Abstract
Personal characteristics, unfavorable weather conditions and air pollution have been linked with reduced physical activity in children. However, among children with asthma the effects of these parameters remain unclear. This study objectively quantified the physical activity of children with asthma and evaluated its association with environmental, personal, and clinical parameters. Participants of the prospective LIFE-MEDEA asthma study wore the EMRACE™ smartwatch daily for continuous monitoring of physical activity and acquisition of global positioning system data. Daily physical activity, personal and clinical data were combined with daily temperature, precipitation, and air pollution levels in adjusted mixed effect regression models to examine the relationship between physical activity and the examined parameters. For a follow-up period of 4 months, 186 children with asthma demonstrated a decrease of 796 steps (95% CI: -1080, -512) on days with precipitation compared to non-precipitation days and a decrease of 96 steps (95% CI: -182, -9) for every 10 µg/m3 increase in PM10. The relationship between temperature and daily steps was characterized by an inverted U-shape. There was also evidence that gender and age-adjusted BMI z-score were negatively associated with daily steps. These results can further inform the design of physical activity interventions targeting children with asthma.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-025-87426-5.
Keywords: Childhood asthma, Physical activity, Pedometer, Weather, Air pollution
Subject terms: Paediatric research, Epidemiology
Introduction
Asthma is the most common chronic condition of childhood1 and despite the use of existing medications, it may impact physical development, school attendance, physical activity, and overall quality of life of children2–5. The relationship between asthma and physical activity is complex. Intense physical activity may trigger asthma symptoms for 40–90% of patients, while outdoor exercise can increase exposure to asthma exacerbation triggers such as cold air, and air pollution2,6. On the other hand, studies have demonstrated that engaging in physical activity is associated with better asthma control and2–4reduced exercise-induced bronchoconstriction (EIB)7. Therefore, children with asthma not only can participate in physical activity, but should be encouraged to do so, as a method to control asthma symptoms and reduce EIB6,7. However, many children with asthma do not reach the recommended levels of physical activity, either due to physiological limitations and or habits of physical inactivity7–9. Parental or individual anxiety related to EIB may also hinder children reaching adequate physical activity levels, with a vicious cycle of inactivity often established, resulting in both worsened EIB and the loss of other benefits related to physical activity7,8.
Generally, exercise during early childhood establishes patterns and defines behaviors and obesity later in life10, making childhood a critical period to study the relationship between asthma and physical activity11. To date, most of the literature on asthma and physical activity has focused on comparing the physical activity levels of children with and without asthma2,12 and has found that people with asthma engage in less physical activity compared to those without13. Most previous studies have used self-reported measures for physical activity which are limited by non-response and recall biases, as well as lack of validation2. Only few studies have objectively quantified physical activity in this group with the use of accelerometers, even for limited periods of few days, and explored factors affecting physical activity levels among children with asthma12,14. Furthermore, although several studies have found that environmental parameters impact physical activity levels of non-asthmatic children15,16, we did not identify any studies investigating the impact of environmental parameters such as particulate matter (PM) levels, temperature, and precipitation, on objectively measured physical activity levels of children with asthma. Studying the impact of weather and pollution on physical activity of asthmatic children is critical, given their vulnerability to environmental exposures compared to non-asthmatic children.
This study aimed to prospectively quantify daily physical activity of children with asthma in Cyprus and Crete-Greece using wearable sensors for a period of four months and examine its association with environmental (PM, temperature, and precipitation), anthropogenic, demographic, and clinical parameters.
Results
In total, 192 children (58% boys, median age 9 years) with asthma participated in the LIFE-MEDEA cohort during the years of 2019 and 2021. Overall, 109 (57%) were recruited in Crete-Greece and 83 (43%) were recruited in Cyprus. Table 1 summarizes their demographic and clinical characteristics. A small subset withdrew from the cohort (n = 2) or participated without wearing the smartwatch (n = 3). After the exclusion of observation days during which participants did not wear the smartwatch at all and observation days with very low smartwatch wear-time, 186 participants and 7,248 observation days were available for analysis.
Table 1.
Demographic and clinical characteristics of children with asthma in the LIFE-MEDEA cohort.
| N = 192 children | N | Median1 | IQR |
|---|---|---|---|
| Age (yrs) | 192 | 9 | (8;11) |
| Gender (boy) | 192 | 111 (57.81) | |
| BMIz (age-adjusted z-score) | 172 | 0.885 | (-0.2;1.84) |
| Atopy | 121 | 71 (58.68) | |
| Baseline c-ACT score | 167 | 24 | (22;26) |
| Baseline FEV1% predicted | 140 | 103.2 | (93.21;111.64) |
| Baseline FVC % predicted | 134 | 103.89 | (96.77;112.9) |
| Intervention group2 | 192 | ||
| Controls | 73 (37.50) | ||
| Outdoor Intervention | 53 (27.60) | ||
| Combined Intervention | 68 (34.90) | ||
| Country | 192 | ||
| Cyprus | 83 (43.223) | ||
| Crete, Greece | 109 (56.77) | ||
| Daily number of steps (total)3 | 7,248 | 9705.5 | (2026;13034) |
| Daily number of steps (outside house & classroom) | 5,150 | 5948 | (3622;8798) |
| Daily number of steps (at school) | 3,599 | 5012 | (3632;6772) |
| Daily number of steps (at school, outside) | 3591 | 4172 | (2758;5928) |
| Daily number of steps (afternoon) | 7,123 | 4439 | (2580;7042) |
| Daily number of steps (afternoon, outside) | 4,221 | 2308 | (839;4671) |
IQR interquartile range, BMI body mass index, c-ACT childhood asthma control test, FEV1 forced expiratory volume in one second, FVC forced vital capacity, pp percent predicted.
1 Number and percentage N (%) are reported for categorical variables.
2 The LIFE-MEDEA study is an intervention study, investigating interventions aimed to reduce desert dust exposure. Participants were assigned to one of three groups: (1) no intervention (2) interventions for outdoor exposure, and (3) interventions for both indoor and outdoor exposure.
3 Number of observation days are reported for step data.
Area weather and atmospheric conditions
Across all observation days, the daily median temperatures were 16.6˚C and 20.9˚C, and the median precent humidity 71.2 (IQR:10.2) and 46.5 (IQR:22) in Crete and Cyprus, respectively (Table S1). Precipitation data were available for 5,674 observation days with Cyprus having 795 (24.6%) and Crete 866 (35.9%) observation days with precipitation. PM10 data were available for all 7,248 observation days, and the median daily PM10 levels were 28.1 µg/m3 (IQR:11.8) in Crete and 33.1 µg/m3 (IQR: 12.1) in Cyprus. PM2.5 data were available for 3,233 days, all of which were observations from Cyprus where the median daily PM2.5 level was 15.6 µg/m3 (IQR:7.9).
Physical activity distributions
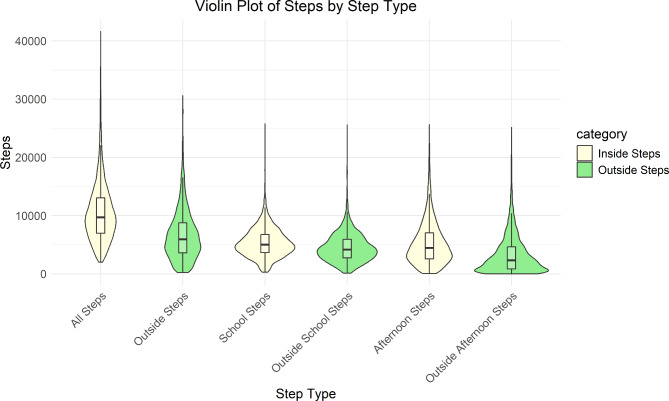
Across all observation days, the median daily steps were 9,706 (IQR: 11,008) (Table 1), while the median daily outside steps were 5,948 (IQR: 5,176). The median daily steps for school and afternoon hours were 5,012 (IQR: 3,140) and 4,439 (IQR: 4,462), respectively. The distributions of daily steps across the different time periods are summarized using violin plots in Fig. 1.
Fig. 1.
Violin plot of daily steps: Distribution of steps, inside and outside home/classroom, across the whole day and during school and afternoon time periods.
Effect of environmental parameters on physical activity
In the adjusted mixed effect regression models, we found that precipitation was associated with a decrease of 796 (β: -796, 95%CI: -1080, -512, pvalue<0.001) steps per day compared to days without any precipitation (Table 2). We also found that an increase in 10 µg/m3 PM10 was associated with a decrease of 96 steps per day (β: -96, 95%CI: -182, -9, pvalue=0.030). In contrast, changes in PM2.5 levels were not found to be significantly associated with physical activity.
Table 2.
Coefficients for environmental parameters of mixed effects model assessing steps per day (all days, hot days, and cold days).
| Environmental Parameter | Coefficient | 95% CI | p value | ||
|---|---|---|---|---|---|
| All days | Temperature per ˚C | 43 | -7 | 93 | 0.093 |
| Rain (binary) | -796 | -1080 | -512 | < 0.001 | |
| PM10 per 10 µg/m3 | -96 | -182 | -9 | 0.030 | |
| PM2.5 per 10 µg/m3 | 69 | -286 | 423 | 0.711 | |
| Hot days1 | Temperature per ˚C | -204 | -349 | -58 | 0.006 |
| Rain (binary) | 595 | -861 | 2051 | 0.423 | |
| PM10 per 10 µg/m3 | 197 | -181 | 576 | 0.307 | |
| PM2.5 per 10 µg/m3 | -33 | -671 | 604 | 0.919 | |
| Cold days2 | Temperature per ˚C | 298 | 129 | 467 | 0.001 |
| Rain (binary) | -1215 | -1749 | -680 | < 0.001 | |
| PM10 per 10 µg/m3 | -199 | -328 | -71 | 0.002 | |
| PM2.5 per 10 µg/m3 | 281 | -755 | 1317 | 0.595 | |
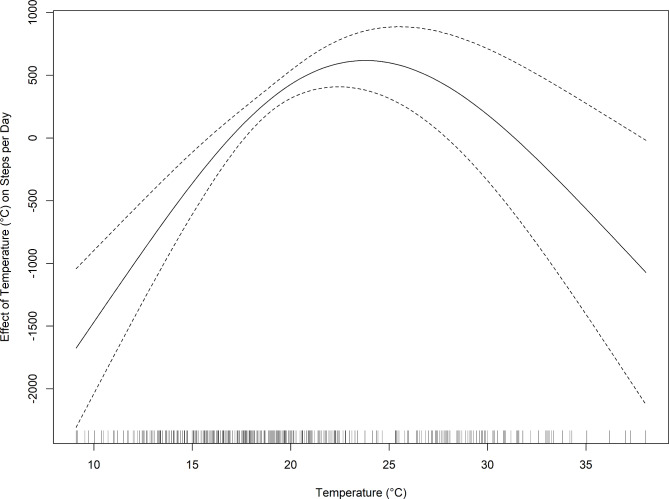
Finally, in the main analysis, which employed a linear function to model the relationship between temperature and daily steps, this was not statistically significant (β: 43, 95%CI: -7, 93, pvalue = 0.093 (Table 2). Nevertheless, in post-hoc assessments with a generalized additive mixed model, we demonstrated that temperature modelled as a natural cubic spline with three knots, best fitted the data (BIC: 121,494.1 and AIC: 121,372.8) and an inverted U-shaped curve summarized the nonlinear relationship between temperature and steps (Fig. 2). In post-hoc analyses stratified by hot and cold days, we found a decrease of 204 total daily steps for every increase in degrees Celsius during hot days (β: -204, 95%CI: -349, -58, pvalue =0.006) and the inverse relationship between temperature and total steps for cold days (β: 298, 95%CI: 129, 467, pvalue=0.001). The effects of rain (β: -1,215, 95%CI: -1,749, -680, pvalue<0.001) and PM10 (β: -199, 95%CI: -328, -71, pvalue=0.002) were retained only for cold days (Table 2).
Fig. 2.
Nonlinear relationship between temperature and daily steps: Inverted U-shaped curve between temperature and daily steps.
In subgroup analyses restricted to either school or afternoon hours, the observed association between PM10 and physical activity remained significant, with every 10 µg/m3 increase in PM10 being associated with a decrease of 77 steps during both school hours (β: -77, 95%CI: -141,-13, pvalue=0.018) and afternoon hours (β: -77, 95%CI: -145, -10, pvalue=0.024) (Table S2). During school hours only, there was evidence of a positive association between PM2.5 and physical activity (pvalue=0.049). Regarding precipitation, the inverse association between rain and physical activity remained significant only during afternoon hours (β: -562, 95%CI: -787, -336, pvalue<0.001). In subgroup analyses stratified by cold and hot days, we found that the effect of rain on school hours and afternoon steps was retained for cold days and was more profound in afternoon hours (β: -911, 95%CI: -1288, -535, pvalue<0.001) compared to school hours (β: -550, 95%CI: -947, -154, pvalue= 0.007). The same was true for PM10 during cold days with a negative relationship observed during afternoon hours (β: -113 steps per 10 µg/m3 PM10 increase, 95%CI: -203, -23, pvalue=0.014) as opposed to a non-significant relationship observed during school hours (β: -57 steps per 10 µg/m3 PM10 increase, 95%CI: -161, 47, pvalue=0.281).
In models for outside home and classroom steps the effect of rain remained (β: -739, 95%CI: -1061, -417, pvalue<0.001) (Table 4). Stratified analyses revealed that this association was strongest for cold days (β: -1268, 95%CI: -1851, -686, pvalue<0.001) (Table S3). As in the main analysis, we found overall a null association between temperature and outside steps per day; however, on cold days we observed an increase in 233 steps per unit increase in degree Celsius (β: 233, 95%CI: 41, 425, pvalue<0.017) and on hot days we found a decrease in 322 steps per unit increase in degree Celsius (β: -322, 95%CI: -485, -158, pvalue<0.001).
Effect of personal and clinical parameters on physical activity
Boys took on average 1,014 (β: 1,014, 95%CI: 84.05, 1,944, pvalue =0.033) more steps per day than girls. In analyses stratified by hot and cold days, we found that the association between gender and physical activity remained consistent with boys demonstrating on average 1,223 and 1,026 more steps per day, compared to girls, on hot and cold days, respectively (pvalue=0.040). There was also evidence of a negative association between BMI z-score with steps per day (β: -297, 95%CI: -636, 43, pvalue=0.087); this relationship has being also consistent during hot (β: -441, 95%CI:-882,1, pvalue=0.050) and cold days (β: -597, 95%CI:-963,-202, pvalue=0.001) (Table 3).
Table 3.
Coefficients for clinical and demographic parameters of mixed effects model assessing steps per day (all days, hot days, and cold days).
| Clinical Characteristics | Coefficient | 95% CI | p value | ||
|---|---|---|---|---|---|
| All days | c-ACT | -4 | -54 | 47 | 0.891 |
| Age (yr) | 18 | -256 | 292 | 0.897 | |
| BMIz | -297 | -636 | 43 | 0.087 | |
| Gender (boy) | 1014 | 84 | 1944 | 0.033 | |
| Atopy | 455 | -657 | 1567 | 0.422 | |
| FEV1% | -15 | -53 | 22 | 0.425 | |
| FVC % | -25 | -68 | 17 | 0.240 | |
| Hot days1 | c-ACT | -26 | -195 | 143 | 0.762 |
| Age (yr) | -57 | -402 | 289 | 0.748 | |
| BMIz | -441 | -882 | 1 | 0.050 | |
| Gender (boy) | 1223 | 56 | 2390 | 0.040 | |
| Atopy | 803 | -818 | 2424 | 0.332 | |
| FEV1% | -6 | -62 | 50 | 0.831 | |
| FVC % | -22 | -87 | 42 | 0.495 | |
| Cold days2 | c-ACT | -2 | -114 | 109 | 0.967 |
| Age (yr) | 35 | -249 | 319 | 0.808 | |
| BMIz | -597 | -963 | -202 | 0.001 | |
| Gender (boy) | 1026 | 49 | 2004 | 0.04 | |
| Atopy | 731 | -374 | 1836 | 0.195 | |
| FEV1% | 4 | -35 | 42 | 0.858 | |
| FVC % | 1 | -43 | 45 | 0.966 | |
CI confidence interval, p-value probability value, BMI body mass index, c-ACT childhood asthma control test, FEV1% forced expiratory volume in one second, FVC % forced vital capacity, percent predicted.
1Hot days refer to days > 80th percentile temperature for each country.
2Cold days refer to days < 20th percentile temperature.
The effect of gender on physical activity was also similar for outside home and classroom steps across all days, with boys taking on average 963 (β: 963, 95%CI: 192, 1734, pvalue=0.014) more steps than girls (Table 4). This effect was strongest for hot days (β: 1334, 95%CI: 391, 2277, pvalue=0.015) (Table S3). We did not find significant associations between any of the other personal or clinical parameters and outside steps for all, cold, or hot days (Table 4) (Table S3).
Table 4.
Coefficients of mixed effects model assessing outside steps per day.
| Parameter | Coefficient | 95% CI | p value | |
|---|---|---|---|---|
| Environmental | ||||
| Temperature (˚C) | 19 | -38 | 75 | 0.516 |
| Rain (binary) | -739 | -1061 | -416 | < 0.001 |
| PM10 per 10 µg/m3 | 39 | -65 | 142 | 0.465 |
| PM2.5 per 10 µg/m3 | 45 | -36 | 45 | 0.826 |
| Clinical & Demographic | ||||
| Baseline ACT | 11 | -46 | 68 | 0.708 |
| Age (yr) | 53 | -171 | 277 | 0.641 |
| BMIz | -96 | -37 | 182 | 0.499 |
| Gender (male) | 963 | 192 | 1734 | 0.014 |
| Atopy | 98 | -680 | 1 | 0.805 |
| FEV1% | 4 | -26 | 34 | 0.798 |
| FVC % | -9 | -44 | 26 | 0.618 |
CI confidence interval, p-value probability value, PM10 particulate matter 10 micrometers and smaller, PM2.5 particulate matter 2.5 micrometers and smaller, BMI body mass index, c-ACT childhood asthma control test, FEV1% forced expiratory volume in one second, percent predicted, FVC % forced vital capacity, percent predicted.
Discussion
In this study, we objectively assessed the impact of environmental and personal parameters on physical activity of children with asthma using wearable sensors. Our findings indicate that among personal parameters, male gender and BMI were positively and negatively associated with total daily steps, respectively. Among environmental parameters, precipitation and PM10 were negatively associated with daily steps. The relationship between temperature and daily steps was nonlinear, characterized by an inverted U-shape.
Gender differences in physical activity among children with asthma are consistent with a previous report from Cyprus that also used objective measures of physical activity, albeit for a shorter duration of follow-up and more narrow age range (8–9 years)14. Similarly, the systematic review by Vasconcello-Casillo et al. ascertained that the majority of studies that conducted sub-analyses by gender found that boys consistently demonstrate higher levels of physical activity compared to girls2. These results mirror the trend among the general population, where from a young age girls are less physically active and have lower levels of cardiorespiratory fitness compared to boys14,17,18. In children with asthma, these findings may also reflect gender differences in asthma treatment, where girls are less likely to receive professional counseling or medical treatment for asthma compared to boys leading to decreased physical activity14. Furthermore, the design and facilities of many playgrounds may be less appealing towards activities often preferred by girls, thereby contributing to this disparity18.
Our results also corroborated pre-existing findings of an inverse relationship of BMI with physical activity. Characteristically, a study from the same region (Greece) assessing pedometer-measured physical activity in 9- to 14-year-old non-asthmatic children found that overweight and obese children were significantly less physically active when compared to normal weight children17. Similar findings were reported for adults with asthma19. In addition, it has been demonstrated that physical activity mediates the relationship between asthma and high BMI in children and adolescents20. Nevertheless, the temporal relationship between asthma, BMI, and physical activity remains unclear. Possible pathways, including negative self-perception or parental and/or personal anxiety related to EIB and other symptoms secondary to physical exertion, lead from asthma to sedentary lifestyle and higher BMI7–9. On the other hand, withstanding inconsistent data, obesity is considered a risk factor for the development and worsening of asthma;21,22 based on this notion, several researchers have examined the aimed to demonstrate the benefits of weight intervention studies with mixed results, especially in children23,24.
Our study found that higher PM10 concentrations decreased daily steps. This result is in line with a previous analysis from this cohort that focused on desert dust storm days and demonstrated that, in general, children with asthma reduced their steps outside home and classroom during desert dust storm days compared to non-desert dust storm days. Especially for children with asthma that received intervention with early warnings and behavioral recommendations to reduce outdoor physical activity during desert dust days, the effect was much more profound. In more detail, the change in daily steps performed outside classrooms and homes during desert dust days, was − 495 steps (pvalue = 0.350) in asthmatic children not receiving any intervention and − 1040 steps (pvalue = 0.003) in asthmatic receiving the intervention25. Similar to our findings, a prospective study by Yu and Zhang of non-asthmatic Chinese children, using objectively measured physical activity, demonstrated that PM2.5 and more so PM10 were associated with a decrease in physical activity15. This decrease in physical activity could be due to a reduction in physical activity following media air pollution alerts15 or due to behavioral adaptations. As air pollution is a known trigger for bronchoconstriction, children with asthma and their care takers may refrain from going outside during periods of high air pollution2,6. This pathway aligns with our finding that PM10 had the greatest effect on cold days, another trigger for bronchoconstriction, because there may extra care to avoid these co-exposures6.
The association between temperature and physical activity in children with asthma is described for the first time in this study. We report an inverted U-shape relationship, which largely aligns with findings from studies involving non-asthmatic children26. Children with asthma may be more sensitive to temperature changes because colder air is a trigger for bronchoconstriction and hot and humid air makes it more difficult to breathe6,27. Not surprisingly, caregivers often monitor weather conditions in advance and may prefer indoor and more sedentary activities to minimize asthma exacerbation risk on days with unfavorable weather28,29. Furthermore, aligning with studies of non-asthmatic children, in our study precipitation was negatively associated with asthmatic children’s daily steps26. Notably, our finding that this impact was strongest for afternoon hours suggests that parental anxiety may predominantly drive this association7. The absence of a negative association between precipitation and daily steps during hot days may be explained by the potential cooling effect of cloud cover that may encourage physical activity on hot days.
Engaging in physical activity is beneficial for children with asthma and can help build healthy habits that continue into adulthood;10 however, many children with asthma are not reaching the recommended physical activity levels6,7. We found that precipitation, extreme temperatures, air pollution, and personal characteristics such as gender and BMI, in conjunction with personal and parental behaviors may create barriers for children with asthma to engage in physical activity.
In terms of weather and air pollution, planning for days with increased precipitation, extreme temperatures -both of which are expected to increase with ongoing climate change- and high air pollution can help children meet physical activity recommendations26. This may include creating indoor spaces for physical activity, such as gymnasiums, organizing indoor physical activities, and planning physical activities to align with seasonal weather patterns26,30. In18addition, special care should be given by local and school authorities to design playground facilities and fund playground activities that appeal to girls18. Further, asthmatic girls’ engagement in physical activities should be supported by their healthcare providers and caretakers, including addressing societal norms and stereotypes related to appropriate kinds of physical activities, body image perception, and conceptions around sweating, which may create poise barriers for girls engaging in physical activity14. Other considerations for the design of urban environments and school infrastructure that can further promote physical activity among asthmatic children include ensuring high air quality in both indoor and outdoor areas used for physical activity. In indoor areas, this can be achieved by appropriate ventilation systems31 or use of indoor air purifiers32,33. In the outdoor setting, this can be achieved with the efficient use of green infrastructure, such as the introduction of hedges of appropriate barrier height, porosity and length between traffic and areas of outdoor physical activity, promoting the creation of urban “green oases” that are characterized by low ventilation and absence of any internal air pollution sources34. Furthermore, as extreme high temperatures are expected to increase in many areas of the world in the context of climate change, shading interventions including enhanced green canopy or shade sails in urban parks are needed to improve thermal comfort, which may also promote physical activity during the warmer months35,36. Beyond the likely direct effects of environmental parameters on physical activity in this sensitive population group, it is likely that some of these associations may be mediated by self/parental fear and anxiety around asthma symptoms and EIB7,8. To address these anxieties, more resources should be provided to families of children with asthma that explain the importance of physical activity, the ways to safely engage in physical activity, and how to control asthma37. Personalized treatment plans could be created that include physical activity and advise parents and children on what conditions are safe or risky for children with asthma38.
To the best of our knowledge, our study is the first study to assess the impact of environmental and other parameters on physical activity among children with asthma in the Eastern Mediterranean region. The major strength of this study is the use of pedometer and geolocation data from wearable sensors to objectively assess physical activity, as opposed to studies based on subjective recall of physical activity, which may be biased. Furthermore, unlike previous studies using objectively measured physical activity data, our study acquired data from a relatively long follow-up period (4 months) and a large number of children with asthma (n = 186).
Nevertheless, our study has some weaknesses. Firstly, a comparison control group of healthy children was not included in the study, and it is unclear if the effects of environmental, demographic and clinical parameters on physical activity would have been similar in healthy children as well. In addition, the study population included mostly children with well controlled asthma and as a result the estimates of this study may be different in children with more severe asthma and reduced lung function. Previous studies have demonstrated that physical fitness is lower in children and adolescents with severe asthma compared to those with mild asthma39 and it is possible that the negative associations between air pollution and unfavorable weather conditions may be even more profound among children with severe asthma. Moreover, the relationship between asthma and determinants of physical activity in children may be influenced by socio-economic status40 and other relevant parameters including race41, housing conditions42 and neighborhood factors43. Similarly, risk perception regarding air pollution44 as well as perceived competence and attitude toward physical activity9 have also been shown to affect physical activity and aerobic fitness among children with asthma. Therefore, additional studies in severe asthma groups and in other geographical regions are required to explore further this relationship.
Furthermore, the smartwatch, used for data collection, needed to be recharged at night; therefore, night-hour activity data is missing. However, children are not expected to be active during the night. Future studies utilizing wearable sensors could consider investigating the sleeping patterns and nighttime activity of children with asthma, who often have problems sleeping45. Likewise, smartwatches may inaccurately represent cycling and walking upstairs and cannot be worn during swimming. As such, more detailed assessments of different types of physical activities were not possible. Lastly, the accuracy of GPS signal is known to be frequently compromised by signal loss in and around buildings; this may have introduced uncertainty in our assessment of inside and outside steps. To account for this uncertainty, we used a 100 m radius “buffer” around a participant’s home or classroom and relied on a GPS data filling algorithm, as suggested in previous studies46.
Conclusions
Among children with asthma, female gender, BMI, precipitation and PM10 are negatively associated with physical activity, while the relationship with temperature is characterized by an inverted U-shaped. These results highlight the role of different parameters on the complex relationship between asthma and physical activity and can further inform the design of interventions to encourage physical activity among children with asthma.
Materials and methods
Setting and study population
Cyprus and Crete-Greece are large islands located in the Eastern Mediterranean basin and are characterized by a subtropical climate with dry hot summers, mild rainy winters, and short autumn (October) and spring (April to May) periods of rapid weather change47 and mild temperatures48.
The design of the LIFE-MEDEA asthma panel study has been described in detail previously49. In brief, the study enrolled children aged 6 to 11 with mild to moderate persistent asthma from primary schools in Cyprus and Crete between 2019 and 2021. A new cohort was enrolled each year, and the children were followed up from February through May. For this analysis we excluded data from 2020 due to changes in personal behavior and asthma morbidity in response to the COVID-19 pandemic and resulting lockdown measures50.
To be included in this study children needed to have a physician diagnosis of asthma and meet additional inclusion criteria, described in detail in Supplementary Material. Following recruitment, participants were randomized into three intervention groups for exposure reduction to air pollution during the desert dust season at the two sites. These were the control group (no intervention), the outdoor intervention group (received early warnings and recommendations to stay indoors and limit outdoor physical activity during desert dust days) and the combined intervention group (also received early warnings and recommendations during desert dust days as well as had installed indoor air purifiers in houses and classrooms). During desert dust days, there was an overall reduction in physical activity outside home and classroom of children with asthma, but this effect was significantly more pronounced in the intervention groups receiving the early warnings and recommendations. Detailed information regarding the impact of these exposure reduction interventions on health outcomes among children with asthma is available elsewhere51 while information on ethics and informed consent is available in Supplementary Material. Briefly, in Cyprus, study approvals were obtained from the Cyprus National Bioethics Committee (EEBK EΠ 2017.01.141), the Data Protection Commissioner (No. 3.28.223) and the Ministry of Education (No 7.15.01.23.5). In Greece, approvals were obtained from the Scientific Committee (25/04/2018, No: 1748) and the Governing Board of the University General Hospital of Heraklion (25/22/08/2018). All research described was performed in accordance with relevant national guidelines and in accordance with the Declaration of Helsinki. Guardians of all participants provided written informed consent for their participation.
Physical activity and GPS tracking
Physical activity and GPS data of participating children were continuously assessed through wearable technology, as previously described25. In brief, upon recruitment the geographic coordinates of children’s home and classroom locations were entered to the MEDnea ® Health-Hub, a bi-directional, patient-centered web-based platform, and each child was given an EMBRACE™ smartwatch that was linked to their participant ID. The EMBRACE™ smartwatch is equipped with multiple sensors to continuously collect global positioning system (GPS) and activity data, as well as software to synchronize the transfer of data to the MEDnea ® Health-Hub. Data were collected in 5-minute intervals and uploaded automatically when participants’ smartwatches connected to their home Wi-Fi network. Participants were asked to wear the smartwatch continuously for seven days a week, excluding time when sleeping or swimming.
Children’s total “daily steps” (24 h period) and “daily outside” home and classroom steps were recorded. “Outside” was defined as outside of a 100-m radius from participants’ residences and classrooms. We used a 100-m radius to account for limitations in the signal accuracy of commercially available GPS receivers and because participants were in urban areas/indoor environments, where buildings may bounce or block GPS signals. Observation days during which participants did not wear the smartwatch at all (identified by absence of heart rate measurements) or observation days characterized by low smartwatch wear time (< 6 h of data collected) were a-priori excluded from this analysis to ensure data quality as described previously25,52.
Personal and clinical measurements
Gender, age, height, weight, lung function, scores on childhood Asthma Control Tests (cACT), information on asthma medication use, and information on unscheduled asthma-related clinician visits were recorded at baseline. Throughout follow-up, repeated assessments of cACT scores, lung function (FEV1% predicted and FVC% predicted) and FeNO were conducted. We also collected information on asthma medications use/clinician visits. Atopic sensitization was assessed at the end of follow-up by skin prick testing to 14 common airborne allergens51. Additional information on clinical measurements is available in Supplementary Material.
Environmental measurements
We obtained daily mean values of temperature, relative humidity, and precipitation from the urban meteorological station closest to participants’ residences while we obtained daily mean values of PM2.5 and PM10 for Nicosia, Cyprus and Heraklion, Crete from the corresponding urban air quality monitoring station. Additional details on data sources are presented in Supplementary Material.
Statistical analysis
Adjusted mixed effect regression models were used to examine the associations of environmental factors (temperature (˚C), precipitation (mm), PM10 (µg/m3), and PM2.5(µg/m3) (Eq. 1, Supplementary Material) and personal characteristics (age (years), gender, age-adjusted BMI z-scores, asthma symptom control, atopy status, and lung function (FEV1% predicted, FVC% predicted) (Eq. 2, Supplementary Material) on physical activity quantified as steps per day (all-day steps, school-hour steps, and afternoon steps). Mixed models were employed to account for repeated observations for each participant, and models were adjusted for seasonality, country, day of the week as well as for intervention group to control for potential confounding from the implementation of behavioral recommendations during dust-days. Public holidays were excluded from the analyses.
In the main analysis, the association between exposure variables and steps per day was modelled using a linear function. However, in post-hoc assessments of the model-fit we found that for temperature, a nonlinear spline model was more appropriate. We examined the fit of cubic spline models with 2, 3, 4, 5, and 6 knots, and chose the final model by comparing Bayesian information criterion (BIC) values. We further investigated the relationship between unseasonal temperatures and physical activity by repeating the analysis for warm (≥ 80th percentile) and cold days (≤ 20th percentile). All statistical analyses were carried out using STATA (Version 17, StataCorp, College Station, TX) and mixed effect regression models were developed using the xtmixed command, which uses Maximum Likelihood Estimation to calculate fixed and random effects, even if some predictor data were missing in certain observation days (rows). With this approach the likelihood function for the other predictors and the outcome variable (steps) was still calculated using the remaining available data, thus maximizing data usage. Statistical significance was set at p < 0.05.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful to all the participating children and their families as well as to the participating teaching and administrative personnel from primary schools in Cyprus and Greece. The study was financed by the European Union LIFE Project MEDEA (LIFE16 CCA/CY/000041) and the Cyprus Harvard Endowment Program for the Environment and Public Health.
Abbreviations
- EIB
Exercise-induced bronchoconstriction
- PM
Particulate matter; GPS: Global Positioning system
- cACT
childhood Asthma Control Test
- FEV1
Forced expiratory volume in 1 s
- FVC
Forced Vital Capacity
- BMI
Body Mass Index
- IQR
Interquartile Range
- BIC
Bayesian Information Criterion
Author contributions
Author’s contributions (CRediT authorship contribution) statementJB: software, data curation, visualization, formal analysis, writing-original draft preparation; PJ: methodology, formal analysis, supervision, writing—review and editing; AM: investigation, methodology, software, data curation, writing—review and editing; EG: project administration, writing—review and editing, supervision; EM: investigation, data curation, writing—review and editing; PK: investigation, data curation, writing—review and editing; NK: resources, data curation, writing—review and editing; GK: resources, data curation, writing—review and editing; EV: resources, data curation, writing—review and editing; CS: resources, data curation, writing—review and editing; FT: resources, data curation, writing—review and editing; PK: methodology, funding acquisition, supervision, writing—review and editing; PKY: conceptualization, methodology, funding acquisition, supervision, writing—review and editing; PK: conceptualization, project administration, methodology, formal analysis, writing-original draft preparation, supervision.
Funding
The study was financially supported by the European Union LIFE Project MEDEA (LIFE16 CCA/CY/000041).
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Univeristy of Cyprus.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors jointly supervised this work: Panayiotis K. Yiallouros and Panayiotis Kouis.
References
- 1.Stern, J., Pier, J. & Litonjua, A. A. Asthma Epidemiology and risk Factors42 (Springer, 2020). Seminars in immunopathology Ser. [DOI] [PubMed]
- 2.Vasconcello-Castillo, L. et al. Levels of physical activity in children and adolescents with asthma: a systematic review and meta‐analysis. Pediatr. Pulmonol.56, 1307–1323 (2021). [DOI] [PubMed] [Google Scholar]
- 3.Zhang, D. & Zheng, J. The burden of childhood asthma by age group, 1990–2019: a systematic analysis of global burden of disease 2019 data. Front. Pead.10, 823399 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang, Z. et al. Global, regional, and national burden of asthma and its attributable risk factors from 1990 to 2019: a systematic analysis for the global burden of Disease Study 2019. Respir. Res.24, 169 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trivedi, M. & Denton, E. Asthma in children and adults—what are the differences and what can they tell us about asthma? Front. Pead.7, 256 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klain, A. et al. Exercise-induced bronchoconstriction in children. Front. Med.8, 814976 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hennegrave, F. et al. Factors associated with daily life physical activity in patients with asthma. Health Sci. Rep.1, e84 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panagiotou, M., Koulouris, N. G. & Rovina, N. Physical activity: a missing link in asthma care. J. Clin. Med.9, 706 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pianosi, P. T. & Davis, H. S. Determinants of physical fitness in children with asthma. Pediatrics113, e225–e229 (2004). [DOI] [PubMed] [Google Scholar]
- 10.Savva, S. C. et al. High cardiorespiratory fitness is inversely associated with incidence of overweight in adolescence: a longitudinal study. Scand. J. Med. Sci. Sports. 24, 982–989 (2014). [DOI] [PubMed] [Google Scholar]
- 11.Landry, B. W. & Driscoll, S. W. Physical activity in children and adolescents. PM&R 4, 826–832 (2012). [DOI] [PubMed]
- 12.Pike, K. C., Griffiths, L. J., Dezateux, C. & Pearce, A. Physical activity among children with asthma: cross-sectional analysis in the UK Millennium cohort. Pediatr. Pulmonol.54, 962–969 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avallone, K. M. & McLeish, A. C. Asthma and aerobic exercise: a review of the empirical literature. J. Asthma. 50, 109–116 (2013). [DOI] [PubMed] [Google Scholar]
- 14.Yiallouros, P. K. et al. Gender differences in objectively assessed physical activity in asthmatic and non-asthmatic children. Pediatr. Pulmonol.50, 317–326 (2015). [DOI] [PubMed] [Google Scholar]
- 15.Yu, H. & Zhang, H. Impact of ambient air pollution on physical activity and sedentary behavior in children. BMC Public. Health. 23, 357 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ridgers, N. D., Fairclough, S. J. & Stratton, G. Variables associated with children’s physical activity levels during recess: the A-CLASS project. Int. J. Behav. Nutr. Phys. Activity. 7, 1–8 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michalopoulou, M. et al. Step counts and body mass index among 9–14 years old Greek schoolchildren. J. Sports Sci. Med.10, 215 (2011). [PMC free article] [PubMed] [Google Scholar]
- 18.Nielsen, G. & Pfister, G. Bo Andersen, L. Gender differences in the daily physical activities of Danish school children. Eur. Phys. Educ. Rev.17, 69–90 (2011). [Google Scholar]
- 19.Westermann, H., Choi, T. N., Briggs, W. M., Charlson, M. E. & Mancuso, C. A. Obesity and exercise habits of asthmatic patients. Ann. Allergy Asthma Immunol.101, 488–494 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leinaar, E., Alamian, A. & Wang, L. A systematic review of the relationship between asthma, overweight, and the effects of physical activity in youth. Ann. Epidemiol.26, 504–510 (2016). e6. [DOI] [PubMed] [Google Scholar]
- 21.Ali, Z. & Ulrik, C. S. Obesity and asthma: a coincidence or a causal relationship? A systematic review. Respir Med.107, 1287–1300 (2013). [DOI] [PubMed] [Google Scholar]
- 22.Scott, H. A. et al. Effect of obesity on airway and systemic inflammation in adults with asthma: a systematic review and meta-analysis. Thorax78, 957–965 (2023). [DOI] [PubMed] [Google Scholar]
- 23.Moreira, A. et al. Weight loss interventions in asthma: EAACI evidence-based clinical practice guideline (part I). Allergy68, 425–439 (2013). [DOI] [PubMed] [Google Scholar]
- 24.Okoniewski, W., Lu, K. D. & Forno, E. Weight loss for children and adults with obesity and asthma. A systematic review of randomized controlled trials. Annals Am. Thorac. Soc.16, 613–625 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kouis, P. et al. Responses of schoolchildren with asthma to recommendations to reduce desert dust exposure: results from the LIFE-MEDEA intervention project using wearable technology. Sci. Total Environ.860, 160518 (2023). [DOI] [PubMed] [Google Scholar]
- 26.Turrisi, T. B. et al. Seasons, weather, and device-measured movement behaviors: a scoping review from 2006 to 2020. Int. J. Behav. Nutr. Phys. Activity. 18, 1–26 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Voelker, R. Asthma forecast: why heat, humidity trigger symptoms. JAMA308, 20 (2012). [DOI] [PubMed] [Google Scholar]
- 28.Ruiz, S. et al. Towards emplaced understandings of risk: how caregivers of children with asthma identify and manage asthma-related risk across different places. Health Place. 75, 102787 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kelada, L. et al. Child and caregiver experiences and perceptions of asthma self-management. npj Prim. Care Respiratory Med.31, 42 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edwards, N. M. et al. Outdoor temperature, precipitation, and wind speed affect physical activity levels in children: a longitudinal cohort study. J. Phys. Activity Health. 12, 1074–1081 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee, Y. & Kim, Y. I. Analysis of indoor air pollutants and guidelines for space and physical activities in multi-purpose activity space of elementary schools. Energies15, 220 (2021). [Google Scholar]
- 32.Pacitto, A. et al. Effect of ventilation strategies and air purifiers on the children’s exposure to airborne particles and gaseous pollutants in school gyms. Sci. Total Environ.712, 135673 (2020). [DOI] [PubMed] [Google Scholar]
- 33.Achilleos, S. et al. Improved indoor air quality during desert dust storms: the impact of the MEDEA exposure-reduction strategies. Sci. Total Environ.863, 160973 (2023). [DOI] [PubMed] [Google Scholar]
- 34.Hewitt, C. N., Ashworth, K. & MacKenzie, A. R. Using green infrastructure to improve urban air quality (GI4AQ). Ambio49, 62–73 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brown, R. D., Vanos, J., Kenny, N. & Lenzholzer, S. Designing urban parks that ameliorate the effects of climate change. Landsc. Urban Plann.138, 118–131 (2015). [Google Scholar]
- 36.Cherian, N. C. & Subasinghe, C. Sun-Safe zones: investigating Integrated shading strategies for children’s play areas in Urban Parks. Int. J. Environ. Res. Public Health. 20, 114 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Searle, A., Jago, R., Henderson, J. & Turner, K. M. Children’s, parents’ and health professionals’ views on the management of childhood asthma: a qualitative study. NPJ Prim. care Respiratory Med.27, 53 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jago, R., Searle, A., Henderson, A. J. & Turner, K. M. Designing a physical activity intervention for children with asthma: a qualitative study of the views of healthcare professionals, parents and children with asthma. Bmj Open.7, e014020 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.D’Agostino, E. M. et al. The longitudinal association between asthma severity and physical fitness among New York City public school youth. Prev. Med.170, 107486 (2023). [DOI] [PubMed] [Google Scholar]
- 40.Gordon, B. et al. Association between Asthma and body mass index and socioeconomic status: a cross-sectional study on 849 659 adolescents. Respirology21, 95–101 (2016). [DOI] [PubMed] [Google Scholar]
- 41.D’Angelo, C. et al. Family Asthma management and physical activity among urban children. Families Syst. Health. 42, 193 (2024). [DOI] [PubMed] [Google Scholar]
- 42.Grant, T. L. & Wood, R. A. The influence of urban exposures and residence on childhood asthma. Pediatr. Allergy Immunol.33, e13784 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kumar, A. et al. The longitudinal association between asthma severity and physical fitness by neighborhood factors among New York City public school youth. Ann. Epidemiol.88, 37–42 (2023). [DOI] [PubMed] [Google Scholar]
- 44.Jordan, K. A. et al. Perceptions surrounding the possible interaction between physical activity, pollution and asthma in children and adolescents with and without asthma. BMC Public. Health. 23, 2416 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reiter, J., Ramagopal, M., Gileles-Hillel, A. & Forno, E. Sleep disorders in children with asthma. Pediatr. Pulmonol.57, 1851–1859 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dias, D. & Tchepel, O. Modelling of human exposure to air pollution in the urban environment: a GPS-based approach. Environ. Sci. Pollut. Res.21, 3558–3571 (2014). [DOI] [PubMed] [Google Scholar]
- 47.https://www.britannica.com/science/Mediterranean-climate
- 48.https://www.interkriti.org/intro/weather.htm
- 49.Kouis, P. et al. The MEDEA childhood asthma study design for mitigation of desert dust health effects: implementation of novel methods for assessment of air pollution exposure and lessons learned. BMC Pediatr.21, 1–9 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kouis, P., Lemonaris, M., Xenophontos, E., Panayiotou, A. & Yiallouros, P. K. The impact of COVID-19 lockdown measures on symptoms control in children with asthma: a systematic review and Meta‐analysis of observational cohort studies. Pediatr. Pulmonol.58, 3213–3226 (2023). [DOI] [PubMed] [Google Scholar]
- 51.Kouis Panayiotis et al. Improved childhood asthma control after exposure reduction interventions for desert dust and anthropogenic air pollution: the MEDEA randomised controlled trial. Thorax79, 495–507 (2024). [DOI] [PubMed] [Google Scholar]
- 52.Michanikou, A., Kouis, P., Karanicolas, K. & Yiallouros, P. K. Setup of consumer wearable devices for exposure and health monitoring in population studies. J. Vis. Exp. (192), e63275. 10.3791/63275 (2023). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Univeristy of Cyprus.