Abstract
BACKGROUND
The healthcare industry carbon footprint is 5.2% of total CO2 equivalent emissions worldwide. The operating rooms are the most resource demanding areas in hospital care and the higher energy demands, lack of effective waste management, and inhaled anaesthetic use, lead to a high carbon footprint. There is wide variation in the carbon footprint of inhaled gases, with desflurane ranking 40 times higher than sevoflurane. Other inhaled agents, including N2O and isoflurane, have additional ozone-depleting properties.
OBJECTIVE
To describe what factors influence the implementation of sustainable anaesthetic strategies.
DESIGN
An international survey.
SETTING
Anaesthesia clinicians worldwide between April 2021 and April 2022.
PARTICIPANTS
One thousand two hundred and thirty-seven anaesthesia clinicians from 75 countries.
MAIN OUTCOME MEASURES
The primary outcome was a determination of the most used anaesthetic plans among anaesthesia practitioners. Secondary outcomes included an assessment of the influence of various socioeconomic variables on anaesthetic decision-making, and on the level of the practitioners’ awareness of peri-operative environmental sustainability.
RESULTS
Sixty-four percent of respondents use inhaled anaesthetics on a daily basis, with 83% preferring sevoflurane, and only 5% using N2O regularly. Forty-five percent do not know which halogen gas has the highest carbon footprint. Fifty-one percent do not use low flow anaesthesia regimes (<1.0 l min-1) due to concerns about CO2 rebreathing (30%), hypoxia (25%), compound A related renal failure (12%) or CO generation (10%). Only 15% use minimal flow anaesthesia (<0.5 l min-1). There is a correlation between higher income countries and implementation of more sustainable strategies, probably due to better access to updated technology and sustainability education programmes. Desflurane is used in 6 to 12% of the cases regardless of the GDP index.
CONCLUSIONS
Halogen gases are the most frequently used anaesthetic drugs worldwide. The majority of respondents are unaware of their global warming impact, or are not influenced in their anaesthetic choices by environmental concerns. More sustainable alternatives of anaesthesia are under-implemented, and vary significantly among countries depending on their GDP index. Further education and training in sustainability is needed.
KEY POINTS
Worldwide, a significant number of anaesthesiologists are unaware of their daily carbon footprint.
Inhaled anaesthetics have different levels of global warming potential, and are the most frequently used anaesthetic drugs worldwide.
High-income countries have better access to technology that provides for more environmentally sustainable care.
Raising awareness and improving education, despite differences in national socioeconomic backgrounds, is essential to reduce the peri-operative carbon footprint.
Introduction
Anthropogenic Green House Gas (GHG) emissions have continued to rise rapidly in the last decade1 in spite of increased public and political awareness of climate change. Even though the COVID-19 pandemic resulted in a temporary drop of fossil fuel and industry emissions in the first half of 2020, they rebounded by the second half of 2020.2 The Intergovernmental Panel on Climate Change (IPCC) report states a likely exceedance of global temperatures above 1.5°C by 2030. Therefore, a significant reduction of GHG emissions in the upcoming century is urgently needed.3,4 Healthcare contributes to global net emissions with a share of 4.7% in the European Union, which ranks as the third largest contributor to the global healthcare industry footprint, with a share of 12% after the United States (27%) and China (17%).5,6 As rising planetary temperatures are one of the biggest threats to health this century,7 healthcare systems should have an intrinsic motivation to lead by example.
Volatile anaesthetic agents have been estimated to be responsible for 0.01 to 0.10%8–10 of total global carbon dioxide equivalent (CO2e) emissions contributing to global warming. On the basis of atmospheric sampling of volatile anaesthetics, their accumulation is increasing, particularly desflurane,10–13 which has the highest warming potential among all anaesthetic gases.10 Although these are a seemingly small contribution to total global emissions, inhaled anaesthetics account for 5% of acute hospital CO2e emissions, and up to 50% of peri-operative department emissions in high-income countries.10–13 Use of these anaesthetics is directly within the control of anaesthesia providers, with often more sustainable alternatives available. Thus, environmental stewardship is an important opportunity for GHG mitigation and professional sustainability leadership.10 A significant global variability exists in anaesthetic practice due to differences in the socioeconomical, infrastructural, and medical situation, which might compromise sustainability programmes for anaesthesia.
There are only a handful of surveys14–18 addressing the impact of peri-operative practice on sustainability, circumscribed on a national level. Therefore, the main objective of this questionnaire is to benchmark anaesthetic practice worldwide in order to determine its potential impact on sustainability, and the need to increase education programmes. Moreover, we wanted to assess the influence of socioeconomic variables in our anaesthetic practice, and the potential influence in sustainability outcomes.
Materials and methods
We obtained prospective ethical approval for our survey (Ethical Committee No. PI-4630) from La Paz University Hospital Ethics Committee, Madrid, Spain (Chairperson Prof A. Castro Conde) on 23 March 2021.
The European Society of Anaesthesia and Intensive Care (ESAIC) and the Spanish Society of Anaesthesia and Critical Care (SEDAR) endorsed the survey in June 2021. Both institutions validated the questions asked, and provided feedback for this survey.
The questionnaire was preceded by a short text explaining that the survey was being conducted under ESAIC purview and General Data Protection Regulation (GDPR) protection. Consent was implied with survey completion.
The survey is an international cross-sectional study, distributed online over one year (April 2021 to April 2022) by different ways and means in order to reach anaesthesiologists worldwide (Supplementary File 1). Once the link was received, the respondent was allowed to anonymously answer the questionnaire, which was available in English and Spanish. Incomplete or repeated surveys were discarded as invalid answers.
The survey consisted of 14 sustainability questions, and seven more to assess demographic data. We gathered opinions from anaesthesiologists (residents and specialists), anaesthesia nurses and veterinary anaesthesiologists about their choice of anaesthetic agents, use of low-flow anaesthesia and anaesthetic carbon footprint awareness (full questionnaire available in Supplementary File 2). Questions 1 to 3 enquired about anaesthetic agent choice. Questions 4 to 9 asked about low flow anaesthesia and the potential risks involved. Questions 10 to 14 gathered information about the carbon footprint of anaesthesia. Questions 15 to 21 collected demographic data.
Data obtained from this survey were geographically distributed by continents and cross-matched against three different World Development Indicators from the World Bank Database: CO2 emissions (metric tons per capita), Gross Domestic Product (GDP per capita: current US$) and current health expenditure (% of GDP). In order to compensate for sampling bias from under-represented regions, we aggregated countries into continents, and distributed their socioeconomic results into quintiles. Thus, comparisons are based on groups of countries with similar geographical and socioeconomic indices, instead of on purely national basis (Supplementary Tables 1S, 2S and 3S).
Statistical analysis
Data were processed using the SAS programme, version 9.4 (SAS Institute Inc. 2013, Cary, North Carolina, USA). Incomplete answers were discarded. Statistically significant differences were considered with a probability of error less than 5% (P < 0.05). For the description of continuous quantitative variables, mean value was used together with standard deviation. Qualitative variables were described by absolute frequencies, and relative frequencies expressed as a percentage. Comparisons between continuous quantitative variables among independent groups were assessed using Student's t-test, or ANOVA when the analysis involved three or more groups. Statistical significance was obtained using nonparametric tests, Kruskal--Wallis or Mann--Whitney U when, in absence of normal distribution, use of discontinuous quantitative variables, or when stratification of subgroups implied a sample size of less than 30 individuals. The analysis of frequencies between qualitative variables was carried out using the Chi-square test (with Yates’ correction) or Fisher's exact test when necessary.
Results
One thousand two hundred and eighty-five online responses were received between April 2021 and April 2022 from 75 different countries. Forty-eight responses were not valid due to missing values (96% valid rate).
Among respondents, 878 (71%) were anaesthesiologists (consultant level), 219 (18%) anaesthesia residents, 7 (1%) anaesthesia nurses, 97 (8%) shared management and clinical duties (chairperson or section chief), and 36 (3%) were veterinary anaesthesiologists. The survey was completed by 657 men (53%), 572 women (46%) and eight respondents who preferred not to declare sex (1%). Age had a pyramidal representation with fewer responses in both extreme groups. One thousand and fifty-four (85%) of responses came from Europe and South America (Table 1). Seven hundred and fifty-five (61%) of respondents worked in countries with a GDP higher than p50.
Table 1.
Survey demographics
| Age | Percentage | Number | |
| < 25 | 0.2 | 3 | |
| 25 to 29 | 8.7 | 108 | |
| 30 to 39 | 30.2 | 374 | |
| 40 to 49 | 24.9 | 308 | |
| 50 to 59 | 23.4 | 290 | |
| > 60 | 12.4 | 154 | |
| Unit | |||
| Day surgery | 7.6 | 94 | |
| General surgery, urology & ENT | 43.9 | 546 | |
| Neurosurgery | 4.2 | 52 | |
| Cardiothoracic surgery | 7.3 | 91 | |
| Paediatric surgery | 13.5 | 168 | |
| OB / GYN surgery | 4.8 | 60 | |
| Trauma & Orthopaedics surgery | 8.0 | 99 | |
| Research & experimental surgery | 0.2 | 3 | |
| Veterinary clinic | 3.2 | 40 | |
| Other | 6.8 | 85 | |
| Sex | |||
| Male | 53 | 658 | |
| Female | 46 | 572 | |
| Prefer not to say | 1 | 8 | |
| Role | |||
| Resident/Fellow | 17.6 | 219 | |
| Consultant | 70.6 | 878 | |
| Managers | 8.0 | 97 | |
| Anaesthesia nurse | 0.6 | 7 | |
| Veterinary anaesthesiologist | 3.2 | 40 | |
| Years of experience | |||
| < 5 | 18.6 | 232 | |
| 5 to 9 | 16.7 | 208 | |
| 10 to 14 | 14.5 | 180 | |
| 15 to 19 | 10.9 | 136 | |
| 20 to 25 | 15.6 | 194 | |
| > 25 | 23.2 | 288 | |
| Geographic distribution | |||
| Europe | 59 | 735 | |
| South America | 26 | 320 | |
| North America | 6 | 80 | |
| Middle East | 3 | 38 | |
| Asia | 2 | 22 | |
| Africa | 2 | 21 | |
| Central America | 1 | 12 | |
| Australia & New Zealand | < 1 | 9 | |
Type of anaesthesia
Sixty-four percent of the respondents preferred inhaled anaesthetics and 23% total intravenous anaesthesia (TIVA), with the latter being more frequently used by experienced anaesthesiologists than by less experienced clinicians (P < 0.01). The remaining 13% used other options on a common basis. Interestingly, veterinary surgery (85%), general surgery (73%), paediatric surgery (72%) and cardiothoracic surgery (70%) are the areas wherein inhaled anaesthetics are used most frequently, whereas neurosurgery (48%) is the area where TIVA is most commonly used (Figure 1S). Supplemental Figure 2S, shows anaesthetic preference according to clinical role (P < 0.001).
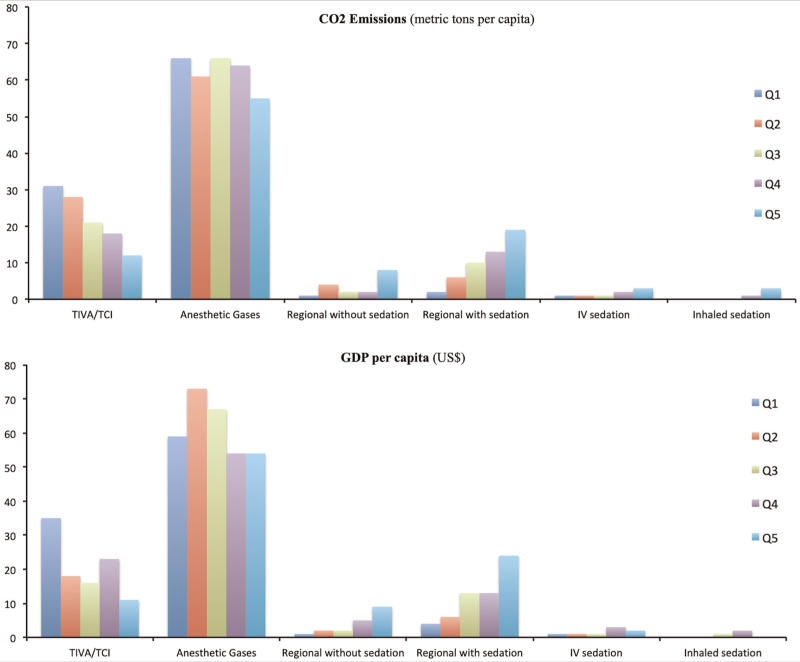
With regards to the geographic distribution of preferences (Table 2), inhaled anaesthetics are the preferred option worldwide, and have the highest use rate in Africa. According to our data, Central America is the region where inhaled anaesthetics are used the least (P < 0.001) (Supplemental figure 3S). Interestingly, if we filter our results per national CO2 emissions criteria, we observe that the preference for inhaled anaesthetics is similar across the board (55–65% preference in all quintiles), whereas TIVA is used mostly in countries with a higher CO2 footprint (P < 0.001), and regional anaesthesia with sedation is used more in less CO2 emitting countries (P < 0.001). The same pattern arises if the data are filtered per GDP per capita (Fig. 1) and health expenditure (% of GDP).
Table 2.
What anaesthetic plan do you use more often?
| Data in % | TIVA | Anaesthetic gases | Regional without sedation | Regional with sedation | i.v. sedation | Inhaled sedation | Number |
| Europe | 27 | 65 | 2 | 6 | 1 | 0.5 | 736 |
| North America | 16 | 76 | 1 | 5 | 1 | 0 | 80 |
| South America | 18 | 60 | 3 | 16 | 2 | 2 | 319 |
| Central America | 8 | 33 | 17 | 33 | 8 | 0 | 12 |
| Africa | 5 | 81 | 5 | 10 | 0 | 0 | 21 |
| Middle East | 16 | 74 | 5 | 5 | 0 | 0 | 38 |
| Asia | 9 | 77 | 0.0 | 14 | 0 | 0 | 22 |
| Australia & New Zealand | 22 | 56 | 11 | 11 | 0 | 0 | 9 |
| Number | 278 | 796 | 31 | 110 | 14 | 8 | 1237 |
Preferred anaesthetic plan according to geographical region represented in percentages with absolute numbers in the last column and row.
i.v., intravenous.
Fig. 1.
Anaesthetic plan preference according to CO2 emissions and GDP per capita. Data expressed in percentages.
The upper graph shows the anaesthetic preference according to CO2 emissions (metric tons per capita). The lower graph shows anaesthetic preference according to GDP per capita in each country. In order to compensate for sampling bias from under-represented regions, we aggregated countries into quintiles (Q1-Q5) of a given value: CO2 emissions in the upper graph and GDP per capita in the lower graph. Thus, comparisons are based on groups of countries with similar socioeconomic indices (P < 0.001).
Type of anaesthetic agent
Among those using inhaled anaesthetics, 83% preferred sevoflurane, 10% desflurane and 6% isoflurane in their clinical practice. Desflurane is most used in cardiothoracic (18%), otolaryngologic and general surgery combined (12%), and preferred by anaesthesiologists in management positions (20%). On the contrary, desflurane is seldom selected in neurosurgery (6%) or paediatric anaesthesia (3%), and was not used in this survey by anaesthesia nurses (0%), research anaesthesiologists (0%) or veterinarians (0%). This information is summarised in supplemental Figures 4S and 5S.
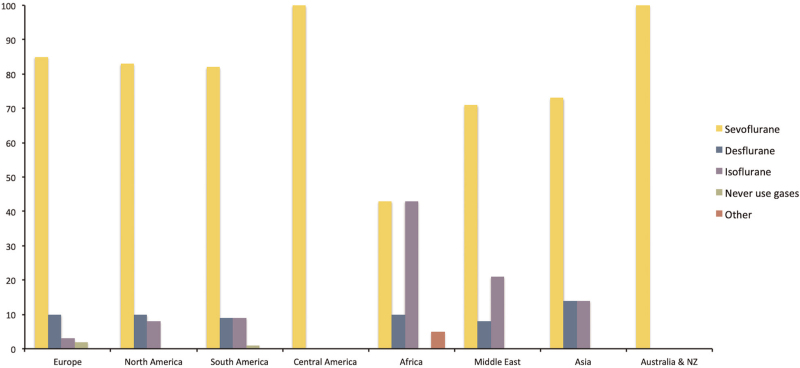
Sevoflurane is the most frequently preferred anaesthetic gas worldwide except in Africa, where its use (43%) equals isoflurane (43%). Interestingly, desflurane maintains a 10% use in this continent as well (P < 0.001) (Table 3 and Fig. 2). There is little correlation between the national CO2 footprint and the use of anaesthetic gas. There is a slightly higher isoflurane consumption (15%) in countries with fewer CO2 emissions per capita, whereas sevoflurane is more often used in countries that produce more CO2per capita. Desflurane shows a constant preference across the board (6 to 12%) regardless of the level of CO2 production per capita.
Table 3.
What anaesthetic gas do you use more often?
| Data in % | Sevoflurane | Desflurane | Isoflurane | Never use gases | Other | Number |
| Europe | 85 | 10 | 3 | 2 | 0 | 736 |
| North America | 83 | 10 | 8 | 0 | 0 | 80 |
| South America | 82 | 9 | 9 | 1 | 0 | 319 |
| Central America | 100 | 0 | 0 | 0 | 0 | 12 |
| Africa | 43 | 10 | 43 | 0 | 5 | 21 |
| Middle East | 71 | 8 | 21 | 0 | 0 | 38 |
| Asia | 73 | 14 | 14 | 0 | 0 | 22 |
| Australia & NZ | 100 | 0 | 0 | 0 | 0 | 9 |
| Number | 1021 | 119 | 77 | 19 | 1 | 1237 |
Preferred anaesthetic gas according to geographical region represented in percentages with absolute numbers in the last row and column.
Fig. 2.
Anaesthetic gas preference according to region. Data expressed in percentages (P < 0.001).
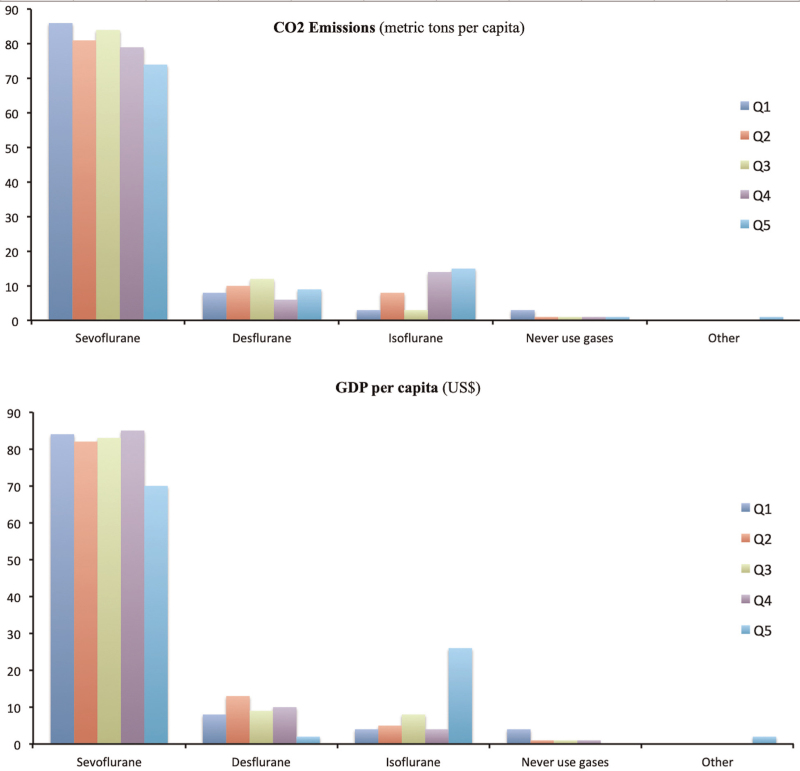
These differences are also shown when analysing GDP and health expenditure (P < 0.001), with a higher isoflurane use in countries with the least GDP and healthcare expenditure per capita (26 and 19%, respectively). There is less desflurane use only in countries that belong to the lowest GDP quintile: 2 versus 10% average use in countries in the top four quintiles. Information regarding anaesthetic gas preference according to CO2 emissions and GDP is summarised in Fig. 3.
Fig. 3.
Anaesthetic gas preference according to CO2 emissions (metric tons per capita) and GDP per capita in each country. Data expressed in percentages.
The upper graph shows the anaesthetic gas preference according to CO2 emissions (metric tons per capita). The lower graph shows anaesthetic gas preference according to GDP per capita in each country. In order to compensate for sampling bias from under-represented regions, we aggregated countries into quintiles (Q1-Q5) of a given value: CO2 emissions in the upper graph and GDP per capita in the lower graph. Thus, comparisons are based on groups of countries with similar socioeconomic indices (P < 0.001).
Regarding N2O, 5% use it on a regular basis and 95% mix oxygen with air. Middle East (21%) and Africa (10%) are the regions in the world where N2O is most used. There is also a correlation between lower CO2 emissions per capita (p10) and higher N2O use (19%) (P < 0.05). Regarding which anaesthetic gas is considered the most pollutant to the atmosphere, 53% of respondents answered desflurane, 11% isoflurane, 7% sevoflurane and 29% did not to know.
Fresh gas flow
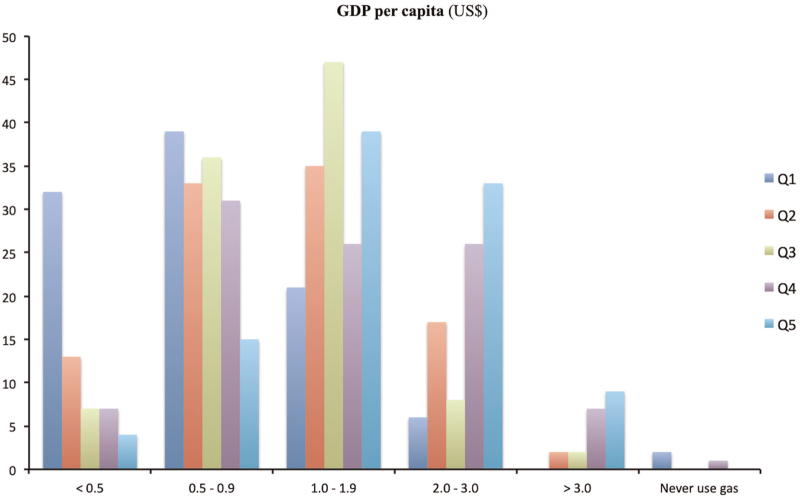
Forty-nine percent of the respondents use low flow anaesthesia (FGF < 1.0 lpm) when inhaled anaesthetics are being used, and only 15% of anaesthesiologists use minimal flow anaesthesia (FGF <0.5 lpm). Regions where a FGF less than 0.5 lpm is used more often are Australia and New Zealand (44%), North America (19%) and Europe (18%) (P < 0.001). Interestingly, there is a clear correlation in which countries with higher rates of CO2 emissions, higher GDP per capita and higher healthcare expenditure per capita are more prone to apply lower FGF rates (P < 0.001), whereas higher FGF rates (>2.0 lpm) are more common in low-income countries (Fig. 4).
Fig. 4.
Fresh gas flow preference according to GDP per capita. Data expressed in percentages.
Countries are stratified into GDP quintiles. Anaesthesiologists working in countries in the first quintile in GDP per capita tend to use lower fresh gas flows than fellow colleagues working in countries with less GDP per capita (P < 0.001).
Reasons to avoid low flow anaesthesia were concerns for CO2 rebreathing (30%), hypoxia (25%), compound A related renal insufficiency (12%) and CO formation (10%). Interestingly, 36% of respondents answered that they did not foresee any risks during low flow anaesthesia. Regarding question number 7, 66% of anaesthesiologists were more reluctant to use low flow anaesthesia in healthy infants than in healthy adults (34%).
Performance of anaesthesia ventilators
Fifty percent of the anaesthesiologists answered that they did not know whether the CO2 absorber used in their institution contained NaOH or KOH. Forty-two percent confirmed that their absorber had one or other of these two components, and only 8% confirmed that they use NaOH/KOH-free CO2 absorbers.
Regarding fresh gas flow efficiency information displayed by ventilators, 52% of respondents said that this information was available, among which 79% actually use it in every day clinical practice. From the remaining group, 85% said that such information was not displayed, and 15% were not sure that they had it available.
Anaesthetic contribution to carbon footprint
Questions 11 to 13 investigated the practitioners’ views about the potential influence that anaesthetic practice, healthcare industry and surgical activity has on the national carbon footprint of each country. These three questions show a broad distribution of answers covering from no impact (0%) to full responsibility (100%), with 50, 49 and 52% as median values, respectively (Supplemental Figures 6S–8S).
Question 14 asked if inhaled anaesthetic drugs are regulated under the Kyoto protocol, to which 70% answered don’t know, and 15% expressed equally both yes and no.
Discussion
The healthcare industry is a major polluter worldwide, responsible for 5.2% of all global GHG emissions.7 Moreover, the operating rooms are the most resource demanding areas in hospital care and the higher energy demands, lack of effective waste management, and inhaled anaesthetic use, lead to a high intrinsic carbon footprint.7,19 Volatile anaesthetics can be responsible for 50% of the peri-operative emissions, with an increasing concern over the use of these gases in the ICU and emergency settings, and by veterinary services: these out-of-the-operating-room sites often lack efficient anaesthesia ventilators and scavenging systems.21 Therefore, it is relevant to benchmark the use of different types of anaesthetic drugs, and ascertain if there are significant correlations with the level of CO2 emissions, population wealth or healthcare expenditure. Although there are a handful of surveys dealing with sustainability during the peri-operative process, this is the first to examine the problem worldwide, with 75 participating countries. It is also the first survey that compares its gathered data with socioeconomic indicators (CO2 emissions, GDP index and healthcare expenditure).
According to our data, 64% of anaesthesiologist use halogenated gases on a daily basis during general anaesthesia maintenance, with sevoflurane ranking first, followed by propofol based TIVA / TCI (23%), and regional anaesthesia (11%). These results resemble data shown in previous studies.14–17 It is worth noting that in African countries, isoflurane, an ozone-depleting drug with a higher warming potential than sevoflurane, is as frequently used as the latter (43%). Despite its higher cost, desflurane shows a 10% preference among African anaesthesiologists, although this result can be influenced by the fact that 29% of respondents from this continent came from South Africa. Inhaled anaesthetics are used by 93% of veterinary anaesthesiologists, with isoflurane ranking first (85%). Interestingly, senior consultants (32%) choose desflurane more often than less experienced consultants (9%) or residents (7%), showing a possible exposure to marketing strategies. Strikingly, only 49% of the anaesthesiologists use low flow anaesthesia (<1.0 lpm) on a daily basis: it is used more frequently in high-income countries, probably due to better access to premium ventilators, and education programmes on sustainability and environmental health. The fact that 48% of respondents do not use, or do not have available the necessary visual displays in the ventilators, adds to this hypothesis. We also observed TIVA preference was significantly higher in countries with a higher GDP index and healthcare expenditure per capita. Possible explanation for such behaviour is again better access to technology (infusion pumps, Target-Controlled-Infusion software and EEG Neuromonitors) and education from Scientific Societies.
N2O, a gas with a high greenhouse effect and ozone-depleting properties, is still used in peri-operative medicine, especially in middle and low-income countries, probably due to its low price and unawareness of its environmental effects. More education is needed in this regard to encourage a global N2O ban, including areas outside the operating room such as in dentistry and the labour ward. Therefore, stakeholders with implemented N2O-free healthcare plans should lead the transition and share their experience.
Concerns expressed for not using low flow anaesthesia are most likely preventable by properly programming alarms (inspired CO2 and O2 levels) according to local safety protocols in order to prevent CO2 rebreathing and hypoxia. Surprisingly, Compound A related renal insufficiency still is a matter of concern for nearly 12% of the clinicians, despite lack of available evidence supporting its clinical repercussion in humans.20,21 On the contrary, only 10% believe that CO formation might have unwanted effects, which is possible if CO2 absorbers containing NaOH/KOH are used, which according to this survey, are the most prevalent worldwide. Therefore, patients at risk for exogenous (smoke inhalation, polytransfusion and children <2 years of age with anaesthetic gas recirculation >50%) or endogenous CO formation (sepsis, trauma, shock or haemolysis) might benefit from COHb monitoring in POCT gas analysis if blood sampling is available, or noninvasively by using pulse co-oximetry devices.22–24
Regarding low flow anaesthesia in paediatric population, 66% of the anaesthetists were more reluctant to apply it in healthy infants, which have a lower minute volume than healthy adults. Infants typically have less dilution effect in the gas mixture delivered by the ventilator than adults, who have higher MV and lower recirculation fraction (FGF/MV). Therefore, it is not surprising that infants are often ventilated in an ‘open circuit’ scheme due to recirculation fractions above 1 (FGF > MV), which delivers fresh nonused anaesthetic gas directly to the atmosphere. This FGF setting increases the economic and environmental burden of our practice. Therefore, we propose that FGF should never exceed the patient's minute volume, and we strongly encourage anaesthesiologists to use low flow anaesthesia even in the paediatric setting.
Our study shows a significant need for further educational programmes on environmental health and sustainability. Figures 1S to 3S depict how little knowledge there is about the impact of healthcare practice to the national carbon footprint. We strongly agree with existing recommendations to include educational initiatives both at a preclinical and clinical level.14,25,26 Furthermore, our daily anaesthetic choices are free from any audit in most centres worldwide, despite inhaled anaesthetics belonging to a cluster of chemicals (N2O and fluorinated greenhouse gases) regulated by different international protocols (Kyoto, Paris, Montreal and Kigali). Despite these facts, 70% of respondents did not know if these drugs are in fact regulated by these Conventions. Similar lack of awareness among anaesthesiologists worldwide has been previously reported.14–17
Limitations of our study include a possible selection bias where more motivated clinicians took the effort to share and respond to the survey, and social media distribution likely took place among groups of anaesthesiologists already interested in sustainability and environmental health. Moreover, many countries were under-represented, and we only obtained answers from 75 countries (from a total of 193 according to the United Nations) mainly from European and South American countries. In order to compensate for this issue and improve the applicability of our study, we grouped countries into continents, and divided their socioeconomic indexes into quintiles to compare answers from similar geographical and socioeconomic origins, instead of on purely national criteria. In fact, the number of responses is more balanced when GDP criteria are applied, with 61% of clinicians working in countries with a GDP over the median value distribution. Nevertheless, the use of professional networks and online methods to disseminate the survey may have excluded a wider participation from low-income countries. This effect becomes more evident with the fact that only 0.1% of respondents answered that they use a gas different to sevoflurane, desflurane or isoflurane on a daily basis, most probably halothane, which is still commonly used in low-income countries. Relevant countries with high CO2 emissions participated very little in this survey, especially within Asia. Further surveys in the future should strive to better describe the sustainability situation in this region.
The broad distribution of answers for questions 11 to 13 into a homogenous cloud of data might not only be interpreted as an absolute lack of knowledge about the healthcare footprint, but also because the questions were poorly understood by the participants. Should the latter be the prevailing reason, again, a lack of awareness in healthcare sustainability facts might contribute to the poor understanding of these questions.
We did not find differences in sex or experience, but the 30 to 39-year-old segment was slightly over-represented.
Conclusion
Halogen gases are the most frequently used anaesthetic drugs worldwide, and the majority of respondents are unaware of their global warming impact, or are not influenced in their anaesthetic choices by environmental concerns. There is an under-implementation of more sustainable strategies of anaesthesia, especially in countries with less access to updated technology. A clear need exists for further education and training worldwide, both at the preclinical and clinical level, in order to make informed decisions that warrant the best possible balance between patient safety and planet health. Furthermore, the availability of adequate technology is essential for both a well tolerated and low carbon care.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Acknowledgements relating to this article
Assistance with the study: the following anaesthesiologists contributed to the distribution of the survey. Without their help, this project would not have been possible.
Gabriela Alcaraz Diez-Tejedor, Monica Hervías Sanz, Silvana Cavallieri, Waldo Merino, Cecilia Acosta, Anna Camporesi, Lucian Covaciu, José Ignacio Redondo, Javier Benito, Federico Bilotta, Gordana Jovanovic.
Financial support and sponsorship: none.
Conflicts of interest: PGP reported no conflicts of interest directly related to this Project. Unrelated to this project, PGP received lecture fees from Mindray, Vygon and Baxter.
SK reported no conflicts of interest directly related to this Project. Unrelated to this project, SK received a grant from the German research foundation, is an inventor of two EEG-based patents being sold to Medtronic and received lecture fees from Medtronic.
JM reported no conflicts of interest directly related to this Project. Unrelated to this project, JM received lecture fees from Aguettant Laboratories.
AT, JDS and FRB have no conflicts to declare.
LB reported no conflicts of interest directly related to this Project. Unrelated to this project, LB received consultancy fees for advisory boards from Gilead and Janssen, and for scientific expert opinion for B-Braun and Siare.
FRB and JDS have no conflicts of interest to declare.
MMRFS reported no conflicts of interest directly related to this Project. Unrelated to this project, his research group/department received (over the last 3 years) research grants and consultancy fees from Masimo (Irvine, California, USA), Becton Dickinson (Eysins, Switzerland), Fresenius (Bad Homburg, Germany), Dräger (Lübeck, Germany), Paion (Aachen, Germany), Medcaptain Europe (Andelst, The Netherlands).
Prior presentations: Partial results were presented at the Chilean Society of Anaesthesia National Congress: OR Sustainability status in Chile. On-line live presentation. 12 November 2021.
SEDAR National Congress: OR Sustainability status in Spain. Santiago de Compostela (Spain). 22 April 2022.
SMART Meeting (Italian Society of Anaesthesia and Intensive Care) Congress: OR Sustainability status in Italy. Milano (Italy). 5 May 2022.
14th Serbian National Congress of Anaesthesia: OR Sustainability status in Eastern Europe. Belgrade (Serbia). 30 September 2022.
Ethical approval was obtained (Ethical Committee N° PI-4630) from La Paz University Hospital Ethics Committee, Madrid, Spain (Chairperson Prof A. Castro Conde) on 23 March 2021. Principal Investigator: Dr Patricio González-Pizarro.
The European Society of Anaesthesia and Intensive Care (ESAIC) Endorsement: 9 June 2021.
The Spanish Society of Anaesthesia and Intensive Care (SEDAR) Endorsement: 23 June 2021.
This manuscript was handled by Patrice Forget.
Footnotes
Supplemental digital content is available for this article.
References
- 1. Shukla J, Skea R, Slade A, et al. IPCC, 2022: climate change 2022: mitigation of climate change. Contribution of Working Group III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change P.R. Cambridge, UK and New York, NY, USA: Cambridge University Press. p.7. [Google Scholar]
- 2. Shukla J, Skea R, Slade A, et al. IPCC, 2022: climate change 2022: mitigation of climate change. Contribution of Working Group III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change P.R. Cambridge, UK and New York, NY, USA: Cambridge University Press. p.5. [Google Scholar]
- 3. Shukla J, Skea R, Slade A, et al. IPCC, 2022: climate change 2022: mitigation of climate change. Contribution of Working Group III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change P.R. Cambridge, UK and New York, NY, USA: Cambridge University Press. p. 15. [Google Scholar]
- 4. Shukla J, Skea R, Slade A, et al. IPCC, 2022: climate change 2022: mitigation of climate change. Contribution of Working Group III to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change P.R. Cambridge, UK and New York, NY, USA: Cambridge University Press. p.24. [Google Scholar]
- 5. Pichler P, Jaccard I, Weisz U, Weisz H. International comparison of healthcare carbon footprints. Environ Res Lett 2019; 14:1–8.35340667 [Google Scholar]
- 6. Boyd R, Ashby B, Steele K (ARUP), et al. (Healthcare without harm) healthcare's climate footprint – how the health sector contributes to the global climate crisis and opportunities for action, 2019, p. 8. https://www.arup.com/perspectives/publications/research/section/healthcares-climate-footprint. [Accessed 20th January 2023] [Google Scholar]
- 7. Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet 2021; 398:1619–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sherman J. A different perspective on anaesthetics and climate change response. Anesth Analg 2013; 116:734–735. [DOI] [PubMed] [Google Scholar]
- 9. Andersen MPS, Nielsen OJ, Wallington TJ, et al. Assessing the impact on global climate from general anesthetic gases. Anesth Analg 2012; 114:1081–1085. [DOI] [PubMed] [Google Scholar]
- 10. Devlin-Hegedus JA, McGain F, Harris RD, Sherman JD. Action guidance for addressing pollution from inhalational anaesthetics. Anaesthesia 2022; 77:1023–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability within anaesthesia and critical care. Br J Anaesth 2020; 125:680–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 2017; 1:e381–e388. [DOI] [PubMed] [Google Scholar]
- 13. Vollmer MK, Rhee TS, Rigby M, et al. Modern inhalation anaesthetics: potent greenhouse gases in the global atmosphere. Geophys Res Lett 2015; 42:1606–1611. [Google Scholar]
- 14. Koch S, Samwer C, Rossaint R, et al. for the DGAI/BDA Commission on Sustainability in Anaesthesiology, Survey regarding routine use of anaesthetic techniques and knowledge of their environmental impact in Germany 2020. Eur J Anaesthesiol 2022; 39:277–286. [DOI] [PubMed] [Google Scholar]
- 15. McGain F, Bishop JR, Elliot-Jones LM, et al. A survey of the choice of general anaesthetic agents in Australia and New Zealand. Anaesth Intensive Care 2019; 47:235–241. [DOI] [PubMed] [Google Scholar]
- 16. Amma RO, Ravindran S, Koshy RC, et al. A survey on the use of low 4 flow anaesthesia and the choice of inhalational anaesthetic agents among anaesthesiologists of India. Indian J Anaesth 2016; 60:751–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Benhamou D, Constant I, Longrois D, et al. Use of volatile anaesthetic agents in anaesthesia: a survey of practice in France in 2012. Anaesth Crit CarePain Med 2015; 34:205–209. [DOI] [PubMed] [Google Scholar]
- 18. MacNeill AJL, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 2017; 1:e381–e388. [DOI] [PubMed] [Google Scholar]
- 19. Sherman JD, Chesebro BB. Inhaled anaesthesia and analgesia contribute to climate change. BMJ 2022; 377:o1301. [DOI] [PubMed] [Google Scholar]
- 20. Kharasch ED, Frink EJ, Jr, Zager R, et al. Assessment of low-flow sevoflurane and isoflurane effects on renal function using sensitive markers of tubular toxicity. Anesthesiology 1997; 86:1238–1253. [DOI] [PubMed] [Google Scholar]
- 21. Sondekoppam RV, Narsingani KH, Schimmel TA, et al. The impact of sevoflurane anesthesia on postoperative renal function: a systematic review and meta-analysis of randomized-controlled trials. Can J Anaesth 2020; 67:1595–1623. [DOI] [PubMed] [Google Scholar]
- 22. Barker SJ, Curry J, Redford D, Morgan S. Measurement of carboxyhemoglobin and methemoglobin by pulse oximetry: a human volunteer study. Anesthesiology 2006; 105:892–897. [DOI] [PubMed] [Google Scholar]
- 23. Levy RJ. Anesthesia-related carbon monoxide exposure: toxicity and potential therapy. Anesth Analg 2016; 123:670–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nasr V, Emmanuel J, Deutsch N. Carbon monoxide re-breathing during low-flow anaesthesia in infants and children. Br J Anaesth 2010; 105:836–841. [DOI] [PubMed] [Google Scholar]
- 25. General Medical Council. Outcomes for graduates. 2019. https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates/outcomes-for-graduates. [Accessed August 2022]. [Google Scholar]
- 26. White SM, Shelton CL, Gelb AW, et al. representing the World Federation of Societies of Anaesthesiologists Global Working Group on Environmental Sustainability in Anaesthesia. Principles of environmentally-sustainable anaesthesia: a global consensus statement from the World Federation of Societies of Anesthesiologists. Anaesthesia 2022; 77:201–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.