Abstract
Background
Constipated patients may exhibit anxious behaviors, but the relationship between the two remains unclear. This population-based study aims to investigate the relationships of anxiety status and anxiety duration with constipation among U.S. adults.
Methods
Using data from the National Health and Nutrition Examination Survey (NHANES) database spanning from 2007 to 2010, a cross-sectional study included 8945 participants was performed to assess the relationships of anxiety status and anxiety duration with constipation. Participants’ characteristics were presented using mean or proportion. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using multivariable logistic regression models. The analysis accounted for potential confounding factors, including gender, age, race/ethnicity, education level, marital status, PIR, BMI, smoking status, drinking status, chronic diseases, and dietary intake. Subgroup analyses were conducted to ensure the stability of the results. Smoothed curve fitting was applied to investigate both linear and nonlinear associations between anxiety duration and constipation risk. Threshold effects were assessed using two-piecewise linear regression models.
Results
Of the 8945 participants, 922 reported constipation, with a prevalence of 10.3%. After adjusting for confounding factors, individuals with anxiety status exhibited an increased risk of constipation (OR: 1.49, 95% CI: 1.28–1.73). Stratified analyses indicated that the association between anxiety status and constipation remained relatively stable across different stratification levels. Smoothed curve fitting and threshold effect analyses revealed a linear association between anxiety duration and constipation among adults aged 20–60, while a nonlinear inverted U-shaped relationship was observed in those aged 60 and older, with an inflection point at 10 days. The two variables correlated positively on the left side of the inflection point but not on the right.
Conclusion
This study showed that a significant association between anxiety status and constipation among U.S. adults. Additionally, an age-dependent association between anxiety duration and constipation was observed, particularly among individuals aged 60 and older.
Keywords: Anxiety, Brain-gut axis, Constipation, Population-based study, National Health and Nutrition Examination Survey
Introduction
Constipation, a prevalent gastrointestinal condition, affects an estimated 0.7–79% of the global population, with significant regional variation [1]. In North America, the prevalence is approximately 16%, with higher rates observed among women, the elderly, and individuals of lower socioeconomic status [2–4]. Constipation is characterized by low bowel frequency, difficulty passing stools, and a feeling of incomplete evacuation [5]. According to a study by Liu et al., we defined constipation in the NHANES dataset using stool consistency and frequency of bowel movements as effective methods for identification [6]. Constipation significantly impacts quality of life, often co-occurring with psychological conditions such as anxiety, depression, and cognitive decline [7, 8].
Anxiety has emerged as a significant global health concern, with a 12-month prevalence of 1.8% and lifetime prevalence of 3.7% across 26 countries [9, 10]. Anxiety is one of the manifestations of a wide range of mental disorders, characterized by acute, overwhelming, and persistent worry [11]. Anxiety status is defined as persistent feelings of worry, nervousness, or fear that interfere with daily activities, encompassing both situational and generalized anxiety [12]. According to recent research, the brain-gut axis plays a significant role in the relationship between anxiety and constipation [13].
The brain-gut axis refers to bidirectional communication between the central nervous system (CNS), enteric nervous system (ENS), and autonomic nervous system (ANS) [14]. This connection facilitates complex interactions influencing gastrointestinal function and mood disorders [15].
From the brain to the gut, anxiety can activate the hypothalamic-pituitary-adrenal (HPA) axis, leading to elevated corticotropin-releasing factor (CRF) levels. CRF has been shown to inhibit intestinal motility via corticotropin-releasing factor 1 (CRF1) receptors, contributing to constipation [16]. Stress-related changes in neurotransmitters like serotonin (5-hydroxy tryptamine, 5-HT) also impair colonic transit, exacerbating constipation symptoms [17].
Conversely, gut-to-brain signaling via the vagus nerve and intestinal microbiota plays a role in anxiety development. Altered gut microbiota in constipation patients can modulate brain activity through microbial metabolites, such as short-chain fatty acids (SCFAs), affecting emotional regulation [18]. Constipation disrupts this balance, perpetuating a cycle of gut and brain dysfunction [15].
There is evidence that prolonged periods of anxiety induce cumulative physiological changes, such as chronic HPA axis activation, that influence gastrointestinal motility differently than shorter episodes [19, 20]. Investigating anxiety duration allows for capturing these subtleties and may provide actionable thresholds for clinical intervention. Furthermore, an epidemiological study of gastrointestinal symptoms in Swiss young and middle-aged adults revealed strong associations (all p < 0.0001) between one-month fatigue and chronic stomach symptoms (OR: 9.96, 99% CI: 5.53–17.94) as well as chronic intestinal symptoms (OR: 9.02, 99% CI: 4.92–16.54) [21]. These findings suggest that the cumulative effect of prolonged symptoms may exacerbate gastrointestinal dysfunction. Drawing upon this evidence, we hypothesize that the cumulative impact of anxiety duration on constipation risk may exhibit distinct patterns across different age groups, reflecting physiological and psychological differences.
Current evidence indicates that constipation is significantly associated with dietary factors, including energy [22], protein [23], fat [24], and fiber [25] intake, as well as chronic conditions such as hypertension [26], diabetes [27], congestive heart failure [28], myocardial infarction [28], stroke [29], emphysema [30], chronic bronchitis [30], and cancer [31]. Therefore, when exploring the relationship between constipation and anxiety, it is crucial to conduct stratified analysis based on these factors.
The National Health and Nutrition Examination Survey (NHANES) was a program designed to assess the health and nutritional status of adults and children in the United States (www.cdc.gov/nchs/nhanes). This survey was distinctive as it combined both physical examinations and interviews. NHANES employed a cross-sectional design to provide nationally representative health data, including demographics, dietary habits, acute and chronic medical issues, mental health conditions, and prescription drug use. Exam components varied across survey cycles and typically included assessments such as blood pressure, vision, dental health, fitness, and body composition. Laboratory components focused on areas such as hematology, metabolic and cardiovascular health, and dietary biomarkers, offering a comprehensive dataset for public health research.
This study is designed with two primary objectives. The first is to examine the potential association between anxiety status and constipation in the U.S. population. The second is to investigate whether the cumulative impact of anxiety duration on constipation risk differs across age groups. To achieve these goals, we used data from the NHANES, a nationally representative survey of the U.S. population, to provide insights into the complex interplay between anxiety and constipation and inform targeted interventions for different demographic groups.
Materials and methods
Data source
The NHANES surveys are cross-sectional surveys that aim to collect health information from a nationally representative sample of the non-institutionalized population in the United States(https://www.cdc.gov/nchs/nhanes/about_nhanes.htm). The Centers for Disease Control and Prevention’s National Center for Health Statistics (NCHS) provided oversight to the design, conduction, management, and storage of data related to the NHANES.
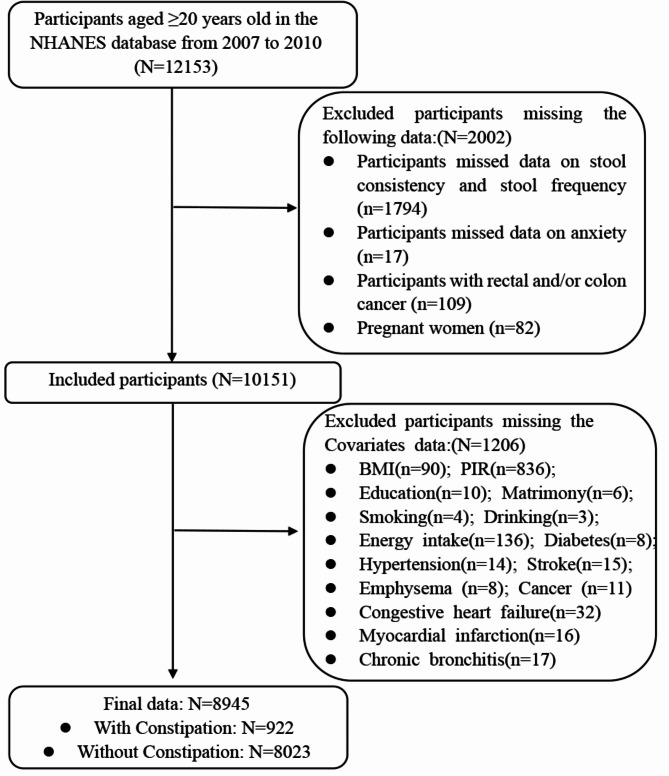
This population-based study analyzed data from the 2007–2008 and 2009–2010 NHANES survey cycles. We excluded participants who had a history of rectal or colon cancer (N = 109) and those who were pregnant (N = 82) [32]. After applying these exclusions, the final analytical sample included 8,945 participants aged 20 years and older. The participant selection process is illustrated in Fig. 1.
Fig. 1.
Flow diagram of the sample selection from the NHANES 2007–2010
Constipation
Constipation in the NHANES database was evaluated using two criteria: stool consistency and bowel movement frequency [33]. Stool consistency was assessed with the Bristol Stool Form Scale, which classifies stool into seven types. Participants selected their typical or most frequent stool type from illustrated cards with detailed descriptions. Those reporting Type 1 (separate, hard lumps, resembling nuts) or Type 2 (sausage-shaped but lumpy) were classified as experiencing constipation. Bowel movement frequency was determined through self-reported data, where participants indicated how often they had bowel movements. Individuals reporting fewer than three bowel movements per week were also categorized as constipated [34, 35].
Definition of anxiety status and anxiety duration
Anxiety status was assessed during the personal interview using the question, “During the past 30 days, about how many days did you feel worried, nervous, or anxious?” This assessment is part of the Health-Related Quality of Life (HRQoL) framework and is based on the 14-item Healthy Days measure developed by the Centers for Disease Control and Prevention (CDC) [36]. According to previous studies, anxiety states were initially categorized into two groups: “no” (feeling anxious for 0–6 days in the past 30 days) and “yes” (feeling anxious for 7–30 days in the past 30 days) [37, 38].
To further explore potential relationships, anxiety duration was categorized into four groups based on the number of self-reported anxious days: 0 days, 1–10 days, 11–20 days, and 21–30 days. While no standardized thresholds exist for anxiety duration, this exploratory categorization was guided by the distribution of responses in the dataset and informed by similar approaches in prior research [39].
Covariates
In our sociodemographic assessment, the included in the statistical models included gender, age, race/ethnicity (Mexican American, non-Hispanic white, non-Hispanic black, other Hispanic, and others), education level, marital status, poverty income ratio (PIR), body mass index (BMI) [40].In this study, age was categorized into three groups: 20–39 years, 40–59 years, and 60 years and older [21, 41]. Educational levels were categorized as less than high school, high school graduate, or college and higher [42]. PIR was classified into low-income (< 1.3), middle-income (≥ 1.3 and < 3.5), and upper-income (≥ 3.5). BMI was divided into underweight (< 18.5 kg/m²), normal weight (18.5–24.9 kg/m²), overweight (25.0–29.9 kg/m²), and obese (≥ 30.0 kg/m²) [43].
For behavioral risk factors, the included in the statistical models included smoking status [44], drinking status [45], and energy [22], protein [23], fat [24], and fiber [25] intake, based on previous studies indicating that these factors influence the occurrence of constipation. Smoking status was categorized into never smokers (fewer than 100 cigarettes in their lifetime), former smokers (more than 100 cigarettes but not currently smoking), and current smokers (actively smoking and having consumed over 100 cigarettes) [43]. Drinking status was classified as drinkers if individuals reported consuming at least 12 alcoholic beverages per year [45]. During the 24-hour dietary recall conducted by NHANES from 2007 to 2010, data on dietary energy, protein, fat, and fiber intake were collected. Based on previous studies, dietary intake of energy [22], protein [23], fat [24], and fiber [25] was divided into quartiles for analysis. Energy intake was classified as follows: lowest quartile (Q1, 164–1,409 kcal/day); middle lower quartile (Q2, 1,409.1–1,909 kcal/day); middle upper quartile (Q3, 1,909.1–2,582 kcal/day); and highest quartile (Q4, 2,582.1–13,509 kcal/day). Similarly, protein intake was divided into quartiles: lowest quartile (Q1, 0.63–51.72 g/day); middle lower quartile (Q2, 51.74–72.77 g/day); middle upper quartile (Q3, 72.78–99.94 g/day); and highest quartile (Q4, 99.95–474.01 g/day). Fiber intake was categorized as follows: lowest quartile (Q1, 0.1–9.1 g/day); middle lower quartile (Q2, 9.2–14 g/day); middle upper quartile (Q3, 14.1–20.5 g/day); and highest quartile (Q4, 20.6–147.6 g/day). Fat intake was also divided into four quartiles: lowest quartile (Q1, 0.2–45.8 g/day); middle lower quartile (Q2, 45.81–69.45 g/day); middle upper quartile (Q3, 69.46–100.3 g/day); and highest quartile (Q4, 100.34–601.33 g/day).
In chronic conditions, the included in the statistical models included hypertension [26], diabetes [27], congestive heart failure [28], myocardial infarction [28], stroke [29], emphysema [30], chronic bronchitis [30], and cancer [31]. Information on congestive heart failure, myocardial infarction, stroke, emphysema, chronic bronchitis, and cancer was obtained through self-reported questionnaire data. Diabetes was defined as a diagnosis by a healthcare professional or the use of anti-diabetic medications. Similarly, hypertension was defined as a diagnosis by a healthcare professional, the use of antihypertensive medications, or meeting clinical diagnostic criteria during physical examination, which included an average systolic blood pressure ≥ 140 mmHg or an average diastolic blood pressure ≥ 90 mmHg.
Statistical analyses
Data were presented as mean ± standard deviation (SD) for continuous variables and as percentages and counts (n) for categorical variables. Based on the distribution and characteristics of the data, group differences were assessed using the χ² test for categorical variables. For continuous variables, those following a normal distribution were analyzed using the t-test, while non-parametric continuous variables were evaluated with the Kruskal–Wallis test.
Separate multivariable regression analyses were conducted to investigate the relationships of anxiety status and anxiety duration with constipation, with Model I adjusted for gender, age, and ethnicity, and Model II further incorporating education level, marital status, poverty income ratio (PIR), body mass index (BMI), smoking status, alcohol consumption, chronic diseases (hypertension, diabetes mellitus, congestive heart failure, myocardial infarction, stroke, emphysema, chronic bronchitis, and cancer), as well as dietary intake (energy, protein, fat, dietary fiber).
Stratified analyses were conducted based on the categories of each covariate to evaluate whether the association between anxiety status and constipation was influenced by these factors.
The generalized additive model and smooth curve fitting were used to explore potential nonlinear relationships between anxiety duration and constipation. This analysis aimed to identify threshold effects and nonlinear trends across different age groups. Anxiety duration was treated as a continuous variable in smoothed curve fitting to explore potential nonlinear relationships. Finally, we employed a threshold effect analysis model to delve deeper into the nature of this relationship and identify potential inflection points between anxiety duration and constipation.
Statistical significance was determined by comparing the adjusted odds ratio (OR) to 1.0 and reporting a 95% confidence interval (CI). The statistical analyses were conducted using Empower Stats statistical software 2.0 (http://www.empowerstats.com, X& Y Solutions, Inc., Boston, MA, USA), incorporating appropriate sampling weights. A P value below 0.05 for both sides was deemed statistically significant.
Results
Basic characteristics of the study population
Table 1 presents a comparison of the characteristics of individuals in the constipated and normal groups. The study included 8945 participants, with an average age of 49.64 years. The distribution of participants was relatively even across age groups (20–39 years, 40–59 years, and 60 years and older). The gender distribution was nearly equal, with males and females each comprising approximately half of the participants.
Table 1.
Basic characteristics of study participants in the constipation and normal groups
| Total | Constipation | Test of significance | P-value | ||
|---|---|---|---|---|---|
| Variables | (N = 8945) | Without | With | ||
| (N = 8023) | (N = 922) | ||||
| Age | 49.64 ± 17.54 | 49.93 ± 17.44 | 47.09 ± 18.14 | T = 4.653 | < 0.001 |
| ≥ 20,<40 | 2947 (32.95) | 2589 (32.27) | 358 (38.83) | ||
| ≥ 40, < 60 | 3005 (33.59) | 2703 (33.69) | 302 (32.75) | ||
| ≥ 60 | 2993 (33.46) | 2731 (34.04) | 262 (28.42) | ||
| Sex | χ2 = 142.155 | < 0.001 | |||
| male | 4467 (49.94) | 4178 (52.08) | 289 (31.34) | ||
| female | 4478 (50.06) | 3845 (47.92) | 633 (68.66) | ||
| Race/ethnicity | χ2 = 22.092 | < 0.001 | |||
| Mexican American | 1517 (16.96) | 1380 (17.20) | 137 (14.86) | ||
| Other Hispanic | 879 (9.83) | 771 (9.61) | 108 (11.71) | ||
| Non-Hispanic White | 4485 (50.14) | 4059 (50.59) | 426 (46.20) | ||
| Non-Hispanic Black | 1697 (18.97) | 1479 (18.43) | 218 (23.64) | ||
| Other Race | 367 (4.10) | 334 (4.16) | 33 (3.58) | ||
| Education | χ2 = 25.834 | < 0.001 | |||
| Below high school | 2451 (27.40) | 2164 (26.97) | 287 (31.13) | ||
| High school graduate | 2140 (23.92) | 1881 (23.45) | 259 (28.09) | ||
| College or above | 4354 (48.68) | 3978 (49.58) | 376 (40.78) | ||
| Marital status | χ2 = 12.729 | < 0.001 | |||
| Others | 3530 (39.46) | 3116 (38.84) | 414 (44.90) | ||
| Currently married/living with partner | 5415 (60.54) | 4907 (61.16) | 508 (55.10) | ||
| PIR | χ2 = 55.606 | < 0.001 | |||
| < 1.3 | 2748 (30.72) | 2380 (29.66) | 368 (39.91) | ||
| ≥ 1.3, < 3.5 | 3414 (38.17) | 3063 (38.18) | 351 (38.07) | ||
| ≥ 3.5 | 2783 (31.11) | 2580 (32.16) | 203 (22.02) | ||
| BMI | χ2 = 31.281 | < 0.001 | |||
| < 18.5 | 135 (1.51) | 115 (1.43) | 20 (2.17) | ||
| ≥ 18.5, < 25 | 2387 (26.69) | 2079 (25.91) | 308 (33.41) | ||
| ≥ 25, < 30 | 3044 (34.03) | 2741 (34.16) | 303 (32.86) | ||
| ≥ 30 | 3379 (37.78) | 3088 (38.49) | 291 (31.56) | ||
| Smoking status | χ2 = 15.702 | < 0.001 | |||
| Never smokers | 4702 (52.57) | 4182 (52.13) | 520 (56.40) | ||
| Former smokers | 2245 (25.10) | 2063 (25.71) | 182 (19.74) | ||
| Current smokers | 1998 (22.34) | 1778 (22.16) | 220 (23.86) | ||
| Drinking status | χ2 = 39.879 | < 0.001 | |||
| NO | 2419 (27.04) | 2089 (26.04) | 330 (35.79) | ||
| YES | 6526 (72.96) | 5934 (73.96) | 592 (64.21) | ||
| Hypertension | χ2 = 8.561 | 0.003 | |||
| NO | 5770 (64.51) | 5135 (64.00) | 635 (68.87) | ||
| YES | 3175 (35.49) | 2888 (36.00) | 287 (31.13) | ||
| Diabetes | χ2 = 0.425 | 0.514 | |||
| NO | 7738 (86.51) | 6934 (86.43) | 804 (87.20) | ||
| YES | 1207 (13.49) | 1089 (13.57) | 118 (12.80) | ||
| Congestive heart failure | χ2 = 0.717 | 0.397 | |||
| NO | 8684 (97.08) | 7793 (97.13) | 891 (96.64) | ||
| YES | 261 (2.92) | 230 (2.87) | 31 (3.36) | ||
| Myocardial infarction | χ2 = 0.022 | 0.880 | |||
| NO | 8575 (95.86) | 7692 (95.87) | 883 (95.77) | ||
| YES | 370 (4.14) | 331 (4.13) | 39 (4.23) | ||
| Stroke | χ2 = 3.600 | 0.058 | |||
| NO | 8626 (96.43) | 7747 (96.56) | 879 (95.34) | ||
| YES | 319 (3.57) | 276 (3.44) | 43 (4.66) | ||
| Emphysema | χ2 = 0.847 | 0.357 | |||
| NO | 8723 (97.52) | 7828 (97.57) | 895 (97.07) | ||
| YES | 222 (2.48) | 195 (2.43) | 27 (2.93) | ||
| Cancer | χ2 = 0.049 | 0.825 | |||
| NO | 8090 (90.44) | 7258 (90.46) | 832 (90.24) | ||
| YES | 855 (9.56) | 765 (9.54) | 90 (9.76) | ||
| Chronic bronchitis | χ2 = 1.246 | 0.264 | |||
| NO | 8426 (94.20) | 7565 (94.29) | 861 (93.38) | ||
| YES | 519 (5.80) | 458 (5.71) | 61 (6.62) | ||
| Total energy intake | χ2 = 47.197 | < 0.001 | |||
| Q1(164–1,409 kcal/day) | 2228 (24.91) | 1927 (24.02) | 301 (32.65) | ||
| Q2(1,409.1–1,909 kcal/day) | 2241 (25.05) | 2000 (24.93) | 241 (26.14) | ||
| Q3(1,909.1–2,582 kcal/day) | 2239 (25.03) | 2024 (25.23) | 215 (23.32) | ||
| Q4(2,582.1–13,509 kcal/day) | 2237 (25.01) | 2072 (25.83) | 165 (17.90) | ||
| Total protein intake | χ2 = 55.340 | < 0.001 | |||
| Q1(0.63–51.72 g/day) | 2236 (25.00) | 1935 (24.12) | 301 (32.65) | ||
| Q2(51.74–72.77 g/day) | 2233 (24.96) | 1983 (24.72) | 250 (27.11) | ||
| Q3(72.78–99.94 g/day) | 2237 (25.01) | 2020 (25.18) | 217 (23.54) | ||
| Q4(99.95–474.01 g/day) | 2239 (25.03) | 2085 (25.99) | 154 (16.70) | ||
| Total fiber intake | χ2 = 79.304 | < 0.001 | |||
| Q1(0.1–9.1 g/day) | 2213 (24.74) | 1891 (23.57) | 322 (34.92) | ||
| Q2(9.2–14 g/day) | 2228 (24.91) | 1988 (24.78) | 240 (26.03) | ||
| Q3(14.1–20.5 g/day) | 2257 (25.23) | 2045 (25.49) | 212 (22.99) | ||
| Q4(20.6–147.6 g/day) | 2247 (25.12) | 2099 (26.16) | 148 (16.05) | ||
| Total fat intake | χ2 = 40.271 | < 0.001 | |||
| Q1(0.2–45.8 g/day) | 2236 (25.00) | 1940 (24.18) | 296 (32.10) | ||
| Q2(45.81–69.45 g/day) | 2235 (24.99) | 1996 (24.88) | 239 (25.92) | ||
| Q3(69.46–100.3 g/day) | 2236 (25.00) | 2018 (25.15) | 218 (23.64) | ||
| Q4(100.34–601.33 g/day) | 2238 (25.02) | 2069 (25.79) | 169 (18.33) | ||
| Anxiety status | χ2 = 31.832 | < 0.001 | |||
| NO | 6574(73.5) | 5968 (74.4) | 606 (65.7) | ||
| YES | 2371(26.5) | 2055 (25.6) | 316 (34.3) | ||
| Anxiety duration | χ2 = 34.360 | < 0.001 | |||
| = 0 | 3906 (43.67) | 3558 (44.35) | 348 (37.74) | ||
| > 0, ≤ 10 | 3412 (38.14) | 3068 (38.24) | 344 (37.31) | ||
| > 10, ≤ 20 | 658 (7.36) | 567 (7.07) | 91 (9.87) | ||
| > 20, ≤ 30 | 969 (10.83) | 830 (10.35) | 139 (15.08) | ||
Note: Continuous variables are presented as mean ± standard deviation (SD) or median (interquartile range), and categorical variables are presented as n (%); χ2 test for categorical variables.; T-test for continuous variables. P-values in bold indicate statistical significance
Abbreviations: BMI, body mass index; PIR, family income to poverty ratio
Among the 8945 participants, 922 individuals were identified as having constipation. These individuals were more likely to be female (N = 633, 68.66%), non-Hispanic White (N = 426, 46.20%), have a college or above education level (N = 376, 40.78%), have a lower poverty income ratio (N = 368, 39.91%), and to have never smoked (N = 520, 56.40%). They were also more likely to be drinkers (N = 592, 64.21%), non-hypertensive (N = 635, 68.87%), non-diabetic (N = 804, 87.20%), and non-heart failure (N = 891, 96.64%), non-myocardial infarction (N = 883, 95.77%), non-stroke (N = 879, 95.34%), non-emphysema (N = 895, 97.07%), or non-cancer (N = 832, 90.24%). Additionally, individuals with constipation had significantly lower daily intake levels of energy, protein, fiber, and fat (P < 0.05).
Association of anxiety status and anxiety duration with constipation
Table 2. The variables age, gender, education, marital status, PIR, BMI, drinking status, hypertension, total energy consumption in diet, protein, fat, and dietary fiber were found to have a significant association with constipation in the univariate analyses (all p < 0.05). Women exhibited a significantly higher risk of constipation compared to men (OR: 2.38, 95% CI: 2.06–2.75, P < 0.0001).
Table 2.
Association between variables and constipation, based on univariate analysis
| OR (95 CI) | P-value | |
|---|---|---|
| Age | ||
| ≥ 20,<40 | Ref | Ref |
| ≥ 40, < 60 | 0.81 (0.69, 0.95) | 0.0101 |
| ≥ 60 | 0.69 (0.59, 0.82) | < 0.0001 |
| Sex | ||
| male | Ref | Ref |
| female | 2.38 (2.06, 2.75) | < 0.0001 |
| Race/ethnicity | ||
| Mexican American | Ref | Ref |
| Other Hispanic | 1.41 (1.08, 1.84) | 0.0115 |
| Non-Hispanic White | 1.06 (0.86, 1.29) | 0.5894 |
| Non-Hispanic Black | 1.48 (1.18, 1.86) | 0.0006 |
| Other Race | 1.00 (0.67, 1.48) | 0.9813 |
| Education | ||
| Below high school | Ref | Ref |
| High school graduate | 1.04 (0.87, 1.24) | 0.6813 |
| College or above | 0.71 (0.61, 0.84) | < 0.0001 |
| Marital status | ||
| Others | Ref | Ref |
| Currently married/living with partner | 0.78 (0.68, 0.89) | 0.0004 |
| PIR | ||
| < 1.3 | Ref | Ref |
| ≥ 1.3, < 3.5 | 0.74 (0.63, 0.87) | 0.0002 |
| ≥ 3.5 | 0.51 (0.42, 0.61) | < 0.0001 |
| BMI | ||
| < 18.5 | Ref | Ref |
| ≥ 18.5, < 25 | 0.85 (0.52, 1.39) | 0.5210 |
| ≥ 25, < 30 | 0.64 (0.39, 1.04) | 0.0696 |
| ≥ 30 | 0.54 (0.33, 0.88) | 0.0142 |
| Smoking status | ||
| Never smokers | Ref | Ref |
| Former smokers | 0.71 (0.59, 0.85) | 0.0001 |
| Current smokers | 1.00 (0.84, 1.18) | 0.9542 |
| Drinking status | ||
| NO | Ref | Ref |
| YES | 0.63 (0.55, 0.73) | < 0.0001 |
| Hypertension | ||
| NO | Ref | Ref |
| YES | 0.80 (0.69, 0.93) | 0.0035 |
| Diabetes | ||
| NO | Ref | Ref |
| YES | 0.93 (0.76, 1.15) | 0.5141 |
| Congestive heart failure | ||
| NO | Ref | Ref |
| YES | 1.18 (0.81, 1.73) | 0.3977 |
| Myocardial infarction | ||
| NO | Ref | Ref |
| YES | 1.03 (0.73, 1.44) | 0.8803 |
| Stroke | ||
| NO | Ref | Ref |
| YES | 1.37 (0.99, 1.91) | 0.0588 |
| Emphysema | ||
| NO | Ref | Ref |
| YES | 1.21 (0.81, 1.82) | 0.3581 |
| Cancer | ||
| NO | Ref | Ref |
| YES | 1.03 (0.82, 1.29) | 0.8248 |
| Chronic bronchitis | ||
| NO | Ref | Ref |
| YES | 1.17 (0.89, 1.54) | 0.2648 |
| Total energy intake | ||
| Q1(164–1,409 kcal/day) | Ref | Ref |
| Q2(1,409.1–1,909 kcal/day) | 0.77 (0.64, 0.92) | 0.0049 |
| Q3(1,909.1–2,582 kcal/day) | 0.68 (0.56, 0.82) | < 0.0001 |
| Q4(2,582.1–13,509 kcal/day) | 0.51 (0.42, 0.62) | < 0.0001 |
| Total protein intake | ||
| Q1(0.63–51.72 g/day) | Ref | Ref |
| Q2(51.74–72.77 g/day) | 0.81 (0.68, 0.97) | 0.0214 |
| Q3(72.78–99.94 g/day) | 0.69 (0.57, 0.83) | < 0.0001 |
| Q4(99.95–474.01 g/day) | 0.47 (0.39, 0.58) | < 0.0001 |
| Total fiber intake | ||
| Q1(0.1–9.1 g/day) | Ref | Ref |
| Q2(9.2–14 g/day) | 0.71 (0.59, 0.85) | 0.0002 |
| Q3(14.1–20.5 g/day) | 0.61 (0.51, 0.73) | < 0.0001 |
| Q4(20.6–147.6 g/day) | 0.41 (0.34, 0.51) | < 0.0001 |
| Total fat intake | ||
| Q1(0.2–45.8 g/day) | Ref | Ref |
| Q2(45.81–69.45 g/day) | 0.78 (0.65, 0.94) | 0.0089 |
| Q3(69.46–100.3 g/day) | 0.71 (0.59, 0.85) | 0.0003 |
| Q4(100.34–601.33 g/day) | 0.54 (0.44, 0.65) | < 0.0001 |
| Anxiety status | ||
| NO | Ref | Ref |
| YES | 1.51 (1.31, 1.75) | < 0.0001 |
| Anxiety duration | ||
| = 0 | Ref | Ref |
| > 0, ≤ 10 | 1.15 (0.98, 1.34) | 0.0874 |
| > 10, ≤ 20 | 1.64 (1.28, 2.10) | < 0.0001 |
| > 20, ≤ 30 | 1.71 (1.39, 2.11) | < 0.0001 |
Note: P-values in bold indicate statistical significance
Abbreviations: BMI, body mass index; PIR, family income to poverty ratio; OR, odd ratio; CI, confidence interval
Table 3 displays the results of the logistic regression analysis examining the relationship between anxiety status and constipation. In the unadjusted model, individuals with anxiety status demonstrated a higher likelihood of experiencing constipation compared to those without anxiety status (OR: 1.29, 95% CI: 1.15–1.44, P < 0.0001). After adjusting for gender, age, and ethnicity (Model I), the association remained significant, and individuals with anxiety status exhibited an elevated risk of constipation (OR: 1.34, 95% CI: 1.16–1.56, P < 0.0001).
Table 3.
Multivariable regression analysis of the relationship between anxiety status and constipation
| Anxiety status | Non-adjusted | Model I | Model II | |||
|---|---|---|---|---|---|---|
| OR (95CI) | p-value | OR (95CI) | p-value | OR (95CI) | p-value | |
| NO | Ref | Ref | Ref | |||
| YES | 1.29 (1.15, 1.44) | < 0.0001 | 1.34 (1.16, 1.56) | < 0.0001 | 1.49 (1.28, 1.73) | < 0.0001 |
Note: Model I: accounted for gender, age, and ethnicity. Model II: further accounted for education level, marital status, PIR, BMI, smoking status, alcohol consumption status, and chronic diseases (hypertension, diabetes mellitus, congestive heart failure, myocardial infarction, stroke, emphysema, chronic bronchitis, and cancer), as well as dietary intake (energy, protein, fat, dietary fiber). P-values in bold indicate statistical significance
Abbreviations: OR, odd ratio; CI, confidence interval
In the fully adjusted model (Model II), which accounted for additional covariates such as education level, marital status, PIR, BMI, smoking status, alcohol consumption, chronic diseases, and dietary intake, individuals with anxiety status were associated with a substantially higher likelihood of experiencing constipation (OR: 1.49, 95% CI: 1.28–1.73, P < 0.0001).
Table 4 illustrates the results of the logistic regression analysis examining the relationship between anxiety duration and constipation.
Table 4.
Multivariable regression analysis of the relationship between anxiety duration and constipation
| Anxiety duration | Non-adjusted | Model I | Model II | |||
|---|---|---|---|---|---|---|
| OR (95CI) | p-value | OR (95CI) | p-value | OR (95CI) | p-value | |
| = 0 | Ref | Ref | Ref | |||
| > 0, <=10 | 1.11 (0.98, 1.26) | 0.0937 | 0.97 (0.85, 1.10) | 0.6303 | 1.17 (1.03, 1.33) | 0.0180 |
| > 10, <=20 | 1.62 (1.33, 1.97) | < 0.0001 | 1.32 (1.08, 1.62) | 0.0071 | 1.68 (1.37, 2.05) | < 0.0001 |
| > 20, <=30 | 1.71 (1.44, 2.02) | < 0.0001 | 1.43 (1.21, 1.70) | < 0.0001 | 1.67 (1.40, 2.00) | < 0.0001 |
Note: Model I: accounted for gender, age, and ethnicity. Model II: further accounted for education level, marital status, PIR, BMI, smoking status, alcohol consumption status, and chronic diseases (hypertension, diabetes mellitus, congestive heart failure, myocardial infarction, stroke, emphysema, chronic bronchitis, and cancer), as well as dietary intake (energy, protein, fat, dietary fiber). P-values in bold indicate statistical significance
Abbreviations: OR, odd ratio; CI, confidence interval
In the unadjusted model, individuals with 1–10 days of anxiety demonstrated a modest, non-statistically significant association with constipation (OR: 1.11, 95% CI: 0.98–1.26, P = 0.0937). For individuals with 11–20 days of anxiety, the likelihood of experiencing constipation was higher (OR: 1.62, 95% CI: 1.33–1.97, P < 0.0001), and those with 21–30 days of anxiety showed a similar elevated likelihood (OR: 1.71, 95% CI: 1.44–2.02, P < 0.0001).
After adjusting for sex, age, and race (Model I), the association between anxiety duration and constipation remained significant for individuals with 11–20 days (OR: 1.32, 95% CI: 1.08–1.62, P = 0.0071) and 21–30 days of anxiety (OR: 1.43, 95% CI: 1.21–1.70, P < 0.0001), while no significant association was observed for individuals with 1–10 days of anxiety (OR: 0.97, 95% CI: 0.85–1.10, P = 0.6303).
In the fully adjusted model (Model II), which accounted for additional education level, marital status, PIR, BMI, smoking status, alcohol consumption, chronic diseases, and dietary intake, a stronger association emerged. Individuals with 1–10 days of anxiety were modestly associated with constipation (OR: 1.17, 95% CI: 1.03–1.33, P = 0.0180). For individuals with 11–20 days of anxiety, the association was more pronounced (OR: 1.68, 95% CI: 1.37–2.05, P < 0.0001), and those with 21–30 days of anxiety exhibited a similarly increased likelihood of constipation (OR: 1.67, 95% CI: 1.40–2.00, P < 0.0001).
Stratified analysis of anxiety status and constipation
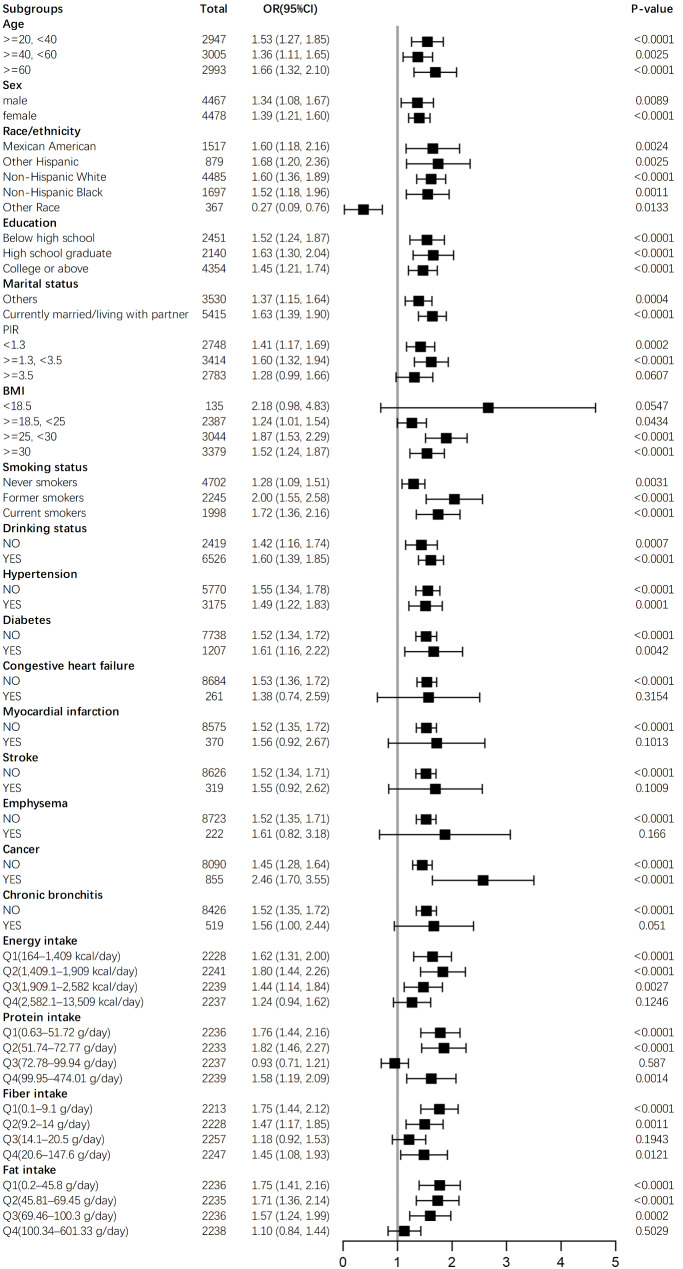
Figure 2 illustrates the stratified analysis, accounting for gender, age, race/ethnicity, education level, marital status, PIR, BMI, smoking status, drinking status, hypertension, diabetes, congestive heart failure, myocardial infarction, stroke, emphysema, chronic bronchitis, cancer, and dietary intake of energy, protein, fat, and fiber. The results indicate that the association between anxiety status and constipation remains relatively stable across different stratification levels.
Fig. 2.
A stratified analysis of the impact of anxiety status on constipation (N = 8945)
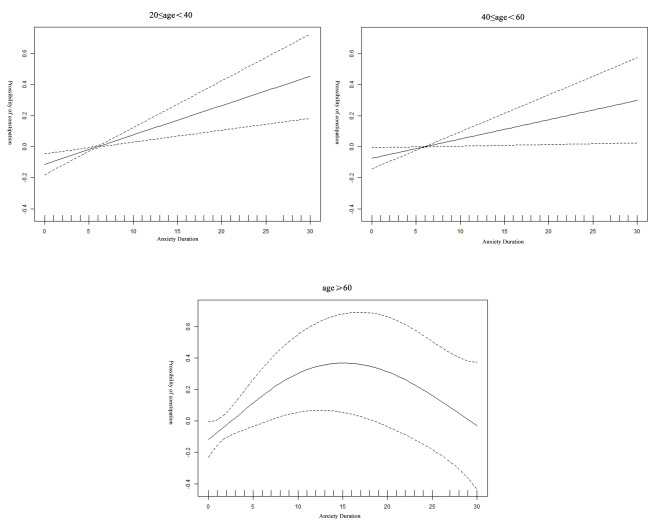
Smoothed curve fitting and threshold effect analysis at different ages in adults
Smooth curve fitting was used to examine the association between anxiety duration and the risk of constipation at different ages in adults. As illustrated in Fig. 3, a linear relationship was observed between anxiety duration and constipation risk in individuals aged 20 to 60. In contrast, for individuals aged 60 and above, the association followed a non-linear pattern, resembling an inverted U-shape.
Fig. 3.
Generalized additive model and Smoothed curve fitting of the association between duration of anxiety and risk of constipation at different ages in adults, NHANES 2007–2010. Notes: The data were adjusted for gender, race/ethnicity, education level, marital status, PIR, BMI, smoking status, drinking status, chronic diseases (hypertension, diabetes mellitus, congestive heart failure, myocardial infarction, stroke, emphysema, chronic bronchitis, and cancer), and dietary intake (energy, protein, fat, dietary fiber)
Table 5 presents the results of the threshold effect analysis using a two-piecewise linear regression model. This analysis showed that the risk of constipation increased linearly with anxiety duration in both the 20 to 40 and 40 to 60 age groups. Specifically, for each additional day of anxiety duration, the risk of constipation increased by 2% in the 20 to 40 age group (OR: 1.02, 95% CI: 1.01–1.03, P < 0.0001) and by 1% in the 40 to 60 age group (OR: 1.01, 95% CI: 1.00–1.02, P = 0.0028).
Table 5.
The threshold effect analysis of the association between anxiety duration and constipation at different ages
| 20 ≤ age < 40 | 40 ≤ age < 60 | age ≥ 60 | |
|---|---|---|---|
| OR (95% CI), p-value | OR (95% CI), p-value | OR (95% CI), p-value | |
| Fitting by the standard linear model | |||
| 1.02 (1.01, 1.03) < 0.0001 | 1.01 (1.00, 1.02) 0.0028 | 1.01 (1.00, 1.02) 0.1639 | |
| Fitting by the two-piecewise linear model | |||
| Inflection point(K) | 0 | 10 | 10 |
| < K | NA | 1.00 (0.96, 1.03) 0.8159 | 1.06 (1.02, 1.10) 0.0019 |
| > K | 1.02 (1.01, 1.03) < 0.0001 | 1.02 (1.00, 1.04) 0.0134 | 0.98 (0.96, 1.00) 0.0925 |
| P for log-likelihood ratio | 1.000 | 0.258 | 0.006 |
Notes: Gender, race/ethnicity, educational attainment, marital status, PIR, BMI, smoking, drinking status, chronic disease, and dietary factors were adjusted
Abbreviations: OR, odd ratio; CI, confidence interval
Furthermore, the threshold analysis identified a significant change in the relationship between anxiety duration and constipation risk at 60 years of age. Specifically, an inflection point was observed at 10 days of anxiety duration. For individuals with less than 10 days of anxiety, the risk of constipation increased positively with anxiety duration (OR: 1.06, 95% CI: 1.02–1.10, P = 0.0019). However, for individuals with more than 10 days of anxiety, the association was no longer statistically significant (OR: 0.98, 95% CI: 0.96–1.00, P = 0.0925). The log-likelihood ratio test indicated a significant change in the association, with a P value of 0.006.
Discussion
This study explored the relationships of anxiety status and anxiety duration with constipation using data from the NHANES database, a large and nationally representative sample of the US population.
The results indicate that after adjusting for confounding factors such as gender, age, ethnicity, education level, marital status, chronic diseases, and dietary intake, anxiety status was significantly associated with an increased risk of constipation (OR: 1.49, 95% CI: 1.28–1.73). Hanna-Jairala et al. found that the relationship between anxiety status and constipation may be closely associated with dysfunction of the gut-brain axis [46]. The relationship between anxiety status and constipation is inherently bidirectional, influenced by an interplay of biological, psychological, and behavioral factors. Anxiety, as a mental health condition, can exacerbate constipation through activation of the hypothalamic-pituitary-adrenal (HPA) axis, increased corticotropin-releasing factor (CRF) secretion, and altered serotonergic signaling [17, 47]. These mechanisms impair gastrointestinal motility, leading to delayed colonic transit and exacerbated constipation symptoms [48]. Conversely, constipation may amplify psychological distress by reducing quality of life and inducing chronic stress, thereby perpetuating a cycle of dysfunction [15].
Beyond these physiological pathways, individuals with anxiety may engage in maladaptive behaviors, such as avoiding social activities or imposing dietary restrictions, which could indirectly affect bowel habits [49, 50].
To further investigate the potential relationship between anxiety and constipation, anxiety duration was categorized into four groups based on the number of self-reported anxious days: 0 days, 1–10 days, 11–20 days, and 21–30 days. The results revealed that, after adjusting for confounding factors such as gender, age, ethnicity, education level, marital status, chronic diseases, and dietary intake, a significant association was observed between anxiety duration of 1–30 days and constipation (all P < 0.05).
A study based on a North American population found that the prevalence of constipation is closely associated with age, with a progressive increase observed among older adults [51]. Furthermore, the review highlighted that the literature on age-related differences in the characteristics of constipation is both sparse and inconsistent, underscoring the need for further research to explore the relationship between constipation and different age groups.
Based on previous studies, we categorized age into three groups: 20–39 years, 40–59 years, and 60 years and older [41]. Anxiety duration was treated as a continuous variable for smooth curve fitting and threshold effect analysis to explore whether the cumulative impact of anxiety duration on constipation risk varies across age groups.
The results showed that after controlling for multiple confounding factors, a significant positive linear relationship was observed between anxiety duration and constipation risk among U.S. adults aged 20–60 years. However, in individuals aged 60 years and older, the relationship was non-linear, exhibiting an inverted U-shaped pattern with a threshold effect at 10 days of anxiety duration. Below this threshold, anxiety duration was positively associated with constipation risk, but the association became statistically insignificant beyond the threshold. These findings highlight the complex nature of the relationship between anxiety and constipation, particularly in older populations.
The curvilinear pattern observed among individuals aged 60 years and above suggests a threshold effect, possibly influenced by physiological changes associated with aging. Research has shown that older adults often experience decreased gut motility, reduced digestive enzyme activity, dysbiosis, decreased resilience of the enteric nervous system, and impaired intestinal barrier function [52, 53]. These factors make older individuals more susceptible to short-term disruptions caused by anxiety, which could explain the noticeable increase in constipation risk observed with a short duration of anxiety (1–10 days).
However, for older individuals experiencing longer durations of anxiety, the relationship with constipation appears to level off or even weaken. Studies have shown that the pathophysiological mechanisms of anxiety and depression differ between younger and older populations [54]. In older adults, chronic exposure to anxiety may induce neuroplastic changes, potentially dampening acute stress responses that exacerbate gastrointestinal dysfunction, thereby mitigating the long-term impact of anxiety on gastrointestinal function [55–57].
In addition, hypertension is closely linked to both anxiety and constipation. A study based on Hispanic/Latino adults demonstrated that anxiety status is closely associated with the incidence of hypertension, with anxiety often accelerating the progression of hypertension through mechanisms involving interleukin-6 (IL-6), interleukin-17 (IL-17), and reactive oxygen species (ROS) [58, 59]. Moreover, research suggests that hypertension often leads to sympathetic hyperactivity, which may reduce colonic motility and subsequently contribute to constipation [60]. A study of older Australian patients found that individuals with constipation had a significantly higher risk for hypertension (OR:1.96, 95% CI:1.94–1.99, P < 0.001) [61]. Therefore, we treated hypertension as a significant confounding factor and conducted stratified analyses. The results indicated that the association between anxiety status and constipation remained relatively stable across hypertensive and non-hypertensive populations.
Dietary factors are widely recognized as being closely associated with the development of constipation. A study by Yang et al. found that moderate energy intake was associated with a decreased risk of constipation (OR: 0.5, 95% CI: 0.29–0.84), whereas lower-middle energy intake was linked to an increased risk of constipation (OR: 1.56, 95% CI: 1.15–2.13) [22]. Similarly, Hong et al. reported that in men, higher protein intake was significantly associated with a lower risk of constipation. In contrast, in women, higher protein intake was correlated with an increased risk of constipation [23]. Moreover, studies have demonstrated that the intake of fat and fiber is closely related to constipation risk [24, 25]. As a result, dietary factors were treated as important confounding variables and included in stratified analyses. The results indicate that the association between anxiety status and constipation remains relatively stable across different dietary intake levels.
Numerous studies have investigated the relationship between anxiety and the risk of constipation; however, the findings remain controversial. A cross-sectional study conducted in a Hong Kong population found that anxiety and depression scores were significantly higher in patients with constipation compared to healthy participants (P < 0.0001) [62]. In contrast, a study by Deng et al. reported that anxiety disorders did not increase the risk of constipation [63]. Additionally, three other studies have indicated that patients with anxiety and related emotional disorders are more likely to experience comorbid constipation [64–66].
This study has several limitations. As a cross-sectional investigation, it was not possible to establish a causal relationship between anxiety duration and constipation. Additionally, the measurement of anxiety duration relied exclusively on participants’ self-reported data collected through the NHANES questionnaire. Notably, this questionnaire does not utilize validated screening tools, such as the GAD-7, which are specifically designed to detect and assess anxiety. As a result, the findings cannot be used to diagnose clinical anxiety disorders. Moreover, while this study defined constipation based on stool frequency and characteristics in accordance with prior research, it did not assess whether participants met the Rome criteria for constipation, which represents the clinical diagnostic standard.
Conclusions
This study found a significant association between anxiety status and constipation among U.S. adults. Additionally, an age-dependent association between anxiety duration and constipation was observed, particularly among individuals aged 60 and older. This provides new insights into the relationship between anxiety duration and the onset of constipation. Furthermore, additional prospective studies are needed to establish the causal link between anxiety and constipation, as well as to identify individuals with constipation early for more effective treatment.
Acknowledgements
The authors want to acknowledge the participants and investigators of the NHANES datasets analyzed in this study, for sharing them publicly for research.
Abbreviations
- NHANES
National Health and Nutrition Examination Survey
- NCHS
National Center for Health Statistics
- CDC
Centers for Disease Control
- MECs
Mobile examination centers
- HSQ
Health Status Questionnaire
- PIR
Poverty income ratio
- BMI
Body mass index
- CNS
Central nervous system
- ENS
Enteric nervous system
- ANS
Autonomic nervous system
- HPA
Hypothalamic-pituitary-adrenal
- NDRIs
Norepinephrine-dopamine reuptake inhibitors
- CRF
Corticotropin-releasing factor
- ACTH
Adrenocorticotropic hormone
- SCFAs
Short-chain fatty acids
- CRF1
Corticotropin-releasing factor 1
- 5-HT
5-Hydroxy tryptamine
- HRQoL
Health-Related Quality of Life
- IL-6
Interleukin-6
- IL-17
Interleukin-17
- ROS
Reactive oxygen species
- OR
Odds ratio
- CI
Confidence interval
Author contributions
Xinran Li: Writing – original draft, Writing – review & editing, Visualization, Validation, Software, Resources, Methodology, Investi-gation, Formal analysis, Data curation, Conceptualization. Conghui Bian: Writing – review & editing, Conceptualization, Methodology, Data curation, Software, Methodology, Resources. Hui Dai: Visualization, Investigation, Resources, Data curation. Xingrui Chen: Methodology, Investigation, Formal analysis, Data curation. Dan Zhang and Haihua Qian: Writing – review & editing, Supervision, Project administration, Meth-odology, Funding acquisition. All authors read and approved the final manuscript.
Funding
This study was funded by National Natural Science Foundation of China (grant number:82374456, 82274514, 82074439).
Data availability
All data used in this study is available in NHANES database. You can find this data at the following link: NHANES (https://www.cdc.gov/nchs/nhanes/index.htm).
Declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the NCHS Institutional Review Board. Written informed consent was obtained from all subjects/patients.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Haihua Qian, Email: haihuaqian@126.com.
Dan Zhang, Email: danaezhang@163.com.
References
- 1.Irvine EJ, Ferrazzi S, Pare P, Thompson WG, Rance L. Health-related quality of life in functional GI disorders: focus on constipation and resource utilization. Am J Gastroenterol. 2002;97(8):1986–93. [DOI] [PubMed] [Google Scholar]
- 2.Bharucha AE, Lacy BE. Mechanisms, evaluation, and management of chronic constipation. Gastroenterology. 2020;158(5):1232–e12491233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(9):1582–91. quiz 1581, 1592. [DOI] [PubMed] [Google Scholar]
- 4.Martin BC, Barghout V, Cerulli A. Direct medical costs of constipation in the United States. Manag Care Interface. 2006;19(12):43–9. [PubMed] [Google Scholar]
- 5.Aziz I, Whitehead WE, Palsson OS, Törnblom H, Simrén M. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Rev Gastroenterol Hepatol. 2020;14(1):39–46. [DOI] [PubMed] [Google Scholar]
- 6.Liu X, Liu Y, Shu Y, Tao H, Sheng Z, Peng Y, Cai M, Zhang X, Lan W. Association between dietary vitamin B6 intake and constipation: a population-based study. Front Nutr. 2024;11:1483515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johanson JF, Kralstein J. Chronic constipation: a survey of the patient perspective. Aliment Pharmacol Ther. 2007;25(5):599–608. [DOI] [PubMed] [Google Scholar]
- 8.Kawamura Y, Yamamoto S, Funaki Y, Ohashi W, Yamamoto K, Ozeki T, Yamaguchi Y, Tamura Y, Izawa S, Hijikata Y, et al. Internet survey on the actual situation of constipation in the Japanese population under 70 years old: focus on functional constipation and constipation-predominant irritable bowel syndrome. J Gastroenterol. 2020;55(1):27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li N, Wang Q, Wang Y, Sun A, Lin Y, Jin Y, Li X. Fecal microbiota transplantation from chronic unpredictable mild stress mice donors affects anxiety-like and depression-like behavior in recipient mice via the gut microbiota-inflammation-brain axis. Stress. 2019;22(5):592–602. [DOI] [PubMed] [Google Scholar]
- 10.Ruscio AM, Hallion LS, Lim CCW, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Andrade LH, Borges G, Bromet EJ, Bunting B, et al. Cross-sectional comparison of the epidemiology of DSM-5 Generalized Anxiety Disorder across the Globe. JAMA Psychiatry. 2017;74(5):465–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park SC, Kim YK. Anxiety disorders in the DSM-5: changes, controversies, and future directions. Adv Exp Med Biol. 2020;1191:187–96. [DOI] [PubMed] [Google Scholar]
- 12.First MB. Diagnostic and statistical manual of mental disorders, 5th edition, and clinical utility. J Nerv Ment Dis 2013, 201(9):727–729. [DOI] [PubMed]
- 13.Li G, Lv T, Jin B, Fan Z. The role of repetitive transcranial magnetic stimulation therapy in functional bowel disease. Front Med (Lausanne). 2023;10:1249672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Vadder F, Plessier F, Gautier-Stein A, Mithieux G. Vasoactive intestinal peptide is a local mediator in a gut-brain neural axis activating intestinal gluconeogenesis. Neurogastroenterol Motil. 2015;27(3):443–8. [DOI] [PubMed] [Google Scholar]
- 15.Koloski NA, Jones M, Kalantar J, Weltman M, Zaguirre J, Talley NJ. The brain–gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut. 2012;61(9):1284–90. [DOI] [PubMed] [Google Scholar]
- 16.Stengel A, Taché Y. Neuroendocrine control of the gut during stress: corticotropin-releasing factor signaling pathways in the spotlight. Annu Rev Physiol. 2009;71:219–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Binder EB, Nemeroff CB. The CRF system, stress, depression and anxiety-insights from human genetic studies. Mol Psychiatry. 2010;15(6):574–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 2015;28(2):203–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Morys J, Małecki A, Nowacka-Chmielewska M. Stress and the gut-brain axis: an inflammatory perspective. Front Mol Neurosci. 2024;17:1415567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li H, Lv N, Li D, Qian Y, Si X, Hua Y, Wang Y, Han X, Xu T. Tongbian decoction restores intestinal microbiota and activates 5-hydroxytryptamine signaling: implication in slow transit constipation. Front Microbiol. 2023;14:1296163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Avramidou M, Angst F, Angst J, Aeschlimann A, Rössler W, Schnyder U. Epidemiology of gastrointestinal symptoms in young and middle-aged Swiss adults: prevalences and comorbidities in a longitudinal population cohort over 28 years. BMC Gastroenterol. 2018;18(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang S, Wu XL, Wang SQ, Guo XL, Guo FZ, Sun XF. Association of Dietary Energy Intake with Constipation among men and women: results from the National Health and Nutrition Examination Survey. Front Nutr. 2022;9:856138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hong Y, Shen H, Chen X, Li G. Gender differences in the association between dietary protein intake and constipation: findings from NHANES. Front Nutr. 2024;11:1393596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taba Taba Vakili S, Nezami BG, Shetty A, Chetty VK, Srinivasan S. Association of high dietary saturated fat intake and uncontrolled diabetes with constipation: evidence from the National Health and Nutrition Examination Survey. Neurogastroenterol Motil. 2015;27(10):1389–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y, Tong WD, Qian Y. Effect of physical activity on the Association between Dietary Fiber and Constipation: evidence from the National Health and Nutrition Examination Survey 2005–2010. J Neurogastroenterol Motil. 2021;27(1):97–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng T, Camargo Tavares L, D’Amato M, Marques FZ. Constipation is associated with an increased risk of major adverse cardiac events in a UK population. Am J Physiol Heart Circ Physiol. 2024;327(4):H956–64. [DOI] [PubMed] [Google Scholar]
- 27.Ito H, Shibuya M, Iwami R, Ina H, Okawa M, Miura IC, Matsumoto S, Inoue S, Antoku H. S : Deterioration of the defecation status after hospitalization in patients with type 2 diabetes is Associated with Albuminuria Rather than Diabetic Neuropathy. Intern Med 2024. [DOI] [PMC free article] [PubMed]
- 28.Ishiyama Y, Hoshide S, Mizuno H, Kario K. Constipation-induced pressor effects as triggers for cardiovascular events. J Clin Hypertens (Greenwich). 2019;21(3):421–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang KY, Yu ZZ, Tu JJ, Tang XY, Huang JM, Lu TM, Lu YQ, Huang MC, Zhou J, Maier AB, et al. Positive association between constipation and mild cognitive impairment in elders: a cross-sectional study. Med (Baltim). 2024;103(40):e39943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuan Y, Qiu L, Li ZY, Zhang L, Xu T, Lang JH, Li ZA, Gong J, Liu Q, Liu XC, et al. An epidemiology study of fecal incontinence in adult Chinese women living in urban areas. Chin Med J (Engl). 2020;133(3):262–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dang Y, He X, Liu X, Wang Y, Geng S, Cheng Y, Ma H, Zhao X. Causal associations between constipation and pan-cancer: a bidirectional mendelian randomization study. Front Oncol. 2024;14:1428003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kang Y, Yan J. Exploring the connection between caffeine intake and constipation: a cross-sectional study using national health and nutrition examination survey data. BMC Public Health. 2024;24(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yang C, Hong Q, Wu T, Fan Y, Shen X, Dong X. Association between Dietary Intake of live microbes and chronic constipation in adults. J Nutr. 2024;154(2):526–34. [DOI] [PubMed] [Google Scholar]
- 34.Duan R, Zheng Y, Kong W, Wang Y, Zhou Y. Association of environmental tobacco smoke exposure with chronic constipation: a nationwide survey (NHANES 2005–2010). Environ Sci Pollut Res Int. 2023;30(54):115776–87. [DOI] [PubMed] [Google Scholar]
- 35.Wang Y, Shen X, Wang P. Constipation is associated with depression of any severity, but not with suicidal ideation: insights from a large cross-sectional study. Int J Colorectal Dis. 2023;38(1):231. [DOI] [PubMed] [Google Scholar]
- 36.Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57(5):339–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dantzer JA, Keet CA. Anxiety associated with food allergy in adults and adolescents: an analysis of data from the National Health and Nutrition Examination Survey (NHANES) 2007–2010. J Allergy Clin Immunol Pract. 2020;8(5):1743–e17461745. [DOI] [PubMed] [Google Scholar]
- 38.Bai L, Wen Z, Zhu Y, Jama HA, Sawmadal JD, Chen J. Association of blood cadmium, lead, and mercury with anxiety: a cross-sectional study from NHANES 2007–2012. Front Public Health. 2024;12:1402715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Li X, Chan VKY, Luo H, Chan SSM, Wong GHY, Wong ICK, Lum TYS. Depression duration and risk of incident cardiovascular disease: a population-based six-year cohort study. J Affect Disord. 2022;305:188–95. [DOI] [PubMed] [Google Scholar]
- 40.Ballou S, Katon J, Singh P, Rangan V, Lee HN, McMahon C, Iturrino J, Lembo A, Nee J. Chronic diarrhea and constipation are more common in depressed individuals. Clin Gastroenterol Hepatol. 2019;17(13):2696–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang J, Zhang C, Zhang A. The Association between blood lead levels and urgency urinary incontinence among adult females: a retrospective study based on NHANES 2005–2020. Biol Trace Elem Res 2024. [DOI] [PubMed]
- 42.Wang C, Zhang L, Li L. Association between Selenium Intake with chronic constipation and chronic diarrhea in adults: findings from the National Health and Nutrition Examination Survey. Biol Trace Elem Res. 2021;199(9):3205–12. [DOI] [PubMed] [Google Scholar]
- 43.Hong Y, Chen X, Liu J. Analysis of Factors Associated with Constipation in the Population with obesity: evidence from the National Health and Nutrition Examination Survey. Obes Facts. 2024;17(2):169–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tan BJ, Zhou ZD, Chan LL, Tan EK. Comments on Association of environmental tobacco smoke exposure with chronic constipation: a nationwide survey (NHANES 2005–2010) Duan R, et. al., doi (10.1007/s11356-023-30542-4). Environ Sci Pollut Res Int. 2024;31(32):45462–3. [DOI] [PubMed] [Google Scholar]
- 45.Wei S, Yu S, Lan Y, Jia Y. Association between the composite dietary antioxidant index and constipation: evidence from NHANES 2005–2010. PLoS ONE. 2024;19(9):e0311168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hanna-Jairala I, Drossman DA. Central neuromodulators in irritable bowel syndrome: why, how, and when. Am J Gastroenterol. 2024;119(7):1272–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taché Y, Martinez V, Million M, Wang L. Stress and the gastrointestinal tract III. Stress-related alterations of gut motor function: role of brain corticotropin-releasing factor receptors. Am J Physiol Gastrointest Liver Physiol. 2001;280(2):G173–177. [DOI] [PubMed] [Google Scholar]
- 48.Heinrichs SC, Lapsansky J, Lovenberg TW, De Souza EB, Chalmers DT. Corticotropin-releasing factor CRF1, but not CRF2, receptors mediate anxiogenic-like behavior. Regul Pept. 1997;71(1):15–21. [DOI] [PubMed] [Google Scholar]
- 49.Zhang XY, Ye F, Yin ZH, Li YQ, Bao QN, Xia MZ, Chen ZH, Zhong WQ, Wu KX, Yao J, et al. Research status and trends of physical activity on depression or anxiety: a bibliometric analysis. Front Neurosci. 2024;18:1337739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen H, Cao Z, Hou Y, Yang H, Wang X, Xu C. The associations of dietary patterns with depressive and anxiety symptoms: a prospective study. BMC Med. 2023;21(1):307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McCrea GL, Miaskowski C, Stotts NA, Macera L, Varma MG. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. J Pain Symptom Manage. 2009;37(4):737–45. [DOI] [PubMed] [Google Scholar]
- 52.Abankwah JK, Wang Y, Wang J, Ogbe SE, Pozzo LD, Chu X, Bian Y. Gut aging: a wane from the normal to repercussion and gerotherapeutic strategies. Heliyon. 2024;10(19):e37883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang Z, Lu Y, Li L, Wu X, Liu J, Tang J, Wang W, Lu L. Relationship between severity of gastrointestinal symptoms and anxiety symptoms in patients with chronic gastrointestinal disease: the mediating role of illness perception. Psychol Res Behav Manag. 2023;16:4921–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bergmann E, Harlev D, Wolpe N. Depressive symptoms are linked to age-specific neuroanatomical and cognitive variations. J Affect Disord. 2025;369:1013–20. [DOI] [PubMed] [Google Scholar]
- 55.McEwen BS, Bowles NP, Gray JD, Hill MN, Hunter RG, Karatsoreos IN, Nasca C. Mechanisms of stress in the brain. Nat Neurosci. 2015;18(10):1353–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gururajan A, van de Wouw M, Boehme M, Becker T, O’Connor R, Bastiaanssen TFS, Moloney GM, Lyte JM, Ventura Silva AP, Merckx B, et al. Resilience to chronic stress is associated with specific neurobiological, neuroendocrine and immune responses. Brain Behav Immun. 2019;80:583–94. [DOI] [PubMed] [Google Scholar]
- 57.Kalisch R, Russo SJ, Müller MB. Neurobiology and systems biology of stress resilience. Physiol Rev. 2024;104(3):1205–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rosas CE, Pirzada A, Durazo-Arvizu R, Gallo LC, Talavera GA, Elfassy T, Cai J, Llabre MM, Perreira KM, Wassertheil-Smoller S, et al. Associations of anxiety symptoms with 6-Year blood pressure changes and Incident Hypertension: results from the Hispanic Community Health Study/Study of latinos. Ann Behav Med. 2024;58(7):488–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qiu T, Jiang Z, Chen X, Dai Y, Zhao H. Comorbidity of Anxiety and Hypertension: Common Risk Factors and Potential Mechanisms. Int J Hypertens 2023, 2023:9619388. [DOI] [PMC free article] [PubMed]
- 60.Mancia G, Grassi G. The autonomic nervous system and hypertension. Circ Res. 2014;114(11):1804–14. [DOI] [PubMed] [Google Scholar]
- 61.Judkins CP, Wang Y, Jelinic M, Bobik A, Vinh A, Sobey CG, Drummond GR. Association of constipation with increased risk of hypertension and cardiovascular events in elderly Australian patients. Sci Rep. 2023;13(1):10943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cheng C, Chan AO, Hui WM, Lam SK. Coping strategies, illness perception, anxiety and depression of patients with idiopathic constipation: a population-based study. Aliment Pharmacol Ther. 2003;18(3):319–26. [DOI] [PubMed] [Google Scholar]
- 63.Deng Z, Zeng X, Wang H, Bi W, Huang Y, Fu H. Causal relationship between major depressive disorder, anxiety disorder and constipation: a two-sample mendelian randomization study. BMC Gastroenterol. 2024;24(1):434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Devroede G, Girard G, Bouchoucha M, Roy T, Black R, Camerlain M, Pinard G, Schang JC, Arhan P. Idiopathic constipation by colonic dysfunction. Relationship with personality and anxiety. Dig Dis Sci. 1989;34(9):1428–33. [DOI] [PubMed] [Google Scholar]
- 65.Karasawa Y, Nozawa K, Nomoto K, Fukudo S. Constipation among workers with depression/anxiety: a retrospective study using a claims database and survey data in Japan. BMJ Open. 2024;14(11):e083668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liang J, Zhao Y, Xi Y, Xiang C, Yong C, Huo J, Zou H, Hou Y, Pan Y, Wu M et al. Association between Depression, Anxiety Symptoms and Gut Microbiota in Chinese Elderly with Functional Constipation. Nutrients 2022, 14(23). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data used in this study is available in NHANES database. You can find this data at the following link: NHANES (https://www.cdc.gov/nchs/nhanes/index.htm).