 8).The trials results showed low heterogeneity, and a sensitivity analysis was conducted (Fig. 9). In comparison to surgical treatment group, FA impingement patients are treated with hip arthroscopy decrease the level of recurrence rate. The Begg’s Test is 0.260 and the Egger’s test is 0.265, so this research results are relatively stable and there is no obvious publication bias.
Fig. 8.
Forest illustration of the recurrence rate
Fig. 9.
Sensitivity analysis of the recurrence rate
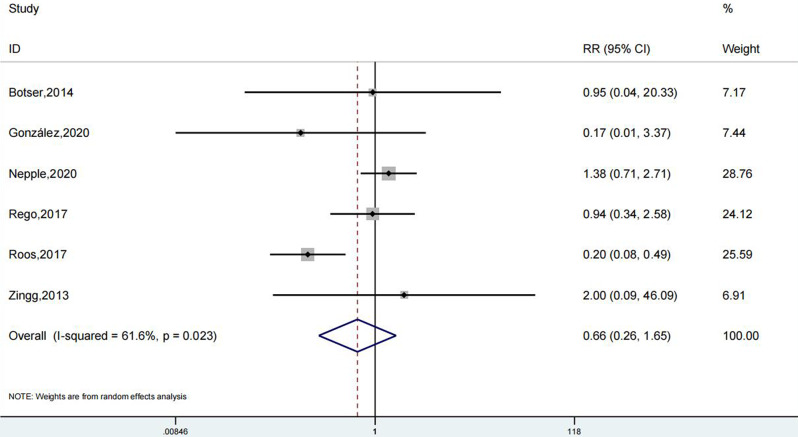
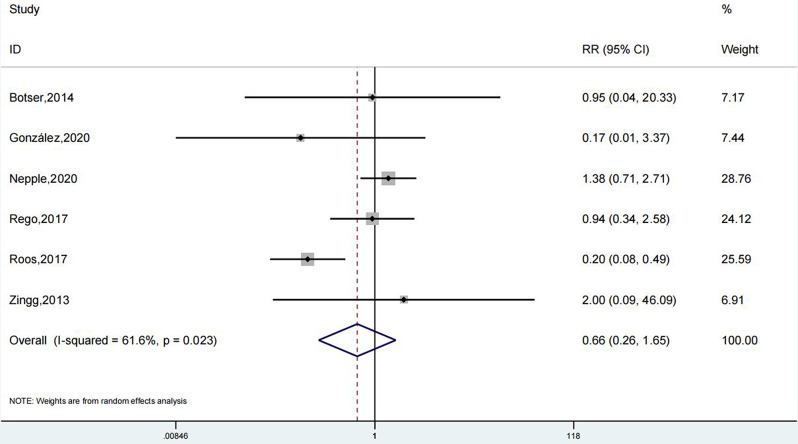
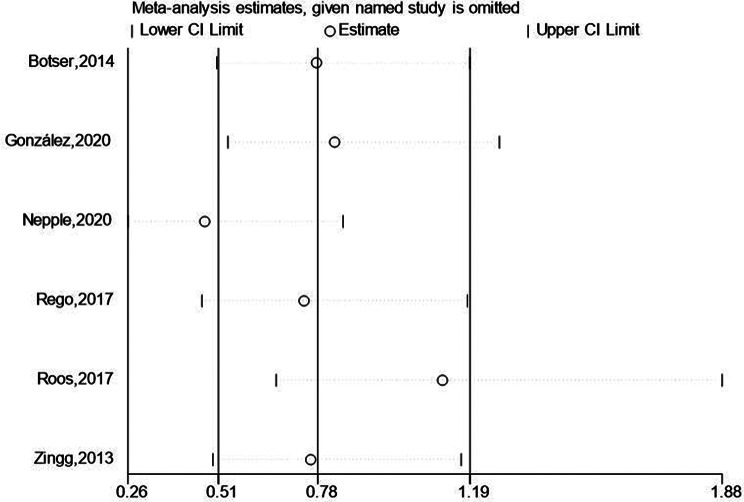
Complication rate
The results of 6 studies revealed that the Complication rate of the Hip Arthroscopy treatment group and the surgical treatment group. Meta-analysis showed that the Complication rate of the Hip Arthroscopy treatment group was no remarkable statistical significance (OR: 0.66; 95% Cl: 0.26, 1.65; P = 0.372, Fig. 10) than the surgical treatment group. The trials results showed high heterogeneity and a sensitivity analysis was carried out (Fig. 11). In comparison to the surgical treatment group, hip arthroscopy in the treatment of patients with FA impingement did not decrease the level of Complication rate. The Begg’s Test is 1.000 and the Egger’s test is 0.769, so this research results are relatively stable and there is no obvious publication bias.
Fig. 10.
Forest illustration of the Complication rate
Fig. 11.
Sensitivity analysis of the Complication rate
Discussion
The objective of this study was to evaluate the efficacy and safety of hip arthroscopy versus open surgical dislocation in the treatment of femoro-hip impingement syndrome (FAI) through published clinical trials. Among the 9 studies included in this meta-analysis, there was no statistically significant difference in α Angle improvement between the hip arthroscopy group and the open surgery group (SMD: -5.54; 95% CI: -12.45,1.38; P = 0.117). At 12 months follow-up, the modified Harris Hip Score (mHHS) in the hip arthroscopy group (SMD: 0.94; 95% CI: -2.87,4.75; P = 0.629) and non-arthritic hip score (NAHS) (SMD:6.31; 95% CI: 0.3,12.09; P = 0.032) showed some improvement, but only the improvement of NAHS was statistically significant. In addition, the rate of recurrence in the hip arthroscopy group (OR: 0.48; 95% CI: 0.29,0.82; P < 0.01) was significantly lower than that of the open surgery group, and the complication rate (OR: 0.66; 95% CI: 0.26,1.65; P = 0.372) had no significant difference. These results suggest that hip arthroscopy may be an effective treatment option for patients with FAI. However, due to the uneven quality of the included studies and the fact that some of the results did not reach statistical significance, these conclusions need to be further validated with more high-quality studies.
Alpha angle is the most common parameter used to define cam-femoral acetabular impingement (FAI) [15]. Some studies have further found that alpha Angle is the most effective parameter for CAM-impingement FAI MRI. The results show that the alpha Angle of CAM-impingement FAI can be accurately restored to a minimum of 55° [16, 17]. Thus improving the prognosis of patients. The alpha Angle is a good predictor of efficacy and is a simple, repeatable, and inexpensive guide that can be used during and after surgery [18]. This meta-analysis found no increase in α Angle improvement in patients with FA impingement who underwent hip arthroscopy compared to the surgical treatment group. This is contrary to the findings of a meta-analysis by Zhang et al., who suggested that open surgical dislocation led to a significant improvement in the Dunn Angle of cam osteoplasty patients from pre-op to post-op compared to hip arthroscopy [19]. Interestingly, Papalia et al. ‘s meta-analysis was consistent with our study and found no difference between the two methods at the alpha Angle [20].
The Non-arthritic Hip Score (NAHS) questionnaire, which is often used to assess hip joints in younger patients, has 20 items divided into four sections: pain, symptoms, function, and activity [21]. Multiple studies using NAHS to assess non-arthritic hip pain and functional recovery after hip surgery consistently found significant improvements in NAHS after hip arthroscopy [23–25]. Unfortunately, these studies did not compare NAHS after hip arthroscopy with that after open surgical dislocation. Our meta-analysis of results found a statistical difference in NAHS between the two groups.
In contrast, the results of our study’s meta-analysis showed no statistically significant difference in alpha angle improvement between hip arthroscopy and surgical treatment groups. While hip arthroscopy did result in satisfactory alpha angle improvement, the difference was not significant (SMD: -5.54; 95% CI: -12.45, 1.38; P = 0.117). This suggests that both treatments may be effective in improving the alpha angle, but the magnitude of improvement may not differ significantly between the two.
Regarding the Modified Harris Hip Score (mHHS) after 12 months of follow-up, both meta-analyses found no significant difference between hip arthroscopy and surgical treatment groups. This indicates that both treatments may result in similar functional outcomes in terms of hip function and mobility. However, when it comes to NAHS after 12 months of follow-up, the results of this study’s meta-analysis showed that hip arthroscopy resulted in a significantly higher NAHS compared to surgical treatment (SMD: 6.31; 95% CI: 0.53, 12.09; P = 0.032). This suggests that hip arthroscopy may provide better pain relief and quality of life outcomes than open surgical dislocation.
Recurrence rate is an important index to evaluate the effectiveness and safety of any operation [25]. The study found a significant increase in the number of patients who relapsed after surgical dislocation compared to hip arthroscopy [25]. Another meta-analysis found that hip arthroscopic recurrence rates were significantly lower than open surgical dislocation [19]. However, in our meta-analysis, there was no difference in recurrence rates between the two groups, which may also be due to the inclusion of results from different studies.
Finally, both meta-analyses found no significant difference between hip arthroscopy and surgical treatment groups. This suggests that both treatments may have similar risks of complications, such as nerve damage, wound infection, and wound dehiscence.In conclusion, while both hip arthroscopy and open surgical dislocation may be effective treatments for FAI, the results of this study’s meta-analysis suggest that hip arthroscopy may provide better pain relief and quality of life outcomes, as well as a lower risk of recurrence, compared to surgical treatment. However, it is important to note that the choice of treatment should be based on individual patient factors and the expertise of the surgeon.
Limitations
The meta-analysis of this study is subject to several limitations. Firstly, the scarcity of randomized controlled trials (RCTs) in the field necessitated the inclusion of controlled clinical trials, potentially diminishing the robustness of our conclusions. Secondly, while the search strategy employed an exhaustive and comprehensive approach across CENTRAL, PUBMED, and EMBASE databases, not all pertinent studies were captured, primarily due to publication bias, which might have obscured significant differences in outcomes between the two treatments. Thirdly, the limited number of trials in each analysis and the absence of treatment provider blinding introduce potential detection bias. Lastly, the insufficient provision of outcome data (such as standard deviations) by the included studies required the application of statistical methods to estimate missing data.
Conclusion
Our results suggest that hip arthroscopy may be an effective treatment for patients with femoro-hip impingement syndrome (FAI). Through 12 months of follow-up, we observed improvements in alpha Angle, improved Harris hip score (mHHS) and non-arthritic hip score (NAHS), and reduced rates of resurgery. However, with the exception of the statistically significant improvement in NAHS, most of the other results did not reach statistical significance. Therefore, these conclusions need to be further validated by more high-quality studies.
Acknowledgements
We would like to thank the reviewers for their valuable suggestions.
Author contributions
Haibo Yin designed the study. Chenlie Ni wrote the original draft. Haiqing Lin collected raw data. Haiqing Lin performed statistical and bioinformatics analyses. Haibo Yin supervised the study.
Funding
No funding was received for this study.
Data availability
The data used to support this study are available from the corresponding author upon request.
Declarations
Human ethics and consent to participate
Not applicable.
Consent to publish
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Matar HE, Rajpura A, Board TN. Femoroacetabular impingement in young adults: assessment and management. Br J Hosp Med (Lond). 2019;80(10):584–8. [DOI] [PubMed] [Google Scholar]
- 2.Cannon J, Kulig K, Weber AE, Powers CM. Gluteal activation during squatting reduces acetabular contact pressure in persons with femoroacetabular impingement syndrome: a patient-specific finite element analysis. Clin Biomech (Bristol). 2023;101:105849. [DOI] [PubMed] [Google Scholar]
- 3.Pennock AT, Bomar JD, Johnson KP, Randich K, Upasani VV. Nonoperative Management of Femoroacetabular Impingement: a prospective study. Am J Sports Med. 2018;46(14):3415–22. [DOI] [PubMed] [Google Scholar]
- 4.Hale RF, Melugin HP, Zhou J, LaPrade MD, Bernard C, Leland D, Levy BA, Krych AJ. Incidence of Femoroacetabular Impingement and Surgical Management Trends over Time. Am J Sports Med. 2021;49(1):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheney CW, Ahmadian A, Brennick C, Zheng P, Mattie R, McCormick ZL, Nagpal A. Radiofrequency ablation for Chronic Hip Pain: a Comprehensive, Narrative Review. Pain Med. 2021;22(Suppl 1):S14–9. [DOI] [PubMed] [Google Scholar]
- 6.Aiyer R, Noori SA, Chang KV, Jung B, Rasheed A, Bansal N, Ottestad E, Gulati A. Therapeutic Ultrasound for Chronic Pain management in joints: a systematic review. Pain Med. 2020;21(7):1437–48. [DOI] [PubMed] [Google Scholar]
- 7.Sankar WN, Matheney TH, Zaltz I. Femoroacetabular impingement: current concepts and controversies. Orthop Clin North Am. 2013;44(4):575–89. [DOI] [PubMed] [Google Scholar]
- 8.Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27(2):252–69. [DOI] [PubMed] [Google Scholar]
- 9.Botser IB, Smith TW Jr, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27(2):270–8. [DOI] [PubMed] [Google Scholar]
- 10.Sponseller PD, Jones KB, Ahn NU, Erkula G, Foran JR, Dietz HC 3. Protrusio acetabuli in Marfan syndrome: age-related prevalence and associated hip function. J Bone Joint Surg Am. 2006;88(3):486–95. [DOI] [PubMed]
- 11.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–6. [PubMed] [Google Scholar]
- 12.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85(2):278–86. [DOI] [PubMed] [Google Scholar]
- 13.Büchler L, Neumann M, Schwab JM, Iselin L, Tannast M, Beck M. Arthroscopic versus open cam resection in the treatment of femoroacetabular impingement. Arthroscopy. 2013;29(4):653–60. [DOI] [PubMed] [Google Scholar]
- 14.Kahlenberg CA, Nwachukwu BU, Schairer WW, McCormick F, Ranawat AS. Patient satisfaction reporting for the Treatment of Femoroacetabular Impingement. Arthroscopy. 2016;32(8):1693–9. [DOI] [PubMed] [Google Scholar]
- 15.Bedi A, Zaltz I, De La Torre K, Kelly BT. Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med. 2011;39(Suppl):S20–8. [DOI] [PubMed] [Google Scholar]
- 16.de Sa D, Urquhart N, Philippon M, Ye JE, Simunovic N, Ayeni OR. Alpha angle correction in femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):812–21. [DOI] [PubMed] [Google Scholar]
- 17.Carreira D, Kurapatti M. Editorial Commentary: Cam Femoroacetabular Impingement requires dynamic Assessment of Beta-Angle (Femoroacetabular Excursion Angle) and consideration of femoral and Acetabular Version: Cam Impingement in patients with Acetabular or femoral Retroversion May Warrant Greater Osteoplasty. Arthroscopy. 2023;39(9):2023–5. [DOI] [PubMed] [Google Scholar]
- 18.Ayeni OR, Banga K, Bhandari M, Maizlin Z, de Sa D, Golev D, Harish S, Farrokhyar F. Femoroacetabular impingement in elite ice hockey players. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):920–5. [DOI] [PubMed] [Google Scholar]
- 19.Hummer ET, Murphy EN, Suprak DN, Brilla LR, San Juan JG. Movement direction impacts knee joint kinematics during elliptical exercise at varying incline angles. Knee. 2021;29:201–7. [DOI] [PubMed] [Google Scholar]
- 20.Zhang D, Chen L, Wang G. Hip arthroscopy versus open surgical dislocation for femoroacetabular impingement: a systematic review and meta-analysis. Med (Baltim). 2016;95(41):e5122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papalia R, Del Buono A, Franceschi F, Marinozzi A, Maffulli N, Denaro V. Femoroacetabular impingement syndrome management: arthroscopy or open surgery? Int Orthop. 2012;36(5):903–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maldonado DR, Padmanabhan S, George T, Domb BG. Defining the percent thresholds for achieving the Maximum Outcome Improvement of the Modified Harris hip score, the non-arthritic hip score, the hip outcome score-sports Subscale, the Visual Analog Scale for Pain, and the International Hip Outcome Tool-12 in revision hip arthroscopy at Minimum 2-Year Follow-Up. Arthroscopy. 2024;40(4):1143–52. [DOI] [PubMed] [Google Scholar]
- 23.Portet A, Lambrey PJ, Benhenneda R, Tanel L, Bauwens PH, Thaunat M. Short-term functional outcomes of Whiteside transfer for massive rupture of gluteus medius tendon in native hips. Int Orthop. 2024;48(1):57–64. [DOI] [PubMed] [Google Scholar]
- 24.Orner CA, Haws BE, Reuter J, Kenney R, Cook PC, Giordano BD. Patient-reported outcomes are similar in the first 2 years after staged Versus Combined Hip Arthroscopy and Periacetabular Osteotomy for Hip Dysplasia. Arthroscopy. 2023;39(8):1857–65. [DOI] [PubMed] [Google Scholar]
- 25.Shankar DS, Bi AS, Buldo-Licciardi M, Rynecki ND, Akpinar B, Youm T. Five-year outcomes of primary hip arthroscopy for Femoroacetabular Impingement Syndrome among female patients: higher body Mass Index is Associated with reduced clinically significant outcomes. Arthroscopy. 2024;40(3):732–41. [DOI] [PubMed] [Google Scholar]
- 26.Li T, Mei L, Xu Y, Cao Y, Shi X, Chen G, Li J. Total hip arthroplasty or arthroscopy for pigmented Villonodular synovitis of the hip: a retrospective study with 3-Year Follow-Up at Minimum. Orthop Surg. 2023;15(6):1498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris JD, Erickson BJ, Bush-Joseph CA, Nho SJ. Treatment of femoroacetabular impingement: a systematic review. Curr Rev Musculoskelet Med. 2013;6(3):207–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support this study are available from the corresponding author upon request.