Abstract
Torsion of uterine leiomyoma is a rare, albeit life-threatening surgical emergency. A 55-year-old woman presented with right iliac fossa pain persisting for the past 15 days, accompanied by nausea and vomiting. Imaging revealed a torsed subserosal pedunculated uterine leiomyoma, which caused ovarian torsion and ipsilateral ureterohydronephrosis. The case was managed surgically, and the diagnosis confirmed intraoperatively as well as through histopathology.
Keywords: Fibroid torsion, Ovarian torsion, MRI, Surgery
Introduction
Uterine leiomyomas are benign gynecological tumors of the female genital tract, commonly observed in women of childbearing age, with an incidence of 20%–40% [1]. Complications such as red degeneration, infection, expulsion of a submucous pedunculated myoma, or torsion of a pedunculated subserosal myoma typically cause acute-onset severe abdominal pain. Nonetheless, torsion of a pedunculated uterine leiomyoma is exceedingly uncommon, with a documented incidence of less than 0.25% [2]. This condition is considered an emergency due to the potential for reactive peritonitis and ischemic gangrene [3]. Since diagnosing a twisted pedunculated leiomyoma based solely on clinical findings is challenging, careful use of radiological imaging becomes essential tool for an accurate diagnosis [4]. This case report describes the imaging findings in a case of a torsed, pedunculated, subserosal uterine leiomyoma.
Case report
A 50-year-old multiliparous woman presented to the emergency department with 10-days history of intermittent diffuse lower abdominal pain, predominantly on the right side. She had a medical history of uterine leiomyoma. There were no symptoms related to the urinary or gastrointestinal tract, and her vital signs were stable with no fever. Physical examination revealed noticeable pain in the lower right abdomen. Laboratory data showed a white blood count of 10000, hemoglobin of 12 g/dl, C-reactive protein of 0.6 mg/l, and a negative pregnancy test.
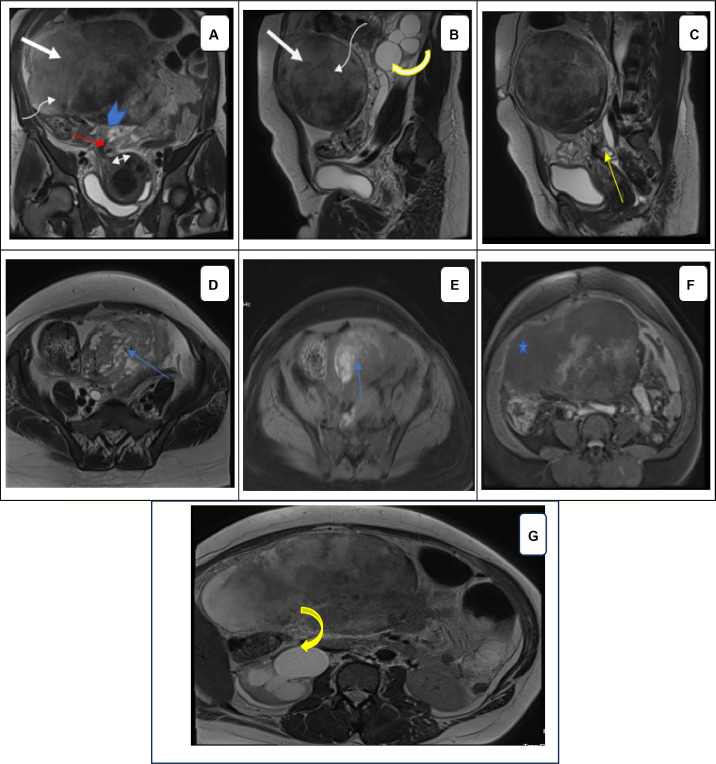
Ultrasonography was inconclusive due to a large abdominopelvic mass causing significant posterior attenuation. The patient refused a transvaginal ultrasound. Due to intractable pain, MRI was performed, revealing a pedunculated, solid abdominopelvic mass continuous with the uterus in the region of the right cornua (Fig. 1A). T2-weighted images showed flow voids at the site of the uterine attachment, indicating the ‘bridging vessel sign’. The mass appeared isointense to the myometrium on T1WI and heterogeneously hyperintense on T2-weighted images with no diffusion restriction. Postcontrast images showed the majority of the mass was nonenhancing with a thin enhancing rim and a small eccentric area of heterogeneous enhancement. The thickened and twisted appearance of the pedicle of a subserosal fibroid, forming a spiral, resulted in right ovarian torsion. The right ovary was enlarged with a heterogeneous T2 signal, containing follicles arranged peripherally, creating a “string of pearls” appearance. Additionally, areas in the ovarian stroma demonstrated hyperintensity on T1 and T2, indicative of hemorrhagic zones. The right pelvic ureter was caught at the twisted pedicle, leading to ipsilateral ureterohydronephrosis (Figs. 1B and G). Based on the clinical and imaging findings, a diagnosis of a torsed subserosal uterine leiomyoma was suggested (Fig. 1).
Fig. 1.
MR imaging in torsion of a subserosal uterine leiomyoma. MR images depict: A large solid abdominal mass (arrow in A, B) continuous with the uterus through a broad pedicle (arrowhead in A) at in the region of the right cornua (double arrow in A). The mass appears heterogeneous on sagittal (B) and coronal (A) T2-weighted images compared to the uterine myometrium. The majority of the mass appears heterogeneously hyperintense on the T2-weighted image (curved arrow in A, B) with an absence of enhancement following contrast material injection (⋆ in F) There is a thin enhancing rim and a small eccentric area of heterogeneous enhancement adjacent to its site of attachment to the uterus. The thickened and twisted appearance of the pedicle of a subserosal fibroid, forming a spiral (red arrow in A) resulted in right ovarian torsion (D, E). The right ovary shows an increased size with a heterogeneous T2 signal, containing follicles arranged peripherally, creating a “string of pearls” appearance. Additionally, there are areas in the ovarian stroma demonstrating hyperintensity on T1 with fat suppression and T2WI (blue arrow in D, E) indicative of hemorrhagic zones. The right pelvic ureter is caught at the twisted pedicle (yellow arrow), leading to ipsilateral ureterohydronephrosis (yellow curved arrow in B, G).
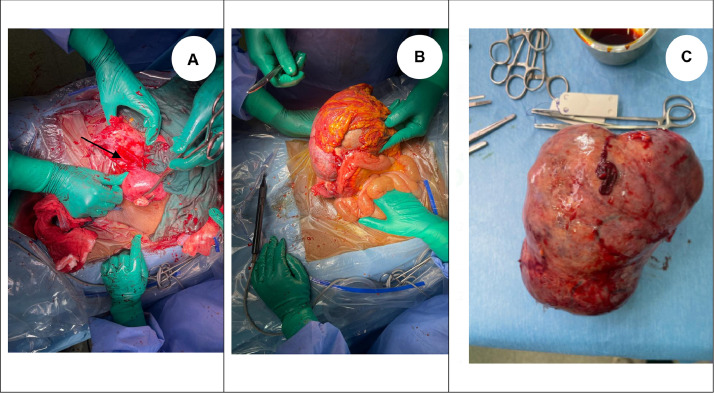
The patient was counseled, written informed consent was obtained, and exploratory laparotomy was performed. Intraoperatively, moderate ascites was found along with a large necrotic pedunculated fibroid, which was twisted and involving the right ovary (Fig. 2). The right ovary was also twisted and necrotic. The patient underwent a total hysterectomy with right annexectomy after resection of the necrotic pedunculated fibroid, which was subsequently sent for histopathological examination.
Fig. 2.
Intraoperatively, the mass was found to be a large subserosal uterine fibroid with a twisted vascular pedicle (arrow in a), involving the right ovary, which was also twisted and necrotic. The patient underwent a total hysterectomy with right annexectomy after resection of the necrotic pedunculated fibroid.
Discussion
Sixty percent of women in their reproductive years have uterine fibroids, also known as leiomyomas, which are benign smooth-muscle neoplasms and the most common gynecologic tumors [3]. Simple fibroids are frequently asymptomatic, however when symptomatic, they can cause infertility, menorrhagia, dysmenorrhea, and abdominal pain. Severe complications include torsion, degeneration, intraperitoneal hemorrhage, prolapse of submucosal fibroids, acute urine retention, and venous thrombosis [5]. Torsion of a uterine leiomyoma is an uncommon cause of acute abdomen, with a reported incidence of 0.25% in complex fibroids requiring surgery, as noted in a single-center retrospective study. As demonstrated in this case study, pedunculated subserosal fibroids are most susceptible to torsion, especially when the stalk is long and thin [2].
US, as the primary imaging modality of choice for the assessment of acute pelvic pain, can identify a subserosal leiomyoma but not its torsion [6]. A simple fibroid usually appears as a hypoechoic lesion that may be well-defined and arises within the surrounding myometrium [7]. Torsion of a subserosal leiomyoma may be suspected when color Doppler demonstrates a twisted pedicle or when there is a space between the leiomyoma and the uterus. However, US may not be effective, especially when the twisted pedicle is thin and invisible, or posterior attenuation hinders the examination, as in the case of our patient.
In cases where ultrasound findings are inconclusive, an MRI is conducted due to its higher sensitivity and specificity. The vascular pedicle of a subserosal leiomyoma is better visualized on MRI, presenting as T2 flow voids at the interface between the uterus and the mass, indicative of the 'bridging vessel sign.' This suggests a uterine origin of the mass, differentiating it from an adnexal mass. In this instance, the attachment site of the pedicle with the uterus was clearly observed on MRI (Fig. 1). It is crucial to distinguish normal ovaries from the mass [8]. Uncomplicated leiomyomas typically appear homogeneously hypointense on T1 and T2 weighted images.
On the contrary, twisted leiomyomas undergo necrosis and gangrene, displaying heterogeneous hyperintensity on T2-weighted images and intermediate to hyperintense signals on T1-weighted images, corresponding to ischemia and hemorrhagic necrosis, respectively. Diffusion restriction on diffusion-weighted images can be observed (though not in this case). Postcontrast images reveal a thin enhancing rim with a lack of enhancement within the mass (as shown in Fig. 1F in this case). The nonenhancing core is consistent with necrosis, while the regular rim of enhancement corresponds to obstructed peripheral veins with edema [9]. Ascites is a frequently associated finding seen in the majority of cases. The 'dark fan sign,' described as a fan-shaped area of poor contrast enhancement in the uterus adjacent to the torsed [10].
Ovarian torsion and leiomyoma with secondary degeneration are common differential diagnoses. In leiomyoma, degeneration occurs more frequently than torsion. Although there is acute pain initially, the clinical presentation is not as alarming. It should be distinguished from torsion since degeneration does not require immediate surgical intervention. Fibroid degeneration is known to occur in various forms. An enlarged edematous ovary showing peripherally displaced follicles with or without hemorrhagic infarction is a characteristic feature. Common CT and MRI of ovarian torsion include fallopian-tube thickening, smooth-wall thickening of twisted adnexal lesions, ascites, and ipsilateral uterine deviation [11]. In our case, the pedicle of the subserosal uterine fibroid was twisted, creating the appearance of a whirlpool sign, leading to ovarian torsion with compression of the ipsilateral pelvic ureter, a finding not previously reported on MRI to the best of our knowledge.
Surgery is also ideal treatment for twisted pedunculated subserosal uterine leiomyomas. Myomectomy, which can be performed via laparoscopy or laparotomy, is the preferred therapy option for pedunculated subserosal leiomyomas in women of reproductive age [12]. For our patient, we opted for a total hysterectomy with right annexectomy. After obtaining the patient's consent, she did not report any postoperative complications (Fig. 2).
Conclusion
Although rare, torsion of a pedunculated subserosal leiomyoma must be considered in females presenting with acute onset lower abdominal pain. The diagnosis should be based on clinical presentations and imaging findings. Torsion of the leiomyoma is a surgical emergency, as delays in treatment may lead to significant morbidity. Once suspected, a gynecologist must be consulted, and surgical intervention should be considered.
Patient consent
Written informed consent for publication was obtained from patient.
Footnotes
Acknowledgments: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Competing Interests: All authors declare no conflict of interest.
References
- 1.Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current perspectives. Int J Womens Health. 2014;6:95–114. doi: 10.2147/IJWH.S51083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lai YL, Chen YL, Chen CA, Cheng WF. Torsion of pedunculated subserous uterine leiomyoma: a rare complication of a common disease. Taiwan J Obstet Gynecol. 2018;57:300. doi: 10.1016/j.tjog.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 3.Le D, Dey CB, Byun K. Imaging findings of a torsed pedunculated uterine leiomyoma: a case report. Radiol Case Rep. 2019;15:144–149. doi: 10.1016/j.radcr.2019.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Costa MDL, Cunha TM. Torsion of a pedunculated subserous leiomyoma: a case report of a rare cause of acute abdominal pain in a pregnant woman. Egypt J Radiol Nucl Med. 2020;51:147. doi: 10.1186/s43055-020-00269-0. [DOI] [Google Scholar]
- 5.Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):609–617. 10.1016/j.bpobgyn.2009.01.012 [PubMed] [Google Scholar] [DOI] [PubMed]
- 6.Wilde S, Scott-Barrett S. Radiological appearances of uterine fibroids. Indian J Radiol Imaging. 2009;19(03):222–231. doi: 10.4103/0971-3026.54887. [PMC free article] [PubMed] [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roy C, Bierry G, El Ghali S, Buy X, Rossini A. Acute torsion of uterine leiomyoma: CT features. Abdom Imaging. 2005;30:120–123. doi: 10.1007/s00261-004-0240-1. [DOI] [PubMed] [Google Scholar]
- 8.Torashima M, Yamashita Y, Matsuno Y, Takahashi M, Nakahara K, Onitsuka Y, et al. The value of detection of flow voids between the uterus and the leiomyoma with MRI. J Magn Reson Imaging. 1998;8(2):427–431. doi: 10.1002/jmri.1880080224. PMID: 9562071. [DOI] [PubMed] [Google Scholar]
- 9.Ueda H, Togashi K, Konishi I, Kataoka ML, Koyama T, Fujiwara T, et al. Unusual appearances of uterine leiomyomas: MR imaging findings and their histopathologic backgrounds. Radiographics. 1999;19(suppl_1):S131–S145. doi: 10.1148/radiographics. PMID: 10517450. [DOI] [PubMed] [Google Scholar]
- 10.Yamashita S, Fujikawa H, Yoshizawa T. A rare cause of acute abdomen: torsion of subserous uterine fibroid in a postmenopausal woman. Balkan Med J. 2022;39(5):378–379. doi: 10.4274/balkanmedj.galenos.2022.2022-4-98. [PMC free article] [PubMed] [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dawood MT, Naik M, Bharwani N, Sudderuddin SA, Rockall AG, Stewart VR. Adnexal torsion: review of radiologic appearances. Radiographics. 2021;41(2):609–624. doi: 10.1148/rg.2021200118. [PubMed] [Google Scholar] [DOI] [PubMed] [Google Scholar]
- 12.Donnez J, Dolmans MM. Uterine fibroid management: from the present to the future. Hum Reprod Update. 2016;22(6):665–686. doi: 10.1093/humupd/dmw023. [PMC free article] [PubMed] [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]