Abstract
The diverse radiation types in medical treatments and the natural environment elicit complex biological effects on both cancerous and non-cancerous tissues. Radiation therapy (RT) induces oncological responses, from molecular to phenotypic alterations, while simultaneously exerting toxic effects on healthy tissue. N6-methyladenosine (m6A), a prevalent modification on coding and non-coding RNAs, is a key epigenetic mark established by a set of evolutionarily conserved enzymes. The interplay between m6A modification and radiobiology of cancerous and non-cancerous tissues merits in-depth investigation. This review summarizes the roles of m6A in the biological effects induced by ionizing radiation and ultraviolet (UV) radiation. It begins with an overview of m6A modification and its detection methods, followed by a detailed examination of how m6A dynamically regulates the sensitivity of cancerous tissues to RT, the injury response in non-cancerous tissues, and the toxicological effects of UV exposure. Notably, this review underscores the importance of novel regulatory mechanisms of m6A and their potential clinical applications in identifying epigenetically modulated radiation-associated biomarkers for cancer therapy and estimation of radiation dosages. In conclusion, enzyme-mediated m6A-modification triggers alterations in target gene expression by affecting the metabolism of the modified RNAs, thus modulating progression and radiosensitivity in cancerous tissues, as well as radiation effects on normal tissues. Several promising avenues for future research are further discussed. This review highlights the importance of m6A modification in the context of radiation biology. Targeting epi-transcriptomic molecules might potentially provide a novel strategy for enhancing the radiosensitivity of cancerous tissues and mitigating radiation-induced injury to normal tissues.
Keywords: Radiation biology, m6A modification, epi-transcriptome, cancer, non-cancer
Introduction
RNA modifications have garnered significant attention over an extensive historical period since their initial identification1. The N6-methyladenosine (m6A) base was first reported in bacteria and yeast in 19582,3, and the mRNA m6A sequence motif was discovered in the 1970s4–6. However, the methyltransferase METTL3 was not identified until the 1990s7. A major breakthrough came in 2012, with the development of a novel method combining RNA immunoprecipitation and next-generation sequencing8, which enabled comprehensive mapping of this post-transcriptional modification. To date, more than 150 chemical modifications have been identified across various cellular RNAs, including N1 (or N6)-methyladenosine (m1A or m6A), N6, 2′-O-dimethyladenosine (m6Am), inosine, 5-methylcytidine (m5C), N4-acetylcytidine (ac4C), 2′-O-methylated nucleotide (Nm), pseudouridine (Ψ), and internal N7-methylguanosine (m7G). These modifications, particularly m6A, have introduced a new paradigm for genetic regulation that has enriched the framework of the central dogma in molecular biology.
Substantial research has revealed the interplay between RNA m6A modification and diverse physiological and pathological processes, including cancer. Aberrant m6A modification, mediated by specific enzymes, has been shown to have tumor promoting or suppressing activity. Given the role of radiation therapy (RT) as a classical treatment method used alongside surgery, chemotherapy, and immunotherapy, the link between m6A and tumorigenesis makes this modification relevant to cancer radiation biology9. Radiation-responsive m6A-modified genes might serve as potential diagnostic or therapeutic targets facilitating the development of strategies to sensitize tumors to radiation. In cancer irradiation, normal tissues inevitably experience iatrogenic radiation exposure during RT, medical workers face occupational radiation exposure, and organisms in the environment are exposed to radioactivity after nuclear accidents. Radiation’s adverse effects encompass a wide range of injuries, including those affecting the skin10, hematopoietic system11, gastrointestinal system12, lungs13, neurological system14, and reproductive system15. These effects are closely associated with molecular, cellular and tissue responses. Genetic transformation after radiation exposure, often associated with epigenetics, has been extensively studied16,17. The epigenetic modifications that occur under low-dose irradiation, because of the sensitivity and dynamic nature of epigenetic components, are particularly noteworthy. In this regard, illustrating the interplay between m6A modification and radiation effects on normal tissues is important in the context of the ongoing Fukushima nuclear contaminated water discharge plan.
Emerging evidence implicates RNA m6A modification in radiation biology. Cancer occurrence and development are accompanied by a series of biological events. RT aimed at curbing cancer growth can restore the aberrant expression status of m6A regulators, including “writer”, “eraser”, and “reader” enzymes, as well as their target genes, which are involved in multiple cellular events such as apoptosis18, ferroptosis19, proliferation20, stem cell self-renewal21, and the tumor microenvironment (TME)22, in an m6A-dependent manner. Thus, RNA m6A modification plays crucial roles in tumor radiation resistance and the efficacy of sensitization approaches. Furthermore, m6A modification participates in radiation-induced biological effects, such as DNA damage repair23, apoptosis24, pyroptosis25, inflammation26, and epithelial-to-mesenchymal transition (EMT)27 of normal tissues, and consequently influences radioactive injury effects.
Despite the importance of RNA m6A modification across various life domains, the interplay between RNA m6A modification and radiation biology in the context of cancerous and non-cancerous tissues remains understudied. This review provides a comprehensive overview of the regulatory roles of RNA m6A modification in ionizing radiation (IR)- and ultraviolet (UV) radiation-induced biological effects. It includes a brief introduction to this modification and its detection methods, as well as an exploration of the regulatory mechanisms of m6A on diverse RNAs involved in cancer sensitivity to RT, non-cancer radiation injury, and UV-related toxicity. This review emphasizes the importance of novel regulatory mechanisms involving m6A and their potential applications in estimating radiation dosage, screening for epigenetic radiation-associated biomarkers, or serving as therapeutic targets in precision therapy. Additionally, potential directions for future research are proposed, to shed light on the importance of RNA m6A modification in cancer and non-cancer radiation biology, and expand the research field of epigenetic modifications.
RNA m6A modification
Epigenetics refers to the study of heritable changes in gene expression that do not involve alterations in the DNA sequence; examples include DNA methylation, RNA editing, histone modification, maternal effects, and genomic imprinting28. All RNA modifications collectively form a new level of gene expression regulation known as the epi-transcriptome. Among the numerous RNA modifications, m6A is the most prevalent post-transcriptional modification in eukaryotic messenger RNAs (mRNAs) and non-coding RNAs—including long noncoding RNAs (lncRNAs), circular RNAs (circRNAs), ribosomal RNAs (rRNAs), transfer RNAs (tRNAs), and small nuclear RNAs (snRNAs)—accounting for more than 60% of the total RNA modifications29–32.
m6A is formed by the addition of a methyl group to the sixth nitrogen atom of adenosine in RNA and is observed across diverse organisms including bacteria and mammals, thus demonstrating evolutionary conservation33,34. Accumulating evidence indicates that m6A modification, governed by specific enzymes, affects virtually every step in the RNA lifecycle, including transcription, splicing, polyadenylation, translation, nuclear export, RNA localization, stability, turnover, the DNA damage response, apoptosis, and chromatin assembly35,36.
Abnormal m6A modification is closely associated with the activation and inhibition of signaling pathways involved in various physiological and pathological processes37,38. According to previous reports, m6A modification plays roles in gametogenesis and pregnancy28, embryonic development39, stem cell renewal and differentiation40, neurogenesis41, and immunity42,43. Moreover, m6A modification has been implicated in a variety of human diseases, including obesity44,45, cardiovascular disease46, metabolic disease47, neuropsychiatric disorders48, viral infection49,50, preeclampsia51, kidney disease52, steatotic liver disease53, rheumatoid arthritis54, and a wide variety of cancers55,56.
Thus, RNA m6A modification is a versatile player across biological kingdoms that influences a wide range of cellular functions and disease states.
Writers, erasers, and readers of RNA m6A modifications
The conserved m6A modification motif DRACH (D = G/A/U, R = G/A, H = A/U/C), frequently identified around the stop codon or in 3′-untranslated regions (3′-UTRs) by whole-transcriptome m6A mapping, is maintained by 3 classes of regulators: writers, erasers, and readers34. Writers and erasers add or remove the methyl group in the motif, respectively, and consequently determine RNA methylation level, whereas the readers recognize m6A modification and mediate the recruitment of downstream functional complexes, which influence the fate of modified RNAs57–60.
The m6A methyltransferase complex adds methyl groups to the adenine nucleotides of RNA transcripts. Within this complex, methyltransferase-like 3 (METTL3) binds S-adenosylmethionine (SAM) and forms a stable dimer with methyltransferase-like 14 (METTL14), which has a substrate recognition function and is a core component of the methyltransferase complex61. Wilms’ tumor 1-associated protein (WTAP) is a crucial bridging protein that interacts with METTL3 and METTL14 in the complex, combines with other components, and forms a functional unit62. Vir-like m6A methyltransferase-associated protein (VIRMA) (KIAA1429) recruits core components and regulates region-specific methylation63. Other essential components of the complex include zinc finger CCCH-type containing 13 (ZC3H13) and RNA binding motif protein 15/15B (RBM15/15B)32,62.
Substantial progress has recently been made in identifying enzymes mediating N6-adenosine methylation on non-coding RNAs (ncRNAs) and mRNAs. Zinc finger CCHC domain-containing protein 4 (ZCCHC4), methyltransferase-like 5 (METTL5), methyltransferase-like 16 (METTL16), and methyltransferase-like 4 (METTL4) are involved in the methylation of ncRNAs64–68. METTL5 and ZCCHC4 are the methyltransferases catalyzing m6A formation on 18S and 28S rRNA, respectively. Adenosines of the U2 and U6 spliceosomal snRNAs are m6Am or m6A methylated by METTL4 and METTL16, respectively69–72. METTL16 also catalyzes m6A modification of the SAM synthetase methionine adenosyltransferase 2A (MAT2A) mRNA71. Another evolutionarily conserved RNA methyltransferase, phosphorylated RNA polymerase II CTD interacting factor 1 (PCIF1), catalyzes further methylation at the N6 position if the first nucleoside of the nascent mRNA is adenosine, and subsequently generates the m6Am modification73–76.
m6A demethylases remove the methyl group from adenine nucleotides bearing m6A substrates, thereby providing insight into the dynamic potential of m6A. Two m6A demethylases have been identified in eukaryotes: the fat mass and obesity-associated protein (FTO)44 and α-ketoglutarate-dependent dioxygenase homolog 5 (ALKBH5)77. Both demethylases contain a similar catalytic center using ferrous iron as a cofactor and α-ketoglutarate as a co-substrate.
The m6A modification recognition enzymes recognize and ensure the diverse biological functions of various m6A motifs, thus influencing the binding between RNA and RNA-binding proteins78. The YT521-B homology (YTH) domain family is the most conventional reader in eukaryotes. Each member of this family contains a conserved C-terminal domain that recognizes RNA and a variable N-terminal domain that binds RNA79. This family is present in both the cytoplasm (YTH N6-methyladenosine RNA binding protein 1/2/3, YTHDF1/2/3) and the nucleus (YTH domain-containing protein 1/2, YTHDC1/2)80. Specifically, YTHDF2 shows selective binding to mRNAs carrying m6A and delivers them to cellular RNA decay sites60. YTHDF3 forms complexes with YTHDF1 that increase RNA translation, as well as complexes with YTHDF2 that accelerate RNA degradation81,82. YTHDC1 is responsible for RNA splicing and export from the nucleus83,84, whereas YTHDC2 is involved in the translation of specific target RNAs85. Other common readers include heterogeneous nuclear ribonucleoproteins86, fragile X messenger ribonucleoprotein (FMRP)87, and insulin-like growth factor 2 mRNA-binding proteins (IGF2BPs)88.
An outline of the identified m6A writers, erasers, and readers, and their corresponding functions is depicted in Figure 1.
Figure 1.
Outline of the identified writers, erasers, and readers and their corresponding functions in the dynamic and reversible m6A modification process (created in Figdraw). m6A modification is governed by a series of enzymes. Writers are m6A methyltransferases including METTL3, METTL14, WTAP, KIAA1429, RBM15/RBM15B, ZC3H13, METTL16 [catalyzes m6A methylation of the S-adenosylmethionine (SAM) synthetase methionine adenosyltransferase 2A (MAT2A) mRNA], and PCIF1 (catalyzes further methylation at the N6 position if the first nucleoside of the nascent mRNA is adenosine, thus generating the m6Am modification), which add methyl groups from the SAM substrate to adenine nucleotides of mRNAs in the nuclear speckles. In addition, ZCCHC4 (28S rRNA), METTL5 (18S rRNA), METTL4 (U2 spliceosomal snRNAs), and METTL16 (U6 spliceosomal snRNAs) are involved in the methylation of ncRNAs. The m6A erasers are demethylases including FTO and ALKBH5; these enzymes use ferrous iron as a cofactor and α-ketoglutarate as a co-substrate. They remove the methyl group from adenine, thus providing a dynamic counterbalance of m6A on the transcripts. Reader proteins recognize the m6A site, and consequently ensure the binding of RNA and RNA-binding proteins, and coordinate the diverse biological functions of distinct methylated transcripts. Readers have been implicated in directing the fate of RNA metabolism—such as splicing (YTHDC1 and HNRNPC), nuclear export (YTHDC1), decay (YTHDF2/3 and YTHDC2), stability (IGF2BP1/2/3), translation (YTHDF1/3, YTHDC2 and FMRP), and miRNA processing (HNRNPA2B1)—and typically have multiple roles.
RNA m6A modification detection methods
Although research on RNA modification began in the 1970s, no substantial progress was made until the development of a novel approach combining RNA immunoprecipitation and next-generation sequencing in 20128. With the continued advancement of existing techniques and the advent of new technologies, the study of m6A modification has great potential in uncovering novel biological regulatory mechanisms and providing therapeutic targets. Here, we briefly introduce the currently available, mature, or exploratory methods for total m6A quantification and identification of m6A within genes.
For determination of overall m6A levels, mass spectrometry, colorimetry, and dot blot assays are frequently used. Among these methods, mass spectrometry is a rapid, low-cost, and relatively accurate approach with high sensitivity and good resolution; in addition, high-performance liquid chromatography can locate specific m6A residues89–92. A colorimetric method based on similar principles to classical enzyme-linked immunosorbent assays can easily detect global RNA m6A levels93. Dot blot assays can be used as a semi-quantitative method to identify m6A alterations in samples90,94. In addition, several novel m6A quantitative technologies have been developed, such as RNA photoactivatable-ribonucleoside-enhanced crosslinking and immunoprecipitation (PAR-CLIP), based on the incorporation of photoactivatable nucleoside analogs into nascent RNA89,95, and electrochemical immunosensors, a simple, sensitive and selective electrochemical method using gold nanoparticle modified glassy carbon electrodes (AuNP/GCE)89.
The development of a series of m6A identification technologies that are antibody-dependent or -independent has been a milestone in the m6A research field. For example, methylated RNA immunoprecipitation sequencing (MeRIP-seq), m6A-seq2, PA-m6A-seq, and m6A individual-nucleotide-resolution cross-linking and immunoprecipitation (miCLIP)-seq have been reported to detect m6A modifications with improved resolution from 100 nt to 200 nt, and eventually to single-base resolution 68,96–99. MeRIP-seq, the primary technology, combines methylated RNA fragments and high-throughput sequencing to detect m6A peaks with 100 nt to 200 nt resolution but is unable to precisely detect m6A sites. The m6A-seq2 method enhances m6A quantification at modification site, gene, or sample resolution. The PA-m6A-seq technique increases the resolution to 30 nt via 4SU strengthening cross-links. This method can access only m6A residues around 4SU operating sites, whereas miCLIP ultimately enhances the detection precision to single-base resolution. m6A-REF-seq can detect m6A sites in the whole transcriptome in an antibody-dependent manner100. DART-seq induces C-to-U deamination at sites adjacent to m6A bases101. m6A-label-seq marks methylation sites to achieve detection at a single-base resolution102. m6A-SEAL uses streptavidin beads to enrich biotin-labeled m6A-modified sites for subsequent sequencing and analysis103. m6A-LAIC-seq uses the spike-in External RNA Controls Consortium to quantitatively detect m6A presence104. SELECT precisely distinguishes m6A modified residues at single-base resolution, independently of antibody immunoprecipitation or isotope labeling105. SCARLET is a digestion-based method used to determine the percentage of m6A at single-nucleotide resolution for mRNAs and lncRNAs106.
Insights into RNA m6A modification in cancer radiation biology
Links between m6A modification and cancer RT
As a major treatment modality for tumors, RT is used in the early, late, or postoperative adjuvant stages of tumor treatment. Multiple cancer types are suitable for RT, primarily head and neck tumors, such as nasopharyngeal carcinoma (NPC), oral cancer, and throat cancer107; thoracic tumors, such as esophageal cancer, lung cancer, and breast cancer108; and pelvic and abdominal tumors, such as locally advanced colorectal cancer (CRC), gastric cancer, cervical cancer, and endometrial cancer in females, or penile and testicular cancer in males, and kidney cancer and bladder cancer of the urinary system109; certain bone metastases or brain metastases109; and soft tissue sarcomas of the extremities110. RNA m6A modification has emerged as an important regulator in radiation oncology, particularly in modulating the sensitivity of tumor cells to RT. The tumor-inhibitory effects of RT can restore the aberrant expression of m6A enzymes including writers, erasers, and readers, as well as the RNA m6A modification levels of target genes. The expression changes in various target RNAs in tumor tissues are reversed via the modulation of their stability, translation, splicing, and localization in an m6A-dependent manner. Consequently, RNA m6A modification contributes to radiation-mediated inhibitory or promoting effects on oncogenes or tumor suppressors, thereby modifying the responses of cancer cells to radiation, and potentially leading to resistance or sensitivity to RT treatment.
m6A modification of diverse RNAs in IR biology of cancer tissues
Importantly, the close relationship between m6A modification and neoplasms has implicated these modifications in cancer RT. Distinct types of RNAs, such as mRNAs, lncRNAs, circRNAs, and microRNAs (miRNAs), are modulated by m6A modification. Elucidating RNA m6A-mediated mechanisms in cancer radiation biology would facilitate improved therapeutic outcomes in clinical practice.
mRNAs
As the primary carriers of genetic information, mRNAs account for most m6A-annotated RNAs. The biological functions of many mRNAs regulated by m6A have been best elucidated in cancer. The particular role of m6A in cancer is exemplified by the regulation of 2 main classes of tumor-related genes: oncogenic genes and oncosuppressive genes32. m6A and its mediators collectively regulate all transcriptional and post-transcriptional regulatory processes, including processing, export, translation, and decay of mRNAs throughout their lifecycle111. Consequently, the expression levels of oncogenic genes or oncosuppressive genes are influenced, thereby determining the fate of cancer development. mRNA m6A modification is involved in cancer radiation sensitivity as well as the efficacy of radiotherapy. The m6A enzymes play major roles, which differ across different tumor types and mechanisms; these roles include affecting DNA damage and repair, regulating tumor cell stemness, and controlling the cell cycle, thus modulating the radioresistance of diverse tumors112.
First, the importance of m6A writers in the radiation sensitivity of various cancers has been reported. In pancreatic cancer cells, METTL3 promotes chemo- and radio-resistance, and METTL3-depleted cells show enhanced sensitivity to anticancer agents and irradiation113. Carbon-ion radiotherapy is a radical nonsurgical treatment with high local control rates and minimal serious adverse events114. Xu et al.114 have reported that METTL3 levels and mediation of m6A modification are elevated in non-small cell lung cancer (NSCLC) cells after carbon-ion radiotherapy. METTL3-mediated m6A modification of mRNA inhibits the decay of H2A histone family member X (H2AX) mRNA, enhances its expression, and consequently enhances DNA damage repair and cell survival114. Thus, METTL3-mediated m6A modification of mRNA contributes to the resistance to carbon-ion radiotherapy in NSCLC. Han and colleagues21 have shown that the recently identified methyltransferase METTL16 is aberrantly overexpressed in human acute myeloid leukemia (AML) cells, particularly in leukemia stem cells and leukemia-initiating cells. Mechanistically, METTL16 exerts its oncogenic role by promoting the expression of branched-chain amino acid (BCAA) transaminase 1 (BCAT1) and BCAT2 in an m6A-dependent manner and reprogramming BCAA metabolism in AML21. In endometrial carcinoma, protein arginine methyltransferase (PRMT) interacts with METTL14 and mediates its arginine methylation. Blocking PRMT enhances tumor suppression in response to cisplatin and RT, through a process involving ferroptosis [promoting methylation modification via an m6A-YTHDF2-dependent mechanism, and consequently decreasing glutathione peroxidase 4 (GPX4) mRNA stability]115. In breast cancer, neuropilin-1 (NRP1) enhances the stem cell properties and confers radioresistance to breast cancer cells. Mechanistically, NRP1 decreases IR-induced apoptosis by downregulating B-cell lymphoma-2 (Bcl-2) via WTAP-mediated m6A modification of Bcl-2 mRNA116.
Second, the roles of the m6A erasers FTO and ALKBH5 have been examined in the radiation sensitivity of NPC and hepatocellular carcinoma (HCC). Huang et al.19 have reported that the demethylase FTO erases the m6A modification of transcripts of OTUB1, a member of the ovarian tumor domain protease (OTU) subfamily of deubiquitinases (DUBs), thus promoting its expression, inhibiting the ferroptosis of cells induced by radiation, and ultimately triggering radiotherapy resistance in NPC. Chen et al.117 have revealed that irradiation upregulates ALKBH5 in hepatic stellate cells and consequently mediates monocyte recruitment; M2 polarization; and secretion of cysteine-cysteine motif chemokine ligand 20 (CCL20), which in turn upregulates ALKBH5 expression, thereby forming a positive feedback loop that promotes radiation-induced liver fibrosis (RILF) and decreases HCC radiosensitivity. This process involves the demethylation of Toll-interleukin 1 receptor domain-containing adaptor protein (TIRAP) mRNA and activation of its downstream NF-κB and JNK/Smad2 pathways117. The dual roles of ALKBH5 as a radiosensitization target and microenvironmental regulator provide new insights for RILF prevention and radiosensitization of HCC117.
Finally, m6A readers also play crucial roles in the radiation tolerance of myeloid-derived suppressor cells, cervical cancer, and lung adenocarcinoma (LUAD). A recent study has revealed the roles of YTHDF2 in tumor radiotherapy and immunotherapy22. YTHDF2 contributes to myeloid-derived suppressor cell (MDSC)-induced immunosuppression and treatment resistance to combined IR and/or anti-PD-L122. Specifically, IR induces immunosuppressive MDSC expansion and YTHDF2 expression in both humans and murine models. IR-induced YTHDF2 expression relies on NF-κB signaling, and YTHDF2 in turn leads to NF-κB activation, thus forming an IR-YTHDF2-NF-κB circuit22. Therefore, YTHDF2 is a promising target for improving radiotherapy and radiotherapy/immunotherapy combinations22. Du et al.118 have reported that YTHDF3 mediates regulation of cervical cancer radio-resistance by hepatocyte nuclear factor 1-alpha (HNF1-α) through promoting the translation of DNA repair protein RAD51 homologue 4 (RAD51D) in an m6A-dependent manner. In LUAD, Hao et al.119 have demonstrated that irradiation causes overexpression of Van Gogh-like protein 1 (VANGL1) through increasing its mRNA m6A levels; consequently, the detrimental effects of irradiation on LUAD are alleviated by protecting DNA from damage, probably through the activation of v-raf murine sarcoma viral oncogene homolog B1 (BRAF)/tumor protein p53 binding protein 1 (TP53BP1)/RAD51 cascades. IGF2BP2/3 facilitates VANGL1 mRNA stability and expression119. Elevated m6A levels of VANGL1 and diminished miR-29b-3p have been found to be responsible for VANGL1 overexpression after irradiation119.
Notably, deciphering novel mechanisms underlying classical molecular processes from a new perspective has contributed to illustrating key biological events. Targeting nuclear factor erythroid 2-related factor 2 (Nrf2), a key transcription factor well known to be responsible for tumor radio-resistance, is a promising strategy to enhance the radiation sensitivity of cancer120. The epi-transcriptomic regulation of Nrf2 in carcinogenesis has gained increasing attention in recent years. m6A-mediated Nrf2 RNA methylation has been reported to be associated with the upregulation of YTHDC2 as well as YTHDF1-3, and the downregulation of FTO and ALKBH5 in HepG2 human hepatoma cells121. Targeting Nrf2 by regulating m6A modification might therefore provide a new strategy for promoting cancer radiotherapy.
lncRNAs
LncRNAs are arbitrarily defined as non-coding transcripts longer than 200 nucleotides, encompassing RNAs transcribed by RNA polymerase I (Pol I), Pol II, and Pol III, as well as RNAs derived from processed introns122,123. LncRNA-annotated genes occupy a substantial portion of the genomes of complex organisms122. One important way in which lncRNAs function is as scaffolds or bridges for protein interactions, thus affecting the formation of protein complexes and regulating protein activity. They recruit chromatin-modifying factors that alter the levels of chromatin modification, and consequently influence gene transcription and expression124. LncRNA LINC00839, modified by METTL3-mediated m6A, maintains glioma stem cells and exerts radiation resistance by acting as a scaffold lncRNA; it promotes c-Src-mediated phosphorylation of β-catenin and subsequently activates the Wnt/β-catenin signaling pathway20. Additionally, Yin et al.125 have identified a lncRNA-RNA component of mitochondrial RNA processing endoribonuclease (RMRP) in NSCLC. The highly methylated RMRP promotes cancer stem cell properties and EMT, and enhances resistance to radiotherapy and cisplatin. Mechanistically, RMRP recruits Y-box binding protein 1 (YBX1) to the transforming growth factor beta receptor 1 (TGFBR1) promoter region, thereby resulting in upregulation of TGFBR1 transcription. The TGFBR1/SMAD2/SMAD3 pathway is also modulated by RMRP125. m6A RNA methylation-mediated RMRP stability has been found to drive the progression of NSCLC through regulating the TGFBR1/SMAD2/SMAD3 signaling pathway125.
circRNAs
Endogenous circRNAs are covalently closed RNA molecules that are more stable than linear RNAs, such as mRNA, miRNA, and lncRNA126. CircRNAs participate in gene expression regulation and perform various functions in plasma, exosomes, and urine126. Therefore, circRNAs are expected to serve as biomarkers and therapeutic targets for many tumors127. The mechanisms of circRNAs in human cancer are diverse, including acting as miRNA sponges, interacting with proteins, regulating gene splicing or transcription, being translated into proteins or peptides, and being involved in epigenetic regulation. m6A modification participates in the diverse functions of circRNAs, although current evidence remains limited127.
Shao et al.128 have identified and characterized circAFF2 as a novel m6A-modified circRNA that binds Cullin-associated NEDD8-dissociated protein 1 (CAND1), promotes the binding of CAND1 to Cullin1 and inhibits the neddylation of Cullin1 and subsequently enhances the radiosensitivity of CRC. Importantly, the regulation of circAFF2 involves ALKBH5-mediated m6A demethylation, followed by recognition and degradation via YTHDF2128. Thus, the ALKBH5/YTHDF2/circAFF2/Cullin-NEDD8 axis might serve as a potential radiotherapy target for CRC128. Zhong et al.129 have revealed that the expression of circ_0124554 is upregulated in CRC tissues and cells, and miR-1184 has been identified as a target of circ_0124554 and targeted LIM and SH3 protein 1 (LASP1). METTL3 mediates m6A modification of circ_0124554, promoting CRC progression and radio-resistance through the miR-1184/LASP1 pathway129. Moreover, m6A modification and its related enzymes affect the resistance of cancer to radiotherapy by regulating circRNAs, and METTL3 promotes the stabilization of circCUX1 through mediating its m6A modification130. Additionally, circCUX1 binds caspase-1 and inhibits its expression, thus decreasing inflammatory factor release and enhancing tolerance to radiotherapy in hypopharyngeal squamous cell carcinoma (HPSCC)130.
The roles of m6A modification and corresponding enzymes involving diverse RNAs in the IR sensitivity of cancer are listed in Table 1.
Table 1.
m6A modification of diverse RNAs involved in ionizing radiation biology in cancer tissues
| RNA type | Cancer | Enzyme | Target | Function |
|---|---|---|---|---|
| mRNAs | Pancreatic cancer | METTL3 | Ubiquitin-dependent process↓ | Promote chemo- and radio-resistance113 |
| NSCLC | METTL3 | H2AX↑ | Enhance DNA damage repair and cell survival, promoting radio-resistance114 | |
| AML | METTL16 | BCAT↑ | Drive leukemogenesis and leukemia stem cell self-renewal21 | |
| Endometrial carcinoma | METTL14 YTHDF2 |
GPX4↓ | Enhance tumor suppression in response to cisplatin and RT by blocking PRMT3115 | |
| Breast cancer | WTAP | Bcl-2↓ | Contribute to stemness and potentiate radioresistance via downregulation of Bcl-2 by NRP1116 | |
| NPC | FTO | OTUB1↑ | Inhibit ferroptosis and trigger radiotherapy resistance19 | |
| HCC | ALKBH5 | TIRAP↑ | Promote liver fibrosis (RILF) and decrease HCC radiosensitivity117 | |
| MDSC | YTHDF2 | Adrb2, Metrnl, smpdl3b↓ | Contribute to MDSC-induced immunosuppression and resistance to combined IR and/or anti-PD-L122 | |
| Cervical cancer | YTHDF3 | RAD51D↑ | Promote radioresistance of cervical cancer118 | |
| LUAD | IGF2BP2/3 | VANGL1↑ | Attenuate detrimental effects of irradiation on LUAD119 | |
| lncRNAs | Glioma | METTL3 YTHDF2 |
LINC00839↑ | Promote tumor progression and radiation resistance20 |
| NSCLC | METTL3 | RMRP (lncRNA-RNA component)↑ | Promote cancer stem cell properties and EMT, enhancing resistance to radiotherapy and cisplatin125 | |
| circRNAs | CRC | ALKBH5 YTHDF2 | circAFF2↓ | Decrease radiosensitivity128 |
| CRC | METTL3 | circ_0124554↑ | Promote progression and radioresistance129 | |
| HPSCC | METTL3 | circCUX1↑ | Enhance tolerance to RT130 |
↑: promotes, ↓: inhibits.
m6A modification with UV-induced radiation in cancer biology
UV radiation, a major carcinogen in the occurrence and development of all cutaneous cancer types131, is a common form of non-IR received by terrestrial organisms. UV can induce melanogenesis and even melanoma. Guo et al.132 have reported that UVB irradiation promotes global m6A modification in melanocytes and upregulates METTL3, thereby increasing the expression of YAP1 via m6A modification, activating the co-transcription factor TEA domain transcription factor 1 (TEAD1), and promoting melanogenesis. An early study on the importance of m6A modification in UV radiation focused on its function in the UV-induced DNA damage response133. Xiang et al.133, in 2017, reported that m6A modification in RNA is rapidly (within 2 min) and transiently induced at DNA damage sites in response to UV irradiation. This modification occurs on numerous poly(A)+ transcripts and is regulated by the methyltransferase METTL3 and the demethylase FTO133. Multiple DNA polymerases participate in the UV response, some of which resynthesize DNA after the lesion has been excised by the nucleotide excision repair pathway, whereas others are involved in trans-lesion synthesis and allow replication past damaged lesions during S phase133. DNA polymerase κ (Pol κ), which has been implicated in both nucleotide excision repair and trans-lesion synthesis, requires METTL3 for immediate localization to UV-induced DNA damage sites133. This notable finding indicates that m6A RNA serves as a beacon for the selective, rapid recruitment of Pol κ to damage sites, and consequently facilitates repair and cell survival133. Recently, the m6A reader protein YTHDC2 has been found to function in regulating UVB-induced DNA damage repair and histone modification H3K27me3; therefore, it may potentially serve as a biomarker in cutaneous squamous cell carcinomas131.
Insights into RNA m6A modification in non-cancer radiation biology
m6A modification participates in a wide variety of biological events. However, studies on the role of this modification in non-cancer radiation biology are relatively scarce. As a dynamic and reversible process, m6A modification responds sensitively to external stimuli133,134. Traditional viewpoints regarding the mechanisms underlying IR-induced injury are centered on the direct or indirect (via oxidative stress) effects causing breakage of DNA strands to varying degrees134,135. With the rapid advancement of epi-transcriptome research in recent years, unraveling novel epigenetic mechanisms from a post-transcriptional perspective is an important mission in radiobiology. To date, studies examining the roles of m6A modification in non-tumor radiation biology have focused on radiation-induced lung injury (RILI), radiation-induced liver disease (RILD), and radiation-induced hematopoietic injury (RIHI).
RILI
Occupational exposure to IR, such as exposure during radiological medical activities, can cause lung injury, denoted RILI136,137. Clinically, RILI is a common complication in some patients undergoing thoracic radiotherapy138,139. The biological roles of EMT in the pathogenesis of RILI have been widely documented. Feng et al.27 have detected markedly increased m6A levels, accompanied by upregulated METTL3 and downregulated ALKBH5, after IR-induced EMT. Forkhead box O1 (FOXO1) has been identified as a key target of METTL3, and its expression is downregulated by METTL3-mediated mRNA m6A modification in a YTHDF2-dependent manner, thus activating the AKT and ERK signaling pathways27. This study has shed light on the novel epigenetic mechanism involved in the pathogenesis of RILI. In parallel, Zhao et al.26 have revealed that zinc finger and BTB domain-containing protein 7B (Zbtb7b) suppresses aseptic inflammation in RILI. Mechanistically, Zbtb7b recruits the RNA demethylase ALKBH5 to interleukin-6 (IL-6) mRNA, and subsequently demethylates m6A modification of IL-6 mRNA and inhibits its nuclear export26. Thus, Zbtb7b epigenetically suppresses irradiation-induced IL-6 production through inhibiting the m6A modification and nucleocytoplasmic transport of IL-6 mRNA in the lungs26.
RILD
RILD is a complication of HCC radiotherapy. Chen et al.140 have found that ALKBH5-modified human high-mobility group box-1 (HMGB1)/stimulator of interferon genes (STING) activation contributes to RILD via the innate immune response. Specifically, hepatic stellate cells show significant differences in methylation patterns after X-ray irradiation at 8 Gy140. Irradiation recruits ALKBH5, which in turn demethylates m6A residues in the 3′-UTR of HMGB1, and results in the activation of STING-interferon regulatory factor 3 (IRF3) signaling. YTHDF2 directly binds m6A-modified sites in HMGB1 and promotes its degradation140. Wang et al.25 have investigated the function of m6A modification in Kupffer cells during RILD and observed significantly increased m6A modification levels after irradiation. Their findings have confirmed that METTL3 is a primary modulator that promotes the methylation and gene expression of TEAD1, and consequently leads to STING/nucleotide-binding oligomerization domain (NOD)-like receptor pyrin domain-containing 3 (NLRP3) signaling activation25. IGF2BP2 recognizes methylated TEAD1 mRNA and promotes its stability25. As previously described, after irradiation, upregulated ALKBH5 mediates m6A demethylation of TIRAP mRNA and promotes RILF in hepatic stellate cells through inducing monocyte recruitment and M2 polarization117.
RIHI
Hematopoiesis is a developmental or physiological process that generates all blood lineages141. Total body irradiation triggers a series of adverse health effects, collectively termed acute radiation syndrome (ARS)142. The hematopoietic system is recognized as the organ with the highest radiation sensitivity, and the hematopoietic subsyndrome of ARS (H-ARS) occurs in humans exposed to total body irradiation of 4 to 6 Gy143,144. Mortality from H-ARS is known to be due to hematopoietic insufficiency (both leukopenia and anemia), opportunistic infection from immune suppression, and coagulation dysfunction144–148. Investigations of the function of m6A modification in hematopoietic injury and recovery under radiation stress are extremely rare. Hematopoietic stem cells (HSCs) are central to the hematopoiesis process, because they are responsible for self-renewal and generation of all hematopoietic lineages, which are essential for various stress conditions, including IR149,150. IR damages the hematopoietic system via direct effects on the viability and/or function of hematopoietic stem/progenitor cells151. Wang et al.152 have generated hematopoietic-specific Ythdf2 knockout mice by using 3 Cre/LoxP systems, and identified a unique role of YTHDF2-mediated m6A recognition in adult mouse HSCs. Mechanistically, the expression of Ythdf2 in HSCs facilitates the decay of the m6A-modified mRNAs of Wnt target genes and consequently contributes to the repression of Wnt signaling at steady state. After deletion of YTHDF2, the number of HSCs expands, and the regenerative ability of HSCs also increases under stress conditions such as radiation152. YTHDF2 deficiency simultaneously prevents the degradation of mRNAs of both Wnt target genes and survival-related genes during hematopoietic stresses, and this combined effect synergistically enhances the regenerative ability of HSCs152. These findings have established the critical role of YTHDF2 in modulating HSC self-renewal, regeneration, and protection, thereby providing preliminary results supporting translation to clinical applications152.
The bone marrow is the primary site for hematopoiesis153, and severe myelosuppression is a common adverse effect of radiotherapy or chemotherapy in clinical settings154. Our group previously revealed the time-varying epi-transcriptome-wide m6A methylome and transcriptome alterations in γ-ray-exposed mouse bone marrow134. We have observed that 4 Gy γ-irradiation rapidly (5 min and 2 h) and severely impairs the mouse hematopoietic system, including spleen and thymus atrophy, alterations in blood cell proportions, tissue inflammation, and malondialdehyde elevation134. The m6A content and expression of m6A-related enzymes are altered, and radiation triggers dynamic and reversible m6A modification profiles and alters mRNA expression, wherein both m6A fold-enrichment and mRNA expression first increase and subsequently decrease134. The affected pathways are closely related to those of classical radiation response and metabolism134. Interestingly, blocking the expression of FTO and ALKBH5 mitigates radiation hematopoietic toxicity; therefore, inhibiting the expression of m6A demethylases might enhance recovery from radiation exposure134. This study indicates the importance of m6A modification in hematopoietic radiobiology and suggests that modulation of the epi-transcriptome might be exploited as a strategy against radiation damage.
The roles of m6A modification and corresponding enzymes in the IR biology of normal tissues are summarized in Table 2.
Table 2.
RNA m6A methylation in ionizing radiation biology in normal tissues
| Organ | Enzyme | Target | Function |
|---|---|---|---|
| Lung | METTL3 ALKBH5 YTHDF2 |
FOXO1 mRNA↓ | Facilitate IR-induced EMT during RILI27 |
| ALKBH5 | IL-6 mRNA↓ | Suppress aseptic inflammation in RILI26 | |
| Liver | ALKBH5 YTHDF2 |
HMGB1 mRNA↓ | Activate STING-IRF3 and contribute to RILD via the innate immune response140 |
| METTL3 IGF2BP2 |
TEAD1 mRNA↑ | Activate STING-NLRP3 and contribute to RILD via pyroptosis25 | |
| ALKBH5 | TIRAP mRNA↑ |
Promote RILF through monocyte recruitment and M2 polarization117 | |
| Hematopoietic organs | YTHDF2 | Wnt target genes↓ | Decrease the regenerative ability of HSC152 |
| FTO ALKBH5 |
Radiation response and metabolism pathways | Inhibit recovery from radiation exposure134 |
↑: promotes, ↓: inhibits.
m6A modification with UV radiation in the biology of normal tissues
Several studies have focused on the roles of RNA m6A modification in non-IR effects on non-cancer tissues. A recent article has revealed that deficiency in ALKBH5 alleviates UVB radiation-induced chronic actinic dermatitis via regulating pyroptosis, in a manner involving alteration of levels of cell proliferation and apoptosis, inflammatory cytokines, and pyroptosis-associated proteins, such as gasdermin D (GSDMD), caspase-1, and caspase-424. Long-term exposure to UV radiation from sunlight facilitates the progression of skin photoaging. A recent study has reported that microRNA m6A modification regulates this process. A single UVB dose of 30 mJ/cm2 elicits a photoaging phenotype in skin fibroblasts, and is accompanied by a decrease in total m6A levels and METTL14 expression. The m6A modification level of pri-miR-100, identified as the target of METTL14, is decreased by photoaging. The modification of pri-miR-100 influences the binding of DiGeorge syndrome critical region 8 (DGCR8) on this pri-miRNA, thereby obstructing the maturation of miR-100-3p. The restrained miR-100-3p maturation eventually results in elevated expression of the target gene epidermal growth factor receptor feedback inhibitor 1 (ERRFI1). Therefore, UVB exposure triggers dermal photoaging by affecting the METTL14/m6A-miR-100-3p/ERRFI1 axis. This finding clarifies the miRNA m6A modification-mediated mechanism underlying skin photoaging, and enriches evidence of the important roles of RNA m6A modification in UVB-induced skin injury155. Supplementing the findings of Xiang et al.133, Liu and colleagues23 have revealed the altered transcriptome and epigenetic signatures in the UV-induced DNA damage response through multi-omic analysis, including the DNA methylation (5 mC) and RNA m6A methylome. They have defined the temporally specific m6A RNA methylation that appears to affect DNA repair by modulating translation23. Evidence of the functions of RNA m6A modification in non-ionizing radiobiology has verified its spatiotemporally sensitive characteristics, which contribute to the precise regulation of genetic information.
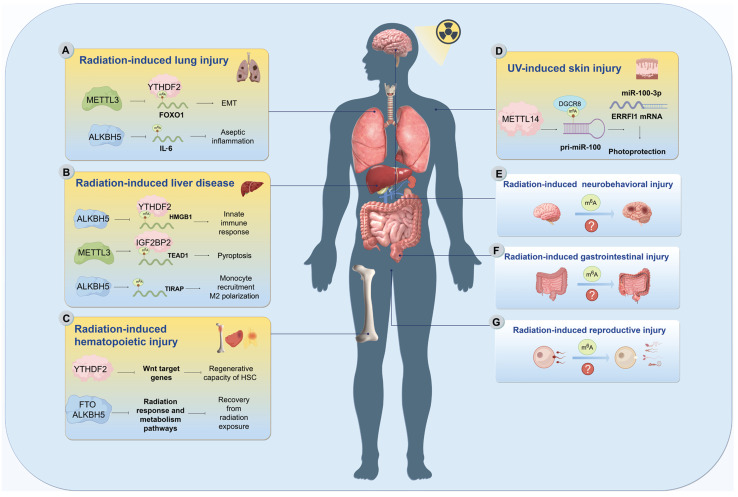
Notably, investigations of the roles of m6A modification in radiation-induced normal tissue injuries are far from comprehensive. How this modification functions in other typical radiation effects, such as radiation-induced gastrointestinal injury, radiation-induced neurobehavioral injury, and radiation-induced reproductive injury, remains unclear and requires urgent elucidation (Figure 2).
Figure 2.
Outline of the interplay between m6A modification and radiation-induced injury effects on distinct normal organ tissues (created in Figdraw). Investigated effects included those on the lungs, liver, and hematopoietic system. A. In radiation-induced lung injury (RILI), the METTL3/m6A-FOXO1 mRNA/YTHDF2/AKT-ERK signaling pathway contributes to epithelial-to-mesenchymal transition (EMT). BTB domain-containing protein 7B (Zbtb7b) recruits ALKBH5 to demethylate of IL-6 mRNA, thereby inhibiting its nucleocytoplasmic transport and production, and alleviating aseptic inflammation in RILI. B. In radiation-induced liver disease (RILD), the ALKBH5/m6A-HMGB1 mRNA/STING-IRF3 signaling pathway contributes to RILD via the innate immune response. In Kupffer cells, irradiation increases m6A modification levels, and the METTL3/m6A-TEAD1 mRNA/IGF2BP2/STING-NLRP3 signaling pathway contributes to the injury effects via pyroptosis. In hepatic stellate cells, irradiation upregulates ALKBH5, and the ALKBH5/m6A-TIRAP mRNA pathway facilitates radiation-induced liver fibrosis (RILF) progression by inducing monocyte recruitment and M2 polarization. C. The hematopoietic process is crucial for recovery and survival after radiation exposure, whereas hematopoiesis is vulnerable during RT. In hematopoietic Ythdf2 knockout mice, the mRNA degradation of both Wnt target genes and survival-associated genes under radiation stress is suppressed, and the regenerative ability of hematopoietic stem cells (HSCs) is therefore restrained. Our previous study has revealed that inhibiting the expression of FTO and ALKBH5 ameliorates radiation-induced hematopoietic injury (RIHI); therefore, suppression of m6A demethylase might improve recovery from radiation exposure. D. MicroRNA m6A modification regulates UV-induced skin photoaging. UVB exposure elicits a photoaging phenotype in skin fibroblasts and is accompanied by a decrease in total m6A level and METTL14 expression. After METTL14 overexpression, the downregulated m6A modification level of pri-miR-100, identified as the target of METTL14, is rescued, thus enhancing binding of DiGeorge syndrome critical region 8 (DGCR8) to this pri-miRNA and restoring miR-100-3p maturation. The resurgent miR-100-3p eventually decreases expression of its target gene, epidermal growth factor receptor feedback inhibitor 1 (ERRFI1). Therefore, UVB exposure triggers dermal photoaging by affecting the METTL14/m6A-miR-100-3p/ERRFI1 axis. Of note, how the m6A modification functions in other typical radiation effects, such as radiation-induced neurobehavioral injury (RINI, E), radiation-induced gastrointestinal injury (RIGI, F), and radiation-induced reproductive injury (RIRI, G), requires further study.
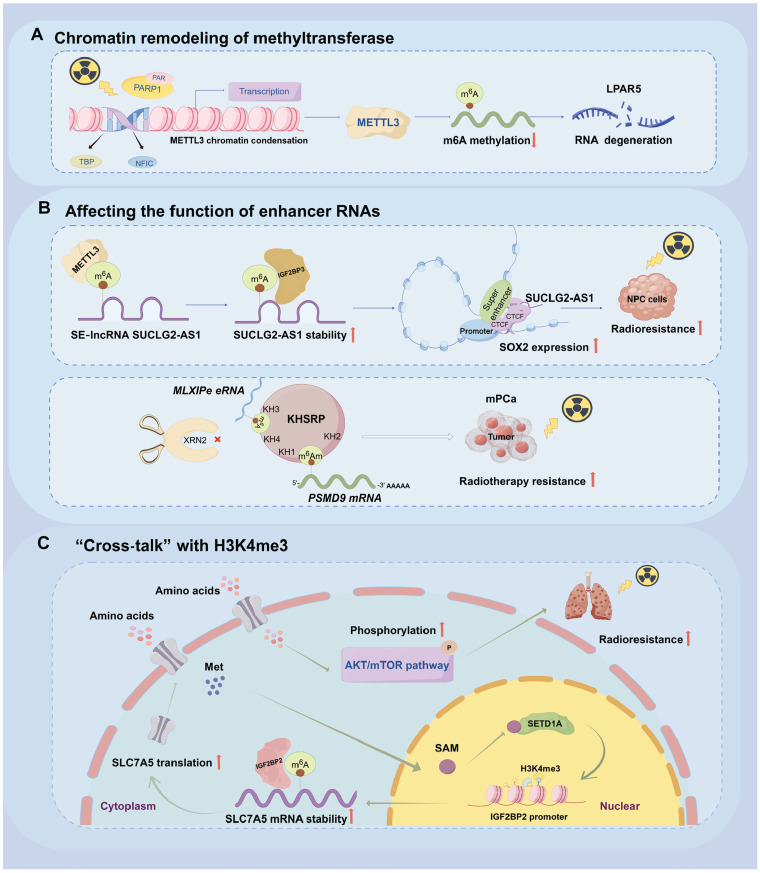
Novel regulatory mechanisms of RNA m6A modification
With the continued advancement of m6A-related research, multiple novel regulatory mechanisms are being elucidated (Figure 3). One novel mechanism of m6A modification in radiobiology affects m6A enzymes’ chromatin remodeling—a critical regulatory layer, alongside m6A modification, in controlling gene expression and DNA damage signaling156,157. Sun et al.157 have reported that poly[adenosine diphosphate (ADP)-ribose] polymerase 1 (PARP1), interacting with the transcription factors nuclear factor I-C (NFIC) and TATA binding protein (TBP), modulates the chromatin accessibility of the METTL3 promoter, and consequently activates METTL3 transcription and influences the m6A modification of poly(A)+ RNA, such as lysophosphatidic acid receptor 5 (LPAR5) mRNA. However, irradiation causes disassociation of PARP1 from the promoter of METTL3, and impairs the accessibility of the transcription factors NFIC and TBP to the promoter region. Subsequently, chromatin condensation and repressed transcription of METTL3 decrease the m6A levels and consequently accelerate the degradation of LPAR5 mRNA157. These findings advance the conventional understanding of PARP’s roles, and may have important implications in exploring valuable therapeutic strategies for PARP1 inhibitors in oncology157.
Figure 3.
The newly elucidated regulatory mechanisms relevant to RNA m6A modification (created in Figdraw). As shown, the novel m6A-associated mechanisms in radiobiology involve the chromatin remolding of m6A regulatory enzymes and the function of m6A-modified enhancer RNAs (eRNAs). A. Irradiation causes disassociation of poly(ADP-ribose) polymerase 1 (PARP1) from the promoter of METTL3 and impairs the accessibility of the transcription factors nuclear factor I-C (NFIC) and TATA binding protein (TBP) to the promoter region. Subsequently, chromatin condensation and repressed transcription of METTL3 occur. Decreased expression of METTL3 abates the m6A levels of its target genes, such as Lysophosphatidic Acid Receptor 5 (LPAR5), whose degradation is consequently accelerated after radiation. B. Top, in nasopharyngeal carcinoma (NPC), METTL3 methylates the super enhancer (SE) RNA lncRNA succinate-CoA ligase GDP-forming beta subunit-antisense 1 (SUCLG2-AS1), located in the SE region of sex-determining region Y-box 2 (SOX2). The stability of SUCLG2-AS1 is enhanced by the recognition of the reader protein insulin-like growth factor 2 mRNA-binding protein 3 (IGF2BP3), and the expression is elevated in an m6A-dependent fashion, thereby facilitating the formation of a complex comprising CCCTC binding factor (CTCF), SUCLG2-AS1, SOX2 promoter, and the SE region through a long chromatin loop; increasing SOX2 expression; and conferring radioresistance to NPC cells. Bottom, the bone-specific enhancer RNA MLXIPe, with an m6A site, along with the mRNA of its target gene PSMD9, with m6Am site on the 5′-UTR, is recognized by, and interacts with, RNA-binding protein KH-type splicing regulator protein (KHSRP). The interaction protects against PSMD9 mRNA degradation by 5′-3′ exoribonuclease 2 (XRN2). Thus, the m6A-methylated eRNA MLXIPe facilitates radioresistance in metastatic prostate cancer (mPa). C. In lung cancer, the reader protein IGF2BP2 is upregulated and augments radioresistance. Mechanistically, the m6A-modified mRNA of solute carrier family 7 member 5 or LAT1 (SLC7A5), encoding a sodium-independent transporter of large neutral amino acids across the cell membrane, is stabilized by IGF2BP2, which is elevated in lung cancer. The upregulation of SLC7A5 promotes the transport of Met, the substrate for SAM synthesis, into cells. Increased intracellular SAM further serves as a substrate for the histone lysine methyltransferase SETD1A, thus leading to formation of trimethylated lysine 4 of histone H3 (H3K4me3) at the promoter region of the IGF2BP2 gene, and enhancing IGF2BP2 transcription through formation of a positive feedback loop between IGF2BP2 and SLC7A5. Consequently, IGF2BP2 enhances lung cancer radioresistance via the AKT/mTOR pathway.
Some studies have focused on m6A modification on enhancer RNAs. METTL3 mediates the methylation of super enhancer (SE) RNA, the lncRNA succinate-CoA ligase GDP-forming beta subunit-antisense 1 (SUCLG2-AS1). SUCLG2-AS1 is recognized and stabilized by the reader protein insulin-like growth factor 2 mRNA-binding protein 3 (IGF2BP3), and the expression of SUCLG2-AS1 increases in an m6A-dependent fashion in NPC18. SUCLG2-AS1, located in the SE region of sex-determining region Y-box 2 (SOX2), regulates the expression of SOX2 through long-range chromatin loop formation, via mediating the occupancy of the CCCTC binding factor CTCF at the SE and promoter regions of SOX2, thus modulating the metastasis and radiosensitivity of NPC18. Zhao et al.158 have screened and identified bone-specific m6A modifications on enhancer RNA (eRNA) that play a post-transcriptional functional role in bone metastatic prostate cancer and correlate with RT resistance. The enhancer RNA MLXIPe with an m6A site, along with the mRNA of its target gene PSMD9, with an m6Am site at the 5′-UTR, are recognized and interact with the RNA-binding protein KH-type splicing regulator protein (KHSRP), thereby protecting against PSMD9 mRNA degradation by 5′-3′ exoribonuclease 2 (XRN2) and increasing the radioresistance of metastatic prostate cancer158.
Novel functions of m6A modification in radiotherapy efficacy are also reflected in regulation of the TME. This epigenetic modification modulates the immune milieu of the radiation-remodeled TME and has a nexus role in both anti-tumor immunity and the radiation response: it influences both tumor cell intrinsic radioresistance and MDSC-mediated extrinsic radioresistance159.
With continued deep examination of the molecular mechanisms underlying cancer radiosensitivity, researchers are delineating the cross-talk between RNA m6A modification and other epigenetic modifications, such as histone modification and DNA methylation. In lung cancer, the reader protein IGF2BP2 is upregulated and enhances radioresistance. Mechanistically, the m6A-modified mRNA of solute carrier family 7 member 5 or LAT1 (SLC7A5), a sodium-independent transporter of large neutral amino acids across the cell membrane, is stabilized by IGF2BP2. The upregulation of SLC7A5 promotes the transportation of Met, the substrate for SAM synthesis in cells. Intracellular SAM enrichment provides a substrate for SETD1A, a histone lysine methyltransferase, thus leading to trimethylation of lysine 4 of histone H3 (H3K4me3) in the promoter of the IGF2BP2 gene, enhancing IGF2BP2 transcription, and forming a positive feedback loop between IGF2BP2 and SLC7A5160. This finding emphasizes the importance of the interactions among multiple regulatory layers underlying the RT sensitivity of cancer. These studies have provided new insights into new types of RNA m6A modification and indicated multiple regulatory paradigms mediated by this modification.
Exploration of the application of RNA m6A modification in radiation medicine
Accurate quantification of IR, particularly low-dose radiation, is important in protecting organisms against damage caused by environmental radioactive incidents or clinical radiotherapy161. As described previously, the abundant m6A modification responds sensitively and rapidly to external stimulation134. By exploiting this feature of m6A modification, Jin et al.161 have reported a Cas13a-microdroplet platform that enables sensitive detection of ultra-low doses of radiation (0.5 Gy vs. 1 Gy traditionally) within 1 h. The micro-platform uses an ideal, specific radiation-sensitive marker, m6A on the nuclear receptor coactivator 4 (NCOA4) gene (NCOA4-m6A)161,162. The microfluidics of the platform generates uniform microdroplets that encapsulate a detection system consisting of CRISPR/Cas13a and NCOA4-m6A targets derived from total RNA extraction, thereby achieving a 10-fold enhancement in sensitivity and significantly decreasing the limit of detection161. Clinical patient samples and systematic mouse models have indicated a limit of detection (0.5 Gy) and superior sensitivity to that of traditional quantitative PCR161. Generally, through screening and identification of radiation-sensitive m6A sites on specific mRNAs or non-coding RNAs and the m6A-correlative enzymes involved in certain cancer types, m6A-related biomarkers can be used for tumor diagnosis in early stages, prediction of RT response before treatment, and evaluation of prognosis after treatment, and can also serve as a target in combination therapy to enhance the efficacy of RT. Thus, strategic and rational utilization of m6A-related biomarkers may enhance the effects of cancer RT in clinical settings.
m6A modification-based biomarkers have also been explored for absorbed IR dose estimation162. A genome-wide screen of radiation-responding mRNAs, whose m6A levels show significant alteration after acute irradiation, has been conducted162. The NCOA4 m6A level shows highly responsive specificity to radiation, which is conserved across mice, monkeys, and humans, and complies with the dose-response relationship observed in peripheral blood mononuclear cells from patients with cancer receiving RT162. In the screening of m6A-based biomarkers for radiation dose estimation, the specifically sensitive genes should be identified, and a dose-m6A level curve should be established for dose derivation. Subsequently, dose-prediction models based on the biomarker of m6A modifications might be established, through which the radiation doses absorbed into the body are prospectively and accurately predicted, thereby maximally alleviating the adverse effect toxicity during RT, as well as injury in the event of accidental nuclear exposure.
Identification of epigenetic biomarkers of radiation sensitivity is beneficial in precision medicine163. Using multi-omics analysis, Zeng et al.163 have identified SETD2, a factor important in repairing DNA double-strand breaks and maintaining chromatin integrity, as a radio-sensitivity signature in LUAD. Moreover, SETD2 is a favorable prognostic factor whose effects are antagonized by RBM15 and YTHDF3; therefore, SETD2 is a promising epigenetic biomarker in patients with LUAD163. These studies have indicated promising prospects of m6A modification in radiation monitoring for radioactive injury management and screening radiosensitivity-related epigenetic biomarkers161,162.
Given that multiple m6A-associated modulators are dysregulated in various patterns of malignancy, targeting overexpressed m6A enzymes is considered a promising strategy for cancer therapy. Small-molecule inhibitors targeting the catalytic domains of writers, erasers, and readers have been designed to diminish their enzymatic activities. For instance, METTL3 or METTL3-14 complex inhibitors such as UZH1a/2 and CDIBA derivative have been found to exhibit anti-tumor efficacy in a glioblastoma PDX mouse model or AML164,165. The most widely investigated METTL3 inhibitor STM2457 impairs stem cell viability in leukemia, by suppressing the cell proliferation of prostate cancer and intrahepatic cholangiocarcinoma, and notably enhancing the anti-PD-1 treatment effects in CRC166–169. Delicaflavone, a natural product from Selaginella doederleinii Hieron, prevents expression of METTL3/14 and promotes the anti-tumor immune response in lung cancer170. Additionally, CS1/CS2 and Dac51, inhibitors of FTO, hinder CSCs self-renewal and facilitate anti-tumor immunity171,172. Cucurbitacin B, targeting IGF2BP1, induces HCC cell apoptosis and suppress PD-L1 expression173. Furthermore, on the basis of the primary effects of small-molecule inhibitors, the nanoparticle delivery system can achieve targeted delivery and controllable release of molecules. A co-delivery nanoplatform carrying the FTO inhibitor (FB23-2) and tumor-associated antigens has been designed to target tumor-infiltrating dendritic cells in HCC, and consequently restrain HCC progression through accelerating dendritic cell maturation as well as effector T cell infiltration174. These studies have indicated that the integrative utility of inhibitors targeting m6A-related regulators or specific m6A-modified oncogenes may achieve radiosensitizing effects in cancer RT in the clinical practice of radiation medicine.
Conclusions and prospects
In the past several years, knowledge of RNA m6A modifications in distinct biological processes has rapidly increased, and the intricate interplay between this modification and radiation biology in both cancer and non-cancer contexts has profound implications for elucidating the molecular mechanisms underlying radiation responses and devising novel strategies for RT or radiation protection. Accumulating evidence suggests that m6A modifications play critical roles in tumor responsiveness to RT and the propagation of radiation injury in normal tissues. This modification is also a potential biomarker and therapeutic target, and modulating the activity of associated enzymes to alter m6A levels might facilitate RT efficacy while mitigating toxic effects on normal tissues. Accordingly, this feature of m6A modification might be used to develop dual-benefit strategies in cancer treatment in the future.
Despite the current exploration of the relationship between RNA m6A modification and radiation biology, studies in this area are far from sufficient. More in-depth efforts are crucial. A goal of molecular biologists is to further decipher the precise novel molecular pathways through which RNA m6A modification governs tumor radio-sensitivity and the radiation injury effects on normal tissues. Subsequently, designing novel radio-sensitizers or radio-protectors based on m6A modification-related pathways could pave the way to personalized RT and radiation protection approaches. Furthermore, clinical trials to validate the potential of m6A modification as a predictive biomarker for cancer prognosis and RT efficacy would help assess the clinical utility of targeted therapies against the m6A pathway in patients with cancer. By monitoring the expression of m6A-based biomarkers, clinicians could tailor RT regimens to individual patients, including optimization of doses and schedules for maximum efficacy and minimal toxicity. This personalized approach might achieve better outcomes and diminished adverse effects for RT. Collectively, m6A-related regulator-mediated m6A-modification triggers the expression alterations of oncogenes or tumor suppressors by affecting the metabolism of modified-RNAs, thus modulating the progression and RT outcomes for cancer tissues. Similarly, radiation-induced aberrantly expressed m6A-related enzymes and the abnormal modification of key target RNAs contribute to the toxic injury effects to normal tissues. Delving deeper into the intrinsic connection between RNA m6A modification and radiation biology promises to enhance RT outcomes, decrease adverse reactions, and mitigate the toxic effects derived from environmental radiation stress, thereby driving advancements in precision medicine.
Supporting Information
Funding Statement
This work was supported by grants from the National Natural Science Foundation of China (Grant No. 82173467 and 82273577) and CAMS Innovation Fund for Medical Sciences (Grant Nos. CIFMS, 2022-I2M-2-003 and 2021-I2M-1-042).
Conflict of interest statement
No potential conflicts of interest are disclosed.
Author contributions
Conceived and designed the analysis: Saijun Fan and Shuqin Zhang.
Collected the data: Yajia Cheng and Shuqin Zhang.
Contributed data or analysis tools: Yajia Cheng and Yue Shang.
Wrote the paper: Shuqin Zhang and Yajia Cheng.
Revised the manuscript and figures: Yajia Cheng, Yue Shang and Saijun Fan.
References
- 1.Sendinc E, Shi Y. RNA m6A methylation across the transcriptome. Mol Cell. 2023;83:428–41. doi: 10.1016/j.molcel.2023.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Adler M, Weissmann B, Gutman AB. Occurrence of methylated purine bases in yeast ribonucleic acid. J Biol Chem. 1958;230:717–23. [PubMed] [Google Scholar]
- 3.Littlefield JW, Dunn DB. Natural occurrence of thymine and three methylated adenine bases in several ribonucleic acids. Nature. 1958;181:254–5. doi: 10.1038/181254a0. [DOI] [PubMed] [Google Scholar]
- 4.Desrosiers R, Friderici K, Rottman F. Identification of methylated nucleosides in messenger RNA from Novikoff hepatoma cells. Proc Natl Acad Sci U S A. 1974;71:3971–5. doi: 10.1073/pnas.71.10.3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schibler U, Kelley DE, Perry RP. Comparison of methylated sequences in messenger RNA and heterogeneous nuclear RNA from mouse L cells. J Mol Biol. 1977;115:695–714. doi: 10.1016/0022-2836(77)90110-3. [DOI] [PubMed] [Google Scholar]
- 6.Wei CM, Moss B. Nucleotide sequences at the N6-methyladenosine sites of HeLa cell messenger ribonucleic acid. Biochemistry. 1977;16:1672–6. doi: 10.1021/bi00627a023. [DOI] [PubMed] [Google Scholar]
- 7.Bokar JA, Shambaugh ME, Polayes D, Matera AG, Rottman FM. Purification and cDNA cloning of the AdoMet-binding subunit of the human mRNA (N6-adenosine)-methyltransferase. RNA. 1997;3:1233–47. [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer KD, Saletore Y, Zumbo P, Elemento O, Mason CE, Jaffrey SR. Comprehensive analysis of mRNA methylation reveals enrichment in 3′ UTRs and near stop codons. Cell. 2012;149:1635–46. doi: 10.1016/j.cell.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Achrol AS, Rennert RC, Anders C, Soffietti R, Ahluwalia MS, Nayak L, et al. Brain metastases. Nat Rev Dis Primers. 2019;5:5. doi: 10.1038/s41572-018-0055-y. [DOI] [PubMed] [Google Scholar]
- 10.Horton L, Brady J, Kincaid CM, Torres AE, Lim HW. The effects of infrared radiation on the human skin. Photodermatol Photoimmunol Photomed. 2023;39:549–55. doi: 10.1111/phpp.12899. [DOI] [PubMed] [Google Scholar]
- 11.Gale RP, Reisner Y. The role of bone-marrow transplants after nuclear accidents. Lancet. 1988;1:923–6. doi: 10.1016/s0140-6736(88)91724-2. [DOI] [PubMed] [Google Scholar]
- 12.Moraitis I, Guiu J, Rubert J. Gut microbiota controlling radiation-induced enteritis and intestinal regeneration. Trends Endocrinol Metab. 2023;34:489–501. doi: 10.1016/j.tem.2023.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Dasgupta Q, Jiang A, Wen AM, Mannix RJ, Man Y, Hall S, et al. A human lung alveolus-on-a-chip model of acute radiation-induced lung injury. Nat Commun. 2023;14:6506. doi: 10.1038/s41467-023-42171-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayo C, Yorke E, Merchant TE. Radiation associated brainstem injury. Int J Radiat Oncol Biol Phys. 2010;76:S36–41. doi: 10.1016/j.ijrobp.2009.08.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kesari KK, Agarwal A, Henkel R. Radiations and male fertility. Reprod Biol Endocrinol. 2018;16:118. doi: 10.1186/s12958-018-0431-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim JG, Park MT, Heo K, Yang KM, Yi JM. Epigenetics meets radiation biology as a new approach in cancer treatment. Int J Mol Sci. 2013;14:15059–73. doi: 10.3390/ijms140715059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weigel C, Schmezer P, Plass C, Popanda O. Epigenetics in radiation-induced fibrosis. Oncogene. 2015;34:2145–55. doi: 10.1038/onc.2014.145. [DOI] [PubMed] [Google Scholar]
- 18.Hu X, Wu J, Feng Y, Ma H, Zhang E, Zhang C, et al. METTL3-stabilized super enhancers-lncRNA SUCLG2-AS1 mediates the formation of a long-range chromatin loop between enhancers and promoters of SOX2 in metastasis and radiosensitivity of nasopharyngeal carcinoma. Clin Transl Med. 2023;13:e1361. doi: 10.1002/ctm2.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang WM, Li ZX, Wu YH, Shi ZL, Mi JL, Hu K, et al. m6A demethylase FTO renders radioresistance of nasopharyngeal carcinoma via promoting OTUB1-mediated anti-ferroptosis. Transl Oncol. 2023;27:101576. doi: 10.1016/j.tranon.2022.101576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yin J, Ding F, Cheng Z, Ge X, Li Y, Zeng A, et al. METTL3-mediated m6A modification of LINC00839 maintains glioma stem cells and radiation resistance by activating Wnt/β-catenin signaling. Cell Death Dis. 2023;14:417. doi: 10.1038/s41419-023-05933-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han L, Dong L, Leung K, Zhao Z, Li Y, Gao L, et al. METTL16 drives leukemogenesis and leukemia stem cell self-renewal by reprogramming BCAA metabolism. Cell Stem Cell. 2023;30:52–68.e13. doi: 10.1016/j.stem.2022.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang L, Dou X, Chen S, Yu X, Huang X, Zhang L, et al. YTHDF2 inhibition potentiates radiotherapy antitumor efficacy. Cancer Cell. 2023;41:1294–308.e8. doi: 10.1016/j.ccell.2023.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu J, Liu L, He J, Xu Y, Wang Y. Multi-omic analysis of altered transcriptome and epigenetic signatures in the UV-induced DNA damage response. DNA Repair (Amst) 2021;106:103172. doi: 10.1016/j.dnarep.2021.103172. [DOI] [PubMed] [Google Scholar]
- 24.He L, Liu L, Xu D, Tu Y, Yang C, Zhang M, et al. Deficiency of N6-methyladenosine demethylase ALKBH5 alleviates ultraviolet B radiation-induced chronic actinic dermatitis via regulating pyroptosis. Inflammation. 2024;47:159–72. doi: 10.1007/s10753-023-01901-7. [DOI] [PubMed] [Google Scholar]
- 25.Wang B, Zhang Y, Niu H, Zhao X, Chen G, Zhao Q, et al. METTL3-mediated STING upregulation and activation in Kupffer cells contribute to radiation-induced liver disease via pyroptosis. Int J Radiat Oncol Biol Phys. 2024;119:219–33. doi: 10.1016/j.ijrobp.2023.10.041. [DOI] [PubMed] [Google Scholar]
- 26.Zhao J, Han DX, Wang CB, Wang XL. Zbtb7b suppresses aseptic inflammation by regulating m6A modification of IL6 mRNA. Biochem Biophys Res Commun. 2020;530:336–41. doi: 10.1016/j.bbrc.2020.07.011. [DOI] [PubMed] [Google Scholar]
- 27.Feng Y, Yuan P, Guo H, Gu L, Yang Z, Wang J, et al. METTL3 mediates epithelial-mesenchymal transition by modulating FOXO1 mRNA N6-methyladenosine-dependent YTHDF2 binding: a novel mechanism of radiation-induced lung injury. Adv Sci (Weinh) 2023;10:e2204784. doi: 10.1002/advs.202204784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sui X, Klungland A, Gao L. RNA m6A modifications in mammalian gametogenesis and pregnancy. Reproduction. 2022;165:R1–8. doi: 10.1530/REP-22-0112. [DOI] [PubMed] [Google Scholar]
- 29.Mauer J, Sindelar M, Despic V, Guez T, Hawley BR, Vasseur JJ, et al. FTO controls reversible m6Am RNA methylation during snRNA biogenesis. Nat Chem Biol. 2019;15:340–7. doi: 10.1038/s41589-019-0231-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mao XL, Li ZH, Huang MH, Wang JT, Zhou JB, Li QR, et al. Mutually exclusive substrate selection strategy by human m3C RNA transferases METTL2A and METTL6. Nucleic Acids Res. 2021;49:8309–23. doi: 10.1093/nar/gkab603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meyer B, Wurm JP, Sharma S, Immer C, Pogoryelov D, Kötter P, et al. Ribosome biogenesis factor Tsr3 is the aminocarboxypropyl transferase responsible for 18S rRNA hypermodification in yeast and humans. Nucleic Acids Res. 2016;44:4304–16. doi: 10.1093/nar/gkw244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhuang H, Yu B, Tao D, Xu X, Xu Y, Wang J, et al. The role of m6A methylation in therapy resistance in cancer. Mol Cancer. 2023;22:91. doi: 10.1186/s12943-023-01782-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwartz S, Agarwala SD, Mumbach MR, Jovanovic M, Mertins P, Shishkin A, et al. High-resolution mapping reveals a conserved, widespread, dynamic mRNA methylation program in yeast meiosis. Cell. 2013;155:1409–21. doi: 10.1016/j.cell.2013.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fu Y, Dominissini D, Rechavi G, He C. Gene expression regulation mediated through reversible m6A RNA methylation. Nat Rev Genet. 2014;15:293–306. doi: 10.1038/nrg3724. [DOI] [PubMed] [Google Scholar]
- 35.He PC, He C. m6 A RNA methylation: from mechanisms to therapeutic potential. EMBO J. 2021;40:e105977. doi: 10.15252/embj.2020105977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boulias K, Greer EL. Biological roles of adenine methylation in RNA. Nat Rev Genet. 2023;24:143–60. doi: 10.1038/s41576-022-00534-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu H, Gao R, Chen S, Liu X, Wang Q, Cai W, et al. Bmi1 regulates Wnt signaling in hematopoietic stem and progenitor cells. Stem Cell Rev Rep. 2021;17:2304–13. doi: 10.1007/s12015-021-10253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shen S, Zhang R, Jiang Y, Li Y, Lin L, Liu Z, et al. Comprehensive analyses of m6A regulators and interactive coding and non-coding RNAs across 32 cancer types. Mol Cancer. 2021;20:67. doi: 10.1186/s12943-021-01362-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wei J, Yu X, Yang L, Liu X, Gao B, Huang B, et al. FTO mediates LINE1 m6A demethylation and chromatin regulation in mESCs and mouse development. Science. 2022;376:968–73. doi: 10.1126/science.abe9582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Batista PJ, Molinie B, Wang J, Qu K, Zhang J, Li L, et al. m(6)A RNA modification controls cell fate transition in mammalian embryonic stem cells. Cell Stem Cell. 2014;15:707–19. doi: 10.1016/j.stem.2014.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rockwell AL, Hongay CF. The m6A dynamics of profilin in neurogenesis. Front Genet. 2019;10:987. doi: 10.3389/fgene.2019.00987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Han D, Liu J, Chen C, Dong L, Liu Y, Chang R, et al. Anti-tumour immunity controlled through mRNA m6A methylation and YTHDF1 in dendritic cells. Nature. 2019;566:270–4. doi: 10.1038/s41586-019-0916-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wan W, Ao X, Chen Q, Yu Y, Ao L, Xing W, et al. METTL3/IGF2BP3 axis inhibits tumor immune surveillance by upregulating N6-methyladenosine modification of PD-L1 mRNA in breast cancer. Mol Cancer. 2022;21:60. doi: 10.1186/s12943-021-01447-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jia G, Fu Y, Zhao X, Dai Q, Zheng G, Yang Y, et al. N6-methyladenosine in nuclear RNA is a major substrate of the obesity-associated FTO. Nat Chem Biol. 2011;7:885–7. doi: 10.1038/nchembio.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Scott LJ, Mohlke KL, Bonnycastle LL, Willer CJ, Li Y, Duren WL, et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science. 2007;316:1341–45. doi: 10.1126/science.1142382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kumari R, Ranjan P, Suleiman ZG, Goswami SK, Li J, Prasad R, et al. mRNA modifications in cardiovascular biology and disease: with a focus on m6A modification. Cardiovasc Res. 2022;118:1680–92. doi: 10.1093/cvr/cvab160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang J, Chen L, Qiang P. The role of IGF2BP2, an m6A reader gene, in human metabolic diseases and cancers. Cancer Cell Int. 2021;21:99. doi: 10.1186/s12935-021-01799-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chang R, Huang Z, Zhao S, Zou J, Li Y, Tan S. Emerging roles of FTO in neuropsychiatric disorders. Biomed Res Int. 2022;2022:2677312. doi: 10.1155/2022/2677312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kostyusheva A, Brezgin S, Glebe D, Kostyushev D, Chulanov V. Host-cell interactions in HBV infection and pathogenesis: the emerging role of m6A modification. Emerg Microbes Infect. 2021;10:2264–75. doi: 10.1080/22221751.2021.2006580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang Y, Zhou X. N6-methyladenosine and its implications in viruses. Genomics Proteomics Bioinformatics. 2023;21:695–706. doi: 10.1016/j.gpb.2022.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhang T, Jiang Z, Yang N, Ge Z, Zuo Q, Huang S, et al. N6-methyladenosine (m6A) modification in preeclampsia. Reprod Sci. 2023;30:3144–52. doi: 10.1007/s43032-023-01250-8. [DOI] [PubMed] [Google Scholar]
- 52.You L, Han Z, Chen H, Chen L, Lin Y, Wang B, et al. The role of N6-methyladenosine (m6A) in kidney diseases. Front Med (Lausanne) 2023;10:1247690. doi: 10.3389/fmed.2023.1247690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petri BJ, Cave MC, Klinge CM. Changes in m6A in steatotic liver disease. Genes (Basel) 2023;14:1653. doi: 10.3390/genes14081653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu Y, Liu W, Ren L. Emerging roles and mechanism of m6A methylation in rheumatoid arthritis. Biomed Pharmacother. 2024;170:116066. doi: 10.1016/j.biopha.2023.116066. [DOI] [PubMed] [Google Scholar]
- 55.Huang H, Weng H, Chen J. m6A modification in coding and non-coding RNAs: roles and therapeutic implications in cancer. Cancer Cell. 2020;37:270–88. doi: 10.1016/j.ccell.2020.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang T, Kong S, Tao M, Ju S. The potential role of RNA N6-methyladenosine in Cancer progression. Mol Cancer. 2020;19:88. doi: 10.1186/s12943-020-01204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jiang X, Liu B, Nie Z, Duan L, Xiong Q, Jin Z, et al. The role of m6A modification in the biological functions and diseases. Signal Transduct Target Ther. 2021;6:74. doi: 10.1038/s41392-020-00450-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen RX, Chen X, Xia LP, Zhang JX, Pan ZZ, Ma XD, et al. N6-methyladenosine modification of circNSUN2 facilitates cytoplasmic export and stabilizes HMGA2 to promote colorectal liver metastasis. Nat Commun. 2019;10:4695. doi: 10.1038/s41467-019-12651-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang X, Zhao BS, Roundtree IA, Lu Z, Han D, Ma H, et al. N(6)-methyladenosine modulates messenger RNA translation efficiency. Cell. 2015;161:1388–99. doi: 10.1016/j.cell.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang X, Lu Z, Gomez A, Hon GC, Yue Y, Han D, et al. N6-methyladenosine-dependent regulation of messenger RNA stability. Nature. 2014;505:117–20. doi: 10.1038/nature12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Qi YN, Liu Z, Hong LL, Li P, Ling ZQ. Methyltransferase-like proteins in cancer biology and potential therapeutic targeting. J Hematol Oncol. 2023;16:89. doi: 10.1186/s13045-023-01477-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sun T, Wu R, Ming L. The role of m6A RNA methylation in cancer. Biomed Pharmacother. 2019;112:108613. doi: 10.1016/j.biopha.2019.108613. [DOI] [PubMed] [Google Scholar]
- 63.Yue Y, Liu J, Cui X, Cao J, Luo G, Zhang Z, et al. VIRMA mediates preferential m6A mRNA methylation in 3′UTR and near stop codon and associates with alternative polyadenylation. Cell Discov. 2018;4:10. doi: 10.1038/s41421-018-0019-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.van Tran N, Ernst FGM, Hawley BR, Zorbas C, Ulryck N, Hackert P, et al. The human 18S rRNA m6A methyltransferase METTL5 is stabilized by TRMT112. Nucleic Acids Res. 2019;47:7719–33. doi: 10.1093/nar/gkz619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ignatova VV, Stolz P, Kaiser S, Gustafsson TH, Lastres PR, Sanz-Moreno A, et al. The rRNA m6A methyltransferase METTL5 is involved in pluripotency and developmental programs. Genes Dev. 2020;34:715–29. doi: 10.1101/gad.333369.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sendinc E, Valle-Garcia D, Jiao A, Shi Y. Analysis of m6A RNA methylation in Caenorhabditis elegans. Cell Discov. 2020;6:47. doi: 10.1038/s41421-020-00186-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ma H, Wang X, Cai J, Dai Q, Natchiar SK, Lv R, et al. N6-methyladenosine methyltransferase ZCCHC4 mediates ribosomal RNA methylation. Nat Chem Biol. 2019;15:88–94. doi: 10.1038/s41589-018-0184-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Linder B, Grozhik AV, Olarerin-George AO, Meydan C, Mason CE, Jaffrey SR. Single-nucleotide-resolution mapping of m6A and m6Am throughout the transcriptome. Nat Methods. 2015;12:767–72. doi: 10.1038/nmeth.3453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Goh YT, Koh CWQ, Sim DY, Roca X, Goh WSS. METTL4 catalyzes m6Am methylation in U2 snRNA to regulate pre-mRNA splicing. Nucleic Acids Res. 2020;48:9250–61. doi: 10.1093/nar/gkaa684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen H, Gu L, Orellana EA, Wang Y, Guo J, Liu Q, et al. METTL4 is an snRNA m6Am methyltransferase that regulates RNA splicing. Cell Res. 2020;30:544–7. doi: 10.1038/s41422-019-0270-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pendleton KE, Chen B, Liu K, Hunter OV, Xie Y, Tu BP, et al. The U6 snRNA m6A methyltransferase METTL16 regulates SAM synthetase intron retention. Cell. 2017;169:824–35.e14. doi: 10.1016/j.cell.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Warda AS, Kretschmer J, Hackert P, Lenz C, Urlaub H, Hobartner C, et al. Human METTL16 is a N6-methyladenosine (m6A) methyltransferase that targets pre-mRNAs and various non-coding RNAs. EMBO Rep. 2017;18:2004–14. doi: 10.15252/embr.201744940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Akichika S, Hirano S, Shichino Y, Suzuki T, Nishimasu H, Ishitani R, et al. Cap-specific terminal N6-methylation of RNA by an RNA polymerase II-associated methyltransferase. Science. 2019;363:eaav0080. doi: 10.1126/science.aav0080. [DOI] [PubMed] [Google Scholar]
- 74.Sendinc E, Valle-Garcia D, Dhall A, Chen H, Henriques T, Navarrete-Perea J, et al. PCIF1 Catalyzes m6Am mRNA methylation to regulate gene expression. Mol Cell. 2019;75:620–30.e9. doi: 10.1016/j.molcel.2019.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boulias K, Toczydlowska-Socha D, Hawley BR, Liberman N, Takashima K, Zaccara S, et al. Identification of the m6Am methyltransferase PCIF1 reveals the location and functions of m6Am in the transcriptome. Mol Cell. 2019;75:631–43.e8. doi: 10.1016/j.molcel.2019.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sun H, Zhang M, Li K, Bai D, Yi C. Cap-specific, terminal N6-methylation by a mammalian m6Am methyltransferase. Cell Res. 2019;29:80–2. doi: 10.1038/s41422-018-0117-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zou S, Toh JD, Wong KH, Gao YG, Hong W, Woon EC. N(6)-methyladenosine: a conformational marker that regulates the substrate specificity of human demethylases FTO and ALKBH5. Sci Rep. 2016;6:25677. doi: 10.1038/srep25677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Roost C, Lynch SR, Batista PJ, Qu K, Chang HY, Kool ET. Structure and thermodynamics of N6-methyladenosine in RNA: a spring-loaded base modification. J Am Chem Soc. 2015;137:2107–15. doi: 10.1021/ja513080v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang Z, Theler D, Kaminska KH, Hiller M, de la Grange P, Pudimat R, et al. The YTH domain is a novel RNA binding domain. J Biol Chem. 2010;285:14701–10. doi: 10.1074/jbc.M110.104711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhou J, Wan J, Gao X, Zhang X, Jaffrey SR, Qian SB. Dynamic m(6)A mRNA methylation directs translational control of heat shock response. Nature. 2015;526:591–4. doi: 10.1038/nature15377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shi H, Wang X, Lu Z, Zhao BS, Ma H, Hsu PJ, et al. YTHDF3 facilitates translation and decay of N6-methyladenosine-modified RNA. Cell Res. 2017;27:315–28. doi: 10.1038/cr.2017.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li A, Chen YS, Ping XL, Yang X, Xiao W, Yang Y, et al. Cytoplasmic m6A reader YTHDF3 promotes mRNA translation. Cell Res. 2017;27:444–7. doi: 10.1038/cr.2017.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Roundtree IA, Luo GZ, Zhang Z, Wang X, Zhou T, Cui Y, et al. YTHDC1 mediates nuclear export of N6-methyladenosine methylated mRNAs. Elife. 2017;6:e31311. doi: 10.7554/eLife.31311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kasowitz SD, Ma J, Anderson SJ, Leu NA, Xu Y, Gregory BD, et al. Nuclear m6A reader YTHDC1 regulates alternative polyadenylation and splicing during mouse oocyte development. PLoS Genet. 2018;14:e1007412. doi: 10.1371/journal.pgen.1007412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hsu PJ, Zhu Y, Ma H, Guo Y, Shi X, Liu Y, et al. Ythdc2 is an N6-methyladenosine binding protein that regulates mammalian spermatogenesis. Cell Res. 2017;27:1115–27. doi: 10.1038/cr.2017.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liu N, Dai Q, Zheng G, He C, Parisien M, Pan T. N(6)-methyladenosine-dependent RNA structural switches regulate RNA-protein interactions. Nature. 2015;518:560–4. doi: 10.1038/nature14234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Edupuganti RR, Geiger S, Lindeboom RGH, Shi H, Hsu PJ, Lu Z, et al. N6-methyladenosine (m6A) recruits and repels proteins to regulate mRNA homeostasis. Nat Struct Mol Biol. 2017;24:870–8. doi: 10.1038/nsmb.3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Huang H, Weng H, Sun W, Qin X, Shi H, Wu H, et al. Recognition of RNA N6-methyladenosine by IGF2BP proteins enhances mRNA stability and translation. Nat Cell Biol. 2018;20:285–95. doi: 10.1038/s41556-018-0045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Meng Q, Schatten H, Zhou Q, Chen J. Crosstalk between m6A and coding/non-coding RNA in cancer and detection methods of m6A modification residues. Aging (Albany NY) 2023;15:6577–619. doi: 10.18632/aging.204836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu W, Wang JZ, Xu Z, Cao M, Hu Q, Pan C, et al. Detection of N6-methyladenosine modification residues (Review) Int J Mol Med. 2019;43:2267–78. doi: 10.3892/ijmm.2019.4169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Deng X, Chen K, Luo GZ, Weng X, Ji Q, Zhou T, et al. Widespread occurrence of N6-methyladenosine in bacterial mRNA. Nucleic Acids Res. 2015;43:6557–67. doi: 10.1093/nar/gkv596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Su D, Chan CT, Gu C, Lim KS, Chionh YH, McBee ME, et al. Quantitative analysis of ribonucleoside modifications in tRNA by HPLC-coupled mass spectrometry. Nat Protoc. 2014;9:828–41. doi: 10.1038/nprot.2014.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yuen KC, Xu B, Krantz ID, Gerton JL. NIPBL controls RNA biogenesis to prevent activation of the stress kinase PKR. Cell Rep. 2016;14:93–102. doi: 10.1016/j.celrep.2015.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Li Z, Weng H, Su R, Weng X, Zuo Z, Li C, et al. FTO plays an oncogenic role in acute myeloid leukemia as a N6-methyladenosine RNA demethylase. Cancer Cell. 2017;31:127–41. doi: 10.1016/j.ccell.2016.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hafner M, Landthaler M, Burger L, Khorshid M, Hausser J, Berninger P, et al. Transcriptome-wide identification of RNA-binding protein and microRNA target sites by PAR-CLIP. Cell. 2010;141:129–41. doi: 10.1016/j.cell.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chen K, Lu Z, Wang X, Fu Y, Luo GZ, Liu N, et al. High-resolution N(6)-methyladenosine (m(6) A) map using photo-crosslinking-assisted m(6) A sequencing. Angew Chem Int Ed Engl. 2015;54:1587–90. doi: 10.1002/anie.201410647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Dierks D, Garcia-Campos MA, Uzonyi A, Safra M, Edelheit S, Rossi A, et al. Multiplexed profiling facilitates robust m6A quantification at site, gene and sample resolution. Nat Methods. 2021;18:1060–7. doi: 10.1038/s41592-021-01242-z. [DOI] [PubMed] [Google Scholar]
- 98.Dominissini D, Moshitch-Moshkovitz S, Amariglio N, Rechavi G. Transcriptome-wide mapping of N6-methyladenosine by m6A-seq. Methods Enzymol. 2015;560:131–47. doi: 10.1016/bs.mie.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 99.Kortel N, Ruckle C, Zhou Y, Busch A, Hoch-Kraft P, Sutandy FXR, et al. Deep and accurate detection of m6A RNA modifications using miCLIP2 and m6Aboost machine learning. Nucleic Acids Res. 2021;49:e92. doi: 10.1093/nar/gkab485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang Z, Chen LQ, Zhao YL, Yang CG, Roundtree IA, Zhang Z, et al. Single-base mapping of m6A by an antibody-independent method. Sci Adv. 2019;5:eaax0250. doi: 10.1126/sciadv.aax0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Meyer KD. DART-seq: an antibody-free method for global m6A detection. Nat Methods. 2019;16:1275–80. doi: 10.1038/s41592-019-0570-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Shu X, Cao J, Cheng M, Xiang S, Gao M, Li T, et al. A metabolic labeling method detects m6A transcriptome-wide at single base resolution. Nat Chem Biol. 2020;16:887–95. doi: 10.1038/s41589-020-0526-9. [DOI] [PubMed] [Google Scholar]
- 103.Wang Y, Xiao Y, Dong S, Yu Q, Jia G. Antibody-free enzyme-assisted chemical approach for detection of N6-methyladenosine. Nat Chem Biol. 2020;16:896–903. doi: 10.1038/s41589-020-0525-x. [DOI] [PubMed] [Google Scholar]
- 104.Molinie B, Wang J, Lim KS, Hillebrand R, Lu ZX, Van Wittenberghe N, et al. m(6)A-LAIC-seq reveals the census and complexity of the m(6)A epitranscriptome. Nat Methods. 2016;13:692–8. doi: 10.1038/nmeth.3898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Xiao Y, Wang Y, Tang Q, Wei L, Zhang X, Jia G. An elongation- and ligation-based qPCR amplification method for the radiolabeling-free detection of locus-specific N6-methyladenosine modification. Angew Chem Int Ed Engl. 2018;57:15995–6000. doi: 10.1002/anie.201807942. [DOI] [PubMed] [Google Scholar]
- 106.Liu N, Parisien M, Dai Q, Zheng G, He C, Pan T. Probing N6-methyladenosine RNA modification status at single nucleotide resolution in mRNA and long noncoding RNA. RNA. 2013;19:1848–56. doi: 10.1261/rna.041178.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Grewal AS, Jones J, Lin A. Palliative radiation therapy for head and neck cancers. Int J Radiat Oncol Biol Phys. 2019;105:254–66. doi: 10.1016/j.ijrobp.2019.05.024. [DOI] [PubMed] [Google Scholar]
- 108.Ghaye B, Wanet M, El Hajjam M. Imaging after radiation therapy of thoracic tumors. Diagn Interv Imaging. 2016;97:1037–52. doi: 10.1016/j.diii.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 109.LaRue SM, Gillette SM, Poulson JM. Radiation therapy of thoracic and abdominal tumors. Semin Vet Med Surg Small Anim. 1995;10:190–6. [PubMed] [Google Scholar]
- 110.Farooqi A, Mitra D, Guadagnolo BA, Bishop AJ. The evolving role of radiation therapy in patients with metastatic soft tissue sarcoma. Curr Oncol Rep. 2020;22:79. doi: 10.1007/s11912-020-00936-5. [DOI] [PubMed] [Google Scholar]
- 111.Zhao BS, Roundtree IA, He C. Post-transcriptional gene regulation by mRNA modifications. Nat Rev Mol Cell Biol. 2017;18:31–42. doi: 10.1038/nrm.2016.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang Y, Gu W, Shao Y. The therapeutic targets of N6-methyladenosine (m6A) modifications on tumor radioresistance. Discov Oncol. 2023;14:141. doi: 10.1007/s12672-023-00759-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Taketo K, Konno M, Asai A, Koseki J, Toratani M, Satoh T, et al. The epitranscriptome m6A writer METTL3 promotes chemo- and radioresistance in pancreatic cancer cells. Int J Oncol. 2018;52:621–9. doi: 10.3892/ijo.2017.4219. [DOI] [PubMed] [Google Scholar]
- 114.Xu X, Zhang P, Huang Y, Shi W, Mao J, Ma N, et al. METTL3-mediated m6A mRNA contributes to the resistance of carbon-ion radiotherapy in non-small-cell lung cancer. Cancer Sci. 2023;114:105–14. doi: 10.1111/cas.15590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wang Y, Wang C, Guan X, Ma Y, Zhang S, Li F, et al. PRMT3-mediated arginine methylation of METTL14 promotes malignant progression and treatment resistance in endometrial carcinoma. Adv Sci (Weinh) 2023;10:e2303812. doi: 10.1002/advs.202303812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang Y, Zhang L, Sun XL, Lu YC, Chen S, Pei DS, et al. NRP1 contributes to stemness and potentiates radioresistance via WTAP-mediated m6A methylation of Bcl-2 mRNA in breast cancer. Apoptosis. 2023;28:233–46. doi: 10.1007/s10495-022-01784-3. [DOI] [PubMed] [Google Scholar]
- 117.Chen Y, Zhou P, Deng Y, Cai X, Sun M, Sun Y, et al. ALKBH5-mediated m6 A demethylation of TIRAP mRNA promotes radiation-induced liver fibrosis and decreases radiosensitivity of hepatocellular carcinoma. Clin Transl Med. 2023;13:e1198. doi: 10.1002/ctm2.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Du H, Zou NY, Zuo HL, Zhang XY, Zhu SC. YTHDF3 mediates HNF1α regulation of cervical cancer radio-resistance by promoting RAD51D translation in an m6A-dependent manner. FEBS J. 2023;290:1920–35. doi: 10.1111/febs.16681. [DOI] [PubMed] [Google Scholar]
- 119.Hao CC, Xu CY, Zhao XY, Luo JN, Wang G, Zhao LH, et al. Up-regulation of VANGL1 by IGF2BPs and miR-29b-3p attenuates the detrimental effect of irradiation on lung adenocarcinoma. J Exp Clin Cancer Res. 2020;39:256. doi: 10.1186/s13046-020-01772-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang P, Long F, Lin H, Wang S, Wang T. Dietary phytochemicals targeting Nrf2 to enhance the radiosensitivity of cancer. Oxid Med Cell Longev. 2022;2022:7848811. doi: 10.1155/2022/7848811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Arumugam T, Ghazi T, Chuturgoon AA. Fumonisin B1 alters global m6A RNA methylation and epigenetically regulates Keap1-Nrf2 signaling in human hepatoma (HepG2) cells. Arch Toxicol. 2021;95:1367–78. doi: 10.1007/s00204-021-02986-5. [DOI] [PubMed] [Google Scholar]
- 122.Mattick JS, Amaral PP, Carninci P, Carpenter S, Chang HY, Chen LL, et al. Long non-coding RNAs: definitions, functions, challenges and recommendations. Nat Rev Mol Cell Biol. 2023;24:430–47. doi: 10.1038/s41580-022-00566-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mercer TR, Dinger ME, Mattick JS. Long non-coding RNAs: insights into functions. Nat Rev Genet. 2009;10:155–9. doi: 10.1038/nrg2521. [DOI] [PubMed] [Google Scholar]
- 124.Wang KC, Chang HY. Molecular mechanisms of long noncoding RNAs. Mol Cell. 2011;43:904–14. doi: 10.1016/j.molcel.2011.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Yin H, Chen L, Piao S, Wang Y, Li Z, Lin Y, et al. M6A RNA methylation-mediated RMRP stability renders proliferation and progression of non-small cell lung cancer through regulating TGFBR1/SMAD2/SMAD3 pathway. Cell Death Differ. 2023;30:605–17. doi: 10.1038/s41418-021-00888-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wang S, Zhang K, Tan S, Xin J, Yuan Q, Xu H, et al. Circular RNAs in body fluids as cancer biomarkers: the new frontier of liquid biopsies. Mol Cancer. 2021;20:13. doi: 10.1186/s12943-020-01298-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kristensen LS, Jakobsen T, Hager H, Kjems J. The emerging roles of circRNAs in cancer and oncology. Nat Rev Clin Oncol. 2022;19:188–206. doi: 10.1038/s41571-021-00585-y. [DOI] [PubMed] [Google Scholar]
- 128.Shao Y, Liu Z, Song X, Sun R, Zhou Y, Zhang D, et al. ALKBH5/YTHDF2-mediated m6A modification of circAFF2 enhances radiosensitivity of colorectal cancer by inhibiting Cullin neddylation. Clin Transl Med. 2023;13:e1318. doi: 10.1002/ctm2.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zhong X, Peng Y, Zhang X, Peng L, Ma K, Huang Y, et al. m6A-modified circ_0124554 promotes colorectal cancer progression and radioresistance through the miR-1184/LASP1 pathway. Pathol Res Pract. 2024;253:154950. doi: 10.1016/j.prp.2023.154950. [DOI] [PubMed] [Google Scholar]
- 130.Wu P, Fang X, Liu Y, Tang Y, Wang W, Li X, et al. N6-methyladenosine modification of circCUX1 confers radioresistance of hypopharyngeal squamous cell carcinoma through caspase1 pathway. Cell Death Dis. 2021;12:298. doi: 10.1038/s41419-021-03558-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yang Z, Verghese M, Yang S, Shah P, He YY. The m6A reader YTHDC2 regulates UVB-induced DNA damage repair and histone modification. Photochem Photobiol. 2024;100:1031–40. doi: 10.1111/php.13904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Guo H, Zeng H, Hu Y, Jiang L, Lei L, Hung J, et al. UVB promotes melanogenesis by regulating METTL3. J Cell Physiol. 2023;238:2161–71. doi: 10.1002/jcp.31077. [DOI] [PubMed] [Google Scholar]
- 133.Xiang Y, Laurent B, Hsu CH, Nachtergaele S, Lu Z, Sheng W, et al. RNA m6A methylation regulates the ultraviolet-induced DNA damage response. Nature. 2017;543:573–6. doi: 10.1038/nature21671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhang S, Dong J, Li Y, Xiao H, Shang Y, Wang B, et al. Gamma-irradiation fluctuates the mRNA N6-methyladenosine (m6A) spectrum of bone marrow in hematopoietic injury. Environ Pollut. 2021;285:117509. doi: 10.1016/j.envpol.2021.117509. [DOI] [PubMed] [Google Scholar]
- 135.Wang B, Dong J, Xiao H, Li Y, Jin Y, Cui M, et al. Metformin fights against radiation-induced early developmental toxicity. Sci Total Environ. 2020;732:139274. doi: 10.1016/j.scitotenv.2020.139274. [DOI] [PubMed] [Google Scholar]
- 136.Mahmood J, Jelveh S, Calveley V, Zaidi A, Doctrow SR, Hill RP. Mitigation of lung injury after accidental exposure to radiation. Radiat Res. 2011;176:770–80. doi: 10.1667/rr2562.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Svendsen ER, Kolpakov IE, Stepanova YI, Vdovenko VY, Naboka MV, Mousseau TA, et al. 137Cesium exposure and spirometry measures in Ukrainian children affected by the Chernobyl nuclear incident. Environ Health Perspect. 2010;118:720–5. doi: 10.1289/ehp.0901412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Giuranno L, Ient J, De Ruysscher D, Vooijs MA. Radiation-induced lung injury (RILI) Front Oncol. 2019;9:877. doi: 10.3389/fonc.2019.00877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hanania AN, Mainwaring W, Ghebre YT, Hanania NA, Ludwig M. Radiation-induced lung injury: assessment and management. Chest. 2019;156:150–62. doi: 10.1016/j.chest.2019.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chen G, Zhao Q, Yuan B, Wang B, Zhang Y, Li Z, et al. ALKBH5-modified HMGB1-STING activation contributes to radiation induced liver disease via innate immune response. Int J Radiat Oncol Biol Phys. 2021;111:491–501. doi: 10.1016/j.ijrobp.2021.05.115. [DOI] [PubMed] [Google Scholar]
- 141.He S, Xu J, Qu JY, Wen Z. Lightening the way of hematopoiesis: infrared laser-mediated lineage tracing with high spatial-temporal resolution. Exp Hematol. 2020;85:3–7. doi: 10.1016/j.exphem.2020.04.009. [DOI] [PubMed] [Google Scholar]
- 142.Orschell CM, Wu T, Patterson AM. Impact of age, sex, and genetic diversity in murine models of the hematopoietic acute radiation syndrome (H-ARS) and the delayed effects of acute radiation exposure (DEARE) Curr Stem Cell Rep. 2022;8:139–49. doi: 10.1007/s40778-022-00214-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Macia IGM, Lucas Calduch A, Lopez EC. Radiobiology of the acute radiation syndrome. Rep Pract Oncol Radiother. 2011;16:123–30. doi: 10.1016/j.rpor.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Rittase WB, Muir JM, Slaven JE, Bouten RM, Bylicky MA, Wilkins WL, et al. Deposition of iron in the bone marrow of a murine model of hematopoietic acute radiation syndrome. Exp Hematol. 2020;84:54–66. doi: 10.1016/j.exphem.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kennedy AR, Maity A, Sanzari JK. A review of radiation-induced coagulopathy and new findings to support potential prevention strategies and treatments. Radiat Res. 2016;186:121–40. doi: 10.1667/RR14406.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wagemaker G. Heterogeneity of radiation sensitivity of hemopoietic stem cell subsets. Stem Cells. 1995;13(Suppl 1):257–60. doi: 10.1002/stem.5530130731. [DOI] [PubMed] [Google Scholar]
- 147.Singh VK, Romaine PL, Newman VL, Seed TM. Medical countermeasures for unwanted CBRN exposures: part II radiological and nuclear threats with review of recent countermeasure patents. Expert Opin Ther Pat. 2016;26:1399–408. doi: 10.1080/13543776.2016.1231805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Peslak SA, Wenger J, Bemis JC, Kingsley PD, Frame JM, Koniski AD, et al. Sublethal radiation injury uncovers a functional transition during erythroid maturation. Exp Hematol. 2011;39:434–45. doi: 10.1016/j.exphem.2011.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Hajishengallis G, Li X, Chavakis T. Immunometabolic control of hematopoiesis. Mol Aspects Med. 2021;77:100923. doi: 10.1016/j.mam.2020.100923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Orford KW, Scadden DT. Deconstructing stem cell self-renewal: genetic insights into cell-cycle regulation. Nat Rev Genet. 2008;9:115–28. doi: 10.1038/nrg2269. [DOI] [PubMed] [Google Scholar]
- 151.Dainiak N, Sorba S. Early identification of radiation accident victims for therapy of bone marrow failure. Stem Cells. 1997;15(Suppl 2):275–85. doi: 10.1002/stem.5530150737. [DOI] [PubMed] [Google Scholar]
- 152.Wang H, Zuo H, Liu J, Wen F, Gao Y, Zhu X, et al. Loss of YTHDF2-mediated m6A-dependent mRNA clearance facilitates hematopoietic stem cell regeneration. Cell Res. 2018;28:1035–8. doi: 10.1038/s41422-018-0082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Gulati GL, Ashton JK, Hyun BH. Structure and function of the bone marrow and hematopoiesis. Hematol Oncol Clin North Am. 1988;2:495–511. [PubMed] [Google Scholar]
- 154.Chen T, Burke KA, Zhan Y, Wang X, Shibata D, Zhao Y. IL-12 facilitates both the recovery of endogenous hematopoiesis and the engraftment of stem cells after ionizing radiation. Exp Hematol. 2007;35:203–13. doi: 10.1016/j.exphem.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 155.Chen L, Hu Y, Zhang M, Liu L, Ma J, Xu Z, et al. METTL14 affects UVB-induced human dermal fibroblasts photoaging via miR-100-3p biogenesis in an m6A-dependent manner. Aging Cell. 2024;23:e14123. doi: 10.1111/acel.14123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Reyes AA, Marcum RD, He Y. Structure and function of chromatin remodelers. J Mol Biol. 2021;433:166929. doi: 10.1016/j.jmb.2021.166929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sun X, Bai C, Li H, Xie D, Chen S, Han Y, et al. PARP1 modulates METTL3 promoter chromatin accessibility and associated LPAR5 RNA m6A methylation to control cancer cell radiosensitivity. Mol Ther. 2023;31:2633–50. doi: 10.1016/j.ymthe.2023.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zhao Y, Wen S, Li H, Pan CW, Wei Y, Huang T, et al. Enhancer RNA promotes resistance to radiotherapy in bone-metastatic prostate cancer by m6A modification. Theranostics. 2023;13:596–610. doi: 10.7150/thno.78687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wang L, Katipally RR, Liang HL, Yang K, Pitroda SP, He C, et al. RNA m6A methylation and MDSCs: roles and therapeutic implications for radiotherapy. Med. 2023;4:863–74. doi: 10.1016/j.medj.2023.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zhou Z, Zhang B, Deng Y, Deng S, Li J, Wei W, et al. FBW7/GSK3β mediated degradation of IGF2BP2 inhibits IGF2BP2-SLC7A5 positive feedback loop and radioresistance in lung cancer. J Exp Clin Cancer Res. 2024;43:34. doi: 10.1186/s13046-024-02959-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Jin Z, Dong Z, Zhao X, Hang X, Lu Y, Zhang Q, et al. Sensitive, rapid detection of NCOA4-m6A towards precisely quantifying radiation dosage on a Cas13a-Microdroplet platform. Biosens Bioelectron. 2023;242:115753. doi: 10.1016/j.bios.2023.115753. [DOI] [PubMed] [Google Scholar]
- 162.Chen H, Zhao X, Yang W, Zhang Q, Hao R, Jiang S, et al. RNA N6-methyladenosine modification-based biomarkers for absorbed ionizing radiation dose estimation. Nat Commun. 2023;14:6912. doi: 10.1038/s41467-023-42665-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zeng Z, Zhang J, Li J, Li Y, Huang Z, Han L, et al. SETD2 regulates gene transcription patterns and is associated with radiosensitivity in lung adenocarcinoma. Front Genet. 2022;13:935601. doi: 10.3389/fgene.2022.935601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Lee JH, Kim S, Jin MS, Kim YC. Discovery of substituted indole derivatives as allosteric inhibitors of m6 A-RNA methyltransferase, METTL3-14 complex. Drug Dev Res. 2022;83:783–99. doi: 10.1002/ddr.21910. [DOI] [PubMed] [Google Scholar]
- 165.Lv D, Gimple RC, Zhong C, Wu Q, Yang K, Prager BC, et al. PDGF signaling inhibits mitophagy in glioblastoma stem cells through N6-methyladenosine. Dev Cell. 2022;57:1466–81.e6. doi: 10.1016/j.devcel.2022.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chen H, Pan Y, Zhou Q, Liang C, Wong CC, Zhou Y, et al. METTL3 inhibits antitumor immunity by targeting m6A-BHLHE41-CXCL1/CXCR2 axis to promote colorectal cancer. Gastroenterology. 2022;163:891–907. doi: 10.1053/j.gastro.2022.06.024. [DOI] [PubMed] [Google Scholar]
- 167.Haigh DB, Woodcock CL, Lothion-Roy J, Harris AE, Metzler VM, Persson JL, et al. The METTL3 RNA methyltransferase regulates transcriptional networks in prostate cancer. Cancers (Basel) 2022;14:5148. doi: 10.3390/cancers14205148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Xu QC, Tien YC, Shi YH, Chen S, Zhu YQ, Huang XT, et al. METTL3 promotes intrahepatic cholangiocarcinoma progression by regulating IFIT2 expression in an m6A-YTHDF2-dependent manner. Oncogene. 2022;41:1622–33. doi: 10.1038/s41388-022-02185-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Yankova E, Blackaby W, Albertella M, Rak J, De Braekeleer E, Tsagkogeorga G, et al. Small-molecule inhibition of METTL3 as a strategy against myeloid leukaemia. Nature. 2021;593:597–601. doi: 10.1038/s41586-021-03536-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Du Y, Yuan Y, Xu L, Zhao F, Wang W, Xu Y, et al. Discovery of METTL3 small molecule inhibitors by virtual screening of natural products. Front Pharmacol. 2022;13:878135. doi: 10.3389/fphar.2022.878135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Liu Y, Liang G, Xu H, Dong W, Dong Z, Qiu Z, et al. Tumors exploit FTO-mediated regulation of glycolytic metabolism to evade immune surveillance. Cell Metab. 2021;33:1221–33.e11. doi: 10.1016/j.cmet.2021.04.001. [DOI] [PubMed] [Google Scholar]
- 172.Su R, Dong L, Li Y, Gao M, Han L, Wunderlich M, et al. Targeting FTO suppresses cancer stem cell maintenance and immune evasion. Cancer Cell. 2020;38:79–96.e11. doi: 10.1016/j.ccell.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Liu Y, Guo Q, Yang H, Zhang XW, Feng N, Wang JK, et al. Allosteric regulation of IGF2BP1 as a novel strategy for the activation of tumor immune microenvironment. ACS Cent Sci. 2022;8:1102–15. doi: 10.1021/acscentsci.2c00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Xiao Z, Li T, Zheng X, Lin L, Wang X, Li B, et al. Nanodrug enhances post-ablation immunotherapy of hepatocellular carcinoma via promoting dendritic cell maturation and antigen presentation. Bioact Mater. 2022;21:57–68. doi: 10.1016/j.bioactmat.2022.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.