Abstract
Background
Mechanical thrombectomy (MT) is an established therapy for acute ischemic stroke (AIS), but recanalization is not always achieved. Common reasons are inadequate removal at the thrombus site and difficulties with the access route. In order to identify risk factors for MT failure we conducted a retrospective study on a high-volume comprehensive stroke center.
Methods
Evaluation of 552 thrombectomies (2019-23; anterior and posterior circulation, direct aspiration +/- stent retriever [SR]). MT failures (= modified Thrombolysis in Cerebral Infarction score 0 or 1) were analyzed for age, sex, pre- and post-MT modified Rankin Scale, bridging intravenous thrombolysis (IVT), occlusion site (anterior / posterior circulation, proximal / distal), the Kaesmacher classification and time trend results.
Results
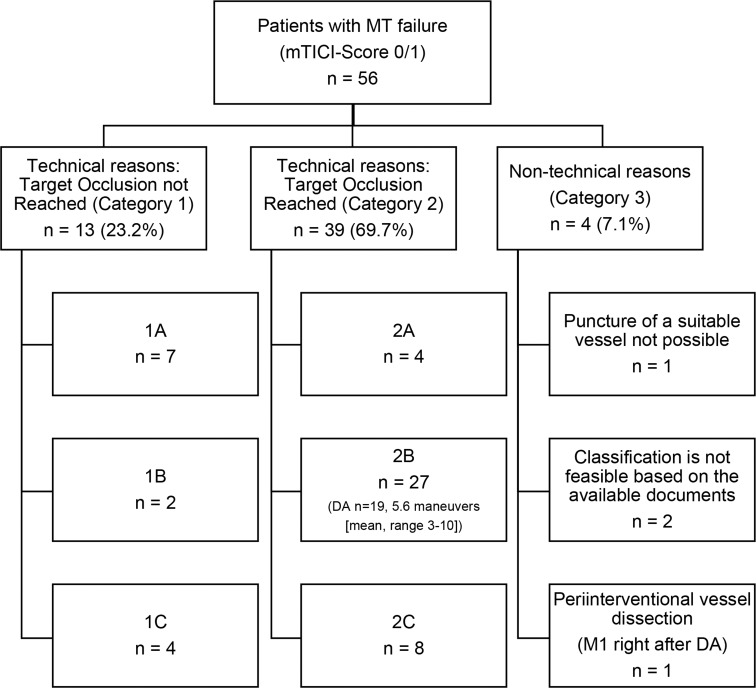
MT failure occurred in 56 patients (10.1%; median age 76; 53.6% female). Nineteen (33.9%) patients received IVT (p = 0.326). Logistic regression analysis did not show a significant association of age, sex or occlusion site with MT failure (p = 0.165, p = 0.738, p = 0.838). Distal MT generally demonstrated lower success rates (p < 0.01). According to the Kaesmacher classification SR failure was the most frequent cause of MT failure (category 2B: 48%, p < 0.001). Time trend analysis suggests improving recanalization rates in the further course (4 times in year-on-year comparison; p < 0.01).
Conclusion
MT failure occurs in AIS treatment, even in high-volume centers and occurs more frequently in distal occlusions. Improvements in device technology, particularly SR, and ongoing refinements in access route selection offer the prospect of better outcomes in the future.
Keywords: Stroke, Large vessel occlusion, Distal medium vessel occlusion, Mechanical thrombectomy failure, Direct aspiration, Stent retriever
Background
In acute ischemic stroke (AIS), mechanical thrombectomy (MT) using aspiration techniques in combination with stent retrievers is established for recanalization of large vessel occlusions (LVO) in both the anterior and posterior circulation [1–6]. The frequency of MT is increasing overall, particularly with regard to the recent positive randomized controlled trial results even in large infarct cores and later time windows [7–11]. In addition, the age range for this endovascular procedure has grown in recent years, with the additional and primarily self-evident inclusion of children and adolescents as well as old and very old patients despite recommended careful selection of them [12, 13]. The spectrum is also extended by increasing evidence for MT of distal arteries [14–17]. MT failure (= modified Thrombolysis in Cerebral Infarction score [mTICI] 0 or 1 respectively 0-2a) is generally a known caveat in the treatment of AIS and has already been reported in several studies with frequencies between 10.6 and 26.1% [18, 19, 20–26; Table 1]. Common reasons for MT failure are a missing device breakdown during the thrombus removal itself and inadequate cervical or intracranial access routes [19, 23, 25, 27]. These findings raise the question of more individualized planning and implementation of interventional stroke therapy to avoid MT failure, especially with a focus more on the specific thrombus optimized devices and potential bailout strategies to control anatomical problems [28–30]. While taking this into account, Kaesmacher et al. developed a classification for MT failure in particular with stent retrievers considering non-technical or technical reasons [19; Table 2].
Table 1.
| Authors, year of publication |
Number of patients | Study design | Study period | MT failure definition (mTICI) | MT failure rate | Technique | Anterior circulation | Posterior circulation | Inclusion of distal vessel occlusions (up to) |
|---|---|---|---|---|---|---|---|---|---|
| Our study | 552 | Single center | 2019–2023 | 0/1 | 10.1% | DA + SR | + | + | M3, P2 |
| Lajthia et al., 2023 | 1010 | Single center | 2013–2021 | 0-2a | 11.9% | DA + SR | + | + | M4 |
|
Marnat et al., 2022 |
5076 | Multicenter (n = 8) | 2015–2020 | 0-2a | 12.4% | DA + SR | + | - | no |
| Flottmann et al., 2021 | 2211 | Multicenter (n = 25) | 2015–2028 | 0-2a | 16.8% | DA + SR | + | - | no |
|
Weyland et al., 2021 |
218 | Single center | 2009–2019 | 0/1 | 13.8% | DA + SR | - | + | no |
|
Heider et al., 2020 |
596 | Single center | 2014–2018 | 0-2a | 16.8% | DA + SR | + | - | no |
|
Goda et al., 2019 |
119 | Single center | 2015–2019 | 0-2a | 26.1% | DA + SR | + | - | M3 |
| Leischner et al., 2019 | 648 | Single center | 2010–2017 | 0/1 | 11.0% | DA + SR | + | - | no |
| Kaesmacher et al., 2018 | 592 | Single center | 2012–2017 | 0/1 | 10.6% | SR | + | + | no |
|
Gascou et al., 2014 |
144 | Single center | 2009–2011 | 0-2a | 13.9% | SR | + | + | n.a. |
Legend: DA - direct aspiration, MT– mechanical thrombectomy, mTICI - modified thrombolysis in cerebral infarction scale, n.a. - not applicable, SR - stent retriever
Table 2.
Known classification of mechanical thrombectomy failure reasons as published by Kaesmacher et al. [19]. The changes we have added are highlighted in italics
| Category | Classification system for mechanical thrombectomy failure |
|---|---|
| 1 |
Technical reasons: Target occlusion not reached 1 A: Intracranial target occlusion was not reached due to marked cervical vessel tortuosity including twisted, looped, or kinked vessels. The proximal cervical vessels were successfully catheterized. 1B: Target occlusion was not reached owing to failed catheterization of proximal supra-aortic vessels. The proximal cervical vessels were not successfully catheterized owing to difficult aortic arch anatomy. 1 C: Target occlusion was not reached due to the inability to pass a cervical ICA occlusion (e.g. unpassable tandem lesion). |
| 2 |
Technical reasons: Target occlusion reached 2 A: Target occlusion was reached, but the operator was unable to pass the thrombus with the microwire/microcatheter. In these cases, no stent retriever was deployed. 2B: Target occlusion was reached, the stent retriever was deployed, but no reperfusion occurred after multiple retrievals (no clot retrieval or dislocation), thus, stent retriever failure. 2 C: Initial reperfusion was achieved, followed by spontaneous or iatrogenic reocclusion (e.g. intracranial stenosis, intracranial dissection, or perforation with subsequent vessel sacrifice). |
| 3 |
Non-technical reasons Presumed futility. Adverse non-neurological event with the need to stop mechanical thrombectomy. Signs of contrast extravasation without perforation (early hemorrhagic transformation). Puncture of a suitable vessel for access route not possible. Periinterventional arterial dissection. Classification is not feasible based on the available documents. |
Legend: ICA - internal carotid artery
Given the urgency of more detailed understanding of MT failure, our large retrospective single center study from a German university hospital aims to comprehensively analyze demographic characteristics (age, sex, pre- and post-MT modified Rankin Scale [mRS] values, bridging intravenous thrombolysis [IVT] with plasminogen activator) and vessel occlusion site (anterior vs. posterior circulation respectively proximal vs. distal segments) as well as other risk factors for MT failure according to the classification of Kaesmacher et al. In addition, we carried out an analysis of MT failure over time.
Methods
Study design
In a retrospective analysis we evaluated 552 patients in total who underwent MT due to AIS in the anterior or posterior cerebral circulation between August 2019 and March 2023 in our high-volume comprehensive stroke center of a German university hospital. Our standard MT approach was as follows: After induction of general anesthesia, a long 6 french (F) sheath is placed in the internal carotid artery (ICA) or vertebral artery via femoral access with a 5 F guide catheter. An appropriately sized aspiration catheter is placed at the face of the thrombus in a triaxial approach and two attempts of direct aspiration are performed. If recanalization was unsuccessful, the decision to employ an additional stent retrieval technique, repeat the aspiration maneuver or to end the interventional procedure was made by the neuro-interventionalist.
Mechanical thrombectomy failure was defined as mTICI score of 0 or 1.
Patients with MT failure were analyzed for demographic characteristics age, sex, mRS values at admission (pre-MT) and at discharge from hospital (post-MT), bridging IVT and site of vessel occlusion (anterior vs. posterior circulation, proximal ICA, M1, M2, A1, A2, basilar artery [BA], P1 vs. distal [A3, M3, P2] segments) as well as reasons for MT failure according to the classification of Kaesmacher et al. [15, 19]. In addition, we analyzed MT failure of patients over time.
All angiographic results were evaluated by two experienced neuro-interventionalists with board certification.
Approval of our institutional review board was obtained, whereby research ethics and informed consent were considered (file reference: 2023 − 662).
Statistics
Statistical analyses were performed using R (version 4.3.1). Pearson’s Chi-square tests (parametric) were employed for categorical variables, logistic regression (parametric) for binary outcomes and Wilcoxon rank-sum and signed-rank tests (non-parametric) for ordinal data. Fisher’s exact test (non-parametric) was used for categorical data and ordinal logistic regression (parametric) for ordered categorical outcomes. The alpha level was set at 0.05, with p-values less than this threshold considered statistically significant.
Results
All vessel occlusions and mechanical thrombectomies
In all 552 patients receiving MT, 469 vessel occlusions (85%) occurred in the anterior circulation and 73 (13.2%) in the posterior circulation. The 10 remaining cases (1.8%) constituted combined occlusions in different territories, whereby two vessel segments alone were affected at the same time (each without simultaneous MT). The occlusion leading to thrombectomy was found in a proximal vessel segment in 527 cases (95.5%) and in a distal vessel segment in 25 cases (4.5%; A3 n = 1 [left], M3 n = 9 [8 left, 1 right], P2 n = 15 [9 left, 6 right]). 496/552 patients (89.9%) showed successful MT after use of direct aspiration and/or stent retriever, with n = 29 (5.8%) undergoing intracranial rescue stenting.
Mechanical thrombectomy failure patients
Demographic characteristics and site of vessel occlusion (anterior vs. posterior circulation, proximal vs. distal segments)
Mechanical thrombectomy failure occurred in 56 patients (10.1%; n = 47 anterior circulation, n = 9 posterior circulation). In these cases, 49 patients (87.5%) finally showed mTICI 0, while in 7 patients (12.5%) MT resulted in mTICI 1. There was no case with rescue stenting that resulted in MT failure. The median age of the patients with an unsuccessful MT was 76 (interquartile range: 69.75-82). Thirty patients (53.6%) with MT failure were female and n = 26 male (46.4%). The distribution of mRS values at admission for patients with MT failure showed a median of 4 (range 1–5), whereas the median at discharge from hospital was 5 (range 2–6). Nineteen patients (33.9%) with MT failure received bridging IVT, while n = 37 (66.1%) did not. There were 48 cases of failed thrombectomies in proximal (85.7%) and 8 (14.3%) in distal vessel occlusions, with M2 branch being the most frequent location of MT failure. Site distribution of MT failure in detail is presented in Table 3.
Table 3.
Site distribution of mechanical thrombectomy failure
| Vessel occlusion | Left (n) | Right (n) |
|---|---|---|
| ICA | 6 | 4 |
| M1 | 7 | 4 |
| M2 | 9 | 8 |
| M3 | 3 | 0 |
| A1 | 1 | 0 |
| A2 | 1 | 3 |
| A3 | 1 | 0 |
| BA | 1 | |
| P1 | 3 | 2 |
| P2 | 1 | 2 |
Legend: BA - basilar artery, ICA - internal carotid artery, mTICI - modified thrombolysis in cerebral infarction scale
Review of MT failure, according to the Kaesmacher classification, shows that stent retriever failure was the most frequent cause in our study cohort (category 2B: 27/56 patients [48%]). The detailed distribution is listed in Table 4.
Table 4.
Mechanical thrombectomy failure reasons in our study using the classification system of Kaesmacher et al. as supplemented by us [19]
Specific statistical analyses including the classification of Kaesmacher et al. and trend over time
A logistic regression analysis showed a statistically non-significant trend towards a negative association of age with MT failure (p = 0.165). We found no significant association between sex and unsuccessful endovascular recanalization (p = 0.738). Bridging IVT was not significantly associated with successful MT (p = 0.326). An improvement in the clinical outcome on the basis of pre- and post-MT mRS was significantly associated with thrombectomy success (TICI ≥ 2a; p < 0.001). There was also no correlation of vessel occlusion localization in the anterior or posterior circulation on angiographic reperfusion after MT (p = 0.838). However, distal vessel occlusions (A3, M3, P2) generally demonstrated lower MT success rates than proximal occlusions (ICA, M1, M2, A1, A2, VA, BA, P1) (p < 0.01).
Our review of MT failure in detail, according to the Kaesmacher classification, showed that stent retriever failure was the most frequent cause (category 2a: 48%, p < 0.001). Furthermore, demographic factors such as age or sex showed no correlation across different failure types (p = 0.610, p = 0.805). Concerning the success rates of MT in different calendar years, the results indicated significant differences between 2020 (MT failure n = 22) and 2022 (n = 8, p < 0.01), 2020 (n = 22) and 2023 (n = 0, p < 0.01), 2021 (n = 23) and 2022 (n = 8, p < 0.01) as well as 2021 (n = 23) and 2023 (n = 8, p < 0.01; Fig. 1). Comparisons between other years did not yield statistically significant findings (p > 0.05).
Fig. 1.
Mechanical thrombectomy failure over time in our study. Legend: MT - mechanical thrombectomy
Discussion
Our aim was to analyze patients with MT failure. Considering this ongoing and dynamic issue, we present results from a large single center study conducted in a high-volume comprehensive center of a German university hospital, including both anterior and posterior circulation strokes. Mechanical thrombectomy failure patients were analyzed for baseline characteristics (age, sex, clinical conditions, bridging IVT) as well as vessel occlusion localization (anterior vs. posterior circulation, proximal [ICA, M1, M2, A1, A2, VA, BA, P1] vs. distal [A3, M3, P2] segments) and other reasons for MT failure according to the classification of Kaesmacher et al. In addition, we carried out an analysis of MT failure over time.
Unsuccessful endovascular recanalization is a well-recognized challenge in the treatment of acute ischemic stroke, with prior studies reporting failure rates ranging from 10.6 to 26.1%, based on the mTICI score [18–26]. Overall, our MT success rate is in line with the results of other work groups, although MT failure was not consistently defined across studies (mTICI 0/1 vs. 0-2a), making comparisons difficult in some cases (18, 19, 20–26; Table 1).
Our logistic regression analysis showed a trend towards a negative association of age with MT failure (p = 0.165) and we found no significant association between sex and unsuccessful endovascular recanalization (p = 0.738). Different from this finding, Goda et al. identified female sex as a predictor of MT failure [18]. Furthermore, in our results, bridging IVT was not significantly associated with MT success (p = 0.326), partly arguing against recent results from the SWIFT DIRECT trial that supported IVT additionally to MT for AIS treatment [31]. However, our data did not result from a randomized trial. Therefore, there is a clear selection bias between both groups that might influence results.
Our study further enhances understanding of MT results across different vascular territories. Several studies have already dealt with this; we refer to a meta-analysis of Adusumilli presenting comparable mechanical recanalization rates in anterior and posterior circulation [32]. Also, our results did not show a correlation of site of vessel occlusion in the different circulations on angiographic reperfusion after MT (p = 0.838). The lack of significant differences between the territories suggests that thrombus location does not compromise MT success, which is in a way in line with results of registry data [33].
We also compared the proximal and distal distribution in relation to thrombectomy success. In our study, the exploration of MT outcomes by the location of occlusion reveals that thrombectomy targeting distal vessels (in our cases A3, M3 and P2) have significantly lower recanalization rates compared to proximal thrombus locations (p < 0.01). In contrast, a systematic review indicates satisfactory MT outcomes for more distal cerebral arteries [34]. Nevertheless, the difference revealed in our study obviously confirms that distal occlusions of small vessels are more challenging, potentially due to increased tortuosity, resulting in less accessibility for MT devices, which may be more difficult to navigate, therefore increasing the complexity of the endovascular procedure. In the case of distal emboli, we see a higher number of left-brain findings in our results (18 of 25 cases). In this context, the literature predominantly describes more effective MT outcomes for LVO associated with left cerebral ischemia [35].
While previous work such as that by Heider et al. has already examined mechanisms and co-factors of MT failure in detail, we would also like to add new aspects to the topic [24]. The additional classification by Kaesmacher et al., which distinguishes between technical and non-technical reasons for MT failure, offers valuable insights into the factors contributing to MT outcomes [19]. We have also used this classification in our collective for patients treated with direct aspiration in connection with AIS. Our review of factors associated with unsuccessful thrombectomies according to the proposal of Kaesmacher et al. shows that stent retriever failure, despite correct positioning and potentially multiple retrieval attempts, is the primary cause (category 2B: 27/56 patients [48%]) and this demonstrated significant differences to the other categories (p < 0.001). Notably, our findings indicate a higher failure rate than reported by Kaesmacher et al., who noted stent retriever failure in 39.7% of their 63 patients [17]. This highlights the need for even greater emphasis on further development of stent retrievers, with a focus more on the specific thrombus optimized devices [30]. However, this kind of MT failure directly at the occlusion may be influenced by challenging vascular anatomy, such as tight curves or extensive atherosclerosis, which complicates the retrieval process itself [28, 30]. Furthermore, especially for the patients classified by us according to Kaesmacher et al., the demographic factors age and sex showed no correlation across different failure types (p = 0.610, p = 0.805). This suggests that they may influence overall stroke outcomes, but not directly impact MT success.
Lastly and as a further new aspect for literature, our time trend results suggest improving MT success rates in the further course. This is particularly noteworthy in the period from 2021 to 2023, with not a single failure documented in the last year in 43 MT patients examined (Fig. 4). It is worth mentioning that a relatively long period of time (almost 4 years) is included in this study, in which the development of new tools has likely played a role in decreasing the number of MT failures over time. The observed improvements in endovascular recanalization rates may be attributed in part to the increased use of thrombectomy especially for distal vessel occlusions with enhanced knowledge of material handling. As neuro-interventionalists become more familiar with the techniques of navigating and using these technologically advanced devices, they are able to perform MT more successfully and with better outcomes [36]. Especially for distal occlusions, therefore, advancements in devices, particularly stent retrievers, are crucial in shaping the future of MT [37]. Temporal trends in thrombectomy success have so far only been systematically investigated for LVO [38].
In general, additive MT procedures through other access routes (radial or direct ICA puncture) present a promising approach as an alternative strategy in cases of initial procedural failure via femoral artery access and certainly require further investigation [39–41]. Additionally, the utilization of simulators capable of replicating intricate anatomical scenarios could provide valuable training opportunities [42]. Furthermore, recent studies have shown that the use of intra-arterial tissue-type plasminogen activators after unsuccessful MT did not result in a higher risk of symptomatic intracranial hemorrhage or mortality, making it a low-risk bailout procedure [43, 44].
Limitations
This study’s retrospective design with single-center focus, different vessel occlusion durations especially due to “drip- and-ship”, use of varying procedural techniques for MT with changing experience levels of the neuro-interventionalists (learning curves) and lack of longer-term follow-up data limits its generalizability and introduces potential biases. As retrospective studies carry inherent limitations, more prospective studies on this topic are crucial.
The mTICI score was not originally intended for the description of therapy results of the posterior circulation, but is also widely used for this purpose [16]. In addition, there are different definitions for distal vessel occlusions and also overlaps with Medium Vessel Occlusions (MeVO), and we have referred to the descriptions of the multicenter initiative Stroke Thrombectomy and Aneurysm Registry (STAR) [15, 45, 46]. In the retrospective approach applied here, the exact reason for a persistent vessel occlusion after MT and possibly the lack of a change in interventional strategy with consideration of rescue stenting, among others, could not be clearly traced, although there are also novel developments in this area in particular [47–50]. Furthermore, in future the goal should be to better assess the additive effect of bridging IVT depending on localization of the vessel occlusion to be mechanically recanalized and achieve a better understanding of predictors for MT failure, particularly in very old patients [51, 52].
Beyond that, with regard to outcome, predictive clinical and radiological parameters [53] as well as other influences such as anticoagulation [54], tandem occlusions with simultaneous emergent ICA stenting [55], collaterals [56] and secondary intracerebral hemorrhages [57, 58] have not been analyzed by us. However, these will certainly also be the subject of future research. In addition, the question of whether the duration of the interventional procedure and the number of thrombectomy maneuvers have a decisive influence on the outcome in the case of unsuccessful endovascular recanalization was also discussed very recently, which was not considered in our survey [59].
Funding
None
Open Access funding enabled and organized by Projekt DEAL.
Data availability
The data that support the findings of this study are available from the authors Alexander Neumann and Paul Schildhauer, upon reasonable request.
Declarations
Ethical approval
Our study has been reviewed by the appropriate ethics committee (University of Lübeck, file reference: 2023 − 662) and has therefore been performed in accordance with the ethical standards laid down in an appropriate version of the 1965 Declaration of Helsinki.
Consent for publication
All authors consent to the publication of this manuscript.
Competing interests
HS: Lecture fee from Cercare Medical. GR: Compensation from Cardinal Health 200 LLC for consultant services; compensation from Novartis Pharma AG for other services; compensation from AstraZeneca for consultant services; travel support from Boehringer Ingelheim; compensation from Boehringer Ingelheim for consultant services; compensation from Ipsen Pharma SAS for consultant services; and compensation from Bristol-Myers Squibb for consultant services. UJK: Payment for attending a training course from Cerenovus. AN, PS, SMW, PS: None.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Munoz A, Jabre R, Orenday-Barraza JM, Eldin MS, Chen CJ, Al-Saiegh F, Abbas R, El Naamani K, Gooch MR, Jabbour PM, Tjoumakaris S, Rosenwasser RH, Herial NA (2023) A review of mechanical thrombectomy techniques for acute ischemic stroke. Interv Neuroradiol 29(4):450–458 Epub 2022 Mar 3. PMID: 35238227; PMCID: PMC10399505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tao C, Nogueira RG, Zhu Y, Sun J, Han H, Yuan G, Wen C, Zhou P, Chen W, Zeng G, Li Y, Ma Z, Yu C, Su J, Zhou Z, Chen Z, Liao G, Sun Y, Ren Y, Zhang H, Chen J, Yue X, Xiao G, Wang L, Liu R, Liu W, Liu Y, Wang L, Zhang C, Liu T, Song J, Li R, Xu P, Yin Y, Wang G, Baxter B, Qureshi AI, Liu X, Hu W (2022) ATTENTION Investigators. Trial of Endovascular Treatment of Acute Basilar-Artery Occlusion. N Engl J Med.;387(15):1361–1372. 10.1056/NEJMoa2206317. PMID: 36239644 [DOI] [PubMed]
- 3.Zhang Y, Zhang Y, Hu C, Zhao W, Zhang Z, Li W (2021) A direct aspiration first-pass technique (ADAPT) versus stent retriever for acute ischemic stroke (AIS): a systematic review and meta-analysis. J Neurol 268(12):4594–4606. 10.1007/s00415-020-10284-wEpub 2020 Oct 29. PMID: 33123777 [DOI] [PubMed] [Google Scholar]
- 4.Roaldsen MB, Jusufovic M, Berge E, Lindekleiv H (2021) Endovascular thrombectomy and intra-arterial interventions for acute ischaemic stroke. Cochrane Database Syst Rev 6(6):CD007574. 10.1002/14651858.CD007574.pub3PMID: 34125952; PMCID: PMC8203212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL (2019) Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke.;50(12):e344-e418. doi: 10.1161/STR.0000000000000211. Epub 2019 Oct 30. Erratum in: Stroke. 2019;50(12):e440-e441. PMID: 31662037
- 6.Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, Schellinger PD, Toni D, de Vries J, White P, Fiehler J (2019) European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in Acute Ischaemic StrokeEndorsed by Stroke Alliance for Europe (SAFE). Eur Stroke J 4(1):6–12 Epub 2019 Feb 26. PMID: 31165090; PMCID: PMC6533858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costalat V, Jovin TG, Albucher JF, Cognard C, Henon H, Nouri N, Gory B, Richard S, Marnat G, Sibon I, Di Maria F, Annan M, Boulouis G, Cardona P, Obadia M, Piotin M, Bourcier R, Guillon B, Godard S, Pasco-Papon A, Eker OF, Cho TH, Turc G, Naggara O, Velasco S, Lamy M, Clarençon F, Alamowitch S, Renu A, Suissa L, Brunel H, Gentric JC, Timsit S, Lamy C, Chivot C, Macian-Montoro F, Mounayer C, Ozkul-Wermester O, Papagiannaki C, Wolff V, Pop R, Ferrier A, Chabert E, Ricolfi F, Béjot Y, Lopez-Cancio E, Vega P, Spelle L, Denier C, Millán M, Arenillas JF, Mazighi M, Houdart E (2024) Mar Freijo M, Duhamel A, Sanossian N, Liebeskind DS, Labreuche J, Lapergue B, Arquizan C; LASTE Trial Investigators. Trial of Thrombectomy for Stroke with a Large Infarct of Unrestricted Size. N Engl J Med.;390(18):1677–1689. 10.1056/NEJMoa2314063. PMID: 38718358
- 8.Winkelmeier L, Maros M, Flottmann F, Heitkamp C, Schön G, Thomalla G, Fiehler J, Hanning U (2024) Endovascular Thrombectomy for Large Ischemic Strokes with ASPECTS 0–2: a Meta-analysis of Randomized Controlled Trials. Clin Neuroradiol. Apr 30. 10.1007/s00062-024-01414-2. Epub ahead of print. PMID: 38687364 [DOI] [PMC free article] [PubMed]
- 9.Khunte M, Chen H, Khunte A, Payabvash S, Gandhi D, Malhotra A (2023) Trends in Use of Intravenous Thrombolysis and Endovascular Thrombectomy in patients with Acute Stroke with large vessel occlusion 2016 to 2020 and impact of COVID-19 pandemic. J Am Heart Assoc 12(21):e029579 Epub 2023 Oct 27. PMID: 37889182; PMCID: PMC10727381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez-Calienes A, Galecio-Castillo M, Vivanco-Suarez J, Mohamed GA, Toth G, Sarraj A, Pujara D, Chowdhury AA, Farooqui M, Ghannam M, Samaniego EA, Jovin TG, Ortega-Gutierrez S Endovascular thrombectomy beyond 24 hours from last known well: a systematic review with meta-analysis. J Neurointerv Surg 2023 Jun 24:jnis–2023. 10.1136/jnis-2023-020443. Epub ahead of print. PMID: 37355251. [DOI] [PubMed]
- 11.Li L, Scott CA, Rothwell PM (2020) Oxford Vascular Study. Trends in Stroke incidence in high-income countries in the 21st Century: Population-based study and systematic review. Stroke 51(5):1372–1380. 10.1161/STROKEAHA.119.028484Epub 2020 Mar 25. PMID: 32208842; PMCID: PMC7185053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bai X, Zhang X, Zhang Y, Yang W, Wang T, Feng Y, Wang Y, Yang K, Wang X, Ma Y, Jiao L (2021) Mechanical thrombectomy in nonagenarians: a systematic review and Meta-analysis. Transl Stroke Res 12(3):394–405 Epub 2021 Feb 2. PMID: 33532934 [DOI] [PubMed] [Google Scholar]
- 13.Sporns PB, Sträter R, Minnerup J, Wiendl H, Hanning U, Chapot R, Henkes H, Henkes E, Grams A, Dorn F, Nikoubashman O, Wiesmann M, Bier G, Weber A, Broocks G, Fiehler J, Brehm A, Psychogios M, Kaiser D, Yilmaz U, Morotti A, Marik W, Nolz R, Jensen-Kondering U, Schmitz B, Schob S, Beuing O, Götz F, Trenkler J, Turowski B, Möhlenbruch M, Wendl C, Schramm P, Musolino P, Lee S, Schlamann M, Radbruch A, Rübsamen N, Karch A, Heindel W, Wildgruber M, Kemmling A (2020) Feasibility, Safety, and Outcome of Endovascular recanalization in Childhood Stroke: the Save ChildS Study. JAMA Neurol 77(1):25–34. 10.1001/jamaneurol.2019.3403PMID: 31609380; PMCID: PMC6802048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clarençon F, Durand-Zaleski I, Premat K, Baptiste A, Chabert E, Ferrier A, Labeyrie MA, Reiner P, Spelle L, Denier C, Tuilier T, Hosseini H, Rodriguez-Régent C, Turc G, Fauché C, Lamy M, Lapergue B, Consoli A, Barbier C, Boulanger M, Bricout N, Henon H, Gory B, Richard S, Rouchaud A, Macian-Montoro F, Eker O, Cho TH, Soize S, Moulin S, Gentric JC, Timsit S, Darcourt J, Albucher JF, Janot K, Annan M, Pico F, Costalat V, Arquizan C, Marnat G, Sibon I, Pop R, Wolff V, Shotar E, Lenck S, Sourour NA, Radenne A, Alamowitch S, Dechartres A (2024) Evaluation of mechanical thrombectomy in acute ischemic stroke related to a distal arterial occlusion: a randomized controlled trial. Int J Stroke 19(3):367–372. 10.1177/17474930231205213Epub 2023 Oct 12. PMID: 37740419 [DOI] [PubMed] [Google Scholar]
- 15.Alawieh AM, Chalhoub RM, Al Kasab S, Jabbour P, Psychogios MN, Starke RM, Arthur AS, Fargen KM, De Leacy R, Kan P, Dumont TM, Rai A, Crosa RJ, Maier I, Goyal N, Wolfe SQ, Cawley CM, Mocco J, Tjoumakaris SI, Howard BM, Dimisko L, Saad H, Ogilvy CS, Crowley RW, Mascitelli JR, Fragata I, Levitt MR, Kim JT, Park MS, Gory B, Polifka AJ, Matouk C, Grossberg JA, Spiotta AM (2023) STAR Collaborators. Multicenter investigation of technical and clinical outcomes after thrombectomy for distal vessel occlusion by frontline technique. J Neurointerv Surg 15(e1):e93–e101. 10.1136/jnis-2022-019023Epub 2022 Aug 2. PMID: 35918129 [DOI] [PubMed] [Google Scholar]
- 16.Meyer L, Stracke CP, Jungi N, Wallocha M, Broocks G, Sporns PB, Maegerlein C, Dorn F, Zimmermann H, Naziri W, Abdullayev N, Kabbasch C, Behme D, Jamous A, Maus V, Fischer S, Möhlenbruch M, Weyland CS, Langner S, Meila D, Miszczuk M, Siebert E, Lowens S, Krause LU, Yeo LLL, Tan BY, Anil G, Gory B, Galván J, Arteaga MS, Navia P, Raz E, Shapiro M, Arnberg F, Zelenák K, Martinez-Galdamez M, Fischer U, Kastrup A, Roth C, Papanagiotou P, Kemmling A, Gralla J, Psychogios MN, Andersson T, Chapot R, Fiehler J, Kaesmacher J, Hanning U (2021) Thrombectomy for primary distal posterior cerebral artery occlusion stroke: the TOPMOST study. JAMA Neurol 78(4):434–444. 10.1001/jamaneurol.2021.0001PMID: 33616642; PMCID: PMC7900924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, Lobotesis K, Meila D, Meyer L, Raphaeli G, Gupta R (2020) Distal Thrombectomy Summit Group*†. Thrombectomy for Distal, Medium Vessel Occlusions: A Consensus Statement on Present Knowledge and Promising Directions. Stroke.;51(9):2872–2884. 10.1161/STROKEAHA.120.028956. Epub 2020 Aug 6. Erratum in: Stroke. 2020;51(10):e296. PMID: 32757757 [DOI] [PubMed]
- 18.Goda T, Oyama N, Kitano T, Iwamoto T, Yamashita S, Takai H, Matsubara S, Uno M, Yagita Y (2019) Factors Associated with unsuccessful recanalization in mechanical thrombectomy for Acute ischemic stroke. Cerebrovasc Dis Extra 9(3):107–113 Epub 2019 Sep 27. PMID: 31563915; PMCID: PMC6792430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaesmacher J, Gralla J, Mosimann PJ, Zibold F, Heldner MR, Piechowiak E, Dobrocky T, Arnold M, Fischer U, Mordasini P (2018) Reasons for reperfusion failures in Stent-Retriever-based thrombectomy: Registry analysis and proposal of a classification system. AJNR Am J Neuroradiol 39(10):1848–1853. 10.3174/ajnr.A5759Epub 2018 Aug 30. PMID: 30166434; PMCID: PMC7410746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, Marks MP, Prabhakaran S, Kallmes DF, Fitzsimmons BF, Mocco J, Wardlaw JM, Barnwell SL, Jovin TG, Linfante I, Siddiqui AH, Alexander MJ, Hirsch JA, Wintermark M, Albers G, Woo HH, Heck DV, Lev M, Aviv R, Hacke W, Warach S, Broderick J, Derdeyn CP, Furlan A, Nogueira RG, Yavagal DR, Goyal M, Demchuk AM, Bendszus M, Liebeskind DS; Cerebral Angiographic Revascularization Grading (CARG) Collaborators; STIR Revascularization working group; STIR Thrombolysis in Cerebral Infarction (TICI) Task Force. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke.;44(9):2650-63. doi:, Almallouhi O, Ali E, Essibayi H, Bass MA, Neyens E, Anadani R, Chalhoub M, Kicielinski R, Lena K, Porto J, Sattur G, Spiotta M, Kasab AM (2013) SA. Failed mechanical thrombectomy: prevalence, etiology, and predictors. J Neurosurg. 2023;139(3):714–720. doi: 10.3171/2022.12.JNS222152. PMID: 36670537 [DOI] [PubMed]
- 21.Marnat G, Gory B, Sibon I, Kyheng M, Labreuche J, Boulouis G, Liegey JS, Caroff J, Eugène F, Naggara O, Consoli A, Mazighi M, Maier B, Richard S, Denier C, Turc G, Lapergue B, Bourcier R (2022) Endovascular treatment in ischemic stroke (ETIS) investigators. Mechanical thrombectomy failure in anterior circulation strokes: outcomes and predictors of favorable outcome. Eur J Neurol 29(9):2701–2707. 10.1111/ene.15429Epub 2022 Jun 18. PMID: 35648445; PMCID: PMC9541042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flottmann F, Broocks G, Faizy TD, McDonough R, Watermann L, Deb-Chatterji M, Thomalla G, Herzberg M, Nolte CH, Fiehler J, Leischner H, Brekenfeld C (2021) GSR investigators. Factors Associated with failure of reperfusion in endovascular therapy for Acute ischemic stroke: a Multicenter Analysis. Clin Neuroradiol 31(1):197–205 Epub 2020 Feb 17. PMID: 32067055; PMCID: PMC7943507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weyland CS, Neuberger U, Potreck A, Pfaff JAR, Nagel S, Schönenberger S, Bendszus M, Möhlenbruch MA (2021) Reasons for failed mechanical thrombectomy in posterior circulation ischemic stroke patients. Clin Neuroradiol 31(3):745–752. 10.1007/s00062-020-00950-xEpub 2020 Sep 7. PMID: 32894352; PMCID: PMC8463404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heider DM, Simgen A, Wagenpfeil G, Dietrich P, Yilmaz U, Mühl-Benninghaus R, Roumia S, Faßbender K, Reith W, Kettner M (2020) Why we fail: mechanisms and co-factors of unsuccessful thrombectomy in acute ischemic stroke. Neurol Sci 41(6):1547–1555 Epub 2020 Jan 23. PMID: 31974796; PMCID: PMC7275938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leischner H, Flottmann F, Hanning U, Broocks G, Faizy TD, Deb-Chatterji M, Bernhardt M, Brekenfeld C, Buhk JH, Gellissen S, Thomalla G, Gerloff C, Fiehler J (2019) Reasons for failed endovascular recanalization attempts in stroke patients. J Neurointerv Surg 11(5):439–442. 10.1136/neurintsurg-2018-014060Epub 2018 Nov 24. PMID: 30472671 [DOI] [PubMed] [Google Scholar]
- 26.Penide J, Mirza M, McCarthy R, Fiehler J, Mordasini P, Delassus P, Morris L, Gilvarry M (2022) Systematic review on Endovascular Access to intracranial arteries for mechanical thrombectomy in Acute ischemic stroke. Clin Neuroradiol 32(1):5–12. 10.1007/s00062-021-01100-7Epub 2021 Oct 12. PMID: 34642788 [DOI] [PubMed] [Google Scholar]
- 27.Gascou G, Lobotesis K, Machi P, Maldonado I, Vendrell JF, Riquelme C, Eker O, Mercier G, Mourand I, Arquizan C, Bonafé A, Costalat V (2014) Stent retrievers in acute ischemic stroke: complications and failures during the perioperative period. AJNR Am J Neuroradiol 35(4):734–740. 10.3174/ajnr.A3746Epub 2013 Oct 24. PMID: 24157734; PMCID: PMC7965801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alverne FJAM, Lima FO, Rocha FA, Bandeira DA, Lucena AF, Silva HC, Lee JS, Nogueira RG (2020) Unfavorable vascular anatomy during Endovascular Treatment of Stroke: challenges and Bailout strategies. J Stroke 22(2):185–202. 10.5853/jos.2020.00227Epub 2020 May 31. PMID: 32635684; PMCID: PMC7341011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Madjidyar J, Pineda Vidal L, Larsen N, Jansen O (2020) Influence of Thrombus composition on Thrombectomy: ADAPT vs. Balloon Guide Catheter and Stent Retriever in a Flow Model. Rofo 192(3):257–263 English. 10.1055/a-0998-4246 [DOI] [PubMed] [Google Scholar]
- 30.Kim BM (2017) Causes and solutions of Endovascular Treatment failure. J Stroke 19(2):131–142. 10.5853/jos.2017.00283Epub 2017 May 31. PMID: 28592777; PMCID: PMC5466284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fischer U, Kaesmacher J, Strbian D, Eker O, Cognard C, Plattner PS, Bütikofer L, Mordasini P, Deppeler S, Pereira VM, Albucher JF, Darcourt J, Bourcier R, Benoit G, Papagiannaki C, Ozkul-Wermester O, Sibolt G, Tiainen M, Gory B, Richard S, Liman J, Ernst MS, Boulanger M, Barbier C, Mechtouff L, Zhang L, Marnat G, Sibon I, Nikoubashman O, Reich A, Consoli A, Lapergue B, Ribo M, Tomasello A, Saleme S, Macian F, Moulin S, Pagano P, Saliou G, Carrera E, Janot K, Hernández-Pérez M, Pop R, Schiava LD, Luft AR, Piotin M, Gentric JC, Pikula A, Pfeilschifter W, Arnold M, Siddiqui AH, Froehler MT, Furlan AJ, Chapot R, Wiesmann M, Machi P, Diener HC, Kulcsar Z, Bonati LH, Bassetti CL, Mazighi M, Liebeskind DS, Saver JL, Gralla J (2022) SWIFT DIRECT Collaborators. Thrombectomy alone versus intravenous alteplase plus thrombectomy in patients with stroke: an open-label, blinded-outcome, randomised non-inferiority trial. Lancet.;400(10346):104–115. 10.1016/S0140-6736(22)00537-2. PMID: 35810756 [DOI] [PubMed]
- 32.Adusumilli G, Pederson JM, Hardy N, Kallmes KM, Hutchison K, Kobeissi H, Heiferman DM, Heit JJ Mechanical thrombectomy in anterior vs. posterior circulation stroke: A systematic review and meta-analysis. Interv Neuroradiol. 2022 May 13:15910199221100796. doi: 10.1177/15910199221100796. Epub ahead of print. PMID: 35549748 [DOI] [PMC free article] [PubMed]
- 33.Feil K, Berndt MT, Wunderlich S, Maegerlein C, Bernkopf K, Zimmermann H, Herzberg M, Tiedt S, Küpper C, Wischmann J, Schönecker S, Dimitriadis K, Liebig T, Dieterich M, Zimmer C, Kellert L, Boeckh-Behrens T (2023) GSR investigators. Endovascular thrombectomy for basilar artery occlusion stroke: analysis of the German Stroke Registry-Endovascular treatment. Eur J Neurol 30(5):1293–1302. 10.1111/ene.15694Epub 2023 Feb 22. PMID: 36692229 [DOI] [PubMed] [Google Scholar]
- 34.Bilgin C, Hardy N, Hutchison K, Pederson JM, Mebane A, Olaniran P, Kobeissi H, Kallmes KM, Fiorella D, Kallmes DF, Brinjikji W (2023) First-line thrombectomy strategy for distal and medium vessel occlusions: a systematic review. J Neurointerv Surg 15(6):539–546. 10.1136/jnis-2022-019344Epub 2022 Oct 12. PMID: 36223996 [DOI] [PubMed] [Google Scholar]
- 35.Li Z, Chu Z, Zhao S, Ma L, Yang Q, Huang X, Zhou Z (2019) Severe stroke patients with left-sided occlusion of the proximal anterior circulation benefit more from Thrombectomy. Front Neurol 10:551. 10.3389/fneur.2019.00551PMID: 31191440; PMCID: PMC6546891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hulscher F, Farouki Y, Mine B, Bonnet T, Wang M, Elens S, Suarez JV, Jodaitis L, Ligot N, Naeije G, Lubicz B, Guenego A (2022) Predictors of good clinical outcome after Thrombectomy for Distal Medium Vessel occlusions. World Neurosurg 160:e566–e572 Epub 2022 Jan 22. PMID: 35077884 [DOI] [PubMed] [Google Scholar]
- 37.Guenego A, Mine B, Bonnet T, Elens S, Vazquez Suarez J, Jodaitis L, Ligot N, Naeije G, Lubicz B (2022) Thrombectomy for distal medium vessel occlusion with a new generation of Stentretriever (Tigertriever 13). Interv Neuroradiol 28(4):444–454 Epub 2021 Sep 13. PMID: 34516332; PMCID: PMC9326865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bourcier R, Consoli A, Desilles JP, Labreuche J, Kyheng M, Desal H, Alias Q, Gory B, Dargazanli C, Janot K, Zhu F, Lapergue B, Marnat G (2023) Temporal trends in results of endovascular treatment of anterior intracranial large cerebral vessel occlusion: a 7-year study. Eur Stroke J 8(3):655–666 Epub 2023 Jun 8. PMID: 37288701; PMCID: PMC10472952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Collette SL, van de Ven EA, Luijckx GR, Lingsma HF, van Doormaal PJ, van Es ACGM, van den Wijngaard IR, Goldhoorn RB, de Groot JC, van Zwam WH, Majoie CBLM, Dippel DWJ, Bokkers RPH, Uyttenboogaart M, On Behalf Of The Mr Clean Registry Investigators (2023) Alternative arterial Access routes for Endovascular Thrombectomy in patients with Acute ischemic stroke: a study from the MR CLEAN Registry. J Clin Med 12(9):3257. 10.3390/jcm12093257PMID: 37176697; PMCID: PMC10179212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hernandez D, Requena M, Olivé-Gadea M, de Dios M, Gramegna LL, Muchada M, García-Tornel Á, Diana F, Rizzo F, Rivera E, Rubiera M, Piñana C, Rodrigo-Gisbert M, Rodríguez-Luna D, Pagola J, Carmona T, Juega J, Rodríguez-Villatoro N, Molina C, Ribo M, Tomasello A (2024) Radial versus femoral Access for Mechanical Thrombectomy in patients with stroke: a Noninferiority Randomized Clinical Trial. Stroke 55(4):840–848 Epub 2024 Feb 1. PMID: 38527149 [DOI] [PubMed] [Google Scholar]
- 41.Diel NJ, Gerner ST, Alhaj Omar O, Kalder J, Manz E, Keschenau PR, Struffert T, Brueckner T, Huttner HB, Doeppner TR (2023) Rendezvous intervention using combined surgical carotid endarterectomy followed by endovascular thrombectomy in patients with acute tandem occlusions: a proof-of-concept experience at a tertiary care center. Neurol Res Pract 5(1):60. 10.1186/s42466-023-00290-4PMID: 38057910; PMCID: PMC10701999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paech D, Lehnen N, Lakghomi A, Schievelkamp A, Gronemann C, Bode FJ, Radbruch A, Dorn F (2023) School of Thrombectomy-A 3-Step Approach to perform Acute Stroke Treatment with Simulator training and virtual Supervision by Remote streaming support (RESS). Clin Neuroradiol 33(2):529–535 Epub 2022 Dec 15. PMID: 36520188; PMCID: PMC9753868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zaidi SF, Castonguay AC, Zaidat OO, Mueller-Kronast N, Liebeskind DS, Salahuddin H, Jumaa MA (2021) Intra-arterial thrombolysis after unsuccessful mechanical thrombectomy in the STRATIS Registry. AJNR Am J Neuroradiol 42(4):708–712. 10.3174/ajnr.A6962Epub 2021 Jan 28. PMID: 33509921; PMCID: PMC8040984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Diprose WK, Wang MTM, Ghate K, Brew S, Caldwell JR, McGuinness B, Barber PA (2021) Adjunctive Intra-arterial Thrombolysis in Endovascular Thrombectomy: A Systematic Review and Meta-analysis. Neurology.;96(24):1135–1143. 10.1212/WNL.0000000000012112. PMID: 33931539 [DOI] [PubMed]
- 45.Liu M, Nasr D, Brinjikji W (2023) The incidence of medium vessel occlusions: a population-based study. Front Neurol 14:1225066. 10.3389/fneur.2023.1225066PMID: 37576020; PMCID: PMC10415218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ospel JM, Goyal M (2021) A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg 13(7):623–630. 10.1136/neurintsurg-2021-017321Epub 2021 Feb 26. PMID: 33637570 [DOI] [PubMed] [Google Scholar]
- 47.Rodriguez-Calienes A, Siddiqui FM, Galecio-Castillo M, Mohammaden MH, Dolia JN, Grossberg JA, Pabaney A, Hassan AE, Tekle WG, Saei H, Miller S, Majidi S, Fifi T, Valestin J, Siegler G, Penckofer JE, Zhang M, Sheth L, Salazar-Marioni SA, Iyyangar S, Nguyen A, Abdalkader TN, Linfante M, Dabus I, Mehta G, Sessa BP, Jumma J, Sugg MA, Linares RM, Nogueira G, Liebeskind RG, Haussen DS, Ortega-Gutierrez DC (2024 May) Rescue therapy for failed mechanical thrombectomy in Acute ischemic stroke: a pooled analysis of the Society of Vascular and Interventional Neurology Registry. Ann Neurol 16. 10.1002/ana.26967Epub ahead of print. PMID: 38752428 [DOI] [PubMed]
- 48.Martins PN, Nogueira RG, Tarek MA, Dolia JN, Sheth SA, Ortega-Gutierrez S, Salazar-Marioni S, Iyyangar A, Galecio-Castillo M, Rodriguez-Calienes A, Pabaney A, Grossberg JA, Haussen DC Early technique switch following failed passes during mechanical thrombectomy for ischemic stroke: should the approach change and when? J Neurointerv Surg. 2024 Apr 4:jnis-2024-021545. 10.1136/jnis-2024-021545. Epub ahead of print. PMID: 38479798. [DOI] [PubMed]
- 49.Cai J, Xu H, Xiao R, Hu L, Xu P, Guo X, Xie Y, Pan M, Tang J, Gong Q, Liu Y, Su R, Deng J, Wang L (2023) Rescue intracranial stenting for acute ischemic stroke after the failure of mechanical thrombectomy: a systematic review, meta-analysis, and trial sequential analysis. Front Neurol 14:1023089. 10.3389/fneur.2023.1023089PMID: 36761342; PMCID: PMC9905111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mosimann PJ, Kaesmacher J, Gautschi D, Bellwald S, Panos L, Piechowiak E, Dobrocky T, Zibold F, Mordasini P, El-Koussy M, Wiest R, Bervini D, Wagner F, Arnold M, Jung S, Galimanis A, Gralla A, Fischer U (2018) Predictors of unexpected early reocclusion after successful mechanical thrombectomy in Acute ischemic stroke patients. Stroke 49(11):2643–2651. 10.1161/STROKEAHA.118.021685. Erratum in: Stroke. 2018;49(12):e343. PMID: 30355192 [DOI] [PubMed]
- 51.D’Anna L, Merlino G, Romoli M, Zhang L, Del Regno C, Aggour M, Levee V, Foschi M, Sponza M, Toraldo F, Algazlan R, Ruggiero M, Longoni M, Lobotesis K, Abu-Rumeileh S, Bagatto D, Mansoor N, Gigli GL, Valente M, Banerjee S (2024 May) Predictors of futile recanalization in nonagenarians treated with mechanical thrombectomy: a multi-center observational study. J Neurol 16. 10.1007/s00415-024-12428-8. Epub ahead of print. PMID: 38753228 [DOI] [PMC free article] [PubMed]
- 52.Marios-Nikos P, Alex B, Jens F, Isabel F, Jan G, Mira K, Ronen L, Paolo M, Marc R, Jeffrey LS, Daniel S, Adriaan VE, Claus Z, Nikki R, Luzia B, Urs F (2024) EnDovascular Therapy Plus Best Medical Treatment (BMT) Versus BMT alone for MedIum distal VeSsel occlusion sTroke (DISTAL): an international, multicentre, randomized-controlled, two-arm, assessor-blinded trial.Eur Stroke J 2024 May 3:23969873241250212. 10.1177/23969873241250212. Epub ahead of print. PMID: 38702876. [DOI] [PMC free article] [PubMed]
- 53.Alexandre AM, Monforte M, Brunetti V, Scarcia L, Cirillo L, Zini A, Scala I, Nardelli V, Arbia F, Arbia G, Frisullo G, Kalsoum E, Camilli A, De Leoni D, Colò F, Abruzzese S, Piano M, Rollo C, Macera A, Ruggiero M, Lafe E, Gabrieli JD, Cester G, Limbucci N, Arba F, Ferretti S, Da Ros V, Bellini L, Salsano G, Mavilio N, Russo R, Bergui M, Caragliano AA, Vinci SL, Romano DG, Frauenfelder G, Semeraro V, Ganimede MP, Lozupone E, Romi A, Cavallini A, Milonia L, Muto M, Candelaresi P, Calabresi P, Pedicelli A, Broccolini A (2024) Baseline clinical and neuroradiological predictors of outcome in patients with large ischemic core undergoing mechanical thrombectomy: a retrospective multicenter study. Int J Stroke 19(7):779–788. 10.1177/17474930241245828Epub 2024 Apr 16. PMID: 38546177; PMCID: PMC11298113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Salim H, Musmar B, Adeeb N, Yedavalli V, Lakhani D, Grewal SS, El Naamani K, Henninger N, Sundararajan SH, Kühn AL, Khalife J, Ghozy S, Scarcia L, Tan BY, Regenhardt RW, Heit JJ, Cancelliere NM, Bernstock JD, Rouchaud A, Fiehler J, Sheth S, Puri AS, Dyzmann C, Colasurdo M, Barreau X, Renieri L, Filipe JP, Harker P, Radu RA, Abdalkader M, Klein P, Marotta TR, Spears J, Ota T, Mowla A, Jabbour P, Biswas A, Clarençon F, Siegler JE, Nguyen TN, Varela R, Baker A, Essibayi MA, Altschul D, Gonzalez NR, Möhlenbruch MA, Costalat V, Gory B, Stracke CP, Aziz-Sultan MA, Hecker C, Shaikh H, Liebeskind DS, Pedicelli A, Alexandre AM, Tancredi I, Faizy TD, Kalsoum E, Lubicz B, Patel AB, Pereira VM, Guenego A, Dmytriw AA (2024 May) MAD MT investigators. Outcomes of mechanical thrombectomy in anticoagulated patients with acute distal and medium vessel stroke. Eur Stroke J 10:23969873241249295. 10.1177/23969873241249295Epub ahead of print. PMID: 38726983 [DOI] [PMC free article] [PubMed]
- 55.Scarcia L, Colò F, Alexandre AM, Brunetti V, Pedicelli A, Arba F, Ruggiero M, Piano M, Gabrieli JD, Ros VD, Romano DG, Cavallini A, Salsano G, Panni P, Limbucci N, Caragliano AA, Russo R, Bigliardi G, Milonia L, Semeraro V, Lozupone E, Cirillo L, Clarençon F, Zini A, Broccolini A emergent Carotid Artery Stenting (eCAS) study group. Effects of emergent carotid stenting performed before or after mechanical thrombectomy in the endovascular management of patients with tandem lesion: a multicenter retrospective matched analysis. AJNR Am J Neuroradiol. 2024 Jul 29:ajnr.A8421. 10.3174/ajnr.A8421. Epub ahead of print. PMID: 39025636 [DOI] [PMC free article] [PubMed]
- 56.Consoli A, Pileggi M, Hasan AH, Rahman MH, Venier A, Sgreccia A, Pizzuto S, Coskun O, Di Maria F, Scarcia L, Lapergue B, Rodesch G, Bracard S, Chen B Unfavorable clinical outcomes in patients with good collateral scores following endovascular treatment for acute ischemic stroke of the anterior circulation: the UNCLOSE study. Interv Neuroradiol 2023 Nov 7:15910199231212519. 10.1177/15910199231212519. Epub ahead of print. PMID: 37936414. [DOI] [PubMed]
- 57.Yedavalli VS, Salim HA, Musmar B, Adeeb N, Essibayi MA, ElNaamani K, Henninger N, Sundararajan SH, Kuhn AL, Khalife J, Ghozy S, Scarcia L, Tan BY, Heit JJ, Regenhardt RW, Cancelliere NM, Bernstock JD, Rouchaud A, Fiehler J, Sheth SA, Puri AS, Dyzmann C, Colasurdo M, Barreau X, Renieri L, Filipe JP, Harker P, Radu RA, Marotta TR, Spears J, Ota T, Mowla A, Jabbour P, Biswas A, Clarençon F, Siegler JE, Nguyen TN, Varela R, Baker A, Altschul D, Gonzalez N, Möhlenbruch MA, Costalat V, Gory B, Stracke P, Aziz-Sultan MA, Hecker C, Shaikh H, Liebeskind DS, Pedicelli A, Alexandre AM, Tancredi I, Faizy TD, Kalsoum E, Lubicz B, Patel AB, Mendes Pereira V, Guenego A, Dmytriw AA (2024) MAD MT Investigators. Symptomatic intracerebral hemorrhage in proximal and distal medium middle cerebral artery occlusion patients treated with mechanical thrombectomy. J Neurointerv Surg. Jul 24:jnis-2024-021879. 10.1136/jnis-2024-021879. Epub ahead of print. PMID: 38977305 [DOI] [PubMed]
- 58.Alexandre AM, Scarcia L, Brunetti V, Scala I, Kalsoum E, Valente I, Camilli A, De Leoni D, Colò F, Frisullo G, Piano M, Rollo C, Macera A, Ruggiero M, Lafe E, Gabrieli JD, Cester G, Limbucci N, Arba F, Ferretti S, Da Ros V, Bellini L, Salsano G, Mavilio N, Russo R, Bergui M, Caragliano AA, Vinci SL, Romano DG, Frauenfelder G, Semeraro V, Ganimede MP, Lozupone E, Romi A, Cavallini A, Milonia L, Muto M, Giordano F, Cirillo L, Calabresi P, Pedicelli A, Broccolini A (2023) Predictors of parenchymal hematoma and clinical outcome after mechanical thrombectomy in patients with large ischemic core due to large vessel occlusion: a retrospective multicenter study. J Neurointerv Surg. Dec 21:jnis-2023-021146. 10.1136/jnis-2023-021146. Epub ahead of print. PMID: 38129110 [DOI] [PubMed]
- 59.Sallustio F, Nicolini E, Saia V, Pracucci G, Mascolo AP, Marrama F, Gandini R, Da Ros V, Diomedi M, Alemseged F, Casetta I, Fainardi E, Castellan L, Del Sette M, Limbucci N, Nencini P, Bergui M, Cerrato P, Saletti A, De Vito A, Cioni S, Tassi R, Simonetti L, Zini A, Ruggiero M, Longoni M, Tessitore A, Ferraù L, Cavasin N, Critelli A, Vallone S, Bigliardi G, Zimatore DS, Petruzzellis M, Boghi A, Naldi A, Comai A, Dall’Ora E, Sanfilippo G, Persico A, Gallesio I, Sepe F, Menozzi R, Pezzini A, Besana M, Giossi A, Sanna A, Tassinari T, Burdi N, Boero G, Augelli R, Cappellari M, Cosottini M, Giannini N, Romano DG, Frauenfelder G, Nuzzi PN, Spinelli MC, Paladini A, Rizzo A, Filizzolo M, Mannino M, Timpani C, De Santis F, Carità G, Russo M, Galvano G, Sicurella L, Mangiafico S, Toni D (2024 Jun) Italian Registry of Endovascular Treatment in Acute Stroke (IRETAS) collaborators. Association between procedural time and outcome in unsuccessful mechanical thrombectomy for acute ischemic stroke: analysis from the Italian Registry of Endovascular Treatment in Acute Stroke. J Neurol 5. 10.1007/s00415-024-12458-2Epub ahead of print. PMID: 38836906 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the authors Alexander Neumann and Paul Schildhauer, upon reasonable request.