Abstract
Abstract
Objectives
In this descriptive study, we aimed to assess how the index mode of birth and subsequent birth modes vary over time for public and private hospital maternity care funding models. The second aim was to determine to what extent the index mode of birth predicts subsequent birth modes in general and whether this differs in public versus private hospital maternity care funding models. With our aim, we have an innovative approach, specifically the women’s life course approach, which is hypothesis-generating and can be assessed in future studies.
Design, setting and participants
New South Wales population-linked data of low-risk women were analysed (2001–2016). Demographics and public/private care were recorded. Modes of the index birth and subsequent modes of second and third births (ie, spontaneous vaginal, instrumental vaginal elective/emergency caesarean birth) were registered. For those with 2 births and 3 births, 16 and 64 subsequent births patterns were created.
Primary and secondary outcome measures
Trend of index modes of birth and subsequent modes of birth over time and the prediction of subsequent birth modes based on the index birth. These outcomes were stratified for the initial maternity care funding model.
Results
In total, 172 041 low-risk nulliparous women were included in the initial cohort, 54.1% had a spontaneous index vaginal birth and 71% had their index birth in public hospitals. During the study period, 131 675 women had 2 births and 44 677 of these women had 3 births, respectively. Among women birthing in public hospitals, higher proportions of index and subsequent vaginal births were observed than in private hospitals, with fewer instrumental vaginal births and caesarean sections. Large differences were observed for birth patterns: vaginal-vaginal (public 55.8% vs private 36.8%) and vaginal-vaginal-vaginal (public 57.2% vs private 38.8%). Women with an index spontaneous vaginal birth showed a high probability (91.3%) of subsequent spontaneous vaginal births. When stratified by maternity care funding model, the probabilities were similar: 91.6% in public hospitals and 90.2% in private hospitals.
Conclusions
Our study of low-risk Australian women (2001–2011) found that those giving birth in public hospitals had higher proportions of spontaneous vaginal births compared with private hospitals, where caesarean sections were more common. Women with an index spontaneous vaginal birth had a very high probability to have subsequent vaginal births. These findings suggest that index mode of birth may be a predictor for subsequent modes of birth.
Keywords: OBSTETRICS, EPIDEMIOLOGY, Pregnant Women
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Large population-based linked study of low-risk women (n=172 041 with first healthy-born infants in New South Wales (NSW) (2001–2011), with at least one birth (n=172 041), two births (n=131 675) or three births (n=44 677).
This descriptive study showed that, in NSW from 2001 to 2016, the proportion of women having two subsequent vaginal births decreased over time, while the rate of two and three subsequent elective caesarean births increased, particularly in private care.
Public and private hospitals differed in the proportions of subsequent vaginal births, including vaginal-vaginal (55.8% vs 36.8%) and vaginal-vaginal-vaginal (57.2% vs 38.8%).
Women with an index spontaneous vaginal birth showed a high probability (91.3%) of a subsequent spontaneous vaginal birth, irrespective of the maternity care funding model.
Regardless of the maternity care funding model, women who had an initial elective caesarean section had a probability of 81.9% undergoing a second elective caesarean section.
Introduction
Around the world, interventions in childbirth have increased dramatically over the last few decades. While there has been a corresponding decline in maternal and perinatal mortality in most countries during this time, this decline has slowed more recently.1 2 In fact, there is evidence from high-income countries, such as the USA, indicating that maternal mortality rates have begun to rise over the past 10–20 years. Additionally, minimal changes in maternal mortality rates have been observed in other high-income nations.1,4 In Europe, the overall caesarean section (CS) rate stands at 26%. However, this rate tends to be lower in northern Europe (with the exception of the UK) compared with southern and central European countries.1 5 The CS rates in North America, South America and China are continuously increasing and are currently at 32%, 41% and 35%, respectively.6 Finally, in Australia, the overall CS rate is more than 38%, with repeat caesarean the biggest contributor to the rise.3 4
In 2018, the WHO released a new guideline with key recommendations on non-clinical interventions to reduce unnecessary CSs, and recognised that the rise in CS is a universal problem affecting low-income, middle-income and high-income countries, due to the potential for consequent iatrogenic harms for both mother and child.7 In some cases, birth interventions are needed to address actual or potential pathology for the mother and/or neonate. Mode of birth, whether vaginal birth or CS is influenced by a complex interplay of, for example, pregnancy factors (eg, complications) as well as demographic factors (eg, advanced maternal age), lifestyle choices (eg, obesity), onset of pregnancy (eg, spontaneous or artificial reproductive technologies) and women’s preference for personal, psychological or social reasons.8
The maternity care funding model also plays a role in the prevalence of CS, mainly through the lead maternal care provider’s discipline.8,11 As an example, Australia has a two-tier system with Medicare being the national publicly funded universal healthcare system providing care to all citizens in public hospitals at no or limited out-of-pocket cost. Australian consumers can also pay for private health insurance which involves an out-of-pocket cost, and this care can be provided in private or public hospitals. Intervention rates for women receiving care from private obstetricians in private hospitals are much higher than women with similar demographics and risk factors in public hospitals.810,12 Specifically, the overuse of CS often occurs in wealthier and more educated women and in private care, in Australia as well as elsewhere.11 13
Both a meta-analysis, and previous Scandinavian population-based registry studies conducted in the past 35 years, reported that women with an operative birth (ie, vaginal birth with instruments or CS) were less likely to have subsequent pregnancies and births, compared with women who had spontaneous vaginal births.14,18 Currently, analyses of the impact of mode of birth tend to be very short term and comprise immediate outcomes of the first or a subsequent birth.19 However, from a life course perspective, it is important for women to know how their index mode of birth might influence subsequent modes of birth. Identifying mode of birth patterns over time for individual women (including one, two or three modes of birth), and contextualising that information by the type of maternity care funding for the index birth (either private or public hospital), is important information for policy-makers and governments to have access to when planning maternity services and monitoring the quality of care.20 Furthermore, by offering probabilities of birth patterns derived from the index birth and maternity care funding model, maternal healthcare providers and women can gain valuable insights into how the index childbirth experience may shape their reproductive life course. This, in turn, provides vital information to enable women to make informed decisions when it comes to childbearing.
As part of addressing this issue, the study objectives were to evaluate index mode of birth and subsequent modes of birth differ over time for public and private hospital maternity care funding models. Additionally, we aimed to determine to what extent the index mode of birth can predict subsequent birth modes overall and whether this prediction varies between public and private hospital maternity care funding models. Our approach is innovative, using the women’s life course perspective, which is hypothesis-generating and can be explored further in future studies.
Methods
This registry-based study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guideline.21
Design
This population-based linked data study used data obtained from the Australian New South Wales (NSW) Centre for Health Record Linkage. The Centre uses probabilistic data linkage techniques to merge data from the following electronic (health) registry datasets: Perinatal Data Collection (PDC); Admitted Patient Data Collection (APDC); the Australian Bureau of Statistics (ABS); Socio-economic Indexes for Areas (SEIFA) and NSW Registry of Birth Deaths and Marriages (RBDM). Probabilistic record linkage assigns ‘linkage weight’ to pairs of records.22 Records that match perfectly or nearly perfectly on first name, surname, date of birth and address have a high-linkage weight and records that match only on date of birth have a low-linkage weight.22 A false-positive rate of 0.3% of records has been reported.22 Studies have reported a tendency towards under-reporting of maternal prenatal medical conditions during linkage.23 24 The process of comparing the PDC and APDC data has increased the sensitivity and specificity for the purpose of identifying those women with medical complications.24 25 Australian linked data have also been analysed in previous studies in which we examined the impact of single birth interventions (CS, induction for non-medical reasons) on maternal and child health.26 27
Demographic, pregnancy and birth characteristics were extracted from both PDC, APDC and ABS. The SEIFA data extract information from socioeconomic position by ranking areas in Australia according to relative socioeconomic advantages and disadvantages and education using women’s postal codes and defined as low (≤30 percentiles), medium (40–60 percentiles) or high (≥70 percentiles). Maternal and infant mortality rates were extracted from RBDM.
Inclusion criteria
Population-based data of low-risk nulliparous women were analysed. Those women who had a healthy index pregnancy and gave birth to a healthy term firstborn were included in the dataset. By selecting a healthy population, this study aimed to minimise potential confounding factors and ensure that the observed probabilities for different birth modes were not biased by pre-existing health conditions prior to the index mode of birth.
The included women gave birth to their first baby in the period 1 January 2001–31 December 2011 in a public or private hospital in NSW, Australia’s most populated state. Subsequent births could occur in the period 2001–2016, meaning that women had at least 5 years to conceive again during the follow-up period. To ensure this population met the criteria for a healthy pregnancy, the following inclusion criteria were applied: women were aged 20–35 years at the time of the index birth, had a term birth that occurred between 37 weeks and 0 days and 41 weeks and 6 days of gestation, with a singleton baby in a cephalic presentation. Women were excluded if, during their index pregnancy, medical risk factors (ie, diabetes and hypertensive disease), mental health risk factors (hospital admissions prior or during pregnancy), social risk factors (domestic violence) or maternal mortality had occurred. Additionally, women who smoked, consumed alcohol or drugs during their index pregnancy were also excluded. If the index birth resulted in a stillbirth or neonatal death, or where the firstborn had any congenital anomalies, were also excluded from the analyses. Infants with congenital abnormalities were excluded based on the International Statistical Classification of Diseases and Health Problems 10th Revision Australian Modification, as recorded in the APDC file (Q0.0–99.9). After applying these inclusion criteria, women and first-born infant pairs were excluded and those with missing data on gestational age, modes of birth, maternal age per birth, substance abuse, birth position, congenital anomalies or first-born infants were excluded from the analyses. Women and first-born infants were excluded in pairs if either one of them did not comply with the criteria. For subsequent births, all women with singleton pregnancies were included, even if complications arose, as these risk factors might have been related to the index mode of birth.
Index birth and birth patterns
Modes of birth were recorded as spontaneous vaginal birth (vag), instrumental vaginal birth with the assistance of forceps or a vacuum device (instr), elective CS (elCS) or emergency CS (emCS). First, we coded the index birth (four modes of birth). If women gave birth twice, all possible 16 birth patterns were created (eg, vaginal-vaginal and elCS-elCS). For women, who had 3 births, all 64 possible birth patterns were created (eg, vaginal-vaginal-vaginal and emCS-elCS-elCS). The birth patterns (including two or three births) were indexed by the date of the first birth.
Statistical analyses
Demographic characteristics and births (including one, two or three modes of birth) were reported for the initial cohort and stratified for the maternity care funding model received at the index birth (public or private hospitals) by using descriptive statistics. Moreover, the proportions of birth patterns over time were visualised by the four most prevalent birth patterns including two or three modes of birth. The accompanying trendlines were stratified for the funding model (public or private hospitals).
With conditional probability analyses, we calculated the probability of an event (ie, second mode of birth) given that a previous event (ie, index mode of birth) has already occurred.28 Additionally, we calculated the probability of the third mode of birth, based on two previous modes of birth. Next, the conditional probability analyses were stratified for the initial maternity care funding model (public or private). We created a contingency table to summarise the accounts of the occurrences of each events. All statistical analyses were performed with SPSS Statistics V.28.0 (SPSS) and R software V.4.1.1.
Patient and public involvement
Women and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
The NSW linked data set contained data on 398 217 singleton nulliparous pregnancies between 2001 and 2011. In this population, the number and proportions of infant mortality of the first-born children were 2438 stillbirths (0.6%) and 954 neonatal deaths (0.2%), respectively. The number and proportion of maternal mortality during the first pregnancy and birth was 14 (0.004%). A total of 66 743 first-born infants (16.8%) were excluded from the analyses due to mortality, diagnosis of congenital anomalies and non-vertex position of the infant prior to labour. In total, 147 938 women (37.2%) were excluded due to mortality, medical complications, mental health disorders and adverse lifestyle behaviours (including substance abuse) during the index pregnancy. Finally, 10 911 first-born infants and 584 women were excluded due to missing data (figure 1).
Figure 1. Flow chart of the included population.
In total, 172 041 women in the cohort had 1 birth in the period 2001–2011, 131 675 of these women had 2 births and 44 677 of these women had 3 births. During the follow-up period, 40 366 women had no further births; of these women, 30 789 (76.3%) gave birth in a public hospital and 9577 (23.7%) women gave birth in a private hospital.
Study population
The median maternal age of the index pregnancy was 28 (IQR 25–31). The majority of women were born in Australia (64.8%), had a partner (71.7%) and almost one-third (31.8%) had medium (40–60 percentiles) socioeconomic status. A total of 67.7% of women had a spontaneous onset of labour and 41.5% had a second baby in the 18–29 months after the birth of their first baby (table 1).
Table 1. Maternal and birth characteristics of the total study population and stratified for maternity care funding model index birth, New South Wales, in the period 2001–2011 (n=172 041).
| Total populationN=172 041 (100%) | Women with index birth in public hospitalN=122 047 (71%) | Women with index birth in private hospitalN=49 994 (29%) | |
| N (%)* | n (%)* | n (%)* | |
| Maternal characteristics at index birth | |||
| Maternal age (in years) | |||
| 20–24 | 36 021 (20.9) | 33 351 (27.3) | 2670 (5.3) |
| 25–29 | 67 674 (39.4) | 49 204 (40.3) | 18 470 (36.9) |
| 30–35 | 68 346 (39.7) | 39 492 (32.4) | 28 854 (57.7) |
| Country of birth | |||
| Australia | 111 497 (64.8) | 74 778 (61.3) | 36 719 (73.4) |
| Outside Australia | 59 952 (34.9) | 46 956 (38.5) | 12 966 (26.0) |
| Missing | 592 (0.3) | 313 (0.3) | 279 (0.6) |
| Socioeconomic status† | |||
| Low | 36 639 (21.3) | 32 364 (26.5) | 4275 (8.6) |
| Middle | 54 764 (31.8) | 43 250 (35.4) | 11 514 (23.0) |
| High | 77 370 (45.0) | 43 585 (35.7) | 33 785 (67.6) |
| Missing | 3268 (1.9) | 2848 (2.3) | 420 (0.8) |
| Marital status | |||
| Single/widow/divorced | 36 067 (21.0) | 29 251 (24.0) | 6816 (13.6) |
| Partner/spouse | 123 275 (71.7) | 84 014 (68.8) | 39 261 (78.5) |
| Missing | 12 699 (7.4) | 8782 (7.2) | 3917 (7.8) |
| Birth characteristics | |||
| Onset of labour at index birth | |||
| Spontaneous | 116 505 (67.7) | 87 603 (71.8) | 28 902 (57.8) |
| Induction of labour‡ | 45 890 (26.7) | 30 625 (25.1) | 15 265 (30.5) |
| Missing | 9646 (5.6) | 3819 (3.1) | 5827 (11.7) |
| Time in months between first and second births§ | |||
| ≤17 | 13 163 (10.0) | 9677 (10.6) | 3486 (8.6) |
| 18–29 | 54 673 (41.5) | 36 054 (39.5) | 18 619 (46.1) |
| 30–41 | 33 094 (25.1) | 22 287 (24.4) | 10 807 (26.7) |
| 42–53 | 14 937 (11.3) | 10 787 (11.8) | 4150 (10.3) |
| ≥54 | 15 808 (12.0) | 12 453 (13.6) | 3355 (8.3) |
| Time in months between third and second births¶ | |||
| ≤17 | 4503 (10.1) | 3527 (11.0) | 976 (7.8) |
| 18–29 | 15 748 (35.2) | 11 070 (34.5) | 4678 (37.3) |
| 30–41 | 11 280 (25.2) | 7816 (24.3) | 3464 (27.6) |
| 42–53 | 6177 (13.8) | 4434 (13.8) | 1743 (13.9) |
| ≥54 | 6969 (15.6) | 5280 (16.4) | 1689 (13.5) |
| Periods first infants were born | |||
| 2001–2003 | 42 813 (24.9) | 29 474 (24.1) | 13 339 (26.7) |
| 2004–2007 | 60 388 (35.1) | 42 399 (34.7) | 17 989 (36.0) |
| 2008–2011 | 68 840 (40.0) | 50 174 (41.1) | 18 666 (37.3) |
Numbers may not always add up to 100% due to truncation.
Socio Eeconomic Sstatus is based on area indices of income and education using women’s postal codes and defined as low (10–30 percentiles), medium (40–60 percentiles) or high (≥70 percentiles).
Induction of labour with synthetic hormones, artificial rupture of membranes or other methods.
Calculated for women who had two or three subsequent births (n=131 675).
Calculated for women who had three subsequent births (n=44 677).
In total, 71% of women had their index birth in a public hospital and 29% in a private hospital. Compared with women who had their first infant in a public hospital, women who had their first infant in a private hospital, were older, were more likely to have a partner, were more often born in Australia, had a higher socioeconomic position and had a lower rate of spontaneous onset of labour (table 1).
Proportions of index birth and subsequent births
More than half of the women (54.1%) had a spontaneous vaginal birth with their first baby (table 2). The proportion of spontaneous vaginal births (vag) was higher for women giving birth in a public hospital versus private hospital (59.8% vs 40.0%). Of the 40 366 women with no subsequent births, we observed the following proportions for the index modes of birth: spontaneous vaginal 22.5%, instrumental vaginal 22.6%, elCS 28.6% and emCS 25.9%. After stratifying these proportions by the maternity care funding model, the proportions for no further births after the index birth were spontaneous vaginal (public 23.9% vs private 17.5%), instrumental vaginal (public 25.3% vs private 17.8%), elCS (public 31.9% vs 26.4%) and emCS (public 28.5% vs private 20.3%), respectively.
Table 2. Patterns of mode of birth across index (n=172 041) and two births (n=131 675), for the total study population and stratified for maternity care funding model index birth, New South Wales, in the period 2001–2016.
| Total population | Women who had their index birth in a public hospital | Women who had their index birth in a private hospital | ||||
| Women with at least one birth (N=172 041) | n=122 047 (70.9%) | n=49 994 (29.1%) | ||||
| N | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |
| Vag | 92 993 | 54.1 (53.8 to 54.3) | 73 003 | 59.8 (59.5 to 60.1) | 19 990 | 40.0 (39.6 to 40.4) |
| Instr | 39 325 | 22.9 (22.7 to 23.1) | 24 917 | 20.4 (20.2 to 20.6) | 14 408 | 28.8 (28.4 to 29.2) |
| ElCS | 9620 | 5.6 (5.5 to 5.7) | 3804 | 3.1 (3.0 to 3.2) | 5816 | 11.6 (11.4 to 11.9) |
| EmCS | 30 103 | 17.5 (17.3 to 17.7) | 20 323 | 16.7 (16.4 to 16.9) | 9780 | 19.6 (19.2 to 19.9) |
| Women with at least two births (N=131 675) | n=91 258 (69.3%) | n=40 417 (30.7%) | ||||
| Vag-vag | 65 771 | 49.9 (49.7 to 50.2) | 50 894 | 55.8 (55.4 to 56.1) | 14 877 | 36.8 (36.3 to 37.3) |
| Vag-instr | 1793 | 1.4 (1.3 to 1.4) | 1152 | 3 (1.2 to 1.3) | 641 | 1.6 (1.5 to 1.7) |
| Vag-elCS | 2770 | 2.1 (2.0 to 2.2) | 2121 | 2.3 (2.2 to 2.4) | 649 | 1.6 (1. to 1.7) |
| Vag-emCS | 1697 | 1.3 (1.2 to 1.4) | 1370 | 1.5 (1.4 to 1.6) | 327 | 0.8 (0.7 to 0.9) |
| Instr-vag | 23 364 | 17.7 (17.5 to 18.0) | 14 583 | 16.0 (15.7 to 16.2) | 8781 | 21.7 (21.3 to 22.1) |
| Instr-instr | 3165 | 2.4 (2.3 to 2.5) | 1591 | 1.7 (1.7 to 1.8) | 1574 | 3.9 (3.7 to 4.1) |
| Instr-elCS | 2595 | 2.0 (1.9 to 2.0) | 1583 | 1.7 (1.7 to 1.8) | 1012 | 2.5 (2.4 to 2.7) |
| Instr-emCS | 1333 | 1.0 (1.0 to 1.1) | 850 | 0.9 (0.9 to 1.0) | 483 | 1.2 (1.1 to 1.3) |
| elCS-vag | 318 | 0.2 (0.2 to 0.3) | 194 | 0.2 (0.2 to 0.2) | 124 | 0.3 (0.3 to 0.4) |
| elCS-instr | 141 | 0.1 (0.1 to 0.1) | 71 | 0.1 (0.1 to 0.1) | 70 | 0.2 (0.1 to 0.2) |
| elCS-elCS | 5625 | 4.3 (4.2 to 4.4) | 1991 | 2.2 (2.1 to 2.3) | 3634 | 9.0 (8.7 to 9.3) |
| elCS-emCS | 788 | 0.6 (0.6 to 0.6) | 333 | 0.4 (0.3 to 0.4) | 455 | 1.1 (1.0 to 1.2) |
| emCS-vag | 2013 | 1.5 (1.5 to 1.6) | 1592 | 1.7 (1.7 to 1.8) | 421 | 1.0 (0.9 to 1.1) |
| emCS-instr | 1269 | 1.0 (0.9 to 1.0) | 907 | 1.0 (0.9 to 1.1) | 362 | 0.9 (0.8 to 1.0) |
| emCS-emCS | 4001 | 3.0 (2.9 to 3.1) | 2751 | 3.0 (2.9 to 3.1) | 1250 | 3.1 (2.9 to 3.3) |
| emCS-elCS | 15 032 | 11.4 (11.2 to 11.6) | 9275 | 10.2 (10.0 to 10.4) | 5757 | 14.2 (13.9 to 14.6) |
elCSelective caesarean sectionemCSemergency caesarean sectionInstrinstrumental vaginal birth with assistance of a forceps or a vacuum deviceVagspontaneous vaginal birth
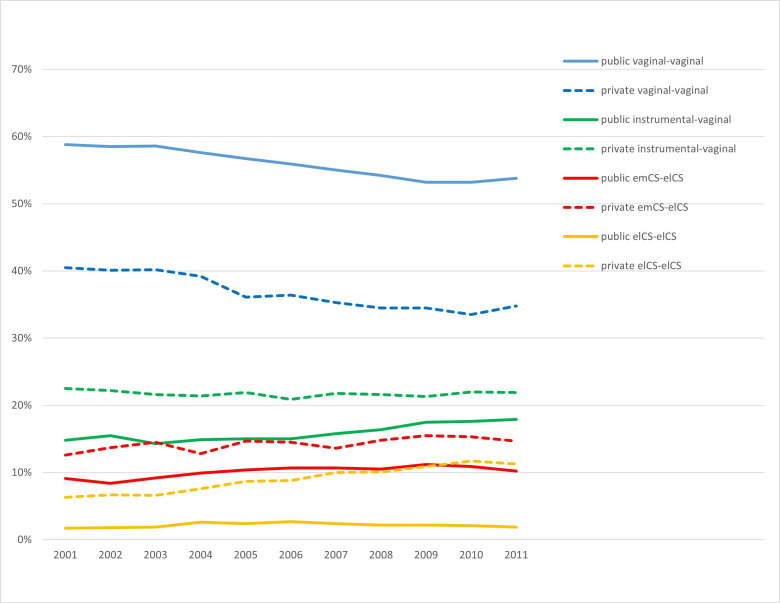
In the total population of women with at least two births, the most frequently observed patterns were vag-vag (49.9%), instr-vag (17.7%), emCS-elCS (11.4%), elCS-elCs (4.3%) and emCs-emCs (3.0%). All other combinations of two modes of birth ranged from 0.1% to 2.4%. After stratifying the analyses for women with an index birth in either public or private hospitals the following birth patterns differed most: vag-vag (public 55.8% vs private 36.8%), elCS-elCS (public 2.2% vs private 9.0%), instrumental-vaginal (public 16.0% vs private 21.7%), emCS-elCS (public 10.2% vs private 14.2%, table 2). Moreover, the proportions of birth patterns changed over time, with a decline in vag-vag for both public and private settings. Differences in trends could also be observed, for example, elCs-elCs remained stable when the index birth occurred in a public hospital, respectively, 1.7% in 2001 and 1.9% in 2011whereas elCs-elCs increased if the index birth occurred in a private hospital, respectively, 6.3% in 2001 and 11.3% in 2011 (figure 2).
Figure 2. Trendlines birth patterns of two modes of birth, of which the index birth occurred between 2001 and 2011. elCS, elective caesarean section; emCS, emergency caesarean section.
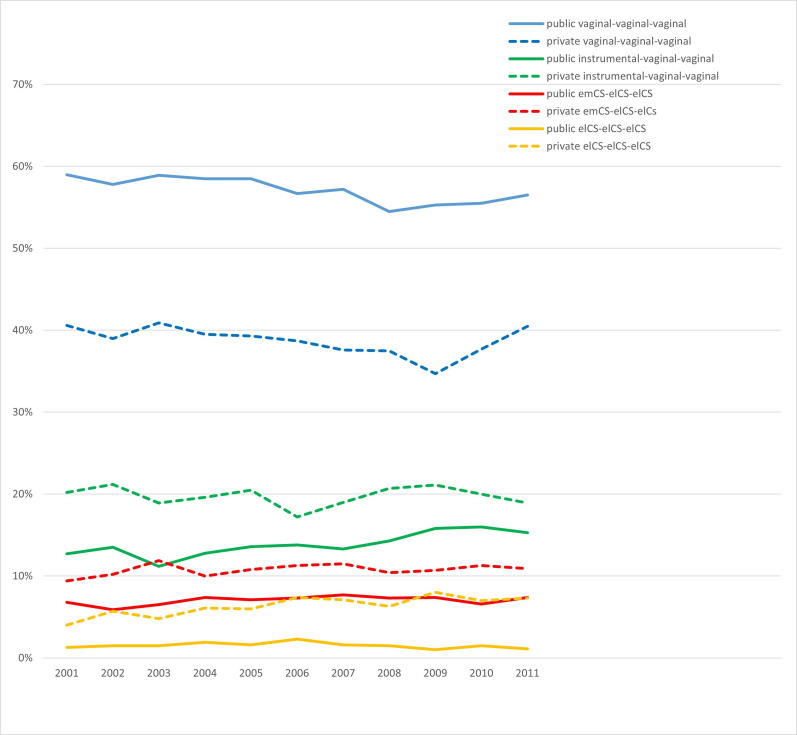
In the total population of women with at least three births, the most frequently observed patterns were vag-vag-vag (52.1%), instr-vag-vag (15.4%), emCS-elCS-elCs (8.1%), elCS-elCS-elCS (2.9%) and emCS-emCS-elCS (2.1%). All other combinations of three modes of birth ranged from 0.004% to 1.7%. After stratifying the analyses for women with an index birth in either a public or private hospital, the following birth patterns differed most: vag-vag-vag (public 57.2% vs private 38.8%), instr-vag-vag (public 13.7% vs private 19.8%), emCS-elCS-elCS (public 7.0% vs private 10.7%) and elCS-elCS-elCS (public 1.6% vs private 6.2%, online supplemental table 1). Moreover, the proportions of birth patterns vag-vag-vag were modestly declining over time in the public hospital setting. In the private hospital, more fluctuations were observed, with a steep decline in 2009 for the birth pattern vag-vag-vag whereas in the same year the birth patterns instr-vag-vag and elCS-elCs-elCs were slightly increasing. In the period 2001–2011, the birth pattern elCs-elCs-elCS remained stable when the index birth occurred in a public hospital, whereas elCs-elCs-elCS increased moderately if the index birth occurred in a private hospital (figure 3).
Figure 3. Trendlines birth patterns of three modes of birth, of which the index birth occurred between 2001 and 2011. elCS, elective caesarean section; emCS, emergency caesarean section.
Probabilities of the subsequent birth depended on previous birth(s)
Irrespective of the maternity care funding model, the probability of women having a second subsequent spontaneous vaginal birth was 91.3% (table 3). This was similar for women who had their index birth in either a public or private hospital (91.6% and 90.2% respectively, table 4). Also, irrespective of the maternity care funding model, women who had an index elCS had a probability of 81.9% of having a second elCS. Compared with public hospitals, those giving birth in private hospitals had a higher probability that the second birth was also an elCS, public 76.9%% and private 84.9%, respectively (table 4).
Table 3. Probabilities of the second mode of birth based on the index mode of birth for the total population (n=131 675 women).
| Probability second birth is vag | Probability second birth is instr | Probability second birth is elCS | Probability second birth is emCS | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Women index birth | ||||
| Vag | 91.3 (91.9 to 91.5) | 2.5 (2.4 to 2.6) | 3.8 (3.7 to 4.0) | 2.4 (2.2 to 2.5) |
| Instr | 76.7 (76.2 to 77.2) | 10.4 (10.1 to 10.7) | 8.5 (8.2 to 8.8) | 4.4 (4.1 to 4.6) |
| elCS | 4.6 (4.1 to 5.2) | 2.1 (1.7 to 2.4) | 81.9 (80.9 to 82.8) | 11.4 (10.7 to 12.2) |
| emCS | 9.0 (8.6 to 9.4) | 5.7 (5.4 to 6.0) | 67.4 (6.7 to 68.0) | 17.9 (17.4 to 18.4) |
elCSelective caesarean sectionemCSemergency caesarean sectionInstrinstrumental vaginal birth with assistance of a forceps or a vacuum deviceVagspontaneous vaginal birth
Table 4. Probabilities of the second mode of birth based on the index mode of birth, stratified for maternity care funding model (N=131 675).
| Women who had their index birth in a public hospitalN=91 258 | Women who had their index birth in a private hospitalN=40 417 | |||||||
| Probability second birth is vag | Probability second birth is instr | Probability second birth is elCS | Probability second birth is em CS | Probability second birth is vag | Probability second birth is instr | Probability second birth is elCS | Probability second birth is emCS | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95%CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Women index birth | ||||||||
| Vag | 91.6 (91.4 to 91.9) | 2.1 (2.0 to 2.2) | 3.8 (3.7 to 4.0) | 2.5 (2.3 to 2.6) | 90.2 (89.7 to 90.6) | 3.9 (3.6 to 4.2) | 3.9 (3.6 to 4.2) | 2.0 (1.8 to 2.2) |
| Instr | 78.4 (77.8 to 79.0) | 8.5 (8.2 to 9.0) | 8.5 (8.1 to 8.9) | 4.6 (4.3 to 4.9) | 74.1 (73.3 to 74.9) | 13.3 (12.7 to 13.9) | 8.5 (8.0 to 9.1) | 4.1 (3.7 to 4.4) |
| elCS | 7.5 (6.5 to 8.6) | 2.7 (2.1 to 3.4) | 76.9 (75.2 to 78.5) | 12.9 (11.6 to 14.2) | 2.9 (2.4 to 3.4) | 1.6 (1.3 to 2.1) | 84.9 (83.7 to 85.9) | 10.6 (9.7 to 11.60 |
| emCS | 11.0 (10.5 to 11.5) | 6.2 (5.9 to 6.7) | 63.9 (63.1 to 64.6) | 18.9 (18.3 to 19.6) | 5.4 (4.9 to 5.9) | 4.6 (4.2 to 5.1) | 74.0 (73.9 to 74.9) | 16.0 (15.2 to 16.9) |
elCSelective caesarean sectionemCSemergency caesarean sectionInstrinstrumental vaginal birth with assistance of a forceps or a vacuum devicevagspontaneous vaginal birth
Women with the birth patterns vag-vag had a probability of 93.2% of having a third spontaneous vaginal birth (table 5). This probability was similar for women who had their index birth in either a public or private hospital (93.4% and 92.3%, respectively, table 6). Women whose birth pattern for their previous two births was instr-vag had a probability of 89.0% for a subsequent spontaneous vaginal birth, which was also not related to whether the index birth was in a public or private hospital (89.3% and 88.4%, respectively).
Table 5. Probabilities of the third mode of birth based on birth patterns including first and second mode of birth of the total population (n=44 677).
| Probability third birth is vag | Probability third birth is instr | Probability third birth is ElCS | Probability third birth is EmCS | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Women with two births | ||||
| Vag-vag | 93.2 (92.9 to 93.5) | 1.6 (1.4 to 1.7) | 3.1 (2.9 to 3.3) | 2.1 (1.9 to 2.3) |
| Vag-instr | 78.1 (74.3 to 81.5) | 10.7 (8.2 to 13.7) | 5.3 (3.6 to 7.6) | 5.9 (4.1 to 8.3) |
| Vag-elCS | 30.6 (27.5 to 33.8) | 2.4 (1.4 to 3.6) | 58.9 (55.5 to 62.2) | 8.1 (6.4 to 10.2) |
| Vag-emCS | 33.6 (29.6 to 37.9) | 1.9 (0.9 to 3.4 | 50.5 (46.1 to 54.8) | 14.0 (11.1 to 17.2) |
| Instr-vag | 89.0 (88.3 to 89.7) | 4.9 (4.4 to 5.4) | 3.6 (3.2 to 4.1) | 2.5 (2.2 to 2.9) |
| Instr-instr | 64.9 (61.7 to 68.0) | 21.1 (18.4 to 23.9) | 9.2 (7.4 to 11.3) | 4.8 (3.5 to 6.4) |
| Instr-elCS | 12.5 (10.1 to 15.3) | 2.6 (1.5 to 4.2) | 73.8 (70.2 to 77.1) | 11.1 (8.8 to 13.8) |
| Instr-emCS | 17.0 (13.2 to 21.4) | 7.0 (4.6 to 10.3) | 66.3 (61.0 to 71.3) | 9.7 (6.8 to 13.3) |
| elCS-vag | 73.1 (64.2 to 80.8) | 4.2 (1.4 to 9.5) | 16.0 (9.9 to 23.8) | 6.7 (2.9 to 12.8) |
| elCS-instr | 59.3 (45.0 to 72.4) | 11.1 (4.2 to 22.6) | 24.1 (13.5 to 37.6) | 5.5 (1.2 to 15.4) |
| elCS-elCS | 0.8 (0.4 to 1.4) | 0.1 (0.0 to 0.5) | 93.6 (92.2 to 94.9) | 5.5 (4.3 to 6.8) |
| elCS-emCS | 2.2 (0.7 to 5.0) | 0.9 (0.1 to 3.1) | 79.4 (73.5 to 84.4) | 17.5 (12.8 to 23.1) |
| emCS-vag | 70.0 (66.7 to 73.1) | 4.4 (3.1 to 6.1) | 17.9 (15.3 to 20.7) | 7.7 (5.9 to 9.7) |
| emCS-instr | 54.9 (50.3 to 59.5) | 12.2 (9.4 to 15.5) | 23.5 (19.7 to 27.6) | 9.4 (6.9 to 12.4) |
| emCS-emCS | 1.7 (1.0 to 2.6) | 0.6 (0.2 to 1.2) | 79.4 (77.0 to 81.7) | 18.3 (16.2 to 20.7) |
| emCS-elCS | 1.0 (0.7 to 1.3) | 0.3 (0.2 to 0.6) | 90.9 (90.0 to 91.8) | 7.8 (7.0 to 8.6) |
elCSelective caesarean sectionemCSemergency caesarean sectionInstrinstrumental vaginal birth with assistance of a forceps or a vacuum devicevagspontaneous vaginal birth
Table 6. Probabilities of the third mode of birth based on birth patterns including first and second birth, stratified for maternity care funding model index birth (N=44 677).
| Women who had their first birth in a public hospitaln=32 127 | Women who had their first birth in a private hospitaln=12 550 | |||||||
| Probability third birth is vag | Probability third birth is instr | Probability third birth is elCS | Probability third birth is emCS | Probability third birth is vag | Probability third birth is instr | Probability third birth is elCS | Probability third birth is emCS | |
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Women with two births | ||||||||
| Vag-vag | 93.4 (93.1 to 93.8) | 1.4 (1.2 to 1.5) | 3.1 (2.9 to 3.4) | 2.1 (1.9 to 2.3) | 92.3 (91.6 to 93.0) | 2.4 (2.0 to 2.8) | 3.2 (2.7 to 3.7) | 2.1 (1.8 to 2.6) |
| Vag-instr | 77.3 (72.5 to 81.6) | 10.3 (7.3 to 14.1) | 5.3 (3.2 to 8.3) | 7.1 (4.6 to 10.4) | 79.4 (72.9 to 85.0) | 11.4 (7.2 to 16.8) | 5.4 (2.6 to 9.7) | 3.8 (1.5 to 7.6) |
| Vag-elCS | 30.1 (26.6 to 33.8) | 2.0 (1.1 to 3.3) | 59.2 (55.3 to 62.9) | 8.8 (6.7 to 4.2) | 32.4 (25.8 to 39.6) | 3.7 (1.5 to 7.5) | 58.0 (50.6 to 65.1) | 5.9 (3.0 to 10.2) |
| Vag-emCS | 34.2 (29.7 to 38.9) | 1.4 (0.5 to 3.0) | 50.3 (45.5 to 55.2) | 14.1 (11.0 to 17.7) | 31.3 (22.2 to 41.5) | 4.2 (1.1 to 10.3) | 51.0 (40.6 to 61.4) | 13.5 (7.4 to 22.0) |
| Instr-vag | 89.3 (88.4 to 90.2) | 4.2 (3.6 to 4.8) | 3.9 (3.4 to 4.5) | 2.6 (2.2 to 3.1) | 88.4 (87.2 to 89.6) | 6.0 (5.2 to 7.0) | 3.2 (2.6 to 3.9) | 2.4 (1.9 to 3.0) |
| Instr-instr | 66.4 (61.8 to 70.7) | 16.4 (13.1 to 20.1) | 11.0 (8.3 to 14.3) | 6.2 (4.2 to 8.8) | 63.4 (58.8 to 67.9) | 25.8 (21.8 to 30.1) | 7.4 (5.1 to 10.2) | 3.4 (1.9 (5.5) |
| Instr-elCS | 13.5 (10.3 to 17.2) | 3.3 (1.7 to 5.5) | 72.0 (67.3 to 76.3) | 11.3 (8.3 to 14.8) | 10.9 (7.3 to 15.5) | 1.6 (0.4 to 4.1) | 76.4 (70.7 to 81.7) | 10.9 (7.3 to 15.5) |
| Instr-emCS | 16.5 (1.8 to 22.2) | 6.6 (3.7 to 10.8) | 69.8 (63.1 to 75.9) | 7.1 (4.0 to 11.4) | 17.8 (11.7 to 25.5) | 7.8 (3.8 to 13.8) | 60.4 (51.5 to 69.0) | 14.0 (8.5 to 21.2) |
| elCS-vag | 70.4 (58.4 to 80.7) | 4.2 (0.9 to 11.9) | 15.5 (8.0 to 26.0) | 9.9 (4.1 to 19.3) | 77.1 (62.7 to 88.0) | 4.1 (0.5 to 14.3) | 16.7 (7.5 to 30.2) | 2.1 (0.1 to 11.1) |
| elCS-instr | 66.6 (47.2 to 82.7) | 10.0 (2.1 to 26.5) | 16.7 (5.6 to 34.7) | 6.7 (0.8 to 22.1) | 50.0 (29.1 to 70.9) | 12.5 (2.7 to 32.4) | 33.3 (15.6 to 55.3) | 4.2 (0.1 to 21.1) |
| elCS-elCS | 1.1 (0.4 to 2.4) | 0.1 (0.0 to 0.7) | 92.7 (90.2 to 94.8) | 6.1 (4.3 to 8.5) | 0.6 (0.2 to 1.4) | 0.2 (0.0 to 0.9) | 94.2 (92.4 to 95.7) | 5.0 (3.6 to 6.7) |
| elCS-emCS | 1.9 (0.2 to 6.6) | 1.9 (0.2 to 6.6) | 76.4 (67.2 to 84.1) | 19.8 (12.7 to 28.7) | 2.4 (0.5 to 7.0) | 0.0 (0.0 to 3.0) | 82.0 (74.0 to 88.3) | 15.6 (9.6 to 23.2) |
| emCS-vag | 69.1 (65.4 to 72.7) | 4.3 (2.8 to 6.2) | 17.9 (15.0 to 6.2) | 8.7 (6.6 to 11.2) | 73.0 (65.9 to 79.4) | 5.1 (2.3 to 9.4) | 18.0 (12.6 to 24.4) | 3.9 (1.6 to 7.9) |
| emCS-instr | 55.7 (50.0 to 61.2) | 11.9 (8.6 to 16.0) | 22.6 (18.2 to 27.6) | 9.8 (6.7 to 13.6) | 53.3 (45.0 to 61.5) | 12.7 (7.8 to 19.1) | 25.3 (18.6 to 33.1) | 8.7 (4.7 to 14.4) |
| emCS-emCS | 1.7 (0.9 to 2.8) | 0.6 (0.2 to 1.4) | 80.4 (77.6 to 83.1) | 17.3 (14.8 to 20.0) | 1.7 (0.6 to 3.6) | 0.6 (0.1 to 2.0) | 76.9 (72.2 to 81.2) | 20.8 (16.7 to 25.4) |
| emCS-elCS | 1.2 (0.8 to 1.7) | 0.4 (0.2 to 0.7) | 90.8 (89.6 to 91.9 | 7.6 (6.5 to 8.7) | 0.6 (0.2 to 1.1) | 0.2 (0.0 to 0.6) | 91.1 (89.6 to 92.5) | 8.1 (6.8 to 9.6) |
elCSelective caesarean sectionemCSemergency caesarean sectionInstrinstrumental vaginal birth with assistance of a forceps or a vacuum deviceVagspontaneous vaginal birth
Women whose birth pattern for their previous two births was emCS-elCS had a probability of 90.9% to have subsequent elCs, the probability was similar for index births in a public and private hospital (90.8% and 91.1%, respectively). Women whose birth pattern was elCs-elCS had a probability of 93.6% to have a third elCs, which also was not related to whether first birth was in a public or private hospital (92.7% and 94.2%, respectively, tables5 6).
Discussion
This descriptive study showed that the proportion of women having two subsequent vaginal births decreased over the years in NSW, period 2001–2016. Particularly, in private care, the rate of two and three subsequent elective caesareans births increased. Birth patterns vaginal-vaginal and vaginal-vaginal-vaginal were much more common in public compared with private hospitals which was mainly determined by a higher rate of index vaginal birth. Women with an index spontaneous vaginal birth showed a high probability of subsequent spontaneous vaginal births, irrespective of the initial birth setting. Women with an index instrumental or caesarean birth had a higher rate of a subsequent vaginal birth in public compared with private hospitals.
The strength of this study is that it is based on a large, complete population data set with established accuracy. This enabled us to compare mode of birth patterns up to three births between public and private settings.22,25 The study explores the prediction of index birth mode, including birth setting, on subsequent modes of birth. The large numbers allowed us to examine detailed patterns of modes of birth (including two and three births) and changes over the years and to compare these patterns between index births in private and public hospitals.
The methodology used, specifically conditional probability analyses, is a reliable approach for estimating the probability of various subsequent modes of birth following an index low-risk pregnancy and birth. This method provides valuable insights into what happens after the index birth in a low-risk nulliparous population by considering the life course approach. For example, the index birth could be related to subsequent adverse outcomes in later pregnancies and births. Therefore, it is not relevant for our approach to adjust for confounding factors. However, we acknowledge that factors such as socioeconomic status, cultural beliefs and personal preferences significantly influence the probability of either vaginal birth or CS. Our findings showed that women who gave birth in private settings had different characteristics compared with those in public settings; they were more likely to be highly educated, older, in a relationship, of Australian origin, and have a higher socioeconomic position. Although these differences could have influenced the mode of birth, we did not examine these factors. This means we cannot provide underlying reasons for the differences observed in modes of birth between public and private settings. Nevertheless, these differences were so substantial that it is unlikely they could be explained by demographic and clinical characteristics alone. In a previous linked data study, we found that even when accounting for the different characteristics of women and focusing only on low-risk women giving birth in the private and public sectors in Australia, intervention rates were much higher in the private sector.12 Other studies have found similar outcomes.9 29 Additionally, we did not examine differences in maternal and perinatal mortality rates. The study lacks the ability to differentiate between models of care (eg, midwife-led or obstetrician-led care). Furthermore, electronic health registry data on home births and other out-of-hospital births were not included in the analyses.
The modes of index birth and birth patterns (including two or three births) changed over time. In particular, subsequent elCS increased over the years in Australia. In contrast, birth patterns starting with an index spontaneous vaginal birth decreased in our study period. It is widely agreed that CS can be life-saving when used when indicated, but it can also put the lives of both mother and child at risk by disrupting normal physiological childbirth when used indiscriminately without medical indications.30 31 CSs are associated with a higher risk of morbidity during the course of subsequent pregnancies and adverse maternal health outcomes compared with vaginal births.32 It is also important to consider changes in obstetrical indications to apply birth interventions between 2001 and 2016, which are influenced by obstetrical studies and public policies. In addition, most women want a physiological labour and birth and the WHO guidelines on intrapartum care are based on this premise.33 34 Therefore, it is important to conduct further research into factors that might contribute to higher rates of CS in private settings, such as local guidelines, cultural norms and professional opinions and values. Moreover, it is important to benchmark rates of CS and pregnancy outcomes across health settings, regions and countries based on different categories of women as recommended by WHO.10 33 These comparisons show areas where CS is likely too high and maternity care can be improved.
To reduce the rate of CS, continuous support during labour has been valued and leads to fewer negative birth experiences as well.35 Watchful attendance by midwives comprises continuous support, clinical assessment and responsiveness to women’s needs.36 The term expresses a combination of continuous support, clinical assessment and responsiveness.
Our study and previous studies have shown that the rate of spontaneous vaginal birth after an instrumental index birth is high, though not as high as when women had a spontaneous vaginal birth in the index pregnancy.14 15 37 Furthermore, our findings revealed that women who had an index elCS had a very high probability of a subsequent elCS (81.9%), particularly if the funding model was private care (84.9%). This finding is consistent with a Brazilian population-based study, in which the overall rate of subsequent elCS was 85%, whereas in private care settings alone this was 96.1%.13 In the Netherlands, the rate of subsequent CS after an index CS (elective and emergency combined) among women at term was only 47.1%.38 A relatively high trial of labour rate after a previous CS is an important contributor to an overall lower national CS rate.38
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists have provided guidelines for subgroups of women, for whom vaginal birth after caesarean section (VBAC) is considered a safe option.39 The Australian Institute of Health and Welfare reported a slight decrease in the proportion of VBACs from 13% in 2007 to 12% in 2021, though it was significantly higher in public hospitals than private hospitals (14% vs 5.4%).3 A successful VBAC increases the chance of uncomplicated spontaneous vaginal birth in the future and is associated with a shorter recovery and hospital stay, as well as reduced abdominal pain and lower risks of respiratory disorders for the baby.40 This has implications for Australian women and health services, especially since the CS rate at the time of writing this paper was 38%, which is among the highest in the OECD.1 4 5 Given the importance of the index birth as a predictor of subsequent births, supporting safe spontaneous labour and vaginal birth could contribute to reducing excessively high CS rates. Even after an index CS, having supportive models of care for women can increase the success of VBAC. Such an approach can also improve the way women feel about their birth, regardless of the actual outcome.40
Women with an index elCS had the highest proportion of no further subsequent births, and this proportion was even higher if the initial birth setting was a public hospital compared with the private hospital. Our study confirms the results of previous Scandinavian population-based studies, which also reported higher proportions of no further subsequent births for women with an index elCS compared with other modes of birth.14 15 Further research is needed to explore why some women opt not to have another child after a CS, possibly due to factors like preferring one child, subfertility, fear of childbirth trauma or simply being older.15 This study raises an additional question for policy-makers around the world who are considering new approaches to the design and delivery of maternity care. As health systems come under increasing pressure, governments and health departments are trying to find ways of minimising costs and maximising outcomes.41 In some settings where healthcare has been largely publicly funded, there is debate about the acceptability and efficacy of private funding for some or all services.9 42 43 Our study indicates that decisions in maternity care should be made cautiously, considering the long-term health implications for mothers and babies as well as the subsequent costs and resource implications for the health sector.
Conclusions
In conclusion, in a population of low-risk Australian women with an index birth in the period 2001–2011, women labouring and giving birth in public hospitals had a higher proportion of spontaneous vaginal birth compared with those using private hospitals. Instrumental vaginal births and CSs (particularly elective) were less common. If a woman had an index spontaneous vaginal birth, the probability of her having a subsequent second and third spontaneous vaginal birth was high and remained so in subsequent pregnancies, no matter where they laboured and gave birth. These supported the hypothesis that index mode of birth may be a predictor for subsequent modes of birth. This may suggest that optimising the opportunity for a spontaneous vaginal first birth is an important public health strategy.
Recommendations
While the data in this study are specific to the Australian population, it is likely that they also hold true for other populations giving birth in similar contexts and settings. Our results are generalisable for women with a low-risk index pregnancy and birth; hence it is recommended that future studies replicate our methodology in populations with medium/high-risk pregnancies and births. Additionally, there is a value in benchmarking index births and birth patterns across nations, taking into account diverse maternity care models including their economic implications. In addition, it would be useful to gain insight into associations between the index birth and birth patterns on both positive and adverse maternal and perinatal health outcomes in the short and longer term.
supplementary material
Acknowledgements
We are grateful to the Centre for Health Data Linkage NSW Health (CHeReL) for their valuable support in supplying linked population datasets. We extend our gratitude to data scientist Viktor Bernal PhD from the University of Groningen (Centre for Information Technology) for his support in linking and coding the detailed birth patterns (two or three births). Finally, we want to thank our research assistants Wia Barkema MSc and Adriella van der Veen MSc, for their support in reviewing and editing the final draft of this manuscript.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2024-086212).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Data availability free text: The New South Wales linkage data used in this study are subject to privacy and legal considerations and are not publicly available as we do not have ethics approval to share data.
Collaborators: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Ethics approval: The data used for this study were routinely collected, deidentified and retrospective in nature. The study was approved by the Ethics Committee of the NSW Population and Health Services Research Committee (HREC/10/CIPHS/96). The committee agreed that consent could be waived due to the size of the dataset, anonymity of the data and retrospective nature of the data; therefore, there is minimal risk of identification of individuals.
Data availability statement
No data are available.
References
- 1.Amyx M, Philibert M, Farr A, et al. Trends in caesarean section rates in Europe from 2015 to 2019 using Robson’s Ten Group Classification System: A Euro-Peristat study. BJOG. 2024;131:444–54. doi: 10.1111/1471-0528.17670. [DOI] [PubMed] [Google Scholar]
- 2.Creanga AA, Syverson C, Seed K, et al. Pregnancy-Related Mortality in the United States, 2011-2013. Obstet Gynecol. 2017;130:366–73. doi: 10.1097/AOG.0000000000002114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian Institute of Health and Welfare . National core maternity indicators. Canberra: AIHW; 2024. [Google Scholar]
- 4.Australian Institute of Health and Welfare . Australia’s mothers and babies. Canberra: AIHW; 2024. [Google Scholar]
- 5.Seijmonsbergen-Schermers AE, van den Akker T, Rydahl E, et al. Variations in use of childbirth interventions in 13 high-income countries: A multinational cross-sectional study. PLoS Med. 2020;17:e1003103. doi: 10.1371/journal.pmed.1003103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liang J, Mu Y, Li X, et al. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: observational study of nearly seven million health facility births. BMJ. 2018;360:k817. doi: 10.1136/bmj.k817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . WHO recommendations: non-clinical interventions to reduce unnecessary caesarean sections. Geneva: WHO; 2018. https://www.who.int/publications/i/item/9789241550338 Available. [PubMed] [Google Scholar]
- 8.Jenabi E, Khazaei S, Bashirian S, et al. Reasons for elective cesarean section on maternal request: a systematic review. J Matern Fetal Neonatal Med. 2020;33:3867–72. doi: 10.1080/14767058.2019.1587407. [DOI] [PubMed] [Google Scholar]
- 9.Miller YD, Tone J, Talukdar S, et al. A direct comparison of patient-reported outcomes and experiences in alternative models of maternity care in Queensland, Australia. PLoS One. 2022;17:e0271105. doi: 10.1371/journal.pone.0271105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Betrán AP, Temmerman M, Kingdon C, et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018;392:1358–68. doi: 10.1016/S0140-6736(18)31927-5. [DOI] [PubMed] [Google Scholar]
- 11.Boerma T, Ronsmans C, Melesse DY, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392:1341–8. doi: 10.1016/S0140-6736(18)31928-7. [DOI] [PubMed] [Google Scholar]
- 12.Dahlen HG, Tracy S, Tracy M, et al. Rates of obstetric intervention and associated perinatal mortality and morbidity among low-risk women giving birth in private and public hospitals in NSW (2000-2008): a linked data population-based cohort study. BMJ Open. 2014;4:e004551. doi: 10.1136/bmjopen-2013-004551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dias BAS, Leal M do C, Esteves-Pereira AP, et al. Variations in cesarean and repeated cesarean section rates in Brazil according to gestational age at birth and type of hospital. Cad Saude Publica. 2022;38:S0102-311X2022000605011. doi: 10.1590/0102-311XPT073621. [DOI] [PubMed] [Google Scholar]
- 14.Elvander C, Dahlberg J, Andersson G, et al. Mode of delivery and the probability of subsequent childbearing: a population-based register study. BJOG. 2015;122:1593–600. doi: 10.1111/1471-0528.13021. [DOI] [PubMed] [Google Scholar]
- 15.Fussing-Clausen C, Geirsson RT, Hansen T, et al. Mode of delivery and subsequent reproductive patterns. A national follow-up study. Acta Obstet Gynecol Scand. 2014;93:1034–41. doi: 10.1111/aogs.12469. [DOI] [PubMed] [Google Scholar]
- 16.Gurol-Urganci I, Bou-Antoun S, Lim CP, et al. Impact of Caesarean section on subsequent fertility: a systematic review and meta-analysis. Hum Reprod. 2013;28:1943–52. doi: 10.1093/humrep/det130. [DOI] [PubMed] [Google Scholar]
- 17.Hemminki E. Impact of caesarean section on future pregnancy--a review of cohort studies. Paediatr Perinat Epidemiol. 1996;10:366–79. doi: 10.1111/j.1365-3016.1996.tb00062.x. [DOI] [PubMed] [Google Scholar]
- 18.O’Neill SM, Kearney PM, Kenny LC, et al. Caesarean delivery and subsequent pregnancy interval: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13:165. doi: 10.1186/1471-2393-13-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Zhou J, Ma Y, et al. Mode of delivery and preterm birth in subsequent births: A systematic review and meta-analysis. PLoS ONE. 2019;14:e0213784. doi: 10.1371/journal.pone.0213784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maine D. Monitoring emergency obstetric care: a handbook: World Health Organization. 2009.
- 21.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Centre for Health Record Linkage Quality assurance report 2012: cherel. 2014. https://www.cherel.org.au/media/24160/qa_report_2012-a.pdf Available.
- 23.Lain SJ, Hadfield RM, Raynes-Greenow CH, et al. Quality of data in perinatal population health databases: a systematic review. Med Care. 2012;50:e7–20. doi: 10.1097/MLR.0b013e31821d2b1d. [DOI] [PubMed] [Google Scholar]
- 24.Hadfield RM, Lain SJ, Cameron CA, et al. The prevalence of maternal medical conditions during pregnancy and a validation of their reporting in hospital discharge data. Aust N Z J Obstet Gynaecol. 2008;48:78–82. doi: 10.1111/j.1479-828X.2007.00818.x. [DOI] [PubMed] [Google Scholar]
- 25.Lam MK. How good is New South Wales admitted patient data collection in recording births? Health Inf Manag . 2011;40:12–9. doi: 10.1177/183335831104000302. [DOI] [PubMed] [Google Scholar]
- 26.Dahlen HG, Thornton C, Downe S, et al. Intrapartum interventions and outcomes for women and children following induction of labour at term in uncomplicated pregnancies: a 16-year population-based linked data study. BMJ Open. 2021;11:e047040. doi: 10.1136/bmjopen-2020-047040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peters LL, Thornton C, de Jonge A, et al. The effect of medical and operative birth interventions on child health outcomes in the first 28 days and up to 5 years of age: A linked data population-based cohort study. Birth. 2018;45:347–57. doi: 10.1111/birt.12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lucas P, Gaag L. Chapter 2: Conditional probabilities and Bayes Theorem.: Intelligent Systems - an introductory AI course. https://www.cs.ru.nl/~peterl/teaching/DM/intro-prob2.pdf Available.
- 29.Yu S, Fiebig DG, Viney R, et al. Private provider incentives in health care: The case of caesarean births. Soc Sci Med. 2022;294:S0277-9536(22)00032-6. doi: 10.1016/j.socscimed.2022.114729. [DOI] [PubMed] [Google Scholar]
- 30.Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet. 2016;388:2176–92. doi: 10.1016/S0140-6736(16)31472-6. [DOI] [PubMed] [Google Scholar]
- 31.Çalik KY, Karabulutlu Ö, Yavuz C. First do no harm - interventions during labor and maternal satisfaction: a descriptive cross-sectional study. BMC Pregnancy Childbirth. 2018;18:415. doi: 10.1186/s12884-018-2054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018;15:e1002494. doi: 10.1371/journal.pmed.1002494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Betran AP, Torloni MR, Zhang JJ, et al. WHO Statement on Caesarean Section Rates. BJOG. 2016;123:667–70. doi: 10.1111/1471-0528.13526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kingdon C, Downe S, Betran AP. Non-clinical interventions to reduce unnecessary caesarean section targeted at organisations, facilities and systems: Systematic review of qualitative studies. PLoS One. 2018;13:e0203274. doi: 10.1371/journal.pone.0203274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bohren MA, Hofmeyr GJ, Sakala C, et al. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;7:CD003766. doi: 10.1002/14651858.CD003766.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Jonge A, Dahlen H, Downe S. “Watchful attendance” during labour and birth. Sex Reprod Healthc. 2021;28:S1877-5756(21)00024-0. doi: 10.1016/j.srhc.2021.100617. [DOI] [PubMed] [Google Scholar]
- 37.Lurie S, Steinberg N, Tannus S, et al. Mode of delivery in a subsequent pregnancy following previous instrumental delivery. J Perinat Med. 2013;41:283–6. doi: 10.1515/jpm-2012-0104. [DOI] [PubMed] [Google Scholar]
- 38.Zhang J, Geerts C, Hukkelhoven C, et al. Caesarean section rates in subgroups of women and perinatal outcomes. BJOG. 2016;123:754–61. doi: 10.1111/1471-0528.13520. [DOI] [PubMed] [Google Scholar]
- 39.Labour and Birth Clinical Governance Group Vaginal birth after caesarean (VBAC): women’s health. 2017. https://www.nationalwomenshealth.adhb.govt.nz/assets/Womens-health/Documents/Policies-and-guidelines/Vaginal-Birth-After-Caesarean-VBAC.pdf Available.
- 40.Keedle H, Peters L, Schmied V, et al. Women’s experiences of planning a vaginal birth after caesarean in different models of maternity care in Australia. BMC Pregnancy Childbirth. 2020;20:381. doi: 10.1186/s12884-020-03075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Jonge A, Downe S, Page L, et al. Value based maternal and newborn care requires alignment of adequate resources with high value activities. BMC Pregnancy Childbirth. 2019;19:428. doi: 10.1186/s12884-019-2512-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duckett S. Commentary: The Consequences of Private Involvement in Healthcare - The Australian Experience. Healthc Policy. 2020;15:21–5. doi: 10.12927/hcpol.2020.26228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mann N. NHS privatisation is real. BMJ. 2022;379:2668. doi: 10.1136/bmj.o2668. [DOI] [PubMed] [Google Scholar]