Abstract
Rhabdomyolysis ranges from an asymptomatic illness with elevation in the creatine kinase level to a life-threatening condition associated with extreme elevations in creatine kinase, electrolyte imbalances, acute renal failure and disseminated intravascular coagulation. Muscular trauma is the most common cause of rhabdomyolysis. Less common causes include muscle enzyme deficiencies, electrolyte abnormalities, infectious causes, drugs, toxins and endocrinopathies. Weakness, myalgia and tea-colored urine are the main clinical manifestations. The most sensitive laboratory finding of muscle injury is an elevated plasma creatine kinase level. The management of patients with rhabdomyolysis includes early vigorous hydration.
Keywords: creatinine kinase, muscle damage, myoglobin, myoglobinuria, renal failure, rhabdomyolysis
Introduction
Rhabdomyolysis means destruction or disintegration of striated muscle [1]. This syndrome is characterized by muscle breakdown and necrosis resulting in the leakage of the intracellular muscle constituents into the circulation and extracellular fluid [2]. Rhabdomyolysis ranges from an asymptomatic illness with elevation in the creatine kinase (CK) level to a life-threatening condition associated with extreme elevations in CK, electrolyte imbalances, acute renal failure (ARF) and disseminated intravascular coagulation.
The cause of rhabdomyolysis is usually easily identified; however, in some instances the etiology is elusive. Muscular trauma is the most common cause of rhabdomyolysis. Less common causes include muscle enzyme deficiencies, electrolyte abnormalities, infectious causes, drugs, toxins and endocrinopathies. Rhabdomyolysis is commonly associated with myoglobinuria, and if this is sufficiently severe it can result in ARF. Weakness, myalgia and tea-colored urine are the main clinical manifestations.
The most sensitive laboratory finding of muscle injury is an elevated CK level. In the absence of myocardial or brain infarction, CK >5000 U/l indicates serious muscle injury. The management of patients with rhabdomyolysis includes advanced life support (airway, breathing and circulation) followed by measures to preserve renal function – the latter includes vigorous hydration. The use of alkalizing agents and osmotic diuretics, while commonly used, remains of unproven benefit.
Historical aspects
Rhabdomyolysis has been described for millennia. In the Bible a condition with characteristics similar to rhabdomyolysis is described when the Jews suffered a 'plague' during their exodus from Egypt, after abundant consumption of quail [3]. This biblical catastrophe is assumed to have been caused by intoxication with hemlock herbs that quails consume during spring migration [4].
Musculoskeletal trauma, in particular crush syndrome, accounts for a large proportion of the cases of rhabdomyolysis. The first cases of crush syndrome were reported in 1908 in the German military literature [5]. Crush victims who developed ARF were reported during the bombing of London during the Second World War. Pigmented casts were found in the renal tubules at autopsy; however, at that time the relationship between muscle injury and renal failure was unclear [5]. Additional cases were described during the Korean War [6]. The incidence of posttraumatic ARF decreased during the Vietnam War – this was ascribed to the faster evacuation techniques and improved fluid resuscitation of injured soldiers [7].
The role of myoglobin in the development of rhabdomyolysis was first described in experimental studies in the early 1940s. Bywaters and Stead injected rabbits with myoglobin and reported this 'toxin' to be responsible for the ARF following muscle injury [8]. In 1959, Korein and colleagues divided rhabdomyolysis into exertional and nonexertional groups [9]. In 1972, Rowland and Penn described a series of inherited enzyme deficiencies associated with myoglobinuria [10]. Increased recognition of nontraumatic, nonexertional causes of rhabdomyolysis soon occurred [11].
Epidemiology
About 10–50% of patients with rhabdomyolysis develop ARF [12]. Indeed, it has been suggested by some authors that rhabdomyolysis from all causes leads to 5–25% of cases of ARF [11]. A recent clinical series of patients developing ARF reports mortality rates of 7–80% [13]. Rhabdomyolysis occurs in up to 85% of patients with traumatic injuries. Patients with severe injury who develop rhabdomyolysis-induced renal failure have a mortality of approximately 20% [14]. Mortality is higher in patients with multiorgan dysfunction syndrome [15].
Rhabdomyolysis and crush syndrome are common results of natural disasters such as earthquakes. The Marmara region of Turkey was devastated by one of the most catastrophic earthquakes recorded, registering a magnitude of 7.4 on the Richter Scale, on 17 August 1999 [16]. The Marmara region, a densely populated and highly industrialized area, is located in the northwestern part of Turkey with a population of 20 million. According to official reports, the disaster caused 17,480 deaths. Owing to the efforts of the Turkish Society of Nephrology and the International Society of Nephrology, detailed epidemiological data were collected [16]. Since almost all of the hospitals situated in the disaster area were partly or completely destroyed, victims were transferred by boat, helicopter or road to 35 reference hospitals located in adjacent cities. A total of 9843 patients were admitted to these reference hospitals, of whom 5392 were hospitalized and 425 died. Age was the only independent predictor of outcome. The average time under the rubble was 11.7 hours, which was not significantly different between survivors and nonsurvivors. Six hundred and thirty-nine patients developed renal failure (12% of all hospitalized patients), of whom 477 (74.6%) were treated by dialysis.
Causes and pathophysiology
There are multiple causes of rhabdomyolysis, which can be classified as physical and nonphysical causes (see Table 1).
Table 1.
Causes of rhabdomyolysis
| Physical causes | |
| Trauma and compression | Crush injuries |
| Motor vehicle accidents | |
| Long-term confinement without changing position | |
| Physical torture and abuse | |
| Prolonged hours of surgery without changing position | |
| Vessel occlusion | Embolism |
| In situ thrombosis | |
| Vessel clamping during surgery | |
| Shock states | |
| Strainful muscle exercise | Amphetamine overdose |
| Excessive muscle activity | Delirium tremens |
| Epilepsy | |
| Overexertion (e.g. long distance running) | |
| Tetanus | |
| Electrical current | Cardioversion |
| High-voltage electrical injury | |
| Lightning | |
| Hyperthermia | Exercise |
| Malignant hyperthermia | |
| Neuroleptic malignant syndrome | |
| Sepsis | |
| Nonphysical causes | |
| Metabolic syndromes | Carnitine deficiency |
| Creatinine palmitoyl transferase deficiency | |
| McArdle disease (myophosphorylase deficiency) | |
| Mitochondrial respiratory chain enzyme deficiencies | |
| Phosphofruktokinase deficiency | |
| Toxins | Heavy metals |
| Insect venoms | |
| Snake venoms | |
| Drugs | See Table 2 |
| Infections | Coxsackievirus |
| Falciparum malaria | |
| Herpes viruses | |
| HIV | |
| Legionella | |
| Salmonella | |
| Streptoccocus | |
| Tularemia | |
| Electrolyte imbalances | Hyperosmotic conditions |
| Hypernatremia | |
| Hypocalcemia | |
| Hyponatremia | |
| Hypokalemia | |
| Hypophosphatemia | |
| Endocrine disorders | Hyperaldosteronism |
| Hypothyroidism | |
| Ketoacidosis | |
| Hyperaldosteronism | |
| Autoimmune diseases | Polymyositis |
| Dermatomyositis | |
The major causes of rhabdomyolysis in patients admitted to the emergency department of an urban population in the United States were reported to be cocaine, exercise and immobilization [17]. In the United States, rhabdomyolysis is commonly diagnosed in intoxicated patients subjected to prolonged muscle compression as they lay motionless, in elderly patients following a fall or stroke and in patients with seizure disorders [17]. Trauma and crush injuries following motor vehicle accidents and the collapse of buildings are other common causes of rhabdomyolysis [18,19]. During the collapse of the World Trade Center on 11 September 2001, nephrologists in New York City were prepared to dialyze large numbers of people with ARF in the days following the terrorist attack. Few patients were hospitalized with crush injuries, however, with only one reported case of rhabdomyolysis [20,21]. This case occurred in a 38-year-old policeman who was trapped under debris for 24 hours, who required hemodialysis for 1 month before fully recovering. Traumatic rhabdomyolysis may also occur in people who struggle against restraints and in children following abuse. Rhabdomyolysis has rarely been reported when a surgical procedure is performed in an improper position or following the prolonged use of a tourniquet [22-25].
Myoglobinemia and myoglobinuria and a mild elevation of creatine phosphokinase (CK) may occur after strenuous physical exertion [26]. When physical exertion is extreme, however, it can cause myolysis with severe rhabdomyolysis; this is especially likely to occur when strenuous exercise is performed under conditions of high temperature and humidity [27]. Hypokalemia increases the risk of rhabdomyolysis during strenuous exercise. This may be related to the fact that hypokalemia limits vasodilatation in the muscle microvasculature [28]. Athletes who abuse diuretics are therefore at a high risk of developing rhabdomyolysis during strenuous exercise. The pathogenesis of rhabdomyolysis following severe exertion appears to be due to a combination of mechanical and thermal muscle injury and ATP depletion. Excess muscle activity may also lead to rhabdomyolysis in conditions such as status epilepticus myoclonus and severe dystonia [29].
Rhabdomyolysis may complicate a high-voltage electrical injury and lightning strikes [30]. Rhabdomyolysis has been reported in 10% of subjects that survive an electrical shock. The degree of rhabdomyolysis is not related to the size of the wounds or to the site of entry [31]. The clinical course following an electrical burn is similar to that following a crush injury [32]. Myolysis following an electrical injury is attributed to the electrical disruption of sarcolemmal membranes, with loss of barrier function and massive calcium influx [33].
Hyperthemia may cause muscle damage. The syndromes of malignant hyperthermia and neuroleptic malignant syndrome are characterized by fever, generalized muscular contraction and rigidity, metabolic acidosis and rhabdomyolysis [34]. Malignant hyperthermia is an autosomal dominant genetic disorder in 50% of cases and an autosomal recessive genetic disorder in 20% of cases that affects males more frequently than females [35]. It occurs abruptly with the administration of anesthetic agents. The most common agents that cause malignant hyperthermia are succinylcholine and halothane [36]. The onset of malignant hyperthermia is usually within 1 hour of the administration of general anesthesia. Malignant hyperthermia results in excessive sweating, causing hypokalemia, which as previously stated potentiates the muscle injury [37].
Neuroleptic malignant syndrome is an idiosyncratic reaction to antipsychotic agents such as butyrophenones, phenothiazines and thioxanthenes, with haloperidol being the most common offending agent [38]. In this syndrome, there is a gradual development of hyperthermia, muscle rigidity, rhabdomyolysis, fluctuating consciousness and autonomic instability [39]. This clinical entity is believed to result from central nervous system dopamine receptor blockade, or from withdrawal of exogenous dopaminergic agonists [40]. Neuroleptic malignant syndrome can also develop in patients with Parkinson's disease following withdrawal of levodopa therapy [41-43].
Heat stroke is another cause of hyperthermia leading to rhabdomyolysis. By definition, patients with heat stroke have a core body temperature in excess of 40.5°C and their course is often complicated by acute respiratory distress syndrome, disseminated intravascular coagulation, renal or hepatic failure, rhabdomyolysis and seizures [44,45]. Heat stroke has a reported mortality approaching 21% [46]. Hypothermia can also cause rhabdomyolysis [47]. By reducing muscle perfusion, cold induces tissue ischemia and freezing causes cellular destruction [48,49].
Inherited disorders of carbohydrate metabolism can cause rhabdomyolysis [50]. McArdle's disease (myophosphorylase deficiency) is an autosomal recessive condition in which there is selective necrosis of type 2 muscle fibers [51]. These fibers are more dependent on glycolysis for generation of ATP and are therefore more sensitive to an enzyme defect that prevents the formation of glucose from glycogen. ATP depletion is responsible for rhabdomyolysis in this disease. Other diseases that affect the glycolytic/glycogenolytic pathways and cause rhabdomyolysis include Tarui's disease (congenital phosphofruktokinase deficiency) and phosphoglycerate mutase deficiency [52]. Other inherited metabolic disorders that are associated with rhabdomyolysis include carnitine palmitoyltransferase deficiency, an autosomal recessive disorder that has been considered the most common hereditary disease causing rhabdomyolysis [53]. In this deficiency disease, muscle pain and rhabdomyolysis develop after prolonged exercise with inadequate nutrient intake [54].
Medications and recreational drugs are important causes of rhabdomyolysis (see Table 2). Drug-induced rhabdomyolysis encompasses a large group of substances that can affect muscles by different mechanisms. Any drug that directly or indirectly impairs the production or use of ATP by skeletal muscle, or increases energy requirements that exceed the rate of ATP production, can cause rhabdomyolysis [55]. The potential mechanism of drug-induced sarcolemmal injury is presumably due to changes in the viscosity of sarcolemma caused by activation of phospholipase A. These changes result in increased permeability of the sarcolemma, permitting leakage or intracellular contents, as well as an increase in the entry of sodium ions into the cell [56-58]. The increased intracellular sodium ion concentration activates Na+,K+-ATPase, a process that requires energy. This exhausts the supplies of ATP and impairs cellular transport proteins [59]. The increase in cellular sodium ion concentration leads to the accumulation of intracellular calcium, which activates neutral proteases causing further cellular injury [60].
Table 2.
Drugs that may induce rhabdomyolysis
| Antipsychotics and antidepressants | Drugs of addiction |
| Heroin | |
| Amitriptyline | Cocaine |
| Amoxapine | Amphetamine |
| Doxepine | Methadone |
| Fluoxetine | D-lysergic acid diethylamide (LSD) |
| Fluphenazine | Antihistamines |
| Haloperidol | Diphenhydramine |
| Lithium | Doxylamine |
| Protriptyline | Other drugs |
| Phenelzine | Alcohol |
| Perphenazine | Amphotericin B |
| Promethazine | Azathrioprine |
| Chlorpromazine | Butyrophenones |
| Loxapine | Emetics |
| Promazine | Epsilon-aminocaproic acid |
| Trifluoperazine | Halothane |
| Sedative hypnotics | Laxatives |
| Benzodiazepines | Moxalactam |
| Diazepam | Narcotics |
| Nitrazepam | Oxprenolol |
| Flunitrazepam | Paracetamol |
| Lorazepam | Penicillamine |
| Triazolam | Pentamidine |
| Barbiturates | Phencyclidine |
| Gluthetimide | Phenylpropanolamine |
| Antilipemic agents | Quinidine |
| Lovastatin | Salicylates |
| Pravastatin | Strychnine |
| Simvastatin | Succinylcholine |
| Bezafibrate | Theophyline |
| Clozafibrate | Terbutaline |
| Ciprofibate | Thiazides |
| Clofibrate | Vasopressin |
The use of 3-hydroxy-3-methyl glutaryl coenzyme A reductase inhibitors, or statins, has been shown to reduce major cardiovascular events in both primary and secondary prevention. Statins have consequently become one of the most widely prescribed class of medications, with more than 76 million prescriptions filled in the United States in 2000 [61]. Statins are well tolerated by most patients. The most serious side effects of these drugs are myositis with rhabdomyolysis. This risk was emphasized by the withdrawal of cerivastatin in August 2001 after the drug was associated with approximately 100 rhabdomyolysis-related deaths [62]. Statins have been postulated to interfere with ATP production by reducing levels of coenzyme Q, a component of the electron transport chain [63]. Rhabdomyolysis may developed acutely soon after initiating therapy (2–3 weeks) or months or years later after a precipitating event such as an intercurrent illness or infection, strenuous exercise or a drug interaction. Clinically important rhabdomyolysis with statins is rare, with an overall reported incidence of fatal rhabdomyolysis of 0.15 deaths per one million prescriptions [64]. The FDA MedWatch Reporting system lists 3339 cases of statin-associated rhabdomyolysis reported between 1 January 1990 and 31 March 2002 [61].
Statins are also associated with a chronic myositis syndrome, characterized by muscle pain and weakness with or without evidence of clinically detectable rhabdomyolysis [65]. Few data are available on the frequency of the chronic myositis syndrome, which may affect between 0.1% and 1% of patients. Risk factors for the development of a statin-induced myopathy include high dosages, increasing age, female sex, renal and hepatic insufficiency, diabetes mellitus and concomitant therapy with drugs such as fibrates, cyclosporine, macrolide antibiotics, warfarin and digoxin [61]. Individual statins may differ in their risk of inducing rhabdomyolysis, with some patients developing this syndrome when switching from one statin to another. Other patients develop rhabdomyolysis when exposed to any statin. It is probable that genetic factors play a role in the pathogenesis of this syndrome.
Rhabdomyolysis has been reported in solid organ transplant recipients [66]. The use of immunosuppressive drugs, particularly cyclosporine, has been implicated in these cases. Alcohol directly injures the sarcolemma and increases sodium permeability [67]. Analysis of skeletal muscle from chronic alcoholics and experimental animals fed ethanol demonstrates a marked depletion of intracellular potassium, phosphorus and magnesium, and demonstrates elevated sodium, chloride, calcium and water content [68,69]. Acute alcohol-induced rhabdomyolysis can occur after binge drinking or a sustained period of alcohol abuse, and is associated with pain and swelling of muscles, particularly the quadriceps [70]. Drugs such as D-lysergic acid diethylamide (known as LSD), sympathomimetics and phencyclidine, which induce delirium or agitation, and those that cause prolonged involuntary muscle contraction, lead to increased ATP demand and to eventual exhaustion of its energy stores [71].
Cocaine is a common cause of both traumatic and nontraumatic rhabdomyolysis. Twenty-four percent of emergency department patients presenting with cocaine-related disorders have acute rhabdomyolysis [72]. Cocaine produces rhabdomyolysis by several different mechanisms. Prolonged vasoconstriction of intramuscular arteries can produce muscle ischemia and acute rhabdomyolysis. In addition, large doses of cocaine can have a direct toxic effect and can produce acute skeletal myofibrillar degeneration. Cocaine may also produce traumatic rhabdomyolysis by causing generalized tonic–clonic seizures, or by coma and secondary physical compression of a major muscle group for prolonged periods of time [73].
A number of electrolyte abnormalities are associated with rhabdomyolysis [74]. Examples include chronic hypokalemia, hypophosphatemia and hyponatremia as well as rapid correction of hyponatremia [11,75,76]. Overuse of diuretic or cathartic drugs can lead to massive total body potassium depletion, causing rhabdomyolysis [77]. Potassium depletion-induced rhabdomyolysis can occur in the presence of normal or elevated serum potassium levels, which are maintained by the ongoing release of potassium from dying myocytes [28,31]. Any condition that produces major electrolyte losses, such as hyperemesis gravidarum, can be associated with rhabdomyolysis [78].
Polymyositis and dermatomyositis are chronic autoimmune conditions that in rare cases can progress to rhabdomyolysis [79,80]. An interesting and challenging cause of rhabdomyolysis is the ingestion of large quantities of licorice. It is well known that licorice contains a mineralocorticoid-type agent that causes renal potassium wasting [81]. Hyperosmolar states such as hyperglycemic hyperosmolar nonketotic coma have been reported to cause rhabdomyolysis [82,83]. On rare occasions rhabdomyolysis has been associated with thyroid storm and pheochromocytoma; both conditions increase sympathetic stimulation and metabolic demands, resulting in an extreme hypermetabolic state [84].
Infections have also been reported to cause rhabdomyolysis [85]. This includes bacterial pyomyositis, which presents with localized signs of muscle infection with erythema, edema and tenderness [86]. Legionella infection is classically associated with rhabdomyolysis [87]. Rhabdomyolysis can be seen in septic patients without direct muscle infection [88]. In these instances, muscle damage can be caused by a toxin, or from associated fever, rigors and dehydration [89]. Acute viral infections with influenza A and influenza B, Coxsackievirus, Epstein–Barr virus, herpes simplex virus, parainfluenza, adenovirus, echovirus, HIV and cytomegalovirus have been associated also with rhabdomyolysis [90,91].
Muscle injury, regardless of mechanism, results in a cascade of events that leads to leakage of extracellular calcium ions into the intracellular space [57] (Fig. 1 and Table 3). The excess of calcium causes a pathologic interaction of actin and myosin, and activates cellular proteases with muscle destruction and fiber necrosis [51]. The final common effector pathway is thought to be an increase in free cytosolic ionized calcium, which may start a cascade of effects leading to major cell permeability and capillary leak [22]. Mechanisms affecting membrane ion channels, activity of the membrane sodium–potassium pump and the production of ATP link the initial causes of rhabdomyolysis to the final effector pathway. Such mechanisms are initiated by direct damage to the membrane caused by toxins, severe exercise or compression, or failure to provide adequate ATP following ischemia or a defective oxidative metabolism. With muscle injury, large quantities of potassium, phosphate, myoglobin, CK and urate leak into the circulation. Myoglobin in the renal glomerular filtrate can precipitate and cause renal tubular obstruction, leading to renal damage [57].
Figure 1.

Overview of the pathophysiology of rhabdomyolysis. CK, creatine kinase.
Table 3.
Mechanisms of cellular destruction in rhabdomyolysis
| Method | Mechanism |
| Direct injury to cell membrane | Crushing, tearing, burning, pounding, poisoning, dissolving |
| Muscle cell hypoxia leading to depletion of ATP | Anerobic conditions: shock states, vascular occlusion, and tissue compression |
| Electrolyte disturbance disrupting the sodium–potassium pump | Hypokalemia: vomiting, diarrhea, extensive diuresis |
| Hyponatremia: water intoxication |
Mechanisms of ARF in rhabdomyolysis patients
It has been suggested that there are two crucial factors in the development of myoglobinuric ARF; these include hypovolemia/dehydration and aciduria. Three main mechanisms influence heme protein toxicity: renal vasoconstriction with diminished renal circulation, intraluminal cast formation and direct heme protein-induced cytotoxicity. In the absence of hypovolemia and aciduria, heme proteins have minimal nephrotoxic effects; when these conditions are present, however, heme proteins can induce renal dysfunction by a variety of mechanisms [67]. Released heme proteins produce a synergistic effect on renal vasoconstriction initiated through hypovolemia and activation of the cytokine cascade [92] (Fig. 2). This effect possibly occurs through the scavenging of nitric oxide, which acts as a vasodilatory mediation, or through the activation of endothelin receptors consequent upon free-radical formation induced by heme protein. The enhanced renal vasoconstriction and resultant ischemia add, through depletion of tubular ATP, to the potential for damage to the renal tubular cells, already threatened by the heme-protein-induced free radicals [93].
Figure 2.
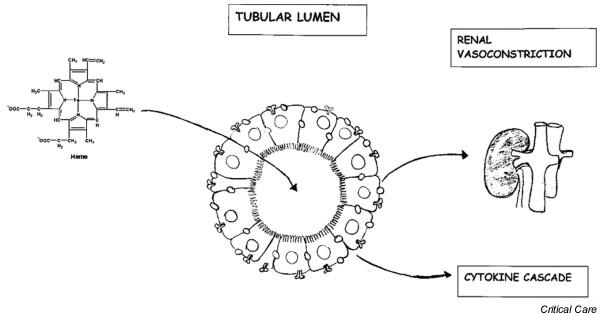
Mechanisms of heme-induced renal failure.
Pigmented casts are a characteristic of rhabdomyolysis-associated ARF (see Fig. 3). These are a result of the interaction of Tamm–Horsfall protein with myoglobin, which is enhanced at a low pH [53]. It has been suggested that ARF is caused by a tubular obstruction causing increased intraluminal pressure and thus opposing glomerular filtration [94].
Figure 3.
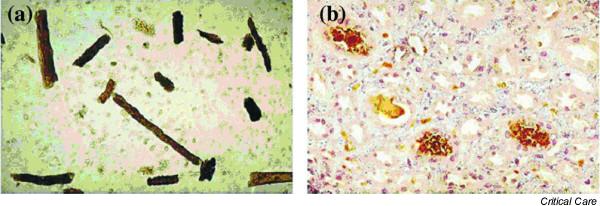
Pigmented casts. Analysis of urinary sediment (×400) pigmented casts, leukocyturia, and hematuria without dysmorphic red cells. (a) Pigmented casts, leukocyturia, hematuria with dysmorphic cells; (b) with antibody against human myoglobin.
Alternative mechanisms that have been suggested include the precipitation of heme protein providing a ready supply of material that can generate toxic free radicals [95]. The propensity for cast formation is determined by the pH, the filtered load of myoglobin and the flow through the renal tubule [96]. Heme-produced free radicals induce oxidative damage to the renal tubule [95]. Investigational work has suggested that myoglobin is central to the oxidative injury manifested as lipid peroxidation, and that this may be inhibited by an alkaline pH [97].
Clinical manifestations
There is a wide variation in the clinical presentation of rhabdomyolysis. The 'classic' triad of symptoms includes muscle pain, weakness and dark urine [98]. The clinical manifestations can be classified as musculo-skeletal signs, general manifestations and complications. The muscle pain, weakness, tenderness and contracture may involve specific groups of muscles or may be generalized [99]. The most frequently involved muscle groups are the calves and the lower back. The muscles can be tender and swollen, and there can be skin changes indicating pressure necrosis. However, these classic features are seen in less than 10% of the patients. Some patients experience severe excruciating pain. The calf pain may erroneously result in a work-up for deep venous thrombosis and the back pain can mimic renal colic. Similarly, involvement of the chest musculature can present with 'anginal' type chest pain. Over 50% of the patients may not complain of muscle pain or weakness [17]. The initial clinical sign of rhabdomyolysis may be the appearance of discolored urine. Urine can range from pink-tinged, to cola-colored, to dark black [100].
The general manifestations of rhabdomyolysis include malaise, fever, tachycardia, nausea and vomiting. The complications can be classified as early or late complications. The early complications include hyperkalemia, hypocalcemia, elevated liver enzymes, cardiac dysrrhythmias and cardiac arrest, while the late complications include ARF and disseminated intravascular coagulation.
Severe hyperkalemia occurs secondary to massive muscle breakdown, causing cardiac dysrrhythmias and possibly cardiac arrest. Hepatic dysfunction occurs in 25% of patients with rhabdomyolysis. Proteases released from injured muscle cause hepatic injury [101]. ARF and diffuse intravascular coagulation are late complications, developing 12–72 hours after the acute insult.
Laboratory findings
Although the patient history and physical examination can provide clues, the diagnosis of rhabdomyolysis is confirmed by laboratory studies. CK levels are the most sensitive indicator of myocyte injury in rhabdomyolysis [47]. Normal CK enzyme levels are 45–260 U/l. CK rises in rhabdomyolysis within 12 hours of the onset of muscle injury, peaks in 1–3 days, and declines 3–5 days after the cessation of muscle injury. The peak CK level may be predictive of the development of renal failure [12]. Abnormal CK levels are commonly seen in injured intensive care unit patients, and a level of 5000 U/l or greater is related to renal failure [102]. The half-life of CK is 1.5 days and so it remains elevated longer than serum myoglobin levels [29]. Estimation of myoglobin in serum and urine is useful, particularly in the early phases of the disease [103]. Myoglobin is filtered by the kidney and appears in the urine when the plasma concentration exceeds 1.5 mg/dl [29,104]. It imparts a dark red–brown color to urine when the urine concentration exceeds 100 mg/dl. Myoglobin has a short half-life (2–3 hours) and is rapidly cleared by renal excretion and metabolism to bilirrubin [17]. Serum myoglobin levels may return to normal within 6–8 hours.
Other muscle markers can also be used. For example, carbonic anhydrase III is present in skeletal muscles but not in myocardium, and an increase in its levels is more specific for skeletal muscle injury than are CK levels [105]. Aldolase is another glycolytic pathway enzyme that is found in high concentration in skeletal muscle, the liver and the brain. While increased aldolase levels are not as specific or as sensitive for muscle disease as CK levels, increased aldolase together with an increased CK level is highly suggestive of muscle injury [106]. In addition to these enzymes, troponin I and troponin T can be helpful in diagnosing early rhabdomyolysis [107].
Both ARF and the increased release of creatinine from skeletal muscle increase the serum concentrations of urea nitrogen and creatinine. However the creatinine is elevated to a greater extent than the blood urea nitrogen, narrowing the normal 10:1 ratio of urea nitrogen to creatinine to a ratio of 6:1 or less [108]. A classic pattern of changes in serum electrolytes occurs in rhabdomyolysis. Serum levels of potassium and phosphate increase as these components are released from the cells; levels then decrease as they are excreted in urine [109]. Serum concentrations of calcium are initially decreased as calcium moves into the cells and then gradually increase. Electrolyte levels in each patient depend on the severity of the rhabdomyolysis, the stage of the illness and the therapeutic interventions that have been initiated [18]. The classic laboratory finding is an elevated serum CK of at least five times the normal value, where the creatinine kinase isoenzyme found predominately in striated muscle (CK-MM) predominates [109]. Myoglobin becomes detectable in urine and produces pigmenturia. Other findings include hyperkalemia, hypocalcemia, hyperphosphatemia and hyperuricemia along with elevated levels of other muscle enzymes like lactate dehydrogenase, aldolase, aminotransferases and carbonic anhydrase III [29].
Clotting studies are useful for detecting rhabdomyolysis – disseminated intravascular coagulation and toxicological screening should be performed if drugs are the suspected causal agent [110]. Urinalysis in patients with rhabdomyolysis will reveal the presence of protein, brown casts and uric acid crystals, and may reflect electrolyte wasting consistent with renal failure [111]. A urine dipstick is a quick way to screen for myoglobinuria, as the reagent on the dipstick that reacts with hemoglobin also reacts with myoglobin [18]. These reactants will detect hemoglobin at concentrations of 0.3 mg/l, and a similar concentration would be predicted for myoglobin [112]. Myoglobin imparts its characteristic red–brown color to urine at concentrations above 300 mg/l (see Table 3).
Management
The treatment of rhabdomyolysis includes initial stabilization and resuscitation of the patient while concomitantly attempting to preserve renal function [113]. Retrospective analysis demonstrates that early aggressive fluid replacement with saline is beneficial in minimizing the occurrence of renal failure. The longer it takes for rehydration to be initiated, the more likely it is that renal failure will develop [22,24]. Forced diuresis, when started within 6 hours of admission, has been reported to minimize the risk of ARF [53,114].
Mannitol and bicarbonate are commonly employed following the initial resuscitation with saline [115-119]. Experimental studies suggested that mannitol may be protective due to the associated diuresis that minimizes intratubular heme pigment deposition [53,67,116]. It has also been suggested that mannitol acts as a free-radical scavenger, thereby minimizing cell injury [22]. Furthermore, mannitol reduces blood viscosity and is a renal vasodilator [120-125]. Furosemide and other loop diuretics have also been advocated for use in patients with myoglobinuric renal impairment in an attempt to initiate diuresis and convert anuric to oliguric renal failure [126-128].
Alkalinization of the urine has been suggested to minimize renal damage after rhabdomyolysis [129]. After resuscitation and restoration of normal renal perfusion, the kidneys clear a large acid load resulting in an acidic urine. It has been postulated that these patients may be unable to alkalinize their urine without the administration of bicarbonate, and this increases the risk of tubular cast development and renal injury [130-132]. Knochel and Moore, and Knottenbelt, however, have argued that large-volume infusion of crystalloid alone creates a solute diuresis sufficient to alkalinize the urine [133,134]. Furthermore, large doses of bicarbonate may worsen the degree of hypocalcemia, especially if hypovolemia is corrected [135].
While mannitol and bicarbonate are considered the standard of care in preventing ARF in patients with rhabdomyolysis [115-119], there is little clinical evidence to support the use of these agents. While randomized controlled trials are lacking, the available evidence suggests that mannitol and bicarbonate have no benefit over and above aggressive fluid resuscitation [120-123]. In a retrospective study of 24 patients Homsi and colleagues demonstrated that volume expansion with saline alone prevented progression to renal failure and that the addition of mannitol and bicarbonate had no additional benefit [119]. Using their Trauma Registry and intensive care unit database, Brown and colleagues reviewed the case records of 1771 trauma patients with increased CK levels [102]. Overall 217 patients (12%) developed renal failure, with 97 requiring dialysis. In this study, peak CK >5000 U/l was associated with an increased risk of developing renal failure. Of the 382 patients with CK >5000 U/l, 154 patients (40%) received mannitol and bicarbonate whereas 228 patients did not. There was no significant difference in the incidence of renal failure (22% versus 18%), of dialysis (7% versus 6%) or of mortality (15% versus 18%) between the two groups. Based on these data it would appear that mannitol and bicarbonate have little additional benefit over aggressive volume replacement with saline alone.
The role of free-radical scavengers and antioxidants
The magnitude of muscle necrosis caused by ischemia-reperfusion injury has been reduced in experimental models by the administration of free-radical scavengers [136]. Many of these agents have been used in the early treatment of crush syndrome to minimize the amount of nephrotoxic material released from the muscle [137]. Pentoxyphylline is a xanthine derivative used to improve microvascular blood flow. In addition, pentoxyphylline acts to decrease neutrophil adhesion and cytokine release [138]. Vitamin E (alfa tocopherol), vitamin C (ascorbic acid), lazaroids (21-aminosteroids) and minerals such as zinc, manganese and selenium all have antioxidant activity and may have a role in the treatment of the patient with rhabdomyolysis [139,140].
Dialysis
Despite optimal treatment, some patients will develop ARF, often with severe acidosis and hyperkalemia [141]. These patients will require renal replacement therapy to correct fluid, electrolyte and acid–base abnormalities. Daily hemodialysis or continuous hemofiltration may be required initially to remove urea and potassium that are released from damaged muscles [142]. This allows gradual removal of solutes and the slow correction of fluid overload. Normalization of potassium is the priority, because hyperkalemic cardiac arrest is a life-threatening early complication [143]. Peritoneal dialysis is inadequate to remove the large solute loads in patients with rhabdomyolysis-induced ARF, but it can offer temporary help [144]. The removal of myoglobin by plasma exchange has not demonstrated any benefit [145].
A unique management issue in rhabdomyolysis-induced ARF is the development of hypercalcemia during the recovery phase in 20–30% of patients [146,147]. To minimize this complication, the administration of calcium should be avoided during the renal failure phase, unless the patient has symptomatic hypocalcemia or severe hyperkalemia [148-150].
Conclusions
Rhabdomyolysis is a potentially life-threatening condition that must be suspected in all patients with a history of any circumstance that can result in damage of skeletal muscle. Important clinical signs and symptoms (i.e. muscle pain, muscle tenderness and dark urine) and laboratory tests such as an elevated serum CK level and a urinalysis that reveal casts and is positive for hemoglobin, without red blood cells on microscope examination, are common. Aggressive hydration may prevent the complications of this illness. Mannitol and bicarbonate, although commonly recommended, are of unproven benefit.
Abbreviations
ARF = acute renal failure; CK = creatine kinase.
Competing interests
The author(s) declare that they have no competing interests.
Contributor Information
Joseph Varon, Email: Joseph.Varon@uth.tmc.edu.
Paul E Marik, Email: pmarik@zbzoom.net.
References
- Farmer J. Rhabdomyolysis. In: Civetta J, Taylor R, Kirby R, editor. In Critical Care. 2. Philadephia, PA: Lippincott; 1997. pp. 1785–1791. [Google Scholar]
- Warren J, Blumberg P, Thompson P. Rhabdomyolysis: a review. Muscle Nerve. 2002;25:332–347. doi: 10.1002/mus.10053. [DOI] [PubMed] [Google Scholar]
- Book of Numbers . The Bible The New English Bible, 1970 Joint Comitee on the New Translation of the Bible. Vol. 11. New York: Cambridge University Press; pp. 31–35. [Google Scholar]
- Rizzi D, Basile C, Di Maggio A. Clinical spectrum of accidental hemlock poisoning: neurologic manifestations, rhabdomyolysis and acute tubular necrosis. Nephrol Dial Transplant. 1991;6:939–943. doi: 10.1093/ndt/6.12.939. [DOI] [PubMed] [Google Scholar]
- Bywaters E, Beall D. Crush injuries with impairment of renal function. Br Med J. 1941;1:427–432. doi: 10.1136/bmj.1.4185.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L, Post R, Teschan P, Abernathy R, Davis J, Gray D, Howard J, Johnson K, Klopp E, Mundy R, et al. Postraumatic renal insufficiency in military casualties. II Management, use of an artificial kidney, prognosis. Am J Med. 1955;18:187–198. doi: 10.1016/0002-9343(55)90234-5. [DOI] [PubMed] [Google Scholar]
- Stone W, Knepshield J. Post traumatic acute renal insufficiency in Vietnam. Clin Nephrol. 1974;2:189–190. [PubMed] [Google Scholar]
- Bywaters EGI, Stead BJK. The production of renal failure following injection of solutions containing myohaemoglobin. Q J Exp Physiol. 1944;33:53–70. [Google Scholar]
- Korein J, Coddon D, Mowrey F. The clinical spectrum of paroxysmal paralytic myoglobinuria. Neurology. 1959;9:767–785. doi: 10.1212/wnl.9.11.767. [DOI] [PubMed] [Google Scholar]
- Rowland L, Penn A. Myoglobinuria. Med Clin North Am. 1972;56:1233–1256. doi: 10.1016/s0025-7125(16)32319-7. [DOI] [PubMed] [Google Scholar]
- Grossman R, Hamilton R, Morse B, Penn A, Goldberg M. Nontraumatic rhabdomyolysis and acute renal failure. N Engl J Med. 1974;291:807–811. doi: 10.1056/NEJM197410172911601. [DOI] [PubMed] [Google Scholar]
- Ward M. Factors predictive of acute renal failure in rhabdomyolysis. Arch Intern Med. 1988;148:1553–1557. doi: 10.1001/archinte.148.7.1553. [DOI] [PubMed] [Google Scholar]
- Brivet F, Keinknecht D, Loirat P, Landais P. Acute renal failure in intensive care units – causes, outcomes, and prognostic factors of hospital mortality: a prospective multicenter study. Crit Care Med. 1996;24:192–198. doi: 10.1097/00003246-199602000-00003. [DOI] [PubMed] [Google Scholar]
- Mohaupt M. Rhabdomyolysis. Ther Umsch. 2003;60:391–397. doi: 10.1024/0040-5930.60.7.391. [DOI] [PubMed] [Google Scholar]
- Splendiani G, Mazzarella V, Cipriani S, Zazzaro D, Casciani C. Dialytic treatment of rhabdomyolysis-induced acute renal failure: our experience. Ren Fail. 2001;23:183–191. doi: 10.1081/JDI-100103490. [DOI] [PubMed] [Google Scholar]
- Sever M, Erek E, Vanholder R, Akoglu E, Yavaz M, Ergin H, Tekce M, Korular D, Tulbek M, Keven K, et al. The Marmara earthquake: epidemiological analysis of the victims with nephrological problems. Kidney Int. 2001;60:1114–1123. doi: 10.1046/j.1523-1755.2001.0600031114.x. [DOI] [PubMed] [Google Scholar]
- Gabow P, Kaehny W, Kelleher S. The spectrum of rhabdomyolysis. Medicine. 1982;62:141–152. doi: 10.1097/00005792-198205000-00002. [DOI] [PubMed] [Google Scholar]
- Vanholder R, Sever M, Erek E, Lemeire N. Acute renal failure related to the crush syndrome: towards an era or seismonephrology? Nephrol Dial Transplant. 2000;15:1517–1521. doi: 10.1093/ndt/15.10.1517. [DOI] [PubMed] [Google Scholar]
- Kantarci G, Vanholder R, Tuglular S, Akin H, Koc M, Ozeenr C, Akogu E. Acute renal failure due to crush syndrome during Marmara earthquake. Am J Kidney Dis. 2002;40:682–689. doi: 10.1053/ajkd.2002.35673. [DOI] [PubMed] [Google Scholar]
- Lane R, Phillips M. Rhabdomyolysis. BMJ. 2003;327:115–116. doi: 10.1136/bmj.327.7407.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldfarb D, Chung S. The absence of rhabdomyolysis induced renal failure following the world trade center collapse [letter] Am J Med. 2002;113:260. doi: 10.1016/S0002-9343(02)01188-9. [DOI] [PubMed] [Google Scholar]
- Odeh M. The role of reperfusion-induced injury in the pathogenesis of the crush syndrome. N Engl J Med. 1991;324:1417–1422. doi: 10.1056/NEJM199105163242007. [DOI] [PubMed] [Google Scholar]
- Defraigne JO, Pincmail J. Local and systemic consequences of severe ischemia and reperfusion of the skeletal muscle: physiopathology and prevention. Acta Chir Belg. 1998;98:176–186. [PubMed] [Google Scholar]
- Adiseshiah M, Round J, Jones D. Reperfusion injury in skeletal muscle: a prospective study in patient with acute limb ischemia and claudication treated by revascularization. Br J Surg. 1992;79:1026–1029. doi: 10.1002/bjs.1800791013. [DOI] [PubMed] [Google Scholar]
- Biswas S, Gnanasekaran I, Ivatury R, Simon R, Patel A. Exaggerated lithotomy position-related rhabdomyolysis. Am Surg. 1997;63:361–364. [PubMed] [Google Scholar]
- Schiff H, MacSearraigh E, Kallmeyer J. Myoglobinuria, rhabdomyolysis and marathon running. Q J Med. 1978;47:463–472. [PubMed] [Google Scholar]
- Schafer M, Less H, Steiner I, Breezier M. Hazard of sauna after strenuous exercise. Ann Intern Med. 1994;120:441–442. doi: 10.7326/0003-4819-120-5-199403010-00029. [DOI] [PubMed] [Google Scholar]
- Visweswaran P, Guntupalli J. Rhabdomyolysis. Crit Care Clin. 1999;15:415–412. doi: 10.1016/s0749-0704(05)70061-0. [DOI] [PubMed] [Google Scholar]
- Poels P, Gabreels F. Rhabdomyolysis: a review of literature. Clin Neurol Neurosurg. 1995;95:175–192. doi: 10.1016/0303-8467(93)90122-W. [DOI] [PubMed] [Google Scholar]
- Rosen C, Adler J, Rabban J, Sethi R, Arkoff L, Blair J, Sheridan R. Early predictors of myoglobinuria and acute renal failure following electrical injury. J Emerg Med. 1999;17:783–789. doi: 10.1016/S0736-4679(99)00084-0. [DOI] [PubMed] [Google Scholar]
- Slater M, Mullins R. Rhabdomyolysis and myoglobinuric acute renal failure in trauma and surgical patients: a review. J Am Coll Surg. 1998;186:693–716. doi: 10.1016/S1072-7515(98)00089-1. [DOI] [PubMed] [Google Scholar]
- Frank D, Fisher J. Complications of electrical injury. In: Greenfield LJ, editor. In Complications in Surgery and Trauma. Philadelphia, PA: Lippincott-Raven; 1990. [Google Scholar]
- Brumback R, Feeback D, Leech R. Rhabdomyolysis following electrical injury. Semin Neurol. 1995;15:329–334. doi: 10.1055/s-2008-1041040. [DOI] [PubMed] [Google Scholar]
- Denborough M. Malignant hyperthermia. Lancet. 1998;352:1131–1136. doi: 10.1016/S0140-6736(98)03078-5. [DOI] [PubMed] [Google Scholar]
- Ali S, Taguchi A, Rosenberg H. Malignant hyperthermia. Best Pract Resp Clin Anaesthesiol. 2003;4:519–533. doi: 10.1016/j.bpa.2003.09.012. [DOI] [PubMed] [Google Scholar]
- Abraham B, Cahana A, Krivosic-Horber R, Perel A. Malignant hyperthermia susceptibility: anaesthetic implications and risk stratification. Q J Med. 1997;90:13–18. doi: 10.1093/qjmed/90.1.13. [DOI] [PubMed] [Google Scholar]
- Simon H. Hyperthermia. N Eng J Med. 1993;329:483–487. doi: 10.1056/NEJM199308123290708. [DOI] [PubMed] [Google Scholar]
- Schneider S. Neuroleptic malignant syndrome: controversies in treatment. Am J Emerg Med. 1991;9:360–362. doi: 10.1016/0735-6757(91)90058-R. [DOI] [PubMed] [Google Scholar]
- Guze B, Baxter L. Neuroleptic malignant syndrome. N Engl J Med. 1985;313:163–166. doi: 10.1056/NEJM198507183130306. [DOI] [PubMed] [Google Scholar]
- Mann SC, Caroff SN, Fricchione G, Campbell EC. Central dopamine hypoactivity and the pathogenesis of the neuroleptic malignant syndrome. Psychiatr Annals. 2000;30:363–374. [Google Scholar]
- Gibb W, Griffith D. Levodopa withdrawal syndrome identical to neuroleptic malignant syndrome. Postgrad Med J. 1986;62:59–60. doi: 10.1136/pgmj.62.723.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato Y, Asoh T, Metoki N, Satoh K. Efficacy of methylprednisolone pulse therapy on neuroleptic malignant syndrome in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2003;74:574–576. doi: 10.1136/jnnp.74.5.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varon J, Jacobs M. Treating the progressive stages of Parkinson's disease. Postgrad Med. 1991;90:63–71. doi: 10.1080/00325481.1991.11700979. [DOI] [PubMed] [Google Scholar]
- Bross M, Nash B, Carlton F. Heat emergencies. Am Fam Physician. 1994;50:389–396. [PubMed] [Google Scholar]
- Tek D, Olshaker J. Heat illness. Emerg Med Clin North Am. 1992;10:299–310. [PubMed] [Google Scholar]
- Dematte J, O'Mara K, Buescher J, Whitney C, Forsythe S, McNamee T, Adiga R, Ndukwu I. Near fatal heat stroke during the 1995 heat wave in Chicago. Ann Intern Med. 1998;129:173–181. doi: 10.7326/0003-4819-129-3-199808010-00001. [DOI] [PubMed] [Google Scholar]
- Moghtader J, Brady W, Bonadio W. Exertional rhabdomyolysis in an adolescent athelete. Pediatr Emerg Care. 1997;13:382–385. doi: 10.1097/00006565-199712000-00006. [DOI] [PubMed] [Google Scholar]
- Varon J, Sadovnikoff N, Sternbach G. Hypothermia: saving patients from the big chill. Postgrad Med. 1992;92:47–59. doi: 10.1080/00325481.1992.11701549. [DOI] [PubMed] [Google Scholar]
- Varon J, Varon S, Fromm R, Sternbach G. Hypothermia – ABCs of diagnosis and treatment. Med Interam. 1994;13:189–192. [Google Scholar]
- Vissing J, Haller R. The effect of oral sucrose on exercise tolerance in patients with McArdle's disease. N Engl J Med. 2003;349:2503–2509. doi: 10.1056/NEJMoa031836. [DOI] [PubMed] [Google Scholar]
- Brumback R, Feeback D, Leech R. Rhabdomyolysis in childhood. Pediatr Neurol. 1992;39:821–858. doi: 10.1016/s0031-3955(16)38377-8. [DOI] [PubMed] [Google Scholar]
- Nakajima H, Hamaguchi T, Yamasaki T, Tarui S. Phosphofructokinase deficiency: recent advances in molecular biology. Muscle Nerve. 1995;3:S28–S34. doi: 10.1002/mus.880181408. [DOI] [PubMed] [Google Scholar]
- Zager R. Rhabdomyolysis and myohemoglobinuric acute renal failure. Kidney Int. 1996;49:314–326. doi: 10.1038/ki.1996.48. [DOI] [PubMed] [Google Scholar]
- Lofberg M, Jankala H, Paetau A, Harkonen M, Somer H. Metabolic causes of recurrent rhabdomyolysis. Acta Neurol Scand. 1998;98:268–275. doi: 10.1111/j.1600-0404.1998.tb07307.x. [DOI] [PubMed] [Google Scholar]
- Kakulas B. Experimental myopathies. In: Walton SJ, editor. In Disorders of Voluntary Muscle. New York: Churchill Livingstone; 1981. pp. 393–400. [Google Scholar]
- Haskins N. Rhabdomyolysis and acute renal failure in intensive care. Nurs Crit Care. 1998;3:283–238. [PubMed] [Google Scholar]
- Knochel J. Mechanisms of rhabdomyolysis. Curr Opin Rheumatol. 1993;5:725–731. doi: 10.1097/00002281-199305060-00006. [DOI] [PubMed] [Google Scholar]
- Jackson M, Jones D, Edwards R. Experimental skeletal muscle damage: the nature of the calcium activated degenerative processes. Eur J Clin Invest. 1984;14:369–374. doi: 10.1111/j.1365-2362.1984.tb01197.x. [DOI] [PubMed] [Google Scholar]
- Rubin B, Liauw S, Tittley J, Romaschin A, Walker P. Prolonged adenine nucleotide resynthesis and reperfusion injury in post-ischemic skeletal muscle. Am J Physiol. 1992;262:H1538–H1547. doi: 10.1152/ajpheart.1992.262.5.H1538. [DOI] [PubMed] [Google Scholar]
- Armstrong R, Warren G, Warren J. Mechanisms of exercise-induced muscle fiber injury. Sports Med. 1991;12:184–207. doi: 10.2165/00007256-199112030-00004. [DOI] [PubMed] [Google Scholar]
- Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003;289:1681–1690. doi: 10.1001/jama.289.13.1681. [DOI] [PubMed] [Google Scholar]
- Fuhrmans V. Bayer discloses higher death toll from Baycol. Wall Street J. p. A10. 21 January 2002.
- Ghirlanda G, Oradei A, Manto A, Lippa S, Uccioli L, Caputo S, Greco A, Littaru G. Evidence of plasma CoQ 10-lowering effect by HMG-CoA reductase inhibitors: a doble blind, placebo-controlled study. J Clin Pharmacol. 1992;33:226–229. doi: 10.1002/j.1552-4604.1993.tb03948.x. [DOI] [PubMed] [Google Scholar]
- Staffa JA, Chang J, Green L. Cerivastatin and reports of fatal rhabdomyolysis. N Engl J Med. 2002;346:539–540. doi: 10.1056/NEJM200202143460721. [DOI] [PubMed] [Google Scholar]
- Phillips PS, Haas RH, Bannykh S, Hathaway S, Gray NL, Kimura BJ, Vladutiu G, England JD. Statin-associated myopathy with normal creatine kinase levels. Ann Intern Med. 2002;137:581–585. doi: 10.7326/0003-4819-137-7-200210010-00009. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Bolton D, Haynes S, Smith J. Acute rhabdomyolysis after cardiac transplantation: a diagnostic conundrum. Paediatr Anaesth. 2002;12:729–732. doi: 10.1046/j.1460-9592.2002.00936.x. [DOI] [PubMed] [Google Scholar]
- Zager R. Studies of mechanisms and protective maneuvers in myoglobinuric acute renal injury. Lab Invest. 1989;60:619–629. [PubMed] [Google Scholar]
- Knochel J, Bilbrey G, Fuller T, Carter N. The muscle cell in chronic alcoholism. The possible role of phosphate depletion in alcoholic cardiomyopathy. Ann NY Acad Sci. 1975;252:274–286. doi: 10.1111/j.1749-6632.1975.tb19168.x. [DOI] [PubMed] [Google Scholar]
- Ferguson E, Blachley J, Carter N, Knochel J. Derangements of muscle composition, ion transport and oxygen consumption in chronically alcoholic dogs. Am J Physiol. 1984;246:F700–F709. doi: 10.1152/ajprenal.1984.246.5.F700. [DOI] [PubMed] [Google Scholar]
- Victor M. Toxic and nutritional myopathies. In: Engel AG, Banker BQ, editor. In Myology. II. New York: McGraw-Hill; 1986. pp. 1807–1842. [Google Scholar]
- Akmal M, Valdin J, McCarron M, Massry S. Rhabdomyolysis with and without acute renal failure in patients with phencyclidine intoxication. Am J Nephrol. 1981;1:91–96. doi: 10.1159/000166498. [DOI] [PubMed] [Google Scholar]
- Welch RD, Todd K, Krause GS. Incidence of cocaine-associated rhabdomyolysis. Ann Emerg Med. 1991;20:154–157. doi: 10.1016/s0196-0644(05)81215-6. [DOI] [PubMed] [Google Scholar]
- Singhal P, Rubin B, Peters A, Santiago A, Neugarten J. Rhabdomyolysis and acute renal failure associated with cocaine abuse. Clin Toxicol. 1990;28:321–330. doi: 10.3109/15563659008994433. [DOI] [PubMed] [Google Scholar]
- Koffler A, Friedler RM, Massry SG. Acute renal failure due to nontraumatic rhabdomyolysis. Ann Intern Med. 1976;85:23–28. doi: 10.7326/0003-4819-85-1-23. [DOI] [PubMed] [Google Scholar]
- Timarchi H, Gonzalez J, Olivero J. Hyponatremia-associated rhabdomyolysis. Nephron. 1999;82:274–277. doi: 10.1159/000045413. [DOI] [PubMed] [Google Scholar]
- Cheney P. Early management and physiologic changes in crush syndrome. Crit Care Nurs Q. 1994;17:62–73. doi: 10.1097/00002727-199408000-00007. [DOI] [PubMed] [Google Scholar]
- Shintani S, Shliigai T, Tsukagoshi H. Marked hypokalemic rhabdomyolysis with myoglobinuria due to diuretic treatment. Eur Neurol. 1991;31:396–398. doi: 10.1159/000116702. [DOI] [PubMed] [Google Scholar]
- Fukada Y, Oha S, Mizuno K, Hoshi K. Rhabdomyolysis secondary to hyperemesis gravidarum [case report] Acta Obstet Gynecol Scand. 1999;78:71. doi: 10.1034/j.1600-0412.1999.780115.x. [DOI] [PubMed] [Google Scholar]
- Pirovino M, Neff MS, Sharon E. Myoglobinuria and acute renal failure with acute polymyositis. NY State J Med. 1979;79:764–767. [PubMed] [Google Scholar]
- Kagan L. Myoglobinemia in inflammatory myopathies. JAMA. 1977;237:1448–1452. doi: 10.1001/jama.237.14.1448. [DOI] [PubMed] [Google Scholar]
- Heidemann H, Kruezfelder E. Hypokalemic rhabdomyolysis with myoglobinuria due to licorice ingestion and diuretic treatment. Klin Wochenschr. 1983;61:303–305. doi: 10.1007/BF01497780. [DOI] [PubMed] [Google Scholar]
- Chang P, Lin C, Tsai M, Chien B, Cheng T, Lin C. Rhabdomyolysis associated with hperosmolar non-ketotic coma: a case report. Zhonghua Yi Xue Za Zhi. 1988;41:309–310. [PubMed] [Google Scholar]
- Nishigara G, Higashi H, Matsuo S, Yasunaga C, Sakemi T, Nakamoto M. Acute renal failure due to hypokalemic rhabdomyolysis in Gitelman's syndrome. Clin Nephrol. 1998;50:330–332. [PubMed] [Google Scholar]
- Alshanti M, Eledrisi M, Jones E. Rhabdomyolysis associated with hyperthyroidism [case report] Am J Emerg Med. 2001;19:317. doi: 10.1053/ajem.2001.22483. [DOI] [PubMed] [Google Scholar]
- Singh U, Scheld M. Infectious etiologies of rhabdomyolysis: three case reports and review. Clin Infect Dis. 1996;22:642–649. doi: 10.1093/clinids/22.4.642. [DOI] [PubMed] [Google Scholar]
- Armstrong J. Tropical pyomyositis and myoglobinuria. Arch Intern Med. 1978;138:1145–1146. doi: 10.1001/archinte.138.7.1145. [DOI] [PubMed] [Google Scholar]
- Malvy D, Desalles P, Monseau Y, Bonhoure J. Legionnaire's disease and rhabdomyolysis. Intensive Care Med. 1992;18:132–133. doi: 10.1007/BF01705052. [DOI] [PubMed] [Google Scholar]
- Bagnulo H, Rodriguez F. Rhabdomyolysis during a case of streptococcal toxic shock syndrome. Enferm Infecc Microbiol Clin. 2001;19:82–83. doi: 10.1016/s0213-005x(01)72569-4. [DOI] [PubMed] [Google Scholar]
- Naschitz J, Yeshurun D, Shagrawi I. Rhabdomyolysis in pneumococcal sepsis. Am J Med. 1989;87:479–480. doi: 10.1016/0002-9343(89)90672-4. [DOI] [PubMed] [Google Scholar]
- Pesik N, Otten E. Severe rhabdomyolysis following a viral illness: a case report and review of literature. J Emerg Med. 1996;14:425–428. doi: 10.1016/0736-4679(96)00078-9. [DOI] [PubMed] [Google Scholar]
- Fodili F, van Bommel EF. Severe rhabdomyolysis and acute renal failure following recent Coxsackie B virus infection. Neth J Med. 2003;61:177–179. [PubMed] [Google Scholar]
- Beetham R. Biochemical investigation of suspected rhabdomyolysis. Ann Clin Biochem. 2000;37:581–587. doi: 10.1258/0004563001899870. [DOI] [PubMed] [Google Scholar]
- Abassi Z, Hoffman A, Better O. Acute renal failure as complication or muscle injury. Semin Nephrol. 1998;18:558–565. [PubMed] [Google Scholar]
- Flamenbaum W, Gehr M, Gross M, Kaufman J, Hamburger R. Acute renal failure associated with myoglobinuria and hemoglobinuria. In: Brenner B, Lazarus J, editor. In Acute Renal Failure. Philadelphia, PA: WB Saunders; 1983. pp. 269–282. [Google Scholar]
- Salahudeen A, Wang C, Bigler S, Dai Z, Tachikawa H. Synergistic renal protection by combining alkaline-diuresis with lipid peroxidation inhibitors in rhabdomyolysis: possible interaction between oxidant and non oxidant mechanisms. Nephrol Dial Transplant. 1996;11:635–642. doi: 10.1093/oxfordjournals.ndt.a027352. [DOI] [PubMed] [Google Scholar]
- Zager R, Burkhart K. Differential effects of glutathione and cysteine on Fe2+, Fe3+, H2O2 and myoglobin-induced proximal tubule cell attack. Kidney Int. 1998;53:1661–1672. doi: 10.1046/j.1523-1755.1998.00772.x. [DOI] [PubMed] [Google Scholar]
- Moore K, Holt S, Patel R, Zacker W, Goodier D, Reeder B. A causative role for redox cycling and its inhibition by alkalinization in the pathogenesis and treatment of rhabdomyolysis-induced renal failure. J Biol Chem. 1998;273:31731–31737. doi: 10.1074/jbc.273.48.31731. [DOI] [PubMed] [Google Scholar]
- Clozel M, Anand R, Cooper C, Morrow J. Resolution of muscle calcification in rhabdomyolysis and acute renal failure. Ann Intern Med. 1978;89:928–930. doi: 10.7326/0003-4819-89-6-928. [DOI] [PubMed] [Google Scholar]
- Sauret J, Marinides G, Wang G. Rhabdomyolysis. Am Fam Physician. 2002;65:907–912. [PubMed] [Google Scholar]
- Dayer-Berenson L. Rhabdomyolysis a comprehensive guide. ANNA J. 1994;21:15–18. [PubMed] [Google Scholar]
- Akmal M, Massry S. Reversible hepatic dysfunction associated with rhabdomyolysis. Am J Nephrol. 1990;10:49–52. doi: 10.1159/000168053. [DOI] [PubMed] [Google Scholar]
- Brown C, Rhee P, Chan L, Evans K, Demetriades D, Velmahos G. Preventing renal failure in patients with rhabdomyolysis: do bicarbonate and mannitol make a difference? J Trauma. 2004;56:1191–1196. doi: 10.1097/01.ta.0000130761.78627.10. [DOI] [PubMed] [Google Scholar]
- Koppel C. Clinical features, pathogenesis and management of drug-induced rhabdomyolysis. Med Toxicol Adverse Drug Exp. 1989;4:108–126. doi: 10.1007/BF03259907. [DOI] [PubMed] [Google Scholar]
- Adams EC. Differentiation of myoglobin and hemoglobin in biological fluids. Ann Clin Lab Sci. 1980;10:493–499. [PubMed] [Google Scholar]
- Syrjala H, Vuori J, Huttunen K. Carbonic anhydrase III as a serum marker for the diagnosis of rhabdomyolysis [letter] Clin Chem. 1990;36:696. [PubMed] [Google Scholar]
- Bohlmeyer TJ, Wu AH, Perryman MB. Evaluation of laboratory tests as a guide to diagnosis and therapy of myositis. Rheum Dis Clin North Am. 1994;20:845–856. [PubMed] [Google Scholar]
- Benoist JF, Cosson C, Mimoz O, Edouard A. Serum cardiac troponin I, creatine kinase (CK), and CK-MB in early posttraumatic rhabdomyolysis. Clin Chem. 1997;43:416–417. [PubMed] [Google Scholar]
- Harper J. Rhabdomyolysis and acute renal failure. Crit Care Nurs. 1990;10:32–36. [PubMed] [Google Scholar]
- Knochel J. Hypophosphatemia and rhabdomyolysis. Am J Med. 1992;92:455–457. doi: 10.1016/0002-9343(92)90739-X. [DOI] [PubMed] [Google Scholar]
- Hoogwerf B, Kern J, Bullock M, Comty C. Phencyclidine-induced rhabdomyolysis and acute renal failure. Clin Toxicol. 1979;14:47–53. doi: 10.3109/15563657909030113. [DOI] [PubMed] [Google Scholar]
- Russel T. Acute renal failure related to rhabdomyolysis: pathophysiology, diagnosis, and collaborative management. Nephrol Nurs J. 2000;27:567–577. [PubMed] [Google Scholar]
- Hamilton R, Hopkins M, Shihabi Z. Myoglobinuria, hemoglobinuria and acute renal failure. Clin Chem. 1989;35:1713–1720. [PubMed] [Google Scholar]
- Varon J. Practical Guide to the Care of the Critically Ill Patient. St Louis, MO: Mosby; 1994. pp. 317–319. [Google Scholar]
- Sinert R, Kohl L, Rainone T, Scalea T. Exercise induced rhabdomyolysis. Ann Emerg Med. 1994;23:1301–1306. doi: 10.1016/s0196-0644(94)70356-6. [DOI] [PubMed] [Google Scholar]
- Better O, Rubinstein I. Management of shock and acute renal failure in casualties suffering from the crush syndrome. Renal Failure. 1997;19:647–653. doi: 10.3109/08860229709109030. [DOI] [PubMed] [Google Scholar]
- Curry S, Chang D, Connor D. Drug and toxin-induced rhabdomyolysis. Ann Emerg Med. 1989;18:1068–1084. doi: 10.1016/s0196-0644(89)80933-3. [DOI] [PubMed] [Google Scholar]
- Gunal A, Celiker H, Dogukan A, Ozalp G, Kiraiman E, Simsekli H, Gunay I, Demiran M, Belhan O, Yidirim M, et al. Early and vigorous fluid resuscitation prevents acute renal failure in the crush victims of catastrophic earthquakes. J Am Soc Nephrol. 2004;15:1862–1867. doi: 10.1097/01.ASN.0000129336.09976.73. [DOI] [PubMed] [Google Scholar]
- Luke R, Linton A, Briggs J, Kennedy A. Mannitol therapy in acute renal failure. Lancet. 1965;1:980–982. doi: 10.1016/S0140-6736(65)91216-X. [DOI] [PubMed] [Google Scholar]
- Homsi E, Barreiro M, Orlando J, Higa E. Prophylaxis of acute renal failure in patients with rhabdomyolysis. Ren Fail. 1997;19:283–288. doi: 10.3109/08860229709026290. [DOI] [PubMed] [Google Scholar]
- Zager R. Combined mannitol and deferoxamine therapy for myohemoglobinuric renal injury and oxidant tubular stress. Mechanistic and therapeutic implications. J Clin Invest. 1992;90:711–719. doi: 10.1172/JCI115942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger J. Interventions in clinical acute renal failure: where are the data? Am J Kidney Dis. 1995;26:565–576. doi: 10.1016/0272-6386(95)90590-1. [DOI] [PubMed] [Google Scholar]
- Shilliday I, Allison M. Diuretics in acute renal failure. Ren Fail. 1994;16:3–17. doi: 10.3109/08860229409044843. [DOI] [PubMed] [Google Scholar]
- Lieberthal W, Levinsky N. Treatment of acute tubular necrosis. Semin Nephrol. 1990;10:571–583. [PubMed] [Google Scholar]
- Thadhani R, Pascual M, Bonventre J. Acute renal failure. N Engl J Med. 1996;334:1448–1460. doi: 10.1056/NEJM199605303342207. [DOI] [PubMed] [Google Scholar]
- Eneas J, Schoenfeld P, Humphreys M. The effect of infusion of mannitol–sodium bicarbonate on the clinical course of myoglobinuria. Arch Intern Med. 1979;139:801–805. doi: 10.1001/archinte.139.7.801. [DOI] [PubMed] [Google Scholar]
- Corwin H, Bonventre J. Factors influencing survival in acute renal failure. Semin Dial. 1989;2:220–225. [Google Scholar]
- Ali H, Neito J, Rhamy R, Chandarlapaty S, Vaamonde C. Acute renal failure due to rhabdomyolysis associated with the extreme lithotomy position. Am J Kidney Dis. 1993;22:865–869. doi: 10.1016/s0272-6386(12)70347-5. [DOI] [PubMed] [Google Scholar]
- Pensado A, Ferreira T, Dominguez L, Molins N. Diagnosis and treatment of rhabdomyolysis and myoglobinuria [letter] Rev Esp Anestesiol Reanim. 1996;43:263. [PubMed] [Google Scholar]
- Dhawan R, Jyothingagaram M, Schwartz A. Pathogenesis and Management of Rhabdomyolysis. 1998. http://www.mcphu.edu/continuing/cme/medicine/pathogen/introduc.htm
- Ron D, Taitelman U, Michaelson M, Bar-Joseph G, Bursztein S, Better O. Prevention of acute renal failure in traumatic rhabdomyolysis. Arch Intern Med. 1984;144:277–280. doi: 10.1001/archinte.144.2.277. [DOI] [PubMed] [Google Scholar]
- Mathes D, Assimos D, Donfrio P. Rhabdomyolysis and myonecrosis in a patient in the lateral decubitus position. Anaesthesioogy. 1996;84:727–729. doi: 10.1097/00000542-199603000-00030. [DOI] [PubMed] [Google Scholar]
- Marik PE, Kussman BD, Lipman J, Kraus P. Acetazolamide in the treatment of metabolic alkalosis in critically ill patients. Heart Lung. 1991;20:455–459. [PubMed] [Google Scholar]
- Knochel J, Moore G. Rhabdomyolysis in malaria. N Engl J Med. 1993;329:1206–1207. doi: 10.1056/NEJM199310143291618. [DOI] [PubMed] [Google Scholar]
- Knottenbelt J. Traumatic rhabdomyolysis from severe beating experience of volume diuresis in 200 patients. J Trauma. 1994;37:214–219. [PubMed] [Google Scholar]
- Owen C, Mubarak S, Hargens A. Intramuscular pressures with limb compression. Clarification of the drug-induced muscle-compartment syndrome. N Engl J Med. 1979;300:1169–1172. doi: 10.1056/NEJM197905243002101. [DOI] [PubMed] [Google Scholar]
- Walker P, Lindsay T, Labbe R, Mickle D, Romaschin A. Salvage of skeletal muscle with free radical scavengers. J Vasc Surg. 1987;5:68–75. doi: 10.1067/mva.1987.avs0050068. [DOI] [PubMed] [Google Scholar]
- Youn Y, LaLonde C, Dremling R. Use of antioxidant therapy in shock and trauma. Circ Shock. 1991;35:245–249. [PubMed] [Google Scholar]
- Mandell G. ARDS, neutrophils, and pentoxifylline. Am Rev Resp Dis. 1988;136:1103–1105. doi: 10.1164/ajrccm/138.5.1103. [DOI] [PubMed] [Google Scholar]
- Maclin L. Free radical tissue damage: protective role of antioxidant nutrients. FASEB J. 1987;1:441–445. [PubMed] [Google Scholar]
- Braughler J, Pregenzer J, Chase R, Duncan L, Jacobsen E, McCall J. Novel 21-aminosteroids as potent inhibitors of iron dependent lipid preoxidation. J Biol Chem. 1987;262:1438–1440. [PubMed] [Google Scholar]
- Homsi E, Barreiro M, Orlando J, Higa E. Prophylaxis of acute renal failure in patients with rhabdomyolysis. Ren Fail. 1997;19:283–288. doi: 10.3109/08860229709026290. [DOI] [PubMed] [Google Scholar]
- Forni L, Hilton P. Continuous hemofiltration in the treatment of acute renal failure. N Engl J Med. 1997;336:1303–1309. doi: 10.1056/NEJM199705013361807. [DOI] [PubMed] [Google Scholar]
- Oda J, Tanaka H, Yoshioka T, Iwai A, Yamamura H, Ishikawa K, Matsuoka T, Kuwagata Y, Hiraide A, Shimazu T, et al. Analysis of 372 patients with crush syndrome caused by Hanshin-Awaji earthquake. J Trauma. 1997;42:470–476. doi: 10.1097/00005373-199703000-00015. [DOI] [PubMed] [Google Scholar]
- Nolph K, Qhitcomb M, Schrier R. Mechanisms for inefficient peritoneal dialysis in acute renal failure associated with heat and exercise. Ann Intern Med. 1969;71:317–336. doi: 10.7326/0003-4819-71-2-317. [DOI] [PubMed] [Google Scholar]
- Vanholder R, Sever M, Erek E, Lameire N. Rhabdomyolysis. J Am Soc Nephrol. 2000;11:1553–1561. doi: 10.1681/ASN.V1181553. [DOI] [PubMed] [Google Scholar]
- Llach F, Felsenfeld A, Haussler M. The pathophysiology of altered calcium metabolism in rhabdomyolysis induced acute renal failure. Interactions of parathyroid hormone, 25-hydroxycholecalciferol, and 1,25-dihidroxycholecalciferol. N Engl J Med. 1981;305:117–123. doi: 10.1056/NEJM198107163050301. [DOI] [PubMed] [Google Scholar]
- Akmal M, Bishop J, Telfer N, Norman A, Massry S. Hypocalcemia and hypercalcemia in patients with rhabdomyolysis and without acute renal failure. J Clin Endocrinol Metab. 1986;63:137–142. doi: 10.1210/jcem-63-1-137. [DOI] [PubMed] [Google Scholar]
- Bilezikian JP. Clinical review 51: management of hypercalcemia. J Clin Endocrinol Metab. 1993;77:1445–1449. doi: 10.1210/jc.77.6.1445. [DOI] [PubMed] [Google Scholar]
- Bourke E, Delaney V. Assessment of hypocalcemia and hypercalcemia. Clin Lab Med. 1993;13:157–181. [PubMed] [Google Scholar]
- Dent DM, Miller JL, Klaff L, Barron J. The incidence and causes of hypercalcemia. Postgrad Med J. 1987;63:745–750. doi: 10.1136/pgmj.63.743.745. [DOI] [PMC free article] [PubMed] [Google Scholar]


