Abstract
Purpose
To analyze the outcomes of corneal transplantation procedures over a 13-year period at Farabi Eye Hospital, Tehran, Iran, to identify trends and determinants influencing the frequency and success of primary and re-transplantations.
Methods
Utilizing a comprehensive dataset from the hospital’s Hospital Information System, the study reviewed the records of 8,378 patients who underwent corneal transplants between 2009 and 2022. This analysis included demographic information, surgical details, and follow-up data. Statistical methods were applied to assess the impact of variables such as age, gender, surgeon experience, and surgical techniques on the likelihood of re-transplantation.
Results
Of the 8,378 transplants, 7,660 (91.4%) were primary procedures while 718 (8.6%) involved re-transplantation. The most common primary transplant was penetrating keratoplasty (PKP, 50.3%), followed by Descemet’s stripping endothelial keratoplasty (DSAEK, 29.3%), and deep anterior lamellar keratoplasty (DALK, 18.5%). Analysis revealed no significant association between re-transplantation rates and patient gender or nationality. Older recipient age correlates with higher re-transplantation rates, likely due to reduced regenerative capacity and increased comorbidities in older patients. Pre-transplant comorbidities (e.g., keratoconus, ulcers), concurrent surgeries (e.g., vitrectomy), and prior procedures (e.g., glaucoma surgeries, IOL implantation) significantly increase re-transplantation risk, likely due to additional ocular stress and inflammation.
Conclusion
The study highlights the importance of patient age, surgeon experience, and the choice of surgical technique in the success rates of corneal transplants. These factors are crucial for optimizing patient outcomes and minimizing the necessity for re-transplantations.
Keywords: Corneal transplantation, Re-transplantation rates, Surgical outcomes, Penetrating keratoplasty (PKP), Retrospective analysis
Introduction
Corneal blindness, a significant global health concern, ranks as the third leading cause of vision loss worldwide, trailing only cataract and glaucoma [1]. Affecting millions, with an estimated 10 million individuals experiencing bilateral corneal blindness [2, 3], this condition necessitates effective interventions to alleviate its burden.
For over a century, corneal transplantation has emerged as a beacon of hope for those suffering from corneal blindness [4]. Since its inception, this procedure has evolved into the most prevalent form of allogeneic transplantation globally. Individuals receive corneal transplants for a diverse array of reasons, which demonstrate variations both geographically and over time [5]. These variations in the prevalence of underlying causes for corneal transplantation can be attributed to a multitude of factors including shifts in disease patterns, advancements in medical understanding and technology, as well as changes in environmental and demographic factors [6]. This highlights the dynamic nature of the indications for corneal transplantation, which are influenced by both spatial and temporal factors. While the underlying etiologies may differ across populations, the ultimate goal remains consistent: to restore vision and improve quality of life [7].
Over the years, keratoplasty techniques have undergone significant refinement, fueled by innovation in surgical approaches and postoperative management [8]. These advancements have significantly improved graft survival rates, paving the way for wider accessibility and enhanced efficacy of corneal transplantation worldwide. This continuous evolution underscores the commitment to providing optimal care for individuals suffering from corneal blindness [9, 10].
Traditionally, corneal transplantation has been synonymous with penetrating keratoplasty (PKP), a technique involving the replacement of the entire corneal thickness [11]. While widely practiced, PKP has its limitations, including the risk of immune rejection and suboptimal graft integration. To address these challenges, lamellar keratoplasty (LK) re-emerged, offering a less invasive alternative [12]. LK selectively replaces specific layers of the cornea, preserving healthy tissue and potentially reducing the risk of complications associated with full-thickness replacement. Over the past decade, LK has experienced rapid progress, driven by conceptual advancements and the development of sophisticated instrumentation [3]. This evolution has solidified LK’s position as a valuable alternative to PKP, offering tailored treatment options for a wider range of corneal conditions. The advent of selective corneal transplantation, where only the diseased corneal layers are replaced, has ushered in a new era of corneal graft surgery [13]. This approach offers numerous advantages over traditional full-thickness transplantation, including a reduced risk of intraoperative complications, preservation of globe integrity, and a lower incidence of postoperative graft rejection [14]. Among the various selective techniques, Deep Anterior Lamellar Keratoplasty (DALK) stands out. However, DALK is not without its challenges. Rupture of Descemet’s membrane and graft rejection, while uncommon, remain significant concerns in DALK procedures [15, 16]. Endothelial keratoplasty (EK), another form of lamellar keratoplasty, has emerged as a compelling alternative to penetrating keratoplasty for various endothelial disorders and focal dystrophy [17]. EK offers several advantages, including faster visual recovery, shorter surgical duration, less corneal tissue removal, fewer suture-related complications, and a reduced risk of astigmatism. Consequently, EK has gained significant traction in developed countries, accounting for a substantial proportion of corneal transplants [3].
Hospital Information Systems (HIS) play a pivotal role in supporting a wide array of operations and activities within healthcare institutions. By enhancing data quality and accessibility, HIS aim to facilitate efficient and effective decision-making, ultimately improving the delivery of healthcare services [18].
This retrospective large scale study leverages the robust HIS of Farabi Eye Hospital in Tehran, Iran, a leading tertiary referral and educational center. The study encompasses a comprehensive 13-year dataset (2009–2022) of corneal transplantation and re-transplantation procedures, providing valuable insights into long-term outcomes and potential risk factors associated with these procedures.
Materials and methods
This retrospective study delves into the outcomes of corneal transplantation procedures performed at Farabi Eye Hospital in Tehran, Iran, over a significant period. The study draws upon a robust dataset spanning from 2009 to 2022, extracted from the hospital’s comprehensive HIS and meticulously maintained inpatient/outpatient medical records.
The study population encompasses two distinct cohorts. The first cohort comprises individuals who underwent primary corneal transplantation at the hospital between 2008 and 2011. Researchers utilized the HIS to access and analyze the recorded data of these patients, encompassing pre- and post-transplantation hospitalization details, treatment interventions, and follow-up data. The second cohort focuses on patients who underwent corneal re-transplantation at Farabi Eye Hospital between 2009 and 2022. By leveraging the HIS and meticulously reviewing corresponding inpatient/outpatient records, researchers compiled a comprehensive dataset for this cohort. This data includes demographic information, hospitalization records, medical interventions administered before and after re-transplantation, and subsequent follow-up details.
Given the retrospective nature of this study involving the analysis of existing patient data, stringent ethical considerations were prioritized throughout the research process. The study protocol was reviewed and approved by the Institutional Review Board (IRB) of Tehran University of Medical Science, ensuring adherence to all relevant ethical guidelines and regulations. To protect patient privacy and confidentiality, all data were anonymized during collection and analysis. No personally identifiable information was accessed or utilized in this study. The research team adhered to strict data security protocols to prevent unauthorized access or disclosure of sensitive patient information.
Results
Over a 13-year period, the data of 8,378 patients who had corneal transplants conducted at Farabi Eye Hospital, Tehran were reviewed. The vast majority of these procedures, 7,660 (91.4%), were primary transplants, while 718 (8.6%) were re-transplantations. Table 1 provides a summary of patient demographics and transplant details collected from this study over a 13-year period. The study revealed that 8.4% of the transplants were performed on non-Iranian patients, highlighting the hospital’s reputation as a regional center of excellence for corneal transplantation. However, statistical analysis demonstrated no significant association between patient nationality and the likelihood of re-transplantation (P = 0.654). Out of a total of 8,378 patients, 5,371 (64.1%) were male and there was no statistically significant relationship between patient gender and the occurrence of re-transplantation (P = 0.788).
Table 1.
Summary of patient demographics and transplant details
| Data | ||
|---|---|---|
| Patients Reviewed | Primary | 7,660 (91.4%) |
| Re-transplantations | 718 (8.6%) | |
| Total | 8,378 (100%) | |
| Mean age ± SD | 49.4 ± 22.7 years | |
| Gender | Male | 5,371 (64.1%) |
| Female | 3,007 (35.9%) | |
| Eye | Right Eye | 4,340 (51.8%) |
| Left Eye | 4,038 (48.2%) | |
To investigate potential risk factors associated with re-transplantation, the study stratified all transplant recipients into three age groups. Among the 8,378 individuals surveyed, 637 (7.6%) were aged 0–19 years, 3,184 (38.0%) were young adults aged 20–44 years, and 4,557 (54.4%) were middle-aged or older, aged 45 years and above. There was a statistically significant relationship between patient age group and the likelihood of re-transplantation (P < 0.001).
The study also examined the relationship between the type of anesthesia used during transplantation and re-transplantation rates. The majority of transplants, 85.9%, were performed under general anesthesia, while the remaining cases utilized intravenous sedation or local anesthesia administered by an anesthesiologist and technician. However, statistical analysis indicated no significant association between the type of anesthesia employed and the occurrence of re-transplantation (P = 0.286).
Also, the data analyses revealed a statistically significant relationship between the surgeon’s level of experience and the likelihood of re-transplantation (P = 0.028). Specifically, 36.9% of transplants were performed by attending physicians, while 63.1% were conducted by corneal fellowship trainees. Notably, a higher percentage of patients who underwent transplantation by attending physicians required re-transplantation. This finding can likely be attributed to attending physicians often managing more complex cases and high-risk transplants that may be beyond the scope of fellowship trainees.
Analysis of the geographic distribution of transplant recipients revealed that 14.8% resided in rural villages, while the majority hailed from various cities across Iran. Statistical analysis, however, demonstrated no significant association between a patient’s place of residence (urban versus rural) or the distance from their residence to the transplant hospital and the likelihood of re-transplantation (P = 0.323 and P = 0.771, respectively). This finding suggests that geographic factors do not play a substantial role in the long-term outcomes of corneal transplants.
Over the past 13 years at Farabi Eye Hospital, there were 1,553 DALK transplants (18.5%), 4,217 PKP transplants (50.3%), 2,458 Descemet’s Stripping Endothelial Automated Keratoplasty (DSAEK) transplants (29.3%), and 147 Keratolimbal allograft (KLAL) transplants (1.8%), totaling 8,375 transplants. There were significant differences in re-transplantation rates among these techniques (P < 0.001), with PKP associated with the highest rates of re-transplantation, followed by DALK, and DMEK/DSAEK showing the lowest rates. Furthermore, statistical analysis revealed a statistically significant relationship between the type of transplantation procedure performed and the incidence of re-transplantation (P < 0.001).
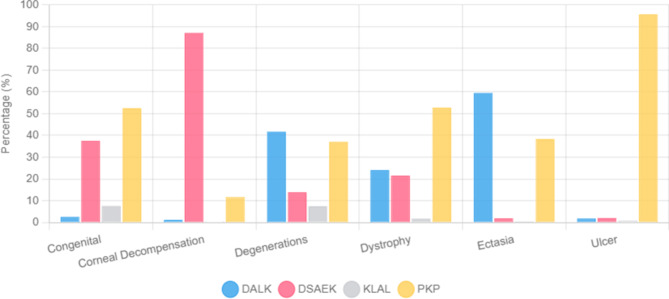
To investigate the influence of the underlying indication for corneal transplantation on re-transplantation rates, the study meticulously categorized a total of 63 primary transplant reasons into six distinct categories. Figure 1 visually depicts the distribution of transplants across these six categories over the 13-year study period at Farabi Eye Hospital. Statistical analysis unveiled a compelling association between the primary transplant indication and the likelihood of re-transplantation. Notably, ten specific causes exhibited a statistically significant relationship with re-transplantation risk: Congenital Causes (P = 0.004), Corneal Deformities (P = 0.030), Ectasia category (P < 0.001), Keratoconus (KCN) (P < 0.001), Endophthalmitis (P = 0.020), Ulcers (P < 0.001), Fungal Keratitis (P < 0.001), Glaucoma (P = 0.015), Infectious Crystalline Keratopathy (ICE) (P = 0.007), Ocular Surface Diseases (P = 0.020).
Fig. 1.
Percent frequency of transplants by 6 categories of primary transplant causes in the last 13 years at Farabi Eye Hospital. DALK: Deep Anterior Lamellar Keratoplasty; DSAEK: Descemet’s Stripping Endothelial Automated Keratoplasty; KLAL: Keratolimbal allograft; PKP: penetrating keratoplasty
Statistical analysis revealed a statistically significant relationship between ten specific types of prior ocular surgeries and an increased risk of re-transplantation. These procedures include: any type of IOL Surgery (P = 0.050), Ahmed glaucoma valve surgery (P = 0.043), Other glaucoma surgeries (P < 0.001), Intrastromal Avastin injection (P < 0.001), Examination under anesthesia (P = 0.018), Suture removal surgery (P = 0.001), Amniotic Membrane Transplantation (AMT) or Conjunctival Flap Surgery (P < 0.001), Blepharorrhaphy or tarsorrhaphy surgery (P < 0.001), Symblepharon surgery (P = 0.005), Pterygium surgery (P = 0.027).
Notably, the study also revealed that in 58.7% of corneal transplants performed, at least one additional ocular surgery was conducted concurrently. However, statistical analysis did not demonstrate a statistically significant relationship between the performance of concurrent surgeries and the incidence of re-transplantation (P = 0.465). This suggests that the act of combining procedures during a single surgical session does not inherently increase the risk of requiring a repeat corneal transplant.
The study categorized all surgeries performed concurrently with the primary corneal transplant into 17 categories. Statistical analysis revealed that four specific concurrent surgical procedures were significantly associated with an increased risk of re-transplantation: AMT or Conj. Flap Surgery (P < 0.001), any surgery associated with keratitis (P = 0.024), Silicone injection (P = 0.041), vitrectomy (anterior/posterior) (P = 0.001).
The study further categorized all surgical procedures performed between the primary corneal transplant and re-transplantation into 36 categories. Statistical analysis identified twelve specific interim surgical interventions significantly associated with an increased re-transplantation risk: AMT or Conj. Flap Surgery (P = 0.028), any type of IOL Surgery (P = 0.002), Phaco + PCIOL (P < 0.002), Artisan or Artiflex surgery (P = 0.033), Strabismus surgery (P = 0.038), Intravitreous injection (P = 0.022), Anterior chamber injection (P = 0.015), Eyelid surgeries (P = 0.030), Re-suture surgery (P = 0.003), Surgeries related to keratitis (P = 0.008), Lensectomy surgery (P = 0.017), Vitrectomy surgery (P < 0.001).
The study also investigated the relationship between medications administered during hospitalization for primary corneal transplantation and re-transplantation rates. Categorizing these medications into 46 categories, statistical analysis revealed a statistically significant association between four specific drugs and an increased re-transplantation risk: cyclosporine eye drop (P = 0.050), remifentanil (P = 0.002), tacrolimus drop (P = 0.005), tacrolimus capsule (P < 0.001).
Discussion
This retrospective study, conducted at Farabi Eye Hospital in Tehran, Iran, analyzed 13 years of corneal transplantation data (2009–2022) to investigate trends and outcomes, including re-transplantation rates.
The study encompassed a substantial cohort of 8,378 corneal transplant recipients.
We examined the differential outcomes associated with DALK, DMEK/DSAEK, and PKP, specifically focusing on patient-specific corneal pathologies. We found that DALK is particularly beneficial for managing anterior stromal diseases, effectively minimizing endothelial rejection risks, which are more prevalent in PKP. Our data also confirmed that DMEK and DSAEK offer significantly lower rejection rates compared to PKP, aligning with the specialized nature of these procedures for endothelial dysfunction. However, the requirement for precise surgical execution in DMEK and DSAEK limits their universal applicability.
Analysis of the gender distribution within this cohort revealed a notable disparity: 64.1% of transplant recipients were male and 35.9% of transplant recipients were female. This finding aligns with previous research conducted by Eghtedari et al. [19], which also reported a higher proportion of male corneal transplant recipients (65%). Similarly, a study by Derkhshan et al. conducted at a hospital in Mashhad, Iran, observed a comparable gender distribution, with 68% male and 32% female recipients [20]. The consistent observation of a higher prevalence of corneal transplantation among men across multiple studies suggests potential underlying factors contributing to this disparity. Differences in gender distribution reported in the literature may stem from a variety of factors, including differences in the prevalence of corneal diseases between genders, cultural and socioeconomic disparities influencing healthcare access, and regional variations in disease patterns. For instance, conditions such as keratoconus and ocular trauma, which are more common in males in certain populations, may contribute to the higher proportion of male recipients reported in some studies [21]. However, in other regions or datasets, these trends may differ due to variations in healthcare-seeking behavior, environmental factors, or differing inclusion criteria for studies.
The present study revealed that the age group with the highest frequency of corneal transplant patients was above 45 years (54.4%), followed by the 20 to 44 years age group (38%), and lastly, the under 19 years age group (7.6%). These findings are consistent with a study by Ostadian et al., which found the highest frequency of corneal transplant patients in the 60 to 70 years and 70 to 80 years age groups, with the lowest frequency in the below 10 years and above 90 years age groups [22]. The average age of transplant recipients in Ostadian et al.‘s study was 50.93 years. Other studies have reported similar average ages for corneal transplant recipients, such as 52 years in Soleimani et al.‘s study [23], and 42 years in Zare et al.‘s study [24]. However, Jafari et al. reported a lower average age of 30.4 years for corneal transplant recipients in their study, with an age range of 5–51 years [25]. These varying average ages and age ranges across different studies highlight the wide range of diseases that can lead to corneal transplantation, affecting individuals across nearly the entire human lifespan. In addition, our analysis revealed that older patients had a higher likelihood of requiring re-transplantation compared to younger patients. This trend is likely due to age-related factors such as reduced regenerative capacity, increased prevalence of systemic and ocular comorbidities, and greater exposure to prior ocular surgeries, all of which can negatively impact graft survival.
The relationship between surgeon experience and corneal transplant outcomes has been a subject of recent investigation. Data from the Australian Corneal Graft Registry (ACGR) suggest that greater surgeon volume and a higher frequency of postoperative follow-up are independently associated with improved corneal allograft survival, echoing observations in solid organ transplantation [26]. However, these findings appear incongruent with the present study’s observation of increased re-transplantation rates among patients operated on by attending surgeons. This discrepancy might be attributed to the unique characteristics of the study cohort and the academic medical center setting. Attending surgeons at this tertiary referral center often manage complex corneal transplant cases that exceed the scope of fellowship training, inherently increasing the risk of complications and subsequent re-transplantation, irrespective of surgeon experience.
Regarding surgical techniques, this study, consistent with several others [20, 24, 27], found PKP to be the predominant method for corneal transplantation. This observation underscores the enduring relevance of PKP as a cornerstone technique in corneal transplantation, particularly within certain geographical contexts. However, it is essential to acknowledge the evolving landscape of corneal surgery. A study conducted by Chan et al. in Toronto, Canada, revealed a significantly higher prevalence of partial thickness keratoplasty (PTK), potentially reflecting variations in regional disease prevalence and access to advanced surgical technologies [28]. It should be noted that our hospital’s status as a regional referral center is a primary reason we predominantly receive more severe cases, contributing to PKP remaining the most prevalent surgery performed in Iran.
These contrasting findings highlight the importance of considering epidemiological nuances and resource availability when interpreting surgical trend data.
The current study identified DSAEK as the second most common corneal transplant procedure performed, following invasive grafting. This finding aligns with observations from Rock et al. at a German eye transplant center, where DSAEK emerged as the most frequently employed technique [29]. However, it’s important to acknowledge the evolving adoption of DSAEK over time. Zare et al. reported a significantly lower prevalence of DSAEK (3.5%), likely reflecting its relative novelty as a corneal grafting method at the time of their study [24]. The increasing popularity of DSAEK in recent years can be attributed, at least in part, to its lower graft rejection rate compared to traditional penetrating keratoplasty.
While anterior lamellar keratoplasty (ALK) was first described in 2002, its adoption at Farabi Eye Hospital has been more limited, accounting for 18.5% of all corneal grafts performed. Several factors might contribute to this lower utilization rate, including the technically demanding nature of the big bubble technique initially used in ALK, its comparatively longer surgical time, the emergence of corneal cross-linking as an alternative treatment for progressive keratoconus, and the steeper learning curve associated with mastering this procedure [30]. Despite these challenges, ongoing research continues to refine ALK techniques, aiming to minimize graft rejection rates, enhance visual outcomes, and ultimately reduce the incidence of graft failure [31]. These advancements hold promise for expanding the role of ALK in corneal transplantation in the future.
This study found that 8.6% of corneal transplant recipients underwent re-transplantation, a figure consistent with rates reported in other investigations. Eghtedari et al. and Soleimani et al. observed re-transplantation rates of 6.38% and 11.5% respectively [19], while Shuja et al. reported a rate of 10.2% [32]. Similarly, a Canadian study by Benson et al. identified a re-transplantation prevalence of 9.91% [33]. While a study by Rezai et al. found a lower re-transplantation rate of 5.2% [34], it is important to note that their study focused specifically on eye bank data and may not fully reflect overall surgical trends. Furthermore, there is evidence suggesting a global increase in corneal re-transplantation rates in recent years, likely driven by the expanding utilization of corneal transplantation procedures [24, 35].
The present study also sought to identify risk factors associated with re-transplantation. Consistent with data from the Australian Corneal Graft Registry (ACGR) and the USA Cornea Disease Study [26, 36], this study revealed a significant association between pre-transplantation ocular inflammation/steroid use and elevated intraocular pressure (IOP)/glaucoma, and the need for subsequent re-transplantation. Specifically, a history of Ahmed glaucoma valve surgery (P = 0.043) or other glaucoma surgeries (P < 0.001) prior to the initial corneal transplant emerged as significant risk factors. Interestingly, while the ACGR report found no independent association between peripheral iridectomy or anterior vitrectomy performed concurrently with transplantation and graft failure [26], this study did identify a statistically significant relationship between vitrectomy (both anterior and posterior) performed at the time of the primary transplant and the occurrence of re-transplantation (P = 0.001). This discrepancy highlights the need for further investigation to clarify the potential influence of surgical adjunctive procedures on long-term corneal graft outcomes.
The influence of lens status on corneal graft outcomes remains a point of ongoing discussion. While the ACGR identified aphakia, whether pre-existing or occurring after full-thickness transplantation, as a risk factor for reduced graft survival, the Cornea Donor Study did not find lens status to be a significant predictor of graft failure [26, 36]. Conversely, the study identifies a correlation between the speed of stripping in Descemet membrane endothelial keratoplasty procedures and clinical outcomes, highlighting that slower stripping speeds lead to wider scroll widths but also result in a more significant reduction in endothelial cell density, potentially impacting long-term graft viability and visual recovery [37].
This study contributes to this dialogue by demonstrating a statistically significant association between any IOL surgery, performed either before or after the primary corneal transplant, and the occurrence of re-transplantation (P = 0.050). Furthermore, specific IOL-related procedures conducted after the primary transplant, including phacoemulsification with posterior chamber IOL implantation (P < 0.002), Artisan or Artiflex surgery (P = 0.033), and lensectomy (P = 0.017), were also significantly linked to re-transplantation.
Recent advancements in EK are focusing on innovative techniques and therapies to minimize associated complications. These developments include Descemet stripping only, cellular therapies, Rho-associated protein kinase inhibitors, gene therapy, bioengineered grafts, endothelial regeneration, and artificial endothelial substitutes. Such interventions provide novel approaches to managing endothelial dysfunction, potentially enhancing the availability of high-quality donor tissues, reducing immune rejection rates, and decreasing dependency on steroid treatments [38, 39].
While large-scale registry studies provide invaluable insights into corneal transplant trends and risk factors, they are not without limitations. Inconsistent reporting of key variables, such as rejection diagnoses, and attrition due to loss to follow-up can impact data accuracy and generalizability over time [40]. Similarly, this study encountered practical limitations inherent to retrospective analyses, including inconsistent follow-up intervals, incomplete patient records, and missing clinical examination data. In addition, the lack of data on Avastin injections and suture removal procedures, due to their non-recording in the hospital’s HIS, represents another limitation of this study. These limitations underscore the need for robust, prospective studies with standardized data collection protocols and high patient retention rates to advance our understanding of corneal transplant outcomes and optimize patient care.
A high percentage of corneal transplantations were primary transplants, highlighting the hospital’s role as a regional center for such procedures. Key findings include no significant gender or nationality effects on re-transplantation rates. However, age and surgeon experience were notable factors; older patients and cases handled by more experienced surgeons, often involving complex conditions, showed higher re-transplantation rates. The type of surgical procedure also significantly affected outcomes, with PKP being the most prevalent method. The findings underscore the importance of careful patient selection and management, especially considering the significant impact of factors such as the surgeon’s experience and the specific transplantation technique on the outcomes of corneal transplantations. Future studies should focus on optimizing surgical techniques and post-operative care strategies to improve the long-term success rates of corneal transplants, potentially reducing the need for re-transplantations.
Acknowledgements
Not applicable.
Author contributions
Mohammad Nasser Hashemian, Mohammad Javad Zia and Hesam Hashemian contributed to the design and implementation of the research. Mohammad Nasser Hashemian, Mohammad Javad Zia, Masoud Khorrami-Nejad, Qaysser Sattar Abed analyzed the results and to the writing of the manuscript. Also, Hesam Hashemian read and approved the final manuscript.
Funding
The authors did not receive any financial support from any public or private sources. The authors have no financial or proprietary interest in a product, method, or material described herein.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The ethical committee of Tehran university of medical sciences approved the protocol of this study and this study adhered to the tenets of the Declaration of Helsinki and HIPAA. As it was a retrospective study, informed consent was waived by the ethical committee of Tehran University of Medical Sciences.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Resnikoff S, Pascolini D, Etya’Ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844–51. [PMC free article] [PubMed] [Google Scholar]
- 2.Mariotti A, Pascolini D. Global estimates of visual impairment. Br J Ophthalmol. 2012;96(5):614–8. [DOI] [PubMed] [Google Scholar]
- 3.Tan DT, Dart JK, Holland EJ, Kinoshita S. Corneal transplantation. Lancet. 2012;379(9827):1749–61. [DOI] [PubMed] [Google Scholar]
- 4.Crawford AZ, Patel DV, McGhee CN. A brief history of corneal transplantation: from ancient to modern. Oman J Ophthalmol. 2013;6(Suppl 1):S12–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh R, Gupta N, Vanathi M, Tandon R. Corneal transplantation in the modern era. Indian J Med Res. 2019;150(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, et al. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol. 2016;134(2):167–73. [DOI] [PubMed] [Google Scholar]
- 7.Prem Senthil M, Chakraborty R, Lim J. Assessment of patient-reported outcome measures used in corneal transplantation: a systematic review. Clin Experimental Optometry. 2022;105(8):783–92. [DOI] [PubMed] [Google Scholar]
- 8.Singh R, Gupta N, Vanathi M, Tandon R. Corneal transplantation in the modern era. Indian J Med Res. 2019;150(1):7–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malleron V, Bloch F, Zevering Y, Vermion J-C, Semler-Collery A, Goetz C, et al. Evolution of corneal transplantation techniques and their indications in a French corneal transplant unit in 2000–2020. PLoS ONE. 2022;17(4):e0263686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alio JL, Montesel A, El Sayyad F, Barraquer RI, Arnalich-Montiel F, Del Barrio JLA. Corneal graft failure: an update. Br J Ophthalmol. 2020;105(8):1049-58. [DOI] [PubMed]
- 11.Rahman I, Carley F, Hillarby C, Brahma A, Tullo A. Penetrating keratoplasty: indications, outcomes, and complications. Eye. 2009;23(6):1288–94. [DOI] [PubMed] [Google Scholar]
- 12.Henein C, Nanavaty MA. Systematic review comparing penetrating keratoplasty and deep anterior lamellar keratoplasty for management of keratoconus. Contact Lens Anterior Eye. 2017;40(1):3–14. [DOI] [PubMed] [Google Scholar]
- 13.John T. Selective tissue corneal transplantation: a great step forward in global visual restoration. Expert Rev Ophthalmol. 2006;1(1):5–7. [Google Scholar]
- 14.Liu S, Wong YL, Walkden A. Current perspectives on corneal transplantation. Clin Ophthalmol. 2022:631–46. [DOI] [PMC free article] [PubMed]
- 15.Maumenee A, editor. Clinical patterns of corneal graft failure. Ciba Foundation Symposium 15-Corneal Graft Failure; 1973: Wiley Online Library.
- 16.Noble BA, Agrawal A, Collins C, Saldana M, Brogden PR, Zuberbuhler B. Deep anterior lamellar keratoplasty (DALK): visual outcome and complications for a heterogeneous group of corneal pathologies. Cornea. 2007;26(1):59–64. [DOI] [PubMed] [Google Scholar]
- 17.Anshu A, Price MO, Tan DT, Price FW Jr. Endothelial keratoplasty: a revolution in evolution. Surv Ophthalmol. 2012;57(3):236–52. [DOI] [PubMed] [Google Scholar]
- 18.Mehdipour Y, Zerehkafi H. Hospital information system (his): at a glance. Asian J Comput Inform Syst. 2013;1(2).
- 19.Eghtedari M, Kamalzadeh M. Frequency of causes of corneal re-graft during 5 years at Khalili Hospital, Shiraz. Bina J Ophthalmol. 2019;24(2):99–104. [Google Scholar]
- 20.Derakhshan A, Khakshour H. Corneal grafting investigation in 100 cases of grafting operated in Imam Reza Hospital (FROM 1.1. 75. TO 1.1. 76). 2000.
- 21.Hashemi H, Beiranvand A, Khabazkhoob M, Asgari S, Emamian MH, Shariati M, et al. Prevalence of keratoconus in a population-based study in Shahroud. Cornea. 2013;32(11):1441–5. [DOI] [PubMed] [Google Scholar]
- 22.Ostadian F, Panahi Bazzaz MR, Shahsavari V, Mirdehghan MS. Evaluation of operations and causes of corneal transplantation in patients referred to the ophthalmology ward of Imam Khomeini Hospital in Ahvaz 2003 to 2019. Jundishapur Sci Med J. 2023;21(6):846–58. [Google Scholar]
- 23.Soleimani M, Javadi M, Zare M, Sharifee A. Indications for corneal transplantation in Labbafinejad medical center, Tehran, Iran. Bina J Ophthalmol. 2005;10(5):597–603. [Google Scholar]
- 24.MA J, AR BR. Indications for corneal transplantation at Labbafinejad medical center. 2011.
- 25.Jafari R, Feizi S, Javadi M, Hosseini S, Yaseri M. Predictors of endothelial cell density of corneal grafts after DSAEK. Bina J Ophthalmol. 2016;21(3):218-6.
- 26.Williams K, Keane M, Coffey N, Jones V, Mills R, Coster D. The Australian corneal graft registry 2018 report. 2018.
- 27.Ono T, Ishiyama S, Hayashidera T, Mori Y, Nejima R, Miyata K, et al. Twelve-year follow-up of penetrating keratoplasty. Jpn J Ophthalmol. 2017;61:131–6. [DOI] [PubMed] [Google Scholar]
- 28.Chan SWS, Yucel Y, Gupta N. New trends in corneal transplants at the University of Toronto. Can J Ophthalmol. 2018;53(6):580–7. [DOI] [PubMed] [Google Scholar]
- 29.Röck T, Landenberger J, Bramkamp M, Bartz-Schmidt KU, Röck D. The evolution of corneal transplantation. Ann Transplant. 2017;22:749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thanitcul C, Mathews P, Woreta FA, Akpek EK, Varadaraj V, Srikumaran D. Surgeon preference for keratoplasty techniques and barriers to performing deep anterior lamellar keratoplasty. Cornea. 2021;40(11):1406–12. [DOI] [PubMed] [Google Scholar]
- 31.Yoeruek E, Schmidt KB. Current approaches to combat the shortage of corneal tissues: split-DMEK and double-split keratoplasty. Cornea. 2015;34(3):e6–9. [DOI] [PubMed] [Google Scholar]
- 32.Shoja M, Besharati M. Penetrating keratoplasty for keratoconus: visual outcomes and complications. Bina J Ophthalmol. 2005;10(5):604–12. [Google Scholar]
- 33.Benson MD, Kurji K, Tseng C, Bao B, Mah D. Analysis of penetrating keratoplasty in Northern Alberta, Canada, from 2000 to 2015. Can J Ophthalmol. 2018;53(6):568–73. [DOI] [PubMed] [Google Scholar]
- 34.REZAEI KM, Javadi M, Kheiri B, Safi S. Evolving indications for corneal transplantation and trends in surgical techniques in Iran from 2006 to 2013; an eight-year review. Bina J Ophthalmol. 2016;21(3):227-234.
- 35.Crawford AZ, Patel DV, McGhee CN. A brief history of corneal transplantation: from ancient to modern. Oman J Ophthalmol. 2013;6(Suppl 1):S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sugar A, Gal RL, Kollman C, Raghinaru D, Dontchev M, Croasdale CR, et al. Factors associated with corneal graft survival in the cornea donor study. JAMA Ophthalmol. 2015;133(3):246–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borroni D, Gadhvi K, Wojcik G, Pennisi F, Vallabh NA, Galeone A, et al. The influence of speed during stripping in descemet membrane endothelial keratoplasty tissue preparation. Cornea. 2020;39(9):1086–90. [DOI] [PubMed] [Google Scholar]
- 38.Rocha-de-Lossada C, Rachwani-Anil R, Borroni D, Sánchez-González JM, Esteves-Marques R, Soler-Ferrández FL, et al. New horizons in the treatment of corneal endothelial dysfunction. J Ophthalmol. 2021;2021:6644114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Borroni D, Rocha de Lossada C, Parekh M, Gadhvi K, Bonzano C, Romano V, et al. Tips, tricks, and guides in descemet membrane endothelial keratoplasty learning curve. J Ophthalmol. 2021;2021:1819454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Massie AB, Kuricka L, Segev DL. Big data in organ transplantation: registries and administrative claims. Am J Transplant. 2014;14(8):1723–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.