Abstract
Background
Gestational diabetes mellitus is hyperglycemia in special populations (pregnant women), however gestational diabetes mellitus (GDM) not only affects maternal health, but also has profound effects on offspring health. The prevalence of gestational diabetes in my country is gradually increasing.
Objective
To study the application effect of self-transcendence nursing model in GDM patients.
Methods
One hundred fourteen GDM patients undergoing prenatal examination in Hai'an People’s Hospital from January 2019 to November 2021 were selected and divided into two groups of 57 cases respectively according to the principle of random single blind. The patients in the control group should receive pregnancy health care under the routine nursing mode, while those in the observation group should receive pregnancy health care under the self-transcendence nursing mode. Then, we would compare the insulin utilization rate, admission before delivery, gestational weeks, delivery outcome and neonatal conditions between the two groups, examine the changes of blood glucose related indexes in the two groups and evaluate the differences between the two groups' Diabetes Distress Scale (DDS) scores and Chinese Versions of Diabetes Management Self-efficacy Scale (C-DMSES) scores.
Results
The number of hospital admissions (1.12 ± 0.31) and the hospital stay (7.54 ± 1.45) days in the observation group were less than those in the control group (1.56 ± 0.42) and (10.23 ± 2.32) days. There was no difference between the two groups after statistical analysis of gestational weeks and insulin utilization rate (P > 0.05). After the intervention, the total DDS score and emotional burden, doctor/life law/interpersonal relationship related distress score of GDM in the two groups were lower than those before the intervention, while the scores of healthy diet, regular exercise, regular monitoring of blood glucose and medication compliance in C-DMSES were higher than those before the intervention. In addition, the improvements of overall DDS scores and C-DMSES scores of GDM in the observation group were significantly better than those in the control group, so there was statistical significance (P < 0.05). In terms of the pregnancy outcomes and neonatal conditions, the rates of premature delivery and neonatal delivery in the observation group were higher than those in the control group, and there was no difference (P > 0.05) in other aspects of pregnancy outcomes and neonatal conditions.
Conclusion
Self-transcendence nursing mode intervention can improve blood sugar, reduce psychological distress, and improve self-efficacy in GDM patients, thereby reducing the rate of pregnancy-induced hypertension and premature birth.
Keywords: Self-transcendence nursing mode, Gestational diabetes mellitus, Blood glucose, Degree of psychological distress, Pregnancy outcome
Introduction
Gestational diabetes mellitus
Gestational diabetes mellitus (GDM) is defined as abnormal glucose metabolism first discovered or occurred during pregnancy rather than pregestational diabetes mellitus (PGDM) [1]. The recorded prevalence of GDM varies considerably worldwide, ranging from 1–30% [2, 3], and the global prevalence of GDM is increasing annually as a result of lifestyle changes and updated diagnostic criteria. In China, the prevalence of GDM was as high as 24.4% [4]. GDM is signifcantly associated with an increased risk of various adverse pregancy outcomes, including postpartum hemorrhage, miscarriage, premature delivery, macrosomia, intrauterine infection, asphyxia and other adverse pregnancy outcomes [5]. In addition, offspring of women with GDM have a higher likelihood of developing obesity and glucose metabolism disorders, and cardiovascular disease in childhood or early adulthood [6].
Therefore, it is necessary to actively control blood glucose through lifestyle management. In 2020, a national guideline for GDM screening and management was issued, emphasizing the need for standardized GDM care for all pregnant women,that includes health education, GDM screening, lifestyle management (such as diet and exercise), reminders, blood glucose monitoring, and insulin therapy [7]. However, the current intervention measures are only implemented during the diagnosis and treatment of patients during the obstetric examination, and mainly focus on health education regarding diet, exercise, medication and obesity control. Several studies show that pregnant women with gestational diabetes are more likely to have sub-health mental state [8]. Previous qualitative studies have found that following a GDM diagnosis, people with GDM experience high levels of stress, face major barriers to incorporating nutritional recommendations into their daily social lives, and possess an overall lack of education (e.g., on healthy dietary choices, skills necessary to make lifestyle changes and support glucose management) [9]. Considering that forced lifestyle changes may lead to negative mental and physical health outcomes, such as diabetes distress, stigma, decreased psychological resilience, and lower quality of life, attending to the psychological health of individuals with GDM remains critically important.This also shows the importance of integrating mental health promotion strategies to enhance the quality of life of pregnant women with GDM.
Self-transcendence theory
In foreign countries, the implementers of self-transcendence theory mainly include doctors, psychotherapists and responsible nurses [10], and the intervention targets of self-transcendence theory are mainly cancer patients, mental illness patients and terminal patients [11]. The psychological characteristics of these patients are that they are unable to face their illnesses positively or have difficulty in facing their illnesses positively in the face of major illnesses or mental and psychological stresses and traumas. However, the special characteristics of cancer patients are that their illnesses are serious and their psychological traumas are deep, and they are under tremendous pressure both physically and psychologically.
The theory of self-transcendence includes four dimensions: inner activity of the self, attention to others, structured recall [12], practice of promoting transpersonal expansion [13] (meditative breathing), and gathering personal spiritual power, which corresponds to the personal, interpersonal, and transcendental practice of time to achieve self-transcendence. Self-transcendence theory uses meditation practice as a key intervention within the theoretical framework. Self-transcendence occurs in the context of vulnerability, i.e., the individual becomes aware of his or her own mortality or experiences something challenging and difficult, and in the face of a crisis, the individual is able to continually search for himself or herself and connect with others through introspection, reflection, and meditative activities, transforming behaviours, determining further goals, and continually expanding in relation to others and the environment [14]. Temporary expansion can help individuals to structure their memories by connecting with the past and the future, recalling the past, perceiving the present, enhancing their spiritual power, creating meaning in the present [15], gaining a sense of well-being, and ultimately achieving self-transcendence.
In foreign countries, research on self-transcendence theory has been widely conducted, and related intervention studies have achieved certain results. In China, however, there is less relevant literature, and most of the studies are descriptive, focusing on the measurement of self-transcendence level and the analysis of related factors, and very few intervention studies, probably due to the fact that the theory originated in the West, and its positive interpretations of aging and disease are different from the traditional Chinese thinking. At the same time, the theory has no specific explanation of how individuals achieve self-transcendence, and related concepts such as "personal ceiling" and "self-transcendence" are abstract and macroscopic, so it may be difficult for nursing practitioners with weak theoretical foundations to apply the theory to guide clinical practice.
This study builds a self-transcendence care model for gestational diabetes patients based on self-transcendence theory. The intervention programme of the model is based on the four dimensions of self-transcendence theory, focusing on the centre of gestational diabetes patients, helping them to understand their inner selves, alleviate their bad moods and improve their psychological distress through communication with patients, shifting from concern for themselves to concern for others, and cherishing the present moment in structured memories.We will also help the patients to understand their inner self, alleviate negative emotions, improve psychological distress, shift from concern for themselves to concern for others, cherish the present moment in structured reminiscence, look forward to the future, build up personal spiritual strength, increase confidence in the treatment of gestational diabetes, raise the level of hope, and thus improve clinical outcomes.
We hypothesised that the self-trancedence care model based on the self-trancedence theory would improve diabetes distress of pregnant woman with GDM and that the self-trancedence nursing model would produce beneficial effects in relation to perceived social support and quality of life. Thus, The primary objective of this study was to prospectively investigate the effects of the self-transcendence care model on psychological distress.The secondary objective was to examine the effects of the self-transcendence care model on their dynamic change of blood glucose, and pregnancy outcomes in patients with GDM in second-third trimester pregnancy.
Materials and methods
Trial desigin
This study was a single-centre, single-blind, randomised controlled trial (RCT) designed to study the application effect of self-transcendence nursing model in GDM patients.The primary outcome was patients' Diabetes Distress Scale (DDS) scores and Chinese Versions of Diabetes Management Self-efficacy Scale (C-DMSES) scores, and the secondary outcomes were the number of admissions and hospitalization time before delivery, insulin utilization rate, gestational weeks of delivery, delivery outcomes (such as delivery mode, oligohydramnios, pregnancy-induced hypertension, etc.) and neonatal conditions (such as macrosomia, intrauterine distress, premature delivery, etc.).
Participants
Recruitment
Patients with GDM who underwent prenatal examination in Hai'an People’s Hospital from January 2019 to November 2021 were selected.Simple randomisation was used to divide the patients into two groups according to the random number table method, and patients were blinded. The study was approved by the Ethics Committee of Haian County People's Hospital (HLK2018042).
Inclusion criteria: (1) GDM meeting the criteria of < Obstetrics and Gynecology > [16] 2 consecutive abnormal oral glucose tolerance test results or fasting blood glucose ≥ 5.1 mmol/L; (2)18–35 year-old patients with singleton pregnancy; (3) Patients that can understand and cooperate with the investigator to complete the questionnaire; (4) Patients carrying out pregnancy care in our hospital and completing the delivery; (5) Patients with 25–28 pregnancy weeks; (6) Patients agreeing to participate in the study.
Exclusion criteria: (1) Patients with other pregnancy complications; (2) Patients with abnormal blood glucose before pregnancy; (3) Patients with a history of high-risk pregnancy(e.g. ①Pregnant woman's age < 18 years or > 35 years. ② History of abnormal pregnancy, such as miscarriage, preterm delivery, etc. ③ Various pregnancy complications,such as eclampsia、heart disease. ④ Those who may have abnormal delivery. ⑤ Placental insufficiency. ⑥ Other pathological obstetric problems and abnormal pregnancies, etc.); (4) Patients with thyroid disease, hematopoietic system disease, neurological disease, etc.; (5) Patients with a history of smoking and alcoholism; (6) Patients with known fetal abnormality.
Sample size
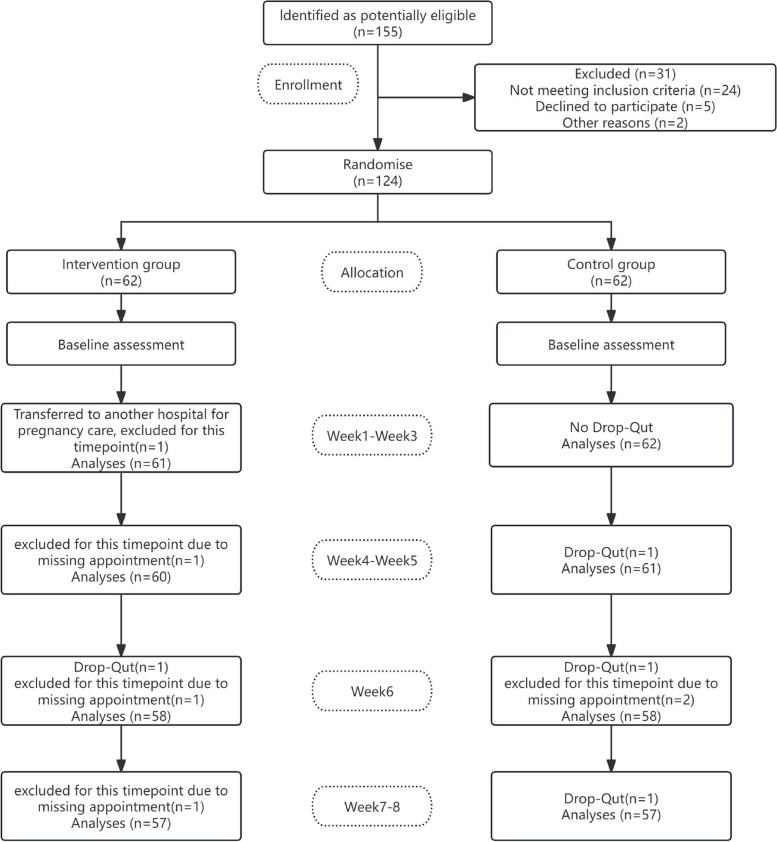
We used the G-Power programme (Version 3.1 software) to calculate the sample size.The sample size was calculated based on the expected difference in the primary outcome of previous studies [17] i.e., the difference in patients' psychological status between the usual care and intervention groups. The required sample for each group was determined as 20 with a power of 0.8, an alpha value of 0.05, and a 1.5 effect size using a t-test. Of the 124 patients included, 62 patients were randomly allocated to the usual care group and 62 to the intervention group. Details of the number of participants at each time point are shown in Fig. 1 below, and details of the total number of participants for each variable are shown in Tables 1, 2, 3, 4, 5, and 6.
Fig. 1.
Flowchart
Table 1.
Comparison of health care data between two groups of GDM patients
| Health information | Control group (n = 57) | Observation group (n = 57) | χ2/t | Cohen's d/Phi/Cramer V | P | |
|---|---|---|---|---|---|---|
| Maternal type | Primipara | 31 (54.39) | 34 (59.65) | 0.332 | 0.124 | 0.570 |
| Multiparous women | 26 (45.61) | 23 (40.35) | ||||
| Age (year) | 56.85 ± 11.47 | 55.93 ± 12.05 | 0.418 | 0.289 | 0.677 | |
| Body mass (kg) | 55.89 ± 5.23 | 55.73 ± 5.61 | 0.157 | 0.204 | 0.875 | |
| Gestational weeks (week) | 26.36 ± 1.41 | 26.43 ± 1.35 | 0.270 | 0.459 | 0.787 | |
| Pregnancy times (second) | 1.85 ± 0.45 | 1.88 ± 0.43 | 0.364 | 0.334 | 0.717 | |
| Systolic pressure (mmHg) | 123.47 ± 9.52 | 122.53 ± 10.04 | 0.513 | 0.365 | 0.609 | |
| Diastolic pressure (mmHg) | 76.56 ± 4.89 | 76.51 ± 5.02 | 0.054 | 0.503 | 0.957 | |
| Degree of education (n) | Junior high school and below | 12 (21.05) | 8 (14.04) | 1.613 | 0.012 | 0.657 |
| Technical secondary school and College | 13 (22.81) | 12 (21.05) | ||||
| Undergraduate | 22 (38.60) | 28 (49.12) | ||||
| Bachelor degree or above | 10 (17.54) | 9 (15.79) | ||||
| Family per capital monthly income (Yuan) | < 1700 | 10 (18.54) | 10 (17.54) | 0.394 | 0.129 | 0.821 |
| 1700–5000 | 29 (50.88) | 26 (45.61) | ||||
| > 5000 | 18 (31.58) | 21 (36.84) | ||||
| Marital status (n) | Married | 48 (84.21) | 51 (89.47) | 0.691 | 0.236 | 0.406 |
| Unmarried | 9 (15.79) | 6 (10.53) | ||||
| Occupation (n) | On the job | 46 (80.70) | 48 (84.21) | 0.243 | 0.412 | 0.622 |
| No occupation | 11 (19.30) | 9 (15.79) | ||||
Table 2.
Comparison of general indicators of GDM patients in health care period between the two groups
| Group | n | Insulin use rate (%) | Number of hospital admissions before delivery (second) | Hospital stay before delivery (d) | Gestational week of delivery (week) |
|---|---|---|---|---|---|
| Control group | 57 | 6 (10.53) | 1.56 ± 0.42 | 10.23 ± 2.32 | 38.08 ± 1.73 |
| Observation group | 57 | 1 (1.75) | 1.12 ± 0.31 | 7.54 ± 1.45 | 38.32 ± 1.56 |
| χ2/t | 3.805 | 6.364 | 7.423 | 0.778 | |
| Cohen's d/Phi | 0.221 | 0.681 | 0.880 | 0.798 | |
| P | 0.051 | 0.000 | 0.000 | 0.438 |
Table 3.
Comparison of blood glucose related indexes between the two groups of GDM
| Group | n | FPG (mmol/L) | 2hPG (mmol/L) | HbA1c (%) | |||
|---|---|---|---|---|---|---|---|
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | ||
| Control group | 57 | 5.96 ± 0.37 | 5.01 ± 0.23* | 7.78 ± 0.41 | 6.23 ± 0.36* | 6.72 ± 0.31 | 5.57 ± 0.24* |
| Observation group | 57 | 6.02 ± 0.35 | 4.67 ± 0.20* | 7.69 ± 0.46 | 5.72 ± 0.34* | 7.65 ± 0.33 | 5.11 ± 0.21* |
| t | 0.889 | 8.422 | 1.103 | 7.776 | 15.508 | 10.890 | |
| Cohen's d | 0.356 | 0.754 | 0.223 | 0.781 | 0.651 | 0.873 | |
| P | 0.376 | 0.000 | 0.273 | 0.000 | 0.000 | 0.000 | |
*Represents the comparison before and after intervention in the same group; p < 0.05
Table 4.
Comparison of DDS scores of GDM patients in the two groups (point)
| Group | n | Emotional burden | Doctor related distress | Life law related distress | Interpersonal relationship related distress | Total DDS score | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | ||
| Control group | 57 | 13.74 ± 2.59 | 10.86 ± 1.94* | 8.68 ± 2.16 | 7.61 ± 1.67* | 14.12 ± 3.21 | 12.01 ± 2.14* | 7.85 ± 1.67 | 6.31 ± 1.21* | 44.39 ± 5.29 | 36.79 ± 4.28* |
| Observation group | 57 | 13.81 ± 2.46 | 9.08 ± 1.61* | 8.81 ± 2.03 | 6.52 ± 1.38* | 14.05 ± 3.19 | 8.25 ± 1.71* | 7.79 ± 1.81 | 4.89 ± 1.04* | 44.46 ± 5.13 | 28.74 ± 4.12* |
| t | 0.148 | 5.331 | 0.331 | 3.799 | 0.117 | 10.363 | 0.184 | 6.719 | 0.072 | 10.230 | |
| Cohen's d | 0.367 | 0.769 | 0.561 | 0.889 | 0.531 | 0.731 | 0.221 | 0.976 | 0.349 | 0.641 | |
| P | 0.883 | 0.000 | 0.741 | 0.000 | 0.907 | 0.000 | 0.854 | 0.000 | 0.943 | 0.000 | |
*Represents the comparison before and after intervention in the same group; p < 0.05
Table 5.
Comparison of C-DMSES scores of GDM patients in the two groups (point)
| Group | n | Healthy diet | Regular movement | Regular blood glucose monitoring | Medication compliance | Total C-DMSES score | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | ||
| Control group | 57 | 58.96 ± 6.81 | 82.12 ± 8.11* | 10.23 ± 2.89 | 13.23 ± 3.11* | 21.13 ± 5.98 | 35.85 ± 6.41* | 10.13 ± 2.74 | 14.91 ± 3.08* | 100.45 ± 12.25 | 146.11 ± 16.58 |
| Observation group | 57 | 59.23 ± 6.57 | 91.68 ± 8.76* | 10.19 ± 2.72 | 15.63 ± 3.27* | 20.89 ± 6.07 | 40.52 ± 5.85* | 10.19 ± 2.53 | 17.17 ± 3.37* | 100.50 ± 13.27 | 165.00 ± 15.28 |
| t | 0.215 | 6.046 | 0.076 | 4.015 | 0.213 | 4.063 | 0.121 | 3.737 | 0.021 | 6.325 | |
| Cohen's d | 0.341 | 0.719 | 0.221 | 0.671 | 0.013 | 0.971 | 0.231 | 0.865 | 0.139 | 0.621 | |
| P | 0.830 | 0.000 | 0.939 | 0.000 | 0.832 | 0.000 | 0.904 | 0.000 | 0.983 | 0.000 | |
*Represents the comparison before and after intervention in the same group; p < 0.05
Table 6.
Comparison of delivery outcomes and neonatal conditions between the two groups of GDM patients
| Delivery outcome and neonatal status | Control group (n = 57) | Observation group (n = 57) | χ2 | Phi | P | |
|---|---|---|---|---|---|---|
| Delivery outcome | ||||||
| Mode of delivery (n) | Vaginal delivery | 29 (50.88) | 42 (73.68) | 6.311 | 0.546 | 0.012 |
| Cesarean section | 28 (49.12) | 15 (26.32) | ||||
| Pih (n) | yes | 9 (15.79) | 2 (3.51) | 4.930 | 0.479 | 0.026 |
| no | 48 (84.21) | 55 (96.49) | ||||
| Oligohydramnios (n) | yes | 12 (21.05) | 8 (14.04) | 0.970 | 0.091 | 0.325 |
| no | 45 (78.95) | 49 (85.96) | ||||
| Premature rupture of membranes (n) | yes | 9 (15.79) | 7 (12.28) | 0.291 | 0.124 | 0.590 |
| no | 48 (84.21) | 50 (87.72) | ||||
| Neonatal condition | ||||||
| Giant (n) | yes | 4 (7.02) | 1 (1.75) | 1.883 | 0.341 | 0.170 |
| no | 53 (92.98) | 56 (98.25) | ||||
| Low body mass infants (n) | yes | 6 (10.53) | 4 (7.02) | 0.439 | 0.125 | 0.508 |
| no | 51 (89.47) | 53 (92.98) | ||||
| Premature delivery (n) | yes | 8 (14.04) | 2 (3.51) | 3.946 | 0.731 | 0.047 |
| no | 49 (85.96) | 55 (96.49) | ||||
| Fetal distress (n) | yes | 8 (14.04) | 6 (10.53) | 0.326 | 0.236 | 0.568 |
| no | 49 (85.96) | 51 (89.47) | ||||
Methods
Control group
The patients in the control group received health care during pregnancy under the routine nursing mode. Firstly, they were told about hypoglycemia, precautions for glucose control, diet and exercise guidance, prevention and treatment of common complications during the diagnosis and treatment interval on the day of the obstetric examination. Secondly, they were instructed to check their blood glucose regularly, and record the results. Finally, they were provided with Gestational Diabetes Health Knowledge Handbook, and were instructed to pay full attention to blood glucose control. In addition, those patients with invalid effects on diet and exercise intervention should be given insulin drug treatment in time.
Observation group
The patients in the observation group adopted self-transcendence nursing mode for pregnancy care. First, a self-transcendence theory nursing intervention group was established, which consisted of head nurses, psychotherapists, and nursing staff with titles above nurses and all of them had solid nursing expertise and good communication skills. All interventionists are uniformly trained by qualified psychotherapists. The intervention programme based on the Self-transcendence theory model of care is shown in Table 7.
Table 7.
The intervention programme based on the Self-transcendence theory model of care
| Intervention time | Theme of intervention | Content of the intervention | Duration of intervention | Forms of intervention |
|---|---|---|---|---|
| Week1-Week3 | Inner activities and experience | The patients were given the group intervention in the first two weeks, and were guided to improve their emotional management ability by means of special lectures and group discussions. The patients were helped to practice meditation by listening to soft music, through which they would feel comfortable, and to improve their awareness and acceptance of inner experience. In the third week, group intervention was conducted for about 30 min. The patients were instructed to practice on-site meditation according to the voice prompts, and were asked to practice meditation at home for 30 min in a day. The patients were also asked to describe their own personality, strengths and weaknesses in the form of pictures and language, and were guided to deepen their self-understanding through self-reflection | 60 min/time, 1 week/time | group intervention |
| Week4-Week5 | Caring about others | In the 4th week, Patients were organized and encouraged to discuss the treatment process and mental journey, and try to think from the perspective of others and beyond the problem itself. They were also encouraged to build a harmonious relationship, and be more willing to care about and help others. In the 5th week, encourage patients to communicate with their families, share housework, send thanksgiving messages, and proactively express their gratitude | 60 min/time, 1 week/time |
Week4:one-to-one intervention Week5:group intervention |
| Week6 | Reviewing the past and expecting the future | Guide patients to recall their experiences step by step, reconstruct past episodes, think about the meaning of life from it, and experience the positive emotions induced by good memories to increase happiness | 60 min/time, 1 week/time | group intervention |
| Week7-Week8 | Individual mental strengt | A supportive group course was carried out to introduce the concept and intervention methods of self-transcendence theory to the patients for the first time, and guide them to think about how to accept and surpass themselves. For the second time, the sentences included in Chicken Soup for the Soul were selected to guide patients to think about things and conduct discussions to enhance their perception of life and to strengthen the individual's spiritual strength | 30 min/time, 1 week/time | group intervention |
Detection methods
Before and after the intervention, 5 ml fasting peripheral venous blood samples were taken, fasting and drinking for at least 8 h before blood collection, placed in vacuum blood collection, placed at room temperature for 1 h after centrifuge processing, 3000r/min centrifugal 15 min, centrifugal radius 8 cm. Fasting blood glucose ( FPG) was detected by hexokinase method. Detection instrument:ROCHE cobas8000, according to the operation steps of biochemical analyzer. Hemoglobin A1c ( HbA1c) was detected by Bio-Rad Variant II glycosylated hemoglobin analyzer. Blood was taken again at 2 h after feeding, and the blood vessels were collected in vacuum. After being placed at room temperature for 1 h, the blood was centrifuged at 3000 r/min for 15 min, and the centrifuge radius was 8 cm. Serum was collected to detect 2 h postprandial plasma glucose(2hPG) by hexokinase method.
Measurable outcomes
Primary outcome
Diabetes Psychological Distress Scale (DDS) [18]: The Cronbach's α coefficient for the Chinese version of the total scale was 0.951, and the Cronbach's α coefficients for the four subscales, namely, emotional burden, doctor-related pain, routine-related pain, and relationship-related pain, were 0.842, 0.951, 0.850, and 0.931, respectively. There are 17 entries, with individual scores of 1–6 indicating the degree of the problem, and the total score of DDS is 17–102 that represents the degrees of psychological distress of the patient.
Diabetes Management Self-efficacy Scale (C-DMSES) score [19]: including healthy diet, regular exercise, regular monitoring of blood sugar, and medication compliance and a total of 20 items, where a single score of 0–10 points indicates the degrees of management effectiveness and the total score of C-DMSES is 0–200 that represents the degrees of patient management self-efficacy. The Cronbach's α coefficients for the main measures of the scale ranged from 0. 611 to 0. 947.
Secondary outcome
The number of admissions and hospitalization time before delivery, insulin utilization rate, gestational weeks of delivery, delivery outcomes (such as delivery mode, oligohydramnios, pregnancy-induced hypertension, etc.), neonatal conditions (such as macrosomia, intrauterine distress, premature delivery, etc.), blood glucose related indexes including FPG, HbA1c, 2hPG(all are average blood glucose levels)of GDM patients in the two groups were recorded.
Statistical methods
The data were processed by SPSS19.0. The K-S method was used to test the normality of measurement data such as body weight, number of admissions, length of stay, blood glucose index, DDS score and C-DMSES score. The measurement data conforming to the normal distribution were described by (‾χ ± s). Paired samples t-tests were used for within-group comparisons, and independent samples t-tests were used for between-group comparisons. The enumeration data such as education level, occupation, maternal type, insulin utilization rate, delivery outcome and neonatal condition were described by the number of cases ( percentage). The enumeration data were compared by χ2 test, and P < 0.05 was statistically significant.
Results
Generally, the demographic data of the two groups were comparable, while the results of the general indicators in the health care period, blood glucose related indexes, DDS scores, C-DMSES scores, delivery outcomes and neonatal conditions were better in the observation group than in the control group. Followings were the detailed results.
Comparison of health care data between the two groups of GDM patients
The maternal type, age, body mass, gestational weeks, pregnancy times, systolic pressure, diastolic pressure, degree of education, family per capital monthly income, marital status, and occupation of the two groups were not significantly different (P > 0.05). See Table 1 for more details.
Comparison of general indicators of GDM Patients in the health care period between the two groups
The number of hospital admissions and the hospital stay before delivery of GDM patients in the observation group were less than those in the control group (P < 0.05). There was no significant difference in the gestational week and insulin use rate between the two groups (P > 0.05). See Table 2 for more details.
Comparison of blood glucose related indexes between the two groups of GDM patients
Before intervention, the FPG, 2hPG and HbA1c of two groups were not significantly different (P > 0.05). After intervention, the FPG, 2hPG, and HbA1c of the GDM patients in the two groups were lower than those before the intervention, and these data were lower in the observation group than in the control group (P < 0.05). See Table 3 for more details.
Comparison of DDS scores of the GDM patients in the two groups
Before intervention, the DDS total score and the 4 dimensions (including emotional burden/doctor/life law/interpersonal relationship related distress) scores of the two groups were not significantly different (P > 0.05). After intervention, the DDS total score and the 4 dimensions scores of the two groups increased significantly (P < 0.05), and the DDS total score and the 4 dimensions scores of the observation group were higher than those of the control group (P < 0.05). See Table 4 for more details.
Comparison of C-DMSES scores of GDM patients in the two groups
Before the intervention, there was no difference (P > 0.05) in the C-DMSES scores of the two groups of GDM patients. After the intervention, the total C-DMSES scores of the two groups of GDM patients and the scores of 4 dimensions of healthy diet, regular exercise, regular blood glucose monitoring, and medication compliance were higher than those before intervention. In addition, the improvements of overall C-DMSES scores of GDM patients in the observation group were higher than those in the control group, which was of statistical significance (P < 0.05). See Table 5 for more details.
Comparison of delivery outcomes and neonatal conditions between the two groups of GDM patients
In terms of the delivery outcomes, the vaginal delivery rate of the observation group was higher than that of the control group, the pregnancy-induced hypertension rate was lower than that of the control group, and there was no difference in other delivery outcomes (P > 0.05). In terms of the neonatal conditions, the premature delivery rate of the observation group was lower than that of the control group, and there was no difference in macrosomia, intrauterine distress and other aspects (P > 0.05). See Table 6 for more details.
Discussion
As a common complication during pregnancy and one of the common types of high-risk pregnancy in obstetrics, GDM has certain adverse effects on both mother and fetus. Epidemiological surveys finds that the incidence of GDM was about 1%−5% [20], and there is a gradual upward trend, which brings new problems and challenges to clinical work in obstetrics [21]. With the increasing awareness of obstetric health care, more and more attention has been paid to prenatal examinations, and the detection rate of GDM has also increased [22, 23]. Some studies have found that the self-management behaviors of GDM patients were poor. And this seriously affected their self-management behaviors such as diet, exercise, and medication compliance, and even affected their emotional state, which is not conducive to the health of mothers and fetus [24]. Conventional perinatal nursing interventions mostly focus on oral education, publicity materials, etc. between diagnosis and treatment. GDM patients often receive education passively because they cannot fully understand and implement the materials, and cannot gain the feedback of existing doubts timely. Therefore, the overall intervention effect is not that ideal [25].
In this study, all the intervention groups had better glycaemic control than the control group, and the variance is large,which is the same as the findings of Yan Meichen et al. [26]. The intervention programme based on the self-transcendence care model stimulated the subjective initiative in the self-management of the pregnant women's disease, and the pregnant women changed from passively accepting the guidance of the healthcare personnel to actively participating in the pregnancy care and actively seeking for ways to effectively control the blood glucose level, thus effectively controlling the blood glucose level. However, there was no difference in insulin use rate between the two groups,and the variance is small. The reason for this may be analysed as the pregnant women's concern about poor blood glucose control affecting the foetus, and even if the blood glucose level is within the normal range, the pregnant women will continue to routinely inject insulin in accordance with medical advice. In addition, the number of hospital admissions and the length of antenatal stay were reduced in GDM patients, the rate of vaginal delivery was higher than that of patients who received routine nursing interventions, and the incidence of gestational hypertension and preterm labour was lower than that of patients who received routine nursing interventions, and the variance is large,which was similar to the results of the study conducted by Chen Yuyi and Ma Xiangfei et al. [27, 28]. These results suggested that self-transcendence nursing mode intervention could maintain the health status of GDM patients, reduce the risk of hospital admission during pregnancy, and improve pregnancy outcomes. This is because the self-transcendence nursing model can guide patients to pay attention to their hearts through interventions such as rational emotional therapy and meditation practice so as to improve patients' acceptance of the disease and control over their emotions, and reduce the negative emotions of patients due to illness. Social support has a significant impact on the level of hope and it can provide a platform for patients to share their experiences through communication between patients [29]. It can help patients to gain new insights of the life, and build confidence in disease recovery. And it is helpful for the patients to strengthen their emotional communication between patients and their families through expressions of gratitude, so that the patients can obtain more emotional support from their families, and be encouraged to continuously surpass, improve their level of hope, better cope with diseases, and actively cooperate with treatment. This will be conducive to the stable control of blood glucose to provide a positive growth and development environment for the fetus, and improve the outcome of the mother and fetus [30–32]. However, for patients who received usual care interventions, there were no differences between the two groups in terms of gestational age, other birth outcomes and neonatal status,and the variance is also small. The reason for this may be analysed because the sample size of this study was small and insufficient to detect differences between the two groups. It may also be because the pregnant women in the control group, after the diagnosis of gestational diabetes mellitus, increased their attention to it and more consciously adjusted their lifestyles, as well as continuously controlling their blood glucose levels in a variety of ways under the guidance of professional obstetricians and endocrinologists, which reduced its impact on pregnancy outcomes.
This study also used the DDS score to evaluate the degree of psychological distress of the patients and adopted the C-DMSES score to evaluate the self-management efficacy. It was found that the total score of DDS and its scores of emotional burden, doctor/life law/interpersonal relationship related distress in the two groups after intervention were lower than those before intervention. The scores of healthy diets, regular exercise, regular monitoring of blood glucose and medication compliance in the C-DMSES score were higher than those before intervention. The improvement of DDS score and C-DMSES score in the self-transcendence nursing intervention group was significantly higher than that in the routine nursing intervention group,and all the variance is large. The nursing intervention programme based on the trans-theoretical model constructed by Zou Yujiao et al. can improve the self-management ability of pregnant women with high risk of gestational diabetes mellitus, help them to do a good job of pregnancy health management, and improve their postprandial blood glucose level [17]. Ren Yonglian et al. used network cognitive-behavioural therapy to improve pregnant women's negative emotions, which can meet the needs of pregnant women's health care during pregnancy [33]. The above results suggest that self-transcendence nursing intervention can reduce the psychological distress of GDM patients and improve their self-efficacy. Under the intervention of self-transcendence nursing mode, GDM patients can respond to diseases more actively and optimistically, maintain emotional stability, and actively cooperate with medical instructions such as diet, exercise, medication, and blood glucose monitoring, so as to stabilize the blood glucose level during pregnancy.
In conclusion, the intervention of self-transcendence nursing mode can improve GDM patients’ blood glucose, alleviate their psychological distress, improve their self-efficacy, and reduce their rate of pregnancy-induced hypertension and premature delivery.
Strengths and limitations
At present, few studies at home and abroad have applied the self-transcendence nursing model to high-risk pregnant women with gestational diabetes mellitus. Based on the self-transcendence nursing model, this study constructed a nursing intervention programme for high-risk pregnant women with gestational diabetes mellitus with certain scientific validity and feasibility. The intervention program focuses on cultivating positive attitudes in pregnant women with high risk of GDM, and starts from the actual needs of pregnant women with high risk of GDM, establishes the belief of self-transcendence, helps them to establish healthy behaviours, and does a good job of health management during pregnancy, so as to reduce the risk of GDM, and provides new references for the primary prevention of gestational diabetes mellitus.
However, due to the limitations of various objective conditions such as time, manpower and research funding, the sample size of this study was small and all the study subjects came from the same hospital, the representativeness of the study subjects was poor, which may not be able to satisfy the need to find out the differences between the intervention group and the control group in terms of the incidence of GDM and the pregnancy outcome, thus limiting the results of the study. In the future, it is necessary to further optimise the study design, conduct a randomised controlled trial, and expand the sample size and sample source to improve the representativeness of the sample, so as to facilitate more precise observation of the differences between the two groups, improve the level of evidence of the study results, and promote a better dissemination of the study results. In addition, the intervention duration and follow-up time of this study were short. In the future, the intervention time can be advanced to pre-pregnancy and the follow-up time can be lengthened, and more appropriate research tools can be found to increase the evaluation indexes, so as to more comprehensively and accurately observe the near-, medium- and long-term effects of the nursing intervention programme based on the self-transcendence nursing model in assisting pregnant women to establish healthy behaviours and improve maternal and infant health.
Conclusions
Gestational diabetes mellitus is hyperglycemia in special populations (pregnant women), however gestational diabetes mellitus (GDM) not only affects maternal health, but also has profound effects on offspring health. The prevalence of gestational diabetes in my country is gradually increasing. This study constructed an intervention programme for pregnant women at high risk of gestational diabetes mellitus using the self-transcendence care model as a guide. The intervention programme has certain scientific validity and feasibility. Compared with the conventional nursing intervention, the nursing intervention based on the self-transcendence nursing model is more effective in reducing the degree of psychological distress and enhancing the sense of self-efficacy of high-risk pregnant women with GDM, and it can assist high-risk pregnant women with GDM in controlling their blood glucose levels effectively to a certain extent,and reduce their rate of pregnancy-induced hypertension and premature delivery.
Authors’ contributions
MP X and JJ F conceived and designed the study. Y W performed the literature search. Y W and ZM Lacquired data and drafted the manuscript.MP X and W C wrote the original draft. YQ Z and JJ F assisted in revising the manuscript. YQ Z and JJ F wrote, reviewed and edited the manuscript. YQ Z, and JJ F the authenticity of all the raw data. All authors have read and approved the final manuscript.
Funding
This work was supported by Nantong municipal bureau on science and technology, Jiangsu [grant numbers MSZ2023231].
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Medical Ethics Committee of the Hai’an People’s Hospital on December 21, 2018 (approval number: HKL201842). Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mengpei Xu and Ying Wu contributed equally to this work and should be considered as co-first authors.
References
- 1.ACOG Clinical Practice Update. Screening for Gestational and Pregestational Diabetes in Pregnancy and Postpartum. Obstet Gynecol. 2024;144(1):e20-3. [Google Scholar]
- 2.Voaklander B, Rowe S, Sanni O, Campbell S, Eurich D, Ospina MB. Prevalence of diabetes in pregnancy among Indigenous women in Australia, Canada, New Zealand, and the USA: a systematic review and meta-analysis. Lancet Glob Health. 2020;8(5):e681-98. [DOI] [PubMed] [Google Scholar]
- 3.Mantri N, Goel AD, Patel M, Baskaran P, Dutta G, Gupta MK, Yadav V, Mittal M, Shekhar S, Bhardwaj P. National and regional prevalence of gestational diabetes mellitus in India: a systematic review and Meta-analysis. BMC Public Health. 2024;24(1):527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Q, Li X, Liu X, Dong M, Xiao J, Wang J, Zhou M, Wang Y, Ning D, Ma W, et al. Association between maternal antimony exposure and risk of gestational diabetes mellitus: A birth cohort study. Chemosphere. 2020;246: 125732. [DOI] [PubMed] [Google Scholar]
- 5.Liang G, Lai M, Wang Y, Li N, Kang M, Lu J, Su Y, Fang F, Peng Y, Xu X, et al. Decreased complexity of glucose time series index associated with adverse pregnancy outcomes in gestational diabetes mellitus. Diabetes Obes Metab. 2024;26(9):3587–96. [DOI] [PubMed] [Google Scholar]
- 6.Biete M, Vasudevan S. Gestational diabetes mellitus: Impacts on fetal neurodevelopment, gut dysbiosis, and the promise of precision medicine. Front Mol Biosci. 2024;11:1420664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsakiridis I, Giouleka S, Mamopoulos A, Kourtis A, Athanasiadis A, Filopoulou D, Dagklis T. Diagnosis and Management of Gestational Diabetes Mellitus: An Overview of National and International Guidelines. Obstet Gynecol Surv. 2021;76(6):367–81. [DOI] [PubMed] [Google Scholar]
- 8.Grinberg K, Yisaschar-Mekuzas Y. Assessing Mental Health Conditions in Women with Gestational Diabetes Compared to Healthy Pregnant Women. Healthcare-Basel. 2024;12(14):1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun S, Pellowski J, Pisani C, Pandey D, Go M, Chu M, Ruan J, Werner EF. Experiences of stigma, psychological distress, and facilitative coping among pregnant people with gestational diabetes mellitus. Pregnancy Childb. 2023;23(1):643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fiske E. Self-transcendence theory and contemplative practices. Holistic Nursing Practice. 2019;33(5):266–72. [DOI] [PubMed] [Google Scholar]
- 11.Liu Z. The effect of hospice care on the quality of life and psychological status of patients with advanced cancer. Renowned Doctor. 2021;6:157–8. [Google Scholar]
- 12.Stison CK. Structured group reminiscence:an intervention forolder adults. J Contin Educ Nurs. 2009;40(11):521–8. [DOI] [PubMed] [Google Scholar]
- 13.Bormann JE, Thorp SR, Wetherell IL, et al. Meditation-based mantram intervention for veterans with posttraumatic stress disorder: a randomized trial. Psychol Trauma. 2013;5(3):259–67. [Google Scholar]
- 14.Yong J, Park J, Kim J, et al. The effects of holy name meditation on spiritual well-being, depression and anxiety of patients with cancer. J Hosp Palliat Nurs. 2018;20(4):386–376. [DOI] [PubMed] [Google Scholar]
- 15.REED. Self-transcendence: from moving spintual disequilibrium to well-being across the cancer trajectory. Semin Oncol Nurs. 2021;37(5):151212. [DOI] [PubMed] [Google Scholar]
- 16.Luo J, Li F, Zheng L, Fu X. Continuity of care model in the application of gestational diabetes postpartum care. J Nurs Pract Res. 2022;8:1202–5. [Google Scholar]
- 17.Zou Y, Wei L, Zhang Y, et al. Nursing intervention based on transtheoretical model of change for pregnant women at high risk of gestational diabetes mellitus. J Nurs Sci. 2022;37(04):20–3. [Google Scholar]
- 18.Liu Y, Zhang Y. Effect of online platform and pregnant women’s school on quality of pregnancy care in patients with gestational diabetes mellitus. Clin Med Res Pract. 2022;7(10):154–7+184. [Google Scholar]
- 19.Chen JX, Cai HM, Weng Y, et al. Application of evidence-based nursing practice in improving blood glucose management and pregnancy outcome in pregnant women with gestational diabetes mellitus. Chin J Med Res. 2022;20(9):74–7. [Google Scholar]
- 20.Sartayeva A, Danyarova L, Begalina D, et al. Gestational diabetes: prevalence and risks for the mother and child(review). Georgian Med News. 2022;328–329:47–52. [PubMed] [Google Scholar]
- 21.Da Q, Wang YQ, Xa JQ, et al. Bibliometric analysis of epidemiological research papers on gestationaldiabetes mellitu in China from 1996 to 2018. Chin J Woman Child Health Res. 2019;10(3):67–70. [Google Scholar]
- 22.Juan J, Yang H. Prevalence, Prevention, and Lifestyle Intervention of Gestational Diabetes lMellitus in China. Int J Environ Res Public Health. 2020;17(24):9517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang JW, Zhang LW, Xie WT, etal. Effects of dietary and exercise management on the incidence of gestational diabetes mellitus in obese or overweight women before pregnancy: a Meta-analysis. Proceedings of the 12th National Conference on Sports Science, 2022:331–333.
- 24.Zhu YQ, Fan LY, Zhou Y. Application of remote motivational interview in continuous care of obstetric patients with type 2 diabetes mellitus. Qilu J Nur. 2022;28(6):152–5. [Google Scholar]
- 25.Zhuang XY, Zhuang ZK, Huang RL. The relationship between lipid metabolism and blood glucose and cytokine levels in gestational diabetes mellitus. Chin J Math Med. 2022;35(3):373–5. [Google Scholar]
- 26.Yan MG, Wang J, Liu YM. Observation on the effect of group health care model during pregnancy in childbirth outcome of pregnantwomen with gestational diabetes. Chin J Nurs. 2021;56(09):1305–11. [Google Scholar]
- 27.Chen YY, Xie J, Lang XE. Impaet of nursing intervention based on information-motivation-behavioral skills model onmaternal-infantdelivery outcomesinpatients with gestational diabetes mellitus. J Pract Med. 2022;38(14):1731–5. [Google Scholar]
- 28.Ma XF, Zhong C, Li W. Application of ADOP’T mode nursing intervention in patients with gestational diabetes mellitus. J Nurs Sci. 2020;35(18):29–32. [Google Scholar]
- 29.Zhao AH, Zhao J. Relationship between disease uncertainty and social support, coping style inpregnant women with gestational diabetes mellitus. China J Health Psychol. 2021;29(09):1319–22. [Google Scholar]
- 30.Lv SJ. Effect of systematic nursing on blood glucose in pregnant women with gestational diabetes mellitus. China Urban and Rural Enterprise Health. 2022;37(3):205–7. [Google Scholar]
- 31.Ren MJ, Liang WL. Application of early nursing intervention in patients with gestational diabetes mellitus. China Urban and Rural Enterprise Health. 2022;37(3):220–2. [Google Scholar]
- 32.Syed HR, Adamu AA, Emenyeonn CO, et al. The Influences of Political Values Manifested in Advertisements on Political Participation: Moderating Roles of Self-transcendence and Conservation. J Creat Commun. 2020;15(3):318–41. [Google Scholar]
- 33.Ren YL, Yan MG, Zhang HJ. The impact of online cognitive-behavioral therapy on negative emotions of women with gestational diabetes mellitus. J Nurs Sci. 2021;36(10):10–3. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.