Abstract
Introduction
Pain from the cervical facet joints, either due to degenerative conditions or due to whiplash‐related trauma, is very common in the general population. Here, we provide an overview of the literature on the diagnosis and treatment of cervical facet‐related pain with special emphasis on interventional treatment techniques.
Methods
A literature search on the diagnosis and treatment of cervical facet joint pain and whiplash‐associated disorders (WAD) was performed using PubMed, Cochrane, and Embase databases. All relevant literature was retrieved and summarized.
Results
Facet‐related pain is typically diagnosed based on history and physical examination of the patients, combined with a diagnostic block (eg, with local anesthetic) of the medial branches innervating the joints. There is no additive value for imaging techniques to diagnose cervical facet pain, but imaging may be used for procedure planning. First‐line therapy for pain treatment includes focused exercise, graded activity, and range‐of‐motion training. Pharmacological treatment may be considered for acute facet joint pain; however, for chronic facet joint pain, evidence for pharmacological treatment is lacking. Considering the lack of evidence for treatment with botulinum toxin, intra‐articular steroid injections, or surgery, these interventions are not recommended. Diagnostic blocks are not considered a viable treatment option, though some patients may experience a prolonged analgesic effect. Long‐term analgesia (>6 months) has been observed for radiofrequency treatment of the medial branches.
Conclusions
Cervical facet pain is diagnosed based on history, physical examination, and a diagnostic block of the medial branches innervating the painful joints. Conservative management, including exercise therapy, is the first line of treatment. When conservative management does not result in adequate improvement of pain, radiofrequency treatment of the medial branches should be considered, which often results in adequate pain relief.
Keywords: cervical facet joint, cervical pain, neck pain, radiofrequency treatment, whiplash‐associated disorder
INTRODUCTION
Neck pain is a common and debilitating cause of pain in the general population. The annual and lifetime prevalence rates are estimated to be 37.2% (range 16.7%–75.1%) and 48.5% (range 14.2%–71.0%), respectively. 1 , 2 , 3 The pain may be self‐limiting; however, in about 50% of individuals, neck pain becomes recurrent or chronic with a diminution in quality of life, physical functioning, and work productivity, and a concomitant increase in health care utilization. 2 According to the systematic analysis of data from the Global Burden of Disease 2017 study, neck pain remains a serious health problem, especially in Western Europe, that leads to considerable pain, disability, and economic costs. 3 Neck pain is defined as pain in the posterior area between the base of the skull and the first thoracic vertebra. The pain may extend into adjacent regions such as the head (cervicogenic headache), shoulder, or upper arm (radicular or non‐radicular) and is graded according to symptom severity as described by the 2000–2010 Bone and Joint Task Force on Neck Pain and Its Associated Disorders (see also Table 1). 2 Several structures may be involved as sources of pain, including vertebrae, discs, uncovertebral (Luschka) joints, ligaments, muscles, and facet (zygapophyseal) joints. 2 Risk factors for the development and persistence of neck pain overlap with those of other musculoskeletal pain syndromes, and include female sex, middle age, genetics, and psychopathology, such as depression, anxiety and poor coping skills, sleep disorders, smoking, obesity, and either a sedentary or high‐risk lifestyle (eg, manual laborers, occupational drivers). Furthermore, neck pain is often accompanied by headache, back pain, and arthralgias. 2 , 4 , 5 , 6 , 7 , 8
TABLE 1.
Classification of neck pain and associated disorders and whiplash‐associated disorders.
| Grade | Definition |
|---|---|
| The 2000–2010 Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders Classification | |
| I | No signs or symptoms of major structural pathology and no or minor interference with daily activities |
| II | No signs or symptoms of major structural pathology but major interference with daily activities |
| III | No signs or symptoms of major structural pathology, but presence of neurological signs (eg decreased deep tendon reflexes, weakness or sensory deficits) |
| IV | Signs or symptoms of major structural pathology (eg fracture, myelopathy, neoplasm, spinal infection) |
| The Quebec Task Force Classification of Whiplash‐Associated Disorders | |
| I | Neck pain and associated symptoms in the absence of objective physical signs |
| II | Neck pain and associated symptoms in the presence of objective physical signs but without evidence of neurological involvement |
| III | Neck pain and associated symptoms with evidence of neurological involvement including decreased or absent reflexes, decreased or limited sensation, or muscular weakness |
| IV | Neck pain and associated symptoms with evidence of fracture or dislocation |
Cervical facet joints
In more than 50% of patients presenting to pain clinics with neck pain, the cervical facet joints are the primary source of pain, either due to degenerative alterations or whiplash‐related trauma. 1 The cervical facet joint is a diarthrodial joint with bony joint surfaces, a synovial membrane, and a joint capsule. It forms an angle of approximately 45° with the longitudinal axis of the cervical spinal column, though the range varies significantly by person and spinal level (20°–78° vs. the axial plane). 9 Innervation of the facet joints is mediated by the medial branches of the dorsal rami of the segmental nerve at the levels above or below the affected level (ie, the C4–C5 facet joint is innervated by branches from C4 and C5; see also Figure 1). 9 In some cases, innervation of a facet joint derives from only a single dorsal ramus. However, there is also a high frequency of multiple branches deriving from a single dorsal ramus providing innervation to a given facet joint, especially at upper levels (C1–C4) where this may even be more of a rule than an exception. 10 , 11 For example, there are usually two medial branches at C3: a superficial branch, which is referred to as the third occipital nerve (TON), which innervates the C2–C3 facet joint alone, and a deep branch, which innervates the C3–C4 facet joint along with the C4 medial branch. Compared to the lumbar facet joints, the cervical facet joints have a higher density of mechanoreceptors and nociceptive afferent fibers, which predisposes them to pain generation. 7 , 12 Clinically, the C2–C3 and C5–C6 joints are the most commonly implicated pain generators, 13 , 14 , 15 while on radiological imaging, the C2–C5 levels are most frequently affected. 16 , 17
FIGURE 1.

Anatomical illustration of the cervical vertebral column, including the innervation of the facet joints.
The cervical facet joints are sensitive to injury from degenerative alterations and trauma, leading to whiplash‐associated disorders (WAD). 9 , 18 , 19 , 20 The underlying cause of the development of degenerative changes within the facet joints is not fully understood. Hypotheses that may explain the development of anatomical alterations within the facet joint include the presence of increased “facet loading” due to narrowing of the intervertebral discs, microtrauma due to overload, and processes similar to those responsible for the development of arthrosis in other joints such as the knee and hip. 9 , 18 WAD is most often caused by an acceleration‐deceleration mechanism due to a rear‐end or side‐impact motor vehicle collision but can also be caused by diving accidents or other mishaps. 21 The abnormal kinematics produced during a whiplash‐related trauma induce microstructural damage to the collagen fibrous matrix of the capsular ligament, synovial fold punching, and degenerative alterations. In addition to flexion‐extension injuries, another prominent mechanism relates to cervical spine compression resulting from exaggerated thoracic kyphosis in the seat‐back position. 21 The densely innervated ligaments that encapsulate the synovial joint are especially prone to injury and the generation of facet‐mediated neck pain. 9 , 19 , 20 , 22 Afferent nerve fibers of the facet joint ligament directly projecting toward the dorsal root ganglion and with prolonged nociception can induce peripheral and central sensitization. 18 , 22 , 23 , 24 , 25 , 26 , 27
In this review, we focus on degenerative facet‐related pain and WAD and provide an overview of the literature on the diagnosis and treatment of cervical facet pain and WAD (except the treatment of the atlantoaxial joint), with special emphasis on interventional treatment techniques.
METHODOLOGY
This narrative review is based on the articles “cervical facet pain” and “whiplash‐associated disorders” published in 2010 in the series “Evidence‐based Interventional Pain Medicine according to Clinical Diagnosis.” 28 , 29 In 2015, an independent company, Kleijnen Systematic Reviews (KSR), performed a systematic review of the literature for the period 2009–2015, based on existing systematic reviews (SRs) and randomized controlled trials (RCTs). 30 , 31 For the current article, an updated search was conducted for the period 2015–January 2024 using PubMed, Cochrane, and Embase databases (see File S1 for the search strategy). Additionally, authors could select relevant missing articles from reference sources and general search databases (eg, Google and Google Scholar). Two authors (MH and MN) screened all articles for content and relevance. In case of disagreement on selection, a third reviewer (MvE) was consulted.
DIAGNOSIS
History
Pain originating from the cervical facet joint is regularly characterized by unilateral pain, rarely radiating past the shoulder (though the extent of radiation is partly dependent on the magnitude of stimulation). Rotation, lateral, and retroflexion are usually reported as painful or limited. 25 The referral pattern of cervical facet joint pain has been investigated in both healthy volunteers and patients by both pain provocation and drawings from individuals whose pain was relieved by diagnostic blocks. 32 , 33 , 34 , 35 In Figure 2, the referral patterns for each cervical facet level are shown, and these radiation patterns can help the clinician determine which cervical level the pain is arising from. Cervical facet joints that most commonly induce chronic neck pain are at the level of C2–C3 (36%), C5–C6 (35%), and C6–C7 (17%). The other facet joints are thought to be individually symptomatic in <10% of cases. 33
FIGURE 2.
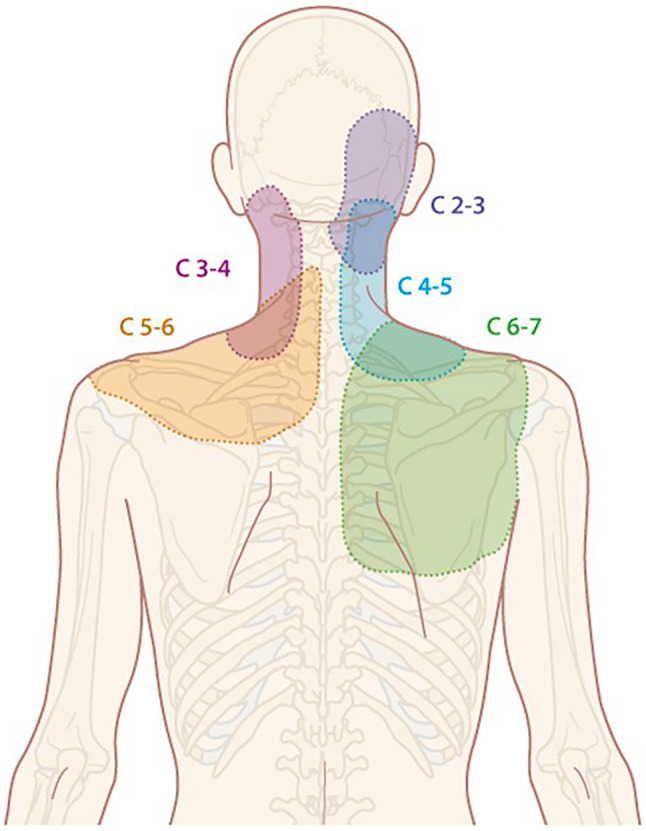
Radiation patterns of cervical facet joint pain (Illustration: Rogier Trompert Medical Art). Adapted from Dwyer et al. 35
Patients with WAD describe a mechanical injury, such as trauma, as a cause of their pain. 13 , 36 , 37 The trauma often occurs during a motor vehicle collision wherein the patient was either the driver or a front‐seat passenger. 38 , 39 Typical symptoms of acute whiplash injury include pain in the neck, shoulders, and sometimes the arms; headache (particularly in the occipital area, sometimes radiating to the forehead); and restricted mobility of the neck as a result of myofascial involvement and neck stiffness immediately after the trauma. WAD is typically accompanied by concomitant symptoms such as dizziness, visual impairment, nausea, tinnitus, loss of hearing, paresthesias in the hands, localized spasms and tenderness, lower back pain, and cognitive disorders (see also Table 1 for the Quebec classification of WAD). 26 , 27 , 40 , 41 After the acute phase, a subacute phase can occur in which often most of the symptoms improve or even disappear. If symptoms persist after 3 months, chronic WAD is diagnosed, with 38% (32%–45%) of patients continuing to experience neck pain 12 months post‐injury. 20 Post‐injury pain and disability, whiplash grade, psychopathology, cold hyperalgesia, and secondary gain have been linked to persistent pain, while imaging abnormalities, motor dysfunction, and collision‐related factors have not. 42 Facet joint involvement has been reported in 54%–60% of patients (range 40%–73%) with WAD. 36 , 37
Attention should be paid to signs and symptoms suggestive of serious underlying pathology of the neck pain (grade III or IV neck pain; see also Table 1). It is important to inquire about radiation patterns beyond the shoulder, which may indicate the presence of cervical herniated intervertebral discs or symptomatic spinal stenosis. When symptoms such as weight loss, fever, nausea, vomiting, dysphagia, coughing, or frequent infections are reported (red flags), a more extensive history and physical examination are warranted to exclude infectious and malignant causes. 43
Physical examination
Physical examination of the neck may help in the diagnostic evaluation of facet joint‐related pain. 44 , 45 , 46 Typical abnormalities observed on physical examination suggestive of facetogenic pain include the presence of paraspinal muscle tenderness, local pressure pain over the facet joints, and pain during cervical extension‐rotation and lateral flexion movements. Rotation in a neutral position determines the rotational movement of the entire cervical spinal column. Rotation during flexion assesses movement in the higher cervical segments, while rotation during extension assesses the movement in the lower cervical segments. 25 Typical findings for WAD include local muscle tenderness, which can be accompanied by muscle spasm, and limited active range of motion, including latero‐flexion and extension. The physical examination should aim to rule out focal neurological signs such as decreased or abnormally increased deep tendon reflexes, neurological muscle weakness, dermatomal sensory deficits, and radicular signs (eg, Spurling test). In case of trauma, special attention should be paid to the possible presence of cervical fractures. 43
Cervical facet‐mediated pain should be considered when the following symptoms are present: (1) axial neck pain (rarely radiating past the shoulders); (2) pain upon posteroanterior pressure applied over the articular pillars of the facet joints or during palpation of the segmental muscles overlying the facet joints; (3) pain with limited extension, lateral flexion, and rotation of the cervical spine; and (4) absence of neurological symptoms. 25 In WAD, restricted mobility as a result of neck stiffness after the accident may be more prominent than with insidious etiologies, and the syndrome may be characterized by concomitant symptoms including shoulder weakness, dizziness, visual impairment, nausea, tinnitus, posttraumatic stress disorder, and cognitive dysfunction including memory loss. 4 , 20 , 26 , 27
Additional tests
Imaging studies
Several studies have evaluated the usefulness of imaging studies, such as plain radiography, CT, and MRI, for the diagnosis of cervical facet‐related pain and WAD. 16 , 25 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 Although some studies have found weak correlations between the presence of imaging abnormalities on CT and MRI (eg, edema surrounding the facet joint) and neck pain, most studies have not, and the studies indicating an association failed to confirm the facet joints as pain generators via diagnostic blocks. 16 , 59 , 60 This is due in part to the low specificity of advanced imaging. For whiplash‐related trauma, plain radiography directly after trauma can illustrate the extent of injury to the cervical facet joints. One study revealed that mean pain intensity 6 months after the trauma was correlated to baseline imaging findings of facet joint degeneration. 54 However, most other studies investigating the correlation between radiological studies and pain persistence after whiplash trauma failed to replicate these findings. 42 , 49 , 58 Notably, postmortem images of victims of fatal accidents have identified lesions and small fractures undetectable on plain radiographs, indicating the possibility that some types of injuries that correlate with symptoms may be missed using plain radiography. 19 , 61 Currently, the use of imaging techniques to diagnose or predict the response to diagnostic blocks is not useful, though the cervical facet guidelines assert that imaging may be used for the purpose of procedure planning. 25 Imaging studies are indicated, however, when history or physical examination provides evidence for the possible presence of severe pathology such as a fracture, disc herniation, subluxation, or tumor. 43
Diagnostic and prognostic medial branch blocks
Blockade of anatomical structures using local anesthetics can be used to isolate a structure considered to be a potential source of pain. Since history, physical examination, and radiological studies are unable to definitively diagnose cervical facet joint pain, diagnostic blocks with local anesthetic are the most widely accepted approach to identify putatively painful facet joints and select patients for RF ablation. 62 Given the high false‐positive and false‐negative rates of the facet joint blocks and the absence of any reference standard, non‐placebo‐controlled blocks are perhaps better referred to as “prognostic.” 25 In 1988, Bogduk and Marsland described the analgesic effects of local anesthetic injections at the facet joints in patients with neck pain. 13 The facet joint can be blocked either by intra‐articular injection or by blockade of the medial branches of the dorsal ramus that innervate the facet joint (for innervation, see the Section 1). Often multiple (maximum of 3) levels are blocked to diagnose cervical facet pain, as the pain is usually not restricted to a single level. However, failed injections in which the targeted structure is not captured have been reported in 7% of fluoroscopically‐guided medial branch blocks and around 22% of fluoroscopically‐ or ultrasound intra‐articular injections, with over 90% of intra‐articular injections being accompanied by extra‐articular extravasation, thereby undermining the specificity. 63 , 64 , 65 In addition to a higher technical success rate, medial branch blocks (MBB) are preferred over the intra‐articular blocks because they may be safer and have been shown in the lumbar spine to have greater predictive value for RF ablation outcomes. 25 , 66 , 67 , 68 , 69
The most influential factor that affects the specificity of diagnostic MMB is the spread of the injected local anesthetic, which might extend to adjacent structures at volumes as low as 0.3 mL and lead to false positive results. A diagnostic/prognostic block is generally considered positive if ≥50% pain relief is achieved, though some organizations propose thresholds exceeding 70%. 25 However, numerous studies observed no difference in RF ablation outcomes stratified by a cutoff of 50% versus higher thresholds. 57 , 70 , 71 , 72 , 73 , 74 To overcome the controversy, for the latest guideline on cervical facet pain, a consensus was reached to consider a diagnostic block positive at a cutoff of ≥50% pain relief. 25 , 75 There has been extensive controversy surrounding whether more than one prognostic block should be performed in order to increase the success rate of RF therapy. Whereas there are no studies evaluating the utility of dual‐blocks in the cervical spine, studies in patients with suspected lumbar facet pain show that the use of dual‐blocks (two separate occasions) may significantly increase the proportion of false‐negative results, is not cost‐effective, infrequently results in a different outcome (ie, a negative 2nd block after a positive 1st block), and, though it has been demonstrated to increase the RF ablation success, will result in a decreased overall success rate because of false‐negative results and eliminating placebo responders. 69 , 75 , 76 , 77 , 78 The main rationale for dual‐blocks is to reduce the false‐positive rate, which is lower in the neck than the low back because the prevalence (ie, true positive rate) of cervical facetogenic pain is higher. Hence, they are even more cost‐ineffective in the cervical region.
In summary, medial branch blocks are used to confirm the diagnosis of cervical facet‐related pain. A block is considered positive if the patient experiences ≥50% pain relief.
Differential diagnosis
The most common benign diagnoses that should be considered in the differential diagnosis of cervical facet pain are tendomyalgia of the neck musculature and shoulder pathology. 79 , 80 , 81 Serious underlying pathology of neck pain, such as tumors, infections, fractures, or systemic diseases, is rare. Red flags that should alert the physician to possible serious conditions include fevers, night sweats, unexplained weight loss, decrease in appetite, general malaise, and a history of cancer. Every patient with motor function loss, reflex changes, or loss of sensation and neurological symptoms involving non‐cervical levels should be thoroughly assessed. Conditions that should be excluded when neurological symptoms or red flags are present include metastases, cervical herniated nucleus pulposus with radiculopathy, discitis, inflammatory arthritis, fractures, myelopathy, subluxation, carotid/vertebral artery dissection, and brain hemorrhage. 43
TREATMENT OPTIONS
Conservative management
Several meta‐analyses have been performed on the conservative management of chronic neck pain and WAD. 82 , 83 , 84 , 85 , 86 , 87 Exercise treatment, including graded activity, stretching, strengthening, and range‐of‐motion exercises, is effective in the treatment of chronic cervical pain, with a 10%–30% reduction in pain intensity and neck disability scores. 82 , 83 , 84 , 85 , 86 , 87 There is no evidence that supervised training is more effective than home exercises; however, guided training appears to be more effective than no training or just the advice to stay active. 83 Multimodal rehabilitation programs based on the biopsychosocial model, which include manual therapy, education, and exercise therapy, are also effective in pain reduction, but there is no evidence that these programs yield better results than simple, graded activity programs. 82 Cognitive behavioral therapy has been shown to be effective in inducing pain relief and reducing psychological distress after whiplash injury, whereby early intervention (within 6 months after injury) was demonstrated to be more effective than cognitive behavioral therapy starting more than 6 months after the accident. 88 The evidence supporting pharmacological therapy for cervical facet joint pain or pain due to WAD is scarce. Placebo‐controlled and comparative‐effectiveness trials have demonstrated evidence for small effect sizes (NRS pain score decrease of 1–2 points for <3 months) for both topical and systemic NSAIDs, though superiority over other therapies has not been established. 89 , 90 , 91 Pregabalin was shown to be beneficial for acute WAD in high‐risk patients through 6 months after injury (effect size of −4.0 (−1.7 to −6.2 NRS points)), but data on long‐term use demonstrated no clear benefit. 92 Notably, high use of prescribed opioids, benzodiazepines, and antidepressants has been observed in patients with chronic cervical neck pain, and therefore clinicians should be cautious when prescribing these drugs to prevent misuse. 93
Interventional management
Botulinum injections
Botulinum toxin is a drug used to treat aberrant muscle contractions, thereby reducing muscle tightness or spasms. In addition to blocking the presynaptic release of acetylcholine, it also inhibits the release of neurotransmitters involved in neuropathic pain, such as calcitonin gene‐related peptide. The toxin has been evaluated for chronic neck pain and pain due to WAD, with or without associated cervicogenic headache; however, studies have failed to consistently demonstrate the effectiveness of botulinum toxin on pain. The therapy is therefore not advised in the treatment of chronic cervical facet pain. 94 , 95 , 96
Intra‐articular steroid injections
A total of 6 prospective studies (5 on neck pain, 1 on WAD) have been published on the effectiveness of intra‐articular steroid injections of the cervical facet joints. 13 , 97 , 98 , 99 , 100 , 101 Most studies observed short‐term pain relief in the majority of patients (>75%) following intra‐articular injections with local anesthetic (lidocaine or bupivacaine) and steroids. 97 , 98 , 99 , 100 , 101 A minority of patients (<5%) experienced prolonged pain relief (longer than the expected duration of the local anesthetic) lasting between 3 and 13 months. 97 , 98 , 99 , 100 , 101 Two randomized controlled trials evaluated the effect of intra‐articular steroid injection of the cervical facet joint. 102 , 103 The first randomized study performed by Barnsley et al. evaluated 41 patients with chronic cervical facet pain following trauma‐induced whiplash who received either intra‐articular injection with bupivacaine or betamethasone after obtaining definitive pain relief on a 4‐point scale: complete, definitive, partial, or none, after comparative cervical medial branch blocks with lidocaine and bupivacaine. 102 A total of 13 out of 20 patients in the local anesthetic group experienced pain relief of >50% with a median duration of 3 days. For the steroid group, similar results were observed in 15 out of 21 patients. In both groups, 10% of patients experienced pain relief lasting over 3 months. The second RCT involved 400 patients with myofascial and facet joint pathology who received bilateral C5‐C6 and C6‐C7 intra‐articular injections with local anesthetic and steroids combined with conservative treatment or conservative treatment alone (no injections). 103 The conservative treatment in both groups consisted of exercise therapy, medication, and trigger point injections, including with botulinum toxin. After a 1‐year follow‐up, the treatment group reported increased cervical range of motion and greater pain relief (85% of patients had >50% of pain reduction); however, the confounding effect of numerous co‐interventions makes it difficult to determine the contribution from intra‐articular injections. 103 In summary, the majority of patients will experience pain relief of only a few days after intra‐articular steroid injections, with or without local anesthetic, and therefore routine use is not recommended.
Local infiltration of the medial branch of the dorsal ramus
Medial branch blocks of the dorsal rami are primarily considered a diagnostic tool; however, similar to intra‐articular injections, there is some evidence that repetitive infiltration of local anesthetic with or without steroids can provide a prolonged therapeutic effect (longer than the expected analgesic duration of the local anesthetic) in a small subset of patients. 25 Three prospective cohort studies have been published evaluating the ability of (diagnostic) MBB to provide prolonged pain relief. 13 , 104 , 105 In the first study by Bogduk and Marsland, 13 24 patients with cervical neck pain received bupivacaine alone, and 8 patients received bupivacaine combined with steroids. Prolonged pain relief was only observed in the patient group who received bupivacaine combined with steroids, with pain relief lasting between 4 days and 12 months in 7 patients and 1 patient reporting relief of headaches for 1 month. A second study in 47 patients who received dual blocks with lidocaine followed by bupivacaine reported prolonged pain relief in 13 patients (exact duration unknown). 104 Lord et al. reported prolonged pain relief in 4% of patients who received triple blocks with lidocaine, bupivacaine, and saline, with none of the responders experiencing prolonged pain relief after saline injection. 105
Two RCTs evaluated the therapeutic value of MBB blocks. 106 , 107 In the first RCT by Manchikanti et al., 106 patients were randomized to either receive local anesthetics and sarapin (an extract of the pitcher plant) or the same mixture combined with steroids. Blocks were repeated over a 2‐year period if pain relief returned to more than 50% of baseline. Significant pain relief (≥50%) was reported in the majority of patients (>85%). The average duration of pain relief for each procedure was 4 months in both groups, indicating there was no additional analgesic effect with the addition of steroids. However, serious methodological flaws (eg, an enriched enrollment design, failure to control for concurrent interventions, and an unclear methodology for evaluating outcomes) limit generalization, and the results should be interpreted with caution. A more recent RCT by Hussain et al. 107 in 60 patients with cervical pain compared two‐level cervical MBB to local trigger point injections. Both groups received local anesthetic with steroids. The results reported significantly lower pain scores in the patients who received the MBB, with larger functional improvement noted in the first 12 weeks after treatment.
In summary, the current literature on the effectiveness of cervical MBB with local anesthetics with or without steroids demonstrates prolonged pain relief in only a small portion of patients. Hypotheses on why prolonged relief may occur in a subset of individuals include prolonged neuronal conduction blockade, a reduction in neuronal inflammation, a prolonged placebo effect, or the reversal of peripheral or central sensitization. 108 , 109 Recent guidelines recommend against the routine use of steroids, as no strong evidence exists that the addition of steroids enhances analgesia or prolongs pain relief. 25
Radiofrequency (RF) treatment of the medial branch of the dorsal ramus
Percutaneous RF treatment is considered the treatment of choice after a positive diagnostic block (ie, ≥50% pain relief after blockade of the medial branches with local anesthetic). The effectiveness of RF treatment of the cervical facet joints has mainly been studied in observational studies, with 13 studies conducted in neck pain (7 prospective, 6 retrospective) and 4 prospective studies performed in patients with WAD. 57 , 70 , 73 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 Results are comparable between the studies, showing that RF treatment resulted in ≥50% pain relief for at least 6 months in 70%–85% of patients. Several studies had longer follow‐up time periods, reporting pain relief for at least 12 months in 60%–65% of patients. Two randomized trials have been performed evaluating the effectiveness of RF treatment of cervical facet joint pain. 124 , 125 The first study by Lord et al. 124 randomized 24 patients with cervical facet pain after trauma to RF treatment or a sham procedure (needle placement without RF treatment). RF treatment was observed to be superior to sham treatment with a median elapsed time before pain returned to at least 50% of baseline of 263 days in the treatment group compared to 8 days in the sham group. A significantly higher percentage of patients treated with RF therapy were pain‐free after 27 weeks compared to the sham group. A second RCT by van Eerd et al., 125 performed in 76 patients with putative cervical facet joint pain based on clinical presentation, randomized participants to receive either bupivacaine without RF treatment or bupivacaine with RF treatment. The study showed a prolonged analgesic effect (pain relief ≥30%) for RF treatment (42 months) compared to local injection alone (12 months). In this study, no significant differences were observed at the 6‐months follow‐up. The small number of studies evaluating the effect of RF treatment on psychological parameters also observed an improvement after RF treatment. 123 , 126 , 127 See Table 2 for a summary of the randomized controlled trials on RF treatment for cervical facet joint pain.
TABLE 2.
Randomized controlled trials evaluating radiofrequency treatment of the cervical facet joint.
| Study characteristics | Patients | Outcome measures | Results |
|---|---|---|---|
|
Lord et al. (1996) 124 Randomized, double‐blind, sham‐controlled (with bupivacaine) trial |
24 patients with WAD |
|
|
|
van Eerd et al. (2021) 125 Randomized, sham‐controlled (with bupivacaine) trial |
76 patients with chronic neck pain |
|
|
Abbreviations: HADS, hospital anxiety and depression scale; NDI, neck disability index; PGIC, patients global impression of change; QoL, quality of life; RAND36, research and development 36; WAD, whiplash‐associated disorder.
In summary, RF treatment after a positive diagnostic block has been shown to induce long‐term pain relief in most patients with cervical facet joint pain. RF treatment of the medial branch of the dorsal ramus should be performed in those failing to respond to conservative therapy who experience significant relief after a diagnostic block.
Surgical treatment
There is currently no place for surgery in the treatment of primary non‐radicular neck pain. Although weak evidence grounded in methodologically flawed studies suggests that anterior cervical fusion therapy might have long‐term analgesic effects in some patients, this therapy is not recommended by guidelines. 25 , 43 , 128 , 129 , 130 For neck pain complicated by symptomatic spinal stenosis or disc herniation, referral to a neurosurgeon should be considered. 25 , 43
Complications of interventional management
Cervical facet joint interventions performed using fluoroscopic guidance rarely result in serious complications. 25 , 131 Reported minor complications, including soreness at the procedure site, light‐headedness, sweating, and nausea, tend to be mild and of short duration. 25 For the first 2 weeks after the procedure, patients may experience an exacerbation of pain, which is mostly observed after RF treatment (4%). 114 , 132 Needle placement in close vicinity to nerve roots or the cervical/brachial plexus, or the use of large volumes of local anesthetic, may result in temporary sensorimotor neurological deficits in the back of the head, neck, and upper extremity (0.15% of patients). Vascular complications such as intravascular injection or hematoma formation (2.3% of patients) resulting from needle damage to blood vessels that lie in the vicinity of the cervical facet joint, such as the vertebral artery and the deep, ascending, and transverse cervical arteries, have been reported. 131 The use of ultrasound has been investigated to reduce the risk of vascular complications. A recent meta‐analysis which compared the use of fluoroscopy and ultrasound to perform cervical medial branch blocks confirmed there was less vascular penetration using ultrasound guidance. 133 Other potential complications include injury to a nerve (root) or the spinal cord from direct needle trauma, spinal cord compression from a large or unrecognized hematoma, dural puncture with high or total spinal block, and spinal cord infarction due to disruption of the arterial blood supply (described for transforaminal injections from the inadvertent arterial injection of local anesthetic or steroids). 133 , 134 , 135 , 136 , 137 , 138 Furthermore, facet capsule rupture can occur after joint infiltration with excessive volumes, and pneumothorax can occur with poor needle placement. Infection of superficial tissue is observed in between 0% and 2.9% of patients.
Evidence for interventional management
Table 3 provides a summary of the evidence for interventional treatment of cervical facet joint pain according to previously published guidelines. 30 , 31 , 70
TABLE 3.
Recommendations from previously published guidelines.
| Author (Date) | Technique | Quality of evidence | Conclusion | Recommendation |
|---|---|---|---|---|
| Huygen (2019) 30 , 31 | Intra‐articular injection |
Low Based on: 2 RCTs |
One study showed no effect of intra‐articular injections. The other study had significant methodological flaws | Weak recommendation against use |
| Huygen (2019) 30 , 31 | Therapeutic cervical medial branch block with local anesthetic with or without corticosteroids |
Moderate Based on: 1 observational study 1 RCT |
The observational study observed improvements compared to baseline in pain relief, the RCT showed pain relief in over 85% of patients | Weak recommendation for use |
| Huygen (2019) 30 , 31 | Radiofrequency treatment of the medial branch |
Low Based on: 3 observational studies 1 RCTs |
All studies were supportive of radiofrequency ablation but they were few and mostly observational. The RCT had some methodological limitations | Weak recommendation for use |
| Hurley (2022) 25 | Intra‐articular injection |
Low to moderate Based on: 6 observational studies 2 RCTs |
Recommendation against the routine use of intra‐articular injections but they might be considered in patients with prolonged pain relief upon diagnostic block or contraindications to radiofrequency therapy | Recommendation against routine use |
| Hurley (2022) 25 | Therapeutic cervical medial branch block with local anesthetic with or without corticosteroids |
Low to moderate Based on: 3 observational studies 2 RCTs |
In a minority of patients, a therapeutic effect may be provided by local anesthetic. Recommendation against the routine use of corticosteroids due to lack of evidence that steroids enhance prolonged pain relief combined with the side effect profile of steroids | Recommendation against routine use |
| Hurley (2022) 25 | Radiofrequency treatment of the medial branch |
Moderate Based on 2 RCTs |
Radiofrequency ablation might provide benefit to well‐selected individuals | Recommendation for use in selected individuals |
Abbreviation: RCT, randomized controlled trial.
RECOMMENDATIONS
Based on the evidence available regarding the effect and complications of interventions for cervical facet‐related pain, the following recommendations are made.
Conservative management, including graded activity and exercise training, is effective in the management of chronic cervical facet‐related pain.
Evidence for pharmacological treatment of cervical facet‐related pain is scarce, and long‐term pharmacological treatment is not recommended without proper monitoring and surveillance because of the side effect profile of many drugs and their abuse potential.
Intramuscular botulinum toxin injection and intra‐articular infiltration with local anesthetics or steroids for the treatment of cervical facet joint pain are not recommended.
Medial branch block infiltration with local anesthetics is primarily considered a diagnostic aid. It may induce long‐term pain relief in a minority of patients.
RF treatment could be considered for cervical facet joint pain after a positive diagnostic/prognostic block due to its prolonged treatment effect (>6 months) compared to other therapies.
Clinical practice algorithm
A practice algorithm for the management of cervical facet pain is illustrated in Figure 3. We recommend, after excluding the presence of serious neurological diagnosis, starting with conservative treatment for general neck pain. If adequate pain relief is not obtained, and cervical facet joint pain is suspected, performing a diagnostic block of the facet joints before RF treatment should be considered.
FIGURE 3.

Clinical practice algorithm for the treatment of cervical facet joint pain. For the MBB (medial branch block), it is recommended to perform only one diagnostic block. MB, medial branch.
Technique(s)
Medial branch blocks (diagnostic and therapeutic using RF treatment) are usually performed under fluoroscopic guidance. 25 Different techniques of RF treatment of the medial branch have been described. They can be classified based on the position of the patient (prone, supine, and lateral), on the position of the C‐arm (lateral, anteroposterior, and oblique) or most commonly, on the needle trajectory toward the anatomical planes of the neck (posterolateral, posterior or lateral; Figure 4). 139 The posterolateral technique is the oldest technique, first described by Sluijter et al. in 1980, and is the technique adopted by the World Institute of Pain. 140 The procedure is performed with the patient in the supine position and the C‐arm situated at an oblique angle (±30°) in a trajectory such that the X‐ray beam runs parallel with the exiting nerve root and the pedicles from the contralateral side project onto the anterior half of the vertebral body. The target point of the RF needle lies at the anterolateral aspect of the facet column, inferoposterior to the neuroforamen (Figures 4 and 5A). The needle insertion point is slightly posterior to the target point to facilitate an anterior angle of the RF needle and a perpendicular position of the needle relative to the medial branch. This maximizes contact of the active tip of the needle with the nerve to increase the size of the lesion. The needle is advanced until bony contact is achieved. A disadvantage of the posterolateral technique is that it is not performed using a co‐axial approach (“tunnel‐vision” view with the needle parallel to the X‐ray beam), which makes the technique more difficult to execute, especially in inexperienced hands. To overcome this disadvantage, a modified posterolateral approach has been proposed by van Eerd et al. 139 whereby the C‐arm is placed in a lateral position and a near “tunnel‐vision” approach can be used to advance the needle to its target position. The technique facilitates clear insertion and target points, with the needle insertion point lying at the dorsal side of the facet column and the target point midway between the facet joint spaces (with the needle positioned in a slightly anterior direction, Figure 5B). Potential complications using the posterolateral approach include inadvertent needle placement within the neuroforamen if the needle is advanced too anteriorly. When the needle is positioned too far medially and anteriorly, transgression into the spinal canal may occur. In order to prevent this, the needle position should be regularly checked in the anteroposterior direction to monitor needle depth. The final position of the needle in the AP direction lies in the concave “waist” of the facet column (see Figure 5C). 139
FIGURE 4.
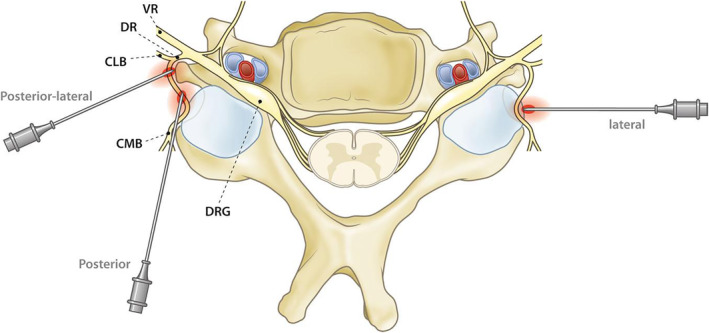
Three approaches for radiofrequency treatment of the cervical medial branch: The posterolateral, the posterior, and lateral approaches. CLB, cervical lateral branch from the dorsal ramus; CMB, cervical medial branch from the dorsal ramus; DR, dorsal ramus of the cervical segmental spinal nerve; DRG, dorsal root ganglion; VR, ventral ramus of the cervical segmental spinal nerve. Adapted from van Eerd et al. 139
FIGURE 5.

(A) Needle position for the postero‐lateral approach with the C‐arm positioned at an oblique angle. The target point of the RF needle is at the anterolateral aspect of the facet column, infero‐posterior to the neuroforamen. (B) Needle position for the lateral approach with the needle insertion point lying at the dorsal side of the facet column and the target point midway between the facet joint spaces (line a). (C) Needle position in the antero‐posterior view with the needle positioned in the concave “waist” of the facet column (for the postero‐lateral and lateral approach). (D) Needle position for the posterior approach with the needle advanced in the sagittal plane parallel to the expected course of the medial branch and the center of the facet column as target point.
Other techniques include the posterior and lateral approaches. The posterior approach was first described in 1996 by Lord et al. 124 and is the technique recommended by the International Pain and Spine Intervention Society (IPSIS). 141 The technique is performed with the patient in the prone position. An RF needle is advanced in the sagittal plane, parallel to the expected course of the cervical medial branch at the waist of the facet column, using the center of the facet column as the target point (see Figure 5D). Disadvantages of the posterior technique are that the spinal column above C4 may be hard to visualize due to the prone positioning, and because more tissue is traversed, it may be more painful and technically difficult. 141 The lateral approach was first described in 1998 by Bogduk and colleagues primarily as a technique used for diagnostic blocks only. 142 , 143 For this technique, the patient is positioned in a supine or lateral position with the C‐arm oriented laterally. The target point of the needle is the midpoint of the rhomboid‐shaped silhouette of the facet column (Figure 4). 139 Disadvantages of this technique are that the needle is placed perpendicular to the medial branch, which minimizes contact between the active tip of the needle and the nerve. Furthermore, due to large individual variations in the course of the medial branch over the facet column, the medial branch is not always present at the target point of this approach. 11 One randomized trial that compared the accuracy of the lateral approach and the posterior approach found no significant difference between the two. 63 A novel technique using a multi‐tined RF cannula might theoretically overcome some of the disadvantages of the lateral technique. With this novel approach, 3 tines are deployed from the tip of the needle when positioned at the cervical facet joint, increasing the active area. A recent observational study using the multi‐tined RF cannula showed significant analgesia after a singular ablation (instead of multilevel), which might possibly also lead to a reduction in procedure time, radiation dose, patient discomfort, and costs. 144
Although studies evaluating cervical medial branch rhizotomy comparing the posterior, lateral, and posterolateral approaches have not observed meaningful differences, two studies in the lumbar spine reported better outcomes when the electrodes were oriented parallel rather than perpendicular (lateral approach in the cervical spine) to the target nerves. 145 , 146 , 147 The latest recommendation guideline on MBB recommends using a fluoroscopically‐guided lateral approach for the C3‐C7 MBB and a posterior or posterior oblique approach for the C8 MBB. 25 The choice of approach ultimately depends on the experience and preference of the treating physician and should balance the risks and benefits individually for each patient.
Once optimal anatomical localization for the needle tip is attained and correct position confirmed using fluoroscopy, local anesthetic can be administered when a diagnostic block is performed. In the case of RF treatment, sensory electrical stimulation can be performed before lesioning to confirm that the active tip of the needle is in close proximity to the medial branch. For this, stimulation at 50 Hz should provide a concordant sensory reaction at <0.6 V. To confirm the absence of inadvertent intraforaminal needle positioning or aberrant spinal nerve anatomy in the trajectory of the RF electrode, motor stimulation at 2 Hz can be applied, which should not result in distal muscle contraction. If this occurs, the needle should be repositioned in a more posterior direction. Contractions of the paraspinal muscles are permitted. IPSIS guidelines, however, do not recommend sensory and motor stimulation but instead recommend using fluoroscopic imaging in multiple views to confirm that the RF electrode is not in close proximity to the cervical nerve root. To prevent intravascular injection, contrast administration may be considered. Once correct needle position has been confirmed, 0.5–1 mL local anesthetic (1% or 2% lidocaine) is administered to reduce the procedure‐related pain of the RF lesion and to enhance lesion size. 148 An RF lesion at 80–90°C for at least 90 s is then carried out. Bilateral and multilevel (>2 levels) RF treatment is not recommended within a single visit due to the possibility of a loss of function of cervical extension muscles. 25 Although rare, case reports of patients who developed a dropped head syndrome after bilateral RF treatment have been described. 149
CONCLUSIONS
Cervical facet joint pain is common in the general population, either due to degenerative alterations or after whiplash‐induced trauma. Diagnosis is difficult to confirm based upon history, physical examination, and radiological tests, and therefore diagnostic injection of the medial branch of the dorsal ramus is often used to confirm the diagnosis. Conservative management is the first choice of therapy, which includes graded activity and exercise therapy. In cases of persistent neck pain refractory to conservative management, RF treatment of the medial branch often results in adequate pain relief.
AUTHOR CONTRIBUTIONS
M. D. Hellinga and M. Niesters performed the literature search. Both, together with M. van Eerd, reviewed the literature. M.D. Hellinga wrote the article, and M. Niesters and M. van Eerd revised it. S. P. Cohen, M. P. Stojanovic, and J. de Andrès Ares provided additional references and comments; they also edited the paper; J. W. Kallewaard and K. Van Boxem provided additional references and comments; they also edited the paper; J. Van Zundert controlled the paper, provided comments, and has full responsibility for the end product.
FUNDING INFORMATION
The authors have no sources of funding to declare for this manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
Supporting information
File S1
ACKNOWLEDGMENTS
The authors thank Nicole Van den Hecke for the administrative support and coordination.
Hellinga MD, van Eerd M, Stojanovic MP, Cohen SP, de Andrès Ares J, Kallewaard JW, et al. 7. Cervical facet pain: Degenerative alterations and whiplash‐associated disorder. Pain Pract. 2025;25:e70005. 10.1111/papr.70005
J. Van Zundert and K. Van Boxem are Editorial Board member of Pain Practice and a co‐author of this article. To minimize bias, he was excluded from all editorial decision‐making related to the acceptance of this article for publication.
DATA AVAILABILITY STATEMENT
Data sharing is not applicable, as no new data were created or analyzed in this study.
REFERENCES
- 1. Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15:834–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Haldeman SDC, Carroll L, Cassidy JD, Schubert J, Nygren A. The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: executive summary. Spine. 2008;33:S5–S7. [DOI] [PubMed] [Google Scholar]
- 3. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators . Global, regional and national incidence, prevalence and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Diseas Study 2015. Lancet. 2016;388:1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hogg‐Johnson S, van der Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33:S39–S51. [DOI] [PubMed] [Google Scholar]
- 5. Manchikanti L, Manchikanti KN, Cash KA, Singh V, Giordano J. Age‐related prevalence of facet‐joint involvement in chronic neck and low back pain. Pain Physician. 2008;11:67–75. [PubMed] [Google Scholar]
- 6. Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007;57:656–665. [DOI] [PubMed] [Google Scholar]
- 7. Candido KD, Bryant E. Cervical spine pain related to the facet joints. Tech Reg Anesth Pain Manag. 2015;19:109–118. [Google Scholar]
- 8. Cohen SP, Hooten WM. Advances in the diagnosis and management of neck pain. BMJ. 2017;358:j3221. [DOI] [PubMed] [Google Scholar]
- 9. Jaumard NV, Welch WC, Winkelstein BA. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng. 2011;133:071010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Büsken F, Lataster A, Herrler A. The innervation of the cervical facet joints – an anatomical and histological approach. Clin Anat. 2022;35:780–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kweon TD, Kim JY, Lee HY, Kim MH, Lee YW. Anatomical analysis of medial branches of dorsal rami of cervical nerves for radiofrequency thermocoagulation. Reg Anesth Pain Med. 2014;39:465–471. [DOI] [PubMed] [Google Scholar]
- 12. Büsken F, Lataster A, Herrler A. The innervation of the cervical facet joints – an anatomical and histological approach. Clin Anat. 2002;35:780–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bogduk N, Marsland A. The cervical zygapophysical joints as a source of neck pain. Spine. 1988;13:610–617. [PubMed] [Google Scholar]
- 14. Aprill C, Bogduk N. The prevalence of cervical zygapophyseal joint pain. A first approximation. Spine. 1992;17:744–747. [DOI] [PubMed] [Google Scholar]
- 15. Manchikanti L, Singh V, Rivera J, Pampati V. Prevalence of cervical facet joint pain in chronic neck pain. Pain Physician. 2002;5:243–249. [PubMed] [Google Scholar]
- 16. Nevalainen MT, Foran PJ, Roedl JB, Zoga AC, Morrison WB. Cervical facet oedema: prevalence, correlation to symptoms, and follow‐up imaging. Clin Radiol. 2016;71:570–575. [DOI] [PubMed] [Google Scholar]
- 17. Lee MJ, Riew KD. The prevalence cervical facet arthrosis: an osseous study in a cadveric population. Spine J. 2009;9:711–714. [DOI] [PubMed] [Google Scholar]
- 18. Ita ME, Zhang S, Holsgrove TP, Kartha S, Winkelstein BA. The physiological basis of cervical facet‐mediated persistent pain: basic science and clinical challenges. J Orthop Sports Phys Ther. 2017;47:450–461. [DOI] [PubMed] [Google Scholar]
- 19. Bogduk N. On cervical zygopophysial joint pain after whiplash. Spine. 2011;36:194–199. [DOI] [PubMed] [Google Scholar]
- 20. Al‐Khazali HM, Ashina H, Iljazi A, Liptom RB, Ashina M, Ashina S, et al. Neck pain and headache after whiplash injury: a systematic review and meta‐analysis. Pain. 2020;161:880–888. [DOI] [PubMed] [Google Scholar]
- 21. Bogduk N, Yoganandan N. Biomechanics of the cervical spine part 3: minor injuries. Clin Biomech (Bristol, Avon). 2001;16:267–275. [DOI] [PubMed] [Google Scholar]
- 22. Chen C, Lu Y, Kallakuri S, Patwardhan A, Cavanaugh JM. Districbution of A‐delta and C‐fiber receptors in the cervical facet joint capsule and their response to stretch. J Bone Joint Surg Am. 2006;88:1807–1816. [DOI] [PubMed] [Google Scholar]
- 23. Bontinck J, Lenoir D, Cagnies B, Murillo C, Timmers I, Cnockaert E, et al. Temporal changes in pain processing after whiplash injury, based on quantitative sensory testing: a systematic review. Eur J Pain. 2022;26:227–245. [DOI] [PubMed] [Google Scholar]
- 24. Loeser JD, Treede RD. The Kyoto protocol of IASP basic pain terminology. Pain. 2008;137:473–477. [DOI] [PubMed] [Google Scholar]
- 25. Hurley RW, Adams MCB, Barad M, Bhaskar A, Bhatia A, Chadwick A, et al. Consensus practice guidelines on interventions for cervical spine (facet) joint pain from a multispecialty international working group. Reg Anesth Pain Med. 2022;47:3–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Campbell L, Smith A, McGregor L, Sterling M. Psychological factors and the development of chronic whiplash‐associated disorders. A systematic review. Clin J Pain. 2018;34:755–768. [DOI] [PubMed] [Google Scholar]
- 27. Baydal‐Bertomeu JM, Page AF, Belda‐Lois JM, Garrido‐Jaén D, Prat JM. Neck motion patterns in whiplash‐associated disorders: quantifying variability and spontaneity of movement. Clin Biomech. 2011;26:29–34. [DOI] [PubMed] [Google Scholar]
- 28. van Eerd M, Patijn J, Lataster A, Rosenquist RW, van Kleef M, Mekhail N, et al. Cervical facet pain. Pain Pract. 2010;10:113–123. [DOI] [PubMed] [Google Scholar]
- 29. van Suijlekom H, Mekhail N, Patel N, van Zundert J, van Kleef M, Patijn J. Whiplash‐associated disorders. Pain Pract. 2010;10:131–136. [DOI] [PubMed] [Google Scholar]
- 30. Huygen F, Kallewaard JW, van Kleef M, van Tulder M, van Boxem K, van Zundert J, et al. Evidence based interventional pain practice: according to clinical diagnoses. 2018. https://richtlijnendatabase.nl/gerelateerde_documenten/f/20783/Evidence%20based%20interventional%20pain%20practice.pdf. [DOI] [PMC free article] [PubMed]
- 31. Huygen F, Kallewaard JW, van Tulder M, van Boxem K, Vissers K, van Kleef M, et al. “Evidence‐based interventional pain medicine according to clinical diagnoses”: update 2018. Pain Pract. 2019;19:664–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Aprill C, Dwyer A, Bogduk N. Cervical zygapophyseal joint pain patterns. II: a clinical evaluation. Spine. 1990;15:458–461. [DOI] [PubMed] [Google Scholar]
- 33. Cooper G, Bailey B, Bogduk N. Cervical zygapophysial joint pain maps. Pain Med. 2007;8:344–353. [DOI] [PubMed] [Google Scholar]
- 34. Fukui S, Ohseto K, Shiotani M, Ohno K, Karawasa H, Naganuma Y, et al. Referred pain distribution of the cervical zygapophyseal joints and cervical dorsal rami. Pain. 1996;68:79–83. [DOI] [PubMed] [Google Scholar]
- 35. Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: a study in normal volunteers. Spine. 1990;15:453–457. [DOI] [PubMed] [Google Scholar]
- 36. Barnsley L, Lord SM, Wallis BJ, Bogduk N. The prevalence of chronic cervical zygapophysial joint pain after whiplash. Spine. 1995;20:20–25. [DOI] [PubMed] [Google Scholar]
- 37. Lord SM, Barnsley L, Wallis BJ, Bogduk N. Chronic cervical zygapophysial joint pain after whiplash. A placebo‐controlled prevalence study. Spina. 1996;121:1737–1744. [DOI] [PubMed] [Google Scholar]
- 38. Chen H, Yang KH, Wang Z. Biomechanics of whiplash injury. Chin J Traumatol. 2009;12:305–314. [PubMed] [Google Scholar]
- 39. Krafft M, Kullgren A, Lie A, Nygren A, Tingvall C. The effects of emergency breaking on fatal and serious injuries. J Traffic Med. 1997;25:89–96. [Google Scholar]
- 40. Spitzer WO, Skovron ML, Salmi LR, Cassidy JD, Duranceau J, Suissa S, et al. Scientific monography of the Quebec Task Force on Whiplash‐associated disorders: redefining “whiplash” and its management. Spine. 1995;15:1S–73S. [PubMed] [Google Scholar]
- 41. Sterling M. A proposed new classification system for whiplash associated disorders – implications for assessment and management. Man Ther. 2004;9:60–70. [DOI] [PubMed] [Google Scholar]
- 42. Sarrami P, Armstrong E, Naylor JM, Harris IA. Factors predicting outcome in whiplash injury: a systematic meta‐review of prognostic factors. J Orthop Traumatol. 2017;18:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Coté P, Wong JJ, Sutton D, Shearer HM, Mior S, Randhawa K, et al. Management of neck pain and associated disorders: a clinial practice guideline from the Ontario protocol for traffic injury management (OPTIMa) collaboration. Eur Spine J. 2016;25:2000–2022. [DOI] [PubMed] [Google Scholar]
- 44. King W, Lau P, Lees R, Bogduk N. The validity of manual examination in assessing patients with neck pain. Spine J. 2007;7:22–26. [DOI] [PubMed] [Google Scholar]
- 45. Schneider GM, Jull G, Thomas K, Smith A, Emery C, Faris P, et al. Intrarater and interrater reliability of select clinical tests in patients referred for diagnostic facet joint blocks in the cervical spine. Arch Phys Med Rehabil. 2013;94:1628–1634. [DOI] [PubMed] [Google Scholar]
- 46. Schneider GM, Jull G, Thomas K, Smith A, Emery C, Faris P, et al. Derivation of a clinical decision guide in the diagnosis of cervical facet joint pain. Arch Phys Med Rehabil. 2014;95:1695–1701. [DOI] [PubMed] [Google Scholar]
- 47. van der Donk J, Schouten JS, Passchier J, Romunde LK, Valkenburg HA. The associations of neck pain with radiological abnormalities of the cervical spine and personality traits in a general population. J Rheumatol. 1991;18:1884–1889. [PubMed] [Google Scholar]
- 48. Heller CA, Stanley P, Lewis‐Jones B, Heller RF. Value of X ray examinations of the cervical spine. BMJ. 1983;287:1276–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gore DR, Sepic SB, Gardner GM, Murray MP. Neck pain: a long‐term follow‐up of 205 patients. Spine. 1987;12:1–5. [DOI] [PubMed] [Google Scholar]
- 50. Rudy IS, Poulos A, Owen L, Batters A, Kieliszek K, Willox J, et al. The correlation of radiographic findings and patient symptomatology in cervical degenerative joint disease: a cross‐sectional study. Chiropr Man Therap. 2015;23:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kim JH, Sharan A, Cho W, Emam M, Hagen M, Kim SY. The prevalence of asymptomatic cervical and lumbar facet arthropathy: a computed tomography study. Asian Spine J. 2019;13:417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Morishita K, Kasai Y, Uchida A. Hypertrophic change of facet joint in the cervical spine. Med Sci Monit. 2008;14:CR62–CR64. [PubMed] [Google Scholar]
- 53. Tiwari P, Kaur H, Kaur H, Jha V, Singh N, Ashraf A. Prevalence of facet joint arthritis and its association with spinal pain in mountain population – a cross‐sectional study. J Craniovertebr Junction Spine. 2020;11:36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Rydman E, Kasina P, Ponzer S, Järnbert‐Pettersson H. Association between cervical degeneration and self‐perceived nonrecovery after whiplash injury. Spine J. 2019;19:1986–1994. [DOI] [PubMed] [Google Scholar]
- 55. Hechelhammer L, Pfirrmann CWA, Zanetti M, Hodler J, Boos N, Schmid MR. Imaging findings predicting the outcome of cervical facet joint blocks. Eur Radiol. 2007;17:959–964. [DOI] [PubMed] [Google Scholar]
- 56. Le Clec'h Y, Peterson CK, Brunner F, Pfirrmann CWA. Cervical facet joint imaging‐guided injections: a comparison of outcomes in patients referred based on imaging findings vs palpation for pain. J Manipulative Physiol Ther. 2016;39:480–486. [DOI] [PubMed] [Google Scholar]
- 57. Cohen SP, Bajwa ZH, Kraemer JJ, Dragovich A, Williams KA, Stream J, et al. Factors predicting success and failure for cervical facet radiofrequency denervation: a multi‐center analysis. Reg Anesth Pain Med. 2007;32:495–503. [DOI] [PubMed] [Google Scholar]
- 58. Daimon K, Fujiwara H, Nishiwaki Y, Okada E, Nojiri K, Shimizu K, et al. A 20‐year prospective longitudinal MRI study on cervical spine after whiplash injury: follow‐up of a cross‐sectional study. J Orthop Sci. 2019;24:579–583. [DOI] [PubMed] [Google Scholar]
- 59. Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic‐resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:1178–1184. [PubMed] [Google Scholar]
- 60. Okada E, Matsumoto M, Ichihara D, Chiba K, Toyama Y, Fujiwara H, et al. Aging of the cervical spine in healthy volunteers: a 10‐year longitudinal magnetic resonance imaging study. Spine (Phila Pa 1976). 2009;34:706–712. [DOI] [PubMed] [Google Scholar]
- 61. Uhrenholt L, Grunnet‐Nilsson N, Hartvigsen J. Cervical spine lesions after road traffic accidents: a systematic review. Spine. 2002;27:1934–1941. [DOI] [PubMed] [Google Scholar]
- 62. Manchikanti L, Kosanovic R, Cash KA, Pampati V, Soin A, Kaye AD, et al. Assessment of prevalence of cervical facet joint pain with diagnostic cervical medial branch block: analysis based on chronic pain model. Pain Physician. 2020;23:531–540. [PubMed] [Google Scholar]
- 63. Cohen SP, Strassels SA, Kurihara C, Forsythe A, Buckenmaier CC 3rd, McLean B, et al. Randomized study assessing the accuracy of cervical facet joint nerve (medial branch) blocks using different injectate volumes. Anesthesiology. 2010;112:144–152. [DOI] [PubMed] [Google Scholar]
- 64. Bureau NJ, Moser TP, Gouvion A, Julien AS. CT fluoroscopy‐guided transforaminal and intra‐articular facet steroid injections for the treatment of cervical radiculopathy: injectate distribution patterns and association with clinical outcome. Eur Radiol. 2020;30:5933–5941. [DOI] [PubMed] [Google Scholar]
- 65. Freire V, Grabs D, Lepage‐Saucier M, Moser TP. Ultrasound‐guided cervical facet joint injections: a viable substitution for fluoroscopy‐guided injections? J Ultrasound Med. 2016;35:1253–1258. [DOI] [PubMed] [Google Scholar]
- 66. Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence‐based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12:699–802. [PubMed] [Google Scholar]
- 67. Manchikanti L, Falco FJE, Singh V, Benyamin RM, Racz GB, Helm S 2nd, et al. An udate of comprehensive evidence‐based guidelines for interventional techniques in chronic spinal pain. Part I: introduction and general considerations. Pain Physician. 2013;16:S1–S48. [PubMed] [Google Scholar]
- 68. Manchikanti L, Abdi S, Atluri S, Benyamin RM, Boswell MV, Buenaventura RM, et al. An update of comprehensive evidence‐based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician. 2013;16:S49–S283. [PubMed] [Google Scholar]
- 69. Cohen SP, Moon JY, Brummett CM, White RL, Larkin TM. Medial branch blocks or intra‐articular injections as a prognostic tool before lumbar facet radiofrequency denervation: a multicenter, case‐control study. Reg Anesth Pain Med. 2015;40:376–383. [DOI] [PubMed] [Google Scholar]
- 70. Burnham T, Conger A, Salazar F, Petersen R, Kendall R, Cunningham S, et al. The effectiveness of cervical medial branch radiofrequency ablation for chronic facet joint syndrome in patients selected by a practical medial branch block paradigm. Pain Med. 2020;20:2071–2076. [DOI] [PubMed] [Google Scholar]
- 71. Holz SC, Sehgal N. What is the correlation between facet joint radiofrequency outcome and response to comparative medial branch blocks? Pain Physician. 2016;19:163–172. [PubMed] [Google Scholar]
- 72. Burnham T, Conger A, Kuo K, Lider J, Caragea M, Kendall R, et al. Comparison of the effectiveness of cervical medial branch radiofrequency ablation for chronic facet joint syndrome in patients selected by a common medial branch block paradigm. Interv Pain Med. 2022;1(1):100032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Shin W‐R, Kim H‐I, Shin D‐G, Shin D‐A. Radiofrequency neurotomy of cervical medial branches for chronic cervicobrachialgia. J Korean Med Sci. 2006;21:119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Burnham T, Clements N, Conger A, Kuo K, Lider J, Caragea M, et al. A comparison of the effectiveness of cervical medial branch radiofrequency ablation for chronic facet joint syndrome in patients selected by two common medial branch block paradigms. Interv Pain Med. 2022;1(2):100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Cohen SP, Bhaskar A, Bhatia A, Buvanendran A, Deer T, Garg S, et al. Consensus practice guidelines on interventions for lumbar facet joint pain from a multispecialty, international working group. Reg Anesth Pain Med. 2020;45:424–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Derby R, Melnik I, Lee J‐E, Lee S‐H. Correlation of lumbar medial branch neurotomy results with diagnostic medial branch block cutoff values to optimize therapeutic outcome. Pain Med. 2012;13:1533–1546. [DOI] [PubMed] [Google Scholar]
- 77. Cohen SP, Williams KA, Kurihara C, Nguyen C, Shields C, Kim P, et al. Multicenter, randomized, comparative cost‐effectiveness study comparing 0, 1, and 2 diagnostic medial branch (facet joint nerve) block treatment paradigms before lumbar facet radiofrequency denervation. Anesthesiology. 2010;113:395–405. [DOI] [PubMed] [Google Scholar]
- 78. Provenzano DA, Leech JE, Kilgore JS, Sugden LA. Evaluation of lumbar medial branch blocks: how does the second block influence progression to radiofrequency ablation? Reg Anesth Pain Med. 2022;47:719–721. [DOI] [PubMed] [Google Scholar]
- 79. Kazeminasab S, Nejadghaderi SA, Amiri P, Pourfathi H, Araj‐Khodaei M, Sullman MJM, et al. Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 2022;23:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Mork R, Falkenberg HK, Fostervold KI, Schiotz Thorud HM. Discomfort glare and psychological stress during computer work: subjective responses and associations between neck pain and trapezius muscle blood flow. Int Arch Occup Environ Health. 2022;93:29–42. [DOI] [PubMed] [Google Scholar]
- 81. Katsuura Y, Bruce J, Taylor S, Gullota L, Kim HJ. Overlapping, masquerading, and causative cervical spine and shoulder pathology: a systematic review. Global Spine J. 2020;10:195–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Sutton DA, Coté P, Wong JJ, Varatharajan S, Randhawa KA, Yu H, et al. Is multimodel care effective for the management of patients with whiplash‐associated disorders or neck pain and associated disorders? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Spine J. 2016;16:1541–1565. [DOI] [PubMed] [Google Scholar]
- 83. Southerst D, Nordin MC, Coté P, Shearer HM, Varatharajan S, Yu H, et al. Is exercise effective for the management of neck pain and associated disorders or whiplash‐associated disorders? A systematic review by the Ontario protocol for traffic injury management (OPTIMa) Collaboration. Spine J. 2016;16:1503–1523. [DOI] [PubMed] [Google Scholar]
- 84. Wong JJ, Coté P, Shearer HM, Yu H, Varatharajan S, Southerst D, et al. Clinical practice guidelines for the management of conditions related to traffic collisions: a systematic review by the OPTIMa collaboration. Disabil Rehabil. 2015;37:471–489. [DOI] [PubMed] [Google Scholar]
- 85. Chrcanovic B, Larsson J, Malmström E‐M, Westergren H, Häggman‐Henrikson B. Exercise therapy for whiplash‐associated disorders: a systemic review and meta‐analysis. Scand J Pain. 2022;22:232–261. [DOI] [PubMed] [Google Scholar]
- 86. Anderson C, Yeung E, Tong T, Reed N. A narrative review on cervical interventions in adults with chronic whiplash‐associated disorder. BMJ Open Sport Exerc Med. 2018;4:e000299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Corp N, Mansell G, Stynes S, Wynne‐Jones G, Morsø L, Hill JC, et al. Evidence‐based treatment recommendations for neck and low back pain across Europe: a systematic review of guidelines. Eur J Pain. 2021;25:275–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Andersen TE, Ravn SL, Mejldal A, Roessler KK. Values‐based cognitive behavioural therapy for the prevention of chronic whiplash associated disorders: a randomized controlled trial. Eur J Pain. 2022;26:1256–1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hsieh LF, Hong CZ, Chern SH, Chen CC. Efficacy and side effects of diclofenac patch in treatment of patients with myofascial pain syndrome of the upper trapezius. J Pain Symptom Manage. 2010;39:116–125. [DOI] [PubMed] [Google Scholar]
- 90. Predel HG, Giannetti B, Pabst H, Schaefer A, Hug AM, Burnett I. Efficacy and safety of diclofenac diethylamine 1.16% gel in acute neck pain: a randomized, double‐blind, placebo‐controlled study. BMC Musculoskelet Disord. 2013;14:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, Grimm RH. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Ann Intern Med. 2012;156:1–10. [DOI] [PubMed] [Google Scholar]
- 92. Nikles J, Keijzers G, Mitchell G, Farrell SF, Perez S, Schug S, et al. Pregabalin vs placebo to prevent chronic pain after whiplash injury in at‐risk individuals: results of a feasibility study for a large randomised controlled trial. Pain. 2022;163:e274–e284. [DOI] [PubMed] [Google Scholar]
- 93. Ritchie C, Hollingworth SA, Warren J, Sterling M. Medicine use during acute and chronic postinjury periods in whiplash‐injured individuals. Pain. 2019;160:844–851. [DOI] [PubMed] [Google Scholar]
- 94. Langevin P, Lowcock J, Weber J, Nolan M, Gross AR, Peloso PM, et al. Botulinum toxin intramuscular injections for neck pain: a systematic review and metaanalysis. J Rheumatol. 2011;38:203–214. [DOI] [PubMed] [Google Scholar]
- 95. Langevin P, Peloso PM, Lowcock J, Nolan M, Weber J, Gross A, et al. Botulinum toxin for subacute/chronic neck pain. Cochrane Database Syst Rev. 2011;7:CD008626. [DOI] [PubMed] [Google Scholar]
- 96. Zhang T, Adatia A, Zarin W, Moitri M, Vijenthira A, Chu R, et al. The efficacy of botulinum toxin type A in managing chronic musculoskeletal pain: a systematic review and meta‐analysis. Inflammopharmacology. 2011;19:21–34. [DOI] [PubMed] [Google Scholar]
- 97. Dory MA. Arthrography of the cervical facet joints. Radiology. 1983;148:379–382. [DOI] [PubMed] [Google Scholar]
- 98. Lee DW, Huston C. Fluoroscopically‐guided cervical zygapophyseal therapeutic joint injections may reduce the need for radiofrequency. Pain Physician. 2018;21:E661–E665. [PubMed] [Google Scholar]
- 99. Smith AD, Jull G, Schneider G, Frizzell B, Hooper RA, Sterling M. A comparison of physical and psychological features of responders and non‐responders to cervical facet blocks in chronic whiplash. BMC Musculoskelet Disord. 2013;14:313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Hove B, Gyldensted C. Cervical analgesic facet joint arthrography. Neuroradiology. 1990;32:456–459. [DOI] [PubMed] [Google Scholar]
- 101. Roy DF, Fleury J, Fontaine SB, Dussault RG. Clinical evaluation of cervical facet joint infiltration. Can Assoc Radiol J. 1988;39:118–120. [PubMed] [Google Scholar]
- 102. Barnsley L, Lord SM, Wallis BJ, Bogduk N. Lack of effect of intraarticular corticosteroids for chronic pain in the cervical zygapophyseal joints. N Engl J Med. 1994;330:1047–1050. [DOI] [PubMed] [Google Scholar]
- 103. Park S‐C, Kim K‐H. Effect of adding cervical facet joint injections in a multimodal treatment program for long‐standing cervical myofascial pain syndrome with referral pain patterns of cervical facet joint syndrome. J Anesth. 2012;26:738–745. [DOI] [PubMed] [Google Scholar]
- 104. Barnsley L, Lord S, Bogduk N. Comparative local anaesthetic blocks in the diagnosis of cervical zygapophysial joint pain. Pain. 1993;55:99–106. [DOI] [PubMed] [Google Scholar]
- 105. Lord SM, Barnsley L, Bogduk N. The utility of comparative local anesthetic blocks versus placebo‐controlled blocks for the diagnosis of cervical zygapophysial joint pain. Clin J Pain. 1995;11:208–213. [DOI] [PubMed] [Google Scholar]
- 106. Manchikanti L, Singh V, Falco FJE, Cash KA, Fellows B. Comparative outcomes of a 2‐year follow‐up of cervical medial branch blocks in management of chronic neck pain: a randomized, double‐blind controlled trial. Pain Physician. 2010;13:437–450. [PubMed] [Google Scholar]
- 107. Hussain A, Usmani H, Huda MF. Comparison of cervical medial branch nerve block versus trigger point injection in patients with chronic neck pain. Indian J Pain. 2020;34:27–33. [Google Scholar]
- 108. Bisby MA. Inhibition of axonal transport in nerves chronically treated with local anesthetics. Exp Neurol. 1975;47:481–489. [DOI] [PubMed] [Google Scholar]
- 109. Cassuto J, Sinclair R, Bonderovic M. Anti‐inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand. 2006;50:265–282. [DOI] [PubMed] [Google Scholar]
- 110. MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Cervical medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2012;13:647–654. [DOI] [PubMed] [Google Scholar]
- 111. Speldewinde GC. Outcomes of percutaneous zygapophyseal and sacroiliac joint neurotomy in a community setting. Pain Med. 2011;12:209–218. [DOI] [PubMed] [Google Scholar]
- 112. van Eerd M, de Meij N, Dortangs E, Kessels A, van Zundert J, Lataster A, et al. Long‐term follow‐up of cervical facet medial branch radiofrequency treatment with the single posterior‐lateral approach: an exploratory study. Pain Pract. 2014;14:8–15. [DOI] [PubMed] [Google Scholar]
- 113. McDonald GJ, Lord SM, Bogduk N. Long‐term follow‐up of patients treated with cervical radiofrequency neurotomy for chronic neck pain. Neurosurgery. 1999;45:61–67. [DOI] [PubMed] [Google Scholar]
- 114. Barnsley L. Percutaneous radiofrequency neurotomy for chronic neck pain: outcomes in a series of consecutive patients. Pain Med. 2005;6:282–286. [DOI] [PubMed] [Google Scholar]
- 115. Royal MA, Bhakta B, Gunyea I, Jenson M, Movva V, Taqi D, et al. Radiofrequency neurolysis for facet arthropathy: a retrospective case series and review of the literature. Pain Pract. 2002;2:47–52. [DOI] [PubMed] [Google Scholar]
- 116. Husted DS, Orton D, Schofferman J, Kine G. Effectiveness of repeated radiofrequency neurotomy for cervical facet joint pain. J Spinal Disord Tech. 2008;21:406–408. [DOI] [PubMed] [Google Scholar]
- 117. Manchikanti L, Kosanovic R, Pampati V, Sanapati MR, Hirsch JA. Outcomes of cervical therapeutic medial branch blocks and radiofrequency neurotomy: clinical outcomes and cost utility are equivalent. Pain Physician. 2022;25:35–47. [PubMed] [Google Scholar]
- 118. Duff P, Das B, McCrory C. Percutaneous radiofrequency rhizotomy for cervical zygapophyseal joint mediated neck pain: a retrospective review of outcomes in forty‐four cases. J Back Musculoskelet Rehabil. 2016;29:1–5. [DOI] [PubMed] [Google Scholar]
- 119. Akgul MH, Akgun MY. Effect of radiofrequency denervation on pain severity among patients with cervical, thoracic or lumbar spinal pain: a clinical retrospective study. Heliyon. 2022;8:e10755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Sapir DA, Gorup JM. Radiofrequency medial branch neurotomy in litigant and nonlitigant patients with cervical whiplash. Spine. 2001;26:E628–E673. [DOI] [PubMed] [Google Scholar]
- 121. Smith AD, Jull G, Schneider G, Frizzell B, Hooper RA, Sterling M. Cervical radiofrequency neurotomy reduces central hyperexcitability and improves neck movement in individuals with chronic whiplash. Pain Med. 2014;15:128–141. [DOI] [PubMed] [Google Scholar]
- 122. Smith AD, Jull G, Schneider G, Frizzell B, Hooper RA, Sterling M. Modulation of cervical facet joint nociception and pain attenuates physical and psychological features of chronic whiplash: a prospective study. PM R. 2015;7:913–921. [DOI] [PubMed] [Google Scholar]
- 123. Prushansky T, Pevzner E, Gordon C, Dvir Z. Cervical radiofrequency neurotomy in patients with chronic whiplash: a study of multiple outcome measures. J Neurosurg Spine. 2006;4:365–373. [DOI] [PubMed] [Google Scholar]
- 124. Lord SM, Barnsley L, Wallis BJ, McDonald G, Bogduk N. Percutaneous radio‐frequency neurotomy for chronic cervical zygapophyseal‐joint pain. N Engl J Med. 1996;335:1721–1726. [DOI] [PubMed] [Google Scholar]
- 125. van Eerd M, de Meij N, Kessels A, Patijn J, Weber W, Wintraecken V, et al. Efficacy and long‐term effect of radiofrequency denervation in patients with clinically diagnosed cervical facet joint pain. Spine. 2021;46:285–293. [DOI] [PubMed] [Google Scholar]
- 126. Smith AD, Jull G, Schneider G, Frizzell B, Hooper RA, Dunne‐Proctor R, et al. Cervical radiofrequency neurotomy reduces psychological features in individuals with chronic whiplash symptoms. Pain Physician. 2014;17:265–274. [PubMed] [Google Scholar]
- 127. Wallis BJ, Lord SM, Bogduk N. Resolution of psychological distress of whiplash patients following treatment by radiofrequency neurotomy: a randomised, double‐blind, placebo‐controlled trial. Pain. 1997;73:15–22. [DOI] [PubMed] [Google Scholar]
- 128. Garvey TA, Transfeldt EE, Malcolm JR, Kos P. Outcome of anterior cervical discectomy and fusion as perceived by patients treated for dominant axial‐mechanical cervical spine pain. Spine. 2002;27:1887–1895. [DOI] [PubMed] [Google Scholar]
- 129. Palit M, Schofferman J, Goldthwaite N, Reynolds J, Kerner M, Keaney D, et al. Anterior discectomy and fusion for the management of neck pain. Spine. 1999;24:2224–2228. [DOI] [PubMed] [Google Scholar]
- 130. Oliver JD, Goncalves S, Kerezoudis P, Alvi MA, Freedman BA, Nassr A, et al. Comparison of outcomes for anterior cervical discectomy and fusion with or without anterior plate fixation. Spine. 2018;43:E413–E422. [DOI] [PubMed] [Google Scholar]
- 131. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. Complications of fluoroscopically directed facet joint nerve blocks: a prospective evaluation of 7,500 episodes with 43,000 nerve blocks. Pain Physician. 2012;15:E143–E150. [PubMed] [Google Scholar]
- 132. Park KD, Lim D‐J, Lee WY, Ahn J, Park Y. Ultrasound versus fluoroscopy‐guided cervical medial branch block for the treatment of chronic cervical facet joint pain: a retrospective comparative study. Skeletal Radiol. 2017;46:81–91. [DOI] [PubMed] [Google Scholar]
- 133. Manchikanti L, Kaye AD, Soin A, Albers SL, Beall D, Latchaw R, et al. Comprehensive evidence‐based guidelines for facet joint interventions in the management of chronic spinal pain: American Society of Interventional Pain Physicians (ASIPP) guidelines facet joint interventions 2020 guidelines. Pain Physician. 2020;23:S1–S127. [PubMed] [Google Scholar]
- 134. Rathmell JP, Michna E, Fitzgibbon DR, Stephens L, Posner KL, Domino KB. Injury and liability associated with cervical procedures for chronic pain. Anesthesiology. 2011;114:918–926. [DOI] [PubMed] [Google Scholar]
- 135. Rathmell JP, Benzon HT, Dreyfuss P, Huntoon M, Wallace M, Baker R, et al. Safeguards to prevent neurologic complications after epidural steroid injections: consensus opinions from a multidisciplinary working group and national organizations. Anesthesiology. 2015;122:974–984. [DOI] [PubMed] [Google Scholar]
- 136. Fitzgibbon DR, Posner KL, Domino KB, Caplan RA, Lee LA, Cheney FW. Chronic pain management: American Society of Anesthesiologists closed claims project. Anesthesiology. 2004;100:98–105. [DOI] [PubMed] [Google Scholar]
- 137. Abrecht CR, Saba R, Greenberg P, Rathmell JP, Urman RD. A contemporary medicolegal analysis of outpatient interventional pain procedures: 2009–2016. Anesth Analg. 2019;129:255–262. [DOI] [PubMed] [Google Scholar]
- 138. Pollak KA, Stephens LS, Posner KL, Rathmell JP, Fitzgibbon DR, Dutton RP, et al. Trends in pain medicine liability. Anesthesiology. 2015;123:1133–1141. [DOI] [PubMed] [Google Scholar]
- 139. van Eerd M, Lataster A, Sommer M, Patijn J, van Kleef M. A modified posterolateral approach for radiofrequency denervation of the medial branch of the cervical segmental nerve in cervical facet joint pain based on anatomical consideration. Pain Pract. 2016;17:596–603. [DOI] [PubMed] [Google Scholar]
- 140. Sluijter ME, Koetsveld‐Baart CC. Interruption of pain pathways in the treatment of the cervical syndrome. Anaesthesia. 1980;35:302–307. [DOI] [PubMed] [Google Scholar]
- 141. Bogduk N, International Spine Intervention Society . Cervical medial branch thermal radiofrequency neurotomy. Practice guidelines: spinal diagnostic and treatment procedures. 2nd ed.. Hinsdale: IPSIS; 2013. [Google Scholar]
- 142. Bogduk N, Lord SM. Cervical zygapophysial joint pain. Neurosurg Q. 1998;8:107–117. [Google Scholar]
- 143. Vallejo R. Cervical facet radiofrequency. Tech Reg Anesth Pain Manag. 2005;9:81–85. [Google Scholar]
- 144. Künzle A, van Kuijk SMJ, Koetsier E. Efficacy of cervical facet joint radiofrequency ablation using a multitined cannula, a technical note, and observational study. Pain Physician. 2023;26:E353–E361. [PubMed] [Google Scholar]
- 145. Cheng J, Gutenberg LV, Dalton JE. Comparative long‐term outcomes of lateral versus posterior approach to cervical facet medial branch radiofrequency ablation. (American Academy of Pain Medicine 2013 meeting abstract #179). Pain Med. 2013;2013(144):586. [Google Scholar]
- 146. Loh JT, Nicol AL, Elashoff D, Ferrante FM. Efficacy of needle‐placement technique in radiofrequency ablation for treatment of lumbar facet arthropathy. J Pain Res. 2015;8:687–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. De Andrés Ares J, Gilsanz F. Randomized pragmatic pilot trial comparing perpendicular thin electrode versus parallel thick electrode approaches for lumbar medial branch neurotomy in facetogenic low back pain. Pain Pract. 2020;20:889–907. [DOI] [PubMed] [Google Scholar]
- 148. Provenzano DA, Lassila HC, Somers D. The effect of fluid injection on lesion size during radiofrequency treatment. Reg Anesth Pain Med. 2010;35:338–342. [DOI] [PubMed] [Google Scholar]
- 149. Niño AO, Lasa OM, Fabre CG, Nebrada‐Clavo CL, Ferreira‐Dos‐Santos G, Armand‐Ugon R. Dropped head syndrome after bilateral cervical radiofrequency ablation. A case report and literature review. Interv Pain Med. 2024;3:1004109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
File S1
Data Availability Statement
Data sharing is not applicable, as no new data were created or analyzed in this study.


