Abstract
Background
Tai Chi (TC) is widely acknowledged for its positive impact on improving motor function in older adults. Nevertheless, limited research has directly compared the effects of different TC styles on older adults with functional impairments.
Objective
This study aimed to assess the impact of different TC styles on motor function in older adults with functional impairments.
Method
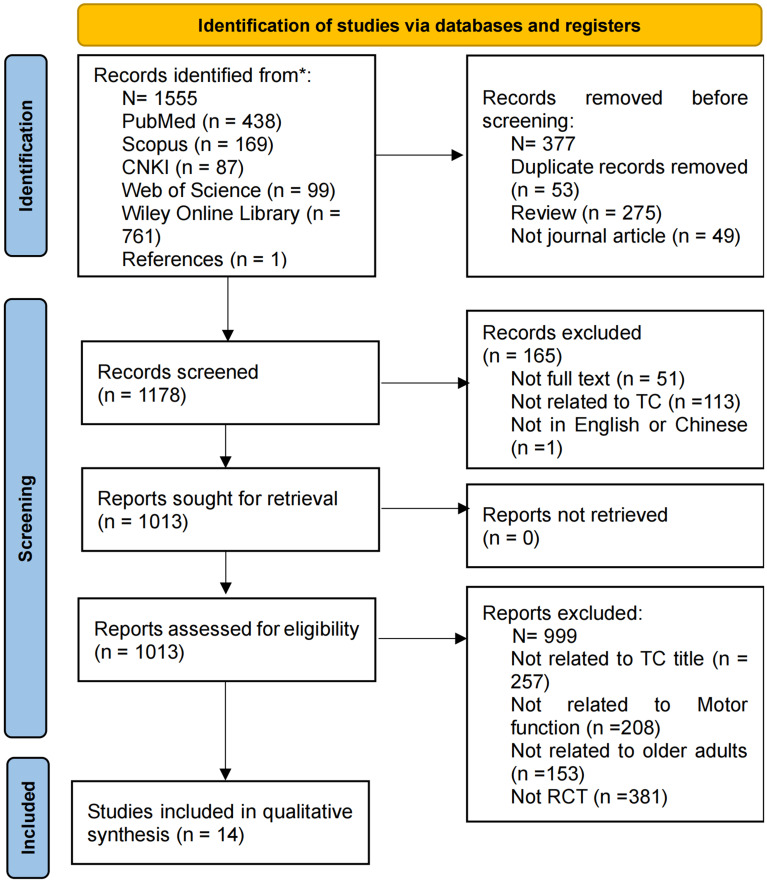
We searched five databases—PubMed, Scopus, Chinese National Knowledge Infrastructure (CNKI), Web of Science, and Wiley Online Library—including studies published up to September 2024. The selection of literature adhered to PRISMA guidelines, with quality assessment independently carried out by two researchers.
Results
Fourteen studies met the inclusion criteria for this review. The analysis revealed that TC interventions for functionally impaired older adults primarily employed Yang-style, Sun-style, Chen-style, and simplified-style TC. The populations studied included individuals with mild cognitive impairment (MCI), nonspecific low back pain (NS-LBP), preclinical disabilities, chronic diseases, poor balance, osteoarthritis (OA), Parkinson’s disease (PD), sarcopenia, and those at risk of falls. The findings indicated that motor function in functionally impaired older adults were closely linked to balance, gait, mobility, strength, and fall rates. Among the various TC styles, Yang-style was the most frequently utilised intervention.
Conclusion
This review examined four types of TC interventions and found strong evidence supporting the effectiveness of Yang-style TC in improving motor function in older adults with functional impairments. Additionally, five assessment methods—Single-Leg Stance (SL), Six-Minute Walk Test (6MWT), Timed Up and Go Test (TUGT), Chair Stand Test (CST), and Fall Efficacy Scale (FES)—were identified as suitable for evaluating this population. Based on the findings, it is recommended that individuals with functional impairments engage in Yang-style 24-movement TC, with an intervention duration of 12 weeks, practicing two to five times a week for 60 min each session.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40520-024-02894-5.
Keywords: Tai Chi, Motor function, Older adults, Balance, Gait
Introduction
As the global population ages, there is growing concern about enhancing the quality of life (QoL) for older adults, particularly those with functional impairments [1, 2]. Motor function, which enables the body to move and maintain posture, depends on the coordinated work of muscles and the nervous system [3]. The natural decline in biological systems such as reduced muscle strength and balance has a direct impact on motor function, which is essential for maintaining independence and overall well-being in older adults [4–6]. Motor dysfunction, however, is a common challenge among older adults, often seen as decreased mobility, a heightened risk of falls, and a reduced capacity to perform daily activities. These issues can further impact mental health and QoL [7, 8].
Tai Chi originated in China and is a branch of Chinese martial arts [9, 10]. Over time, it has evolved into various styles such as Chen, Yang, Wu/Hao, Wu, and Sun [11, 12], with Chen style being the oldest [12, 13]. TC is a moderate-intensity mind-body exercise that numerous studies have shown to improve physical performance in older adults, including balance, gait, strength, and mobility [14–17]. However, inconsistencies in findings have been reported across studies, attributed in part to variations in TC styles and forms used [18]. For instance, one study suggested that an 8-form Yang-style TC intervention did not improve gait abilities in Parkinson’s disease (PD) patients [19], whereas another study found positive effects from a 24-form Yang-style intervention [20, 21]. Differences in TC forms and intervention populations have led to inconsistencies in intervention results [22], making it challenging to identify the most suitable TC style for older adults, particularly those with varying functional impairments.
Numerous studies have examined the effects of TC on motor function in older adults, yet it remains unclear which TC style best supports those with functional impairments, such as MCI, PD, OA, NS-LBP, fall risk, preclinical disabilities, chronic diseases, and sarcopenia. Each of these conditions presents unique functional challenges and impacts key physical health indicators, including balance, gait, mobility, strength, and risk of falls. For instance, musculoskeletal conditions often lead to reduced balance and mobility, while cognitive and neurological impairments can significantly affect gait and overall functional performance [23, 24]. This review systematically investigates the effects of different TC interventions on these physical health indicators in older adults with functional impairments. By focusing on specific outcomes such as balance, gait, mobility, strength, and fall prevention, this study seeks to identify the most suitable TC interventions to enhance motor function in this population.
Materials and methods
Protocol and registration
This systematic review was registered in PROSPERO with registration number CRD 42,024,562,526. It was conducted in strict adherence to the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines [25].
Eligibility criteria
Table 1 presents the inclusion criteria established according to the PICOS principles (Population, Intervention, Comparison, Outcome, and Study Design):
Table 1.
Inclusion and exclusion criteria
| Items | Detail | |
|---|---|---|
| Inclusion criteria | Participants | No restriction on gender; participants must be aged ≥ 60 years with functional impairments, including MCI, PD, OA, NS-LBP, sarcopenia, disabilities, or at high risk of falls. |
| Intervention | Tai Chi intervention (including Yang, Chen, Sun, and Simplified styles) | |
| Comparison | Control group, no exercise or exercise group | |
| Outcome | Balance, gait, mobility, strength, falls | |
| Study designs | RCT | |
| Exclusion Criteria | Participants | Healthy older adults |
| Intervention | Tai Chi intervention period of less than 6 weeks | |
| Outcome | Studies that do not primarily focus on outcomes related to motor function, such as those that concentrate solely on mental health | |
| Study designs | Non-RCT designs (observational studies, case reports, or cohort studies) |
Table 1 outlines the inclusion and exclusion criteria. The criteria for this systematic review were established based on the PICOS (Population, Intervention, Comparison, Outcomes, and Study Design) principles. (1) Participants included older adults aged 60 years or older, particularly those with functional impairments related to motor function, such as MCI, PD, OA, NS-LBP, sarcopenia, disabilities affecting movement, and those at high risk of falls. (2) The intervention group must have undergone TC training, incorporating various styles (e.g., Yang, Chen, Sun, simplified), aimed at improving motor function, such as balance, gait, strength, mobility, and fall risk. (3) The control group could have received any alternative intervention (e.g., stretching exercises or usual care) or no intervention. (4) Only randomised controlled trials (RCTs) reporting outcomes related to motor function were included. (5) Studies published in either Chinese or English were considered.
Exclusion criteria included: (1) studies involving healthy older adults. (2) not focusing on exercise outcomes. (3) non-RCT designs (e.g., observational studies, case reports, or theoretical studies). (4) studies published in languages other than Chinese or English. (5) Tai Chi styles and forms (Neither of them mentioned).
Literature search
This systematic review conducted searches across five databases: PubMed, Scopus, CNKI, Web of Science, and Wiley Online Library. The literature search encompassed articles from inception to September 2024. PubMed (MeSH) terms and the following keywords were used in the search: “Tai Ji” OR “Tai-ji” OR “Tai Chi” OR “Chi Tai” OR “Tai Ji Quan” OR “Ji Quan Tai” OR “Quan Tai Ji” OR “Taiji” OR “Taijiquan” OR “T’ai Chi” OR “Tai Chi Chuan” AND “motor” “movement” OR “motion” OR “mobility” OR “function” OR “performance” AND “old people” OR “elderly” OR “senior*” OR “old adult*” OR “aged” OR “older people” OR “older adults” OR “geriatric.” Some keywords are derived from published reviews. Please refer to the supplementary materials for the specific search strategy of each database.
Study selection
All included literature was imported into EndNote reference management software to remove duplicate records. Subsequently, two researchers independently assessed each article’s titles, abstracts, and keywords to determine eligibility based on the inclusion criteria. For articles that passed this initial screening, full-text assessments were performed. In cases of discrepancies between the two researchers, a third researcher was consulted to achieve consensus.
Data extraction and quality assessment
Data extraction included: (1) author and publication year; (2) sample size, gender, and age; (3) health status; (4) intervention type, method, frequency, duration, and number of weeks; (5) research outcomes. The PEDro scale was utilised to assess the quality of included articles. This reliable methodological quality assessment tool [26] comprises 11 items designed to evaluate aspects such as randomisation, blinding, group comparability, and statistical analysis [27]. Each item is scored as either “yes” (1) or “no” (0). Scores range from 0 to 10, with higher scores typically indicating higher quality [28]: 6–10 points suggest high quality, 4–5 points indicate moderate quality, and ≤ 3 points indicate poor quality. The assessment using the PEDro scale was independently conducted by two researchers. In cases of disagreement, a third researcher was consulted to reach a consensus [29]. Please refer to Table 2.
Table 2.
Summary of methodological quality assessment scores
| References | Eligibility criteria | Random allocation | Concealed allocation | Group similar at baseline | Blind subject | Blind therapist | Blind assessor | Follow-up | Intention-to-treat analysis | Between-group comparisons | Point measure and variability | PEDro score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Birimoglu Okuyan and Deveci [30] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Yan, Yang [31] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Chewning, Hallisy [32] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Day, Hill [33] | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 6 |
| Ni, Mooney [34] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Lifeng, Jun [35] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Zhang, Ishikawa-Takata [36] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Li, Harmer [37] | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Liang [38] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Taylor, Hale [39] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Gao, Leung [40] | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Liao, Liu [41] | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 8 |
| Zhu, Peng [42] | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 5 |
| Hwang, Chen [43] | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 7 |
| Total | 14 | 14 | 2 | 14 | 3 | 1 | 3 | 6 | 14 | 14 | 14 |
Results
Study selection and characteristics
Refer to Fig. 1 for the study selection process. A total of 1555 articles were initially retrieved from electronic databases: PubMed (438), Scopus (169), CNKI (87), Web of Science (99), Wiley Online Library (761), and references (1). To streamline the selection process, we used literature management software to automatically remove duplicate entries. Two reviewers (Fan and Kim) then independently screened the articles to retain only those relevant and of high quality for inclusion in this review. Following this, 257 articles were excluded based on title alone, while articles unrelated to motor function (208 articles), not focused on older adults (153 articles), and those not classified as RCTs (381 articles) were further excluded. This process resulted in a final selection of 14 articles for detailed analysis [30–39, 40–43].
Fig. 1.
Prisma study selection process
Study quality assessment
Two researchers independently assessed the 14 articles using the PEDro scale. The assessment results were as follows: Random allocation (n = 14), Group similar at baseline (n = 14), Between-group comparisons (n = 14), Intention-to-treat analysis (n = 14), Point measure and variability (n = 14), Blind assessor (n = 3), Blind subject (n = 3), Blind therapist (n = 1), Follow-up (n = 6), and Concealed allocation (n = 2). According to the PEDro scale, the quality of the articles included in this study was rated as high (n = 8) or moderate (n = 6), with scores ranging from 5 to 8. This indicates a generally high methodological quality among the selected articles, supporting the reliability of this review findings. For detailed results and further information on quality assessment, please refer to Table 2.
Characteristics of included studies
The characteristics of the population included in this study are shown in Table 3. A total of 14 studies were included, focusing on the motor function of older adults. The specific characteristics are as follows:
Table 3.
Sample features, main outcomes, and participants’ characteristics
| References | Participants (N/G/A) |
Sample features | Intervention | TC Style | TC Form | Comparison | Outcomes |
|---|---|---|---|---|---|---|---|
| Birimoglu Okuyan and Deveci [30] |
N = 20, G = M/F Age = 74.21 ± 6.93 |
MCI |
EG: TC CG: Untrained |
Yang style | Not mentioned |
EG: 12wk/2/35–40 min CG: not applicable |
Balance↑ (TAT), Gait ↑ (TAT), Falls behavioral ↓ (FaB) |
| Taylor, Hale [39] |
N = 684, G = M/F Age ≈ 74.5 |
Risk of falling |
EG1: TC EG2: TC CG: LLE |
Sun style | 10-form |
EG1: 20wk/1/1hour EG2: 20wk/2/1hour CG: 20wk/1/1hour+ |
Balance↑ (ST), strength ↑ (CST), Mobility↔ (TUGT) |
| Yan, Yang [31] |
N = 20, G = F Age > 65 |
NS-LBP |
EG: TC CG: No exercise |
Chen style | 18-form |
EG: 6wk/3/1 hour CG: No exercise |
Balance↑ (dynamic), Gait↑ (stride width, gait velocity, stride length) |
| Chewning, Hallisy [32] |
N = 242, G = M/F Age ≥ 65 |
History of falling |
EG: TC CG: not mentioned |
Yang style | Not mentioned |
EG: EG:6-wk/2/90 min CG: no exercise intervention |
Balance↑ (SL), Gait↑ (TUGT), Mobility↑ (TUGT), Strength↑ (CST) |
| Day, Hill [33] |
N = 503, G = M/F Age = 70.8 ± 6.3 |
Preclinically disabled |
EG: TC CG: flexibility and stretching |
Sun style | 46-form |
EG: 24wk/2/60min CG: 24wk/2/60min |
Balance ↔ (SL), Mobility ↔ (TUGT), Strength ↔ (ST), Gait ↔ (DW) |
| Ni, Mooney [34] |
N = 39, G = M/F Age = 74.15 ± 6.99 |
History of falling |
EG1: TC EG2: Balance training CG: Yoga |
Chen style | 18-form |
EG: 12wk/2/60min EG: 12wk/2/60min CG: 12wk/2/60min |
Balance↑ (SL), Gait ↑ (8UG, Walking speed) |
| Lifeng, Jun [35] |
N = 60, G = M/F Age = 65.35 ± 7.76 |
Chronic disease |
EG: TC CG: Lower limb bike |
Not mentioned | 42-form |
EG:12wk/5/30–35 min CG: 12wk/5/30–35 min |
Gait↑ (6MWT), Balance↑ (SPPB), Strength↑ (CST) |
| Zhang, Ishikawa-Takata [36] |
N = 49, G = M/F Age ≥ 60 |
Poor balance |
EG: TC CG: No intervention |
Yang style | 24-form |
EG: 8wk/7/60min CG: No intervention |
Balance↑(SL), Gait↑ (10 MW), FOF↓ (FES score) |
| Li, Harmer [37] |
N = 670, G = M/F Age = 77.5 ± 5.6 |
History of falling |
EG1: TC EG2: Multimodal exercise CG: Stretching exercise |
Not mentioned | 8-form |
EG1: 24wk/2/60min+ EG2: 24wk/2/60min CG: 24wk/2/60min |
Fall rate↓ |
| Liang [38] |
N = 91, G = M/F Age = 60–70 |
OA |
EG1: TC EG2: Resistance training CG: No intervention |
Yang style | 24-form |
EG1: 16wk/4/60min+ EG2: 16wk/4/60min CG: 24wk/4/60min |
Gait↑(6WMT), Mobility↑ (TUGT) |
| Gao, Leung [40] |
N = 76, G = M/F Age = 69.54 ± 7.32 |
PD |
EG: TC CG: No intervention |
Yang style | 24-form |
EG: 12wk/3/60min CG: 12wk/3/60min |
Balance ↑ (BBS), Mobility↑ (TUGT), Fall rate↓ |
| Liao, Liu [41] |
N = 20, G = M/F Age ≥ 65 |
MCI |
EG: tDCS + TC CG: sham + TC |
Yang style | 24-form |
EG: 12wk/3/40min CG: 12wk/3/40min |
Gait performance↑ |
| Zhu, Peng [42] |
N = 79, G = M Age ≥ 85 |
Sarcopenic |
EG1: TC + Health Education EG2: WBV + Health Education CG: Health education |
Simplify | 8-form |
EG1: 8wk/5/40min EG2: 8wk/5/40min CG: 8wk/1/month/40min |
Balance↑(SL), Gait↑ (6WMT), mobility↑ (TUGT), strength↑ (FTSST, handgrip), |
| Hwang, Chen [43] |
N = 456, G = M/F Age = ≥ 60 |
History of falling |
EG: TC CG: LET |
Yang style | 18-form |
EG: 24wk/1/60min CG: 24wk/1/60min |
Balance↑ (TAT), Strength↑ (Handgrip), Fall rate↑ (FES) |
Note N: number of samples; G: gender; A: age; M: male; F: female; EG: experimental group; CG: control group; WK: week, ↓significantly decreased; significantly increased ↑; no significant change ↔; MCI: mild cognitive impairment; LLE: low-level exercise; FES: falls efficacy scale; OA: chronic symptomatic hip or knee osteoarthritis PD: parkinson’s disease; tDCS: transcranial direct current stimulation; WBV: whole-body vibration; M: month; FOF: fear of fall; NS-LBP: non-specific low back pain; TAT: Tinetti scale; FaB: falls behavioral scale; ST: step test; CST: chair stand test; TUGT: time up and go test; SL: single leg balance; DW: Distance walked; 8UG: 8-foot up-and-go test; 6MWT: 6 min walk test; SPPB: short physical performance battery; 10WM: 10 m walking; FES: Falls Efficacy Scale; FTSST: five-times-sit-to-stand test
Total sample size: 3009 participants.
Gender: 12 studies included both males and females [30, 32–38, 40, 41, 43, 39]; one study focused on women [31]; one study described only males [42].
Age: All participants were over 60 years old. 12 studies included participants aged 60–75 years [30–36, 38, 40, 41, 43, 39]; two studies included participants over 75 years [37, 42].
Description of participants health conditions: Two studies involved MCI populations [30, 41]; five studies addressed the risk of falls [32, 34, 37, 43, 39]; and other health conditions were represented as follows: NS-LBP [31], disability [33], chronic disease [35], poor balance [36], OA [38], PD [40], and sarcopenic [42].
Intervention characteristics
Intervention characteristics included intervention frequency, duration, and period. All 14 studies employed TC interventions, with two studies incorporating combined interventions [41, 42]. Nine studies compared two groups [30–33, 35, 36, 40, 41, 43], while five studies conducted three-group comparisons, including two experimental groups and one control group [34, 37, 38, 42, 39].
The intervention cycles varied as follows:
Outcomes
This section includes the research results of 14 articles, all of which used TC as the intervention method and reported the effects on motor function in older adults with functional impairments.
Effects of different Tai Chi interventions on balance
eleven studies examined balance outcomes [30–36, 39, 40, 42–43]. Regarding TC intervention styles used for balance, there was variation: five studies used Yang-style TC [30, 32, 36, 40, 43], two studies used Sun-style TC [33, 39], two studies used Chen TC [31, 34], one study used simplified TC [42], and one studies did not specify the TC style [35]. Notably, one study utilising Sun-style TC did not show improvement in balance outcomes [33].
Regarding the populations studied for balance:
Five studies assessed balance in individuals at risk of falls [32, 34, 37, 43, 39].
There was one study assessing balance in individuals with MCI, NS-LBP, chronic disease, poor balance, PD, and sarcopenia.
One study assessed balance in individuals with preclinically disabled, showing no significant improvement [33].
The following methods were used to assess balance: six studies employed the single-leg balance stand test (SL), a common measure of balance. Most studies reported improved SL test scores following TC intervention, with only one study showing no improvement. Additionally, two studies used the Tinetti Assessment Tool (TAT) scale, both of which indicated enhanced balance. Two other articles applied the Short Physical Performance Battery (SPPB) and the Berg Balance Scale (BBS), each showing improvement in balance scores. In another study focusing on dynamic balance, the specific test method was not specified. However, most studies did not clearly distinguish whether these assessment methods measured dynamic or static balance.
Effects of different Tai Chi interventions on gait
Gait function was evaluated in ten studies [30–36, 38, 41, 42]. The interventions included various styles of TC: five studies used the Yang style [30, 32, 36, 38, 41], one study used the Sun style [33], two studies used the Chen style [31, 34], one study used the Simplified style [42], and one study did not specify the TC style [35].
Specifically, gait function was assessed in:
Two studies involving individuals at risk of falls [32, 34].
One study evaluated gait in patients with chronic disease [35].
One study assessed gait function in individuals with Preclinically disabled, showing no significant improvement [33].
Gait outcomes were measured using the following methods: the 6-minute walk test (6MWT), 10-metre walk test (10MWT), 8-foot up-and-go test (8UG), Timed Up and Go test (TUGT), TAT, and Distance Walked (DW). The 6MWT, used in three studies, was the most common method for assessing gait [35, 38, 42], as it typically evaluates gait speed and provides insight into an individual walking stability [44]. The remaining tests were each used in only one study, with most indicating improvement. However, only one DW test did not show a positive effect on gait ability [33]. Additionally, only one study comprehensively reported gait indicators, including stride width, gait velocity, and stride length [31].
Effects of different Tai Chi interventions on mobility
Six studies reported on mobility [32, 33, 38, 40, 42, 39]. The interventions included two studies using Sun-style TC [33, 39], three studies using Yang-style TC [32, 38, 40], and one study using Simplified-style TC [42].
Mobility function was mainly reported in:
Two studies involving individuals at risk of falls [32, 39].
One study involving individuals with preclinically disabled, showing no significant improvement [33].
There was one study each involving individuals with OA, PD, and sarcopenia.
This study did not find reports on mobility for individuals with MCI, NS-LBP, chronic disease, or poor balance. It is worth noting that TUGT is a widely used tool to measure activity.
Effects of different Tai Chi interventions on strength
Six studies reported on strength function. These included two studies on Sun style TC [33, 39], two studies on Yang style TC [32, 43], one study without specifying the TC style [35], and one study on Simplified style TC [42]. Additionally, this review identified three studies involving individuals at risk of falls [32, 43, 39], one study each on chronic disease and sarcopenia, and one study on individuals with disabilities, though the results were not positive [33].
Four studies focused exclusively on measuring lower body muscle strength in older adults. Of these, three used the Chair Stand Test (CST) [32, 35, 39], and one applied the Step Test (ST) [33]. Two studies examined upper limb strength [42, 43]. Most studies focused on either upper or lower limb strength, with only one study conducting a comprehensive assessment of both [42]. Notably, grip strength was the primary measure for upper limb strength, while the CST was the commonly used method for assessing lower limb strength.
Effects of different Tai Chi interventions on falls
Five studies are related to falls [30, 36, 37, 40, 43]. Among them, four studies focused on Yang style TC [30, 32, 36, 43], and two studies did not specify the TC style [37]. The populations studied include individuals with MCI [30], individuals with poor balance [36], individuals with a history of falls [37], and individuals with PD [40].
The Falls Efficacy Scale (FES) is a commonly used tool for measuring fall risk [36, 43], and two studies included in this review employed this measurement. Another study utilised the Falls Behavior Scale (FaB) to assess falls in a population with mild cognitive impairment (MCI) [30]. Additionally, two studies reported instances of falls without specifying the methods used [37, 40].
Discussion
This study aimed to examine the effects of various TC interventions on motor function in older adults with functional impairments. Our comparison of different intervention groups revealed that the distinct TC styles had varied effects on motor function, including balance, gait, mobility, strength, and fall prevention. Unlike other reviews, this study not only evaluated the overall benefits of TC but also compared the specific effects of different styles (Yang, Sun, Chen, and simplified forms) across diverse populations.
Fourteen articles employed various styles of TC interventions, including Yang, Sun, Chen, and simplified styles. These interventions encompassed six distinct TC movement forms: 8-form, 10-form, 18-form, 24-form, 42-form, and 46-form. TC has demonstrated positive effects on many outcome measures of motor function, particularly in improving balance, gait, mobility, and strength in older adults [45]. However, differences exist among the various TC styles.
Yang style TC was the most frequently used, appearing in a total of seven studies [30, 32, 36, 38, 40, 41, 43]. Specifically, four studies focused on the 24-movement form of Yang style TC [36, 38, 40, 41], while one study examined the 18-movement form Hwang, Chen [43]. Additionally, two studies featured the Chen style with its 18 movements Yan, Yang [31, 34], while the Sun style was represented by two studies using the 10-movement and 46-movement forms [34, 39], respectively. The simplified style included one study 8-movement forms [42]. Four studies did not specify the TC style or form used. Consequently, this review suggests that Yang-style 24-movement TC positively affects the motor function of individuals with PD, MCI, OA, and poor balance. This finding aligns with previous research indicating that Yang-style 24-movement TC can enhance physical function and significantly reduce fall rates in older adults who have experienced a stroke [46].
In this study, we investigated the effects of different styles of TC on motor function in older adults with functional impairments. Variations among TC styles can lead to differences in movement patterns, resulting in diverse exercise outcomes [47]. Four primary TC styles were included in this research. Yang-style TC, characterised by slow and smooth movements, has been shown to enhance balance and coordination, which aligns with our findings [48]. Specifically, studies indicate that Yang-style TC can improve balance in individuals with a history of falls, PD, OA, poor balance, and MCI.
Sun-style TC is recognised for its light movements, which demand agility and flexibility from practitioners [49]. Our results demonstrated that Sun-style TC can enhance balance and strength in older adults with a history of falls; however, another study involving individuals with preclinical disabilities did not report significant improvements in motor function. This discrepancy may arise from the complex movements inherent in Sun-style TC, including jumping and spinning, which require a higher level of balance and strength [50].
Chen-style TC, the oldest form, features more intricate and intense movements compared to Yang and Sun styles [51, 52]. It emphasises low postures, body coordination, and flexibility. Our study found that Chen-style TC can improve balance and gait measures in individuals with a history of falls and NS-LBP. Additionally, we examined simplified TC, which has been adapted to accommodate practitioners’ physical conditions. The results indicated that simplified TC can also enhance balance, flexibility, and strength in individuals with sarcopenia.
The characteristics of the participants in the included studies played a pivotal role in influencing the outcomes. This review focused on older adults with different levels of functional impairment, including PD, OA, MCI, preclinical disability, chronic illness, sarcopenia, and fall-related older adults. They may respond differently to TC interventions based on their baseline functional capacity, severity of impairment, and overall health. For instance, studies involving individuals with milder functional impairment generally reported greater improvements in balance and gait. In contrast, one study of Sun-style 46-posture TC in preclinically disabled people did not observe improvements in outcome measures. In general, the quality and intensity of TC practice also affect the results; higher quality, more intensive programs may lead to better results.
In terms of balance function, Yang style TC, especially the 24-posture TC, was the most effective. This finding is consistent with the results of [53], who also pointed out that Yang style TC significantly improved the balance ability of older adults. Balance is influenced by several key factors, including strength, proprioception, flexibility, and coordination [54]. Yang-style 24-posture Tai Chi incorporates slow movements and encourages a low center of gravity in the lower limbs during practice [55]. These elements contribute to enhancing the practitioner’s muscle strength and stability when standing on one leg. Given these considerations, the results of this study support the use of Yang-style 24-posture Tai Chi as the primary intervention for improving balance. In addition, a 12-week, 2–7 sessions, 35–60 min each time intervention is recommended.
In terms of gait improvement, Yang-style TC consistently outperformed other styles, aligning with findings by [56], who reported similar benefits. Meanwhile, both Chen-style and simplified TC demonstrated significant improvements in gait. Chen-style TC combines slow and fast movements to enhance muscle strength, power, and endurance [57]. It includes explosive movements, known as “fa jin,” which engage fast-twitch muscle fibres, promoting better muscle activation and coordination [58]. This dynamic characteristic of Chen-style TC aids practitioners in better controlling their gait mechanics. In contrast, Sun-style TC did not yield consistent improvements in gait, underscoring the importance of selecting a specific TC style to effectively address gait issues. This review still recommends an intervention duration of 12 weeks, with a frequency of 2–3 sessions per week, each lasting 35–60 min.
Our review also identified Yang-style TC as the most effective for enhancing mobility, while a simplified eight-movement form of TC also demonstrated positive effects. The Timed Up and Go Test (TUGT) is the most commonly used method to assess mobility; it involves a series of tasks that measure gait performance, balance, and overall mobility [59]. This review found that Yang-style TC can significantly improve mobility in individuals with a history of falls, OA, and PD. Furthermore, the simplified eight-movement TC proved beneficial for mobility in the sarcopenic population. Based on these findings, we recommend that older adults with a history of falls engage in Yang-style 24-movement TC to enhance their mobility. In contrast, Sun-style TC did not yield significant improvements in mobility.
Strength can serve as a key indicator of health status. Generally, reduced strength is linked to various negative outcomes, such as falls, disability, and even mortality [60, 61]. The findings from this study indicate that both Yang-style and simplified TC positively impact strength indicators, while Sun-style Tai Chi has beneficial effects specifically for older adults with a history of falls. However, it appears to have no effect on those who are preclinically disabled.
Practising TC engages all the muscles of the body, and as training intensity increases, muscle activation is enhanced throughout [62]. It is important to note that the Chen-style TC intervention did not include strength indicators, indicating that further research is needed to confirm its effects on strength in older adults with functional disabilities. Based on the results of this study, we continue to recommend Yang-style TC as an effective means of improving strength indicators, particularly for older adults with a history of falls.
Fall-related issues are a prevalent concern among older adults. Four studies have shown that Yang-style TC can effectively reduce the incidence of falls in individuals with various functional disabilities, including MCI, poor balance, PD, and a history of falls. Practising TC involves focused, deliberate movements that enhance proprioception [63]. Improved proprioception allows individuals to quickly adjust their posture and respond effectively to sudden changes, which are essential skills for preventing falls [64]. To effectively reduce fall rates, this study recommends an intervention duration of eight to 24 weeks, with sessions lasting 35 to 60 min each.
Study limitations
Several limitations should be acknowledged in this review.
First, while this study included various TC intervention methods, some styles were underrepresented. Greater attention should be given to these less frequently studied TC types in future research.
Additionally, the sample sizes for certain populations with functional impairments were small. For instance, studies involving individuals with nonspecific low back pain, preclinical disabilities, or chronic diseases were limited. Future research should aim to encompass these groups more comprehensively to enhance the generalizability of the findings.
Conclusion
This systematic review investigates the effects of Yang-style, Chen-style, Sun-style, and simplified-style TC on motor function in older adults with functional impairments. The results demonstrate that Yang-style TC, particularly the 24-movement form, significantly enhances balance, gait, mobility, and strength in individuals with MCI, a history of falls, poor balance, OA, and PD. Additionally, Chen-style TC (18 movements) is effective in improving balance and gait for those with NS-LBP and a history of falls. In contrast, Sun-style TC did not produce significant improvements in motor function among individuals with preclinical disabilities. Moreover, there is a notable scarcity of research on simplified-style TC, indicating a need for further exploration in this area. The review utilised various assessment tools, including the SL for balance, the 6MWT for gait, TUGT for mobility, CST for strength, and the FES. Finally, this study suggests that a TC intervention duration of 12 weeks, performed two to five times per week, is recommended to achieve optimal outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Conceptualisation: XF. and KG.; methodology: XF; writing—original draft preparation: XF.; writing—review and editing: XF, KG, CY CH and KL.; Tables and Figures: XF, KG XR and CY.; supervision, KL, ZY and CY. All authors have read and agreed to the published version of the manuscript.
Funding
This work was not supported by external funding.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Human and animal rights
Not applicable.
Informed consent
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Evans CJ et al (2019) Service delivery models to maximize quality of life for older people at the end of life: a rapid review. Milbank Q 97(1):113–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wettstein M et al (2019) Pain Intensity, disability, and quality of life in patients with chronic low back Pain: does Age Matter? Pain Med 20(3):464–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Méndez-Martínez M, Rodríguez-Grande EI (2023) Effects of therapeutic exercise on the motor function of adults with Down syndrome: a systematic review and meta-analysis. Sci Rep 13(1):21962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.St-Onge MP, Gallagher D (2010) Body composition changes with aging: the cause or the result of alterations in metabolic rate and macronutrient oxidation? Nutrition 26(2):152–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naczk M, Marszalek S, Naczk A (2020) Inertial Training improves strength, Balance, and Gait Speed in Elderly nursing home residents. Clin Interv Aging 15:177–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seidler RD et al (2010) Motor control and aging: links to age-related brain structural, functional, and biochemical effects. Neurosci Biobehavioral Reviews 34(5):721–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baeza AC, Aparicio García- VA, Molina, Fernández MD (2009) Efectos Del envejecimiento en las capacidades físicas: implicaciones en las recomendaciones de ejercicio físico en personas mayores. / effects of aging on physical fitness: implications in the recommendations of physical activity for older adults. RICYDE Revista Int De Ciencias Del Deporte 5(17):1–18
- 8.Drenth H et al (2016) The contribution of Advanced Glycation End product (AGE) accumulation to the decline in motor function. Eur Rev Aging Phys Act 13:3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang G (2010) Invented tradition and translated practices: the career of Tai Chi in China and the West. Loughborough University
- 10.Hui J et al (2022) Effects of Tai Chi on health status in adults with chronic heart failure: a systematic review and meta-analysis. Front Cardiovasc Med 9:953657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang G-Y et al (2015) Evidence base of clinical studies on Tai Chi: a bibliometric analysis. PLoS ONE 10(3):e0120655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang GY et al (2021) Tai Chi for health and well-being: a bibliometric analysis of published clinical studies between 2010 and 2020. Complement Ther Med, 60 [DOI] [PubMed]
- 13.Liu HH, Nichols C, Zhang H (2023) Understanding Yin-Yang philosophic concept behind Tai Chi practice. Holist Nurs Pract 37(5):E75–E82 [DOI] [PubMed] [Google Scholar]
- 14.Hallisy KM (2018) Tai Chi beyond Balance and fall Prevention: health benefits and its potential role in combatting social isolation in the Aging Population. Curr Geriatr Rep 7(1):37–48 [Google Scholar]
- 15.Lan C et al (2001) Heart rate responses and oxygen consumption during Tai Chi Chuan practice. Am J Chin Med 29(3–4):403–410 [DOI] [PubMed] [Google Scholar]
- 16.Lan C et al (2013) Tai Chi Chuan exercise for patients with cardiovascular disease. Evid Based Complement Alternat Med 2013:p983208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang X et al (2023) Mitigating effects and mechanisms of Tai Chi on mild cognitive impairment in the elderly. Front Aging Neurosci, 14 [DOI] [PMC free article] [PubMed]
- 18.Amano S et al (2013) The effect of Tai Chi exercise on gait initiation and gait performance inpersons with Parkinson’s disease. Parkinsonism Relat Disorders 19(11):955–960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amano S et al (2013) The effect of Tai Chi exercise on gait initiation and gait performance in persons with Parkinson’s disease. Parkinsonism Relat Disord 19(11):955–960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li F et al (2005) Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol Biol Sci Med Sci 60(2):187–194 [DOI] [PubMed] [Google Scholar]
- 21.Zhang TY et al (2015) Effects of Tai Chi and Multimodal Exercise Training on Movement and Balance function in mild to moderate idiopathic Parkinson Disease. Am J Phys Med Rehabil 94(10 Suppl 1):921–929 [DOI] [PubMed] [Google Scholar]
- 22.Kuang X et al (2023) The effects of different types of Tai Chi exercise on anxiety and depression in older adults: a systematic review and network meta-analysis. Front Public Health 11:1295342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.D’Onofrio G et al (2023) Musculoskeletal exercise: its role in promoting health and longevity. Prog Cardiovasc Dis 77:25–36 [DOI] [PubMed] [Google Scholar]
- 24.McGough EL et al (2011) Associations between physical performance and executive function in older adults with mild cognitive impairment: gait speed and the timed up & go test. Phys Ther 91(8):1198–1207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Morton NA (2009) The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother 55(2):129–133 [DOI] [PubMed] [Google Scholar]
- 27.Albanese E et al (2020) Construct validity of the Physiotherapy evidence database (PEDro) quality scale for randomized trials: item response theory and factor analyses. Res Synthesis Methods 11(2):227–236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moseley AM et al (2002) Evidence for physiotherapy practice: a survey of the Physiotherapy evidence database (PEDro). Aust J Physiother 48(1):43–49 [DOI] [PubMed] [Google Scholar]
- 29.Lucas BR et al (2016) Interventions to improve gross motor performance in children with neurodevelopmental disorders: a meta-analysis. BMC Pediatr 16(1):193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Birimoglu Okuyan C, Deveci E (2021) The effectiveness of Tai Chi Chuan on fear of movement, prevention of falls, physical activity, and cognitive status in older adults with mild cognitive impairment: a randomized controlled trial. Perspect Psychiatr Care 57(3):1273–1281 [DOI] [PubMed] [Google Scholar]
- 31.Yan Z-W et al (2022) Tai Chi for spatiotemporal gait features and dynamic balancing capacity in elderly female patients with non-specific low back pain: a six-week randomized controlled trial. J Back Musculoskelet Rehabil 35(6):1311–1319 [DOI] [PubMed] [Google Scholar]
- 32.Chewning B et al (2020) Disseminating Tai Chi in the community: promoting home practice and improving balance. Gerontologist 60(4):765–775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Day L et al (2012) Impact of tai chi on impairment, functional limitation, and disability among preclinically disabled older people: a randomized controlled trial. Arch Phys Med Rehabil 93(8):1400–1407 [DOI] [PubMed] [Google Scholar]
- 34.Ni M et al (2014) Comparative impacts of Tai Chi, balance training, and a specially-designed yoga program on balance in older fallers. Arch Phys Med Rehabil 95(9):1620–1628e30 [DOI] [PubMed] [Google Scholar]
- 35.Lifeng Z et al (2022) Effect of Tai Chi exercise on exercise ability of elderly patients with chronic diseases. Chin Conval Med 31(08):788–792 [Google Scholar]
- 36.Zhang JG et al (2006) The effects of Tai Chi Chuan on physiological function and fear of falling in the less robust elderly: an intervention study for preventing falls. Arch Gerontol Geriatr 42(2):107–116 [DOI] [PubMed] [Google Scholar]
- 37.Li F et al (2019) Effectiveness of Tai Ji Quan vs Multimodal and stretching Exercise interventions for reducing Injurious Falls in older adults at high risk of falling: follow-up analysis of a Randomized Clinical Trial. JAMA Netw open 2(2):e188280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liang LJC (2019) Effects of Tai Chi and resistance training on symptoms and exercise ability in the elderly with knee osteoarthritis. Chin J Rehabilitation Med 34(11):1304–1309 [Google Scholar]
- 39.Taylor D et al (2012) Effectiveness of Tai Chi as a community-based Falls Prevention intervention: a Randomized Controlled Trial. J Am Geriatr Soc 60(5):841–848 [DOI] [PubMed] [Google Scholar]
- 40.Gao Q et al (2014) Effects of Tai Chi on balance and fall prevention in Parkinson’s disease: a randomized controlled trial. Clin Rehabil 28(8):748–753 [DOI] [PubMed] [Google Scholar]
- 41.Liao YY et al (2021) Combining Transcranial Direct Current Stimulation with Tai Chi to Improve Dual-Task Gait performance in older adults with mild cognitive impairment: a Randomized Controlled Trial. Front Aging Neurosci, 13 [DOI] [PMC free article] [PubMed]
- 42.Zhu Y et al (2019) Tai Chi and whole-body vibrating therapy in sarcopenic men in advanced old age: a clinical randomized controlled trial. Eur J Ageing 16(3):273–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hwang HF et al (2016) Effects of Home-based Tai Chi and Lower Extremity Training and Self-Practice on Falls and Functional outcomes in older fallers from the Emergency Department-A Randomized Controlled Trial. J Am Geriatr Soc 64(3):518–525 [DOI] [PubMed] [Google Scholar]
- 44.Lyons JG et al (2015) Assessing the agreement between 3-meter and 6-meter walk tests in 136 community-dwelling older adults. J Aging Health 27(4):594–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Niño A, Villa-Vicente JG, Collado PS (2022) Functional capacity of Tai Chi-practicing Elderly people. Int J Environ Res Public Health, 19(4) [DOI] [PMC free article] [PubMed]
- 46.Taylor-Piliae RE et al (2014) Effect of Tai Chi on physical function, fall rates and quality of life among older stroke survivors. Arch Phys Med Rehabil 95(5):816–824 [DOI] [PubMed] [Google Scholar]
- 47.Xia T-W et al (2019) Different training durations and styles of tai chi for glucose control in patients with type 2 diabetes: a systematic review and meta-analysis of controlled trials. BMC Complement Altern Med 19(1):1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen KM et al (2007) Well-being of institutionalized elders after Yang‐style Tai Chi practice. J Clin Nurs 16(5):845–852 [DOI] [PubMed] [Google Scholar]
- 49.Lin J et al (2024) The effects of different types of Tai Chi exercises on preventing falls in older adults: a systematic review and network meta-analysis. Aging Clin Exp Res 36(1):65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roberts BL et al (2015) Research Methodology for Tai Chi Chuan. Methodologies for Effectively Assessing Complementary and Alternative Medicine (CAM): Research Tools and Techniques,: p. 249
- 51.Liu H, Frank A (2010) Tai Chi as a balance improvement exercise for older adults: a systematic review. J Geriatr Phys Ther 33(3):103–109 [PubMed] [Google Scholar]
- 52.Lan C, Chen S-Y, Lai J-S (2008) The exercise intensity of Tai Chi Chuan. Tai Chi Chuan 52:12–19 [DOI] [PubMed] [Google Scholar]
- 53.Wang LC et al (2021) Optimal exercise parameters of tai chi for balance performance in older adults: a m eta-analysis. J Am Geriatr Soc 69(7):2000–2010 [DOI] [PubMed] [Google Scholar]
- 54.Emilio EJM-L et al (2014) The association of flexibility, balance, and lumbar strength with balance ability: risk of falls in older adults. J Sports Sci Med 13(2):349 [PMC free article] [PubMed] [Google Scholar]
- 55.Zou L et al (2017) Effect of Yang-style Tai Chi on gait parameters and musculoskeletal flexibility in healthy Chinese older women. Sports, 5(3) [DOI] [PMC free article] [PubMed]
- 56.Lei H et al (2022) The effects of different types of Tai Chi exercises on motor function in patients with Parkinson’s disease: a network meta-analysis. Front Aging Neurosci 14:936027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huang J, Wang D, Wang J (2021) Clinical evidence of Tai Chi exercise prescriptions: a systematic review. Evidence-Based Complement Altern Med 2021:1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chia M, Jan A (2012) Tai Chi Fa jin: Advanced techniques for discharging chi energy. Simon and Schuster
- 59.Jaqueline da Cunha M et al (2021) Functional electrical stimulation of the peroneal nerve improves post-stroke gait speed when combined with physiotherapy. A systematic review and meta-analysis. Ann Phys Rehabil Med 64(1):101388 [DOI] [PubMed] [Google Scholar]
- 60.Huang CY et al (2022) The effect of Tai Chi in elderly individuals with Sarcopenia and frailty: a systematic review and meta-analysis of randomized controlled trials. Ageing Res Rev 82:101747 [DOI] [PubMed] [Google Scholar]
- 61.Sanchez-Rodriguez D, Marco E, Cruz-Jentoft AJ (2020) Defining Sarcopenia: some caveats and challenges. Curr Opin Clin Nutr Metab Care 23(2):127–132 [DOI] [PubMed] [Google Scholar]
- 62.Chen PJ et al (2020) Augmented reality-assisted training with selected Tai-Chi movements improves balance control and increases lower limb muscle strength in older adults: a prospective randomized trial. J Exerc Sci Fit 18(3):142–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu D (2003) The effects of Tai Chi exercise on proprioception and neuromuscular responses in the elderly people. The Chinese University of Hong Kong (Hong Kong)
- 64.Aman JE et al (2015) The effectiveness of proprioceptive training for improving motor function: a systematic review. Front Hum Neurosci 8:1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.