Abstract
Background
Prenatal screening and the promotion of folic acid intake could affect the incidence of neural tube defects (NTDs). We examined trends in the total NTD incidence, as detected in live births, stillbirths and therapeutic abortions, from 1986 to 1999 in Ontario.
Methods
To capture cases of NTDs we used data from the Canadian Congenital Anomalies Surveillance System and hospital data on therapeutic abortions. We calculated the total incidence of NTDs by combining the numbers of NTDs occurring in live births, stillbirths and therapeutic abortions.
Results
The total NTD incidence rate increased from 11.7 per 10 000 pregnancies in 1986 to 16.2 per 10 000 in 1995, and it subsequently decreased to 8.6 per 10 000 by 1999. The NTD birth rate (live births and stillbirths) decreased from 10.6 per 10 000 births in 1986 to 5.3 per 10 000 in 1999. The rate of therapeutic abortions with an NTD or hydrocephalus rose from 17.5 per 10 000 abortions in 1986 to 50.7 per 10 000 in 1995 and fell to 28.7 per 10 000 abortions in 1999.
Interpretation
The total NTD incidence rate increased from 1986 to 1995, probably because of increased prenatal screening and better detection of NTDs. The decline from 1995 to 1999 may have been due to increased folic acid intake among women at the time of conception.
Neural tube defects (NTDs) result in congenital malformations of the nervous system1 and may lead to spontaneous abortion, stillbirth, death in early infancy or a lifetime of disability.2 Studies of congenital anomalies in Alberta, Manitoba and Ontario showed a significant decline in NTD birth prevalence between 1979 and 1993.3 During that time, there was also an increased use of prenatal screening programs, which offer women and their families the option of terminating a pregnancy at high risk of having an NTD.4 Since a large proportion of NTD cases are detected prenatally through routine screening and may result in a therapeutic abortion,5,6,7,8 the NTD birth prevalence may be substantially reduced.7,8,9,10
Canadian,6,11 Australian,5 European9,12,13,14 and American7,15 studies have reported decreases in the birth prevalence of NTDs in their populations over the past decades, with most reporting either no change5,12,14 or a decline7,9,15 in total prevalence rates.
Surveillance systems that monitor only births affected by NTDs underestimate the overall incidence8,16 since they miss cases that are detected prenatally and terminated during pregnancy. Birth incidence rates may reflect differences in screening practices and diagnostic standards rather than the true incidence of NTD cases.
The Canadian Congenital Anomaly Surveillance System (CCASS) estimates birth defect incidence among live births and stillbirths, but it does not capture cases that are spontaneously or therapeutically aborted.3 Therefore we report the total incidence of NTDs in Ontario from 1986 to 1999 by combining data on live births and stillbirths with hospital data on therapeutic abortions.
Methods
The CCASS estimates the incidence of numerous congenital anomalies using hospital administration data from the Canadian Institute for Health Information (CIHI). CCASS methodologies are described elsewhere.16 The CCASS provided us with the number of NTD cases among live births and stillbirths occurring in Ontario hospitals from 1986 to 1999 as well as the total number of live births and stillbirths. Data on live births include data for infants admitted to hospital in the first year of life because of congenital anomalies, since not all anomalies are detected at birth. Health Canada, the administrator of the CCASS, applies an algorithm to remove duplicate records. We also analyzed the type of NTD, whether spina bifida (includes spina bifida with hydrocephalus), anencephaly or encephalocele.
Data on therapeutic abortions with an NTD or hydrocephalus occurring from 1986 to 1999 in Ontario were also based on CIHI hospital administration data, which we obtained through the Central East Health Information Partnership and the Ontario Ministry of Health and Long-Term Care. We defined the termination of pregnancies with NTDs or hydrocephalus as legally induced abortions performed in hospital (International Classification of Diseases, ninth revision [ICD-9] code 635) on an in-patient or day surgery basis in which a central nervous system malformation was identified in the fetus as anencephaly, hydrocephalus or spina bifida (ICD-9 code 655.0).17 Hydrocephalus may have been included in the ICD-9 code because it is more prevalent than encephalocele and is a common manifestation in anencephaly18 and spina bifida cases.19 Because we could not differentiate hydrocephalus from the NTDs in these data, we included hydrocephalus birth incidence rates in the analysis. The Ontario Ministry of Health and Long-Term Care also gave us the total number of therapeutic abortions performed in hospital. We did not include therapeutic abortions conducted in free-standing abortion clinics. We also made no attempt to capture data on spontaneous NTD abortions.
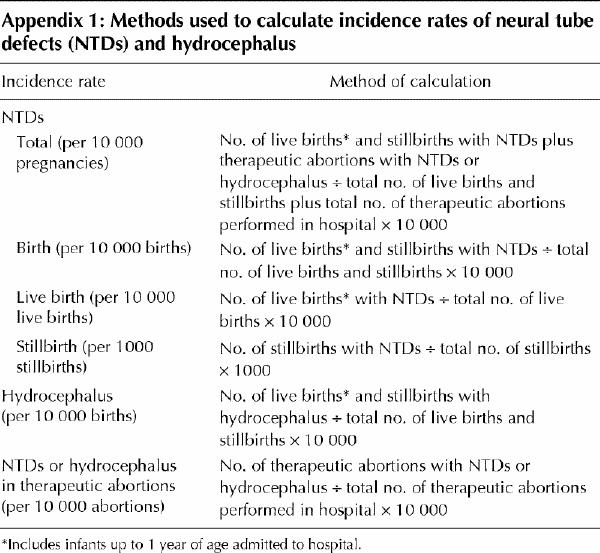
We computed the total NTD incidence rate by combining live births, stillbirths and therapeutic abortions in both numerator and denominator. The birth incidence rate included live births and stillbirths only. Appendix 1 summarizes how we calculated the rates.
We examined overall trends using a Poisson regression analysis for number of NTDs diagnosed per year (1986–1999), with year as a continuous, independent predictor variable.
Results
A total of 3207 NTDs occurred in Ontario from 1986 to 1999: 1503 detected in live births, 425 in stillbirths and 1279 in therapeutic abortions. The total NTD incidence rate increased by 38% from 1986 to 1995, from 11.7 to 16.2 per 10 000 pregnancies (p < 0.001); however, the rate dropped by 47% from 1995 to 1999, to 8.6 per 10 000 pregnancies (p < 0.001) (Fig. 1). The NTD birth incidence rate decreased by 50% from 1986 to 1999, from 10.6 to 5.3 per 10 000 births (p < 0.001) (Fig. 1); overall, 78% of the affected births were live births and 22% were stillbirths. There was no significant change in the hydrocephalus birth rate during the study period (Fig. 1).
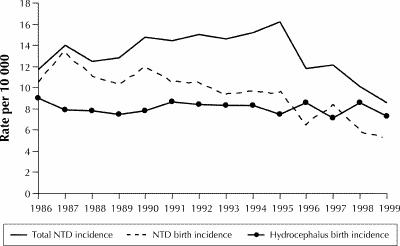
Fig. 1: Total incidence rates of neural tube defects (NDTs) and birth incidence rates of NTDs and hydrocephalus in Ontario, 1986–1999.
The rate of NTDs in live births declined by 50% during the study period, from 8.6 per 10 000 live births in 1986 to 4.3 per 10 000 live births in 1999 (p < 0.001) (Fig. 2). Most of the live births were cases of spina bifida (75%), the remainder being encephalocele (15%) and anencephaly (11%). The rate of spina bifida in live births decreased by 52% over time (p < 0.001); the rates of anencephaly and encephalocele decreased by 42% (p < 0.002) and 45% (p = 0.002) respectively.
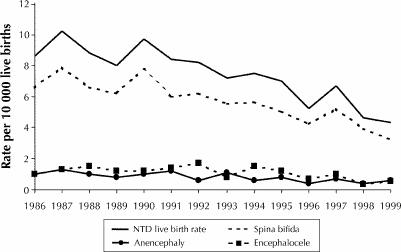
Fig. 2: Incidence rates of NTDs in live births, by type of NTD.
On average, 3.2% of all stillbirths were diagnosed with an NTD, as compared with 0.1% of all live births. The rate of stillbirths with an NTD dropped by 53%, from 33.6 per 1000 stillbirths in 1986 to 15.9 per 1000 in 1999 (p < 0.001) (Fig. 3). In contrast to live births, the most common NTD among stillbirths was anencephaly (57%); spina bifida accounted for 35% and encephalocele for 7% of affected stillbirths. Although stillbirth rates for anencephaly decreased significantly (by 60%, p < 0.001), spina bifida rates showed no significant change. Statistical tests for trend were not analyzed for encephalocele because of the small number of cases.
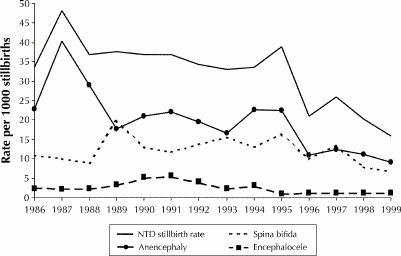
Fig. 3: Incidence rates of NTDs in stillbirths, by type of NTD.
From 1986 to 1995 the rate of therapeutic abortions in which an NTD or hydrocephalus was detected rose 190%, from 17.5 to 50.7 per 10 000 abortions (p < 0.001). By 1999 it had fallen by 43%, to 28.7 per 10 000 abortions (p < 0.001) (Fig. 4). In 1999 the distribution of total NTDs was 42% live births, 10% stillbirths and 47% therapeutic abortions (Fig. 5). This was a shift from 1986, when the distribution was 61%, 15% and 25% respectively.
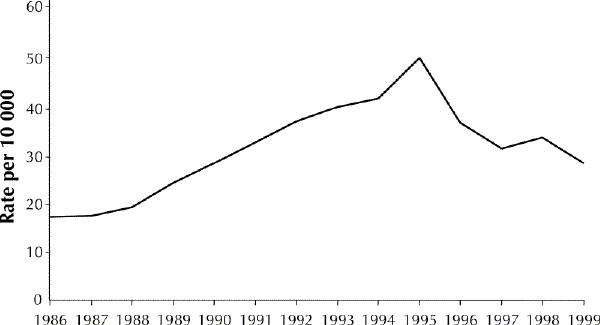
Fig. 4: Incidence rates of NTDs or hydrocephalus in therapeutic abortions.
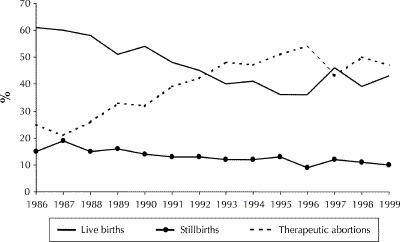
Fig. 5: Distribution of live births, stillbirths and therapeutic abortions with NTDs.
Interpretation
We found that NTD rates detected at birth decreased from 1986 to 1999, with most of the decrease occurring after 1995. The rate of therapeutic abortions with an NTD or hydrocephalus increased from 1986 to 1995 but decreased from 1995 to 1999. In 1986 the ratio of NTD-affected births to therapeutic abortions was 3:1, as compared with 1:1 in 1999.
The increase in the rate of therapeutic abortions with an NTD or hydrocephalus and the subsequent decrease after 1995 may be explained by both artifactual and real influences. Artifactual explanations relate to data quality. The data on therapeutic abortions were problematic because the ICD-9 code 655.0 grouped anencephaly, spina bifida and hydrocephalus together rather than the standard NTD classification of anencephaly, spina bifida and encephalocele. Because the ICD-9 code included hydrocephalus rather than encephalocele, we may have calculated inflated rates of NTD-affected therapeutic abortions. However, the birth incidence of hydrocephalus remained constant over the 14-year study period, which may indicate a similar trend for the incidence of therapeutic abortions affected by hydrocephalus.
We examined data on only therapeutic abortions performed in hospitals owing to the lack of data on those with NTD or hydrocephalus performed in free-standing abortion clinics. It is unlikely that clinics perform many NTD-affected therapeutic abortions since the detection of NTDs usually occurs between 16 and 20 weeks' gestation.
An important consideration for data quality is case ascertainment, particularly if detection or reporting has changed over time. The CCASS uses hospital separation data to identify anomalies and determines the number of individual cases by internally linking the records to remove duplicates. Personal identifiers are removed from the records, which necessitates a probabilistic melding process that links the individual records using variables such as sex, date of birth and postal code. The process depends on complete information. Since NTDs are serious anomalies, few cases would escape hospitalization; however, it may be possible that hospital data have become more complete in recent years, resulting in more accurate identification of duplicates. The completeness of therapeutic abortion data, also based on hospital records, is more difficult to assess. In-depth research through methods such as chart review could provide insight into the quality of these data.
There are 2 recent influences that may explain the trends in NTD incidence rates: prenatal screening and use of folic acid. Prenatal screening is likely the main reason for the decreased rates of live births with an NTD and the increased rates of therapeutic abortions with NTD or hydrocephalus before 1996. The decrease after 1995 is consistent with the release of recommendations for folic acid use before conception by women of child-bearing years and the provision of related preconception education.20,21,22 In the late 1990s initiatives to promote folic acid use expanded, including activities by boards of health23,24 and fortification of flour and pasta in Canada in January 1998.25 It has been suggested that a decrease of 30% to 40% in the incidence of NTDs could be expected even with relatively low levels of fortification.26
Assessments of folic acid intake or serum folate concentrations would strengthen conclusions from this study. Additional research is needed to explore the effectiveness of strategies to promote folic acid use such as preconception education, supplementation, and fortification of flour and pasta. Standardized reporting of NTDs, including cases in therapeutic abortions, is needed to ensure that rates are interpreted correctly.
β See related articles pages 241 and 255
Acknowledgments
We thank the Central East Health Information Partnership for funding and assisting us with this project. We also appreciate the assistance of the Maternal Serum Screening Program at North York General Hospital, the Ontario Ministry of Health and Long-Term Care and Health Canada.
Appendix 1.
Footnotes
This article has been peer reviewed.
Contributors: Ms. Gucciardi conducted the initial study as a practicum project for her MHSc in Community Health and Epidemiology; she conducted the literature review, collected and interpreted the data, and drafted the article. Ms. Pietrusiak supervised the practicum, contributed to the data collection and analysis, reviewed the methodology and contributed to the writing and revising of the article. Dr. Reynolds provided clinical input, reviewed the methodology, interpreted the data and edited the article. Mr. Rouleau provided data from the Canadian Congenital Anomalies Surveillance System, contributed to the data interpretation and reviewed the article.
Competing interests: None declared.
Correspondence to: Enza Gucciardi, University Health Network Women's Health Program, Mulock/Larkin Wing, 2nd floor, Rm. 2-010, 657 University Ave., Toronto ON M5G 2N2; fax 416 340-4185; enza.gucciardi@uhn.on.ca
References
- 1.Moore KL. The developing human: clinically oriented embryology. 3rd ed. Philadelphia: W.B. Saunders Company; 1982. p. 385-403.
- 2.Infant health: measuring up. A health surveillance update on Canadian children and youth. Ottawa: Health Canada; 1999. Cat no H42-2/82-1999E. [DOI] [PMC free article] [PubMed]
- 3.Johnson KC, Rouleau J. Temporal trends in Canadian birth defects birth prevalence. Can J Public Health 1997;88(3):169-76. [DOI] [PMC free article] [PubMed]
- 4.Canadian Perinatal Surveillance System: induced abortion [fact sheet]. Ottawa: Health Canada; 1998.
- 5.Chan A, Robertson EF, Haan EA, Keane RJ, Ranieri E, Carney A. Prevalence of neural tube defects in South Australia, 1966–91: effectiveness and impact of prenatal diagnosis. BMJ 1993;307:703-6. [DOI] [PMC free article] [PubMed]
- 6.DeWals P, Trochet C, Pinsonneault L. Prevalence of neural tube defects in the province of Quebec. Can J Public Health 1999;90:237-9. [DOI] [PMC free article] [PubMed]
- 7.Roberts HE, Moore CA, Cragan JD, Fernhoff PM, Khoury MJ. Impact of prenatal diagnosis on the birth prevalence of neural tube defects, Atlanta, 1990–1991. Pediatrics 1995;96(5):880-3. [PubMed]
- 8.Allen WP, Stevenson RE, Thompson SJ, Dean JH. The impact of prenatal diagnosis on NTD surveillance. Prenat Diagn 1996;16:531-5. [DOI] [PubMed]
- 9.Eurocat Working Group. Prevalence of neural tube defects in 20 regions of Europe and the impact of prenatal diagnosis, 1980–1986. J Epidemiol Community Health 1991;45:52-8. [DOI] [PMC free article] [PubMed]
- 10.Velie EM, Shaw GM. Impact of prenatal diagnosis and elective termination on prevalence and risk estimates of neural tube defects in California, 1989–1991. Am J Epidemiol 1996;144(5):473-9. [DOI] [PubMed]
- 11.Evans JA, Chodirker BN, Harman C, MacDonald K. The impact of maternal serum alphafetoprotein screening on the birth prevalence of neural tube defects in Manitoba:1979–1990 [abstract]. Am J Hum Genet 1992;51:A267.
- 12.Morris JK, Wald NJ. Quantifying the decline in the birth prevalence of neural tube defects in England and Wales. J Med Screen 1999;6(4):182-5. [DOI] [PubMed]
- 13.Alembik Y, Dott B, Roth MP, Stoll C. Prevalence of neural tube defects in northeastern France, 1979–1992: impact of prenatal diagnosis. Ann Genet 1995; 38(1):49-53. [PubMed]
- 14.Rankin J, Glinianaia S, Brown R, Renwick M. The changing prevalence of neural tube defects: a population-based study in the north of England, 1984–96. Paediatr Perinat Epidemiol 2000;14(2):104-10. [DOI] [PubMed]
- 15.Hendricks K, Simpson SJ, Russell DL. Neural tube defects along the Texas–Mexico border. Am J Epidemiol 1999;149:1119-27. [DOI] [PubMed]
- 16.Rouleau J, Arbuckle TE, Johnson, KC, Sherman GJ. Description and limitations of the Canadian Congenital Anomalies Surveillance System (CCASS). Chronic Dis Can 1995;16(1):37-42.
- 17.World Health Organization. International classification of diseases: 1975 revision. Geneva: The Organization; 1977. p. 356,367.
- 18.Sever LE, Strassburg MA. Epidemiologic aspects of neural tube defects. In: Mizejewski G, Porter IH, editors. Alpha-Fetoprotein and congenital disorders. Orlando (FA): Academic Press Inc; 1985. p. 243-62.
- 19.Forman R, Chou S, Koren G. The role of folic acid in preventing neural tube defects. Contemp Pediatr 1995;Aug:16-22.
- 20.MRC Vitamin Study Research Group. Prevention of neural tube defects: results of the Medical Research Council Vitamin Study. Lancet 1991;338:131-7. [PubMed]
- 21.Czeizel AE, Dudas I. Prevention of the first occurrence of neural tube defects by periconceptional vitamin supplementation. N Engl J Med 1992;327:32-5. [DOI] [PubMed]
- 22.Wilson RD, Van Allen MI. The use of folic acid for the prevention of neural tube defects [policy statement 19]. Ottawa: Society of Obstetricians and Gynaecologists of Canada; 1993.
- 23.Mandatory and health services guidelines. Toronto: Ontario Ministry of Health; 1997. p. 39-41.
- 24.Van Allen MI, Fraser FC, Dallaire L, Allanson J, McLeod DR, Andermann E, et al. Recommendations on the use of folic acid supplementation to prevent the recurrence of neural tube defects. CMAJ 1993;149(9):1239-43. [PMC free article] [PubMed]
- 25.Nutrition for a healthy pregnancy: national guidelines for the childbearing years. Ottawa: Health Canada; 1999. p. 28. Cat no H39-459/1999E.
- 26.Koren G. Folic acid and neural tube defects. Good news at last! Can Fam Physician 1999;45:2605-6. [PMC free article] [PubMed]


