Abstract
There have been many studies on human head–neck biomechanical models in the last two decades, and the associated modelling techniques were constantly evolving at the same time. Computational approaches have been widely leveraged, in parallel to conventional physical tests, to investigate biomechanics and injuries of the head–neck system in fields like the automotive industry, orthopedic, sports medicine, etc. The purpose of this manuscript is to provide a global review of the existing knowledge related to the modelling approaches, structural and biomechanical characteristics, validation, and application of the present head–neck models. This endeavor aims to support further enhancements and validations in modelling practices, particularly addressing the lack of data for model validation, as well as to prospect future advances in terms of the topics. Seventy-four models subject to the proposed selection criteria are considered. Based on previously established and validated head–neck computational models, most of the studies performed in-depth investigations of included cases, which revolved around four specific subjects: physiopathology, treatment evaluation, collision condition, and sports injury. Through the review of the recent 20 years of research, the summarized modelling information indicated existing deficiencies and future research topics, as well as provided references for subsequent head–neck model development and application.
Keywords: application, finite element method, human head–neck, multibody method, validation
Introduction
Highlights
Seventy-four models were performed in in-depth investigations during the last two decades, and methodologies primarily focused on application-centered differences, which revolved around four specific subjects: physiopathology, treatment evaluation, collision condition, and sports injury.
Advanced neuromuscular reflex control is being included in biomechanical head–neck models for collision applications, while this important control strategy has yet to be added to the medical models.
Standardization in integrated medicine and engineering can greatly enhance the development and application of modelling processes in this field. By establishing standardized practices, guidelines, and frameworks, the integration of medicine and engineering can become more efficient, reliable, and effective.
Pathogenesis, prevention, treatment, and rehabilitation efforts became the main research directions of head–neck injury biomechanics. To study cervical spine injuries in trauma events in detail, numerical simulation plays an important role in those efforts. It is thus not a surprise that the biomechanical model of the cervical spine has expanded at a rapid pace. Based on the early technique of frequent computational modelling for kinematic analysis1–5, human body models (HBMs) at varying levels have been created by various researchers globally in the last two decades. Previous finite element (FE) or multibody (MB) methods were established and contributed to a better understanding of neck injury mechanisms, which could be used in injury prevention design. Examples included whiplash injuries in traffic accidents, mechanical neck pain in occupational health issues, and degenerative disc diseases in medical intervention. At the application level, several studies developed protective helmets based on the aforementioned models to minimize head and neck injuries under impact loads6,7. Additionally, research has been conducted on the development of cervical traction exoskeletons to aid in the rehabilitation of muscular and neurological injuries in the head and neck region8–11.
However, those models often cast doubt on credibility due to their weak universality12,13. In addition, the MB was employed to analyze the dynamics and motion of the cervical spine or head–neck region, but it cannot easily and accurately obtain tissue stress and strain distribution for detailed injury risk analysis, which probably limits its application. At the beginning of this century, several whole HBMs were developed for injury analysis with the rise of computational resources becoming more accessible14–17. These models are designed to estimate injury under collision conditions regarding automotive safety but are used less in other environments. The development of imaging technologies, in particular, the improved accuracy of computed tomography (CT), makes it possible to reconstruct individualized three-dimensional geometry. Researchers tend to establish individualized models to evaluate and monitor medical interventions in medical simulations18,19. These scenarios include but are not limited to the assessment of driving comfort and the evaluation of motion sickness20–22. In the last two decades, HBMs have had an increasing number of application scenarios. It is believed that models of various applications exhibit disciplinary differences, such as modelling approaches, material properties, validations, etc.
This study aimed to provide a global review of the present knowledge related to human head–neck models over the past two decades. The analysis was performed from global knowledge to dedicated focus on the biomechanical modelling researchers targeted in this work. As shown in Figure 1, the PubMed search terms ‘cervical spine’ and ‘biomechanics model’ showed that the number of articles in this field has increased exponentially over the period23. In addition, this review is intended to provide a thorough understanding of the current state-of-the-art techniques and help inform future developmental efforts to create more accurate and realistic cervical spine models. Although there is a wide array of computational cervical spine models, they have yet to be compared to one another in various aspects of multidisciplinary thresholds to provide information that could be used to improve them so that they better serve current needs. Thus, the modelling approach, structural characteristics, validation, and application of existing computer head–neck models were compared and analyzed. Furthermore, this review outlines what researchers from different backgrounds have achieved with cervical spine models and describes the synthesis of characteristics from multiple disciplines, clarifying the gap in biomechanical head–neck models of interdisciplinary research.
Figure 1.

Frequency of published studies by year.
Methods
Research groups working in the field of cervical spine FE modelling were included in the present study. Only validated models of the head–neck model that were previously published in peer-reviewed journals were considered. This study included common simulation methods that employ either MB models or FE models. The modelling approach, structural characteristics, and validation of different models were reviewed in detail. The selection criteria for studies included in the search were ‘Cervical spine’ OR ‘Head-neck,’ ‘Multibody model’ OR ‘Finite element model,’ Adult HBMs within two decades, Publication in the ‘English’ language. The exclusion criteria were only investigated the upper cervical spine (C0–C2) as well as the lower cervical spine (C3–C7) and unvalidated models, which are regarded as imprecise. The Boolean operators ‘AND,’ ‘OR,’ ‘NOT,’ and the proximity operators ‘PRE/n’ were used to search relevant studies, which were performed through PubMed, Web of Science, Cochrane Library, SAE International, and Google Scholar. Articles cited in all retrieved studies were also searched to gather additional sources, including the grey literature. There were three researchers conducted this survey and collectively reviewed studies that were on the border of inclusion/exclusion criteria. Components evaluated include anatomical structure modelling, muscle structure and its status (active/passive/none), muscle activation type (predefined/feedback-based optimization/EMG driven mode/neuromuscular feedback), personalized muscle parameters, and validation methods (dynamic/quasi-static). A flowchart illustrating the study search and selection process is shown in Figure 2.
Figure 2.

Flowchart illustrating literature search and selection process.
Results
Summary of modelling, validation, and application
A total of 74 neck or hea–-neck models satisfy our selection criteria in this review. Fifty-nine FE models and 15 MB models are reported. Tables 1 and 2 briefly illustrate the modelling approach, structural characteristics, validations, and applications of these models, respectively. The models are chronologically updated in terms of almost all relevant aspects, for example, from simple to complicated in geometry and anatomy, from rigid-body to deformable on tissue material property, and from passive to active on muscle effect. Advances in imaging technologies, for example, CT and MRI, as well as in controlling theory, are essentially beneficial in this evolution. Significant progress has been made in the study of modelling materials, techniques, and valuation methods during the last two decades24. Recent numerical models also tried to include more complicated control strategies, from simple proportional-integral-derivative (PID) control to complex physiological neural feedback control strategies.
Table 1.
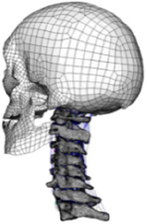
Multipage tables of human head–neck finite element models within retrieved studies in the last two decades.
| First author/year | Robin, 2001 (HUMOS)43 | Ng, 200467 | Meyer, 200444 | Brolin, 2005 (KTH)36 | Ejima, 2005 (JAMA)45 |
|---|---|---|---|---|---|
| Type | FE | FE | FE | FE | FE |
| Software | Radioss | ANSYS | Radioss | LS-DYNA | LS-DYNA |
| Segments | Whole body model | C2–C7 | Head–T1 | Head–T1 | Whole body model |
| Figure |

|

|

|

|

|
| Geometry | CT | 3D digitizer | CT | CT | MRI |
| Head | Viscoelastic | N/A | Rigid/elastoplastic orthotropic68 | Rigid | Head-T1 |
| Vertebra | Elastoplastic | Elastic | Rigid | Viscoelastic/rigid | N/A |
| Disc | Elastic | Elastic | Elastic | Elastic, anisotropic (annulus fibrosis); visco-elastic (annulus matrix); elastic, incompressible (nucleus pulposus) | N/A |
| Facet joint | Contact | Contact | Contact | Contact | Share nodes |
| Ligament | Elastic | Nonlinear cable | Nonlinear spring | Nonlinear beam | N/A |
| Spinal canal | N/A | N/A | Elastic (cerebrospinal fluid)68 | Elastic (dura, pia) incompressible fluid (cerebrospinal fluid)69 | N/A |
| Muscle | Solid with nonlinear springs (passive muscle) | N/A | 1D Hill-type beam (active muscle)68
Solid element (passive muscle) |
1D Hill-type beam (active muscle) 3D solid (passive muscle)70,71 |
3D solid (passive muscle) |
| Muscle activation | N/A | N/A | Predefined68 | Predefined/EMG71 | N/A |
| Muscle structure | N/A | N/A | N/A | Cadaver measurement/MRI modelling70,71 | MRI modelling |
| Elements | 9223 solids 13 458 shells 504 springs |
18 731 elements | 9223 solids 13 458 shells 504 springs |
N/A | 14 734 nodes 7306 solids 6976 shells |
| Validation | 15 g frontal impact 7 g lateral impact 10 g oblique impact72 |
Quasi-static Flx/Ext/LB/AR73,74 | 15 g frontal impact/7 g lateral impact75,76; oblique impact77; rear impact78 | Quasi-static compression/shear/ torsion for LCS5,79,80; Flx/Ext/LB/AR/tension for UCS81–84; compression/Flx/LB/oblique impacts for whole cervical spine5,72,85–89; frontal/rear/lateral/oblique impacts72,87,90 | 4 g rear impact91 |
| Application | In Tropiano, 200492: whiplash trauma simulation based on the HUMOS model43 by imposing a rear impact | In Ng, 2004, 200539,67,93: intersegment stability and osteophyte formation in C2–C7 laminectomy with unilateral and bilateral facetectomy | In Meyer, 2013, 2019, 202168,94,95: injury risk criteria and forces/moments in cervical segments based on Meyer, 200444 under different impact scenarios | In Kleiven, 200669, Hedenstierna, 2008, 200970,71: Evaluation of head injury criteria and neck muscles responses based on the KTH model36 during different impact scenarios | Evaluation of neck passive muscles responses during rear impact |
| First author/year | Zhang, 200640 | Frechede, 200696 | del Palomar, 200841 | Kitagawa, 2008 (THUMS)15 | Tchako, 200942 |
| Type | FE | FE | FE | FE | FE |
| Software | ANSYS/LS-DYNA | RADIOSS | ABAQUS | LS-DYNA | ANSYS |
| Segments | Head–C7 | Head–T1 | C1–C7 | Whole body model | C1–T1 |
| Figure |

|

|

|

|

|
| Geometry | 3D digitizer | Hybrid III dummy (Head) Geometric modelling (C2-T1) |
CT | CT | Digitized geometrical measurement |
| Head | Elastic | Rigid | N/A | Hyperelastic | N/A |
| Vertebra | Elastic | Rigid | Rigid | Elasto-viscoplastic (cortical bone) Elastic viscoplastic (cancellous bone) |
Elastic |
| Disc | Elastic | Viscoelastic | Hyperelastic (annulus matrix/nucleus pulposus); elastic (annulus fibrosis) | Seatbelt (annulus fibrosis); viscoelastic (annulus matrix); isotropic plasticity (nucleus pulposus) | Elastic |
| Facet joint | Contact | Contact | Frictional contact | Contact | Contact |
| Ligament | Elastic/nonlinear link97 | Viscoelastic spring | Nonlinear truss | Nonlinear shell | Nonlinear spring |
| Spinal canal | N/A | N/A | N/A | Hyperelastic (epidural fat) Orthotropic nonlinear elastic (dura, pia) Incompressible fluid (cerebrospinal fluid) Viscoelastic (cord) |
N/A |
| Muscle | 1D springs (passive muscle)98 | 3D viscoelastic solid (passive muscle) | N/A | Hill-type 1D beam (active muscle)99 3D hyperelastic solid (passive muscle) | 1D elastic spring (passive muscle) |
| Muscle activation | N/A | N/A | N/A | EMG99,100 | N/A |
| Muscle structure | Cadaver measurement | Cadaver measurement | N/A | Visible human subject101 | Cadaver measurement |
| Elements | 22 094 elements | N/A | N/A | About 80 000 elements | 19 953 solids 7605 shells 434 springs/cables |
| Validation | Quasi-static Flx/Ext/LB/AR73,74,102–107; 5 g/8 g rear impact108; In Zhang et al.109: 3.2 m/s drop test110; 2.6 m/s rear impact111 | 15 g frontal impact 7 g lateral impact 10 g oblique impact 7 g rear impact72,78,112–114 |
Quasi-static Flx/Ext/LB/AR40,102,115 | 3 g/15 g frontal impact75,116–118
7 g lateral impact119 4 g rear impact91 Dynamic axial loading86 |
Quasi-static Flx/Ext/LB/AR74,120,121 |
| Application | In Teo, 2007122, Zhang, 200897,98: Head–neck kinematics based on Zhang, 200440 during different impact orientations/accelerations | Relation between curvature and risk of injury during omni-directional impacts | Mechanisms of disc injury (maximum shear strains) under quasi-static loading | In Iwamoto, 200999, Kato, 2018101: Muscle Effects of muscle activity in pre-impact on the bone responses based on the THUMS model15 | In Tchako, 200942,123: external and internal responses of the spinal components to disc herniation and clinical instability under diving and football accidents; simulated stress response in intervertebral discs of partial discectomies and fusion surgeries |
| First author/year | Laville, 200955 | Espinha, 2010124 | Kallemeyn, 2010125 | Li, 2010126 | Toosizadeh, 2011127 |
| Type | FE | FE | FE | FE | FE |
| Software | Radioss | ABAQUS | ABAQUS | ABAQUS | ANSYS |
| Segments | C0–T4 | C1–T1 | C2–C7 | C1–C7 | C0–C7 |
| Figure |

|

|

|

|

|
| Geometry | EOS/MRI (biplanar X-rays) | CT | CT | CT | CT |
| Head | Rigid | N/A | N/A | N/A | Rigid |
| Vertebra | Elastic | Elastic | Elastic | Anisotropy elastic (cortical/cancellous bone) | Orthotropic/isotropic elastic |
| Disc | Elastic | Elastic | Elastic (annulus fibrosis/matrix) Incompressible fluid (nucleus pulposus) |
Elastic | Hyperelastic (annulus matrix) Nonlinear link (annulus fibrosis) Incompressible fluid (nucleus pulposus) |
| Facet joint | Contact | Hard contact | Elastic | N/A | Frictional contact |
| Ligament | Bilinear spring/shell | N/A | Nonlinear truss | Elastic | Nonlinear spring |
| Spinal canal | N/A | N/A | N/A | N/A | N/A |
| Muscle | Hill-type 1D spring (active muscle) 3D solid (passive muscle) |
N/A | N/A | N/A | Optimization (equilibrium algorithm) |
| Muscle activation | Predefined | N/A | N/A | N/A | N/A |
| Muscle structure | MRI modelling | N/A | N/A | N/A | N/A |
| Elements | 37 000 solids 30 500 shells 41 500 springs 60 000 nodes |
N/A | About 130 000 elements | 264 301 elements 67 033 nodes | N/A |
| Validation | Quasi-static compression/Flx/Ext/LB/AR73,74,115,128–131 | Physiological model measurement for bone mass | Quasi-static Flx/Ext/LB/AR (in house experiments) | Quasi-static Flx/Ext/LB/AR40,73,109,115 | Quasi-static Flx/Ext/LB/AR40,104,115,132 |
| Application | Influence of geometrical parameters (cervical spine) on the motion patterns | Influence of the spine instrumentation on bone remodelling (fusion process) after an ACDF | In Kode, 2014133, Gandhi, 2019134, Stoner, 2020135: Based on Kallemeyn, 2010125, investigated kinematics and stress/strain responses (tissue/instrument) of disc degeneration, multi-level laminoplasty, laminectomy, ACDF, and ADR | In Li, 2010126: Association between degenerative disc extent and responses of cervical spine; In Qi, 2016136: Kinematics and stress (instrument/graft material) response of ACD, ACDF, and ADR | Relationship between required muscle forces and neck angle for the quasi-static condition (Risk factor for neck pain and arthritis) |
| First author/year | Panzer, 2011137 | Zhang, 2011138 | Lee, 201118 | Rosli, 2011139 | Wagnac, 2012 (S2MS)140 |
| Type | FE | FE | FE | FE | FE |
| Software | LS-DYNA | LS-DYNA | ABAQUS | CosmosWork | Radioss |
| Segments | Head–T1 | C1–T1 | C2–C7 | C1–C7 | Complete spine |
| Figure |

|

|

|

|

|
| Geometry | CT | CT | CT | CT | CT |
| Head | Rigid | Rigid | N/A | N/A | N/A |
| Vertebra | Rigid | Elastic | Elastic | Elastic | Elastoplastic |
| Disc | Hyperelastic (annulus matrix) Nonlinear elastic (annulus fibrosis) Linear visoelastic (nucleus pulposus) | Elastic | Elastic | N/A | Viscoelastic |
| Facet joint | Contact | N/A | Contact | N/A | Contact |
| Ligament | Nonlinear spring | Elastic cable/solid | Elastic | Elastic | Nonlinear spring/shell |
| Spinal canal | N/A | N/A | N/A | N/A | N/A |
| Muscle | Hill-type 1D beam (active muscle) | 1D beam (passive muscle) | N/A | N/A | N/A |
| Muscle activation | Predefined | N/A | N/A | N/A | N/A |
| Muscle structure | Cadaver measurement | Literatures observations | N/A | N/A | N/A |
| Elements | 108 354 elements | 35 042 nodes 22 618 elements | 38 984 nodes 77 991 elements | N/A | 740 000 elements |
| Validation | 8 g/22 g frontal impact141,142
In Fice, 201154: 4 g/7 g/8 g rear impact143–147 Ligaments strain threshold148 |
4 g rear impact143
Dynamic response in injury position149 |
Quasi-static Flx/Ext/LB/AR67,73,150–152 | C4-6 1.0 N-m extension73,153,154 | Quasi-static compression/Flx/Ext; dynamic Flx and Ext |
| Applicatiioonn | In Fice, 2012155, Cronin, 2014156, Shateri, 2015157: Biofidelic kinematic and local tissue response of full head-neck in different impact scenarios based on Panzer and Fice’s model54,137 | Kinematic and local tissue response of cervical spine in whiplash injury | In Lee, 2016158: biomechanical response of different types in ADR devices based on the Lee, 201118 | In Rosli, 2014159: stability of cervical spine after one-level corpectomy using different numbers of screws and plate systems based on the Rosli, 2011139 | Healthy spine subject approximating to the 50th percentile of European male |
| First author/year | Gayzik, 2012 (GHBMC)37 | Wei, 2013160 | Xie, 2013161 | Mesfar, 2013162 | Erbulut, 2014163 |
| Type | FE | FE | FE | FE | FE |
| Software | LS-DYNA | ANSYS | ABAQUS | ABAQUS | ABAQUS |
| Segments | Whole body model | C1–C7 | C2–C7 | Head–T1 | C2–T1 |
| Figure |

|

|

|
|

|
| Geometry | MRI and CT | CT | CT | CT/MRI | CT |
| Head | Viscoelastic | N/A | N/A | Rigid | N/A |
| Vertebra | Elastoplastic | Elastic | Elastic | Rigid | Elastic |
| Disc | Viscoelastic (annulus matrix) Orthotropic nonlinear elastic (annulus fibrosis) Elastic fluid (nucleus pulposus) |
Elastic | Elastic | Elastic | Elastic |
| Facet joint | Contact | Contact | Frictionless contact | Contact | Contact |
| Ligament | Nonlinear spring | Nonlinear spring | Nonlinear spring | Nonlinear spring/shell | Elastic truss |
| Spinal canal | Visoelastic (spinal cord/ cerebrospinal fluid); elastic (arachnoid/dura) | N/A | N/A | N/A | N/A |
| Muscle | Separated muscle bundles with 3D solid elements (passive muscle) Hill-Type 1D beam (active muscle) |
N/A | N/A | N/A | N/A |
| Muscle activation | Predefined164 | N/A | eN/A | N/A | N/A |
| Muscle structure | MRI modelling | N/A | N/A | N/A | N/A |
| Elements | Whole body model: 2 192 031 elements | 189 527 solids 62 834 shells 596 springs |
352 029 elements | N/A | 106 547 elements |
| Validation | High-rate Flx/Ext (C2–T1) [University of Waterloo experimental testing]; Quasi-static Flx/Ext (C2–T1)115,132,149,165; Quasi-static tension (C2–T1)166; Spine intervertebral junctions from C2–C3 through C6–C7 for Frontal/rear Impact, investigating strain in CL, PLL, ALL, anterior and posterior disk shear strain141,146,147,167,168; C0–T1 AR169,170; Full neck model for tension166; 3.6 g/7 g rear impact77,143,171,172; 7 g lateral impact77,172; 8 g/15 g front impact77,172 | Quasi-static Flx/Ext/LB/AR74,102 | Quasi-static Flx/Ext/LB/AR18,40,73,115 | Quasi-static Flx-Ext73,115 | Quasi-static Flx/Ext/LB/AR40,115,132,137,149,173 |
| Application | In White, 2015174, Corrales, 202156,175,176, Whyte, 2021177: base on the GHBMC model37, investigated neck response and kinematics under impact scenarios and multiaxial transverse shear loading; the influences of capsular joint cartilage geometry, sex, age, stature, vestibulocollic, and cervicocollic muscle reflexes under quasi-static/dynamic loading; quantifying the active muscle repositioning under flexion178; spinal cord affect brain tissue strains in impact179 | Comparison between straightened and normal physiological curvature in cervical spine | Comparison among laminectomy, hemilaminectomy, and novel MIS treatment of multilevel intradural tumour | Effect of the transverse ligament rupture on biomechanical response of head-neck under a compression | In Erbulut, 2014163, Zafarparandeh, 2016180, Mumtaz, 2022181: role of soft tissues in stability, and sensitivity of FE model to geometry; biomechanical differences among single, multilevel and hybrid disc replacement surgery with dynamic cervical implant and fusion |
| First author/year | Howley, 2014182 | Wang, 2014183 | Chung, 2015184 | Khuyagbaatar, 201519 | Wang, 2016185 |
| Type | FE | FE | FE | FE | FE |
| Software | LS-DYNA | ABAQUS | ABAQUS | ABAQUS | ABAQUS |
| Segments | Head–T6 | Head–T1 | C2–C7 | C2–C7 | C2–T1 |
| Figure |

|

|

|

|

|
| Geometry | MRI | CT | CT | CT | Visible human project/MRI |
| Head | Rigid | Rigid | N/A | N/A | N/A |
| Vertebra | Elastic | Elastic | Elastic | Rigid | Elastic |
| Disc | Hyperelastic (annulus matrix) Hyperelastic anisotropic transverse (annulus fibrosis) Incompressible fluid (nucleus pulposus) |
Elastic | Hyperelastic (annulus fibrosis/nucleus pulposus) | Rigid | Hyperelastic |
| Facet joint | Contact | Frictionless contact | Frictionless contact | N/A | Frictional contact |
| Ligament | Bilinear spring | Elastic truss | Elastic truss | Rigid | Nonlinear spring |
| Spinal canal | N/A | N/A | N/A | Hyperelastic (spinal cord); elastic (dura matter/nerve roots); viscoelastic (cerebrospinal fluid) | N/A |
| Muscle | Hill-type 1D spring (active muscle) 3D solid (passive muscle) |
N/A | N/A | N/A | N/A |
| Muscle activation | EMG | N/A | N/A | N/A | N/A |
| Muscle structure | MRI combined with personalisation (mesh deformation) | N/A | N/A | N/A | N/A |
| Elements | N/A | N/A | N/A | N/A | N/A |
| Validation | Quasi-static Flx/Ext/LB/AR | / in quasi-static Flx/Ext/LB/AR (in vivo kinematic capture) | Quasi-static Flx/Ext/LB/AR125 | Impact compression for dural sheath and whole spinal cord186,187 | Quasi-static Flx/Ext/LB/AR115,129,130 |
| Application | A framework for orthopaedic applications towards personalisation and active muscle integration in a head–neck FE model | A novel method towards in vivo experiment (motion capture) and FE model integration | Kinematics and instrument stress of two-level ADR and intervertebral Cage (hybrid cervical surgery) | In Khuyagbaatar, 2015, 201619,188: Simulated different types of OPLL on mechanical stress in spinal cord, and biomechanical mechanisms in three types of SCI; in Khuyagbaatar, 2016, 2017, 201863,189–191: evaluated stress and strain of spinal cord due to OPLL in the cervical spine under flexion after laminectomy; postoperative C5 palsy due to OPLL in different types of cervical spinal alignment; biomechanical effects between open-door and double-door laminoplasty on spinal cord and nerve root following laminoplasty for OPLL | In Wang, 2016, 2017185,192: kinematics and load-sharing pattern of resection or degeneration of uncovertebral joints altered; anterior plating failure in treating distractive flexion injury In Liu, 2021193: length and density of instruments in anterior/posterior cervical approach for ankylosing spondylitis cervical spine fracture |
| First author/year | Östh, 201614 | Deng, 2017194 | Wang, 2017195 | Rong, 2017196 | Gadomski, 2018197 |
| Type | FE | FE | FE | FE | FE |
| Software | LS-DYNA | ABAQUS | ABAQUS | ABAQUS | ABAQUS |
| Segments | Head–neck model | C2–T1 | C0–T1 | C2–C7 | C0–C7 |
| Figure |

|

|

|

|

|
| Geometry | CT | CT | CT | CT | CT |
| Head | Rigid | N/A | Elastic | N/A | Elastic/orthotropic |
| Vertebra | Elastoplastic | Elastic | Elastic | Elastic | Elastic/orthotropic |
| Disc | Viscoelastic (annulus matrix/nucleus pulposus) Orthotropic nonlinear elastic (annulus fibrosis) |
Elastic | Elastic | Elastic | Elastic |
| Facet joint | Contact | Frictionless contact | Frictionless contact | Frictionless contact | Contact |
| Ligament | Nonlinear membrane | Elastic truss | Elastic truss | Elastic | Nonlinear spring |
| Spinal canal | N/A | N/A | N/A | N/A | Hyperelastic (spinal cord) |
| Muscle | 1D beam elements of Hill muscles (active muscle) | N/A | N/A | N/A | N/A |
| Muscle activation | Feedback-based optimization198 | N/A | N/A | N/A | N/A |
| Muscle structure | Cadaver measurement199 | N/A | N/A | N/A | N/A |
| Elements | 115 801 elements, 35 441 nodes | N/A | 255 401 elements, 351 541 nodes | N/A | N/A |
| Validation | Anatomic measurements200,201; ligaments tension202–204; quasi-static Flx/Ext/LB/AR73,115,149; LCS segment compliance153; spinal alignment assessment205; modelling reflex recruitment of neck muscles in a HBM for simulating omnidirectional head kinematics199; segmental instantaneous centres of rotation evaluation199; 1.3 m/s and 2.6 m/s rear impact206–208 | Quasi-static Flx/Ext/LB/AR73,74,115,132,209 | Quasi-static Flx/Ext/LB/AR40,73 | Quasi-static Flx/Ext/LB/AR73,158,210 | FE-modeled motion was compared with experimentally measured motion |
| Application | In Putra, 2019, 2021, 202257,198,211: Implemented a control strategy to neural feedback from the vestibular system and muscle spindles under whiplash injury based on the VIVA model14,199; active reflexive muscles suitable for sex based whiplash injury prediction212 | Disc responses of cervical traction therapy with and without neck support; Disc nucleus pulposus pressure in cervical spine positioning rotation manipulation213 | Disc responses of traditional Chinese manipulation | Influence of facet tropism on the intervertebral disc and facet joints in the cervical spine | Kinematics and spinal cord responses of intact cervical spines undergoing endotracheal intubation |
| First author/year | Mihara, 2018214 | Yan, 2018215 | John, 2019216 | Park, 2019217 | Xie, 2019218 |
| Type | FE | FE | FE | FE | FE |
| Software | LS-DYNA | LS-DYNA | LS-DYNA | ABAQUS | ABAQUS |
| Segments | C2–T2 | Head–neck | Head–neck | C2–C7 | C2–C7 |
| Figure |

|

|

|

|

|
| Geometry | Visible human project | MRI | CT | CT | CT |
| Head | N/A | Elastic | Rigid | N/A | N/A |
| Vertebra | Elastic | Elastoplastic | Elastoplastic | Elastic | Elastic |
| Disc | Elastic | Elastic | Viscoelastic (annulus matrix) Orthotropic nonlinear elastic (annulus fibrosis) Viscoelastic (nucleus pulposus) |
Elastic | Elastic |
| Facet joint | Contact | Contact | Contact | Contact | Frictionless contact |
| Ligament | N/A | Nonlinear spring | Nonlinear membrane | Nonlinear truss | Nonlinear truss |
| Spinal canal | Elastic (dura mater/nerve root/brachial plexus) | Elastic (pia matter/falx and tentorium) Viscoelastic (cerebral/cerebellum/brain stem/cerebrospinal fluid) |
N/A | N/A | N/A |
| Muscle | N/A | Hill-type 1D beam (active muscle) 3D solid (passive muscle) |
Hill-type 1D truss (passive muscle) | N/A | N/A |
| Muscle activation | N/A | Predefined | N/A | N/A | N/A |
| Muscle structure | N/A | MRI | Cadaver measurement | N/A | N/A |
| Elements | 82 011 elements 285 694 nodes | 554 154 elements 620 899 nodes |
N/A | N/A | 130 429 elements 30 181 nodes |
| Validation | Based on brachial plexus injury reported clinically219,220 | 15 g front impact87
4 g rear impact143,221 7 g lateral impact76 |
Anatomical measurement200,222,223; 2.3 m/s rear impact208 |
Quasi-static Flx/Ext/LB/AR73 | Quasi-static Flx/Ext/LB/AR73,74,224 |
| Application | Kinematics in pathological conditions of brachial plexus injuries | Influence of neck active force on the head–neck dynamic response and whiplash injury (low-speed collision) | In John, 2019216, Purushothaman, 2021225: effect of variations in cervical spine morphology, sex and head inertia properties on segmental rotation in rear-impact whiplash loading/G-x accelerative loading; in Yoganandan, 2020226: effects of different severities of disc degeneration on the range of motion of cervical spine based on the John, 2019216; in Choi, 2020, 2021227,228, John, 2020229, Purushothaman, 2020230: kinematics and tissue responses in the index and adjacent levels of the human cervical spine after ACDF, and ADR with different types; influence of sagittal alignment of the cervical spine on the development of radiological adjacent segment pathology after central corpectomy. In Varghese, 2022231: a normalization technique was developed for scaling MRI data into FE model | Influence of extragraft bone formation on operated motion segment after ACDF | Biomechanical strategy for hybrid surgical strategy in three-level cervical degenerative disc disease |
| First author/year | Bailly, 202049 | Herron, 202050 | Hua, 2020232 | Li, 2020233 | Subramani, 2020234 |
| Type | FE | FE | FE | FE | FE |
| Software | Radioss | FEBio | OptiStruct | ABAQUS | LS-DYNA |
| Segments | C2–T1 | C0–T1 | C2–C7 | C2–T1 | C2–C7 |
| Figure |

|
|

|

|

|
| Geometry | CT | Previous FE model and visible human project | CT | CT | BodyParts3D |
| Head | N/A | Rigid | N/A | N/A | N/A |
| Vertebra | Rigid | Orthotropic elastic/neo-Hookean | Elastic | Elastic | Elastoplastic |
| Disc | Hyperelastic (annulus matrix/nucleus pulposus) Nonlinear spring (annulus fibrosis) |
Hyperelastic (annulus matrix/nucleus pulposus) Fiber-exponential-power (annulus fibrosis) |
Elastic | Elastic | Hyperelastic (annulus matrix/nucleus pulposus) |
| Facet joint | Frictionless contact | Sliding-tension-compression contact | Frictionless contact | Frictional contact | Contact |
| Ligament | Nonlinear shell | Nonlinear spring | Linear contact elements | Elastic | Linear beam |
| Spinal canal | Elastic (dura mater/pia matter/denticulate ligaments) Viscoelastic (white matter/grey matter) |
N/A | N/A | N/A | N/A |
| Muscle | N/A | N/A | N/A | N/A | N/A |
| Muscle activation | N/A | N/A | N/A | N/A | N/A |
| Muscle structure | N/A | N/A | N/A | N/A | N/A |
| Elements | 391 941 elements 90 523 nodes (spinal canal excluded)62 |
185 826/185 382/164 118 elements (3 models, respectively) | 2 908 691 elements 783 503 nodes235 |
152 608 elements 41 797 nodes |
N/A |
| Validation | FSU moment-rotation of 500 deg/s hyperextension236; In Beauséjour, 202062: Quasi-static Flx-Ext115,149; IDP (Flx) in C3-C4, C5-C6237 | Quasi-static Flx/Ext/LB/AR14,73,104,153,209,238–240; Facet Contact Force238,241,242; IDP in C2-C3, C6-C7237,243,244; Disc measurements245 |
Quasi-static Flx/Ext/LB/AR18,73 | Quasi-static Flx/Ext/LB/AR115,129,130,246 | Anatomical measurement247,248; Quasi-static Flx/Ext/LB/AR73 |
| Application | In Bailly, 202049, Lévy, 2020249, Beauséjour, 202062: effect of spinal cord compression types, disc bulging and ligamentum flavum hypertrophy on degenerative cervical myelopathy; effect of injured posterior ligamentous complex and intervertebral disc on post-traumatic cervical spine instability | Biomechanical behaviours of morphological differences between various FE models | In Hua, 2020232,235: kinematics and tissue responses of ASD after one-level or two-level ACDF (cage-plate, zero-profile), and ADR | In Li, 2020, 2021233,250: impact of ASD after single-level ACDF with zero-profile versus cage-plate construct | Fatigue damage prediction in the annulus of cervical spine intervertebral discs for neck pain |
| First author/year | Sun, 2020251 | Wong, 202051 | Barker, 2021252 | Cao, 2021253 | Nasim, 2021254 |
| Type | FE | FE | FE | FE | FE |
| Software | ABAQUS | ABAQUS | LS-DYNA | ANSYS | LS-DYNA |
| Segments | C2–C7 | C2–C7 | Head–neck | C1–C7 | Head–neck |
| Figure |

|

|

|

|

|
| Geometry | CT | CT | CT/MRI | CT | Morphometric |
| Head | N/A | N/A | Elastoplastic | N/A | Rigid |
| Vertebra | Elastic | Elastic | Elastoplastic | Elastic/Elastoplastic | Elastic |
| Disc | Elastic | Elastic | Viscoelastic (annulus matrix) Orthotropic nonlinear elastic (annulus fibrosis) Elastic fluid (nucleus pulposus) |
Elastic (annulus matrix/fibrosis) Hyperelastic (nucleus pulposus) |
Elastic (annulus fibrosis) Viscoelastic (nucleus pulposus) |
| Facet joint | Frictionless contact | Frictional contact | Contact | Contact | Contact |
| Ligament | Linear truss | Nonlinear truss | Nonlinear spring | Linear spring | Nonlinear spring |
| Spinal canal | N/A | N/A | N/A | N/A | Hyperelastic (spinal cord) |
| Muscle | N/A | N/A | 3D solid elements (passive muscle) Hill-type 1D spring/cable (active muscle) |
N/A | N/A |
| Muscle activation | N/A | N/A | Predefined | N/A | N/A |
| Muscle structure | N/A | N/A | MRI modelling | N/A | N/A |
| Elements | N/A | 222 788 elements | 253 397 elements | N/A | 94 997 elements 26 908 nodes |
| Validation | Quasi-static Flx/Ext/LB/AR73,210,255,256 | Quasi-static Flx/Ext/LB/AR73,74,224; IDPs in C2-C3, C6-7257,258; Facet contact force107,259 |
Ligamentous cervical spine for axial tension166, AR169, and 8 g frontal/rear impact145; Full neck PMHS for 5–10 g rear impact260; full neck volunteer for 2–15 g frontal impact77,172,261,262, and 4–7 g lateral impact77,263 | Quasi-static Flx/Ext/LB/AR73 | Neck force-time for compressive impacts165,264,265; Quasi-static Flx/Ext115,132 |
| Application | Kinematics and tissue responses of noncontiguous ADR and noncontiguous ACDF in the treatment of noncontinuous cervical degenerative disc disease | Optimization of three-level cervical hybrid surgery to prevent ASD | Biofidelic kinematic and local tissue response of full head-neck in male HBM | Biomechanical performances between single-level triangular and quadrilateral profile anterior cervical plates | Implemented head-first compressive impacts toward the assessment of motorcycle neck protective equipment |
| First author/year | Ovsepyan, 2021266 | Sun, 2021267 | Wo, 2021268 | Xiao, 2021269 | Xie, 2021270 |
| Type | FE | FE | FE | FE | FE |
| Software | ABAQUS | ANSYS | ANSYS | ABAQUS | ABAQUS |
| Segments | Head–neck | C2–C7 | C2–C7 | Head–neck | Head–neck |
| Figure |

|

|

|

|

|
| Geometry | CT | CT | CT | CT | CT |
| Head | Elastic | N/A | N/A | Elastic | Elastic |
| Vertebra | Elastic | Elastic | Elastic | Elastic | Elastic |
| Disc | Hyperplastic (annulus fibrosis/nucleus pulposus) | Elastic | Elastic | Elastic | Elastic |
| Facet joint | Contact | Frictional contact | Frictional contact | N/A | N/A |
| Ligament | N/A | Linear spring | Linear spring | Linear spring | Nonlinear spring |
| Spinal canal | N/A | N/A | N/A | N/A | N/A |
| Muscle | N/A | N/A | N/A | 1D linear spring elements of passive muscles | N/A |
| Muscle activation | N/A | N/A | N/A | N/A | N/A |
| Muscle structure | N/A | N/A | N/A | N/A | N/A |
| Elements | Approximately 1 010 000 elements | N/A | 226 402 elements 446 263 nodes |
86 710 elements 296 644 nodes |
549 717 elements 184 802 nodes |
| Validation | C3–C5 for compression61,271 | Quasi-static Flx/Ext/LB/AR73,158,210 | Quasi-static Flx/Ext/LB/AR73,74,150,151,153,272–277 | Quasi-static Flx/Ext/LB/AR73,115 | Quasi-static Flx/Ext/LB/AR103,272,273,278–280 |
| Application | Functional and dynamic anatomy of nonlinearity of soft tissues as well as local anisotropy in the human head-neck | A lattice topology optimization of cervical interbody fusion and FE comparison with bio-absorbable cage and regular cage | Kinematics and tissue responses of cervical ADR using cervical subtotal discectomy prosthesis, and implanted it in non-human primates as an in-vivo experiment | Clinical effect and tissue responses of a traction exercise neck brace on cervical spondylopathy radiculopathy | Kinematics of the craniovertebral junction after odontoidectomy with anterior C1 arch preservation |
| First author/year | Nishida, 202152 | Sun, 202253 | Liang et al.38 | Li, 2023281 | |
| Type | FE | FE | FE | FE | |
| Software | ABAQUS | ABAQUS | LS-DYNA | LS-DYNA | |
| Segments | C2–C7 | C2–T1 | Head–neck | Head–neck | |
| Figure |

|

|

|

|
|
| Geometry | CT | CT | CT/MRI | CT | |
| Head | N/A | N/A | Rigid | Elastoplastic | |
| Vertebra | Elastic | Elastic/Neo-Hookean | Elastoplastic | Elastoplastic | |
| Disc | Hypoelastic (annulus matrix/annulus fibrosis/nucleus pulposus) | Hypoelastic (annulus matrix/annulus fibrosis/nucleus pulposus) | Hyperelastic (annulus matrix) Elastic fluid (nucleus pulposus) Orthotropic nonlinear elastic (annulus fibrosis) |
Elastic (annulus matrix) Plasticity (annulus fibrosis) Viscoelastic (nucleus pulposus) |
|
| Facet joint | Sliding contact | Soft contact | Contact | Bound contact | |
| Ligament | Nonlinear spring | Nonlinear spring | Nonlinear membrane | Nonlinear spring | |
| Spinal canal | N/A | N/A | Elastic (dura mater/pia matter/denticulate ligaments) Viscoelastic combined with hyperelastic (white matter/grey matter) |
N/A | |
| Muscle | N/A | N/A | 1D beam elements of Hill muscles (active muscle) | 1D spring elements of Hill muscles | |
| Muscle activation | N/A | N/A | Coupled with neuromuscular feedback58 | Predefined | |
| Muscle structure | N/A | N/A | Cadaver measurement199 | Cadaver measurement | |
| Elements | 213 165 elements 173 215 nodes |
N/A | 1 073 668 elements 246 523 nodes |
296 487 elements | |
| Validation | Quasi-static Flx/Ext/LB/AR224; Facet joint forces and IDPs in C2-C6224,237,241,243 |
Cervical lordosis measurement282; maximum heights of intervertebral discs measurement283; Ligament lengths measurement284; Quasi-static Flx/Ext/LB/AR73,115,129,130,210; Facet joint forces in C2-C750,241,242; IDPs in C2-C6210,243,285 |
Anatomy measurements (cervical lordosis, vertebral height, vertebral depth, vertebral width, and spinous process length)200; Compressive impact of spinal cord286,287; Ligaments tension of UCS and LCS202,204,288; FSU compression test271; Quasi-static Flx/Ext/LB/AR73,115,132,149; Kinematic and dynamic response of 4 g rear impact for whole head-neck (PHMS)289; Kinematic and dynamic response of 4 g rear impact for whole head-neck (volunteer experiment)221; Epidemiologic data reviewed |
Head and neck axial impact experiment290; kinematic and dynamic response of 10 g and 15 g front impact for whole head-neck72 | |
| Application | In Nishida, 2021, 202252,291: influences of soft tissue injury in normal cervical spine and laminoplasty scenarios | Continuous biomechanical effects of follower load on the ROM, tissue responses of cervical spine | Protective effect of muscle activation caused by natural neural reflex on neck in impact loading by decreasing tissue responses and injury position to reduce trauma; quantitatively biomechanical response analysis of posterior musculature reconstruction in cervical single-door laminoplasty292 | Effect of muscle activation on dynamic responses of neck of pilot during emergency ejection |
ACDF, anterior cervical discectomy and fusion; ADR, artificial disc replacement; ASD, adjacent segment degeneration; CT, computed tomography; FE, finite element; FSU, functional spinal unit; GHBMC, Global Human Body Models Consortium; HBM, human body model; IDP, intradiscal pressure; MIS, minimally invasive surgery; KTH, Kungliga Tekniska Högskolan; N/A, not application; OPLL, ossification of posterior longitudinal ligament; RMSE, root mean square error; rRMSE, relative root mean square error; SCI, spinal cord injury; THUMS, Total Human Model for Safety.
Table 2.
Multipage tables of human head–neck multibody models within retrieved studies in the last two decades.
| First author/year | Chancey, 2003293 | Van Der Horst, 200446 | Galbusera, 2006294 | Ahn, 2007295 | van Lopik, 2007296 |
|---|---|---|---|---|---|
| Type | MB | MB | MB | MB | MB |
| Software | LS-DYNA | MADYMO | VisualNastran | VisualNastran | VisualNastran |
| Segments | Head–T1 | Head–T1 | C2–C7 | C2–T1 | Head–T1 |
| Figure |

|

|

|

|

|
| Geometry | CT/MRI | Visible human subject | CT | CT | CAD modelling |
| Head | Viscoelastic rigid face | Rigid | N/A | N/A | Rigid |
| Vertebra | Rigid | Rigid | Rigid | Rigid | Rigid |
| Disc | Couple superior vertebra to next inferior vertebra | 6-DOF springs and dampers | N/A | Linear visoelastic | Viscoelastic bushing elements (Flx/Ext); linear (LB/AR) |
| Facet joint | N/A | Contact | Contact | Contact | Frictionless contact |
| Ligament | Nonlinear spring | Nonlinear spring | Linear spring | Nonlinear spring | Viscoelastic spring |
| Muscle | Nonlinear passive and active elastic components (optimization minimizing muscle fatigue) | Active muscle: Hill types | N/A | N/A | Active muscle: Hill types |
| Elements | N/A | N/A | N/A | N/A | N/A |
| Validation | In Oi, 2004297: Muscle moment arms comparison154,298–300 | ROM of intervertebral units74,165,301; dynamic response to frontal/lateral Impact172,302 | ROM of intervertebral units303–305 | ROM of intervertebral units73
Axis-disc angle306 |
ROM of intervertebral units; Coupling characteristics; Ligaments’ response74,81,165,274 |
| Application | Improved estimation of human neck tensile tolerance according to anthropometrically correct muscles and optimized physiologic initial conditions | Human had neck response in frontal, lateral and rear end impact loading | Constructed the flexion-extension motion of cervical spine after ADR surgery | Visualized realistically the kinematics and kinetics of the cadaver cervical spine | Evaluated realistic effect of curved musculature representation of the change in muscle length during the head-neck main and coupled motions |
| First author/year | de Jongh, 200848 | Huber, 2013307 | Khurelbaatar, 2015308 | Happee, 201722 | Cazzola, 2017309 |
| Type | MB | MB | MB | MB | MB |
| Software | LifeMOD | Adams | RECURDYNTM | MATLAB | Opensim |
| Segments | Whole body model | C1–C7 | Head–thoraco–Pelvis | Head–T1 | Whole body model |
| Figure |

|

|

|

|

|
| Geometry | Standard GeBod anthropometric database | White light scanner | CT | MRI and CT | 3D digitizer |
| Head | Rigid | Rigid | Rigid | Rigid | Rigid |
| Vertebra | Rigid | Rigid | Rigid | Rigid | Rigid |
| Disc | 6-DOF bushing elements | Bushing force | 6-DOF bushing elements | 6-DOF bushing elements | 6-DOF elements |
| Facet joint | Contact | Contact | Plane-sphere contact | Contact | Contact |
| Ligament | Nonlinear spring | Force vector | Tensile-only spring | N/A | N/A |
| Muscle | Active muscle: Hill types | EMG | Active muscle: Hill types | Active muscle: Hill types | Active muscle: Hill types |
| Elements | N/A | N/A | N/A | N/A | N/A |
| Validation | Intradiscal pressure310; ROM of intervertebral units311 |
In house: internal load (EMG/optical data) compare to the external load (force plate) | ROM of intervertebral units73,115,129; ligament tensile forces311; Force of facet joint18,312 | Head–neck dynamic responses during bandwidth of pseudorandom313 | Scapula-clavicular joint and moment arms314,315; ROM of intervertebral units272,273,305,316–318; neck muscles activation during functional movements (EMG) |
| Application | Estimated time-varying contact stress and slip velocity distributions at the interface of the cervical disc implant and provided insight into the in vivo biomechanical performance of the implant’s wear rate | Predicted motion, moments on the cervical spine, and calculate loads on the discs as well as co-activation in the muscles that maintain balance of the head-neck | Predicted joint forces and moments applied to vertebral and facet joints and the forces that act on ligaments and muscles in cervical spine | Modulation of head-in-space and head-on-trunk stabilization strategy with the frequency content of trunk perturbations and the presence of visual feedback by vestibulocollic reflex, cervicocollic reflex, and neck muscle co-contraction | Investigated kinematics, joint moments and neuromuscular activations during rugby scrummaging and neck functional movements to explore cervical spine injury mechanisms |
| First author/year | Diao, 2017319 | Mortensen, 2018320 | Kuo, 201947 | Zheng, 202158 | Arshad, 2022321 |
| Type | MB | MB | MB | MB | MB |
| Software | AnyBody | Opensim | Opensim | Opensim | AnyBody |
| Segments | Head–neck model | Head–T1 | Head–T1 | Head–T1 | Head–neck model |
| Figure |

|

|

|

|

|
| Geometry | AnyBody modelling system repository | Hyoid muscles improved base on previous MB model | MRI and CT | Neuromuscular reflex improved base on previous MB model | Visible human project |
| Head | Rigid | Rigid | Rigid | Rigid | Rigid |
| Vertebra | Rigid | Rigid | Rigid | Rigid | Rigid |
| Disc | 6-DOF elements | 6-DOF bushing elements | 6-DOF bushing elements | 6-DOF bushing elements | Spherical joints |
| Facet joint | Plane-sphere contact | Contact | Contact | Contact | N/A |
| Ligament | Linear spring | Rotational stiffness and damping | Nonlinear spring | Rotational stiffness and damping | Nonlinear spring |
| Muscle | Active muscle: Hill types | Active muscle: Hill types | Active muscle: Hill types | Active muscle: Hill types | Active muscle: Hill types |
| Elements | N/A | N/A | N/A | N/A | N/A |
| Validation | / for sensitivity analysis; maximum compressive forces of disc322; facet joint force18,210; ligaments’ force308; ICR A–P translation323 | Previously published validation by both Vasavada and Cazzola309,324 | Response of cervical spine ligaments during head impacts | Posture control experiment (EMG); Cervical joint angles in stable status [X-ray results]; 2/3/8/15 g frontal impact325 |
Correction factor of IDP326–328; axial and shear loads329; qualitatively compared 34 group muscles330–332 |
| Application | Simulated the function of musculature and consider joint internal motion in the head–neck | Capability of hyoid muscles to stabilize the upper cervical spine and provide increased moment generation in head–neck | Stiffen effect of passive ligaments on providing greater deceleration angular impulses than active muscles at high lengthening rates in American football head impacts | Influences of realistic neural reflex control loops of the vestibular system and the muscle-tendon proprioceptors on in-vivo head-neck behaviors and related injury risk during impact loading | Quantifying the differences in disc loads, motion, and muscle force/activities through changing the vary in segmental mass, disc stiffness, and muscle strength |
3D, three dimensional; ADR, artificial disc replacement; A–P, anterior–posterior; CT, computed tomography; ICR, Instantaneous centers of rotation; MB, multibody; R 2, correlation coefficients.
The first step in head and neck simulation tasks is to generate models for specific subjects, with two primary methods for creating personalized models. The first method involves scaling a generic model, while the second involves creating models based on the segmentation of medical images25,26. The primary task in medical image-based processing is to collect medical images (such as MRI and CT scans), while bi-planar X-rays and three-dimensional ultrasound measurements can be utilized to identify specific anatomical landmarks for personalized models. Statistical shape modeling and morphing techniques aid in rapidly and accurately reconstructing bones27. Creating models from medical images is very time-consuming and requires extensive expertise. Therefore, the importance of rapid, personalized modeling methods has been increasingly emphasized in recent years28,29.
Conventional personalized scaling involves resizing the generic skeletal geometry according to individual dimensions. However, the greater the discrepancy between an individual’s anthropometry and the generic model, the less likely the scaled model will accurately represent the anatomy30. Modeling based on weight and segment lengths allows for scaling generic models to specific individuals. The conventional scaling method is linear scaling31,32, which is the standard method for model examples included in the AnyBody modeling system’s user model repository. Proportional scaling is based on an individual’s height and body proportion, selecting the closest model for scaling to the individual33. Linear scaling of generic models, despite being time and cost-effective, probably results in significant errors due to not accounting for anatomical differences between individuals29. Marker-based scaling methods rely on the distance between virtual markers placed on the model and experimental marker positions provided by a photonic system32,34. This method uses a reference record to create a stick-figure model, with joint parameters directly calculated from optical markers placed on anatomical landmarks. The collected kinematic representation is then registered with a cadaver-based musculoskeletal dataset. During registration, a nonlinear transformation is created to scale (morph) the cadaver-based dataset to match the subject-specific joint parameters. Morphing utilizes radial basis functions (RBF) to interpolate data between markers. Thus, with an appropriate marker protocol, this method directly provides scaling of the musculoskeletal model. The RBF-based scaling method allows for scaling the entire model using a small number of anatomical landmarks, thereby reducing subjectivity and manual intervention in the scaling process35.
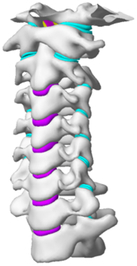
Computational biomechanics seeks to apply the principles of mechanics to living tissues. The results showed that linear materials were mainly used in FE models before 2005. Thereafter, the Kungliga Tekniska Högskolan (KTH) model36, the Total Human Model for Safety (THUMS) model15, and the Global Human Body Models Consortium (GHBMC) model37 were sequentially developed and taken into account the pronounced nonlinearity and anisotropy of human tissues. Compared to collision models in the same period, medical models materials were much simpler. Nonlinearity was mostly concentrated in intervertebral discs and spinal ligaments, which were defined as viscoelastic or hyperelastic characteristics. Although the current constitutive equation can well simulate the mechanical behavior of most spinal tissue, the contents within the spinal canal still need to be improved in terms of modelling and materials. Recently, a hyperelastic Ogden material with linear viscoelasticity (prony series) based on recent experimental studies of in-vivo nonhuman primates was used in Liang et al. 38. However, the mechanical behavior of the synchronized interaction between fluid (blood vessel, cerebospinal fluid) and structure (spinal cord) is currently neglected in head–neck computational models. More experimental studies on spinal cords are needed in the future for more accurate FE modelling.
Validation always plays an important role in the field of computational biomechanics; this field has utilized validation in an attempt to build credibility for models of complex biological systems. As shown in Table 1, the developed FE or MB models used different types of validation methods, which subsequently increased and extended their applicability according to different research needs. Comparisons of segmental ROM between model predictions and experimental measurements were mostly performed under quasi-static or dynamic working conditions, and examples include Ng et al. 39, Zhang et al. 40, del Palomar et al. 41, Tchako and Sadegh42, etc. In addition, FE or MB models for collision applications validated velocity and acceleration parameters to verify complex dynamics responses36,43–47. Recently, studies validated the use of internal parameters to compare the results of in-vitro measurements, such as intradiscal pressure and facet joint force48–53. Anatomical measurement for validation has also been performed in recent years because of the inevitable modifications in the process of geometric reconstruction38. Moreover, recent numerical models have recognized that the involvement of active muscles under neuromuscular feedback plays an important role in the understanding of fundamental principles of human head–neck motion. Efforts have been made to include more complicated control strategies, from predefined active curves54,55 or simple PID control56,57 to complex physiological neural feedback control strategies38,58, in these models. These models in studies were mostly developed to investigate the precise mechanism of cervical spine injuries during sports and traffic collisions.
In addition, the application of computational HBMs revolved around four specific subjects in previous studies: physiopathology, treatment evaluation, collision condition, and sports injury. Based on previously established and validated head–neck computational models, most of the studies investigated cases in depth. Examples included collision, sports injury, a specific pathological model, and instrument assessment. Head–neck computational models in the first decade mostly focused on collision studies, while models applied to large numbers of medical environments in the second decade. The advent of computational models in clinical use stemmed from the integration of biomechanical research and medical needs: clinical researchers gradually realized that biomechanical simulation analysis could play an increasingly important role in cervical spine diseases and treatments59,60. HBMs assisted in understanding the biomechanical mechanisms underlying disease progression, aiding in early disease diagnosis and the formulation of treatment plans19,61–63. They also could be utilized to plan surgical procedures, simulate surgical operations, and evaluate their outcomes and risks64–66. Hence, it is thus not a surprise that biomechanical research on medical applications has increased at a rapid pace.
Discussion
In the last two decades, there has been a yearly rise in the volume of new research in the field of biomechanics relating to the human head–neck. This review places the findings regarding biomechanical modelling, validation, and application of the head–neck part into the context. While conducting a new study is always important, researchers must familiarize themselves with and establish the efforts of their predecessors. To date, the most common head–neck HBMs are adopting FE and MB modelling methods. The former puts particular emphasis on the loading condition, stress responses, and strain responses of local human tissues, while the latter comprises rigid skeletons and one-dimensional muscle components that generally aim to analyze the whole dynamic responses of the head–neck. Due to theoretical differences, although the MB models cannot be used to monitor tissue stress/strain responses in general, they are more computationally efficient in the analysis of dynamic responses than FE models. Although different controllers have been implemented in recent FE head–neck models22,56–58,198,333,334, the larger computational demands inherent in FE models can still restrict their development in modelling methods and their biofidelity, such as their ability to incorporate complicated neural control strategies56,57,198. However, these features have been continuously improved in MB models. These respective features probably lead to various environments concerning simulation requirements22,58.
During the last two decades, the combination of basic and clinical orthopedic knowledge with biological modelling technology has shown a multidisciplinary trend in modern orthopedic research335. Many clinical problems of the cervical spine, such as mechanical neck pain through musculoskeletal disorders, indeed need a biomechanical model that can reveal the essential connection between internal human tissue and external intervention. Hence, the application of physiopathology and treatment evaluation gradually exceeded the observed impact scenarios during the last decade and became the most attractive feature of head–neck biomechanical modelling. In addition, the development of computer science and the use of new imaging technology increased the efficiency of simulation and modelling336,337. As shown in Figure 3 and Figure 4, the studies included in this review approximately revolved around four specific subjects: physiopathology, treatment evaluation, collision condition, and sports injury. Medical scenarios should still be a focus of future research efforts, given the application fields of computational head–neck models.
Figure 3.

Heat map of application in head-neck computational models within four specific subjects.
Figure 4.
(A) Pathological cervical spine FE model for the spinal cord compression of ossification of the posterior longitudinal ligament190; (B) Modified muscle-preserving techniques of single-door laminoplasty in cervical spine surgery through head-neck FE model simulation292; (C) 50th percentile male of GHBMC head-neck FE models under rear impact kinematic sequence that simulated whiplash injury354; (D) Anatomical loads and mechanisms of cervical spine injuries associated with rugby in head-neck multibody model. FE, finite element; GHBMC, Global Human Body Models Consortium.
Physiopathology
At present, inherent differences in human anatomical structures and material properties among individuals and alterations in these parameters due to age, sex, and degeneration can limit the widespread applicability of the reported models. For example, most FE models are generally based on one specific or one idealized subject (exactly symmetrical) with unique mechanical and geometrical characteristics, and some studies have explored the influence of geometric factors in subjects on biomechanical responses, including kinematic change, tissue stress and strain in the head–neck region50,55,163,175,180,196. If a model aims to predict the behavior of an average subject, it should incorporate average anatomical properties and be fully validated for biomechanical responses to increasing predictive ability338,339. Although most biomechanical researchers are aware of the importance of validation, many detailed FE models of medical applications only validated quasi-static segmental ROM. Merely a small fraction of models additionally validate intradiscal pressure and force of facet joint49–53. These parameters provide insights into the internal loading conditions of the cervical spine. In addition, for a variety of conditions from quasi-static loading to dynamic loading, many detailed models lack multilayer model validation from anatomic verification to isolated tissues to subsegments and the whole head–neck model. Inadequate model verification and validation can substantially reduce the robustness of model simulation results in various loading environments. There are certain concerns associated with these environments, including challenging validation processes and the application of the model beyond its validation boundaries338. This implies differences in the definition of loading cases to investigate injuries; on the other hand, it provides differences in terms of their level of accuracy for injury prediction.
Pathological models were established to evaluate underlying variables based on validated mathematical models. The FE model of spinal cord injury (central cord syndrome), which is induced by degenerative cervical myelopathy or ossification of the posterior longitudinal ligament (OPLL), is mostly modelled in the cervical segment, as shown in Figure 4. Imaging scans ignore the dynamic pressure-induced changes in degenerative structures in the spinal canal, especially for cervical spines with high mobility340. Finding a potentially compressive source (disc bulging, ligamentum flavum hypertrophy, etc.) is often an important basis for the early diagnosis of central cord syndrome. FE predictions undoubtedly have higher sensitivity in terms of the respective mechanical behavior of the detailed pathological or clinical type19,188,189,249, which can fully display dynamic changes in the spinal canal under head–neck motion conditions. Thus, the use of biomechanical simulation models can undoubtedly be an essential tool to assess the best clinical option341.
The biomechanical characteristics of the FSU are fundamental for understanding the cervical spine and its various pathologies. Studies on basic mechanisms that support load and enable head–neck movement help to explain clinical problems of musculoskeletal disorders, such as those related to the relationship between internal loads and external muscle forces42,293,308,320, FSUs under a superimposed compression force (follower load)53, cervical disc stiffness123,226,321, facet joint orientation175,196, etc.
Treatment evaluation
Based on the established pathological models, corresponding treatments were analyzed and evaluated biomechanically. Intervertebral fusion and artificial disc replacement are most widely studied in cervical surgery. Discectomies and facetectomy produce iatrogenic injuries that include altered structural responses and redistributed load in the FSUs39,123. To avoid segmental instability, clinicians implanted an interbody cage or artificial disc replacement into the lesion segment. Substantial research over the past 20 years has simulated the responses that occur after prosthesis or osteosynthesis implantation using both FE and MB models. Additional advantages of the FE models are that they allow predictions of the key parameters of mechanical stability, including the cervical Cobb angle, the pull-out force of cages, and stress responses around the zones of implanted screw-plate, cage, or prosthesis. Moreover, by setting different contact relationships between the cage–endplate interface or growth factors of bone creeping substitution, FE models can even predict different periods of intervertebral osseointegration124. Although existing biomechanical models cannot accurately simulate postoperative cage subsidence or prosthesis migration, the models can observe the stress and its distribution on the cage–endplate interface and cancellous bone under the bony endplate as the risk of subsidence and migration. These mechanical responses not only prevent future pathologies derived from an unsuitable positioning of the prostheses or its fixation but also serve as a basis for the design and optimization of dimensions, cavity volume, position, material, fixation methods, and structural characteristics of instrumented implants65,267.
Apart from anterior cervical spinal fixators, posterior fixators have also been widely studied, especially in the first decade of analysis in this review. Laminectomy and laminoplasty are representative surgeries for OPLL. These biomechanical studies are almost all from East Asia because OPLL is fairly common in Asian individuals and is defined as a rare disease in Western countries342,343. Sutures, titanium cables, suture anchors, allograft or autograft bone, synthetic spacers, and miniplates were used in laminoplasty, and current studies primarily compared the biomechanical benefits and complications of instrumented implants19,63,93,133,135,189–191, as shown in Figure 4B. Different from cervical fusion, laminectomy, and laminoplasty preserve the motor function of the intervertebral disc. However, muscle-derived axial neck pain, the most common complication, decreases postoperative ROM and has a negative effect on treatment outcomes344. Moreover, the active muscle force should be considered when evaluating muscle-derived axial pain, but there is a lack of biomechanical studies on the active muscle behavior of laminectomy or laminoplasty, which is surprising considering that these two surgeries are being performed clinically.
Muscle structure and function should be purposefully added to medical models, which would undoubtedly increase the accuracy of clinical treatment predication and evaluation. Howley et al. 182 modelled and integrated three-dimensional deformable muscles with contraction capabilities in an effort to pave the way for various orthopedic simulations. It is believed that biomechanical research for orthopedic and other medical environments will continue to increase. Minimally invasive cervical surgery is the future direction in clinical practice, and now its biomechanical evaluation is gradually being reported66,161. Furthermore, rehabilitation, anesthesia, and alternative medicine started to adopt biomechanical modelling in recent years to solve clinical issues, such as postoperative complications189, conservative strategies194,195,269, endotracheal intubation197, etc.
Collision condition
Compared with the detailed FE models for medical applications, models for collision conditions were developed for a longer period and seem to be more comprehensive and realistic. Several whole HBM have also been developed15,37,43,45,199 (Fig. 4C). In the past decade, an increasing number of FE HBMs for impact injury analysis have consisted of active muscle modelling to reflect the effects of muscle activities on human body injuries, such as in emergency braking and wheel operation101,345–348. First, predefined activation-time curves were defined for muscle activation modelling54,84,137. However, this simplified method cannot represent the complexity of the neural reflex control loop. Recently, artificial controllers of muscle activation were also gradually added to FE models to include neural reflex control loops responding to external stimulation. Of note, Putra and colleagues implemented a PID-based control strategy in the ViVA female OpenHBM that was first established by Östh and colleagues, which included an angle-based and length-based active muscle controller14,57,198. A similar method was also implemented in the head–neck part of the GHBMC model56 and the THUMS model349. However, these simplified sensory feedback control modelling methods were found to be limited in their reactions to environmental perturbation350; moreover, the computational cost is high, especially when the modelling complexity of the neural control method is increased to be humanlike351. Few studies adopted physiologically realistic mathematical models of the neural reflex of the peripheral sensory system and vestibular feedback, implemented them into MB models, and applied them in impact and perturbation analyses; these analyses revealed influences of these proprioceptors on head–neck dynamic responses22,58. However, stress and strain distribution and values in human tissue for detailed injury risk analysis cannot be easily and accurately obtained using the MB models due to their theoretical limitations.
Recently, Liang et al. 38 introduced the combination of the FE and MB head–neck models, who analyzed the Von mises stress or strain responses of local tissues in a whiplash-loading environment by coupling a neuromuscular head–neck MB model and a corresponding FE head–neck model. The results show that muscle activation caused by the neural reflex protects the neck during impact loading by decreasing the strain level and transferring the possible injury to the lower spinal cord level to reduce injury severity. Thus, the FE-MB coupled method with natural neural control modelling is an interesting research field that can provide unique findings from human body biomechanical analysis. This approach combines the advantages of FE and MB methods and enables head-neck models to facilitate stress and strain prediction in local tissue under realistic human body motion, which should be further developed for more accurate biomechanical prediction.
In addition to advanced control strategies, tissue materials of pronounced nonlinearity and local anisotropy are more often applied in collision applications than in the medical environment due to the large deformation in collision requirements. However, more complicated constitutive equations or material modelling methods can increase the computational cost and instability of FE HBMs in the solving process. Therefore, the applicability and simplicity of the HBMs need to be balanced. The FE HBMs for medical applications focus more on anatomical details, while the models for impact injury analysis probably simplify or idealize some anatomical structures. The former often focuses more on subtle tissue deformation in local medical intervention, and the latter is usually used in loading environments with large tissue deformation. Importantly, biological systems are inherently complex and comprised of multiple interdependent variables with subtle relationships to each other, which makes it prohibitively difficult to take all potential variables into account in the computational model352. Sometimes, errors are even caused by the ‘garbage in garbage out’ phenomenon that is inherent to any computational model353. Through the lens of physics and mechanics, biological concepts may conflict with the clinician’s inherent understanding.
In summary, multiple causes make standardize collision FE HBMs. First of all, the design goal of the crash FE HBMs is to comprehensively evaluate the human body injury in the collision process, so the simulation results of the main body injury parts need to be verified in detail. Therefore, models for collision conditions have a broader application than specific medical FE models. Secondly, there is no unified protocol for the establishment of medical detailed FE HBMs, while a complete set of verification protocols has been established for collision models after years of development since it is due to the early start of vehicle collision simulation model, forming a systematic, engineering unified simulation analysis standard. Models for collision conditions have been proposed for widely involved in future virtual evaluation of automobile safety under the relevant regulations. Due to the lack of complete establishment and verification specifications, the application of FE models for medical use is often limited to specific cases and specific conditions.
Sports injury
MB models are ideal for estimating system dynamics during sports impact events, providing a viable approach to test fundamental principles and investigate their injury mechanisms. It also allows simulations to be run at low computational cost. However, the head–neck MB model is still in its infancy for sports injury applications. Recently, some relevant research attention has been placed on American football355–357, as shown in Figure 4D. It is a full-contact sport that, on occasion, can result in serious cervical spine injuries. Similar to whiplash injury, the primary injury mechanisms of the cervical spine in sports injuries are buckling or hyperextension358. A generic full-body MB model (Musculoskeletal model for the Analysis of Spinal Injuries) was developed to investigate cervical spine loading through both inverse and forward simulations309. Then, the model was improved by recent studies investigating collisions in sports and motor vehicles47,58,320. Likewise, the development of head–neck FE models and MB models has facilitated the impact of kinetics and injury metrics of head-neck resulting from various sports, including ice hockey359–361 and boxing362 in recent years. Levy et al. 359 conducted laboratory experiments to determine head kinematics and injury metrics in hockey using FE models. The researchers investigated the head acceleration and rotational velocity of a helmeted head form subjected to various impact scenarios. Similarly, Michio Clark et al. 360 utilized FE models to investigate the distribution of brain strain in the cerebrum for laboratory impacts on ice hockey goaltender masks. The study highlights the need for improved helmet designs that consider not only linear acceleration but also rotational acceleration and brain tissue deformation. In boxing, Razaghi and Biglari362 conducted a comparative numerical model to simulate the ocular injury, which demonstrated the importance of using FE models to predict and analyze ocular injuries in boxing. Li et al. 363 also used a FE head model to simulate the boxing-type impact injury and found the lateral impact was more injurious to the brain than an anterior-posterior impact. Cournoyer and Hoshizaki364 analyzed the head dynamic response and brain tissue deformation for boxing punches with and without loss of consciousness using MB models. Their findings suggest that a loss of consciousness may be caused by a high level of head acceleration, which may lead to brain tissue deformation and neuromuscular responses.
Hence, over the past 10–15 years, there has been a large increase in the occurrence of sports-related spine injuries that result in severe trauma in the spinal cord, interverbal disc, articular capsule, etc.365–368. The design and optimization of subject-specific protective devices are expected to improve, especially in biomechanical models, which monitor head–neck kinematics and consequently reduce the risk of injury to the cervical spine in sports. For example, de Grau et al. 361 further explored the protective capacity of ice hockey helmets, who used FE models to investigate helmet performance at different levels of striking compliance. Their research found that helmets that offer higher levels of impact protection can better reduce head injury risk in ice hockey.
Conclusion
This review systematically summarized existing head and neck models and discussed the novel findings regarding their modelling approach, structural characteristics, validation, and application. These methodologies of biomechanical models primarily focus on application-centred differences. Firstly, medical simulations have become the most researched content in head-neck biomechanical modelling over the last decade, while models for medical scenarios start later and develop slowly, which is probably due to limitations in the medical background. Tissue materials of pronounced nonlinearity have been less utilized in medical FE models when compared with models for collision, which is typically used in loading environments with large tissue deformation. Secondly, several models lack multiple-layer validation, such as anatomical verification, isolated tissues to subsegments, and the whole head–neck model, in a variety of conditions ranging from quasi-static loading to dynamic loading. More comprehensive validations that combine characteristics of interdisciplinarity will strengthen the utility of models and lead to multidirectional scenarios. Thirdly, advanced neuromuscular reflex control is being included in biomechanical head–neck models for collision applications, while this important control strategy has yet to be added to the medical models. It is suggested that the effect of active muscle control would enhance the understanding of treatment evaluation for medical head–neck models, and validate the models using real-world data. Finally, standardization in integrated medicine and engineering can greatly enhance the development and application of modeling processes in this field. By establishing standardized practices, guidelines, and frameworks, the integration of medicine and engineering can become more efficient, reliable, and effective.
Ethical approval
Not applicable.
Consent
Not applicable.
Source of funding
This work was supported by the National Natural Science Foundation of China (Grant No. 52275286), Hunan Outstanding Youth Fund (Grant No. 2023JJ10010), Key Research and Development Program of Hunan Province (Grant No. 2022SK2105), Open Project of Xiangjiang Laboratory (Grant No. 23XJ03015), Shenzhen Science and Technology Program (Grant No. JCYJ20230807122004009), and the Sanming Project of Medicine in Shenzhen (Grant No. SZZYSM202311006).
Author contribution
Z.L.: methodology, writing-original draft, and visualization; K.W.: reviewing and modification; T.T.: investigation and resources; F.M.: conceptualization, supervision, project administration, and funding acquisition.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
Fuhao Mo.
Data availability statement
All data generated or analyzed during this study are included in this article.
Provenance and peer review
No invited.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Ziyang Liang, Email: young8637@sina.com.
Ke Wu, Email: wuke01@hnu.edu.cn.
Tengfei Tian, Email: 202131205029@stu.hebut.edu.com.
Fuhao Mo, Email: fuhaomo@hnu.edu.cn.
References
- 1.Kleinberger M. Application of finite element techniques to the study of cervical spine mechanics. SAE Tech Pap 1993;48:0148–7191. [Google Scholar]
- 2.Dauvilliers F, Bendjellal F, Weiss M, et al. Development of a finite element model of the neck. SAE Tech Pap 1994;103:0148–7191. [Google Scholar]
- 3.Yang KH, Zhu F, Luan F, et al. Development of a finite element model of the human neck. SAE Tech Pap 1998;42:0148–7191. [Google Scholar]
- 4.Li X, Liu Y, Deng Y-C. Modeling of the human cervical spine using finite element techniques. SAE Tech Pap 1999. Report No.: 0148–7191. [Google Scholar]
- 5.Halldin PH, Brolin K, Kleiven S, et al. Investigation of conditions that affect neck compression-flexion injuries using numerical techniques. Stapp Car Crash J 2000;44:127–138. [DOI] [PubMed] [Google Scholar]
- 6.Liu J, Liu H, Bu W, et al. Effects of different helmet-mounted devices on pilot’s neck injury under simulated ejection. Comput Methods Biomech Biomed Eng 2023;26:1510–1521. [DOI] [PubMed] [Google Scholar]
- 7.Gaur SJ, Josfai W, Aravindaksliam B, Aravlnd AS. Determination of helmet CG and evaluation of neck injury potentials using “Knox Box criteria” and neck torque limits. IJASM 2013;57:37–44. [Google Scholar]
- 8.Zhang H, Agrawal SK. Kinematic design of a dynamic brace for measurement of head/neck motion. IEEE Robot Autom Let 2017;2:1428–1435. [Google Scholar]
- 9.Zhang H, Agrawal SK. An active neck brace controlled by a joystick to assist head motion. IEEE Robot Autom Let 2018;3:37–43. [Google Scholar]
- 10.Yoshiko A, Beppu M, Izumida R, et al. Long-term assessment of morphological, functional, and quantitative parameters of skeletal muscle in older patients after unilateral total hip arthroplasty. Exp Gerontol 2020;137:110971. [DOI] [PubMed] [Google Scholar]
- 11.Chang BC, Zhang H, Long S, et al. A novel neck brace to characterize neck mobility impairments following neck dissection in head and neck cancer patients – ADDENDUM. Wearable Technol 2024;5:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liang Z, Cui J, Zhang J, et al. Biomechanical evaluation of strategies for adjacent segment disease after lateral lumbar interbody fusion: is the extension of pedicle screws necessary? BMC Musculoskelet Disord 2020;21:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu GM, Liang ZY, Li W, et al. Finite element analysis of insertion angle of absorbable screws for the fixation of radial head fractures. Orthop Surg 2020;12:1710–1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Osth J, Brolin K, Svensson MY, et al. A female ligamentous cervical spine finite element model validated for physiological loads. J Biomech Eng 2016;138:061005. [DOI] [PubMed] [Google Scholar]
- 15.Kitagawa Y, Yasuki T, Hasegawa J. Research study on neck injury lessening with active head restraint using human body FE model. Traffic Inj Prev 2008;9:574–582. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz D, Guleyupoglu B, Koya B, et al. Development of a computationally efficient full human body finite element model. Traffic Inj Prev 2015;16(suppl 1):S49–S56. [DOI] [PubMed] [Google Scholar]
- 17.Davis ML, Koya B, Schap JM, et al. Development and full body validation of a 5th percentile female finite element model. Stapp Car Crash J 2016;60:509–544. [DOI] [PubMed] [Google Scholar]
- 18.Lee SH, Im YJ, Kim KT, et al. Comparison of cervical spine biomechanics after fixed- and mobile-core artificial disc replacement: a finite element analysis. Spine (Phila Pa 1976) 2011;36:700–708. [DOI] [PubMed] [Google Scholar]
- 19.Khuyagbaatar B, Kim K, Park WM, et al. Influence of sagittal and axial types of ossification of posterior longitudinal ligament on mechanical stress in cervical spinal cord: a finite element analysis. Clin Biomech (Bristol, Avon) 2015;30:1133–1139. [DOI] [PubMed] [Google Scholar]
- 20.Liu H, Inoue S, Wada T. Motion sickness modeling with visual vertical estimation and its application to autonomous personal mobility vehicles. Paper presented at 2022 IEEE Intelligent Vehicles Symposium (IV). 2022;. 4–9 June 2022.
- 21.Roggio F, Ravalli S, Maugeri G, et al. Technological advancements in the analysis of human motion and posture management through digital devices. World J Orthop 2021;12:467–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Happee R, de Bruijn E, Forbes PA, et al. Dynamic head-neck stabilization and modulation with perturbation bandwidth investigated using a multisegment neuromuscular model. J Biomech 2017;58:203–211. [DOI] [PubMed] [Google Scholar]
- 23.Oxland TR. Fundamental biomechanics of the spine--What we have learned in the past 25 years and future directions. J Biomech 2016;49:817–832. [DOI] [PubMed] [Google Scholar]
- 24.Li F, Liu N-s, Li H-g, et al. A review of neck injury and protection in vehicle accidents. Transp Saf Environ 2019;1:89–105. [Google Scholar]
- 25.Kainz H, Modenese L, Lloyd D, et al. Joint kinematic calculation based on clinical direct kinematic versus inverse kinematic gait models. J Biomech 2016;49:1658–1669. [DOI] [PubMed] [Google Scholar]
- 26.Koller W, Baca A, Kainz H. Impact of scaling errors of the thigh and shank segments on musculoskeletal simulation results. Gait Posture 2021;87:65–74. [DOI] [PubMed] [Google Scholar]
- 27.Fernandez J, Mithraratne P, Thrupp S, et al. Anatomically based geometric modelling of the musculo-skeletal system and other organs. Biomech Model Mechanobiol 2004;2:139–155. [DOI] [PubMed] [Google Scholar]
- 28.Gerus P, Sartori M, Besier TF, et al. Subject-specific knee joint geometry improves predictions of medial tibiofemoral contact forces. J Biomech 2013;46:2778–2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ding Z, Tsang CK, Nolte D, et al. Improving musculoskeletal model scaling using an anatomical atlas: the importance of gender and anthropometric similarity to quantify joint reaction forces. IEEE Trans Biomed Eng 2019;66:3444–3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davico G, Pizzolato C, Killen BA, et al. Best methods and data to reconstruct paediatric lower limb bones for musculoskeletal modelling. Biomech Model Mechanobiol 2020;19:1225–1238. [DOI] [PubMed] [Google Scholar]
- 31.Delp SL, Anderson FC, Arnold AS, et al. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Trans Biomed Eng 2007;54:1940–1950. [DOI] [PubMed] [Google Scholar]
- 32.Moissenet F, Cheze L, Dumas R. Influence of the level of muscular redundancy on the validity of a musculoskeletal model. J Biomech Eng 2016;138:021019. [DOI] [PubMed] [Google Scholar]
- 33.Klemt C, Nolte D, Ding Z, et al. Anthropometric scaling of anatomical datasets for subject-specific musculoskeletal modelling of the shoulder. Ann Biomed Eng 2019;47:924–936. [DOI] [PubMed] [Google Scholar]
- 34.Lu T-W, O’connor J. Bone position estimation from skin marker co-ordinates using global optimisation with joint constraints. J Biomech 1999;32:129–134. [DOI] [PubMed] [Google Scholar]
- 35.Pellikaan P, van der Krogt MM, Carbone V, et al. Evaluation of a morphing based method to estimate muscle attachment sites of the lower extremity. J Biomech 2014;47:1144–1150. [DOI] [PubMed] [Google Scholar]
- 36.Brolin K, Halldin P, Leijonhufvud I. The effect of muscle activation on neck response. Traffic Inj Prev 2005;6:67–76. [DOI] [PubMed] [Google Scholar]
- 37.Gayzik FS, Moreno DP, Vavalle NA, et al. Development of the global human body models consortium mid-sized male full body model. Paper presented at IRCOBI Conference, 2011.
- 38.Liang Z, Mo F, Zheng Z, et al. Quantitative cervical spine injury responses in whiplash loading with a numerical method of natural neural reflex consideration. Comput Methods Programs Biomed 2022;219:106761. [DOI] [PubMed] [Google Scholar]
- 39.Ng HW, Teo EC, Zhang QH. Prediction of inter-segment stability and osteophyte formation on the multi-segment C2-C7 after unilateral and bilateral facetectomy. Proc Inst Mech Eng H 2004;218:183–191. [DOI] [PubMed] [Google Scholar]
- 40.Zhang QH, Teo EC, Ng HW, et al. Finite element analysis of moment-rotation relationships for human cervical spine. J Biomech 2006;39:189–193. [DOI] [PubMed] [Google Scholar]
- 41.del Palomar AP, Calvo B, Doblaré M. An accurate finite element model of the cervical spine under quasi-static loading. J Biomech 2008;41:523–531. [DOI] [PubMed] [Google Scholar]
- 42.Tchako A, Sadegh A. A cervical spine model to predict injury scenarios and clinical instability. Sports Biomech 2009;8:78–95. [DOI] [PubMed] [Google Scholar]
- 43.Robin S. HUMOS: human model for safety~ a joint effort towards the development of refined human-like car occupant models. SAE Tech Pap 2001. Report No.: 2001-06-0129. [Google Scholar]
- 44.Meyer F, Bourdet N, Deck C, et al. Human neck finite element model development and validation against original experimental data. Stapp Car Crash J 2004;48:177–206. [DOI] [PubMed] [Google Scholar]
- 45.Ejima S, Ono K, Kaneoka K, et al. Development and validation of the human neck muscle model under impact loading. Paper presented at IRCOBI Conference, 2005.
- 46.Horst Vd. Human head neck response in frontal, lateral and rear end impact loading: Modelling and validation [Doctoral thesis], Eindhoven Technische Universitet, 2004.
- 47.Kuo C, Sheffels J, Fanton M, et al. Passive cervical spine ligaments provide stability during head impacts. J R Soc Interface 2019;16:20190086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de Jongh CU, Basson AH, Scheffer C. Predictive modelling of cervical disc implant wear. J Biomech 2008;41:3177–3183. [DOI] [PubMed] [Google Scholar]
- 49.Bailly N, Diotalevi L, Beauséjour MH, et al. Numerical investigation of the relative effect of disc bulging and ligamentum flavum hypertrophy on the mechanism of central cord syndrome. Clin Biomech (Bristol, Avon) 2020;74:58–65. [DOI] [PubMed] [Google Scholar]
- 50.Herron MR, Park J, Dailey AT, et al. Febio finite element models of the human cervical spine. J Biomech 2020;113:110077. [DOI] [PubMed] [Google Scholar]
- 51.Wong CE, Hu HT, Hsieh MP, et al. Optimization of three-level cervical hybrid surgery to prevent adjacent segment disease: a finite element study. Front Bioeng Biotechnol 2020;8:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nishida N, Mumtaz M, Tripathi S, et al. Biomechanical analysis of posterior ligaments of cervical spine and laminoplasty. Appl Sci 2021;11:7645. [Google Scholar]
- 53.Sun Z, Lu T, Li J, et al. A finite element study on the effects of follower load on the continuous biomechanical responses of subaxial cervical spine. Comput Biol Med 2022;145:105475. [DOI] [PubMed] [Google Scholar]
- 54.Fice JB, Cronin DS, Panzer MB. Cervical spine model to predict capsular ligament response in rear impact. Ann Biomed Eng 2011;39:2152–2162. [DOI] [PubMed] [Google Scholar]
- 55.Laville A, Laporte S, Skalli W. Parametric and subject-specific finite element modelling of the lower cervical spine. Influence of geometrical parameters on the motion patterns. J Biomech 2009;42:1409–1415. [DOI] [PubMed] [Google Scholar]
- 56.Correia MA, McLachlin SD, Cronin DS. Vestibulocollic and cervicocollic muscle reflexes in a finite element neck model during multidirectional impacts. Ann Biomed Eng 2021;49:1645–1656. [DOI] [PubMed] [Google Scholar]
- 57.Putra IPA, Iraeus J, Sato F, et al. Optimization of female head-neck model with active reflexive cervical muscles in low severity rear impact collisions. Ann Biomed Eng 2021;49:115–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zheng Z, Mo F, Liu T, et al. A novel neuromuscular head-neck model and its application on impact analysis. IEEE Trans Neural Syst Rehabil Eng 2021;29:1394–1402. [DOI] [PubMed] [Google Scholar]
- 59.Sun M-S, Cai X-Y, Liu Q, et al. Application of simulation methods in cervical spine dynamics. J Healthc Eng 2020;2020:7289648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li H, Wang Z. Intervertebral disc biomechanical analysis using the finite element modeling based on medical images. Comput Med Imaging Graph 2006;30:363–370. [DOI] [PubMed] [Google Scholar]
- 61.Amirouche F, Solitro GF, Siemionow K, et al. Role of posterior elements in the disc bulging of a degenerated cervical spine. Int J Spine Surg 2015;9:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Beauséjour MH, Petit Y, Hagen J, et al. Contribution of injured posterior ligamentous complex and intervertebral disc on post-traumatic instability at the cervical spine. Comput Methods Biomech Biomed Engin 2020;23:832–843. [DOI] [PubMed] [Google Scholar]
- 63.Khuyagbaatar B, Kim K, Park WM, et al. Effect of posterior decompression extent on biomechanical parameters of the spinal cord in cervical ossification of the posterior longitudinal ligament. Proc Inst Mech Eng H 2016;230:545–552. [DOI] [PubMed] [Google Scholar]
- 64.He T, Zhang J, Yu T, et al. Comparative analysis of the biomechanical characteristics after different minimally invasive surgeries for cervical spondylopathy: a finite element analysis. Front Bioeng Biotechnol 2021;9:772853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Huang H, Liu J, Wang L, et al. A critical review on the biomechanical study of cervical interbody fusion cage. Med Nov Technol Devices 2021;11:100070. [Google Scholar]
- 66.Ke W, Zhi J, Hua W, et al. Percutaneous posterior full-endoscopic cervical foraminotomy and discectomy: a finite element analysis and radiological assessment. Comput Methods Biomech Biomed Engin 2020;23:805–814. [DOI] [PubMed] [Google Scholar]
- 67.Hong-Wan N, Ee-Chon T, Qing-Hang Z. Biomechanical effects of C2-C7 intersegmental stability due to laminectomy with unilateral and bilateral facetectomy. Spine (Phila Pa 1976) 2004;29:1737–1745. [DOI] [PubMed] [Google Scholar]
- 68.Meyer F, Bourdet N, Gunzel K, et al. Development and validation of a coupled head-neck FEM – application to whiplash injury criteria investigation. Int J Crashworthiness 2013;18:40–63. [Google Scholar]
- 69.Kleiven S. Evaluation of head injury criteria using a finite element model validated against experiments on localized brain motion, intracerebral acceleration, and intracranial pressure. Int J Crashworthiness 2006;11:65–79. [Google Scholar]
- 70.Hedenstierna S, Halldin P. How does a three-dimensional continuum muscle model affect the kinematics and muscle strains of a finite element neck model compared to a discrete muscle model in rear-end, frontal, and lateral impacts. Spine (Phila Pa 1976) 2008;33:E236–E245. [DOI] [PubMed] [Google Scholar]
- 71.Hedenstierna S, Halldin P, Siegmund GP. Neck muscle load distribution in lateral, frontal, and rear-end impacts: a three-dimensional finite element analysis. Spine (Phila Pa 1976) 2009;34:2626–2633. [DOI] [PubMed] [Google Scholar]
- 72.Ewing CL, Thomas D, Lustick L, et al. The effect of duration, rate of onset, and peak sled acceleration on the dynamic response of the human head and neck. SAE Tech Pap 1976, Report No.: 0148–7191. [Google Scholar]
- 73.Panjabi MM, Crisco JJ, Vasavada A, et al. Mechanical properties of the human cervical spine as shown by three-dimensional load-displacement curves. Spine (Phila Pa 1976) 2001;26:2692–2700. [DOI] [PubMed] [Google Scholar]
- 74.Moroney SP, Schultz AB, Miller JA, et al. Load-displacement properties of lower cervical spine motion segments. J Biomech 1988;21:769–779. [DOI] [PubMed] [Google Scholar]
- 75.Ewing CL, Thomas DJ, Beeler GW, et al. Dynamic response of the head and neck of the living human to—G x impact acceleration. SAE Tech Pap 1968. Report No.: 0148–7191. [Google Scholar]
- 76.Ewing C, Thomas D, Lustik L, et al. Dynamic response of the human head and neck to+ Gy impact acceleration. SAE Tech Pap 1977. Report No.: 0148–7191. [Google Scholar]
- 77.Wismans J, Van Oorschot H, Woltring HJ. Omni-directional human head-neck response. SAE trans 1986;95:819–837. [Google Scholar]
- 78.Prasad P, Kim A, Weerappuli DPV. Biofidelity of anthropomorphic test devices for rear impact. SAE trans 1997;106:3906–3934. [Google Scholar]
- 79.Liu YK, Krieger K, Njus G, et al. Cervical spine stiffness and geometry of the young human male. Tulane Univ New Orleans La School Med LA USA; 1982. [Google Scholar]
- 80.Halldin P. Injury prevention and numerical modeling of the human head and neck. Department of Aeronautics Royal Inst Tech, 1998.
- 81.Panjabi M, Dvorak J, Crisco J, 3rd, et al. Flexion, extension, and lateral bending of the upper cervical spine in response to alar ligament transections. J Spinal Disord 1991;4:157–167. [DOI] [PubMed] [Google Scholar]
- 82.Goel VK, Winterbottom JM, Schulte KR, et al. Ligamentous laxity across C0-C1-C2 complex. Axial torque-rotation characteristics until failure. Spine (Phila Pa 1976) 1990;15:990–996. [DOI] [PubMed] [Google Scholar]
- 83.Van Ee CA, Nightingale RW, Camacho DL, et al. Tensile properties of the human muscular and ligamentous cervical spine. Stapp Car Crash J 2000;44:85–102. [DOI] [PubMed] [Google Scholar]
- 84.Brolin K, Halldin P. Development of a finite element model of the upper cervical spine and a parameter study of ligament characteristics. Spine (Phila Pa 1976) 2004;29:376–385. [DOI] [PubMed] [Google Scholar]
- 85.Nightingale RW, McElhaney JH, Richardson WJ, et al. Dynamic responses of the head and cervical spine to axial impact loading. J Biomech 1996;29:307–318. [DOI] [PubMed] [Google Scholar]
- 86.Nightingale RW, McElhaney JH, Camacho DL, et al. The dynamic responses of the cervical spine: buckling, end conditions, and tolerance in compressive impacts. Paper presented at SAE Tech Paper 1997.
- 87.Ewing L, Thomas D, Lustick L, et al. Effect of initial position on the human head and neck response to+Y impact acceleration. Paper presented at SAE Tech paper, 1978.
- 88.Halldin P. Prevention and prediction of head and neck injury in traffic accidents, using experimental and numerical methods. Sweden: Department of Aeronautics, Royal Inst Tech; 2003. [Google Scholar]
- 89.Brolin K. Cervical spine injuries-numerical analyses and statistical survey. Sweden: Department of Aeronautics, Royal Inst Tech; 2002. [Google Scholar]
- 90.Leijonhufvud I. Development of an inner car roof design and implementation of muscles in a numerical model of the human neck [Master thesis]. Sweden: Department of Aeronautics, Royal Inst Tech; 2001. [Google Scholar]
- 91.Ono K, Kaneoka K, Wittek A, et al. Cervical injury mechanism based on the analysis of human cervical vertebral motion and head-neck-torso kinematics during low speed rear impacts. SAE Trans 1997;106:3859–3876. [Google Scholar]
- 92.Tropiano P, Thollon L, Arnoux PJ, et al. Using a finite element model to evaluate human injuries application to the HUMOS model in whiplash situation. Spine (Phila Pa 1976) 2004;29:1709–1716. [DOI] [PubMed] [Google Scholar]
- 93.Ng HW, Teo EC, Zhang Q. Influence of cervical disc degeneration after posterior surgical techniques in combined flexion-extension – a nonlinear analytical study. J Biomech Eng 2005;127:186–192. [DOI] [PubMed] [Google Scholar]
- 94.Meyer F, Humm J, Purushothaman Y, et al. Forces and moments in cervical spinal column segments in frontal impacts using finite element modeling and human cadaver tests. J Mech Behav Biomed Mater 2019;90:681–688. [DOI] [PubMed] [Google Scholar]
- 95.Meyer F, Humm J, Yoganandan N, et al. Development of a detailed human neck finite element model and injury risk curves under lateral impact. J Mech Behav Biomed Mater 2021;116:104318. [DOI] [PubMed] [Google Scholar]
- 96.Frechede B, Bertholon N, Saillant G, et al. Finite element model of the human neck during omni-directional impacts. Part II: relation between cervical curvature and risk of injury. Comput Methods Biomech Biomed Eng 2006;9:379–386. [DOI] [PubMed] [Google Scholar]
- 97.Zhang QH, Tan SH, Teo EC. Finite element analysis of head-neck kinematics under simulated rear impact at different accelerations. Proc Inst Mech Eng H 2008;222:781–790. [DOI] [PubMed] [Google Scholar]
- 98.Zhang QH, Tan SH, Teo EC. A numerical study of the effect of axial acceleration on the responses of the cervical spine during low-speed rear-end impact. Proc Inst Mech Eng H 2008;222:1167–1174. [DOI] [PubMed] [Google Scholar]
- 99.Iwamoto M, Nakahira Y, Kimpara H, et al. Development of a human FE model with 3-D geometry of muscles and lateral impact analysis for the arm with muscle activity. SAE Tech Pap 2009. Report No.: 0148–7191. [Google Scholar]
- 100.Iwamoto M, Nakahira Y, Kimpara H, et al. Development of a human body finite element model with multiple muscles and their controller for estimating occupant motions and impact responses in frontal crash situations. Stapp Car Crash J 2012;56:231–268. [DOI] [PubMed] [Google Scholar]
- 101.Kato D, Nakahira Y, Atsumi N, et al. Development of human body model THUMS Version 6 containing muscle controllers and application to injury analysis in frontal collision after brake deceleration. Paper presented at IRCOBI Conference, 2018.
- 102.Panjabi MM. Cervical spine models for biomechanical research. Spine (Phila Pa 1976) 1998;23:2684–2700. [DOI] [PubMed] [Google Scholar]
- 103.Panjabi MM, Nibu K, Cholewicki J. Whiplash injuries and the potential for mechanical instability. Eur Spine J 1998;7:484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Panjabi M, Dvorak J, Duranceau J, et al. Three-dimensional movements of the upper cervical spine. Spine (Phila Pa 1976) 1988;13:726–730. [DOI] [PubMed] [Google Scholar]
- 105.Goel VK, Clark CR, McGowan D, et al. An in-vitro study of the kinematics of the normal, injured and stabilized cervical spine. J Biomech 1984;17:363–376. [DOI] [PubMed] [Google Scholar]
- 106.Goel VK, Clark CR, Gallaes K, et al. Moment-rotation relationships of the ligamentous occipito-atlanto-axial complex. J Biomech 1988;21:673–680. [DOI] [PubMed] [Google Scholar]
- 107.Goel VK, Clausen JD. Prediction of load sharing among spinal components of a C5-C6 motion segment using the finite element approach. Spine (Phila Pa 1976) 1998;23:684–691. [DOI] [PubMed] [Google Scholar]
- 108.Panjabi MM, Ito S, Ivancic PC, et al. Evaluation of the intervertebral neck injury criterion using simulated rear impacts. J Biomech 2005;38:1694–1701. [DOI] [PubMed] [Google Scholar]
- 109.Zhang QH, Teo EC, Ng HW. Development and validation of a CO-C7 FE complex for biomechanical study. J Biomech Eng 2005;127:729–735. [DOI] [PubMed] [Google Scholar]
- 110.Camacho DL, Nightingale RW, Myers BS. Surface friction in near-vertex head and neck impact increases risk of injury. J Biomech 1999;32:293–301. [DOI] [PubMed] [Google Scholar]
- 111.Stemper BD, Yoganandan N, Pintar FA. Validation of a head-neck computer model for whiplash simulation. Med Biol Eng Comput 2004;42:333–338. [DOI] [PubMed] [Google Scholar]
- 112.Dauvilliers F, Bendjellal F, Weiss M, et al. Development of a finite element model of the neck. SAE Trans 1994;103:1645–1659. [Google Scholar]
- 113.Kallieris D, Rizzetti A, Mattern R, et al. Cervical human spine loads during traumatomechanical investigations. Paper presented at IRCOBI Conference, 1996.
- 114.Bertholon N, Robin S, Le Coz J, et al. Human head and cervical spine behaviour during low-speed rear-end impacts: PMHS sled tests with a rigid seat. Paper presented at IRCOBI Conference, 2000.
- 115.Wheeldon JA, Pintar FA, Knowles S, et al. Experimental flexion/extension data corridors for validation of finite element models of the young, normal cervical spine. J Biomech 2006;39:375–380. [DOI] [PubMed] [Google Scholar]
- 116.Ewing CL, Thomas D. Torque versus angular displacement response of human head to-Gx impact acceleration. SAE Tech Pap 1973. Report No.: 0148–7191. [Google Scholar]
- 117.Wismans J, Philippens M, Van Oorschot E, et al. Comparison of human volunteer and cadaver head-neck response in frontal flexion. SAE Trans 1987;96:1323–1335. [Google Scholar]
- 118.Arbogast KB, Balasubramanian S, Seacrist T, et al. Comparison of kinematic responses of the head and spine for children and adults in low-speed frontal sled tests. Stapp Car Crash J 2009;53:329–372. [DOI] [PubMed] [Google Scholar]
- 119.Klinich K, Beebe M, Pritz H, et al. Performance criteria for a biofidelic dummy neck. Draft Report US Department of Transportation, National Highway Traffic Safety Administration, Vehicle Research and Test Center, East Liberty, Ohio, 1992.
- 120.Fuller DA, Kirkpatrick JS, Emery SE, et al. A kinematic study of the cervical spine before and after segmental arthrodesis. Spine (Phila Pa 1976) 1998;23:1649–1656. [DOI] [PubMed] [Google Scholar]
- 121.Palumbo MA, Hulstyn MJ, Fadale PD, et al. The effect of protective football equipment on alignment of the injured cervical spine. Radiographic analysis in a cadaveric model. Am J Sports Med 1996;24:446–453. [DOI] [PubMed] [Google Scholar]
- 122.Teo EC, Zhang QH, Huang RC. Finite element analysis of head-neck kinematics during motor vehicle accidents: analysis in multiple planes. Med Eng Phys 2007;29:54–60. [DOI] [PubMed] [Google Scholar]
- 123.Tchako A, Sadegh AM. Stress changes in intervertebral discs of the cervical spine due to partial discectomies and fusion. J Biomech Eng 2009;131:051013. [DOI] [PubMed] [Google Scholar]
- 124.Espinha LC, Fernandes PR, Folgado J. Computational analysis of bone remodeling during an anterior cervical fusion. J Biomech 2010;43:2875–2880. [DOI] [PubMed] [Google Scholar]
- 125.Kallemeyn N, Gandhi A, Kode S, et al. Validation of a C2-C7 cervical spine finite element model using specimen-specific flexibility data. Med Eng Phys 2010;32:482–489. [DOI] [PubMed] [Google Scholar]
- 126.Li Y, Lewis G. Influence of surgical treatment for disc degeneration disease at C5-C6 on changes in some biomechanical parameters of the cervical spine. Med Eng Phys 2010;32:595–603. [DOI] [PubMed] [Google Scholar]
- 127.Toosizadeh N, Haghpanahi M. Generating a finite element model of the cervical spine: Estimating muscle forces and internal loads. Scientia Iranica 2011;18:1237–1245. [Google Scholar]
- 128.Rousseau MA, Bonnet X, Skalli W. Influence of the geometry of a ball-and-socket intervertebral prosthesis at the cervical spine: a finite element study. Spine (Phila Pa 1976) 2008;33:E10–E14. [DOI] [PubMed] [Google Scholar]
- 129.Yoganandan N, Pintar FA, Stemper BD, et al. Level-dependent coronal and axial moment-rotation corridors of degeneration-free cervical spines in lateral flexion. J Bone Joint Surg Am 2007;89:1066–1074. [DOI] [PubMed] [Google Scholar]
- 130.Yoganandan N, Stemper BD, Pintar FA, et al. Normative segment-specific axial and coronal angulation corridors of subaxial cervical column in axial rotation. Spine (Phila Pa 1976) 2008;33:490–496. [DOI] [PubMed] [Google Scholar]
- 131.Nightingale RW, Doherty BJ, Myers BS, et al. The influence of end condition on human cervical spine injury mechanisms. SAE Trans 1991;100:2040–2048. [Google Scholar]
- 132.Nightingale RW, Carol Chancey V, Ottaviano D, et al. Flexion and extension structural properties and strengths for male cervical spine segments. J Biomech 2007;40:535–542. [DOI] [PubMed] [Google Scholar]
- 133.Kode S, Kallemeyn NA, Smucker JD, et al. The effect of multi-level laminoplasty and laminectomy on the biomechanics of the cervical spine: a finite element study. Iowa Orthop J 2014;34:150–157. [PMC free article] [PubMed] [Google Scholar]
- 134.Gandhi AA, Grosland NM, Kallemeyn NA, et al. Biomechanical analysis of the cervical spine following disc degeneration, disc fusion, and disc replacement: a finite element study. Int J Spine Surg 2019;13:491–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Stoner KE, Abode-Iyamah KO, Fredericks DC, et al. A comprehensive finite element model of surgical treatment for cervical myelopathy. Clin Biomech (Bristol, Avon) 2020;74:79–86. [DOI] [PubMed] [Google Scholar]
- 136.Qi Y, Lewis G. Influence of assigned material combination in a simulated total cervical disc replacement design on kinematics of a model of the full cervical spine: a finite element analysis study. Biomed Mater Eng 2016;27:633–646. [DOI] [PubMed] [Google Scholar]
- 137.Panzer MB, Fice JB, Cronin DS. Cervical spine response in frontal crash. Med Eng Phys 2011;33:1147–1159. [DOI] [PubMed] [Google Scholar]
- 138.Zhang JG, Wang F, Zhou R, et al. A three-dimensional finite element model of the cervical spine: an investigation of whiplash injury. Med Biol Eng Comput 2011;49:193–201. [DOI] [PubMed] [Google Scholar]
- 139.Rosli R, Kashani J, Kadir M. Effects of lateral mass screw rod fixation to the stability of cervical spine after laminectomy. Phys Proc 2011;22:408–413. [Google Scholar]
- 140.Wagnac E, Arnoux PJ, Garo A, et al. Finite element analysis of the influence of loading rate on a model of the full lumbar spine under dynamic loading conditions. Med Biol Eng Comput 2012;50:903–915. [DOI] [PubMed] [Google Scholar]
- 141.Panjabi MM, Pearson AM, Ito S, et al. Cervical spine ligament injury during simulated frontal impact. Spine (Phila Pa 1976) 2004;29:2395–2403. [DOI] [PubMed] [Google Scholar]
- 142.Bolton J, Kent R, Crandall J. Passenger air bag impact and injury response using a hybrid III test dummy and human surrogates: phase 2b. National Highway Traffic Safety Administration NHTSA Biomechanics Test Database 2006:8373. [Google Scholar]
- 143.Davidsson J, Deutscher C, Hell W, et al. Human volunteer kinematics in rear-end sled collisions. J Crash Prev Inj Contr 2001;2:319–333. [Google Scholar]
- 144.Deng B. Kinematics of human cadaver cervical spine during low-speed rear-end impacts. Detroit USA; Wayne State University; 1999. [DOI] [PubMed] [Google Scholar]
- 145.Ivancic PC, Pearson AM, Panjabi MM, et al. Injury of the anterior longitudinal ligament during whiplash simulation. Eur Spine J 2004;13:61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Panjabi MM, Ito S, Pearson AM, et al. Injury mechanisms of the cervical intervertebral disc during simulated whiplash. Spine (Phila Pa 1976) 2004;29:1217–1225. [DOI] [PubMed] [Google Scholar]
- 147.Pearson AM, Ivancic PC, Ito S, et al. Facet joint kinematics and injury mechanisms during simulated whiplash. Spine (Phila Pa 1976) 2004;29:390–397. [DOI] [PubMed] [Google Scholar]
- 148.Siegmund GP, Myers BS, Davis MB, et al. Mechanical evidence of cervical facet capsule injury during whiplash: a cadaveric study using combined shear, compression, and extension loading. Spine (Phila Pa 1976) 2001;26:2095–2101. [DOI] [PubMed] [Google Scholar]
- 149.Nightingale RW, Winkelstein BA, Knaub KE, et al. Comparative strengths and structural properties of the upper and lower cervical spine in flexion and extension. J Biomech 2002;35:725–732. [DOI] [PubMed] [Google Scholar]
- 150.Kubo S, Goel VK, Yang SJ, et al. Biomechanical evaluation of cervical double-door laminoplasty using hydroxyapatite spacer. Spine (Phila Pa 1976) 2003;28:227–234. [DOI] [PubMed] [Google Scholar]
- 151.Pelker RR, Duranceau JS, Panjabi MM. Cervical spine stabilization. A three-dimensional, biomechanical evaluation of rotational stability, strength, and failure mechanisms. Spine (Phila Pa 1976) 1991;16:117–122. [PubMed] [Google Scholar]
- 152.Goto K, Tajima N, Chosa E, et al. Effects of lumbar spinal fusion on the other lumbar intervertebral levels (three-dimensional finite element analysis). J Orthop Sci 2003;8:577–584. [DOI] [PubMed] [Google Scholar]
- 153.Panjabi MM, Summers DJ, Pelker RR, et al. Three-dimensional load-displacement curves due to forces on the cervical spine. J Orthop Res 1986;4:152–161. [DOI] [PubMed] [Google Scholar]
- 154.Moroney SP, Schultz AB, Miller JA. Analysis and measurement of neck loads. J Orthop Res 1988;6:713–720. [DOI] [PubMed] [Google Scholar]
- 155.Fice JB, Cronin DS. Investigation of whiplash injuries in the upper cervical spine using a detailed neck model. J Biomech 2012;45:1098–1102. [DOI] [PubMed] [Google Scholar]
- 156.Cronin DS. Finite element modeling of potential cervical spine pain sources in neutral position low speed rear impact. J Mech Behav Biomed Mater 2014;33:55–66. [DOI] [PubMed] [Google Scholar]
- 157.Shateri H, Cronin DS. Out-of-Position Rear Impact Tissue-Level Investigation Using Detailed Finite Element Neck Model. Traffic Inj Prev 2015;16:698–708. [DOI] [PubMed] [Google Scholar]
- 158.Lee JH, Park WM, Kim YH, et al. A biomechanical analysis of an artificial disc with a shock-absorbing core property by using whole-cervical spine finite element analysis. Spine (Phila Pa 1976) 2016;41:E893–E901. [DOI] [PubMed] [Google Scholar]
- 159.Rosli R, Abdul Kadir MR, Kamarul T. Stability of cervical spine after one-level corpectomy using different numbers of screws and plate systems. Proc Inst Mech Eng H 2014;228:342–349. [DOI] [PubMed] [Google Scholar]
- 160.Wei W, Liao S, Shi S, et al. Straightened cervical lordosis causes stress concentration: a finite element model study. Austr Phys Eng Sci Med 2013;36:27–33. [DOI] [PubMed] [Google Scholar]
- 161.Xie T, Qian J, Lu Y, et al. Biomechanical comparison of laminectomy, hemilaminectomy and a new minimally invasive approach in the surgical treatment of multilevel cervical intradural tumour: a finite element analysis. Eur Spine J 2013;22:2719–2730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Mesfar W, Moglo K. Effect of the transverse ligament rupture on the biomechanics of the cervical spine under a compressive loading. Clin Biomech (Bristol, Avon) 2013;28:846–852. [DOI] [PubMed] [Google Scholar]
- 163.Erbulut DU, Zafarparandeh I, Lazoglu I, et al. Application of an asymmetric finite element model of the C2-T1 cervical spine for evaluating the role of soft tissues in stability. Med Eng Phys 2014;36:915–921. [DOI] [PubMed] [Google Scholar]
- 164.Fice J, Moulton J, Cronin D. Development of a Detailed Finite Element Neck Model for Automotive Safety Research. Paper presented at: Thirty-Ninth International Workshop on Human Subjects for Biomechanical Research, 2011.
- 165.Camacho DL, Nightingale RW, Robinette JJ, et al. Experimental flexibility measurements for the development of a computational head-neck model validated for near-vertex head impact. Paper presented at SAE Trans,1997.
- 166.Dibb AT, Nightingale RW, Luck JF, et al. Tension and combined tension-extension structural response and tolerance properties of the human male ligamentous cervical spine. J Biomech Eng 2009;131:081008. [DOI] [PubMed] [Google Scholar]
- 167.Ivancic PC, Panjabi MM, Ito S, et al. Biofidelic whole cervical spine model with muscle force replication for whiplash simulation. Eur Spine J 2005;14:346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ito S, Ivancic PC, Pearson AM, et al. Cervical intervertebral disc injury during simulated frontal impact. Eur Spine J 2005;14:356–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ivancic PC, Panjabi MM, Tominaga Y, et al. Predicting multiplanar cervical spine injury due to head-turned rear impacts using IV-NIC. Traffic Inj Prev 2006;7:264–275. [DOI] [PubMed] [Google Scholar]
- 170.Ivancic PC, Ito S, Tominaga Y, et al. Effect of rotated head posture on dynamic vertebral artery elongation during simulated rear impact. Clin Biomech (Bristol, Avon) 2006;21:213–220. [DOI] [PubMed] [Google Scholar]
- 171.Hynd D, Svensson M, Trosseille X, et al. Dummy requirements and injury criteria for a low-speed rear impact whiplash dummy. Eur Enhanced Vehicle-Saf Committee 2007;505:2007. [Google Scholar]
- 172.Thunnissen J, Wismans J, Ewing C, et al. Human volunteer head-neck response in frontal flexion: a new analysis. SAE Trans 1995;104:3065–3086. [Google Scholar]
- 173.Traynelis VC, Donaher PA, Roach RM, et al. Biomechanical comparison of anterior Caspar plate and three-level posterior fixation techniques in a human cadaveric model. J Neurosurg 1993;79:96–103. [DOI] [PubMed] [Google Scholar]
- 174.White NA, Moreno DP, Gayzik FS, et al. Cross-sectional neck response of a total human body FE model during simulated frontal and side automobile impacts. Comput Methods Biomech Biomed Eng 2015;18:293–315. [DOI] [PubMed] [Google Scholar]
- 175.Corrales MA, Cronin DS. Importance of the cervical capsular joint cartilage geometry on head and facet joint kinematics assessed in a finite element neck model. J Biomech 2021;123:110528. [DOI] [PubMed] [Google Scholar]
- 176.Corrales MA, Cronin DS. Sex, age and stature affects neck biomechanical responses in frontal and rear impacts assessed using finite element head and neck models. Front Bioeng Biotechnol 2021;9:681134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Whyte T, Barker JB, Cronin DS, et al. Load-sharing and kinematics of the human cervical spine under multi-axial transverse shear loading: combined experimental and computational investigation. J Biomech Eng 2021;143:061013. [DOI] [PubMed] [Google Scholar]
- 178.Hadagali P, Fischer SL, Callaghan JP, et al. Quantifying the importance of active muscle repositioning a finite element neck model in flexion using kinematic, kinetic, and tissue-level responses. Ann Biomed Eng 2024;52:510–525. [DOI] [PubMed] [Google Scholar]
- 179.Rycman A, McLachlin SD, Cronin DS. Spinal cord boundary conditions affect brain tissue strains in impact simulations. Ann Biomed Eng 2023;51:783–793. [DOI] [PubMed] [Google Scholar]
- 180.Zafarparandeh I, Erbulut DU, Ozer AF. Motion analysis study on sensitivity of finite element model of the cervical spine to geometry. Proc Inst Mech Eng H 2016;230:700–706. [DOI] [PubMed] [Google Scholar]
- 181.Mumtaz M, Zafarparandeh I, Erbulut DU. Investigation into cervical spine biomechanics following single, multilevel and hybrid disc replacement surgery with dynamic cervical implant and fusion: a finite element study. Bioengineering 2022;9:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Howley S, Bonneau D, Fréchède B. A framework towards personalisation and active muscle integration in a 3D finite-element neck model for orthopaedic applications. Comput Methods Biomech Biomed Engin 2014;17(suppl 1):74–75. [DOI] [PubMed] [Google Scholar]
- 183.Wang J, Qian Z, Ren L, et al. A dynamic finite element model of human cervical spine with in vivo kinematic validation. Chin Sci Bull 2014;59:4578–4588. [Google Scholar]
- 184.Chung TT, Hueng DY, Lin SC. Hybrid strategy of two-level cervical artificial disc and intervertebral cage: biomechanical effects on tissues and implants. Medicine (Baltimore) 2015;94:e2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Wang Z, Zhao H, Liu JM, et al. Resection or degeneration of uncovertebral joints altered the segmental kinematics and load-sharing pattern of subaxial cervical spine: A biomechanical investigation using a C2-T1 finite element model. J Biomech 2016;49:2854–2862. [DOI] [PubMed] [Google Scholar]
- 186.Jones CF, Kroeker SG, Cripton PA, et al. The effect of cerebrospinal fluid on the biomechanics of spinal cord: an ex vivo bovine model using bovine and physical surrogate spinal cord. Spine (Phila Pa 1976) 2008;33:E580–E588. [DOI] [PubMed] [Google Scholar]
- 187.Persson C, McLure SW, Summers J, et al. The effect of bone fragment size and cerebrospinal fluid on spinal cord deformation during trauma: an ex vivo study. J Neurosurg Spine 2009;10:315–323. [DOI] [PubMed] [Google Scholar]
- 188.Khuyagbaatar B, Kim K, Man Park W, et al. Biomechanical behaviors in three types of spinal cord injury mechanisms. J Biomech Eng 2016;138:081003. [DOI] [PubMed] [Google Scholar]
- 189.Khuyagbaatar B, Kim K, Park WM, et al. Biomechanical investigation of post-operative C5 palsy due to ossification of the posterior longitudinal ligament in different types of cervical spinal alignment. J Biomech 2017;57:54–61. [DOI] [PubMed] [Google Scholar]
- 190.Khuyagbaatar B, Kim K, Park WM, et al. Increased stress and strain on the spinal cord due to ossification of the posterior longitudinal ligament in the cervical spine under flexion after laminectomy. Proc Inst Mech Eng H 2017;231:898–906. [DOI] [PubMed] [Google Scholar]
- 191.Khuyagbaatar B, Kim K, Purevsuren T, et al. Biomechanical effects on cervical spinal cord and nerve root following laminoplasty for ossification of the posterior longitudinal ligament in the cervical spine: a comparison between open-door and double-door laminoplasty using finite element analysis. J Biomech Eng 2018;140:071006. [DOI] [PubMed] [Google Scholar]
- 192.Wang Z, Zhao H, Liu JM, et al. Biomechanics of anterior plating failure in treating distractive flexion injury in the caudal subaxial cervical spine. Clin Biomech (Bristol, Avon) 2017;50:130–138. [DOI] [PubMed] [Google Scholar]
- 193.Liu Y, Wang Z, Liu M, et al. Biomechanical influence of the surgical approaches, implant length and density in stabilizing ankylosing spondylitis cervical spine fracture. Sci Rep 2021;11:6023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Deng Z, Wang K, Wang H, et al. A finite element study of traditional Chinese cervical manipulation. Eur Spine J 2017;26:2308–2317. [DOI] [PubMed] [Google Scholar]
- 195.Wang K, Wang H, Deng Z, et al. Cervical traction therapy with and without neck support: a finite element analysis. Musculoskelet Sci Pract 2017;28:1–9. [DOI] [PubMed] [Google Scholar]
- 196.Rong X, Wang B, Ding C, et al. The biomechanical impact of facet tropism on the intervertebral disc and facet joints in the cervical spine. Spine J 2017;17:1926–1931. [DOI] [PubMed] [Google Scholar]
- 197.Gadomski BC, Shetye SS, Hindman BJ, et al. Intubation biomechanics: validation of a finite element model of cervical spine motion during endotracheal intubation in intact and injured conditions. J Neurosurg Spine 2018;28:10–22. [DOI] [PubMed] [Google Scholar]
- 198.Putra IPA, Iraeus J, Thomson R, et al. Comparison of control strategies for the cervical muscles of an average female head-neck finite element model. Traffic Inj Prev 2019;20(suppl 2):S116–S122. [DOI] [PubMed] [Google Scholar]
- 199.Östh J, Mendoza-Vazquez M, Sato F, et al. A female head-neck model for rear impact simulations. J Biomech 2017;51:49–56. [DOI] [PubMed] [Google Scholar]
- 200.Vasavada AN, Danaraj J, Siegmund GP. Head and neck anthropometry, vertebral geometry and neck strength in height-matched men and women. J Biomech 2008;41:114–121. [DOI] [PubMed] [Google Scholar]
- 201.Francis CC. Dimensions of the cervical vertebrae. Anat Rec 1955;122:603–609. [DOI] [PubMed] [Google Scholar]
- 202.Mattucci SF, Cronin DS. A method to characterize average cervical spine ligament response based on raw data sets for implementation into injury biomechanics models. J Mech Behav Biomed Mater 2015;41:251–260. [DOI] [PubMed] [Google Scholar]
- 203.Mattucci SF, Moulton JA, Chandrashekar N, et al. Strain rate dependent properties of younger human cervical spine ligaments. J Mech Behav Biomed Mater 2012;10:216–226. [DOI] [PubMed] [Google Scholar]
- 204.Myklebust JB, Pintar F, Yoganandan N, et al. Tensile strength of spinal ligaments. Spine (Phila Pa 1976) 1988;13:526–531. [PubMed] [Google Scholar]
- 205.Sato F, Odani M, Miyazaki Y, et al. Effects of whole spine alignment patterns on neck responses in rear end impact. Traffic Inj Prev 2017;18:199–206. [DOI] [PubMed] [Google Scholar]
- 206.Stemper BD, Yoganandan N, Pintar FA. Gender dependent cervical spine segmental kinematics during whiplash. J Biomech 2003;36:1281–1289. [DOI] [PubMed] [Google Scholar]
- 207.Stemper BD, Yoganandan N, Pintar FA. Gender- and region-dependent local facet joint kinematics in rear impact: implications in whiplash injury. Spine (Phila Pa 1976) 2004;29:1764–1771. [DOI] [PubMed] [Google Scholar]
- 208.Stemper BD, Yoganandan N, Pintar FA. Response corridors of the human head-neck complex in rear impact. Annu Proc Assoc Adv Automot Med 2004;48:149–163. [PMC free article] [PubMed] [Google Scholar]
- 209.Lysell E. Motion in the cervical spine. An experimental study on autopsy specimens. Acta Orthop Scand 1969;(Suppl 1)23:121+. [DOI] [PubMed] [Google Scholar]
- 210.Liu Q, Guo Q, Yang J, et al. Subaxial cervical intradiscal pressure and segmental kinematics following atlantoaxial fixation in different angles. World Neurosurg 2016;87:521–528. [DOI] [PubMed] [Google Scholar]
- 211.Putra IPA, Thomson R. Analysis of control strategies for VIVA OpenHBM with active reflexive neck muscles. Biomech Model Mechanobiol 2022;21:1731–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Putra IPA, Iraeus J, Sato F, et al. Finite element human body models with active reflexive muscles suitable for sex based whiplash injury prediction. Front Bioeng Biotechnol 2022;10:968939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Chang L, Wang H, Guo Y, et al. Experimental and numerical analysis of biomechanical effects in cervical spine positioning rotation manipulation. Int J Numeric Methods Biomed Eng 2022;38:e3651. [DOI] [PubMed] [Google Scholar]
- 214.Mihara A, Kanchiku T, Nishida N, et al. Biomechanical analysis of brachial plexus injury: availability of three-dimensional finite element model of the brachial plexus. Exp Ther Med 2018;15:1989–1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Yan Y, Huang J, Li F, et al. Investigation of the effect of neck muscle active force on whiplash injury of the cervical spine. Appl Bionics Biomech 2018;2018:4542750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.John JD, Saravana Kumar G, Yoganandan N. Rear-impact neck whiplash: role of head inertial properties and spine morphological variations on segmental rotations. J Biomech Eng 2019;141:111008. [DOI] [PubMed] [Google Scholar]
- 217.Park WM, Jin YJ. Biomechanical investigation of extragraft bone formation influences on the operated motion segment after anterior cervical spinal discectomy and fusion. Sci Rep 2019;9:18850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Xie YM, Zheng YC, Qiu SJ, et al. The appropriate hybrid surgical strategy in three-level cervical degenerative disc disease: a finite element analysis. J Orthop Surg Res 2019;14:444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Moran SL, Steinmann SP, Shin AY. Adult brachial plexus injuries: mechanism, patterns of injury, and physical diagnosis. Hand Clin 2005;21:13–24. [DOI] [PubMed] [Google Scholar]
- 220.Coene LN. Mechanisms of brachial plexus lesions. Clin Neurol Neurosurg 1993;95 (Suppl):S24–S29. [DOI] [PubMed] [Google Scholar]
- 221.Ono K, Inami S, Kaneoka K, et al. Relationship between localized spine deformation and cervical vertebral motions for low speed rear impacts using human volunteers. SAE Tech Pap 1999. [Google Scholar]
- 222.Gilad I, Nissan M. A study of vertebra and disc geometric relations of the human cervical and lumbar spine. Spine (Phila Pa 1976) 1986;11:154–157. [DOI] [PubMed] [Google Scholar]
- 223.Stemper BD, Yoganandan N, Pintar FA, et al. Anatomical gender differences in cervical vertebrae of size-matched volunteers. Spine (Phila Pa 1976) 2008;33:E44–E49. [DOI] [PubMed] [Google Scholar]
- 224.Finn MA, Brodke DS, Daubs M, et al. Local and global subaxial cervical spine biomechanics after single-level fusion or cervical arthroplasty. Eur Spine J 2009;18:1520–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Purushothaman Y, Humm J, Jebaseelan D, et al. Neck vertebral level-specific forces and moments under G-x accelerative loading. Mil Med 2021;186(suppl 1):625–631. [DOI] [PubMed] [Google Scholar]
- 226.Yoganandan N, Choi H, Purushothaman Y, et al. Effects of different severities of disc degeneration on the range of motion of cervical spine. J Craniovertebr Junction Spine 2020;11:269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Choi H, Purushothaman Y, Baisden J, et al. Unique biomechanical signatures of Bryan, Prodisc C, and Prestige LP cervical disc replacements: a finite element modelling study. Eur Spine J 2020;29:2631–2639. [DOI] [PubMed] [Google Scholar]
- 228.Choi H, Purushothaman Y, Baisden JL, et al. Comparative finite element modeling study of anterior cervical arthrodesis versus cervical arthroplasty with bryan disc or prodisc C. Mil Med 2021;186(Suppl 1):737–744. [DOI] [PubMed] [Google Scholar]
- 229.John JD, Kumar GS, Yoganandan N, et al. Influence of cervical spine sagittal alignment on range of motion after corpectomy: a finite element study. Acta Neurochir 2021;163:251–257. [DOI] [PubMed] [Google Scholar]
- 230.Purushothaman Y, Yoganandan N, Jebaseelan D, et al. External and internal responses of cervical disc arthroplasty and anterior cervical discectomy and fusion: a finite element modeling study. J Mech Behav Biomed Mater 2020;106:103735. [DOI] [PubMed] [Google Scholar]
- 231.Varghese V, Baisden J, Yoganandan N. Normalization technique to build patient specific muscle model in finite element head neck spine. Med Eng Phys 2022;107:103857. [DOI] [PubMed] [Google Scholar]
- 232.Hua W, Zhi J, Wang B, et al. Biomechanical evaluation of adjacent segment degeneration after one- or two-level anterior cervical discectomy and fusion versus cervical disc arthroplasty: a finite element analysis. Comput Methods Programs Biomed 2020;189:105352. [DOI] [PubMed] [Google Scholar]
- 233.Li XF, Jin LY, Liang CG, et al. Adjacent-level biomechanics after single-level anterior cervical interbody fusion with anchored zero-profile spacer versus cage-plate construct: a finite element study. BMC Surg 2020;20:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Subramani AV, Whitley PE, Garimella HT, et al. Fatigue damage prediction in the annulus of cervical spine intervertebral discs using finite element analysis. Comput Methods Biomech Biomed Eng 2020;23:773–784. [DOI] [PubMed] [Google Scholar]
- 235.Hua W, Zhi J, Ke W, et al. Adjacent segment biomechanical changes after one- or two-level anterior cervical discectomy and fusion using either a zero-profile device or cage plus plate: a finite element analysis. Comput Biol Med 2020;120:103760. [DOI] [PubMed] [Google Scholar]
- 236.Barker JB, Cronin DS, Chandrashekar N. High rotation rate behavior of cervical spine segments in flexion and extension. J Biomech Eng 2014;136:121004. [DOI] [PubMed] [Google Scholar]
- 237.Pospiech J, Stolke D, Wilke HJ, et al. Intradiscal pressure recordings in the cervical spine. Neurosurgery 1999;44:379–384; discussion 384-5. [DOI] [PubMed] [Google Scholar]
- 238.Leahy PD. Assessment of the effects of ligamentous injury in the human cervical spine. Fort Collins USA:Colorado State University; 2012. [Google Scholar]
- 239.Leahy PD, Puttlitz CM. The effects of ligamentous injury in the human lower cervical spine. J Biomech 2012;45:2668–2672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.White AA, III, Panjabi MM. Clinical Biomechanics of the Spine, 2nd ed. J.B. Lippincott Company; 1990. [Google Scholar]
- 241.Patel VV, Wuthrich ZR, McGilvray KC, et al. Cervical facet force analysis after disc replacement versus fusion. Clin Biomech (Bristol, Avon) 2017;44:52–58. [DOI] [PubMed] [Google Scholar]
- 242.Zhao X, Yuan W. Biomechanical analysis of cervical range of motion and facet contact force after a novel artificial cervical disc replacement. Am J Transl Res 2019;11:3109–3115. [PMC free article] [PubMed] [Google Scholar]
- 243.Kretzer RM, Hsu W, Hu N, et al. Adjacent-level range of motion and intradiscal pressure after posterior cervical decompression and fixation: an in vitro human cadaveric model. Spine (Phila Pa 1976) 2012;37:E778–E785. [DOI] [PubMed] [Google Scholar]
- 244.Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine (Phila Pa 1976) 2002;27:2431–2434. [DOI] [PubMed] [Google Scholar]
- 245.Lu J, Ebraheim NA, Yang H, et al. Anatomic bases for anterior spinal surgery: surgical anatomy of the cervical vertebral body and disc space. Surg Radiol Anat 1999;21:235–239. [DOI] [PubMed] [Google Scholar]
- 246.Miura T, Panjabi MM, Cripton PA. A method to simulate in vivo cervical spine kinematics using in vitro compressive preload. Spine (Phila Pa 1976) 2002;27:43–48. [DOI] [PubMed] [Google Scholar]
- 247.Mitsuhashi N, Fujieda K, Tamura T, et al. BodyParts3D: 3D structure database for anatomical concepts. Nucleic Acids Res 2009;37(Database issue):D782–D785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Bazaldúa Cruz JJ, González Larios A, Gómez Sánchez A, et al. Morphometric study of cervical vertebrae C3-C7 in a population from Northeastern Mexico. Int J Morphol 2011;29:325–330. [Google Scholar]
- 249.Lévy S, Baucher G, Roche PH, et al. Biomechanical comparison of spinal cord compression types occurring in degenerative cervical myelopathy. Clin Biomech (Bristol, Avon) 2021;81:105174. [DOI] [PubMed] [Google Scholar]
- 250.Li XF, Lv ZD, Yin HL, et al. Impact of adjacent pre-existing disc degeneration status on its biomechanics after single-level anterior cervical interbody fusion. Comput Methods Programs Biomed 2021;209:106355. [DOI] [PubMed] [Google Scholar]
- 251.Sun X, Sun S, Zhang T, et al. Biomechanical comparison of noncontiguous cervical disc arthroplasty and noncontiguous cervical discectomy and fusion in the treatment of noncontinuous cervical degenerative disc disease: a finite element analysis. J Orthop Surg Res 2020;15:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Barker JB, Cronin DS. Multilevel validation of a male neck finite element model with active musculature. J Biomech Eng 2021;143:011004. [DOI] [PubMed] [Google Scholar]
- 253.Cao F, Fu R, Wang W. Comparison of biomechanical performance of single-level triangular and quadrilateral profile anterior cervical plates. PLoS One 2021;16:e0250270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Nasim M, Cernicchi A, Galvanetto U. Development of a finite element neck model for head-first compressive impacts: toward the assessment of motorcycle neck protective equipment. Proc Inst Mech Eng H 2021;235:1001–1013. [DOI] [PubMed] [Google Scholar]
- 255.Wu TK, Meng Y, Wang BY, et al. Biomechanics following skip-level cervical disc arthroplasty versus skip-level cervical discectomy and fusion: a finite element-based study. BMC Musculoskelet Disord 2019;20:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Lee MJ, Dumonski M, Phillips FM, et al. Disc replacement adjacent to cervical fusion: a biomechanical comparison of hybrid construct versus two-level fusion. Spine (Phila Pa 1976) 2011;36:1932–1939. [DOI] [PubMed] [Google Scholar]
- 257.Wigfield CC, Skrzypiec D, Jackowski A, et al. Internal stress distribution in cervical intervertebral discs: the influence of an artificial cervical joint and simulated anterior interbody fusion. J Spinal Disord Tech 2003;16:441–449. [DOI] [PubMed] [Google Scholar]
- 258.Skrzypiec DM, Pollintine P, Przybyla A, et al. The internal mechanical properties of cervical intervertebral discs as revealed by stress profilometry. Eur Spine J 2007;16:1701–1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Chen J-W, Chen W-C, Lai Y-S, et al. Effect of a novel compressible artificial disk on biomechanical performance of cervical spine: a finite element study. Adv Mech Eng 2015;7:1–5. [Google Scholar]
- 260.Deng B, Begeman PC, Yang KH, et al. Kinematics of human cadaver cervical spine during low speed rear-end impacts. Stapp Car Crash J 2000;44:171–188. [DOI] [PubMed] [Google Scholar]
- 261.Bosio AC, Bowman BM. Simulation of head-neck dynamic response in −Gx and +Gy. SAE Tech Pap 1986. Report No.: 0148–7191. [Google Scholar]
- 262.Spenny CH. Performance criteria for a mechanical head/neck that predicts secondary impact force levels during frontal flexion. SAE Trans 1987;96:1360–1370. [Google Scholar]
- 263.Wismans J, Spenny CH. Performance requirements for mechanical necks in lateral flexion. SAE Trans 1983;92:459–470. [Google Scholar]
- 264.Nightingale RW, McElhaney JH, Richardson WJ, et al. Experimental impact injury to the cervical spine: relating motion of the head and the mechanism of injury. J Bone Joint Surg Am 1996;78:412–421. [DOI] [PubMed] [Google Scholar]
- 265.Nightingale RW, McElhaney JH, Camacho DL, et al. The dynamic responses of the cervical spine: buckling, end conditions, and tolerance in compressive impacts. SAE Trans 1997;106:3968–3988. [Google Scholar]
- 266.Ovsepyan AL, Smirnov AA, Pustozerov EA, et al. Biomechanical analysis of the cervical spine segment as a method for studying the functional and dynamic anatomy of the human neck. Ann Anat 2021;240:151856. [DOI] [PubMed] [Google Scholar]
- 267.Sun J, Wang Q, Cai D, et al. A lattice topology optimization of cervical interbody fusion cage and finite element comparison with ZK60 and Ti-6Al-4V cages. BMC Musculoskelet Disord 2021;22:390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Wo J, Lv Z, Wang J, et al. Biomechanical analysis of cervical artificial disc replacement using cervical subtotal discectomy prosthesis. Front Bioeng Biotechnol 2021;9:680769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Xiao LX, Liu CS, Zhong SZ, et al. Effect of a traction exercise neck brace on cervical spondylopathy radiculopathy: a clinical study and finite element analysis. Evid Based Complement Alternat Med 2021;2021:8825150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Xie T, Feng Y, Chen B, et al. Biomechanical evaluation of the craniovertebral junction after odontoidectomy with anterior C1 arch preservation: a finite element study. Clin Neurol Neurosurg 2021;211:106987. [DOI] [PubMed] [Google Scholar]
- 271.Shea M, Edwards WT, White AA, et al. Variations of stiffness and strength along the human cervical spine. J Biomech 1991;24:95–107. [DOI] [PubMed] [Google Scholar]
- 272.Penning L. Normal movements of the cervical spine. Am J Roentgenol 1978;130:317–326. [DOI] [PubMed] [Google Scholar]
- 273.Penning L, Wilmink JT. Rotation of the cervical spine. A CT study in normal subjects. Spine (Phila Pa 1976) 1987;12:732–738. [DOI] [PubMed] [Google Scholar]
- 274.Mimura M, Moriya H, Watanabe T, et al. Three-dimensional motion analysis of the cervical spine with special reference to the axial rotation. Spine (Phila Pa 1976) 1989;14:1135–1139. [DOI] [PubMed] [Google Scholar]
- 275.Holmes A, Wang C, Han ZH, et al. The range and nature of flexion-extension motion in the cervical spine. Spine (Phila Pa 1976) 1994;19:2505–2510. [DOI] [PubMed] [Google Scholar]
- 276.Iai H, Goto S, Yamagata M, et al. Three-dimensional motion of the upper cervical spine in rheumatoid arthritis. Spine (Phila Pa 1976) 1994;19:272–276. [DOI] [PubMed] [Google Scholar]
- 277.Clausen JD, Goel VK, Traynelis VC, et al. Uncinate processes and Luschka joints influence the biomechanics of the cervical spine: quantification using a finite element model of the C5-C6 segment. J Orthop Res 1997;15:342–347. [DOI] [PubMed] [Google Scholar]
- 278.Lind B, Sihlbom H, Nordwall A, et al. Normal range of motion of the cervical spine. Arch Phys Med Rehabil 1989;70:692–695. [PubMed] [Google Scholar]
- 279.Ishii T, Mukai Y, Hosono N, et al. Kinematics of the cervical spine in lateral bending: in vivo three-dimensional analysis. Spine (Phila Pa 1976) 2006;31:155–160. [DOI] [PubMed] [Google Scholar]
- 280.Ito S, Ivancic PC, Panjabi MM, et al. Soft tissue injury threshold during simulated whiplash: a biomechanical investigation. Spine (Phila Pa 1976) 2004;29:979–987. [DOI] [PubMed] [Google Scholar]
- 281.Li TC, Liu CJ, Liu SY, et al. Effect of muscle activation on dynamic responses of neck of pilot during emergency ejection: a finite element study. Med Biol Eng Comput 2023;61:2255–2268. [DOI] [PubMed] [Google Scholar]
- 282.Been E, Shefi S, Soudack M. Cervical lordosis: the effect of age and gender. Spine J 2017;17:880–888. [DOI] [PubMed] [Google Scholar]
- 283.Yukawa Y, Kato F, Suda K, et al. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: radiographic data from over 1,200 asymptomatic subjects. Eur Spine J 2012;21:1492–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Panjabi MM, Oxland TR, Parks EH. Quantitative anatomy of cervical spine ligaments. Part II. Middle and lower cervical spine. J Spinal Disord 1991;4:277–285. [DOI] [PubMed] [Google Scholar]
- 285.Bell KM, Yan Y, Hartman RA, et al. Influence of follower load application on moment-rotation parameters and intradiscal pressure in the cervical spine. J Biomech 2018;76:167–172. [DOI] [PubMed] [Google Scholar]
- 286.Fournely M, Petit Y, Wagnac E, et al. Effect of experimental, morphological and mechanical factors on the murine spinal cord subjected to transverse contusion: a finite element study. PLoS One 2020;15:e0232975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Fournely M, Petit Y, Wagnac É, et al. High-speed video analysis improves the accuracy of spinal cord compression measurement in a mouse contusion model. J Neurosci Methods 2018;293:1–5. [DOI] [PubMed] [Google Scholar]
- 288.Mattucci SF, Moulton JA, Chandrashekar N, et al. Strain rate dependent properties of human craniovertebral ligaments. J Mech Behav Biomed Mater 2013;23:71–79. [DOI] [PubMed] [Google Scholar]
- 289.White NA, Begeman PC, Hardy WN, et al. Investigation of upper body and cervical spine kinematics of post mortem human subjects (PMHS) during low-speed, rear-end impacts. SAE Tech Pap 2009:0148–7191. [Google Scholar]
- 290.Yoganandan N, Pintar F, Butler J, et al. Dynamic response of human cervical spine ligaments. Spine 1989;14:1102–1110. [DOI] [PubMed] [Google Scholar]
- 291.Nishida N, Tripathi S, Mumtaz M, et al. Soft tissue injury in cervical spine is a risk factor for intersegmental instability: a finite element analysis. World Neurosurg 2022;164:e358–e366. [DOI] [PubMed] [Google Scholar]
- 292.Liang Z, Xu G, Liu T, et al. Quantitatively biomechanical response analysis of posterior musculature reconstruction in cervical single-door laminoplasty. Comput Methods Programs Biomed 2023;233:107479. [DOI] [PubMed] [Google Scholar]
- 293.Chancey VC, Nightingale RW, Van Ee CA, et al. Improved estimation of human neck tensile tolerance: reducing the range of reported tolerance using anthropometrically correct muscles and optimized physiologic initial conditions. Stapp Car Crash J 2003;47:135–153. [DOI] [PubMed] [Google Scholar]
- 294.Galbusera F, Raimondi MT, Assietti R, et al. Multibody modeling of the cervical spine in the simulation of flexion-extension after disc arthroplasty. J Appl Biomater Biomech 2006;4:110–119. [PubMed] [Google Scholar]
- 295.Ahn HS, DiAngelo DJ. Biomechanical testing simulation of a cadaver spine specimen: development and evaluation study. Spine (Phila Pa 1976) 2007;32:E330–E336. [DOI] [PubMed] [Google Scholar]
- 296.van Lopik DW, Acar M. Development of a multi-body computational model of human head and neck. Proc Inst Mech Eng Part K: J Multi-body Dynam 2007;221:175–197. [Google Scholar]
- 297.Oi N, Pandy MG, Myers BS, et al. Variation of neck muscle strength along the human cervical spine. Stapp Car Crash J 2004;48:397–417. [DOI] [PubMed] [Google Scholar]
- 298.Seng KY, Lee Peter VS, Lam PM. Neck muscle strength across the sagittal and coronal planes: an isometric study. Clin Biomech (Bristol, Avon) 2002;17:545–547. [DOI] [PubMed] [Google Scholar]
- 299.Peolsson A, Oberg B, Hedlund R. Intra- and inter-tester reliability and reference values for isometric neck strength. Physiother Res Int 2001;6:15–26. [DOI] [PubMed] [Google Scholar]
- 300.Jordan A, Mehlsen J, Bulow PM, et al. Maximal isometric strength of the cervical musculature in 100 healthy volunteers. Spine (Phila Pa 1976) 1999;24:1343–1348. [DOI] [PubMed] [Google Scholar]
- 301.Panjabi M, Dvorak J, Crisco JJ, 3rd, et al. Effects of alar ligament transection on upper cervical spine rotation. J Orthop Res 1991;9:584–593. [DOI] [PubMed] [Google Scholar]
- 302.Ewing CL, Thomas DJ. Human head and neck response to impact acceleration. Naval Aerospace and Regional Medical Centre 1972. [Google Scholar]
- 303.Aho A, Vartiainen O, Salo O. Segmentary antero-posterior mobility of the cervical spine. Ann Med Intern Fenn 1955;44:287–299. [PubMed] [Google Scholar]
- 304.Bhalla SK, Simmons EH. Normal ranges of intervertebral-joint motion of the cervical spine. Can J Surg 1969;12:181–187. [PubMed] [Google Scholar]
- 305.Dvorak J, Froehlich D, Penning L, et al. Functional radiographic diagnosis of the cervical spine: flexion/extension. Spine (Phila Pa 1976) 1988;13:748–755. [DOI] [PubMed] [Google Scholar]
- 306.Milne N. Composite motion in cervical disc segments. Clin Biomech (Bristol, Avon) 1993;8:193–202. [DOI] [PubMed] [Google Scholar]
- 307.Huber ZE. Creation and Validation of a Dynamic, EMG-Driven Cervical Spine Model. Columbus USA: The Ohio State University; 2013. [Google Scholar]
- 308.Khurelbaatar T, Kim K, Hyuk Kim Y. A cervico-thoraco-lumbar multibody dynamic model for the estimation of joint loads and muscle forces. J Biomech Eng 2015;137:111001. [DOI] [PubMed] [Google Scholar]
- 309.Cazzola D, Holsgrove TP, Preatoni E, et al. Cervical spine injuries: a whole-body musculoskeletal model for the analysis of spinal loading. PLoS One 2017;12:e0169329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Kumaresan S, Yoganandan N, Pintar FA, et al. Finite element modeling of the cervical spine: role of intervertebral disc under axial and eccentric loads. Med Eng Phys 1999;21:689–700. [DOI] [PubMed] [Google Scholar]
- 311.Ha SK. Finite element modeling of multi-level cervical spinal segments (C3-C6) and biomechanical analysis of an elastomer-type prosthetic disc. Med Eng Phys 2006;28:534–541. [DOI] [PubMed] [Google Scholar]
- 312.Faizan A, Goel VK, Garfin SR, et al. Do design variations in the artificial disc influence cervical spine biomechanics? A finite element investigation. Eur Spine J 2012;21(suppl 5):S653–S662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Forbes PA, de Bruijn E, Schouten AC, et al. Dependency of human neck reflex responses on the bandwidth of pseudorandom anterior-posterior torso perturbations. Exp Brain Res 2013;226:1–14. [DOI] [PubMed] [Google Scholar]
- 314.Ludewig PM, Phadke V, Braman JP, et al. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am 2009;91:378–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Ludewig PM, Hassett DR, Laprade RF, et al. Comparison of scapular local coordinate systems. Clin Biomech (Bristol, Avon) 2010;25:415–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Dvorak J, Antinnes JA, Panjabi M, et al. Age and gender related normal motion of the cervical spine. Spine (Phila Pa 1976) 1992;17(Suppl 10):S393–S398. [DOI] [PubMed] [Google Scholar]
- 317.Dvorak J, Hayek J, Zehnder R. CT-functional diagnostics of the rotatory instability of the upper cervical spine. Part 2. An evaluation on healthy adults and patients with suspected instability. Spine (Phila Pa 1976) 1987;12:726–731. [DOI] [PubMed] [Google Scholar]
- 318.Dvorák J, Panjabi MM, Grob D, et al. Clinical validation of functional flexion/extension radiographs of the cervical spine. Spine (Phila Pa 1976) 1993;18:120–127. [DOI] [PubMed] [Google Scholar]
- 319.Diao H, Xin H, Dong J, et al. Prediction of cervical spinal joint loading and secondary motion using a musculoskeletal multibody dynamics model via force-dependent kinematics approach. Spine (Phila Pa 1976) 2017;42:E1403–E1409. [DOI] [PubMed] [Google Scholar]
- 320.Mortensen JD, Vasavada AN, Merryweather AS. The inclusion of hyoid muscles improve moment generating capacity and dynamic simulations in musculoskeletal models of the head and neck. PLoS One 2018;13:e0199912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Arshad R, Schmidt H, El-Rich M, et al. Sensitivity of the Cervical disc loads, translations, intradiscal pressure, and muscle activity due to segmental mass, disc stiffness, and muscle strength in an upright neutral posture. Front Bioeng Biotechnol 2022;10:751291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Rasmussen J, Damsgaard M, Voigt M. Muscle recruitment by the min/max criterion - a comparative numerical study. J Biomech 2001;34:409–415. [DOI] [PubMed] [Google Scholar]
- 323.Anderst W, Baillargeon E, Donaldson W, et al. Motion path of the instant center of rotation in the cervical spine during in vivo dynamic flexion-extension: implications for artificial disc design and evaluation of motion quality after arthrodesis. Spine (Phila Pa 1976) 2013;38:E594–E601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Vasavada AN, Li S, Delp SL. Influence of muscle morphometry and moment arms on the moment-generating capacity of human neck muscles. Spine (Phila Pa 1976) 1998;23:412–422. [DOI] [PubMed] [Google Scholar]
- 325.NBDL Human Volunteer Sled Tests Without Car Body 1522 to 1651. 2012. Available at: https://www-nrd.nhtsa.dot.gov/database/VSR/bio/QueryTest.aspx.
- 326.Dreischarf M, Rohlmann A, Zhu R, et al. Is it possible to estimate the compressive force in the lumbar spine from intradiscal pressure measurements? A finite element evaluation. Med Eng Phys 2013;35:1385–1390. [DOI] [PubMed] [Google Scholar]
- 327.Kambin P, Abda S, Kurpicki F. Intradiskal pressure and volume recording: evaluation of normal and abnormal cervical disks. Clin Orthop Relat Res 1980;146:144–147. [PubMed] [Google Scholar]
- 328.Hattori S. Cervical intradiscal pressure in movements and traction of the cervical spine. Z Orthop 1981;119:568–569. [Google Scholar]
- 329.Barrett JM, McKinnon C, Callaghan JP. Cervical spine joint loading with neck flexion. Ergonomics 2020;63:101–108. [DOI] [PubMed] [Google Scholar]
- 330.Assi A, Pomero V, Bonneau D, et al. Cervical muscles forces and spinal loads estimation in standing position: asymptomatic cases. Comput Methods Biomech Biomed Engin 2005;8(suppl 1):9–10. [Google Scholar]
- 331.Ibrahim E. The effects of neck posture and head load on the cervical spine and upper extremities [MSc thesis]. Biomechanics, McMaster University; 2015. [Google Scholar]
- 332.Van den Abbeele M, Li F, Pomero V, et al. A subject-specific biomechanical control model for the prediction of cervical spine muscle forces. Clin Biomech (Bristol, Avon) 2018;51:58–66. [DOI] [PubMed] [Google Scholar]
- 333.Kempter F, Bechler F, Fehr J. Calibration Approach for Muscle Activated Human Models in Pre-Crash Maneuvers with a Driver-in-the-Loop Simulator In: DHM2020 Vol 11. Stuttgart Germany: IOS Press; 2020:227–236. [Google Scholar]
- 334.Östh J, Brolin K, Ólafsdóttir JM, et al. Muscle activation strategies in human body models for the development of integrated safety. Paper presented at: Proceedings of the 24th International Techical Conference on the Enhanced Safety of Vehicles (ESV), Gothenburg, Sweden, 2015.
- 335.Madry H, Grässel S, Nöth U, et al. The future of basic science in orthopaedics and traumatology: Cassandra or Prometheus? Eur J Med Res 2021;26:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Mo F, Li J, Yang Z, et al. In vivo measurement of plantar tissue characteristics and its indication for foot modeling. Ann Biomed Eng 2019;47:2356–2371. [DOI] [PubMed] [Google Scholar]
- 337.Mo F, Li Y, Li J, et al. A three-dimensional finite element foot-ankle model and its personalisation methods analysis. Int J Mech Sci 2022;219:1–10. [Google Scholar]
- 338.Dreischarf M, Zander T, Shirazi-Adl A, et al. Comparison of eight published static finite element models of the intact lumbar spine: predictive power of models improves when combined together. J Biomech 2014;47:1757–1766. [DOI] [PubMed] [Google Scholar]
- 339.Nikkhoo M, Cheng CH, Wang JL, et al. Development and validation of a geometrically personalized finite element model of the lower ligamentous cervical spine for clinical applications(C3-7). Comput Biol Med 2019;109:22–32. [DOI] [PubMed] [Google Scholar]
- 340.Zheng HD, Sun YL, Kong DW, et al. Deep learning-based high-accuracy quantitation for lumbar intervertebral disc degeneration from MRI. Nat Commun 2022;13:841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Herrera A, Ibarz E, Cegonino J, et al. Applications of finite element simulation in orthopedic and trauma surgery. World J Orthop 2012;3:25–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Wu JC, Chen YC, Huang WC. Ossification of the posterior longitudinal ligament in cervical spine: prevalence, management, and prognosis. Neurospine 2018;15:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Kim TJ, Bae KW, Uhm WS, et al. Prevalence of ossification of the posterior longitudinal ligament of the cervical spine. Joint Bone Spine 2008;75:471–474. [DOI] [PubMed] [Google Scholar]
- 344.Kim BJ, Cho SM, Hur JW, et al. Kinematics after cervical laminoplasty: risk factors for cervical kyphotic deformity after laminoplasty. Spine J 2021;21:1822–1829. [DOI] [PubMed] [Google Scholar]
- 345.Osth J, Brolin K, Brase D. A human body model with active muscles for simulation of pretensioned restraints in autonomous braking interventions. Traffic Inj Prev 2015;16:304–313. [DOI] [PubMed] [Google Scholar]
- 346.Iwamoto M, Nakahira Y, Kimpara H. Development and validation of the total HUman model for safety (THUMS) toward further understanding of occupant injury mechanisms in precrash and during crash. Traffic Inj Prev 2015;16(suppl 1):S36–S48. [DOI] [PubMed] [Google Scholar]
- 347.Iwamoto M, Nakahira Y, Sugiyama T. Investigation of pre-impact bracing effects for injury outcome using an active human FE model with 3D geometry of muscles. Paper presented at: Proceedings of the 22nd international technical conference on the enhanced safety of vehicles (ESV)2011; Washington, DC, USA.
- 348.Olafsdottir JM, Östh J, Davidsson J, et al. Passenger kinematics and muscle responses in autonomous braking events with standard and reversible pre-tensioned restraints. Paper presented at: Ircobi conference 2013, 2013. [DOI] [PubMed]
- 349.Iwamoto M, Nakahira Y, Kato D. Finite element analysis for investigating the effects of muscle activation on head-neck injury risks of drivers rear-ended by a car after an autonomous emergency braking. Int J Automot Eng 2018;9:124–129. [Google Scholar]
- 350.Salin D, Arnoux P-J, Kayvantash K, et al. Implementation of reflex loops in a biomechanical finite element model. Comput Methods Biomech Biomed Engin 2016;19:1578–1582. [DOI] [PubMed] [Google Scholar]
- 351.Mo F, Li J, Dan M, et al. Implementation of controlling strategy in a biomechanical lower limb model with active muscles for coupling multibody dynamics and finite element analysis. J Biomech 2019;91:51–60. [DOI] [PubMed] [Google Scholar]
- 352.Anderson PSL, Rivera MD, Suarez AV. “Simple” biomechanical model for ants reveals how correlated evolution among body segments minimizes variation in center of mass as heads get larger. Integr Comp Biol 2020;60:1193–1207. [DOI] [PubMed] [Google Scholar]
- 353.Augat P, Hast MW, Schemitsch G, et al. Biomechanical models: key considerations in study design. OTA International 2021;4(2S):e099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Shen T-WD. Investigation of Whiplash Associated Disorders using Finite Element Neck Models with Active Musculature in Frontal, Rear and Lateral Impact, UWSpace, 2020.
- 355.Tierney GJ, Simms CK. The effects of tackle height on inertial loading of the head and neck in Rugby Union: A multibody model analysis. Brain Inj 2017;31:1925–1931. [DOI] [PubMed] [Google Scholar]
- 356.Corrales MA, Gierczycka D, Barker J, et al. Validation of a football helmet finite element model and quantification of impact energy distribution. Ann Biomed Eng 2020;48:121–132. [DOI] [PubMed] [Google Scholar]
- 357.Bustamante MC, Bruneau D, Barker JB, et al. Component-level finite element model and validation for a modern American Football Helmet. J Dynamic Behav Mater 2019;5:117–131. [Google Scholar]
- 358.Kuster D, Gibson A, Abboud R, et al. Mechanisms of cervical spine injury in rugby union: a systematic review of the literature. Br J Sports Med 2012;46:550–554. [DOI] [PubMed] [Google Scholar]
- 359.Levy Y, Bian K, Patterson L, et al. Head kinematics and injury metrics for laboratory hockey-relevant head impact experiments. Ann Biomed Eng 2021;49:2914–2923. [DOI] [PubMed] [Google Scholar]
- 360.Michio Clark J, Post A, Blaine Hoshizaki T, et al. Distribution of brain strain in the cerebrum for laboratory impacts to ice hockey goaltender masks. J Biomech Eng 2018;140:121007. [DOI] [PubMed] [Google Scholar]
- 361.de Grau S, Post A, Meehan A, et al. Protective capacity of ice hockey helmets at different levels of striking compliance. Sports Eng 2020;23:11. [Google Scholar]
- 362.Razaghi R, Biglari H. A comparative numerical study to compute ocular injury in boxing. Proc Inst Mech Eng P J Sport Eng Technol 2020;234:125–135. [Google Scholar]
- 363.Li H, Lu RJ, Wu P, et al. Numerical simulation and analysis of midfacial impacts and traumatic brain injuries. Ann Transl Med 2021;9:459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Cournoyer J, Hoshizaki TB. Head dynamic response and brain tissue deformation for boxing punches with and without loss of consciousness. Clin Biomech (Bristol, Avon) 2019;67:96–101. [DOI] [PubMed] [Google Scholar]
- 365.Patel DR, Yamasaki A, Brown K. Epidemiology of sports-related musculoskeletal injuries in young athletes in United States. Transl Pediatr 2017;6:160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Schneuer FJ, Bell JC, Adams SE, et al. The burden of hospitalized sports-related injuries in children: an Australian population-based study, 2005–2013. Injury Epidemiology 2018;5:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Fisher H, Gittoes MJ, Evans L, et al. An interdisciplinary examination of stress and injury occurrence in athletes. Front Sports Act Living 2020;2:595619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Prieto-González P, Martínez-Castillo JL, Fernández-Galván LM, et al. Epidemiology of sports-related injuries and associated risk factors in adolescent athletes: an injury surveillance. Int J Environ Res Public Health 2021;18:4857. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article.



